Excitability and excitation. Characteristics of excitable tissues. Biophysics

Excitability and excitation. Characteristics of excitable tissues. Biophysics of membranes and muscle contraction.
Franklin drew 'electric fluid' out of a thundercloud Benjamin Franklin saw the connection between the tiny electric sparks from a sulfur ball and the huge sparks of lightning – they were both flows of electric "fluid." He proved his point in his famous experiment where the moist cord from a kite flying in a thundercloud conveyed the electrical charge in the thundercloud to earth.
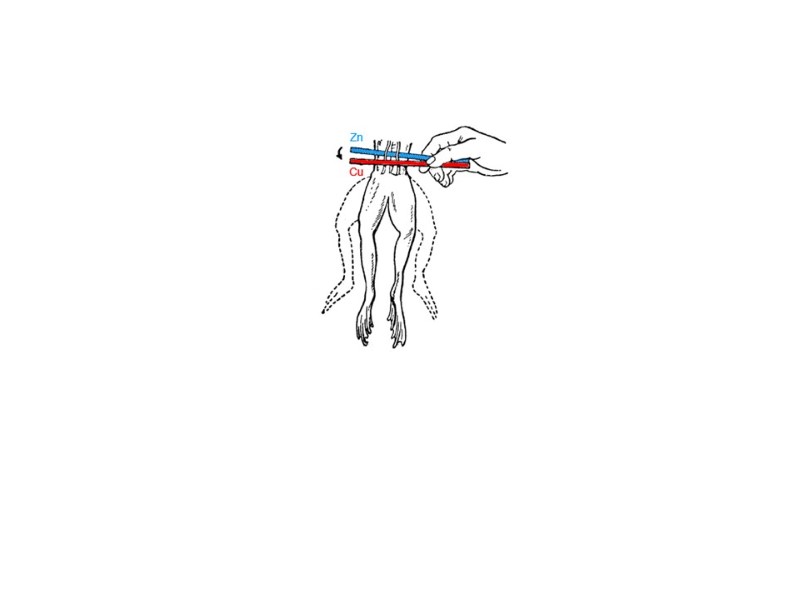
The Italian Galvani made another important, though accidental, discovery toward the end of the 18th century. He found that wires of brass and iron in contact with the leg of a recently killed frog made its muscles contract, as they contracted when the store of electricity from a Leyden jar was passed through the leg. Galvani thought that the leg had, in some mysterious way, produced electricity on its own.


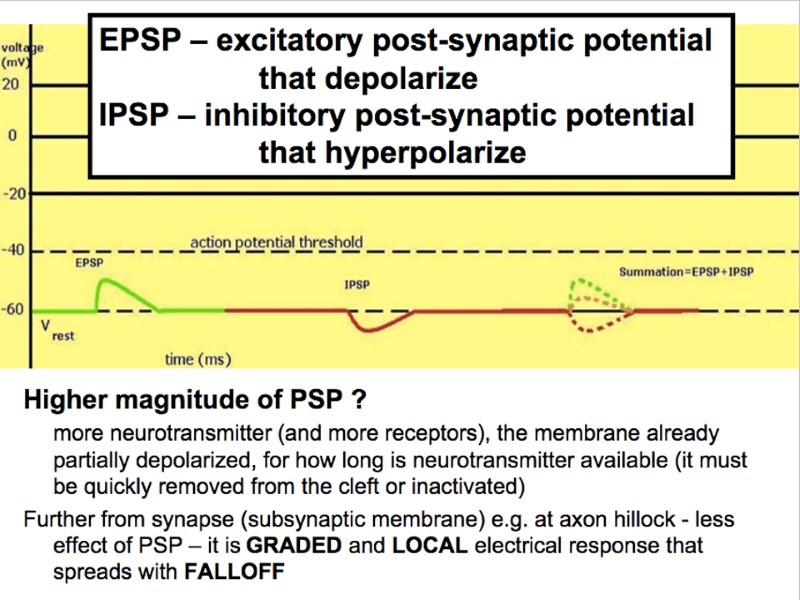
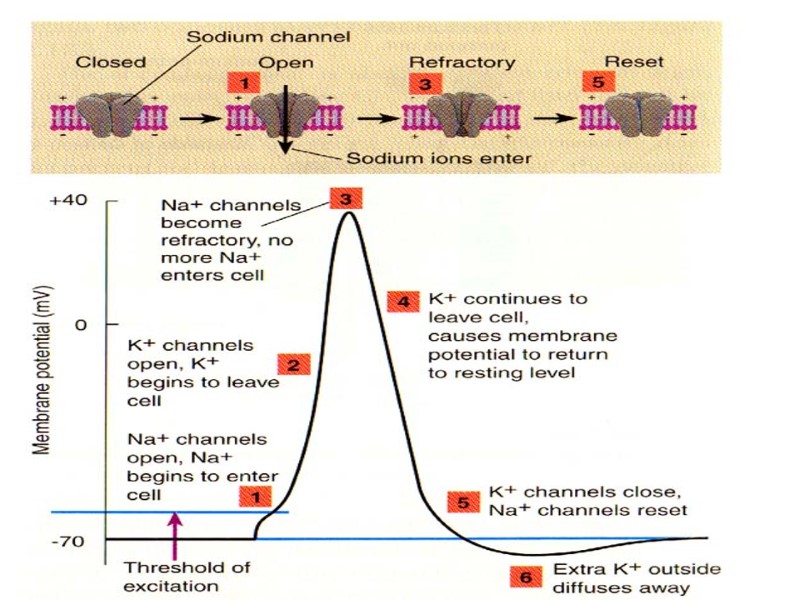
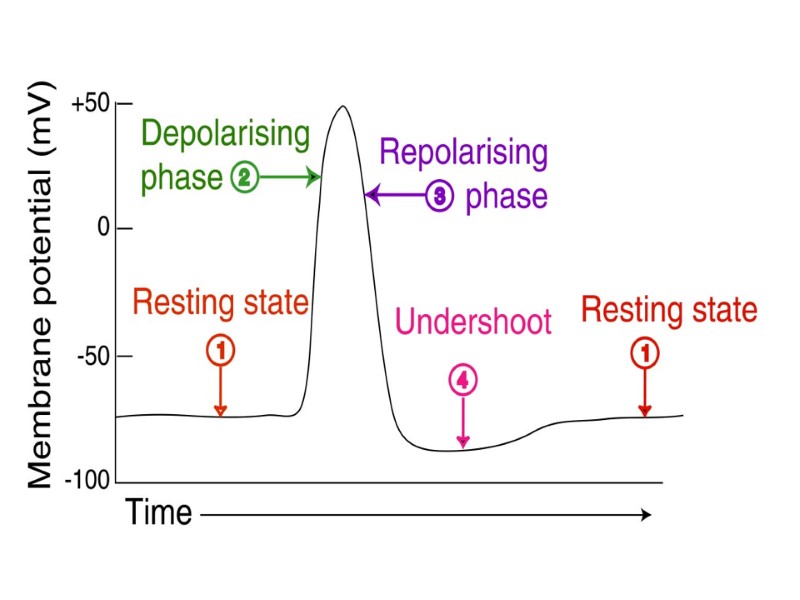
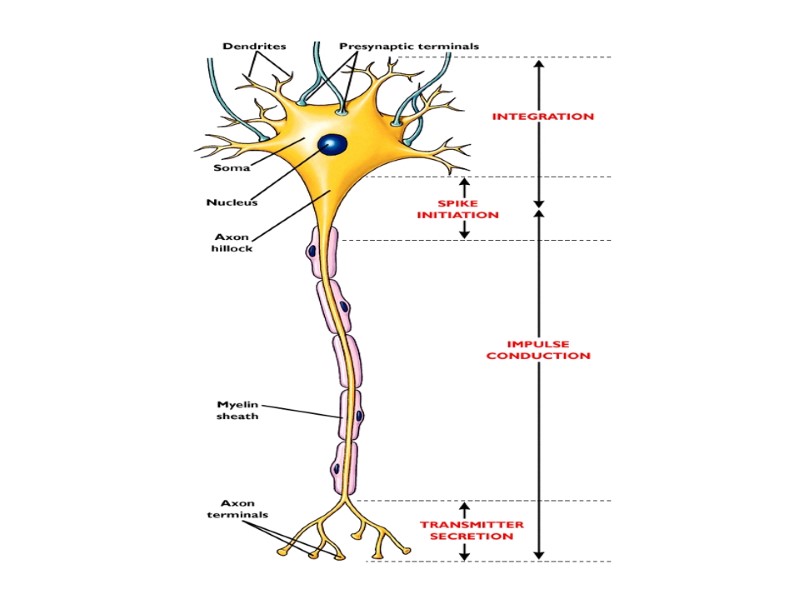
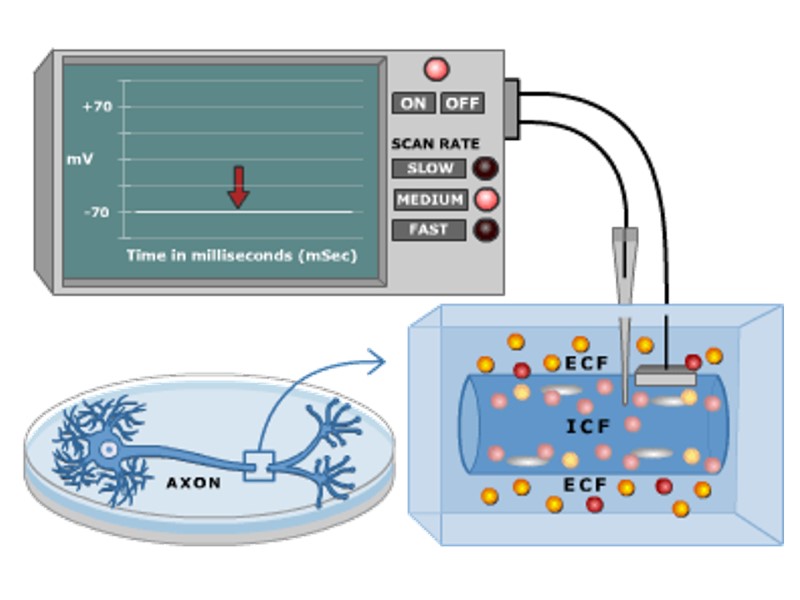
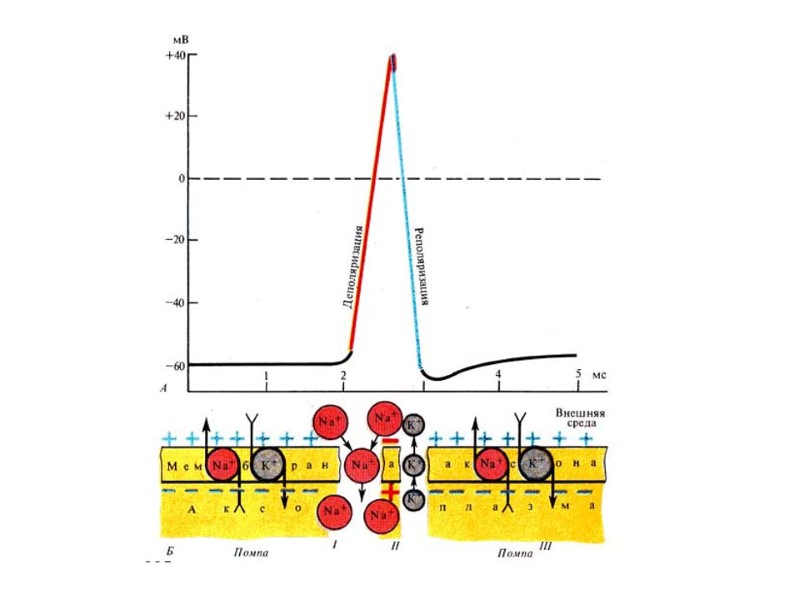
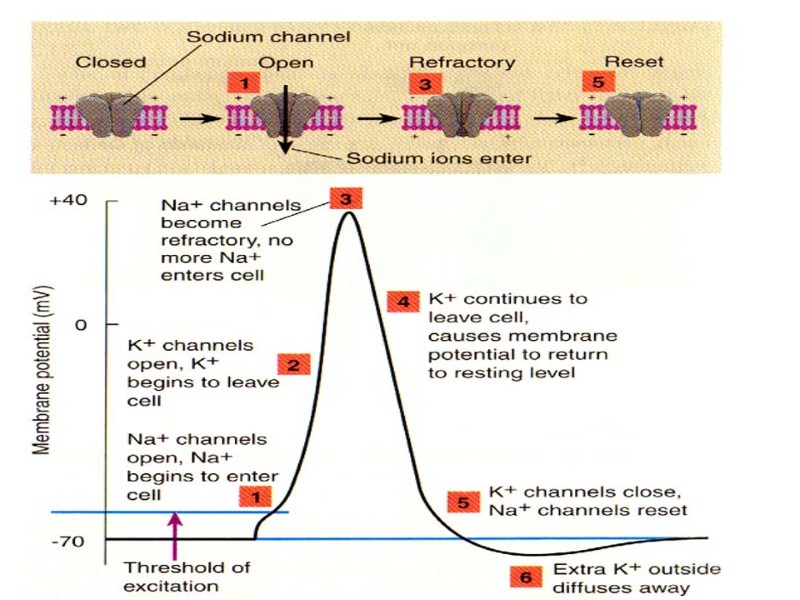
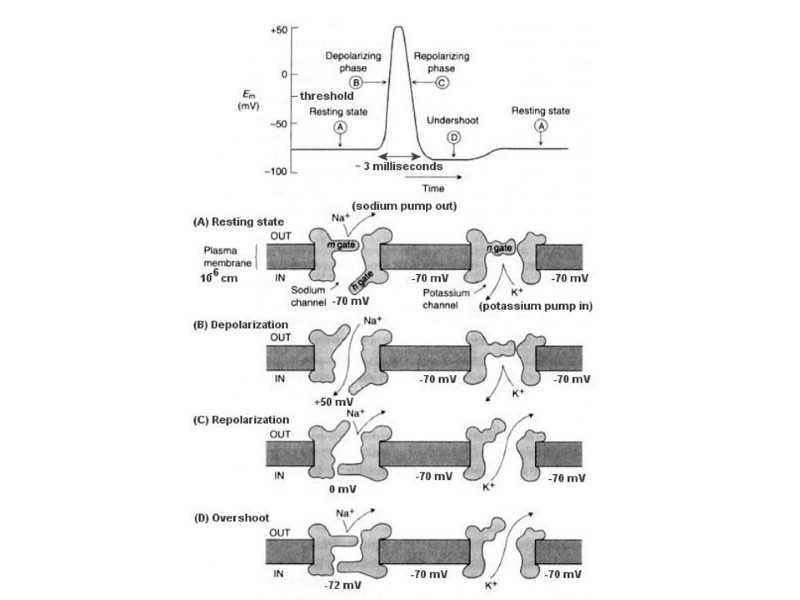
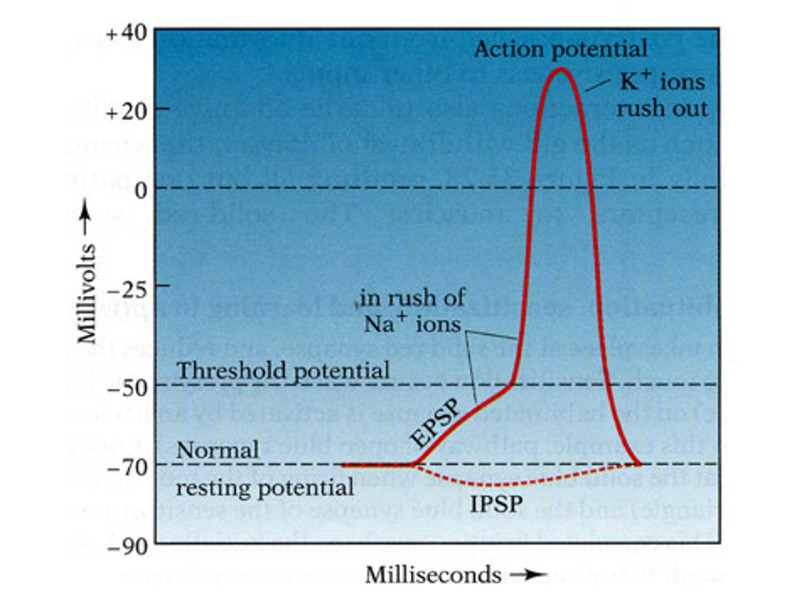
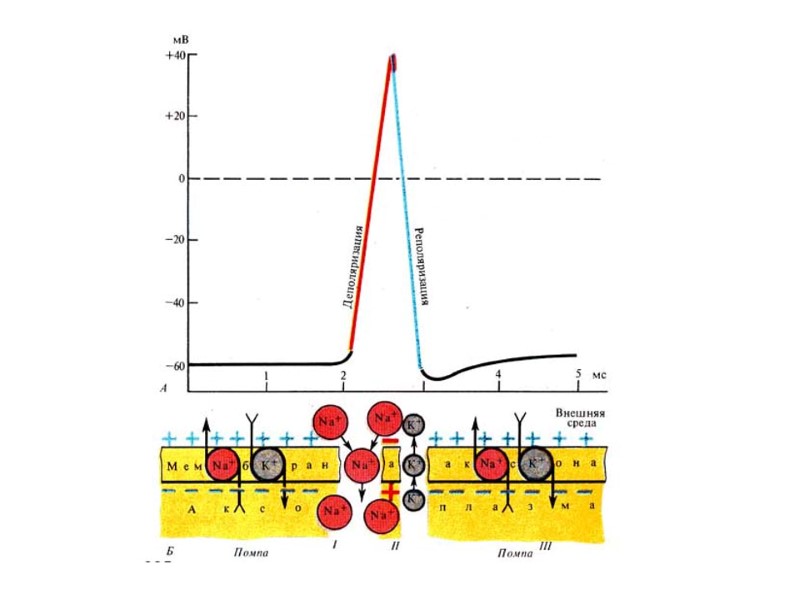
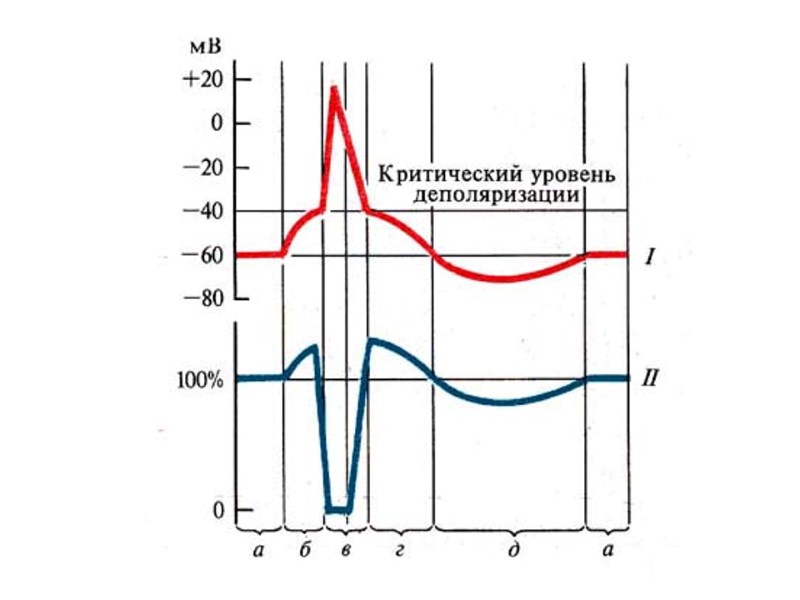
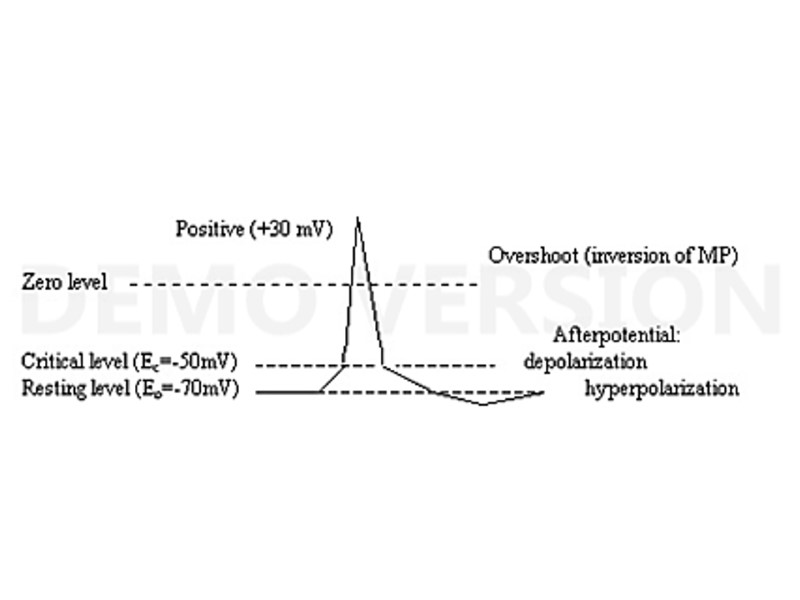
“Excitability” is the ability of several living tissue cells to generate specific active process (electrical excitation) when they are exposed to stimulation. “Polarization” means a presence of large negative potential across inside and outside the cell membrane at the rest (the resting potential). “Depolarization” of the cell membrane means a displacement of resting potential in the positive direction that is a reduction in membrane resting potential. “Hyperpolarization” of cell membrane means a displacement of resting potential in the negative direction that is an increase of membrane resting potential. Nerve and muscle fibers can be experimentally stimulated by many different kinds of stimuli such as physical agents (electrical current, mechanical action (pinching, striking, or cutting) suddenly chilling or heating, etc. ) or chemical agents ( various acids, alkalis, concentrated salt solutions, etc.) Depolarization causes rapid opening of the activation gates of the Na+ channel, the Na+ conductance of the membrane promptly increases, and Na+ ions enter into the cell resulting in additional depolarization of the cell membrane. To excite nerve or muscle electrical stimulus must be of sufficient intensity, duration and stepness of increase (the rate of stimulus rise) to reduce the transmembrane potential from its resting value to a critical voltage which, when achieved, results in the development of a propagated impulse.
