1e4a681991784b698d121fdd196191dd.ppt
- Количество слайдов: 90
Femur and Tibia Fractures Kevin E. Coates, M. D. , M. P. T.

Worker’s Compensation? 2
Femoral Neck Fractures • Epidemiology • 250, 000 Hip fractures annually – Expected to double by 2050 • At risk populations – Elderly: poor balance&vision, osteoporosis, inactivity, medications, malnutrition • incidence doubles with each decade beyond age 50 – higher in white population – Other factors: smokers, small body size, excessive caffeine & ETOH – Young: high energy trauma 3
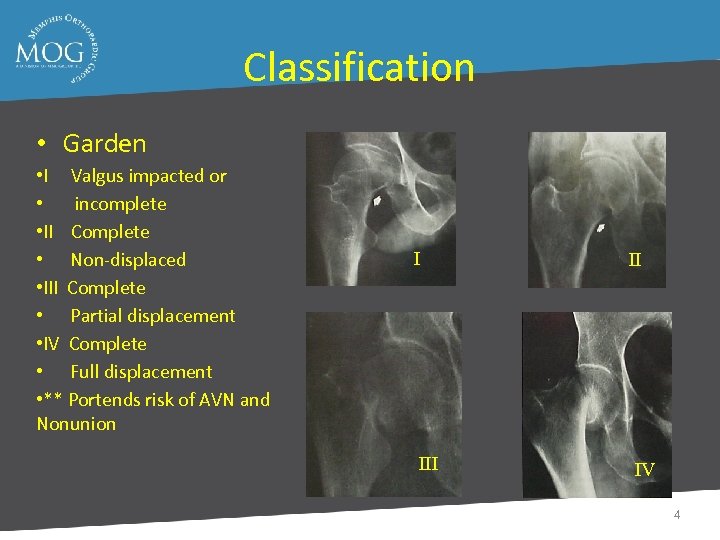
Classification • Garden • I Valgus impacted or • incomplete • II Complete • Non-displaced • III Complete • Partial displacement • IV Complete • Full displacement • ** Portends risk of AVN and Nonunion I II IV 4
Treatment • Goals – Improve outcome over natural history – Minimize risks and avoid complications – Return to pre-injury level of function – Provide cost-effective treatment 5
Treatment Decision Making Variables • Patient Characteristics – Young (arbitrary physiologic age < 65) • High energy injuries – Often multi-trauma – Elderly • Lower energy injury • Comorbidities • Pre-existing hip disease 6
Treatment Young Patients (Arbitrary physiologic age < 65) – Non-displaced fractures • At risk for secondary displacement • Urgent ORIF recommended – Displaced fractures • • Patients native femoral head best AVN related to duration and degree of displacement Irreversible cell death after 6 -12 hours Emergent ORIF recommended 7
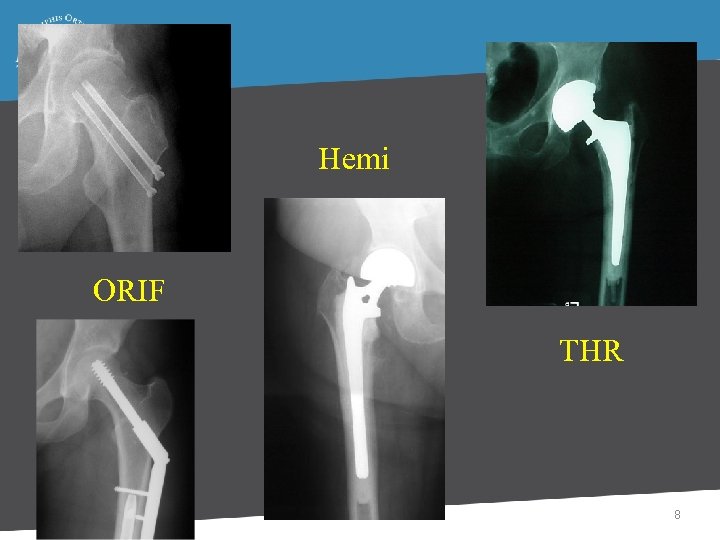
Hemi ORIF THR 8
Non-displaced Fractures • ORIF standard of care • Predictable healing – Nonunion < 5% • Minimal complications – AVN < 8% – Infection < 5% • Relatively quick procedure – Minimal blood loss 9
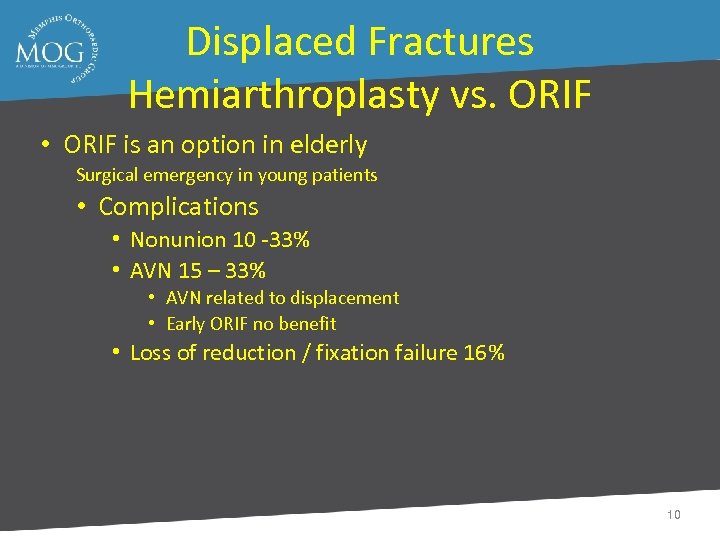
Displaced Fractures Hemiarthroplasty vs. ORIF • ORIF is an option in elderly Surgical emergency in young patients • Complications • Nonunion 10 -33% • AVN 15 – 33% • AVN related to displacement • Early ORIF no benefit • Loss of reduction / fixation failure 16% 10