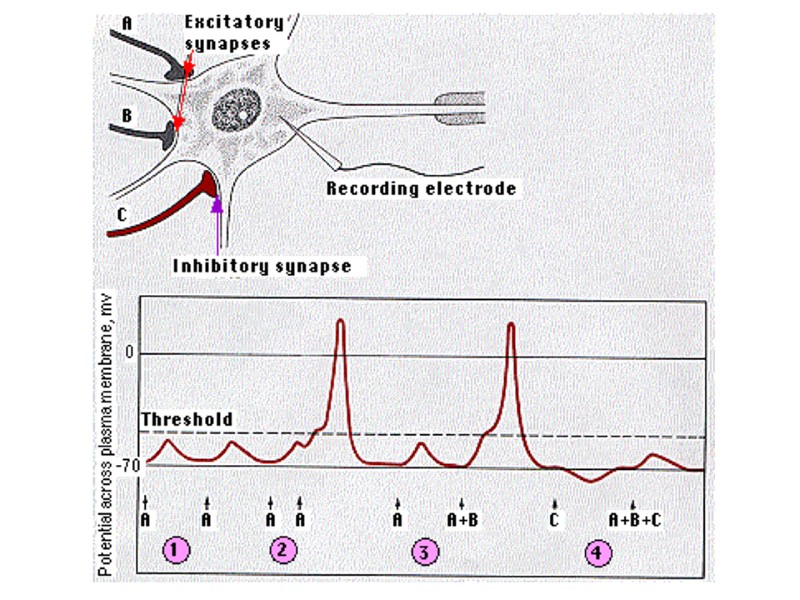
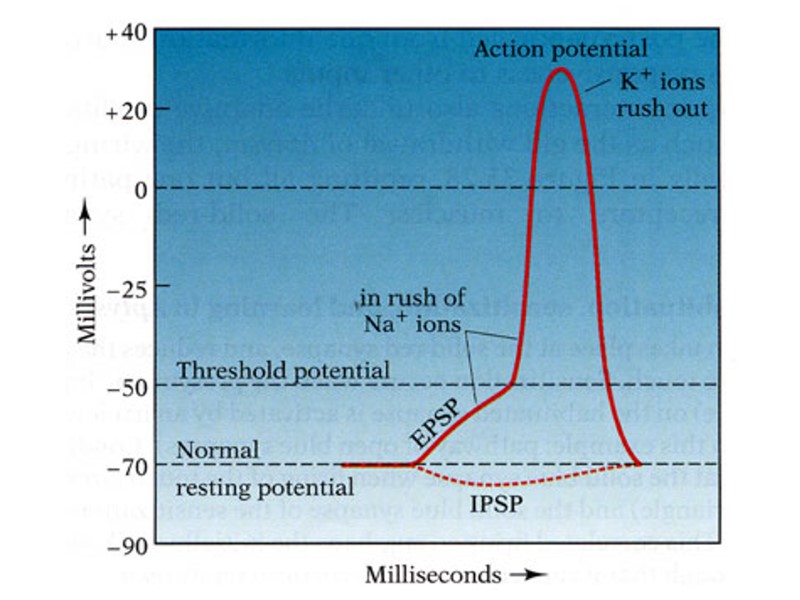
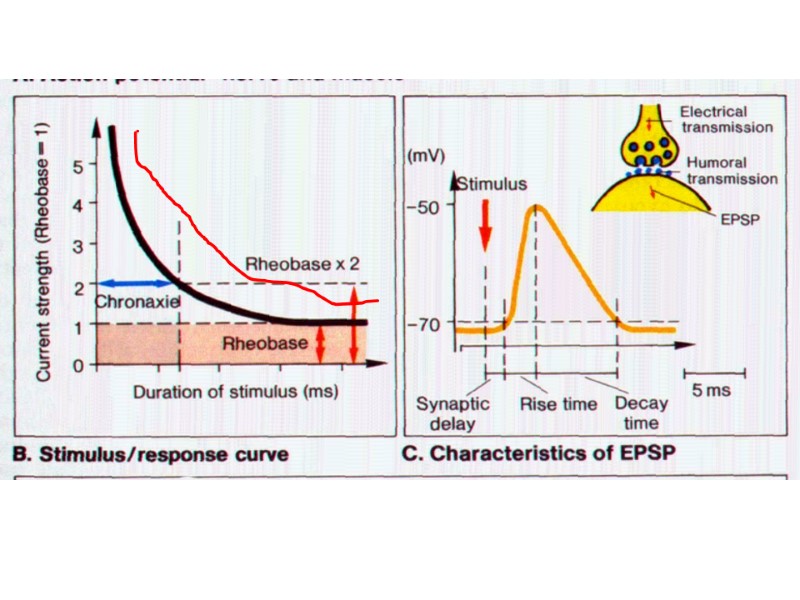
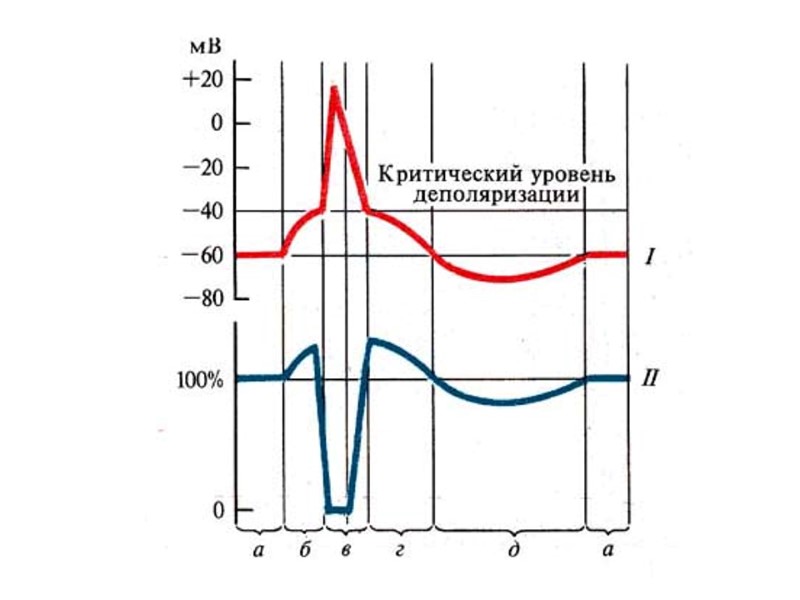
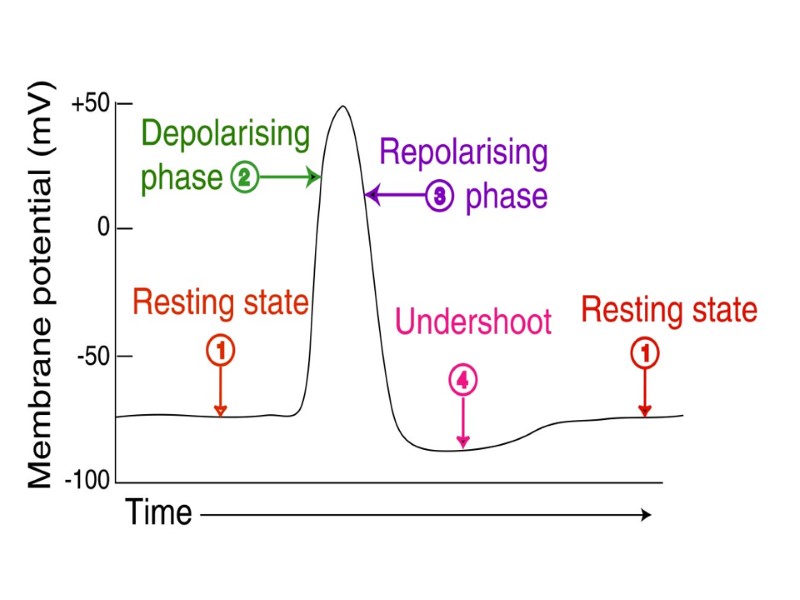
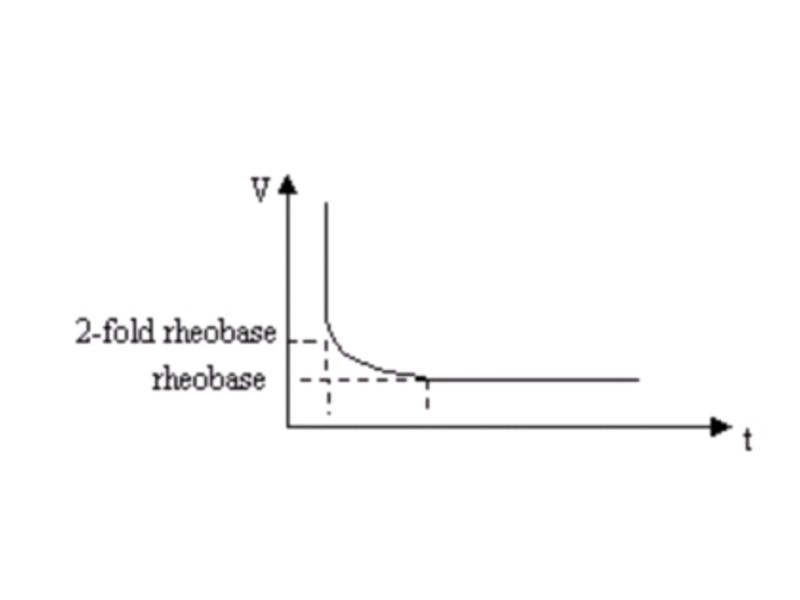
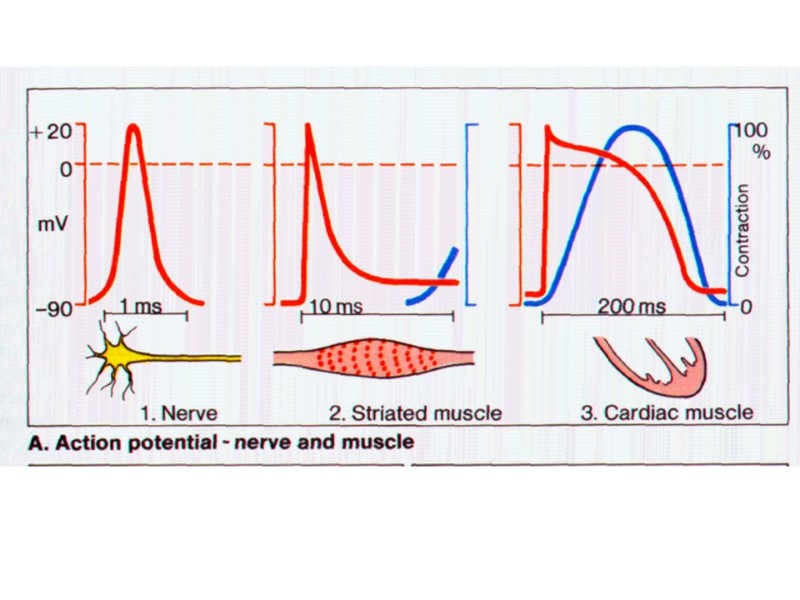
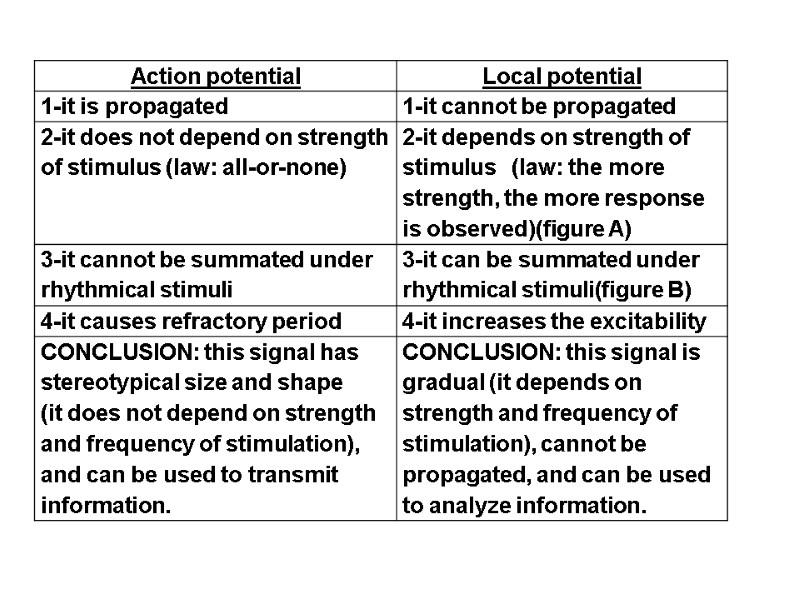
What does the term “threshold stimulus” mean? What does the threshold stimulus value depend on? The most minimal electrical stimulus just adequate to cause an action potential is called a threshold stimulus. The threshold stimulus value depends on the tissue excitability (threshold depolarization). Thresholds vary only slightly if the temperature and external ionic composition are maintained constant. .Figure the diagram of the relationship between the threshold strength stimuli and the duration of these stimuli (the strength - duration curve). Show the points of reobase, utilization time, chronaxie. The diagram of the relationship between the threshold strength stimulus and the duration of this stimulus (the strength -duration relationship) : What does the term “chronaxie” mean? ”Chronaxie” is the least time required for electrical stimulus equal to double reobase to produce excitation in a tissue. What is an action potential termed? Action potential is a property of excitable cells (nerve, muscle) consisting of a rapid depolarization followed by repolarization of the membrane as a reaction of excitable tissue on threshold and superthreshold stimuli.
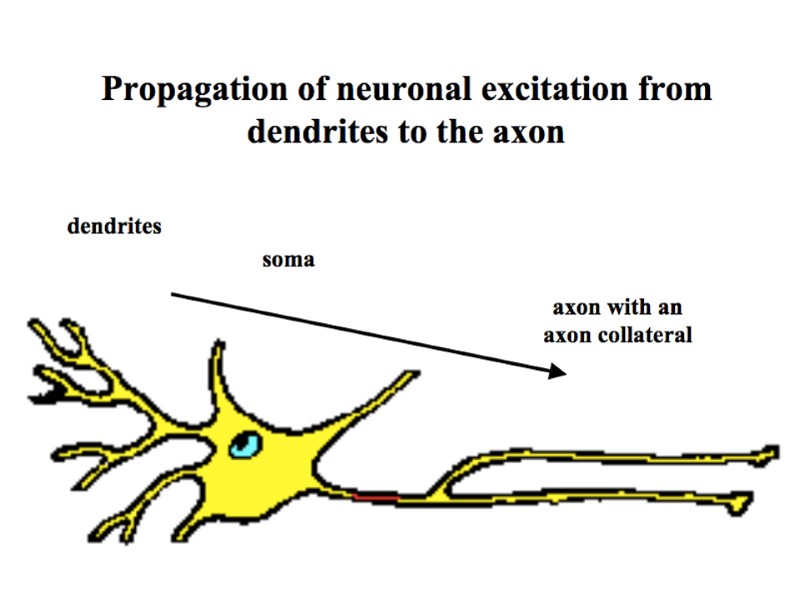
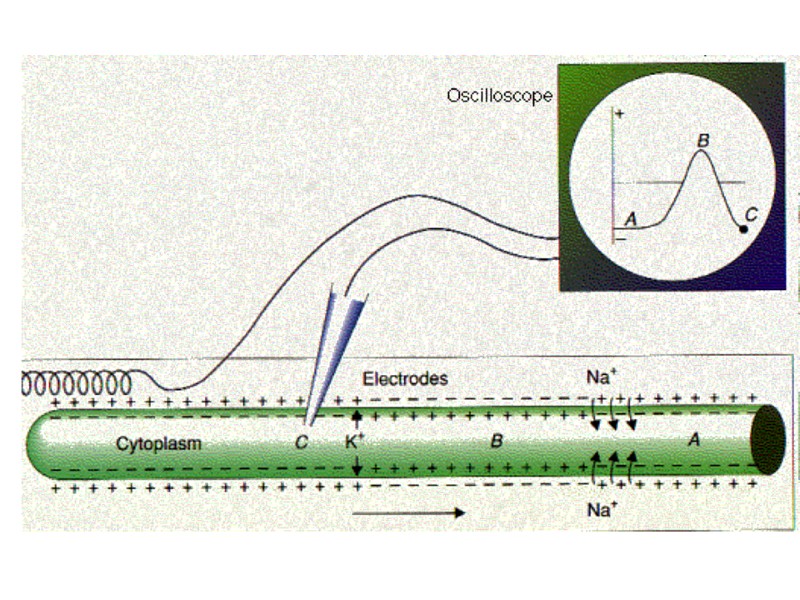
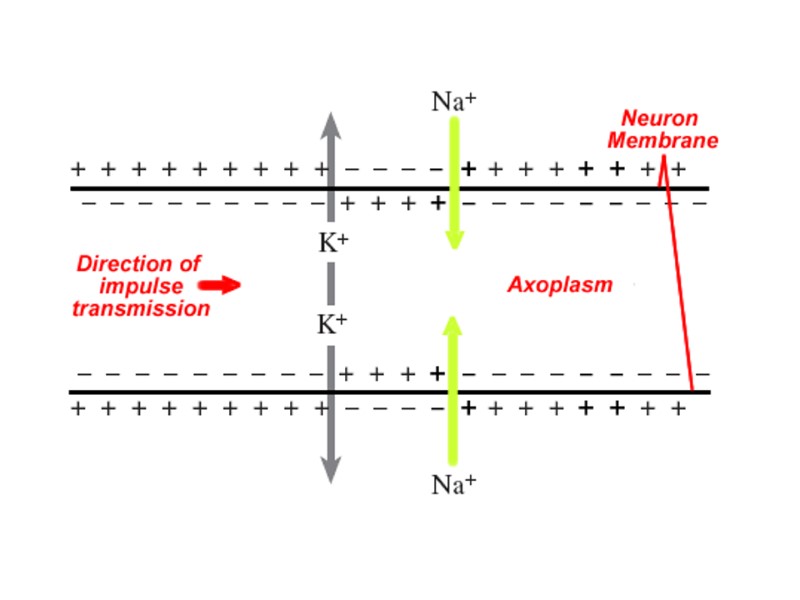
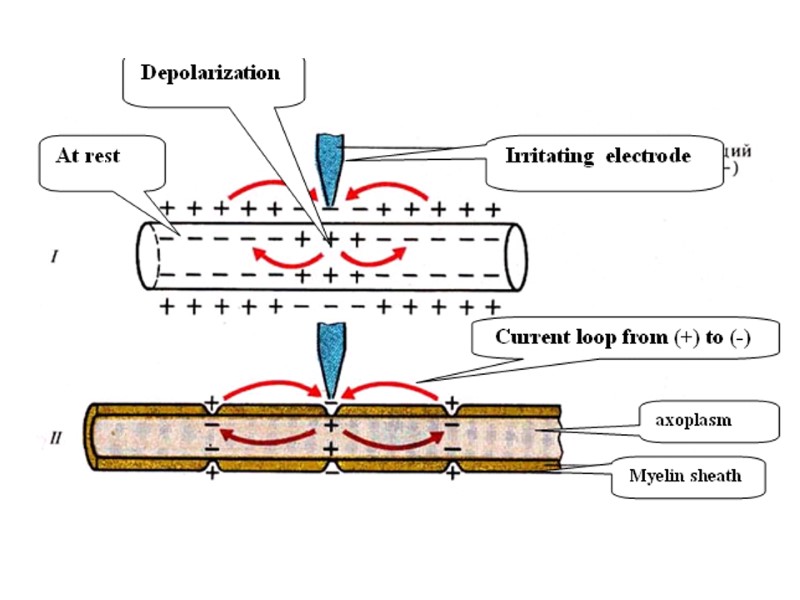
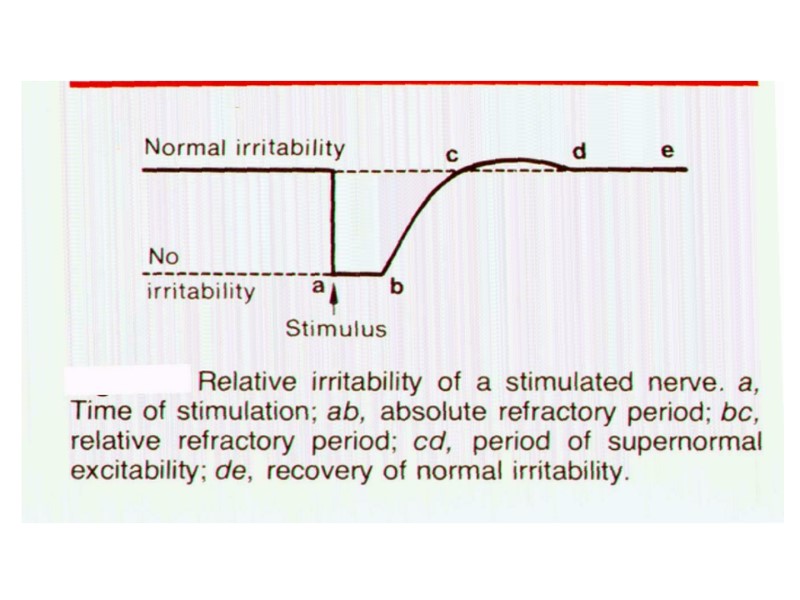
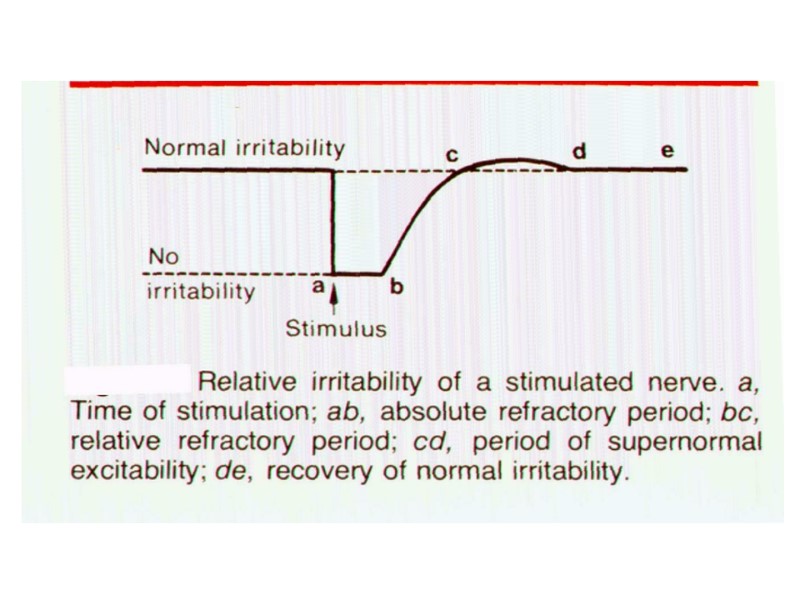
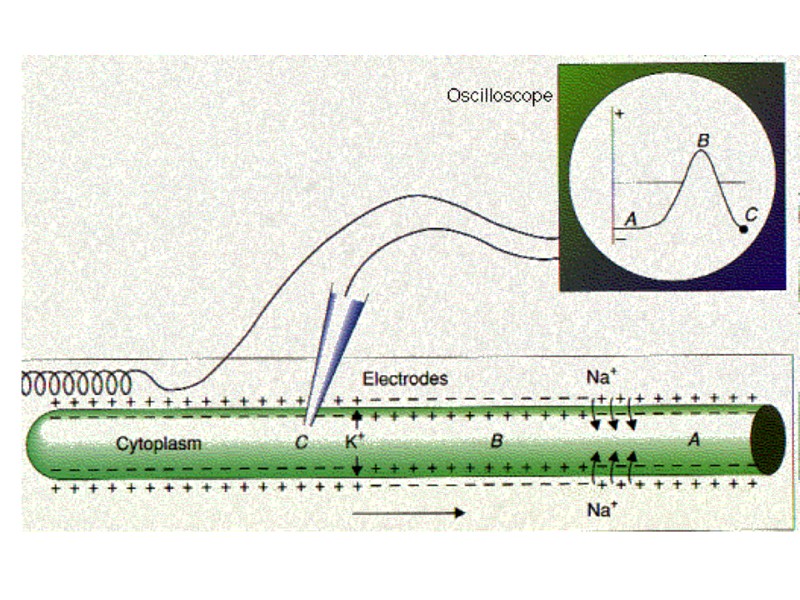
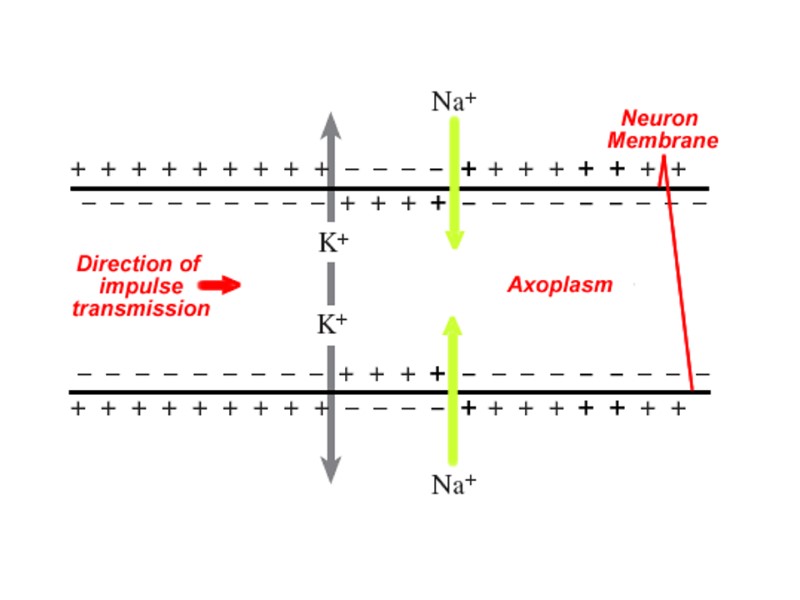
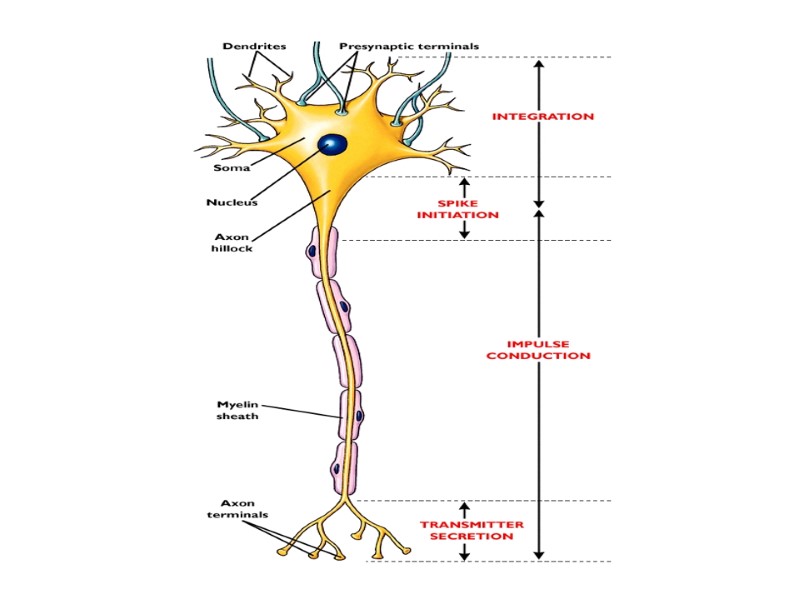
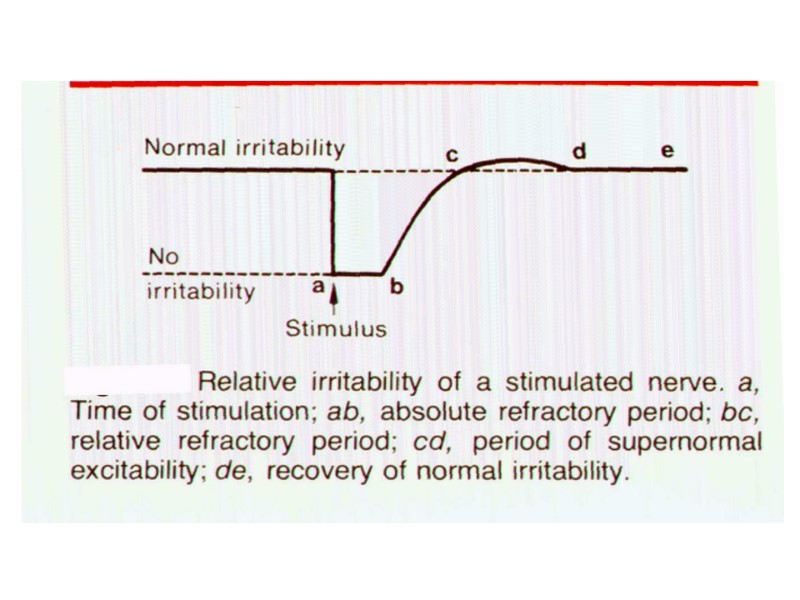
What does the expression “absolutely refractory period” mean? The expression “absolute refractory period” means the period during which another action potential can’t be elicited no matter how large the stimulus. What is the ion mechanism of the absolute refractory period appearance during an action potential development? According Hodgkin’s and Huxley’s ion theory of bioelectrical event origin the absolute refractory period is conditioned by changes in Na+ membrane permeability (inactivation of sodium channels). As result the membrane loses its capacity to react to a stimulus with an increase in sodium permeability. The inactivation gates of the Na+ channels are closed and will remain closed until repolarization occurs. No action potential can occur until the inactivation gates open. Describe shortly process of action potential propagation along a nerve fiber. Assume that a nerve has been exited in its midportion and an action potential is generated. This results in an appearance of local currents to adjacent resting areas of membrane, which are then depolarized to threshold and generate new action potentials. These newly depolarized areas produce local currents still further along the membrane, causing progressively more and more depolarization. Thus, the depolarization process is self-propagated along the entire extent of the axon. What does the term “lability” mean? Who formulated the concept of lability in the end of XIX century? Lability is a property of excitable tissue is related to the velocity of each action potential development during tissue rhythmical stimulation. Vvedensky, he understood the lability as the higher or lower rate of the elementary reactions that accompany the physiological activity of a given apparatus.