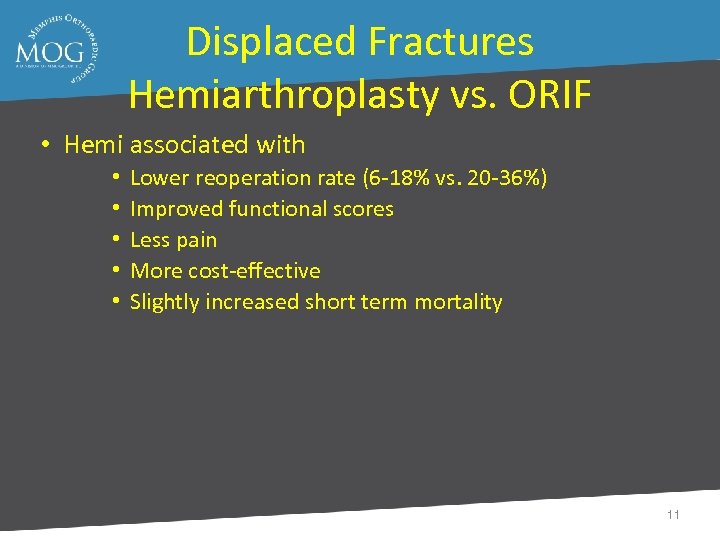
Displaced Fractures Hemiarthroplasty vs. ORIF • Hemi associated with • • • Lower reoperation rate (6 -18% vs. 20 -36%) Improved functional scores Less pain More cost-effective Slightly increased short term mortality 11
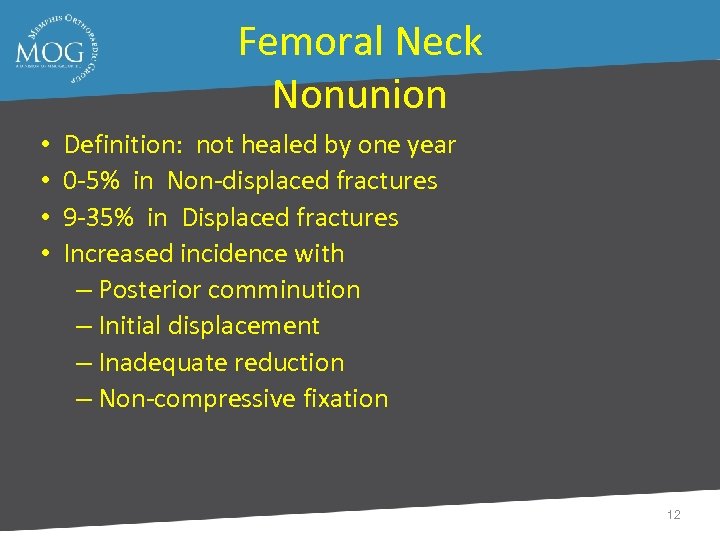
Femoral Neck Nonunion • • Definition: not healed by one year 0 -5% in Non-displaced fractures 9 -35% in Displaced fractures Increased incidence with – Posterior comminution – Initial displacement – Inadequate reduction – Non-compressive fixation 12
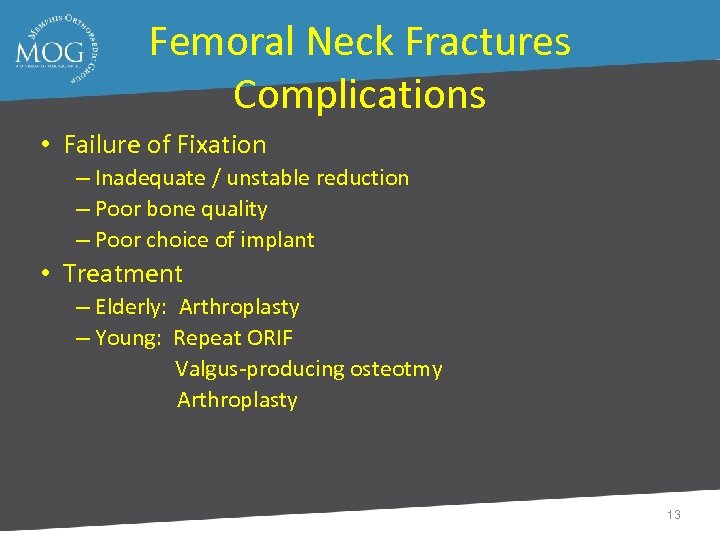
Femoral Neck Fractures Complications • Failure of Fixation – Inadequate / unstable reduction – Poor bone quality – Poor choice of implant • Treatment – Elderly: Arthroplasty – Young: Repeat ORIF Valgus-producing osteotmy Arthroplasty 13
Femoral Neck Fractures Complications • Post-traumatic arthrosis • Joint penetration with hardware • AVN related • Blood Transfusions – THR > Hemi > ORIF – Increased rate of post-op infection • DVT / PE – Multiple prophylactic regimens exist • One-year mortality 14 -50% 14
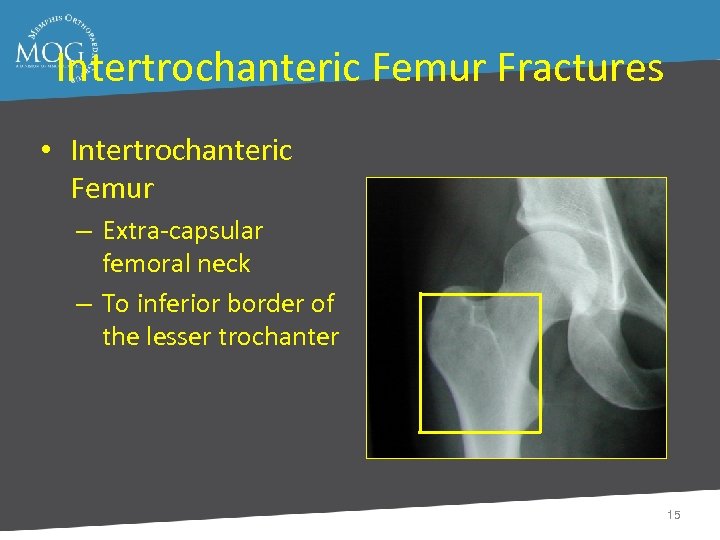
Intertrochanteric Femur Fractures • Intertrochanteric Femur – Extra-capsular femoral neck – To inferior border of the lesser trochanter 15
Etiology • Osteoperosis • Low energy fall – Common • High Energy – Rare 16
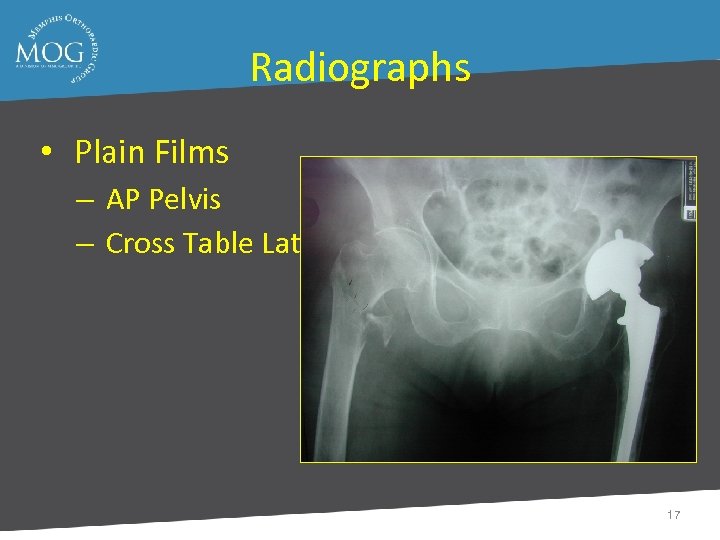
Radiographs • Plain Films – AP Pelvis – Cross Table Lateral 17

Goals of Treatment • Obtain a Stable Reduction • Internal Fixation – Good Position – Mechanically Adequate • Permit Immediate Transfers & Early Ambulation 18
Rehabilitation • Mobilize – Weight Bearing As Tolerated – Cognitive Intact Patients Auto Protect – Unstable Fractures = Less WB – Stable Fractures = More WB • No Difference @ 6 weeks Post op 19
Femoral Shaft Fractures • • • Common injury due to major violent trauma 1 femur fracture/ 10, 000 people More common in people < 25 yo or >65 yo Femur fracture leads to reduced activity for 107 days Motor vehicle, motorcycle, auto-pedestrian, aircraft, and gunshot wound accidents are most frequent causes 20
Femur Fracture Management • Initial traction with portable traction splint or transosseous pin and balanced suspension • Evaluation of knee to determine pin placement • Timing of surgery is dependent on: – Resuscitation of patient – Other injuries - abdomen, chest, brain – Isolated femur fracture 21
Femur Fracture Management • Antegrade nailing is still the gold standard • Antegrade nailing problems: – Varus alignment of proximal fractures – Trendelenburg gait – Can be difficult with obese or multiply injured patients 22
Femur Fracture Management • Retrograde nailing has advantages – Easier in large patients to find starting point – Better for combined fracture patterns (ipsilateral femoral neck, tibia, acetabulum) • Retrograde nailing has its problems: – Intra-articular starting point 23
Femur Fracture Complications • • • Hardware failure Nonunion - less than 1 -2% Malunion - shortening, malrotation, angulation Infection Neurologic, vascular injury Heterotopic ossification 24
Ipsilateral Femoral Neck & Shaft Fractures • Optimum fixation of the femoral neck should be the goal • Varus malunion of the femoral neck is not uncommon, osteotomies can lead to poor results • Vertical femoral neck fracture seen in 26 -59% of cases • Rate of avascular necrosis is low, 3%, even when missed 25
Tibial Plateau Fractures • Mechanism of Injury • Mean age in most series of tibial plateau fractures is about 55 years – Large percentage over age 60 • Elderly population is increasing in numbers 26
Mechanism of Injury • Mechanism of injury is fall from standing height in most patients – MVA is increasing as % of fractures • Most common fracture pattern is splitdepressed fracture of lateral tibial plateau (80% of fractures) 27