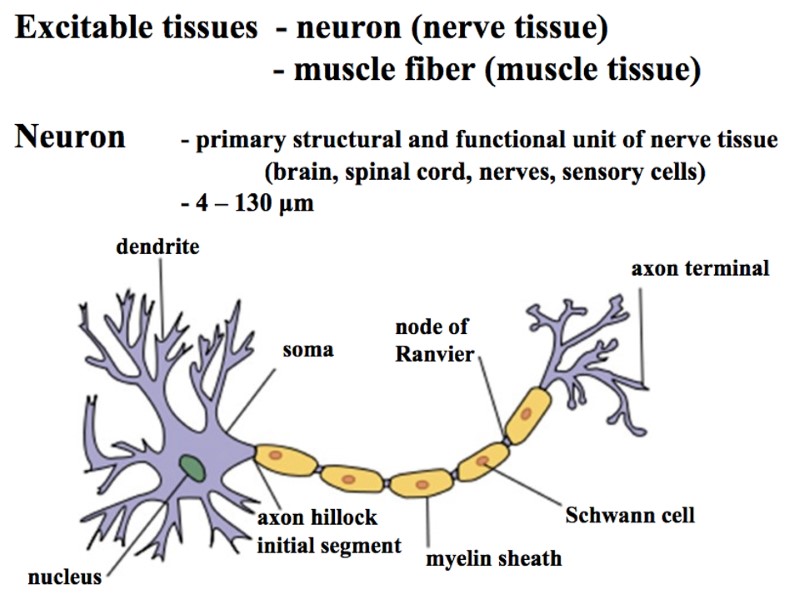
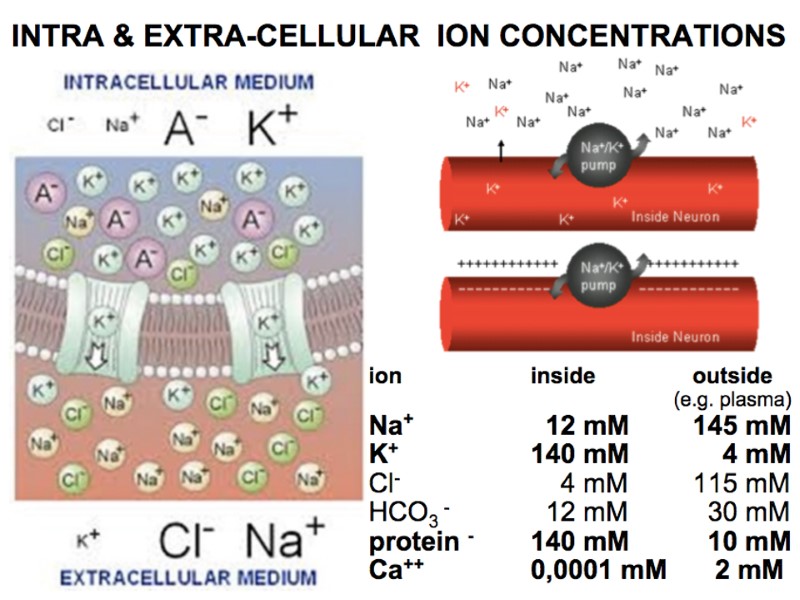
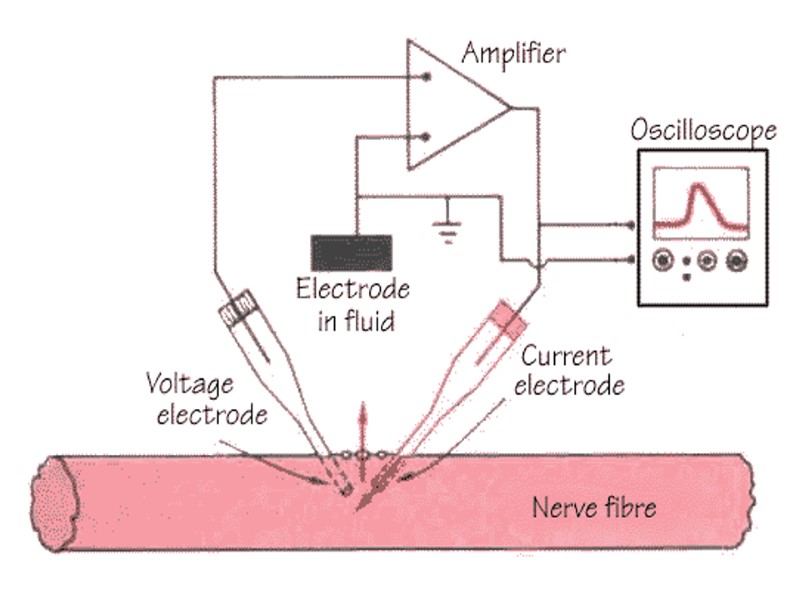
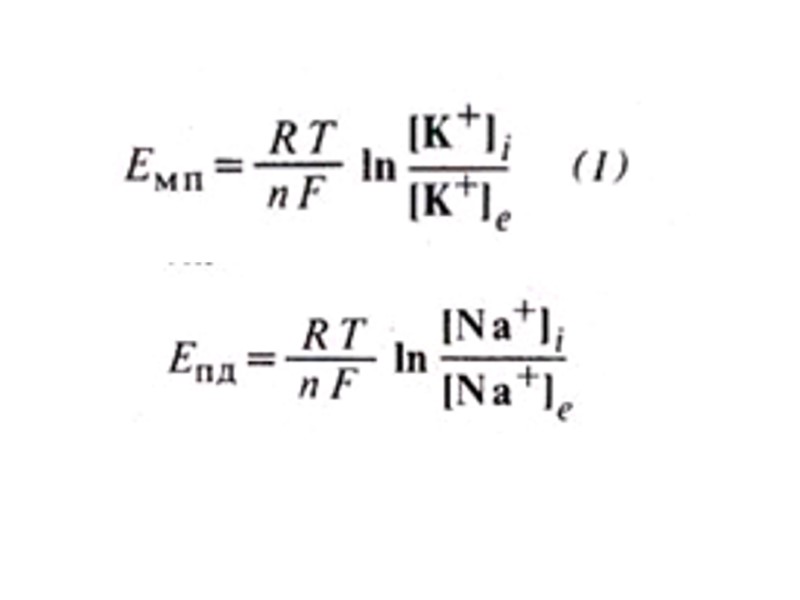
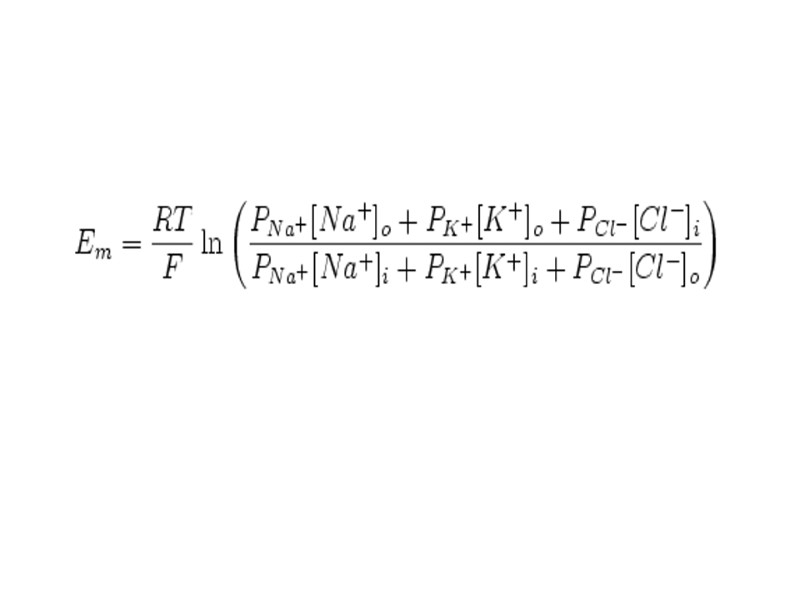
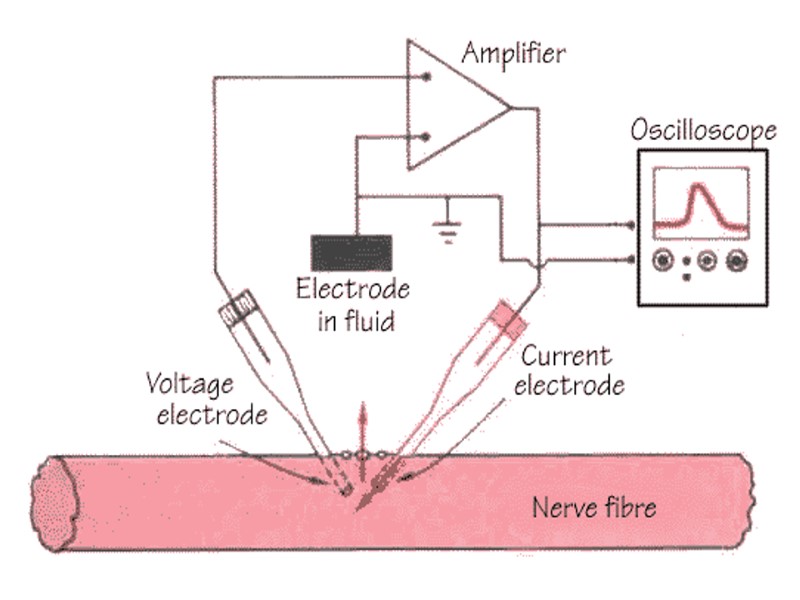
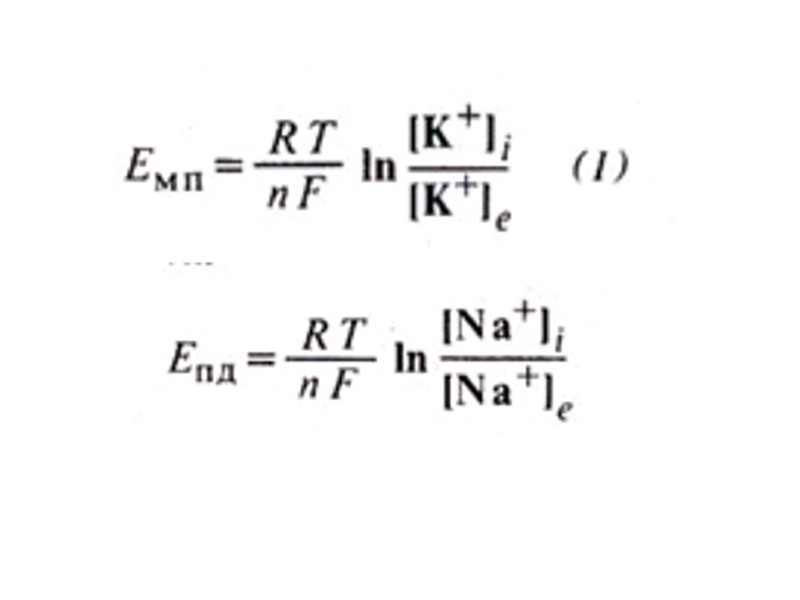
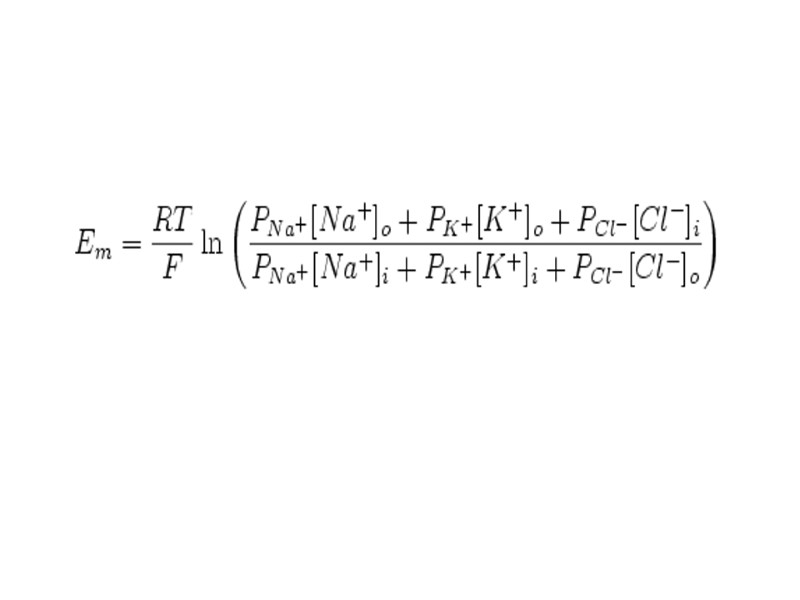
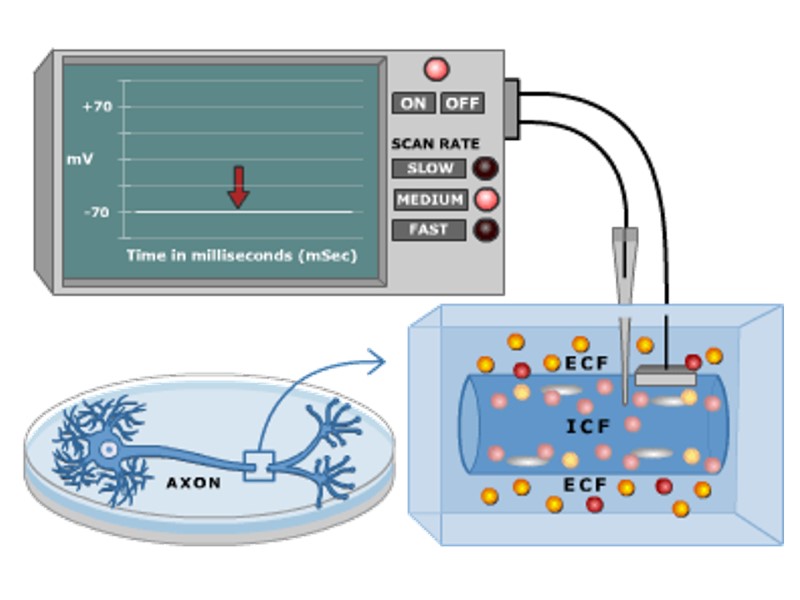
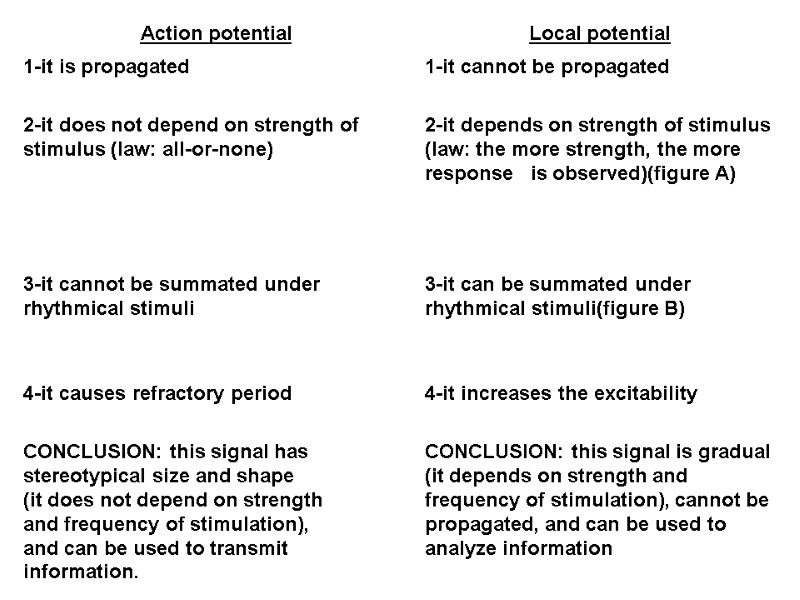
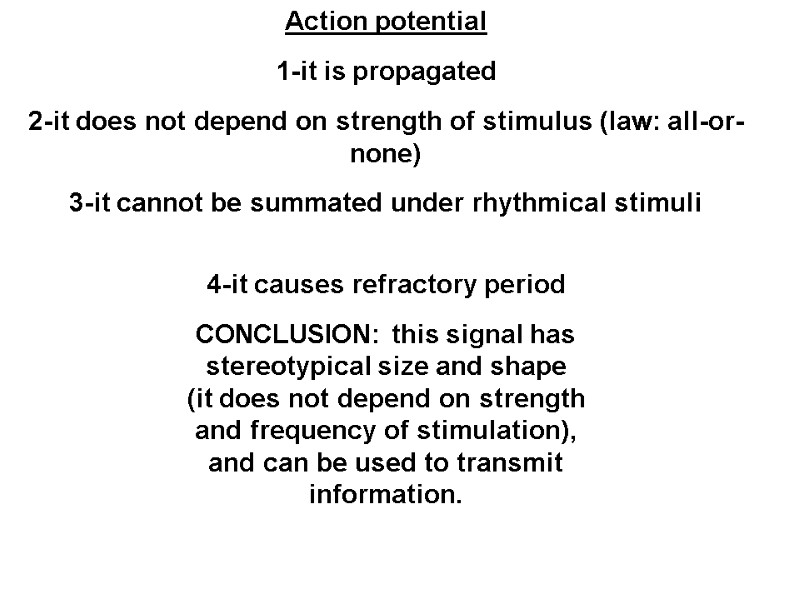
Excitable tissues (nervous and muscle tissues). Irritability and excitability. Cell membrane: Lipid bilayer. Proteins: (a) integral P.-carrier, channels, enzymes; (b) peripheral P. – enzymes. Glycocalyx (carbohydrate coat) – attach among the cells, negative charge, molecular receptors, and immune reactions. Transport: (a) passive (simple diffusion of water and fat-soluble through the bilayer; simple diffusion of ions through the ions channels) “downhill”; and (b) active (ions pumps, using energy of ATP) “uphill”. Ions channels: (a) non-regulated (always opened; leakage of ions); and (b) regulated (can be opened and closed; potential-sensitive type and chemical-sensitive type). Ion channels provide permeability of membrane. Ions moving forces (for simple diffusion): (a) concentration gradient; and (b) electrical gradient. They provide conductance of membrane. Diffusion potential is the potential difference generated across a membrane (if it is permeable to an ion) because of a concentration gradient of the ion. The more gradient, the more size of the diffusion potential, that exists in the cell. Equilibrium potential is the diffusion potential that exactly balances the tendency for diffusion: chemical and electrical driving forces acting on an ion are equal and opposite and there is no more net diffusion. Nernst equation is used to calculate the ion equilibrium potential: E = K ln [conc outside/conc inside]. ENa = +65 mV; EK = -85 mV; ECa = +120 mV; ECl = -90 mV Measurement of membrane potential (intracellular monopolar method; microelectrode). Scheme of record. Normal resting membrane potential (RP) is the measured potential difference across the cell membrane at rest. Mechanism: (a) ions asymmetry (created by ion pumps: high K-concentration inside and high Na-concentration outside); (b) permeability of membrane at rest (high permeability to K+); (c) ions current flow (simple diffusion of K-ions outward creates diffusion potential, which size is about EK); (d) charges on the inner (-) and outer (+) surface of membrane. Change of MP: depolarization (decrease of RP by inward current of cations); hyperpolarization (increase of RP by outward current of cations). Action potential (AP) is rapid change of membrane potential in response to stimulus. Its stages are: (a) depolarization and overshoot; (b) repolarization; (c) afterpotential. Scheme of record. DEPOLARIZATION. ACTION POTENTIAL has stereotypical size and shape, is propagating, and is “all-or-none”. Principle ALL-OR-NONE: if stimulus is subthreshold, AP does not develop; if stimulus is threshold and superthreshold, AP develops as maximum and stereotypical response (independently on parameters of stimulus).
has stereotypical size and shape, is propagating, and is “all-or-none”. Principle ALL-OR-NONE: if stimulus is subthreshold, AP does not develop; if stimulus is threshold and superthreshold, AP develops as maximum and stereotypical response (independently on parameters of stimulus). ACTION POTENTIAL
The action potential is all-or-none The strength of the action potential is an intrinsic property of the cell. So long as they can reach the threshold of the cell, strong stimuli produce no stronger action potentials than weak ones. However, the strength of the stimulus is encoded in the frequency of the action potentials that it generates.
Physiology excitable tissues study various aspects of the electrical phenomena in alive organisms. For the first time experiences under the proof " of an animal electricity " were spent Loudgi Galvani (1786). It was by the beginning of electrophysiological researches. Animal electricity - electrical phenomena accompanying ability to live of tissues and organs alive organisms. Loudgi Galvani has proved existence of animal electricity by two experiences. First - balcony or with metal.
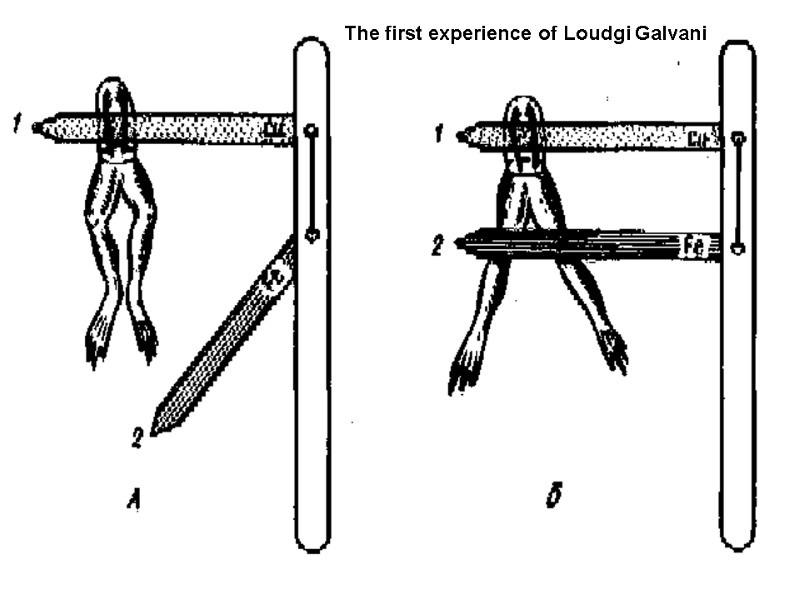
The first experience of Loudgi Galvani
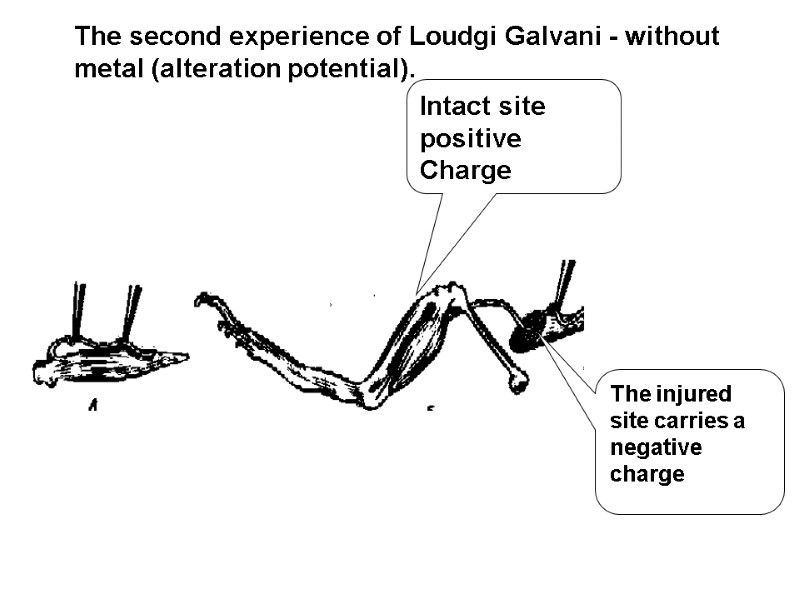
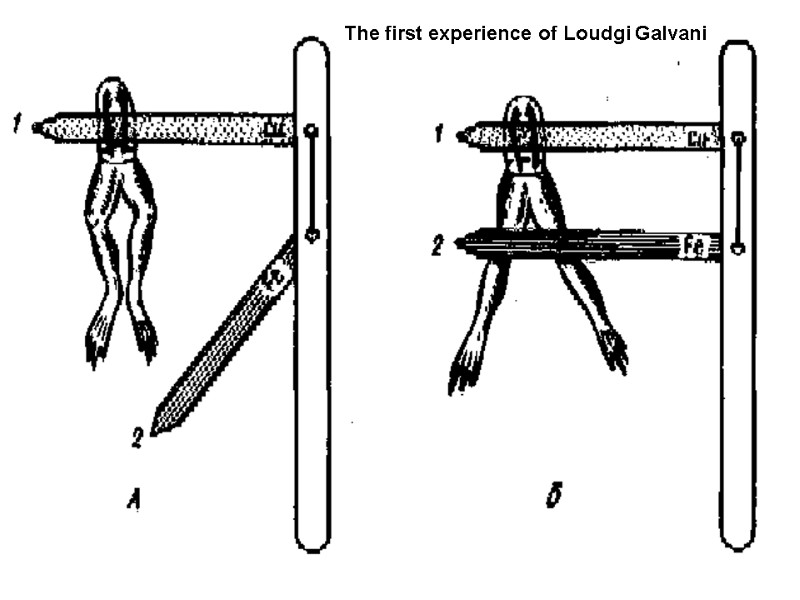
The injured site carries a negative charge Intact site positive Charge The second experience of Loudgi Galvani - without metal (alteration potential).