Physical Exam • Neurologic exam – peroneal nerve! • Vascular exam – popliteal artery and medial plateau injuries – beware the of the knee dislocation posing as a fracture – beware of posteriorly displaced fracture fragments – ABI <0. 9 urgent arterial study 28
Physical Exam • Compartment syndrome • KNEE STABILITY – varus/valgus in full extension – may require premedication • aspiration of knee effusion/hematoma • replace with lidocaine+marcaine 29

Evaluation of Soft Tissues • Proximal and distal tibia subcutaneous • Soft tissue remains compromised for at least 7 days • Early ORIF risks wound slough exposed hardware 30
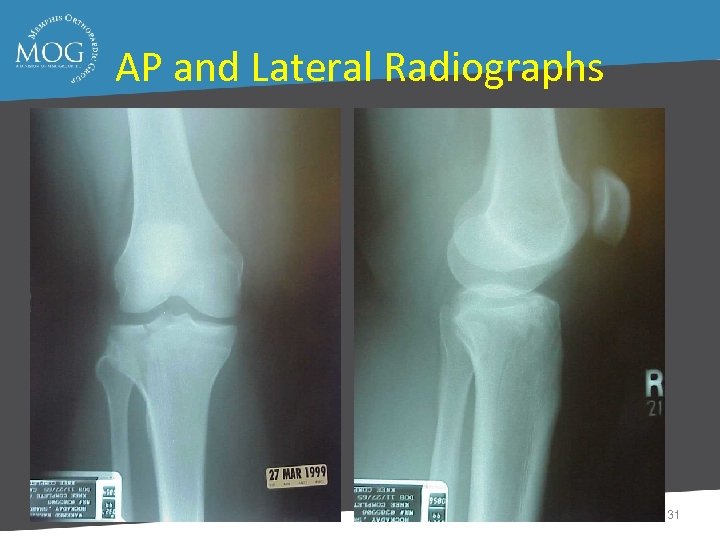
AP and Lateral Radiographs 31

Pre-traction 32
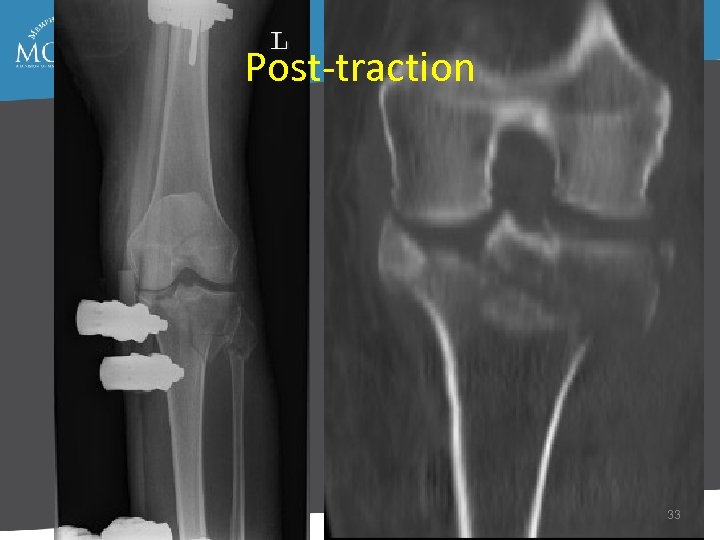
Post-traction 33
Computed Tomography • Indications – Fracture in an active patient for which you are considering nonsurgical care – Complex fracture – To aid surgical planning of approach, technique, screw position, etc. 34
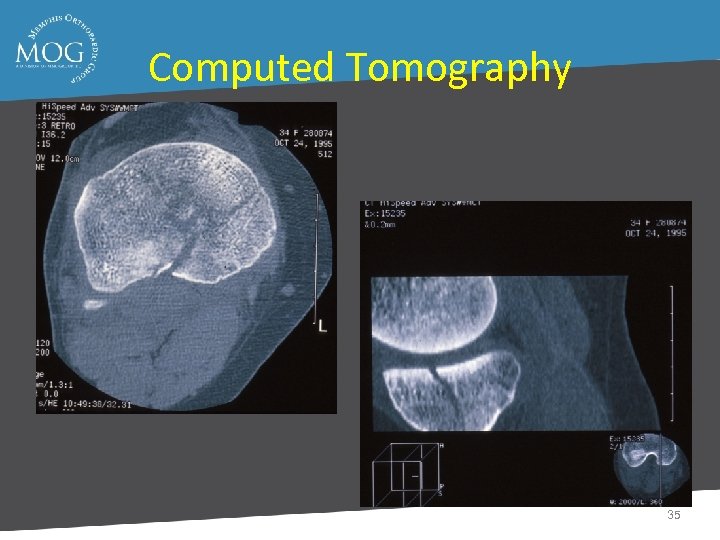
Computed Tomography 35
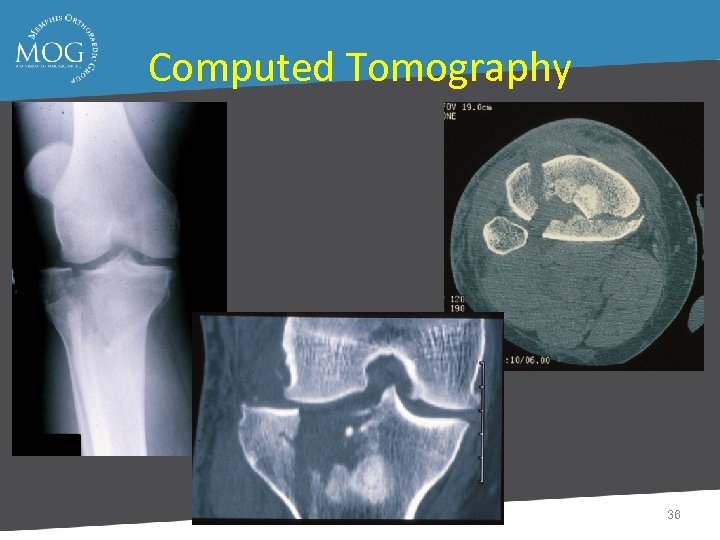
Computed Tomography 36
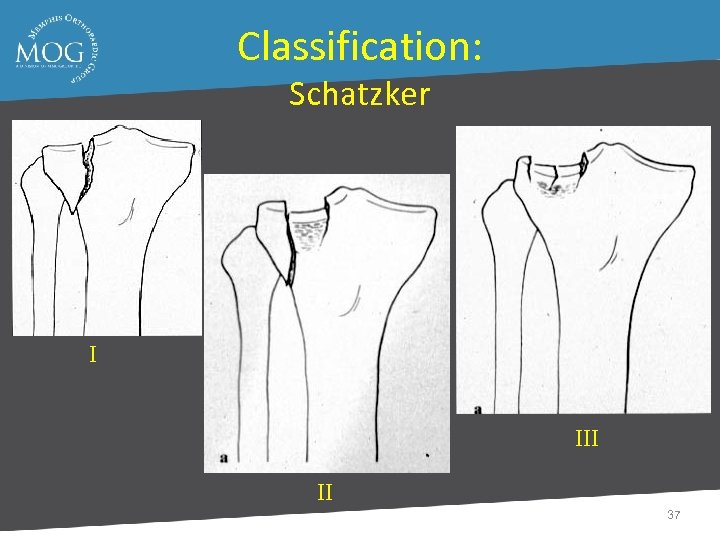
Classification: Schatzker I II 37
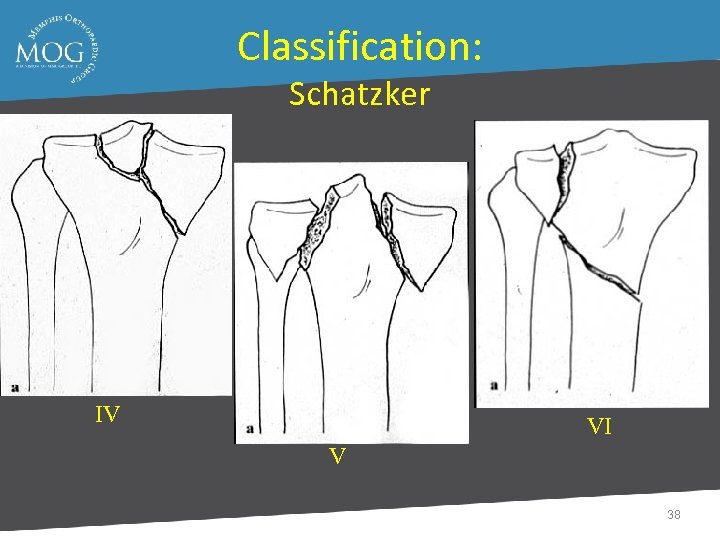
Classification: Schatzker IV VI V 38
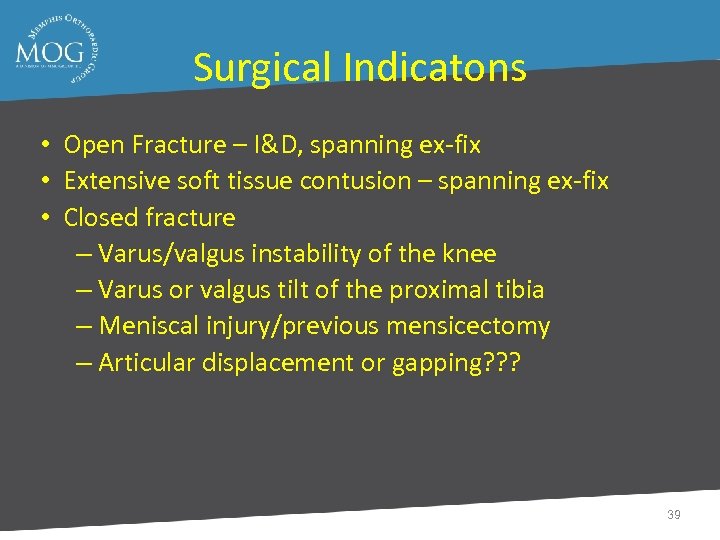
Surgical Indicatons • Open Fracture – I&D, spanning ex-fix • Extensive soft tissue contusion – spanning ex-fix • Closed fracture – Varus/valgus instability of the knee – Varus or valgus tilt of the proximal tibia – Meniscal injury/previous mensicectomy – Articular displacement or gapping? ? ? 39
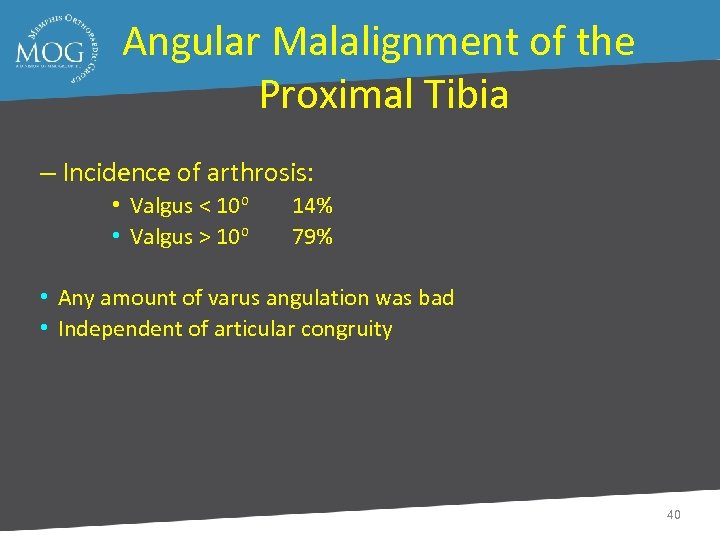
Angular Malalignment of the Proximal Tibia – Incidence of arthrosis: • Valgus < 10 o • Valgus > 10 o 14% 79% • Any amount of varus angulation was bad • Independent of articular congruity 40
Meniscectomy – Higher rate of arthrosis in patients who had undergone meniscectomy at surgery – 70% arthrosis in patients who had undergone meniscectomy – results independent of the amount of articular incongruity 41
Postoperative Management • Immediate PROM/AROM of knee • Routine Pin site care (if ex-fix) • TDWB for 8 -12 weeks 42
Outcomes • Outcome depends on: – Varus valgus stability of the knee – Varus/valgus alignment of the proximal tibia – Presence of an intact meniscus – Articular congruity (to a lesser extent) 43
Treatment Goals • Focus on restoring stability and proximal tibial alignment to the knee, rather than restoring anatomic alignment of the articular surface at all costs • Use minimally invasive techniques, when possible • Other techniques are preferable to hybrid ex-fix • MOVE THE KNEE EARLY IN ALL PATIENTS! 44
Tibial Shaft Fractures Mechanism of Injury ● Can occur in lower energy, torsional type injury (eg, skiing) ● More common with higher energy direct force (eg car bumper) 45
Physical Exam • Soft tissue injury with high-energy crush mechanism may take several days to fully declare itself • Repeated exam often necessary to follow compartment swelling 46
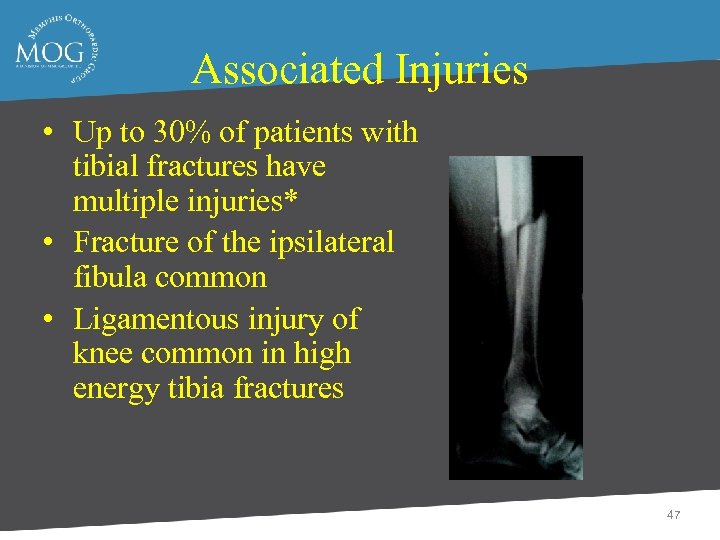
Associated Injuries • Up to 30% of patients with tibial fractures have multiple injuries* • Fracture of the ipsilateral fibula common • Ligamentous injury of knee common in high energy tibia fractures 47
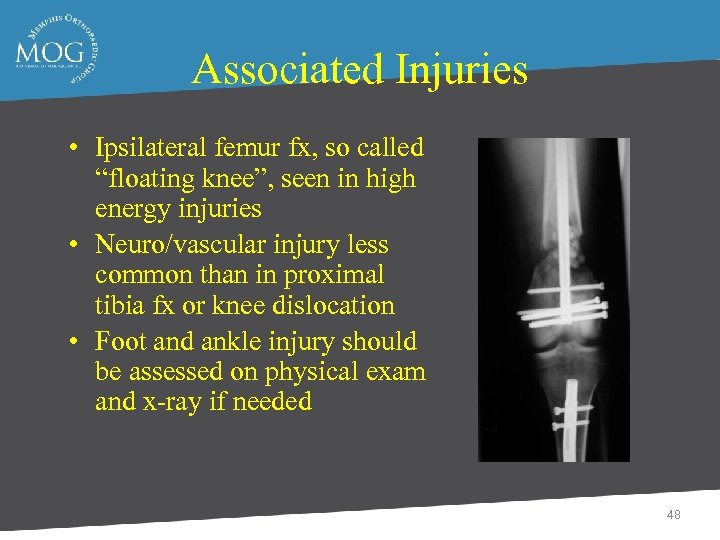
Associated Injuries • Ipsilateral femur fx, so called “floating knee”, seen in high energy injuries • Neuro/vascular injury less common than in proximal tibia fx or knee dislocation • Foot and ankle injury should be assessed on physical exam and x-ray if needed 48
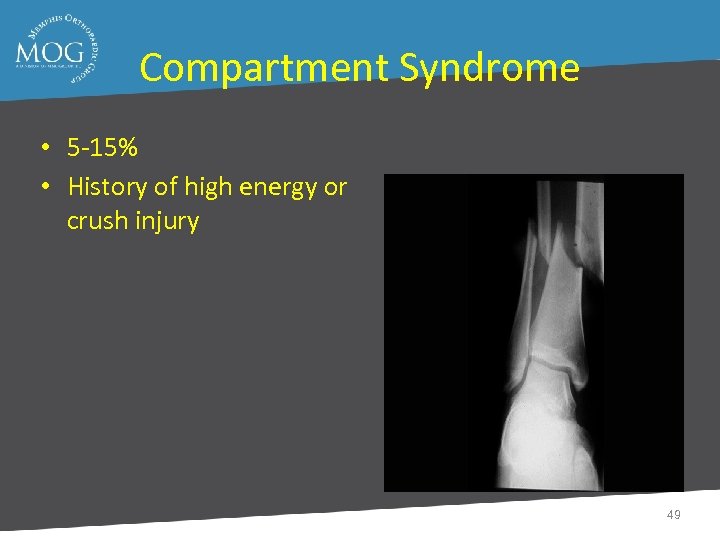
Compartment Syndrome • 5 -15% • History of high energy or crush injury 49
Nerve is the Tissue most Sensitive to Ischemia • PAIN first Symptom • PAIN with Passive Stretch first Sign 50

Each Compartment has Specific Innervation • • Ant Comp Deep- - Peroneal Lateral -Sup Peroneal N. Deep Post. - Tibial N. Sup Post. - Sural N. 51
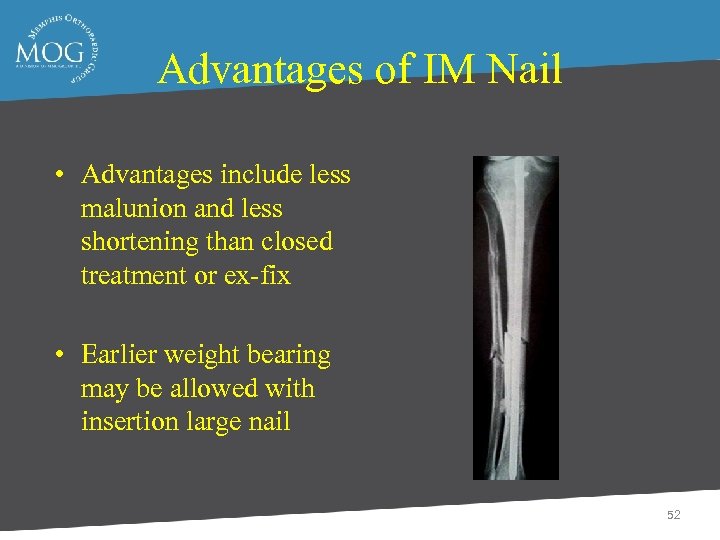