Debut-Raymond has established, that the injured site carries a negative charge, and intact - positive. Therefore in a condition of rest between the outside and inside of the cell membrane there is a difference of potentials so called resting (membrane) potential amounts to 50-100 mV (cell interior is negative) in muscle and nerve cells.
The following phenomena can be explained membrane’s theory (Hojkin, Hacksly, and Katz, 1949 – 1952): The membrane of nervous cells has selective permeability for ions potassium, sodium and chlorine. In a condition of rest the permeability of ions potassium in 25 times is higher, than for ions sodium. At excitation sodium the permeability in 20 times exceeds potassium. Electrogenesis resting (membrane) potential is carried out with the help of two mechanisms: Free diffusion of ions on concentration and electrochemical gradients. Passive transport without an expense ATP. Active Na+/K+ pump.
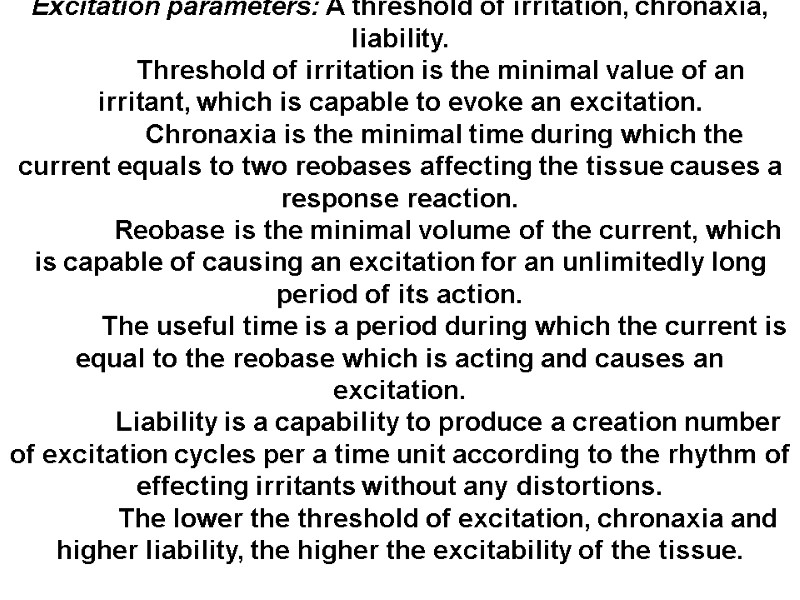
Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to evoke an excitation. Chronaxia is the minimal time during which the current equals to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable of causing an excitation for an unlimitedly long period of its action. The useful time is a period during which the current is equal to the reobase which is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
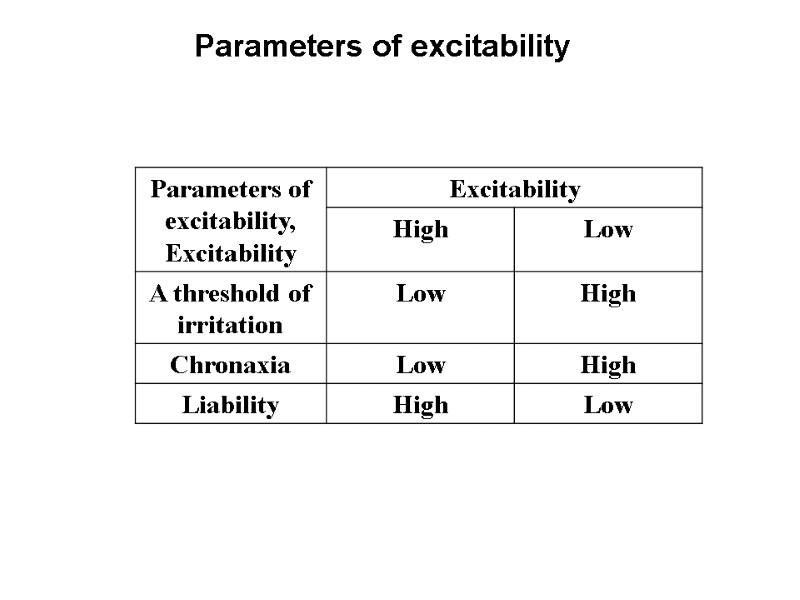
Parameters of excitability
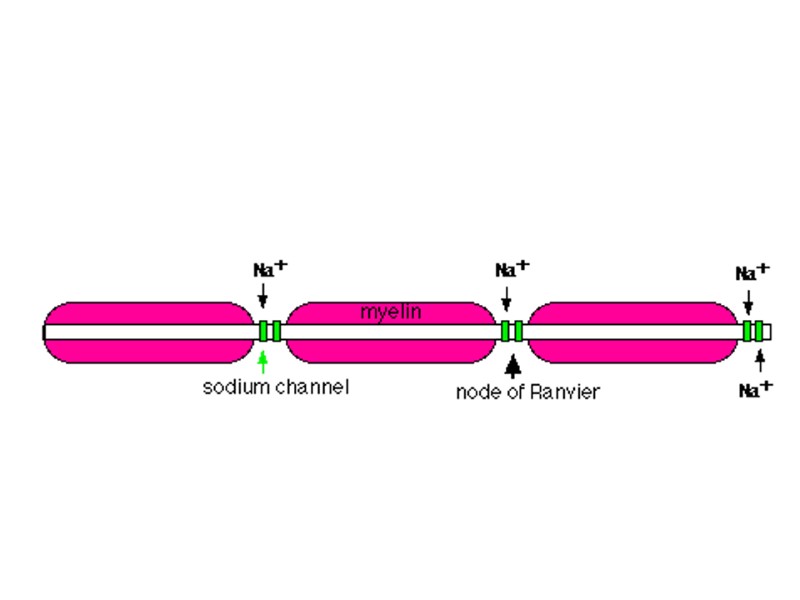
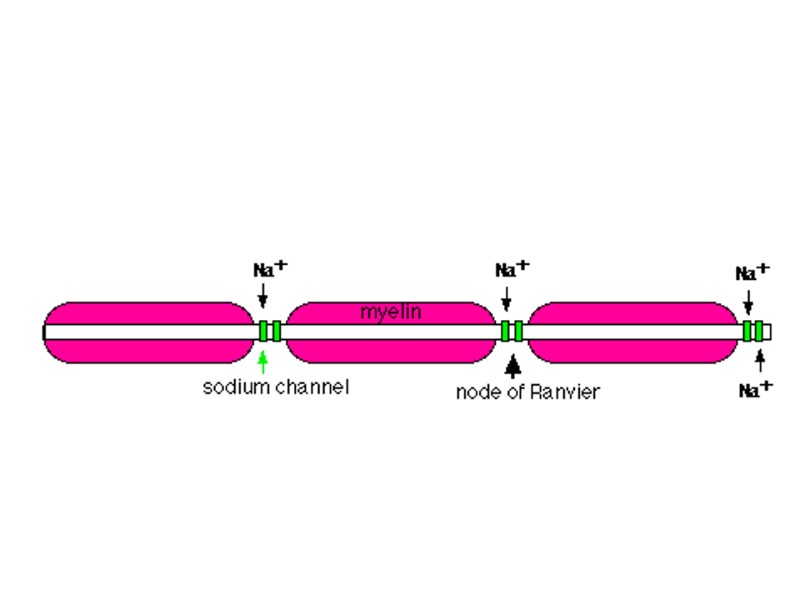
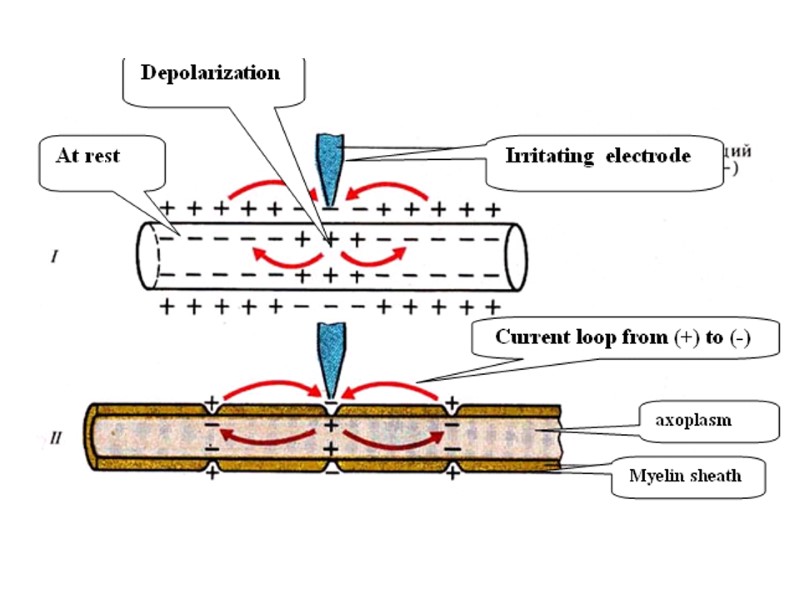
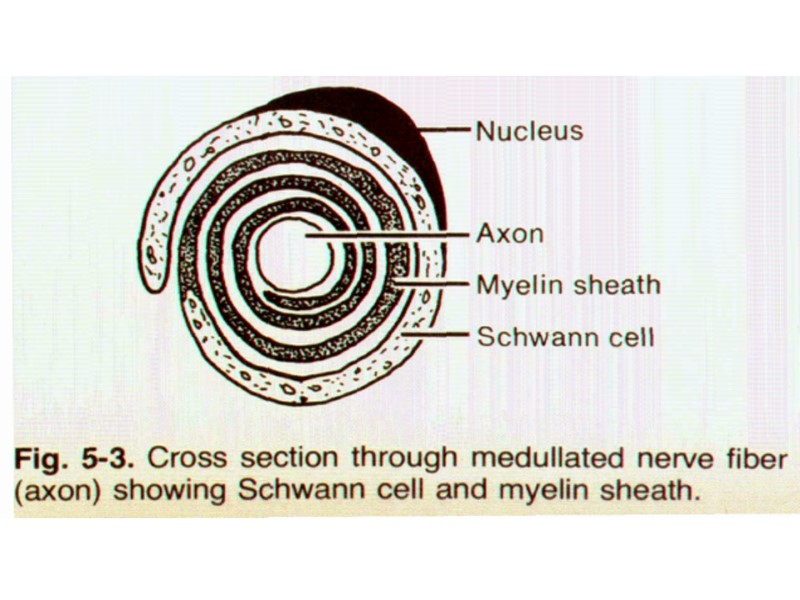
In non-myeliminated fibers an excitation is conducted serial and in myeliminated fibers – saltatoricly (somersault) (from one node of Ranvier to another)
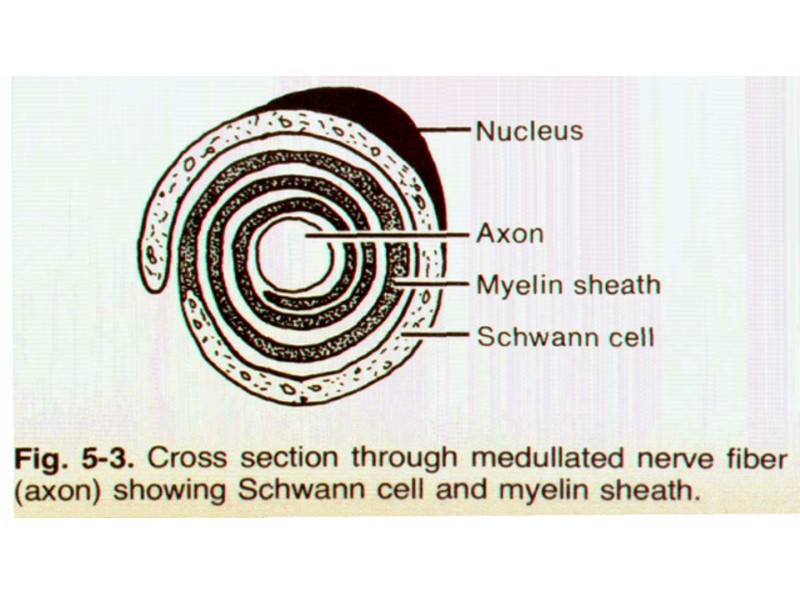
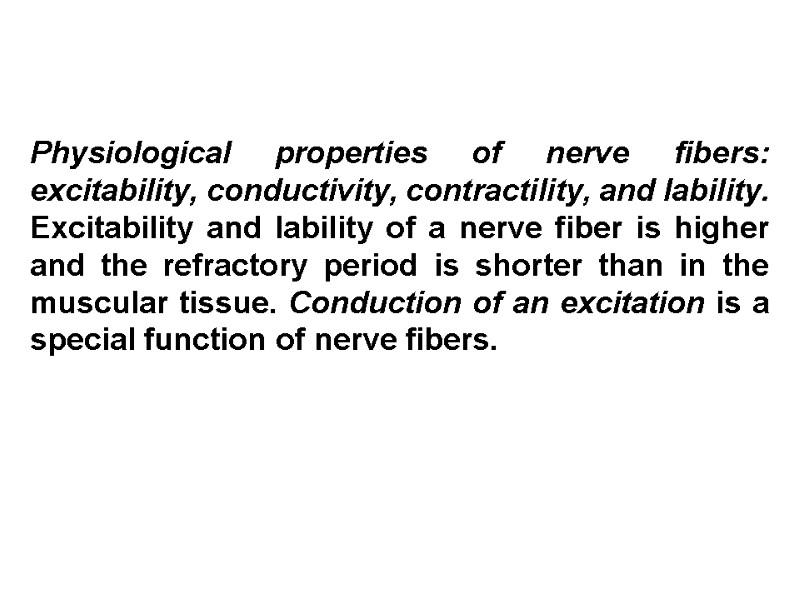
Physiological properties of nerve fibers: excitability, conductivity, contractility, and lability. Excitability and lability of a nerve fiber is higher and the refractory period is shorter than in the muscular tissue. Conduction of an excitation is a special function of nerve fibers.
Laws conduction of excitation via nerve fibers, The law of two-way conduction via a nerve fiber, The law of the anatomic and physiologic integrity, The law of an isolated conduction of excitation through a nerve fiber (Gasser and Erlanger, 1937). Types of nerve fibers: A, B, C. They are characterized according to the conduction rate diameter, the structure (myelinated – non-myelinated).
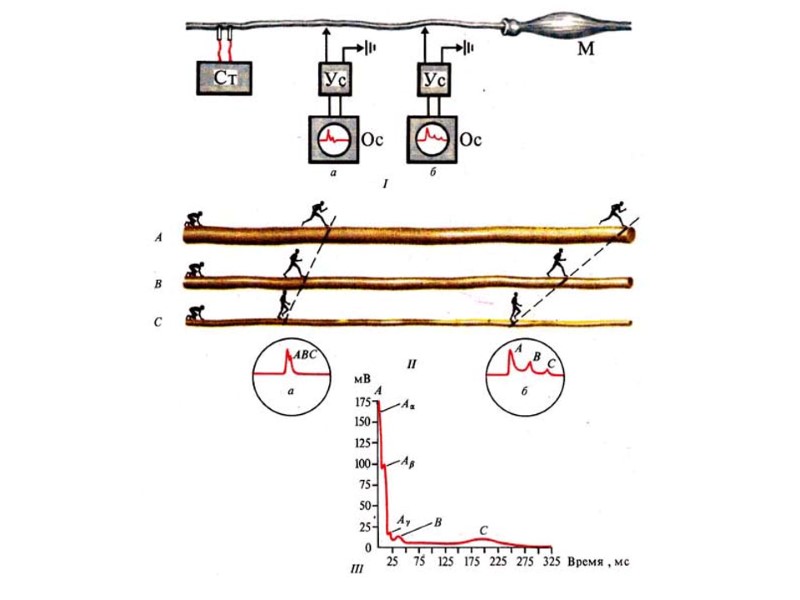
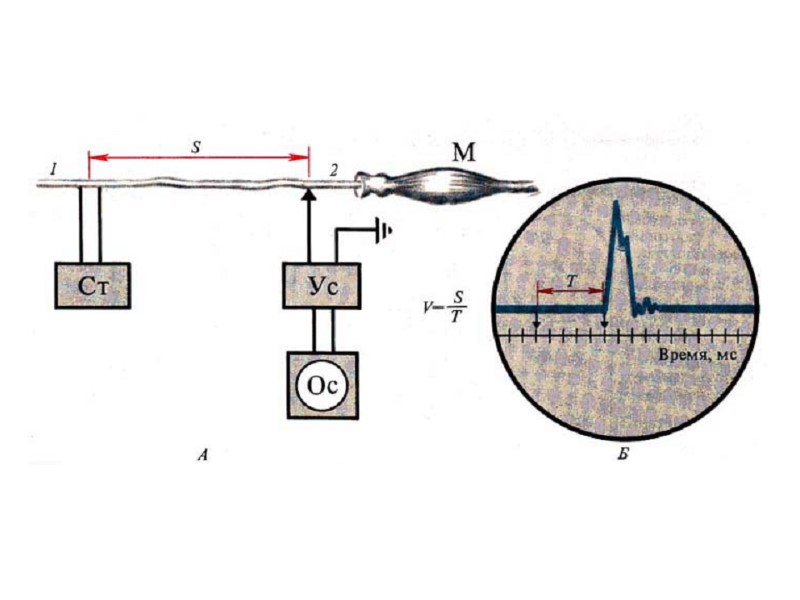
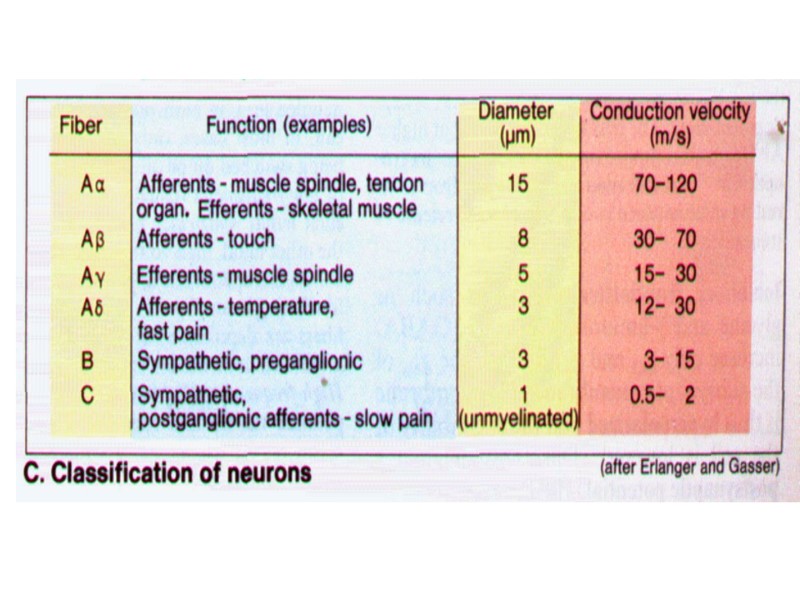
Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs as an isolated propagation. Conduction velocity of AP is directly proportional to a diameter of a nervous and myelinated.
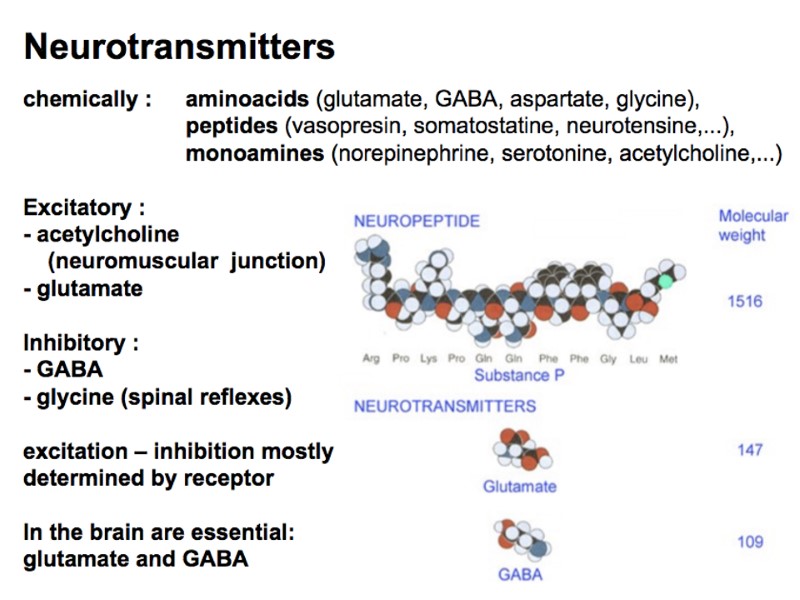
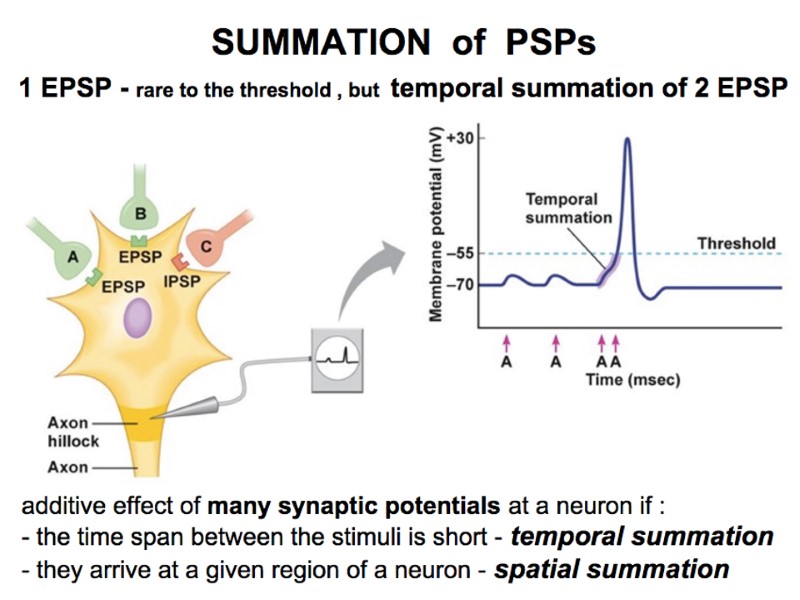
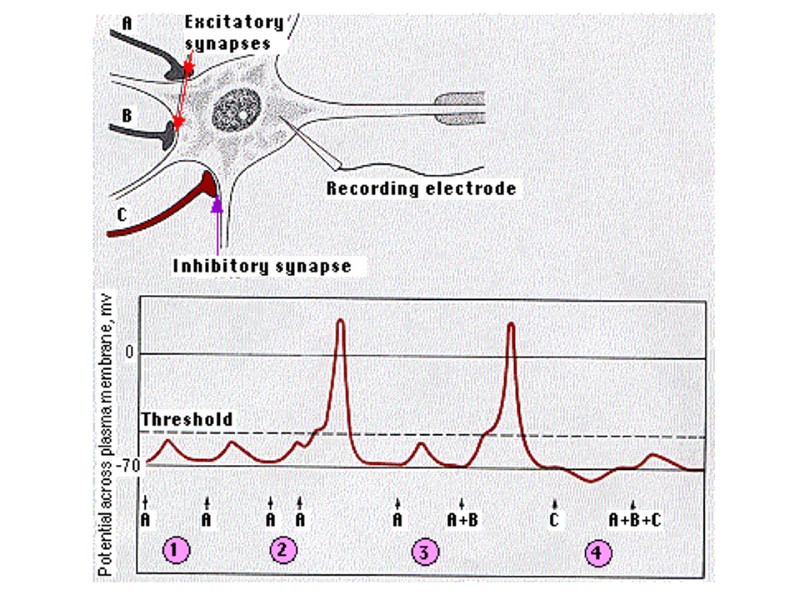
Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0,5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0,5 - 0,9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0,5 - 0,9 from threshold);
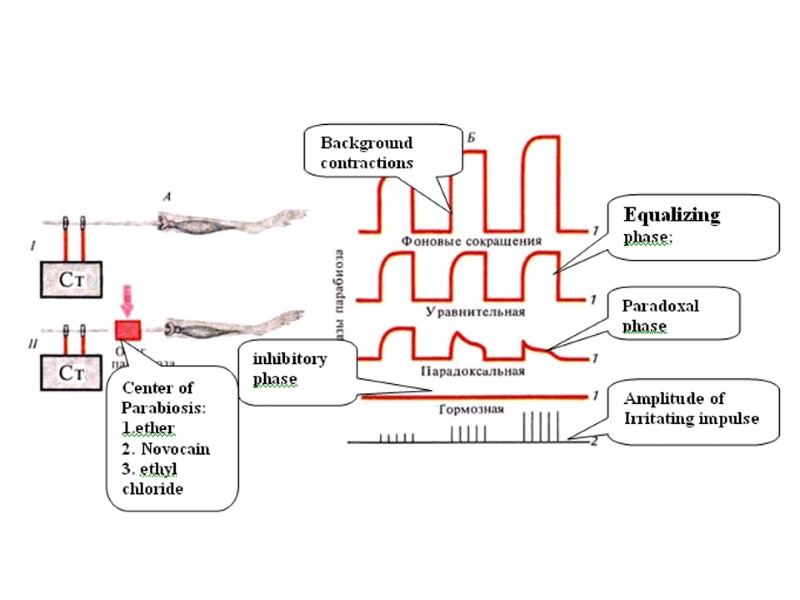
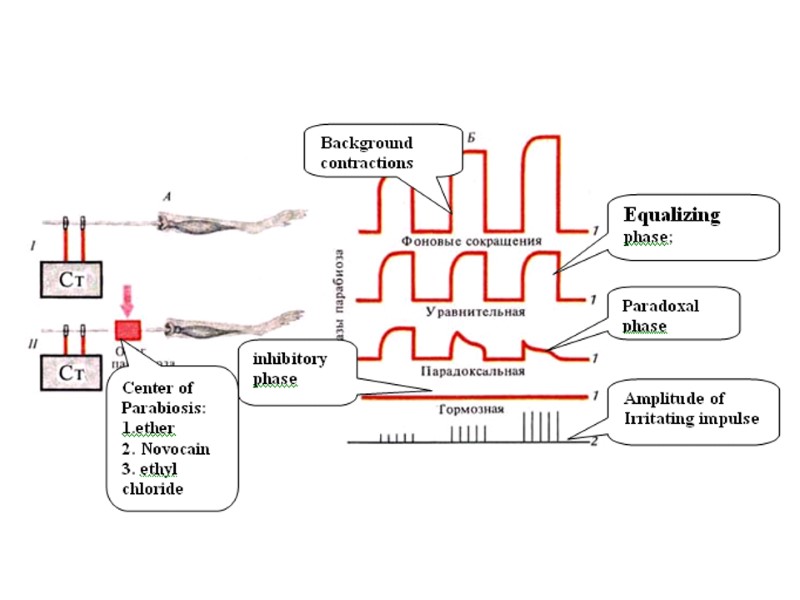
Parabiosis (the near-live status) according to N. E Vvedenky is stable non- conductivity depolarization. The mechanism of stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility, phase changes of excitability, and conduction of a nerve are its characteristics. Phases of parabiosis: equalizing, paradoxical, inhibitory. Parabiotic process is the basis of conducting analgesia (appendectomy).