Advantages of IM Nail • Advantages include less malunion and less shortening than closed treatment or ex-fix • Earlier weight bearing may be allowed with insertion large nail 52
• Proximal Fractrues are technically more challenging • Prone to Valgus & Pro-curvatum deformities 53

54
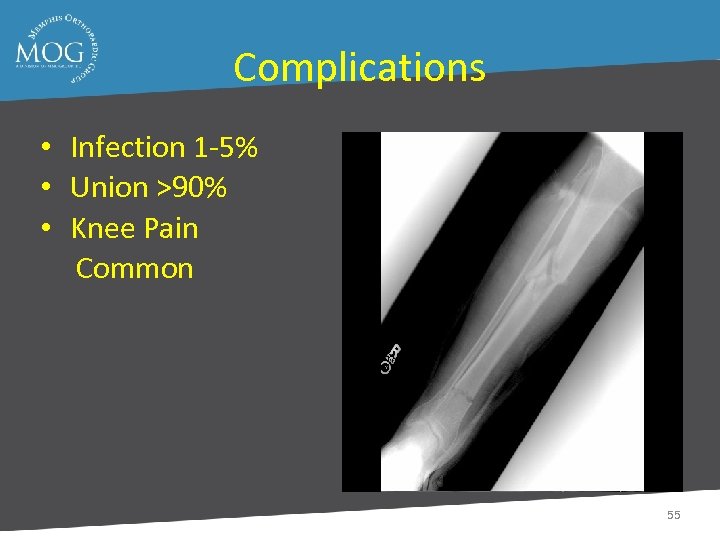
Complications • Infection 1 -5% • Union >90% • Knee Pain Common 55
Knee Pain • Severe 9% • Moderate 22% • Mild 68% • Kneeling 92% • Running 57% • Rest 37% 56
Nail Removal • Resolved 27% • No - 20% 57
Disadvantages of IM Nail • Disadvantages include anterior knee pain (up to 56. 2% *), risk of infection 58
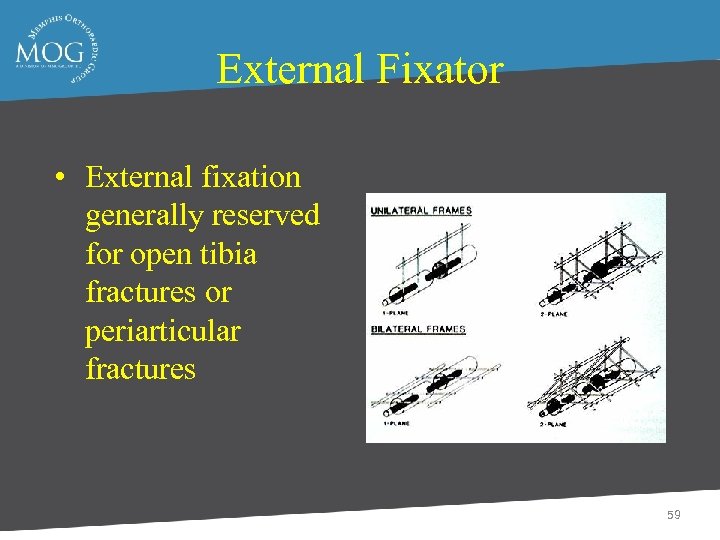
External Fixator • External fixation generally reserved for open tibia fractures or periarticular fractures 59
Disadvantages of External Fixator • Increased incidence of malunion compared to IM nail • Risk of pin tract infection, cellulitis 60
Outcomes of External Fixation • 95% union rate has been reported for group of closed and open tibia fractures, but 20% malunion rate* • Most common complications are pin track infections and malunion • Loss of reduction associated with removing frame prior to union 61
Open Tibia Fractures ● Open fractures of the tibia are more common than in any other long bone ● Rate of tibial diaphysis fractures reported from 2 per 1000 population to 2 per 10, 000 and of these approximately one fourth are open tibia fractures* 62
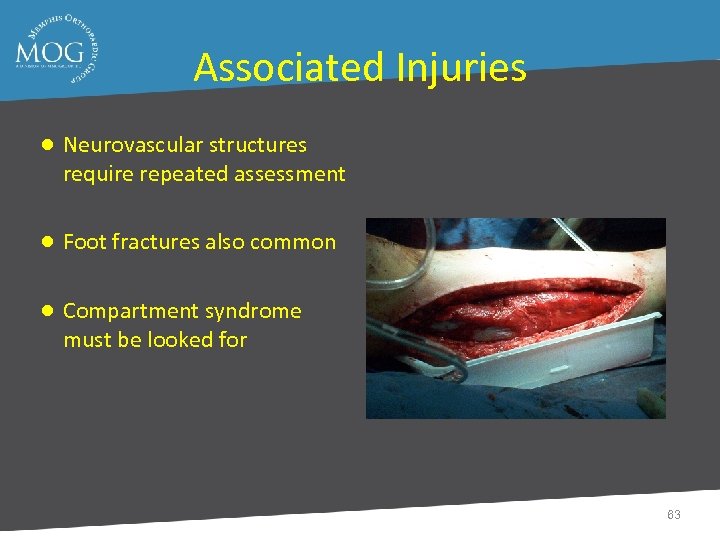
Associated Injuries ● Neurovascular structures require repeated assessment ● Foot fractures also common ● Compartment syndrome must be looked for 63
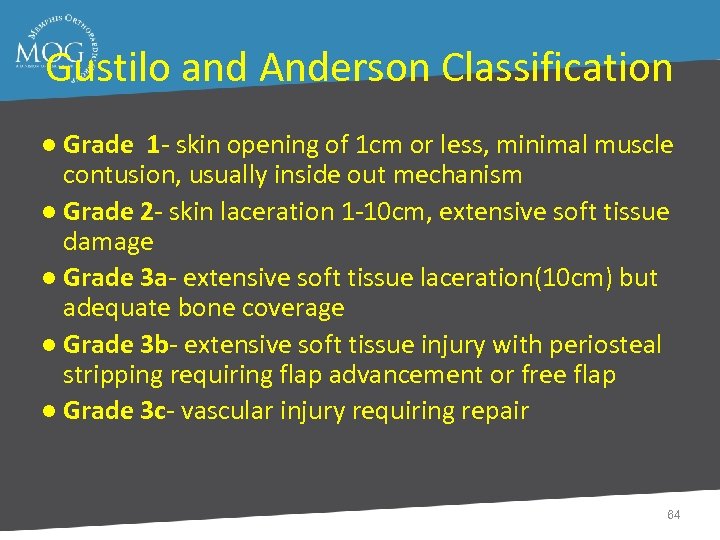
Gustilo and Anderson Classification ● Grade 1 - skin opening of 1 cm or less, minimal muscle contusion, usually inside out mechanism ● Grade 2 - skin laceration 1 -10 cm, extensive soft tissue damage ● Grade 3 a- extensive soft tissue laceration(10 cm) but adequate bone coverage ● Grade 3 b- extensive soft tissue injury with periosteal stripping requiring flap advancement or free flap ● Grade 3 c- vascular injury requiring repair 64