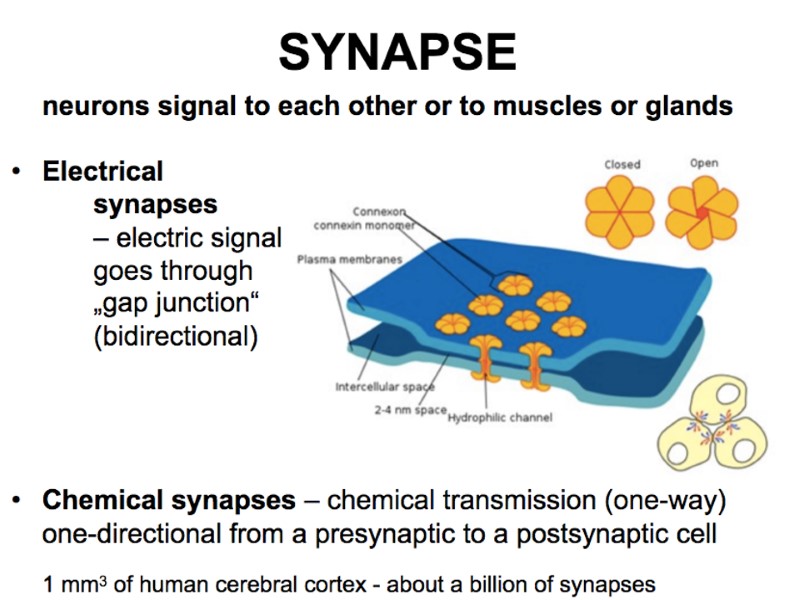
Physiological properties of chemical synapses: One direction conduction of the excitation; synaptic delay; transmission of excitation with the help of a mediator; transformation of the rhythm of excitation, low liability; high fatigability; high sensivity to chemical substances including pharmaceuticals. high sensivity to hypoxia.
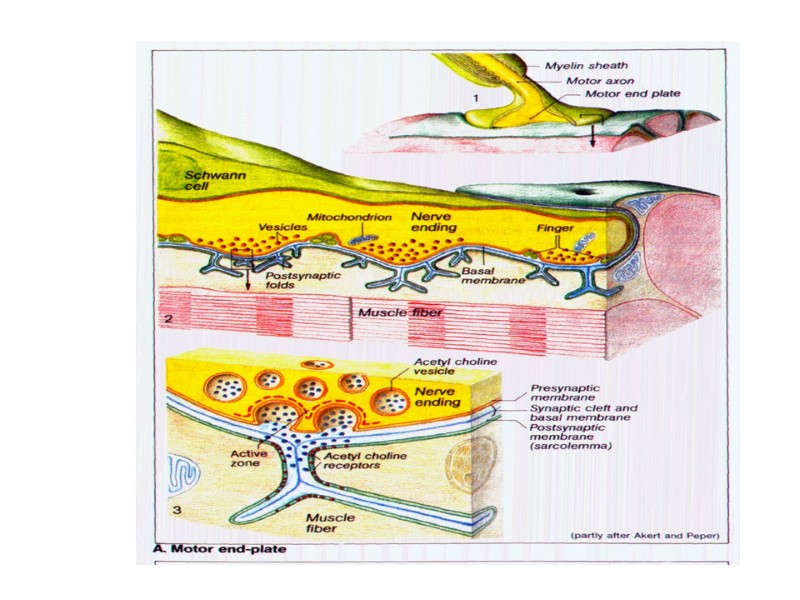
Classification of synapse. Peripheral and central, exciting and inhibiting; chemical, electrical, combined: cholinergic, adrenergic, dopaminergic, serotoninergic etc. (for chemical synapses). The structure of a synapse.

The Muscular System Muscles are responsible for all types of body movement Three basic muscle types are found in the body Skeletal muscle Cardiac muscle Smooth muscle
Characteristics of Muscles Skeletal and smooth muscle cells are elongated (muscle cell = muscle fiber) Contraction of muscles is due to the movement of microfilaments All muscles share some terminology Prefixes myo and mys refer to “muscle” Prefix sarco refers to “flesh”
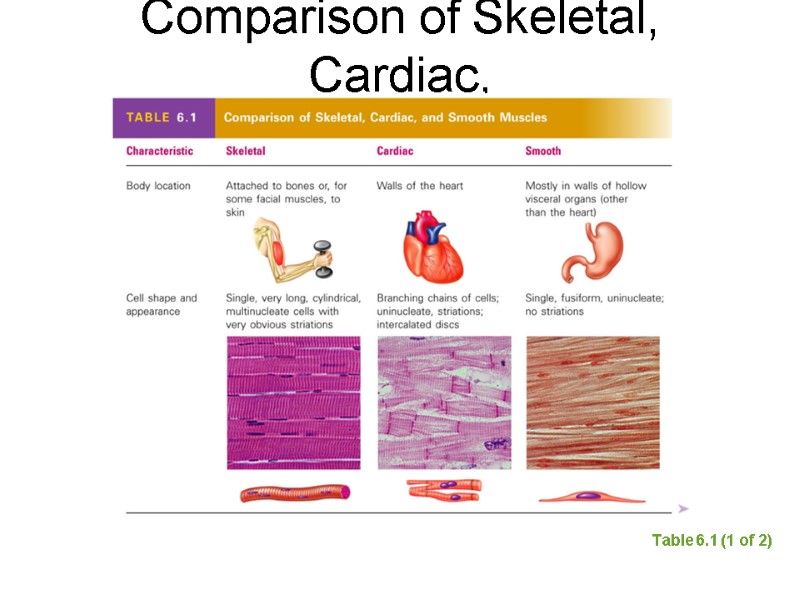
Comparison of Skeletal, Cardiac, and Smooth Muscles Table 6.1 (1 of 2)
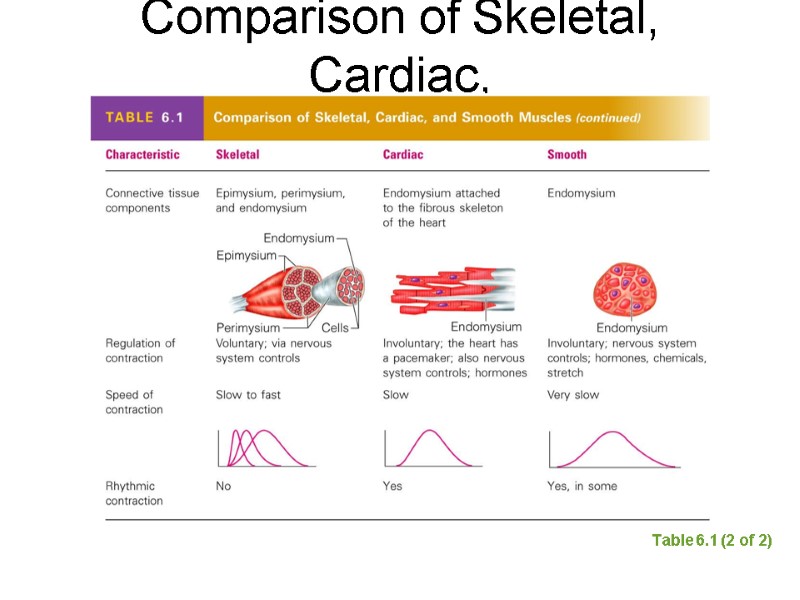
Comparison of Skeletal, Cardiac, and Smooth Muscles Table 6.1 (2 of 2)
Skeletal Muscle Characteristics Most are attached by tendons to bones Cells are multinucleate Striated—have visible banding Voluntary—subject to conscious control
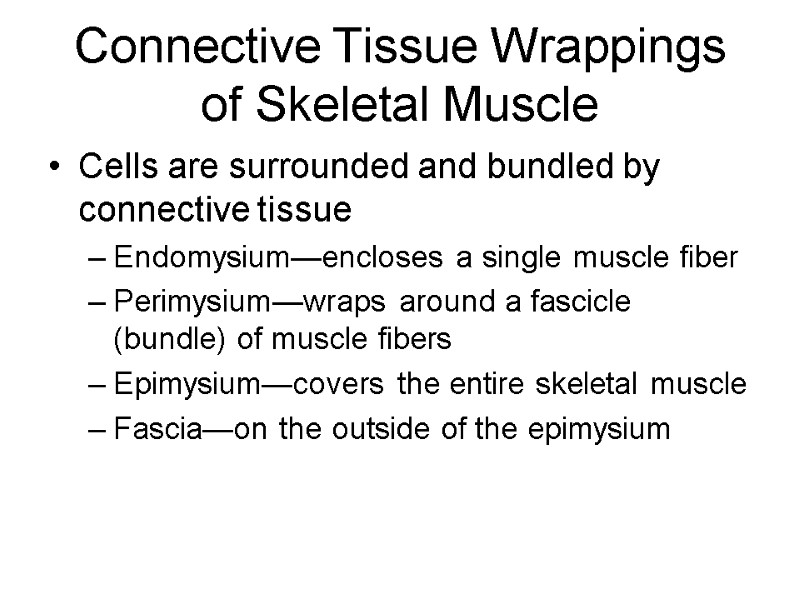
Connective Tissue Wrappings of Skeletal Muscle Cells are surrounded and bundled by connective tissue Endomysium—encloses a single muscle fiber Perimysium—wraps around a fascicle (bundle) of muscle fibers Epimysium—covers the entire skeletal muscle Fascia—on the outside of the epimysium
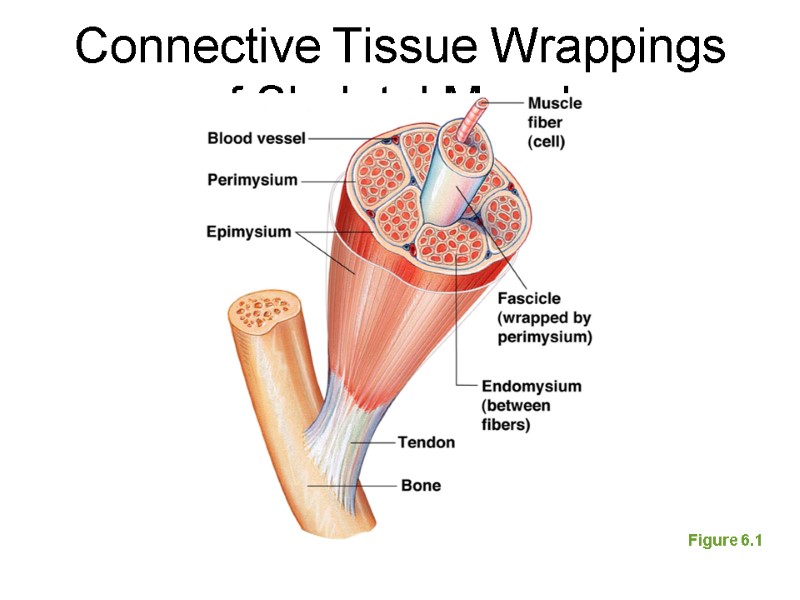
Connective Tissue Wrappings of Skeletal Muscle Figure 6.1
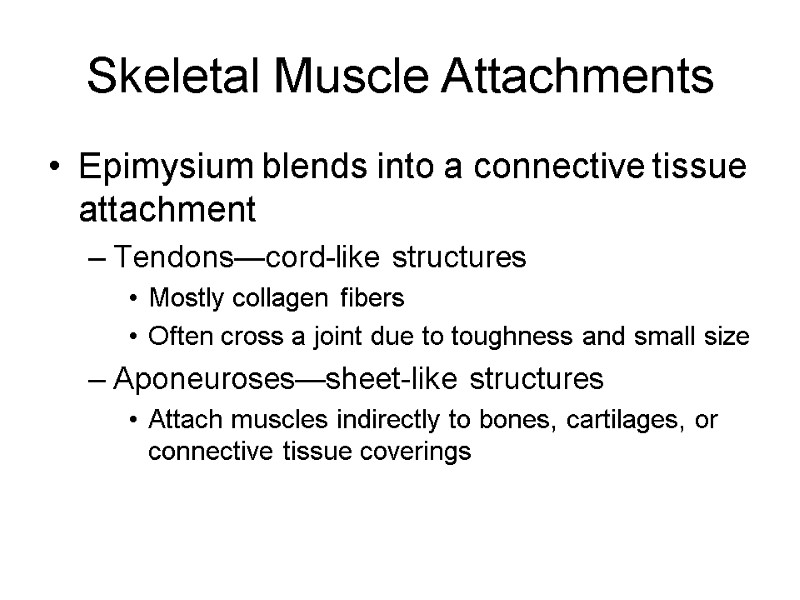
Skeletal Muscle Attachments Epimysium blends into a connective tissue attachment Tendons—cord-like structures Mostly collagen fibers Often cross a joint due to toughness and small size Aponeuroses—sheet-like structures Attach muscles indirectly to bones, cartilages, or connective tissue coverings
Smooth Muscle Characteristics Lacks striations Spindle-shaped cells Single nucleus Involuntary—no conscious control Found mainly in the walls of hollow organs
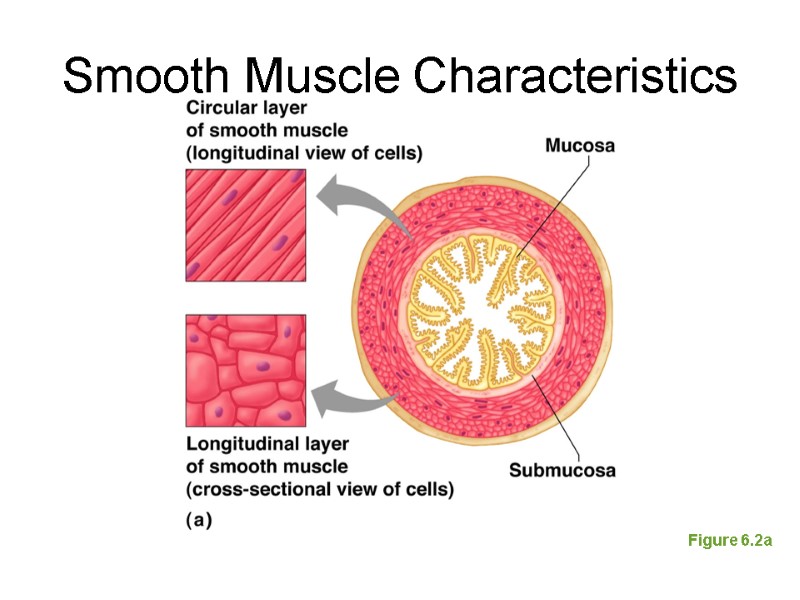
Smooth Muscle Characteristics Figure 6.2a
Cardiac Muscle Characteristics Striations Usually has a single nucleus Branching cells Joined to another muscle cell at an intercalated disc Involuntary Found only in the heart
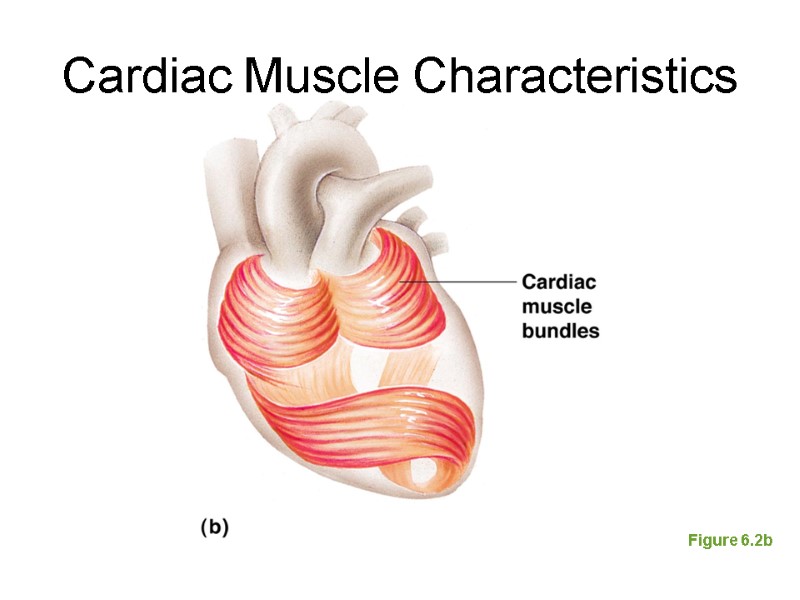
Cardiac Muscle Characteristics Figure 6.2b
Skeletal Muscle Functions Produce movement Maintain posture Stabilize joints Generate heat
Microscopic Anatomy of Skeletal Muscle Sarcolemma—specialized plasma membrane Myofibrils—long organelles inside muscle cell Sarcoplasmic reticulum—specialized smooth endoplasmic reticulum
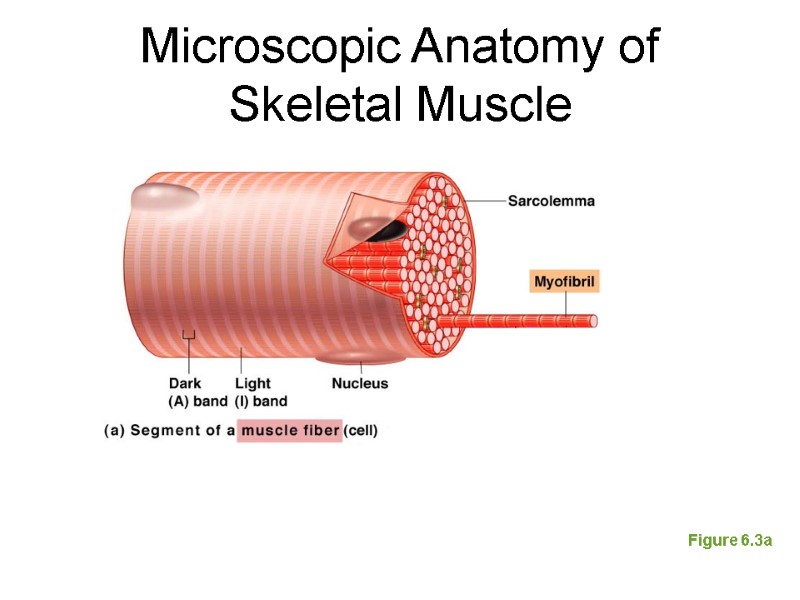
Microscopic Anatomy of Skeletal Muscle Figure 6.3a
Microscopic Anatomy of Skeletal Muscle Myofibrils are aligned to give distinct bands I band = light band Contains only thin filaments A band = dark band Contains the entire length of the thick filaments
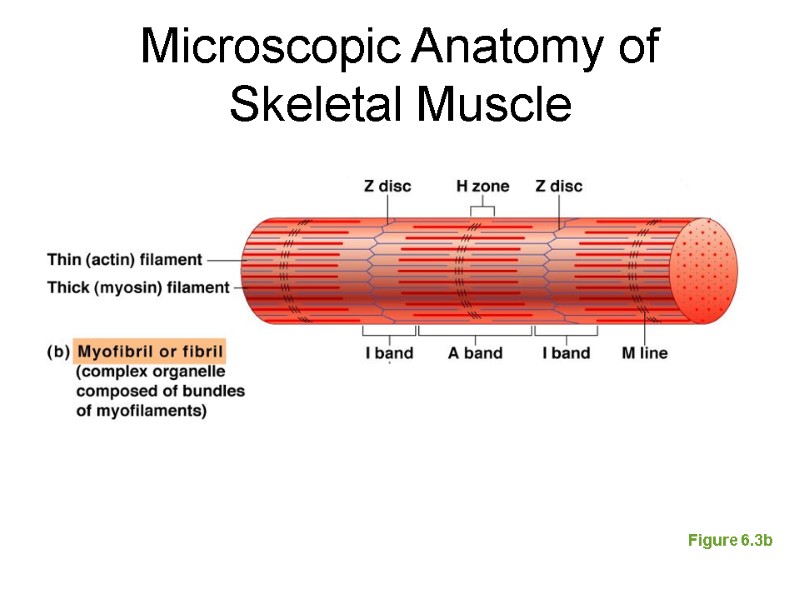
Microscopic Anatomy of Skeletal Muscle Figure 6.3b
Microscopic Anatomy of Skeletal Muscle Sarcomere—contractile unit of a muscle fiber Organization of the sarcomere Myofilaments Thick filaments = myosin filaments Thin filaments = actin filaments
Microscopic Anatomy of Skeletal Muscle Thick filaments = myosin filaments Composed of the protein myosin Has ATPase enzymes Myosin filaments have heads (extensions, or cross bridges) Myosin and actin overlap somewhat Thin filaments = actin filaments Composed of the protein actin Anchored to the Z disc
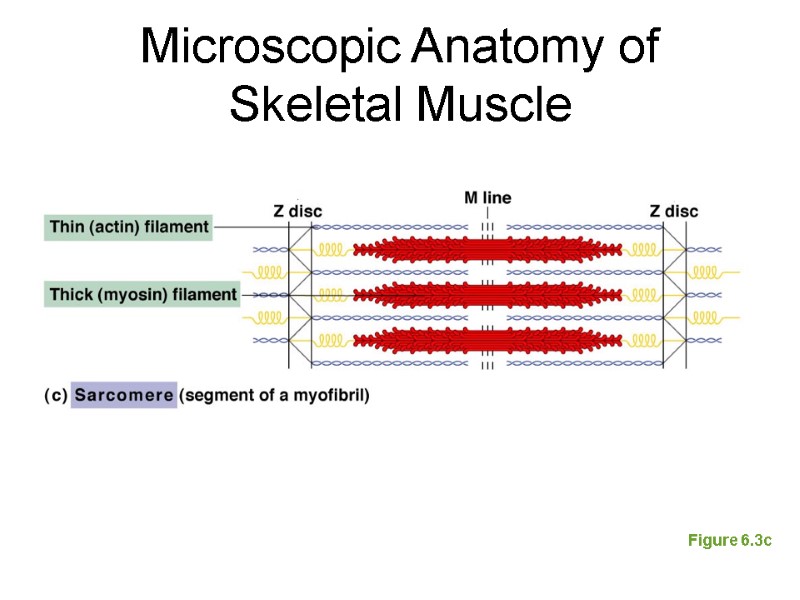
Microscopic Anatomy of Skeletal Muscle Figure 6.3c
Microscopic Anatomy of Skeletal Muscle At rest, there is a bare zone that lacks actin filaments called the H zone Sarcoplasmic reticulum (SR) Stores and releases calcium Surrounds the myofibril
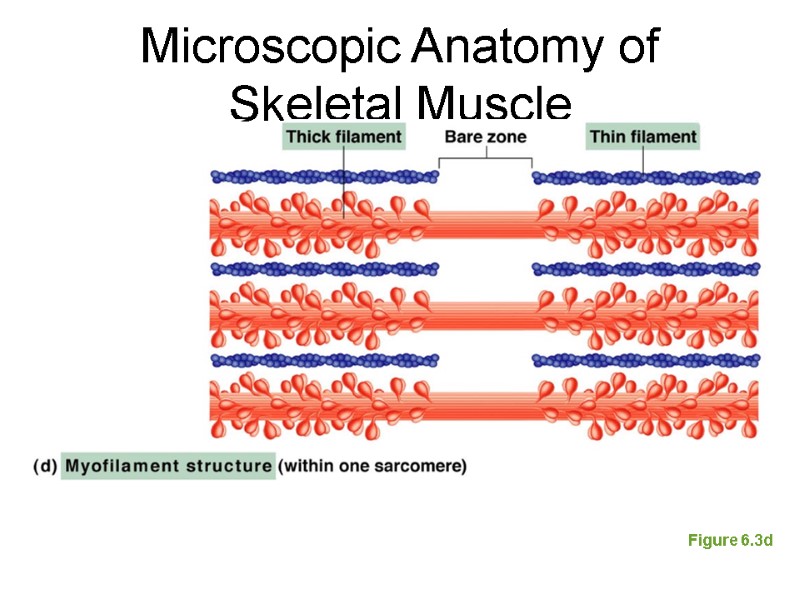
Microscopic Anatomy of Skeletal Muscle Figure 6.3d
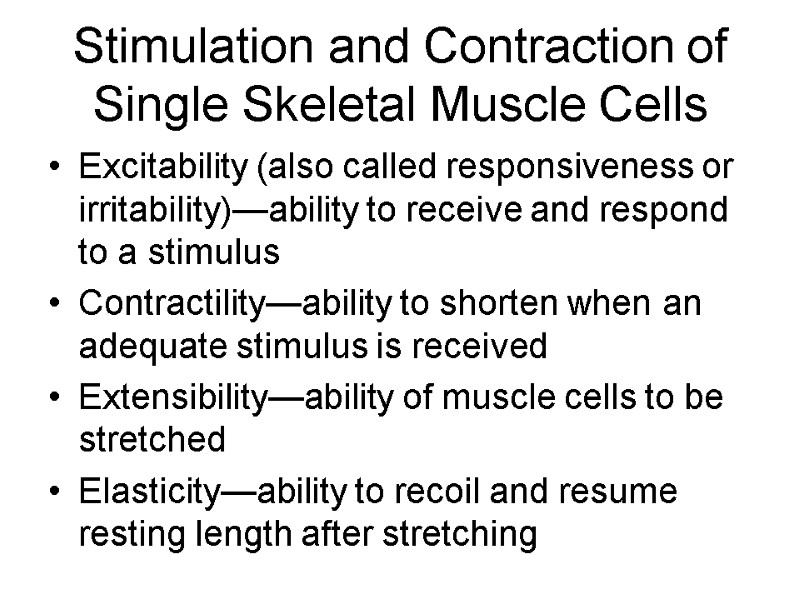
Stimulation and Contraction of Single Skeletal Muscle Cells Excitability (also called responsiveness or irritability)—ability to receive and respond to a stimulus Contractility—ability to shorten when an adequate stimulus is received Extensibility—ability of muscle cells to be stretched Elasticity—ability to recoil and resume resting length after stretching
The Nerve Stimulus and Action Potential Skeletal muscles must be stimulated by a motor neuron (nerve cell) to contract Motor unit—one motor neuron and all the skeletal muscle cells stimulated by that neuron
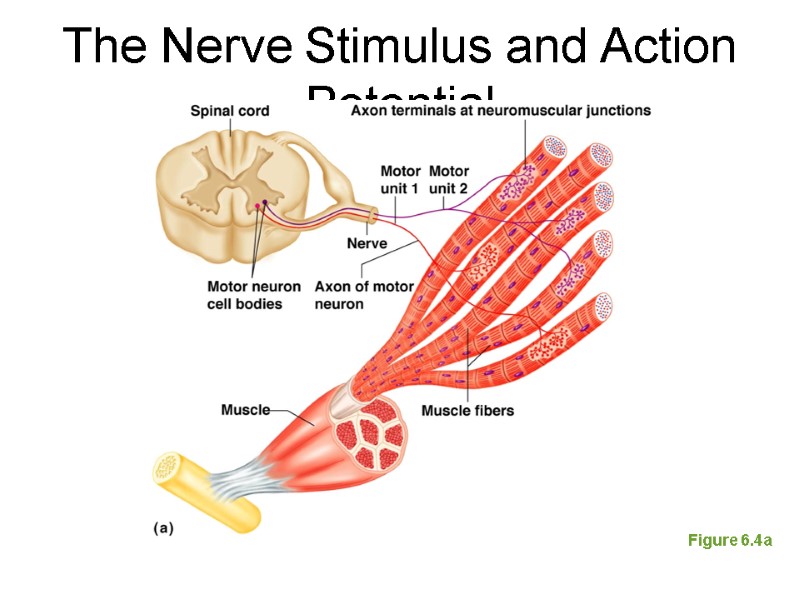
Figure 6.4a The Nerve Stimulus and Action Potential
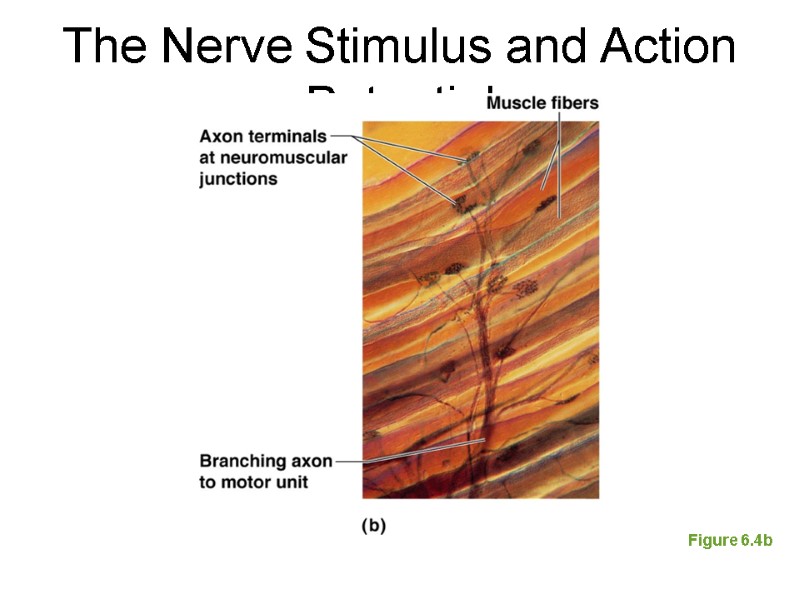
The Nerve Stimulus and Action Potential Figure 6.4b
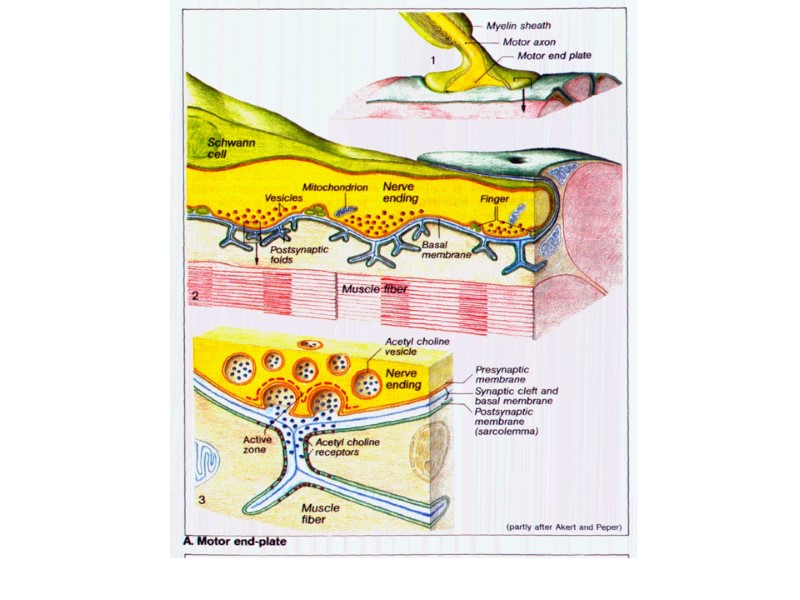
The Nerve Stimulus and Action Potential Neuromuscular junction Association site of axon terminal of the motor neuron and muscle
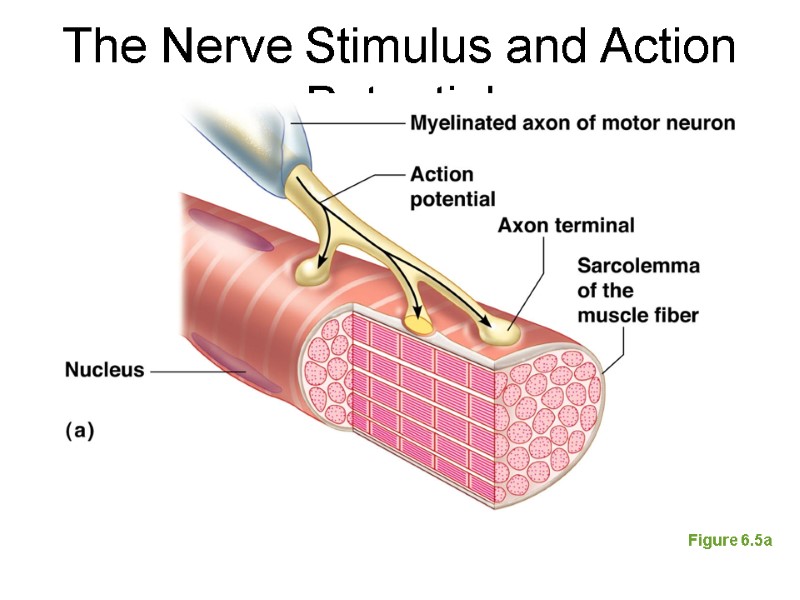
The Nerve Stimulus and Action Potential Figure 6.5a
The Nerve Stimulus and Action Potential Synaptic cleft Gap between nerve and muscle Nerve and muscle do not make contact Area between nerve and muscle is filled with interstitial fluid
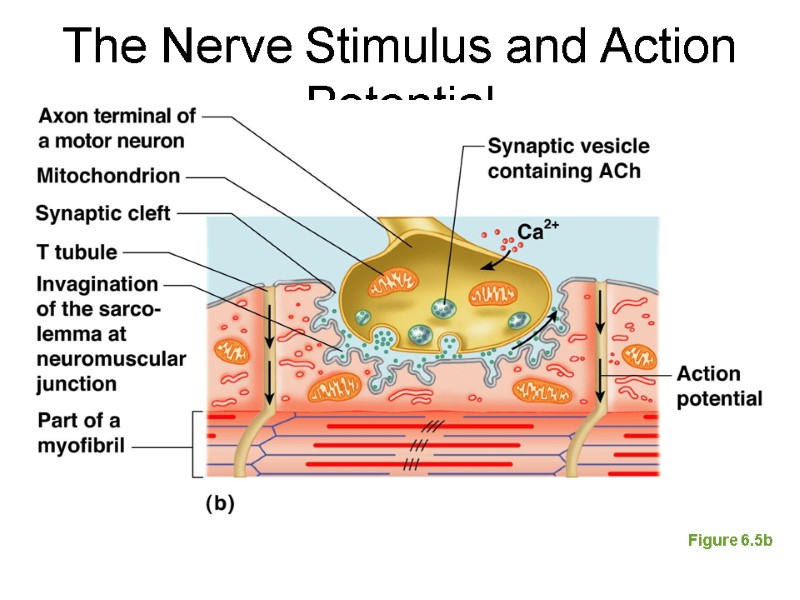
The Nerve Stimulus and Action Potential Figure 6.5b
Transmission of Nerve Impulse to Muscle Neurotransmitter—chemical released by nerve upon arrival of nerve impulse The neurotransmitter for skeletal muscle is acetylcholine (ACh) Acetylcholine attaches to receptors on the sarcolemma Sarcolemma becomes permeable to sodium (Na+), which rushes in, and potassium (K+), which rushes out
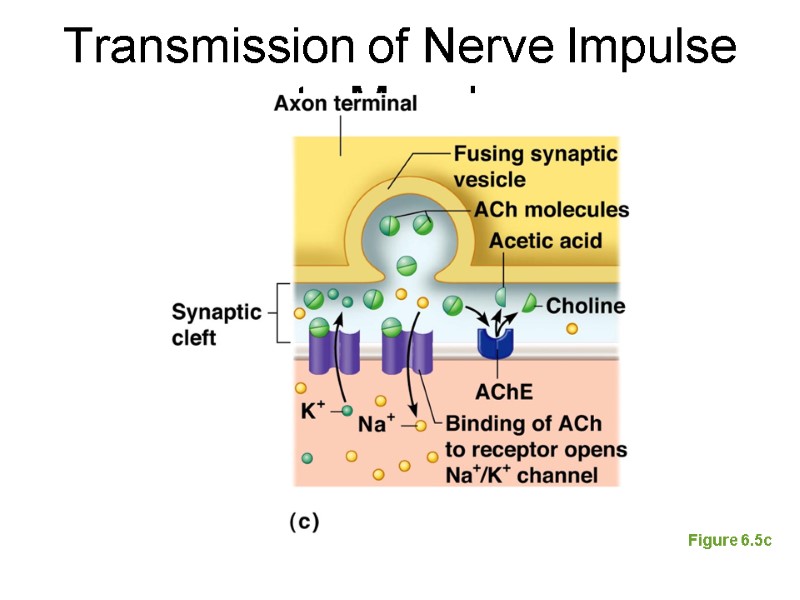
Transmission of Nerve Impulse to Muscle Figure 6.5c
Transmission of Nerve Impulse to Muscle Sodium rushes into the cell generating an action potential Once started, muscle contraction cannot be stopped
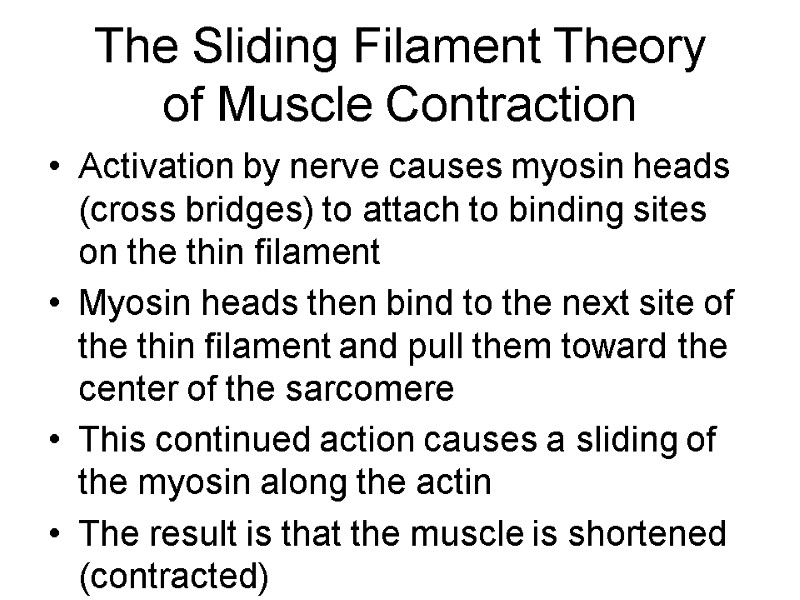
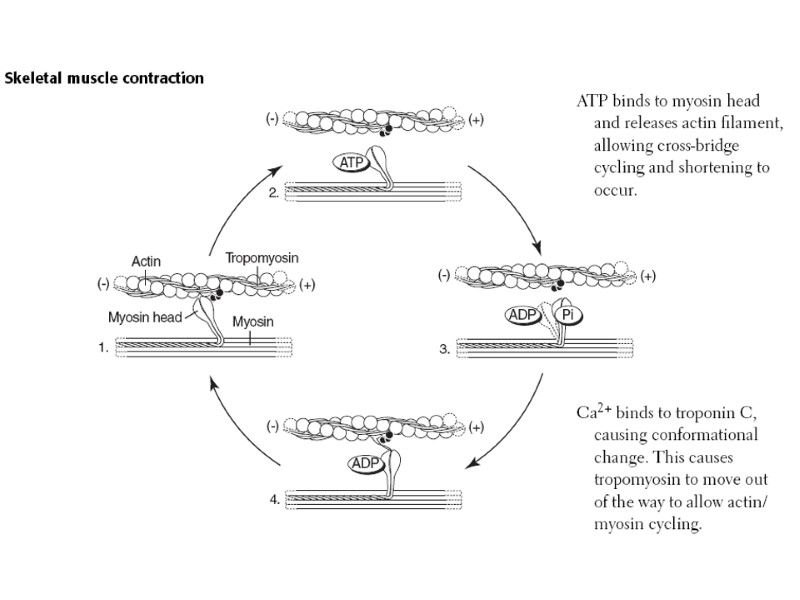
The Sliding Filament Theory of Muscle Contraction Activation by nerve causes myosin heads (cross bridges) to attach to binding sites on the thin filament Myosin heads then bind to the next site of the thin filament and pull them toward the center of the sarcomere This continued action causes a sliding of the myosin along the actin The result is that the muscle is shortened (contracted)
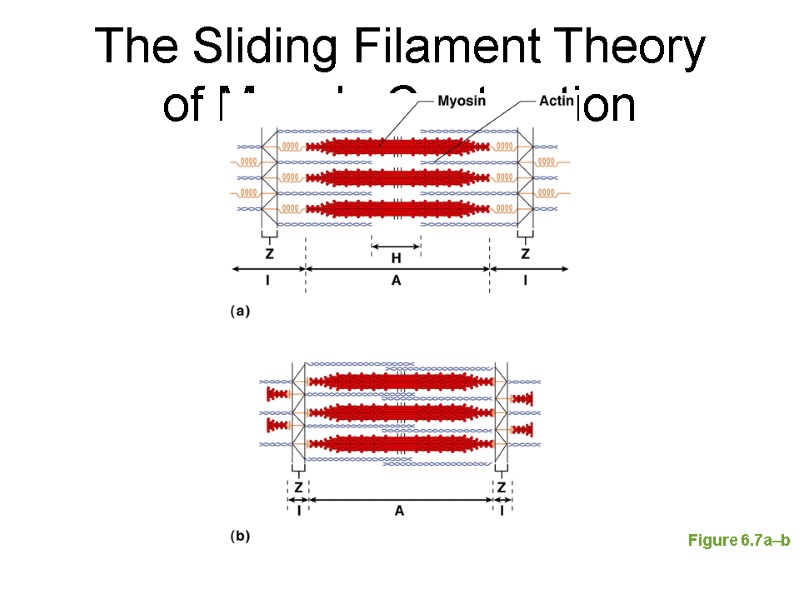
The Sliding Filament Theory of Muscle Contraction Figure 6.7a–b
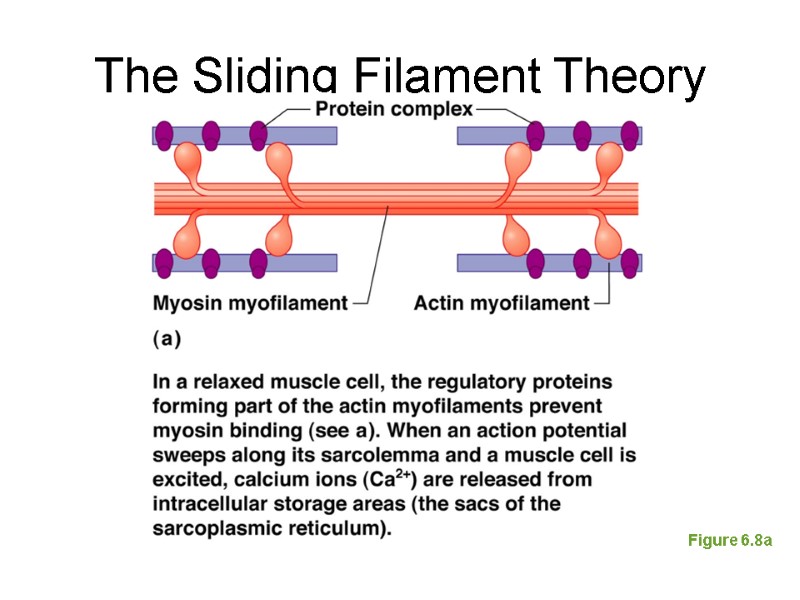
The Sliding Filament Theory Figure 6.8a
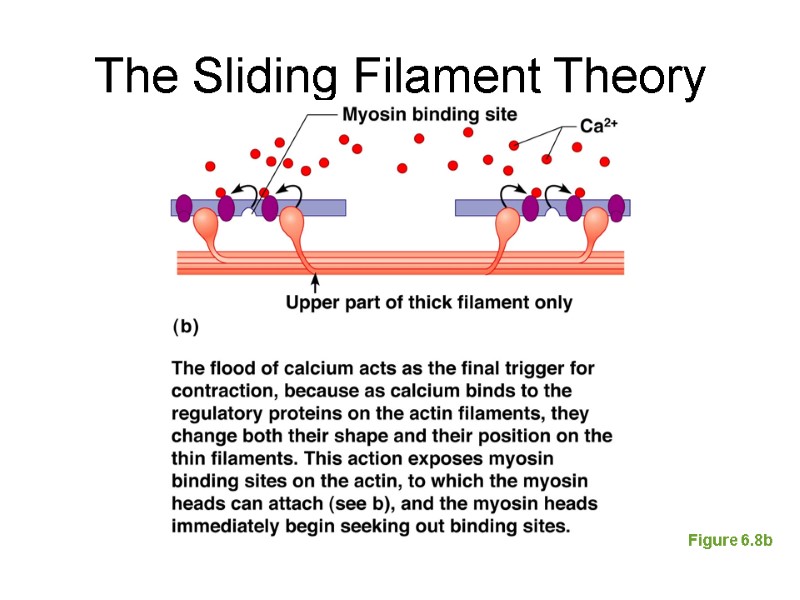
The Sliding Filament Theory Figure 6.8b
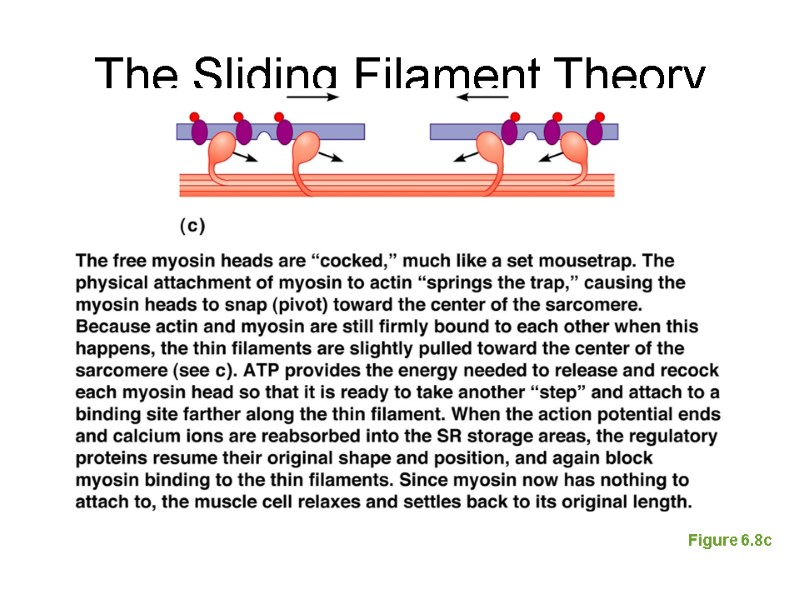
The Sliding Filament Theory Figure 6.8c
Contraction of Skeletal Muscle Muscle fiber contraction is “all or none” Within a skeletal muscle, not all fibers may be stimulated during the same interval Different combinations of muscle fiber contractions may give differing responses Graded responses—different degrees of skeletal muscle shortening
Contraction of Skeletal Muscle Graded responses can be produced by changing The frequency of muscle stimulation The number of muscle cells being stimulated at one time
The action potential is all-or-none The strength of the action potential is an intrinsic property of the cell. So long as they can reach the threshold of the cell, strong stimuli produce no stronger action potentials than weak ones. However, the strength of the stimulus is encoded in the frequency of the action potentials that it generates.
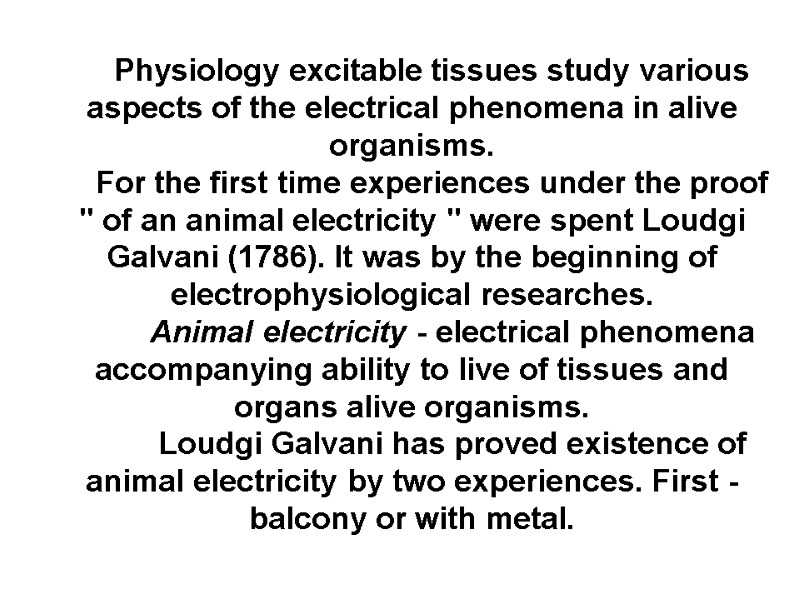
Physiology excitable tissues study various aspects of the electrical phenomena in alive organisms. For the first time experiences under the proof " of an animal electricity " were spent Loudgi Galvani (1786). It was by the beginning of electrophysiological researches. Animal electricity - electrical phenomena accompanying ability to live of tissues and organs alive organisms. Loudgi Galvani has proved existence of animal electricity by two experiences. First - balcony or with metal.
The first experience of Loudgi Galvani
The injured site carries a negative charge Intact site positive Charge The second experience of Loudgi Galvani - without metal (alteration potential).
Debut-Raymond has established, that the injured site carries a negative charge, and intact - positive. Therefore in a condition of rest between the outside and inside of the cell membrane there is a difference of potentials so called resting (membrane) potential amounts to 50-100 mV (cell interior is negative) in muscle and nerve cells.