Objectives Prevent Sepsis ● Union ● Function ● 65
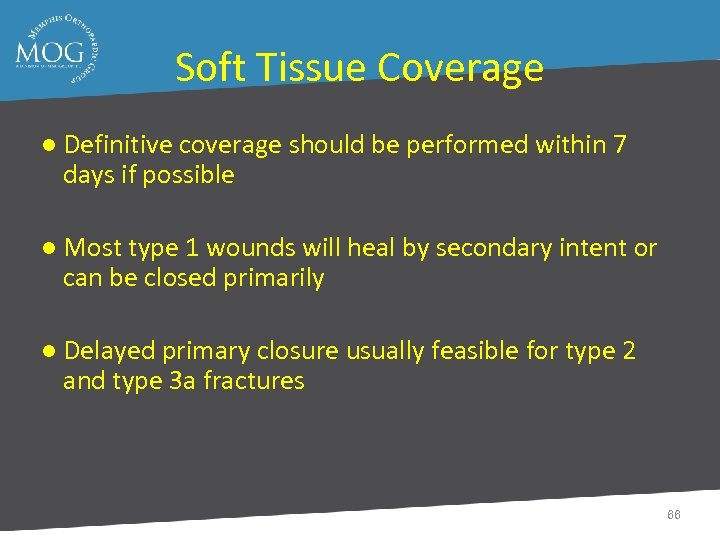
Soft Tissue Coverage ● Definitive coverage should be performed within 7 days if possible ● Most type 1 wounds will heal by secondary intent or can be closed primarily ● Delayed primary closure usually feasible for type 2 and type 3 a fractures 66
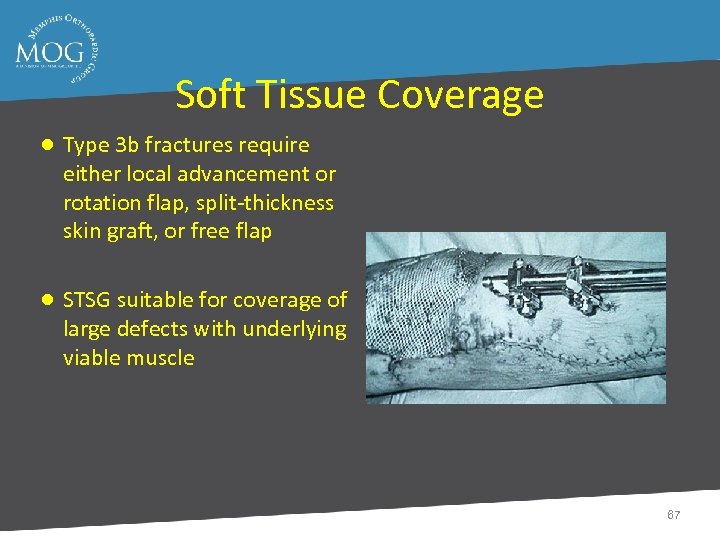
Soft Tissue Coverage ● Type 3 b fractures require either local advancement or rotation flap, split-thickness skin graft, or free flap ● STSG suitable for coverage of large defects with underlying viable muscle 67
Soft Tissue Coverage ● Proximal third tibia fractures can be covered with gastrocnemius rotation flap ● Middle third tibia fractures can be covered with soleus rotation flap ● Distal third fractures usually require free flap for coverage 68
Amputation ● In general amputation performed when limb salvage poses significant risk to patient survival, when functional result would be better with a prosthesis, and when duration and course of treatment would cause intolerable psychological disturbance 69
Complications ● Nonunion ● Malunion ● Infection- deep and superficial ● Compartment syndrome ● Fatigue fractures ● Hardware failure 70
Nonunion ● Time limits vary from 6 months to one year ● Fracture shows no radiologic progress toward union over 3 month period ● Important to rule out infection 71
Malunion ● In general varus malunion more of a problem than valgus ● For symptomatic patients with significant deformity treatment is osteotomy 72

Deep Infection ● Often presents with increasing pain, wound drainage, or sinus formation ● Treatment involves debridement, stabilization (often with ex-fix), coverage with healthy tissue including muscle flap if needed, IV antibiotics, delayed bone graft of defect if needed 73