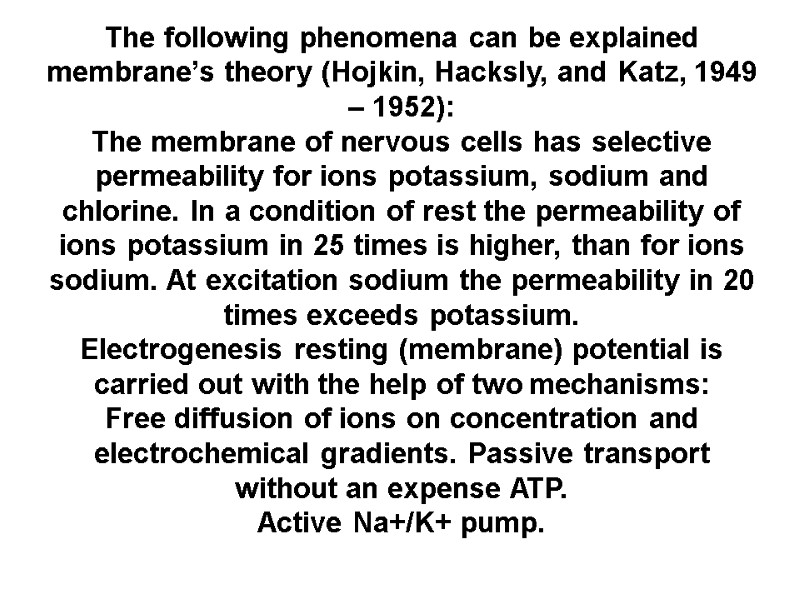
The following phenomena can be explained membrane’s theory (Hojkin, Hacksly, and Katz, 1949 – 1952): The membrane of nervous cells has selective permeability for ions potassium, sodium and chlorine. In a condition of rest the permeability of ions potassium in 25 times is higher, than for ions sodium. At excitation sodium the permeability in 20 times exceeds potassium. Electrogenesis resting (membrane) potential is carried out with the help of two mechanisms: Free diffusion of ions on concentration and electrochemical gradients. Passive transport without an expense ATP. Active Na+/K+ pump.
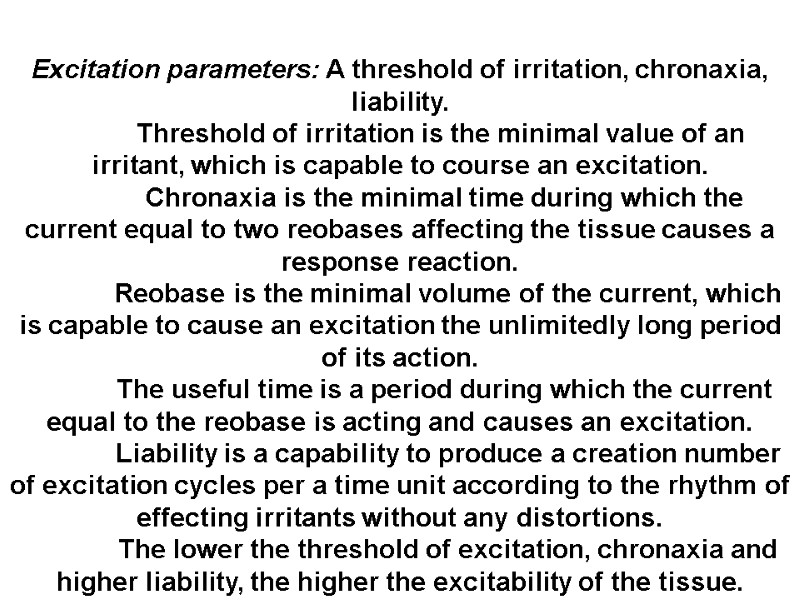
Excitation parameters: A threshold of irritation, chronaxia, liability. Threshold of irritation is the minimal value of an irritant, which is capable to course an excitation. Chronaxia is the minimal time during which the current equal to two reobases affecting the tissue causes a response reaction. Reobase is the minimal volume of the current, which is capable to cause an excitation the unlimitedly long period of its action. The useful time is a period during which the current equal to the reobase is acting and causes an excitation. Liability is a capability to produce a creation number of excitation cycles per a time unit according to the rhythm of effecting irritants without any distortions. The lower the threshold of excitation, chronaxia and higher liability, the higher the excitability of the tissue.
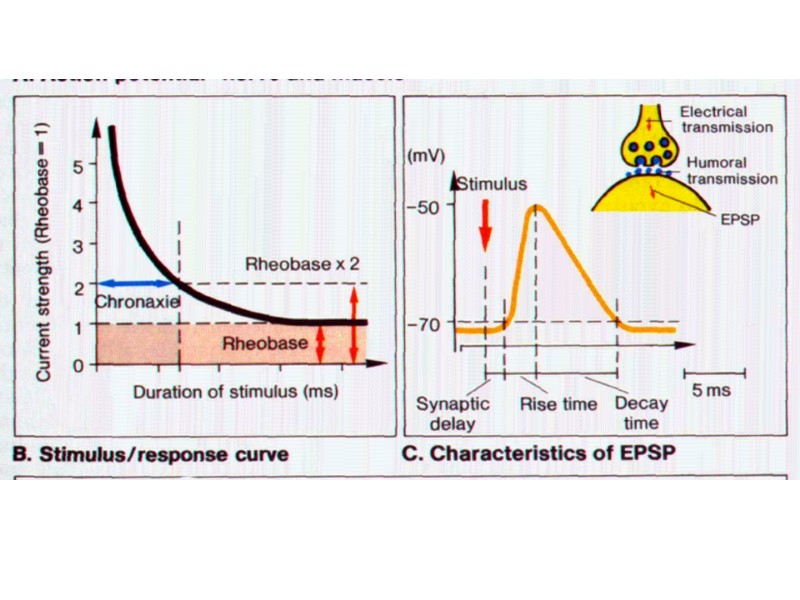
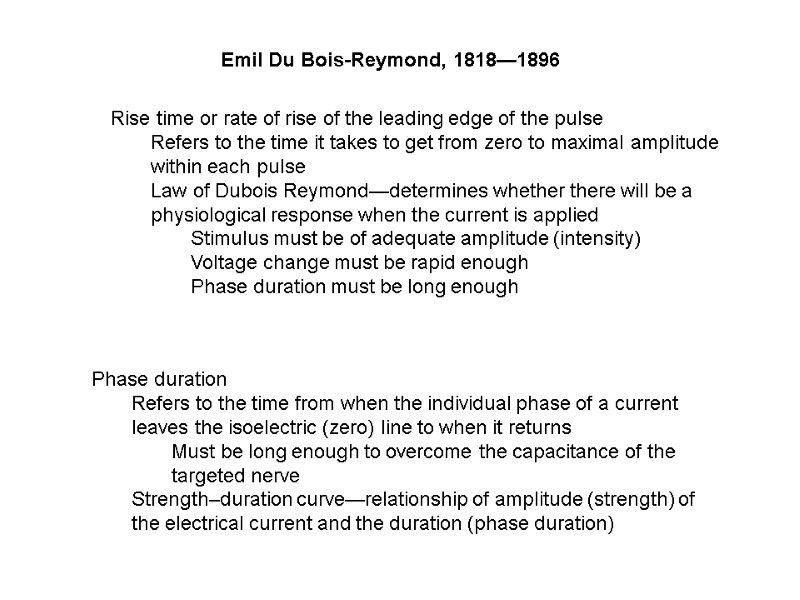
Emil Du Bois-Reymond, 1818—1896 Rise time or rate of rise of the leading edge of the pulse Refers to the time it takes to get from zero to maximal amplitude within each pulse Law of Dubois Reymond—determines whether there will be a physiological response when the current is applied Stimulus must be of adequate amplitude (intensity) Voltage change must be rapid enough Phase duration must be long enough Phase duration Refers to the time from when the individual phase of a current leaves the isoelectric (zero) line to when it returns Must be long enough to overcome the capacitance of the targeted nerve Strength–duration curve—relationship of amplitude (strength) of the electrical current and the duration (phase duration)
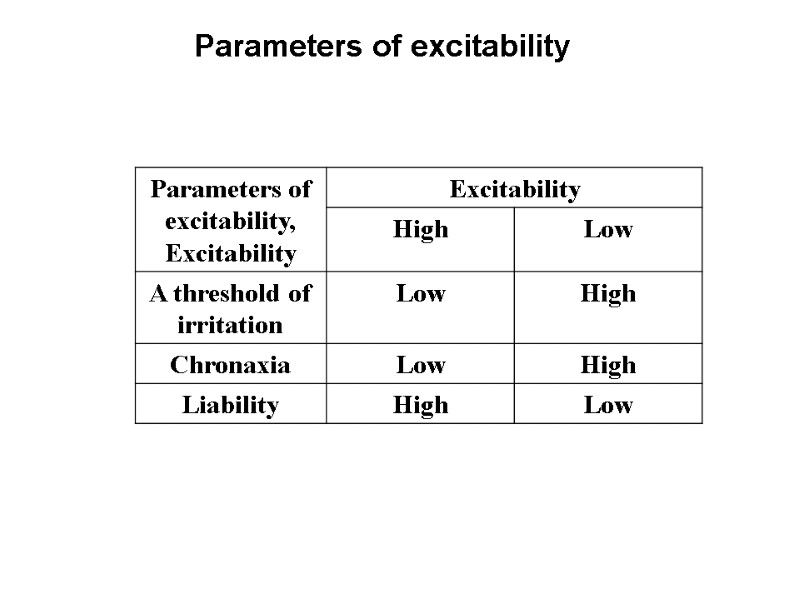
Parameters of excitability
In non-myeliminated fibers an excitation is conducted serial and in myeliminated fibers – saltatoricly (somersault) (from one node of Ranvier to another)
Physiological properties of nerve fibers: excitability, conductivity, contractility, and lability. Excitability and lability of a nerve fiber is higher and the refractory period is shorter than in the muscular tissue. Conduction of an excitation is a special function of nerve fibers.
Laws conduction of excitation via nerve fibers, The law of two-way conduction via a nerve fiber, The law of the anatomic and physiologic integrity, The law of an isolated conduction of excitation through a nerve fiber (Gasser and Erlanger, 1937). Types of nerve fibers: A, B, C. They are characterized according to the conduction rate diameter, the structure (myelinated – non-myelinated).
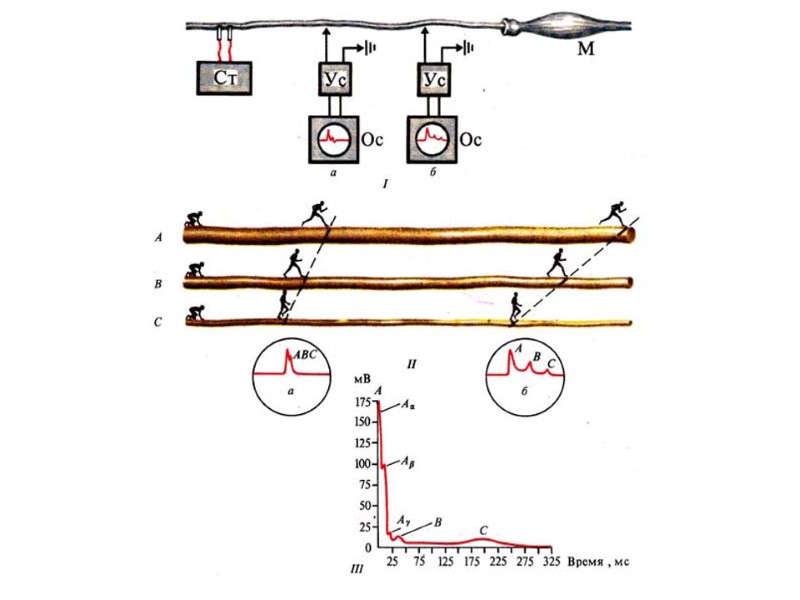
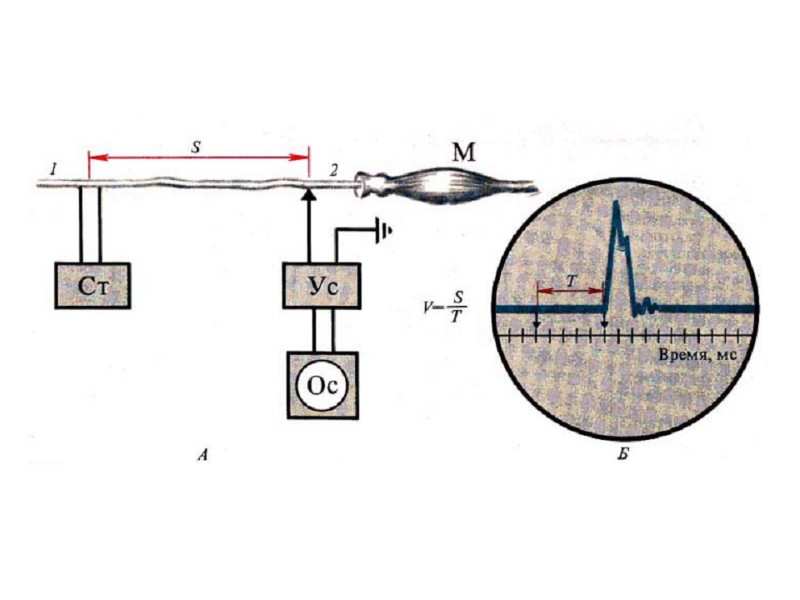
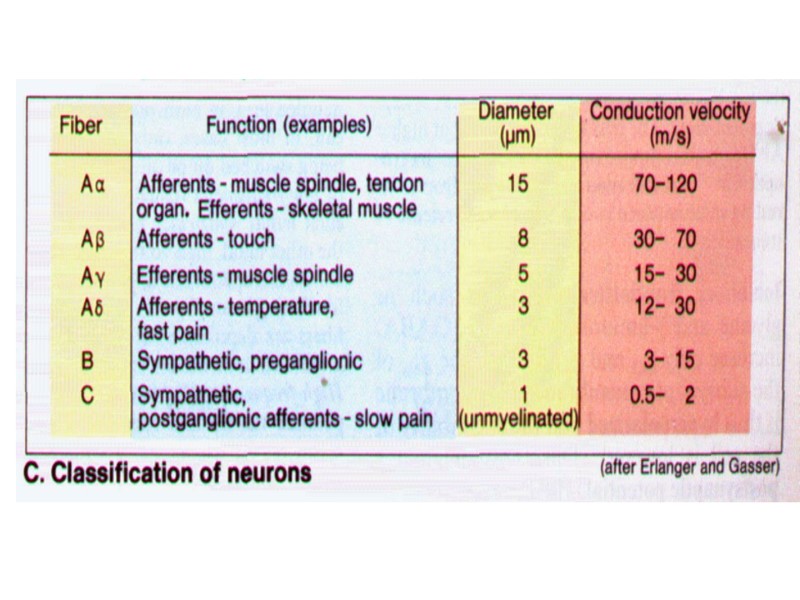
Conclusion from Erlanger-Gasser experiment: The conduction of excitation (action potentials) in a nervous trunk occurs is isolated. Conduction velocity of AP directly proportional to a diameter of a nervous and myelinated.
Generation AP. it is possible to find out the following bioelectrical reactions: In reply to action of stimulus by size < 0,5 from threshold arises electrotonic potential 2. The local answer arises in reply to subliminal [subthreshold] stimulus (0,5 - 0,9 from threshold), local answer (EPSP – excitatory postsynaptic potential; IPSP – inhibitory postsynaptic potential): 1) Arises in reply to action subliminal [subthreshold] stimulus (0,5 - 0,9 from threshold);
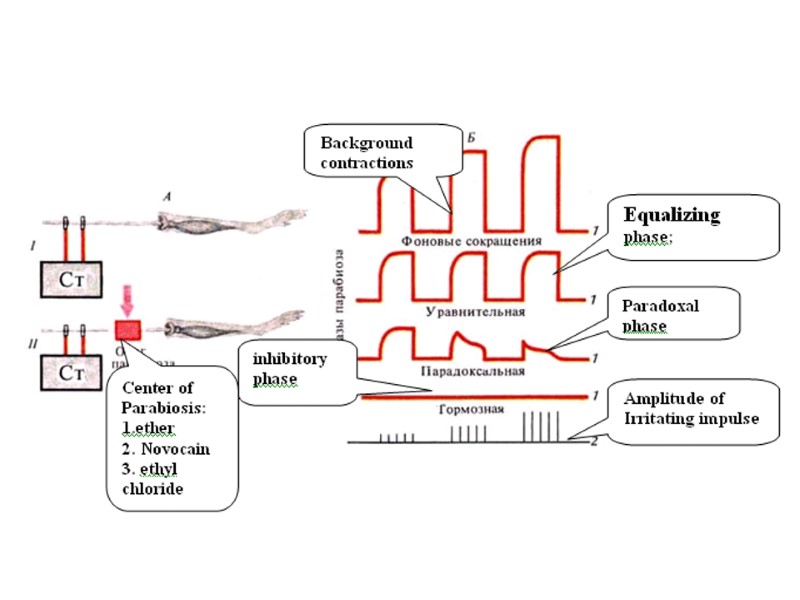
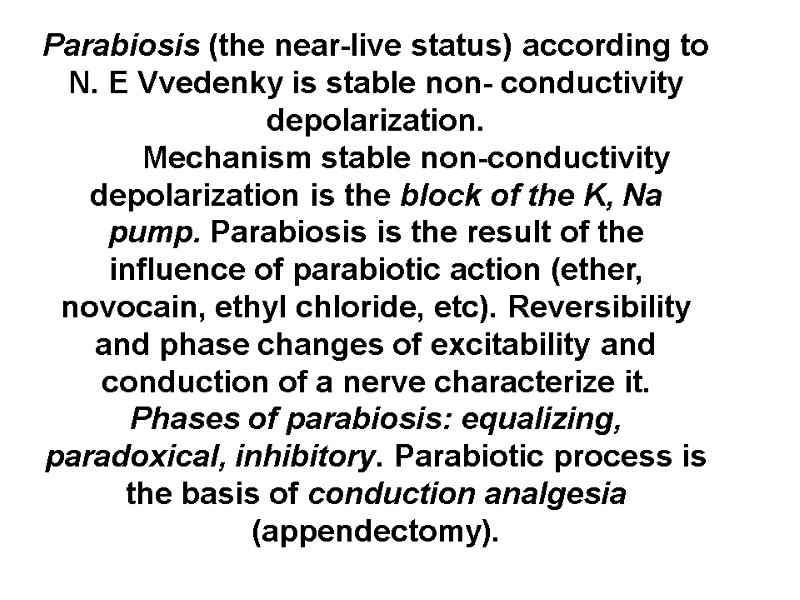
Parabiosis (the near-live status) according to N. E Vvedenky is stable non- conductivity depolarization. Mechanism stable non-conductivity depolarization is the block of the K, Na pump. Parabiosis is the result of the influence of parabiotic action (ether, novocain, ethyl chloride, etc). Reversibility and phase changes of excitability and conduction of a nerve characterize it. Phases of parabiosis: equalizing, paradoxical, inhibitory. Parabiotic process is the basis of conduction analgesia (appendectomy).
Physiologic properties of chemical synapses: One direction conduction of the excitation; synaptic delay; transmission of excitation with the help of a mediator; transformation of the rhythm of excitation, low liability; high fatigability; high sensibility to chemical substances including pharmaceuticals. high sensibility to hypoxia.
Classification of synapse. Peripheral and central, exciting and inhibiting; chemical, electrical, combined: cholinergic, adrenergic, dophaminergic, serotoninergic etc. (for chemical synapses). The structure of a synapse.
THE LAWS OF CONDUCTION IN NERVES 1.The law of physiological continuity of a nerve fiber. Ligation, excessive tension, action of cold or heat, stoppage of blood supply, effect of local anaesthetics will block conduction. 2.The law of two-way conduction. Scheme of experiment: a stimulus is applied between two pairs of measuring electrodes. The AP is recorded on the left and on the right. 3.The law of isolated conduction. A peripheral nerve tract consists of a large number of fibers (motor, sensory, vegetative), but impulses are conducted separately, without passing from one fiber to another. 4.The relative indefatigability of a nerve. A nerve can generate and conduct the impulses continuously for a long time (8-10 hours under experimental conditions). 5.High lability of a nerve. Lability (functional mobility) is ability to generate AP with the most frequency. The shorter refractory period, the higher lability of the excitable tissue is observed. Lability of nerve fibers is 500 to 1000 imp/sec; lability of skeletal muscular fibers is about 250 imp/sec. CONCLUSION: nerve fibers are adapted to conduct impulses in the best form.
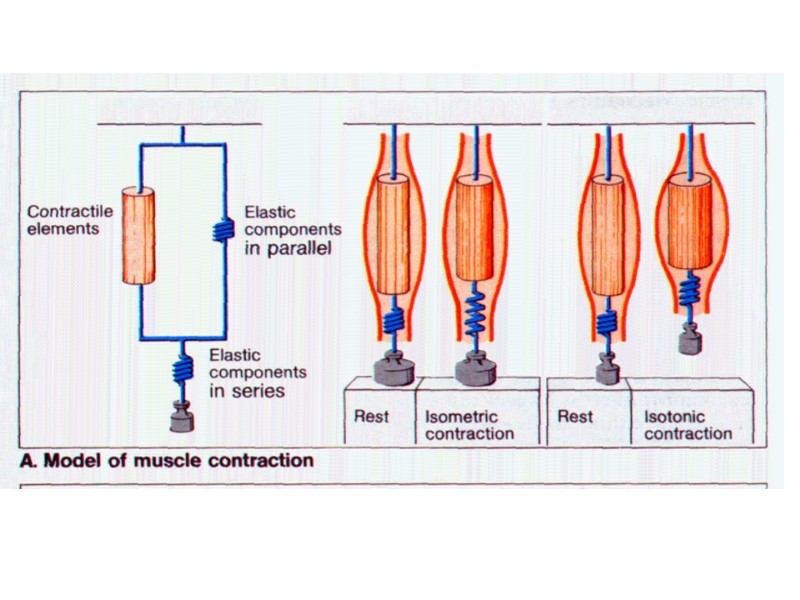
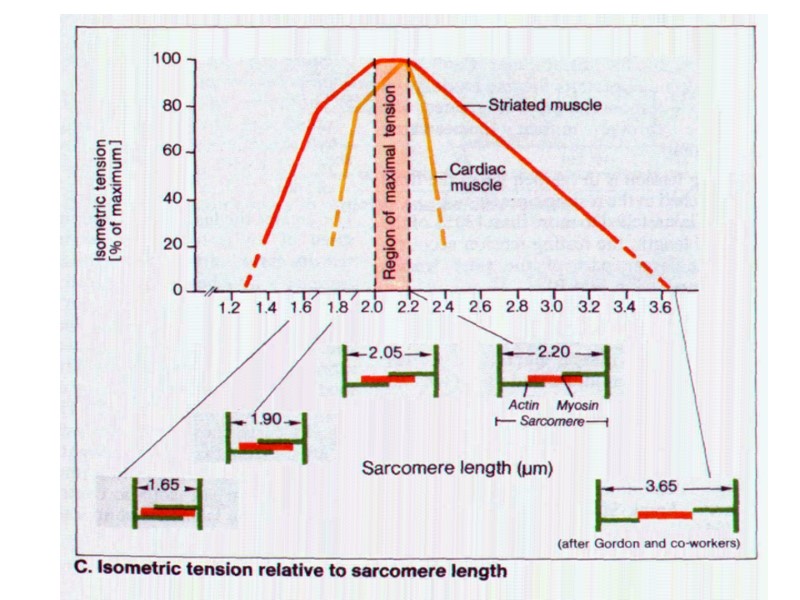
SKELETAL MUSCLE. SKELETAL MUSCLE FIBER Sarcolemma – plasma membrane + thin layer of polysaccharide material that contains collagen fibers. Myofibrils: 100-1000 in each muscle fiber. Each myofibril has about 1500 myosin filaments and 3000 actin filaments. Myosin and actin are large polymerized protein molecules; they are responsible for muscle contraction. Myosin and actin filaments are partly interdigitated, that is why myofibrils have light and dark bands: light band – isotropic (only actin filaments) and dark band – anisotropic (myosin and actin filaments). It is so-called “transverse striation”. There are small projections from the side of the myosin filament. These are cross-bridges. Interaction between myosin cross-bridges and the actin filament causes contraction. The ends of the actin filaments are attached to transverse Z-discs. The portion of the myofibril that lies between two Z-discs is called sarcomere. At rest the length of sarcomere is about 2 mcm (note: at this length the sarcomere is capable of generating its greatest force of contraction).
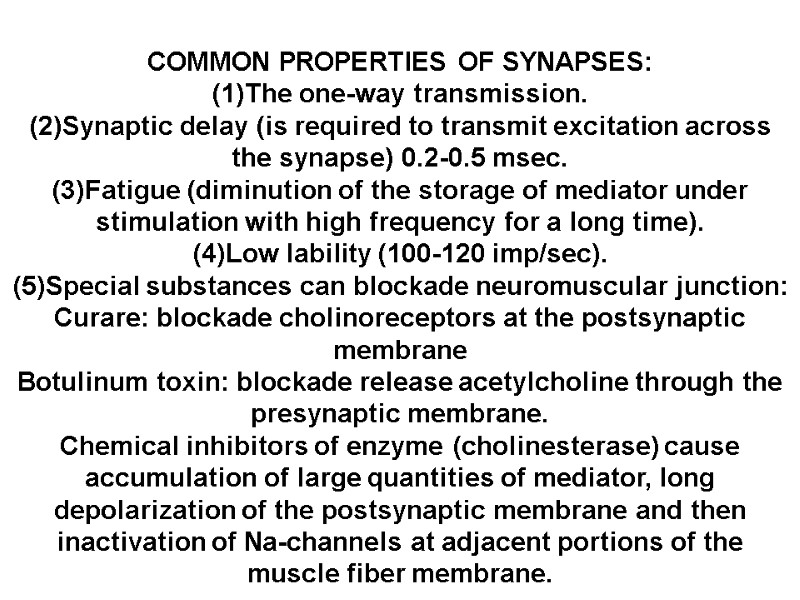
COMMON PROPERTIES OF SYNAPSES: (1)The one-way transmission. (2)Synaptic delay (is required to transmit excitation across the synapse) 0.2-0.5 msec. (3)Fatigue (diminution of the storage of mediator under stimulation with high frequency for a long time). (4)Low lability (100-120 imp/sec). (5)Special substances can blockade neuromuscular junction: Curare: blockade cholinoreceptors at the postsynaptic membrane Botulinum toxin: blockade release acetylcholine through the presynaptic membrane. Chemical inhibitors of enzyme (cholinesterase) cause accumulation of large quantities of mediator, long depolarization of the postsynaptic membrane and then inactivation of Na-channels at adjacent portions of the muscle fiber membrane.