Superficial Infection ● Most superficial infections respond to elevation of extremity and appropriate antibiotics (typically gram + cocci coverage) ● If uncertain whether infection extends deeper and/or it fails to respond to antibiotic treatment, then surgical debridement with tissue cultures necessary 74
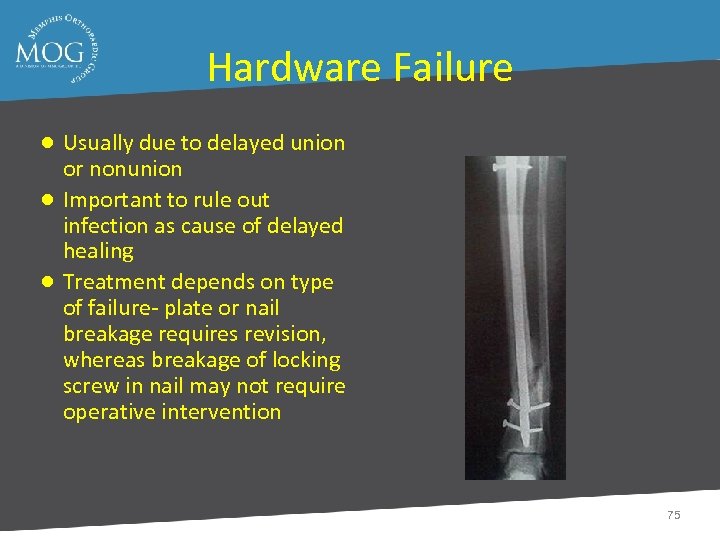
Hardware Failure ● Usually due to delayed union or nonunion ● Important to rule out infection as cause of delayed healing ● Treatment depends on type of failure- plate or nail breakage requires revision, whereas breakage of locking screw in nail may not require operative intervention 75
Outcomes ● Outcome most affected by severity of soft tissue and neurovascular injury ● Most studies show major change in results between type 3 a and 3 b/c fractures ● For type 3 b and 3 c fractures early soft tissue coverage gives best results 76
Tibial Plafond Fractures • • • Terrible Injuries “Excellent Results” rarely achieved Fair to Good Results are the Norm Outcomes are Impossible to Predict Avoid Treatment Complications 77
Treatment Principles • • Delay Until Definitive Surgery Spanning External Fixation Pecutaneous and Limited Approaches Plating Fibula 78

79

80
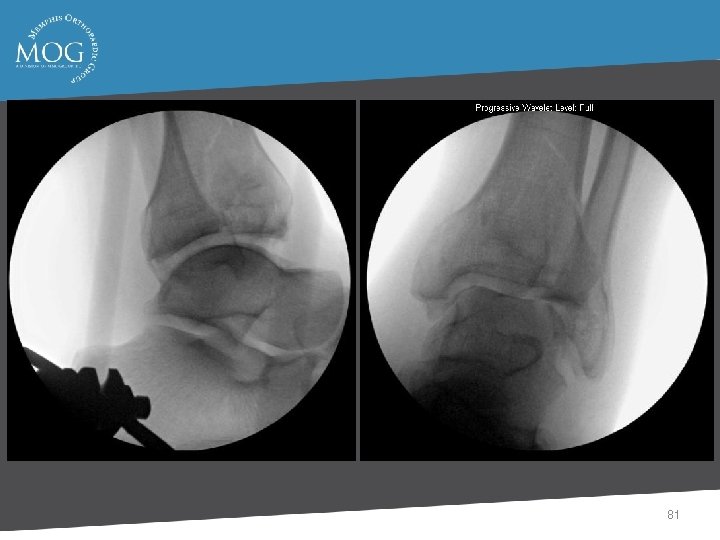
81

82

83

84
Surgical Delay with External Fixation • • • Maintains Length and Aligment Better Imaging Studies Allows Mobilization Pre-Operative Planning Allows Soft Tissue Recovery 85
Plating of Fibula Fracture • Fibular length • Articular reconstruction • Early motion 86
Outcomes • Most Have Some Pain • Most Return to Work • Detectable Arthritis in 50% 87
Outcomes - Pain • 50% Minimal • 35% Pain with WB • 15% Continuous 88

Long Term Outcome • 5 - 11 Years • Most Have Some Degree of Ankle Pain • Most Cannot Run or Play Sports • 70% with Moderate to Severe Arthritis • Most Rate Their Outcome as Good 89
Summary • Bad Injuries with Unpredictable Outcomes • Complications in 10% or Less • Results Generally not Great but not Bad if no Complications 90
1e4a681991784b698d121fdd196191dd.ppt