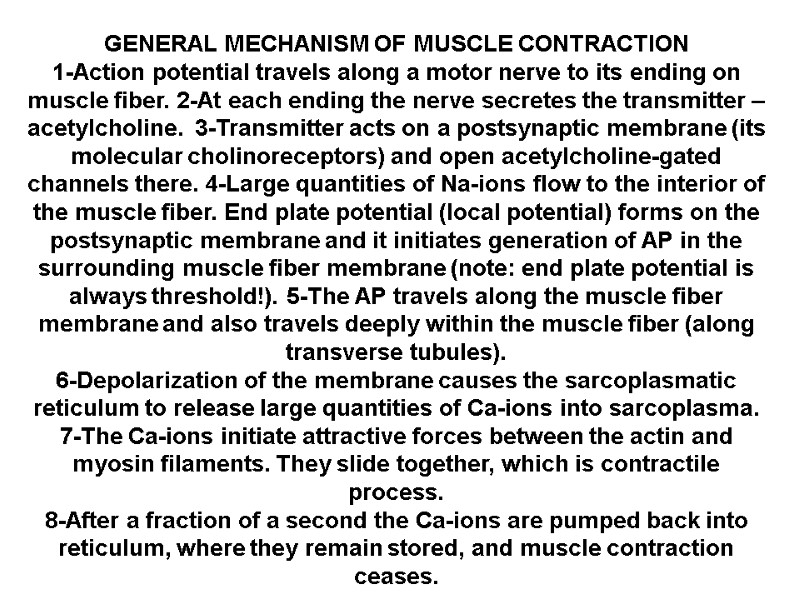
GENERAL MECHANISM OF MUSCLE CONTRACTION 1-Action potential travels along a motor nerve to its ending on muscle fiber. 2-At each ending the nerve secretes the transmitter – acetylcholine. 3-Transmitter acts on a postsynaptic membrane (its molecular cholinoreceptors) and open acetylcholine-gated channels there. 4-Large quantities of Na-ions flow to the interior of the muscle fiber. End plate potential (local potential) forms on the postsynaptic membrane and it initiates generation of AP in the surrounding muscle fiber membrane (note: end plate potential is always threshold!). 5-The AP travels along the muscle fiber membrane and also travels deeply within the muscle fiber (along transverse tubules). 6-Depolarization of the membrane causes the sarcoplasmatic reticulum to release large quantities of Ca-ions into sarcoplasma. 7-The Ca-ions initiate attractive forces between the actin and myosin filaments. They slide together, which is contractile process. 8-After a fraction of a second the Ca-ions are pumped back into reticulum, where they remain stored, and muscle contraction ceases.
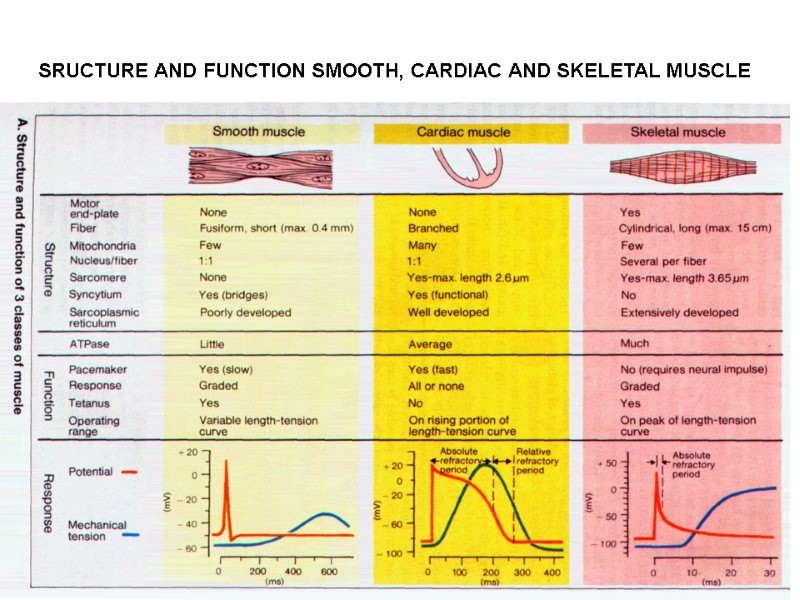
SRUCTURE AND FUNCTION SMOOTH, CARDIAC AND SKELETAL MUSCLE

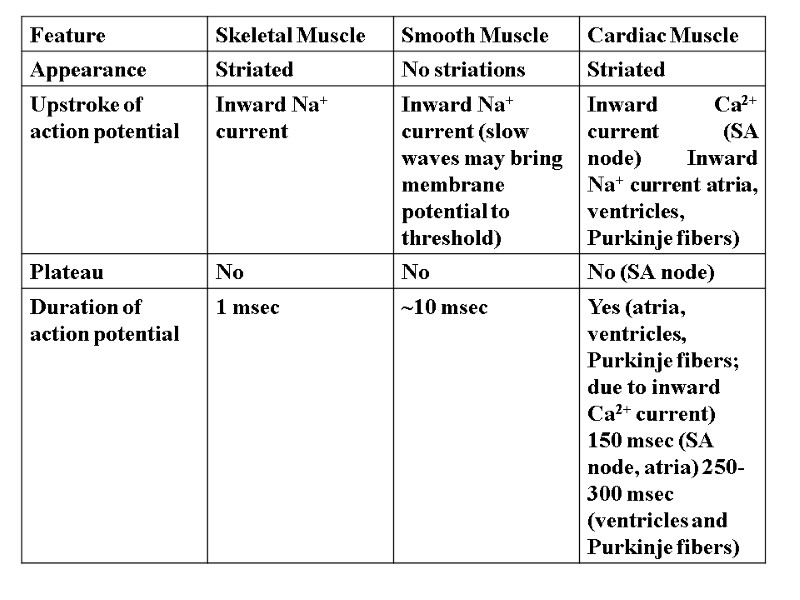
Physiology of muscles. Types of muscles: Striated skeletal muscles, striated cardiac muscles, smooth muscles of the interior organs, vessels. Physical properties of the skeletal muscles: excitability, conduction, contraction, lability.
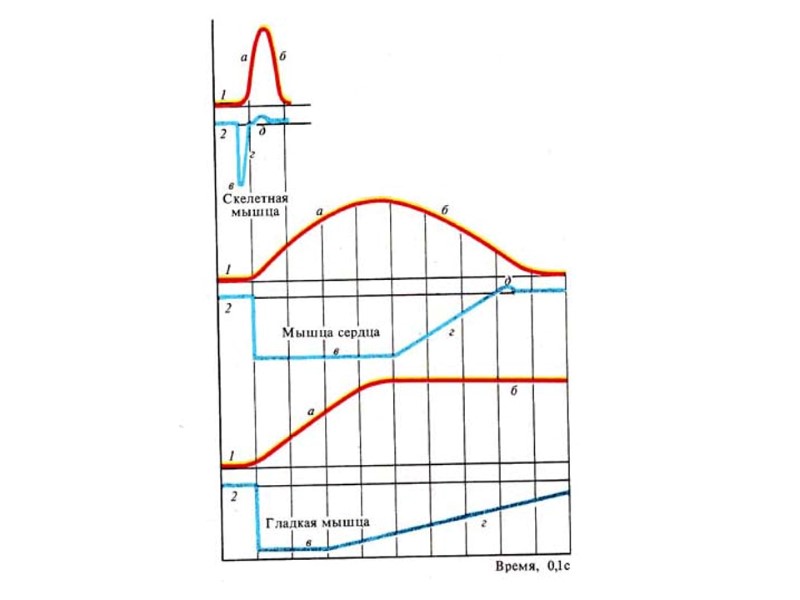
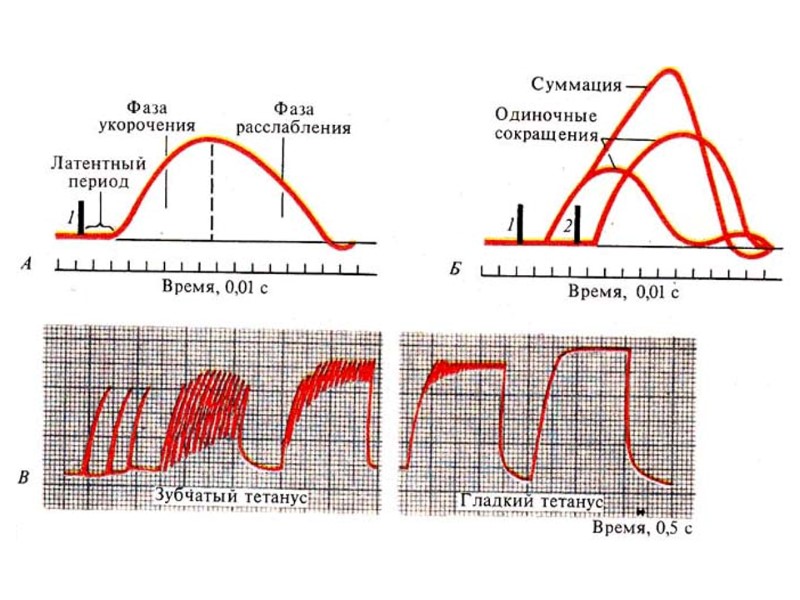
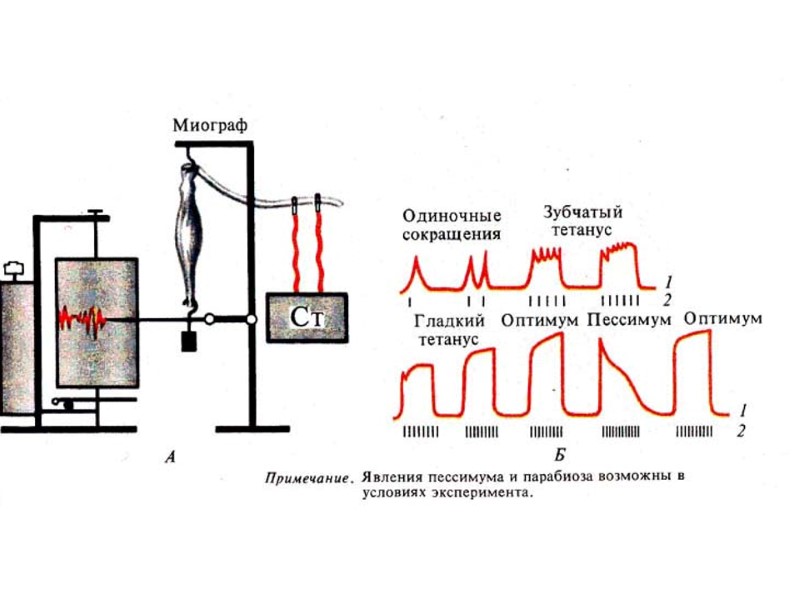
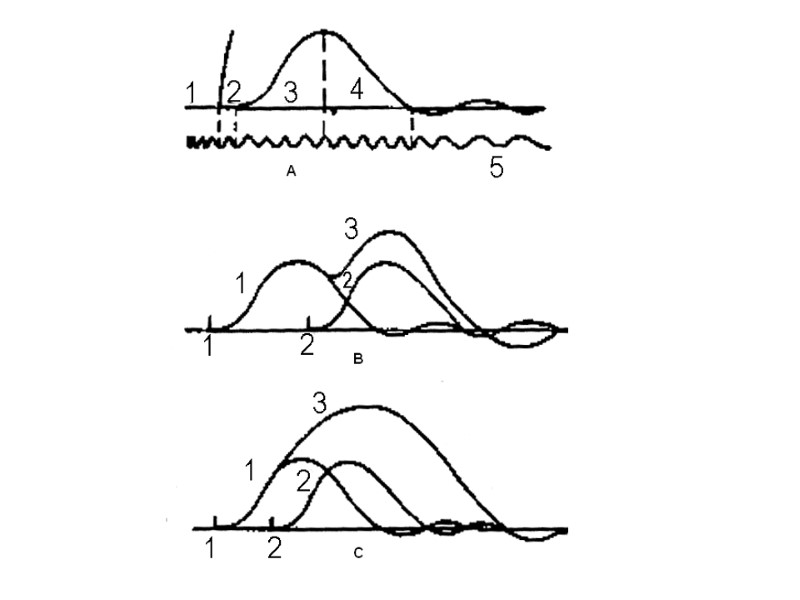
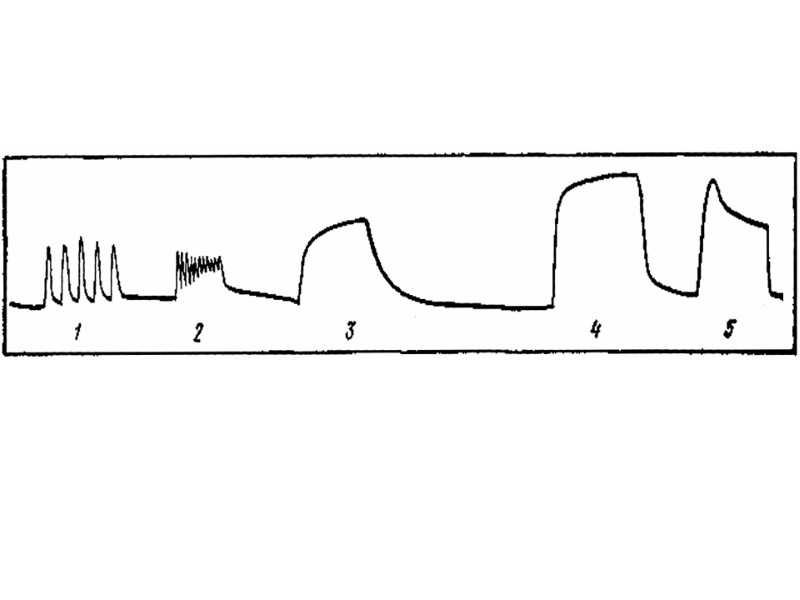
Types of muscular contraction: single muscular contraction are a muscular reaction to a single threshhold or over-threshold stimulus. Phases a single musclurar contraction (only in experiment): a latent period, a phase of relaxation. Summation of single muscular contractions occurs if during a single contraction the second irritation of the muscle comes. The full summation occurs if the second irritation comes during the muscular contraction. Partial summation occurs if the second irritation comes during the relaxation phase. The amplitude of contraction in the full summation is higher compared to the amplitude in the partial summation.
Tetanus is a long-term muscular contraction in response to the rhythmic irritation. It requires a lot of energy. Types of tetanus: Incomplete (every next impulse comes to the muscular during the phase of relaxation) and complete (impulse come during the phase of contraction). Optimum of the phase irritation frequency is the frequency of the complete tetanus under which the maximal amplitude of the smooth tetanus is observed. Pessimum of the irritated frequency is the frequency of the complete tetanus under which the minimal amplitude of the complete tetanus is observed.
Mechanism of muscular contraction: a nerve impulse, Ca-ions release, interaction with the troponin-tropomyosin complex, opening of the active points on the actin filaments, interaction with the active points of the myosinal heads, receiving of the ATP energy, sliding of actin and myosin filaments. Contracture is a long-term muscular contraction lasting also after ceasing of the irritant. It occurs in metabolic disorders or changes of properties of the muscular contracted proteins.
Comparative characteristics of the skeletal cardiac and smooth muscles. Skeletal muscles are characterized by the compliance to the graduality law, the lowest values of chronaxia, refractory period and duration of a single contraction, pronounced degree of elasticity, high velocity of the excitation conduction and lability, they are voluntarily controlled and innervated by the somatic nervous system. Smooth muscles are characterized by the absence of graduality of responses, they don’t comply with the law “all or nothing”, they are able to produce long-term tonic contractions, and they are also characterized by plasticity, a significant refractory period (tenth points of seconds), durable single contractions (dozens of second and longer), they are not controlled voluntarily and they receive innervation from the vegetative nervous system.
The cardiac muscle is characterized by the law “all or none”, the morphology basis is functional syncytium and a long refractory period (0.3 sec); presence of the special atypical tissue with the conductive function and characterized by automatism; the cardiac muscle can’t be controlled voluntarily, it is innervated by the vegetative nervous system.
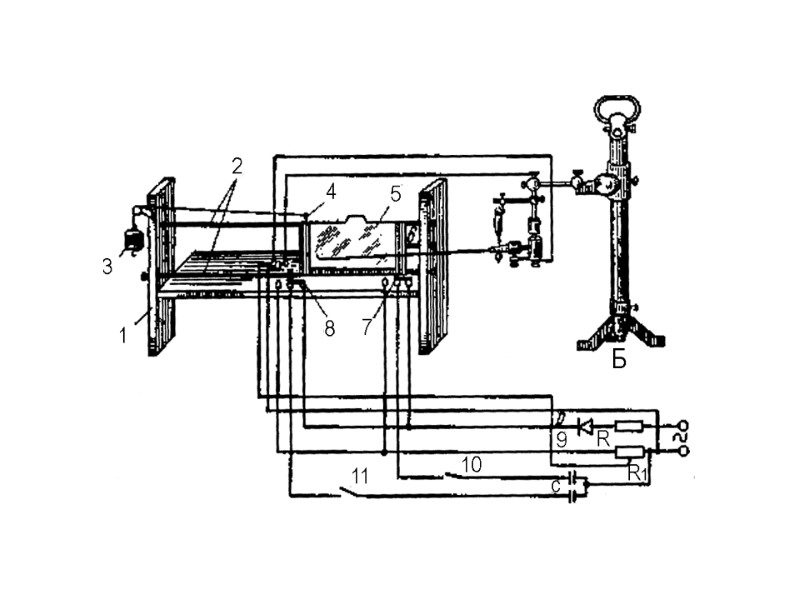
SINGLE MUSCULAR CONTRACTION AND SUMMATION Single muscular contraction is a reaction of a muscle in reply to single threshold or superthreshold stimulus. Apparatus: the fall-apparatus, myograph, time marker, a universal support, a set preparation tools, a pipette, Ringer’s, solution, cotton wool.
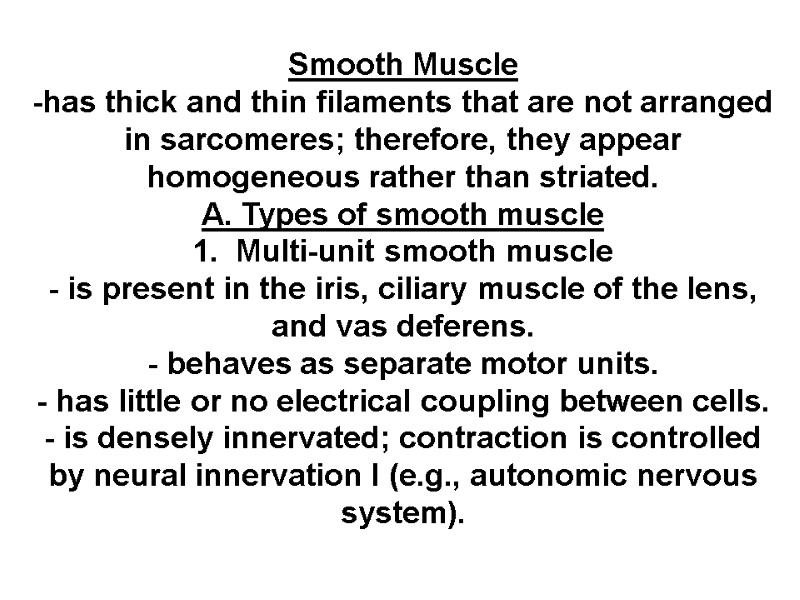
Smooth Muscle -has thick and thin filaments that are not arranged in sarcomeres; therefore, they appear homogeneous rather than striated. A. Types of smooth muscle 1. Multi-unit smooth muscle - is present in the iris, ciliary muscle of the lens, and vas deferens. - behaves as separate motor units. - has little or no electrical coupling between cells. - is densely innervated; contraction is controlled by neural innervation I (e.g., autonomic nervous system).
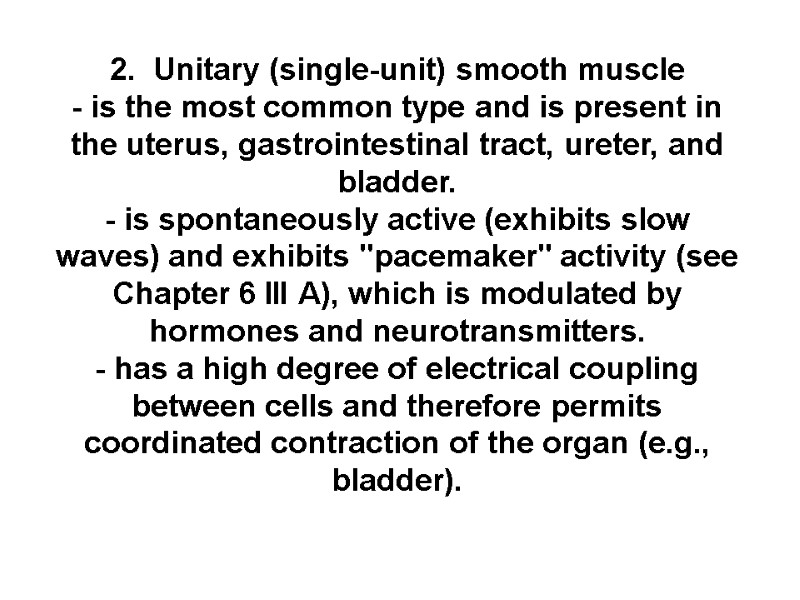
2. Unitary (single-unit) smooth muscle - is the most common type and is present in the uterus, gastrointestinal tract, ureter, and bladder. - is spontaneously active (exhibits slow waves) and exhibits "pacemaker" activity (see Chapter 6 III A), which is modulated by hormones and neurotransmitters. - has a high degree of electrical coupling between cells and therefore permits coordinated contraction of the organ (e.g., bladder).
3. Vascular smooth muscle - has properties of both multi-unit and single-unit smooth muscle.
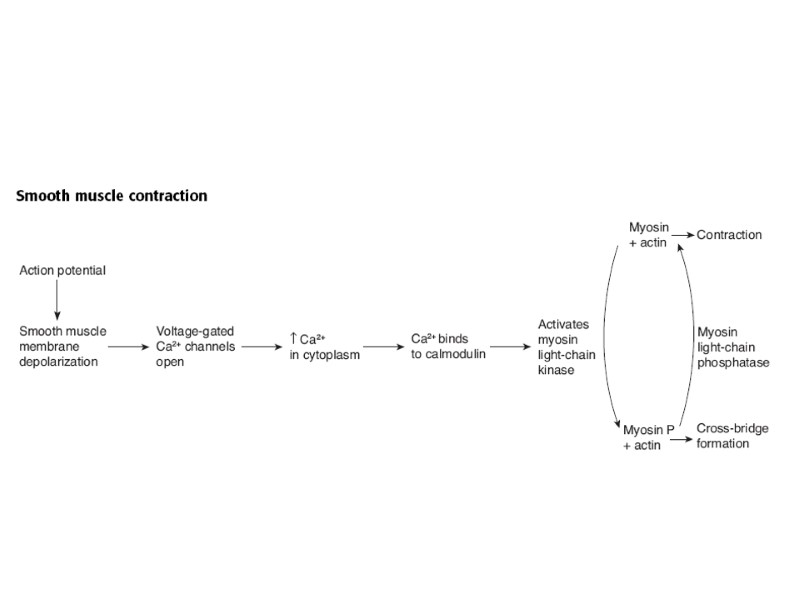
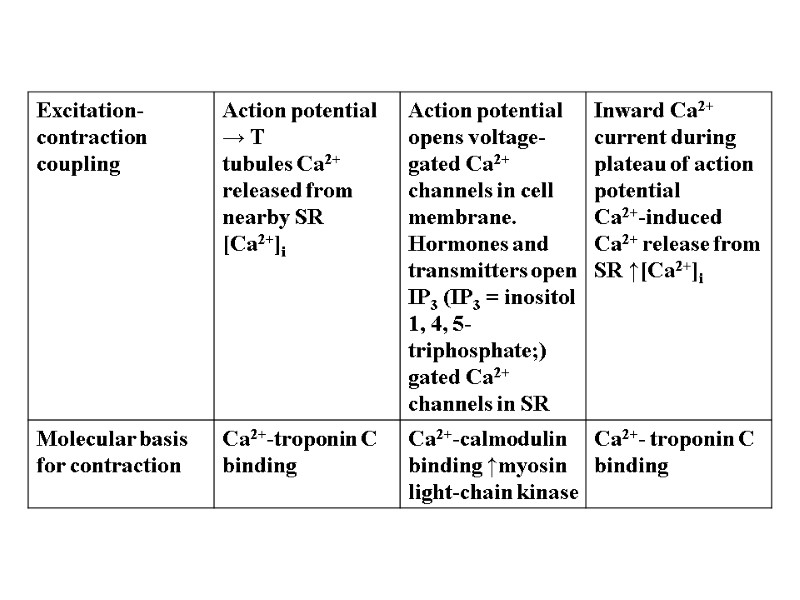
B. Steps in excitation-contraction coupling in smooth muscle - The mechanism of excitation-contraction coupling is different from that in skeletal muscle. - There is no troponin; instead, Ca2+ regulates myosin on the thick filaments.
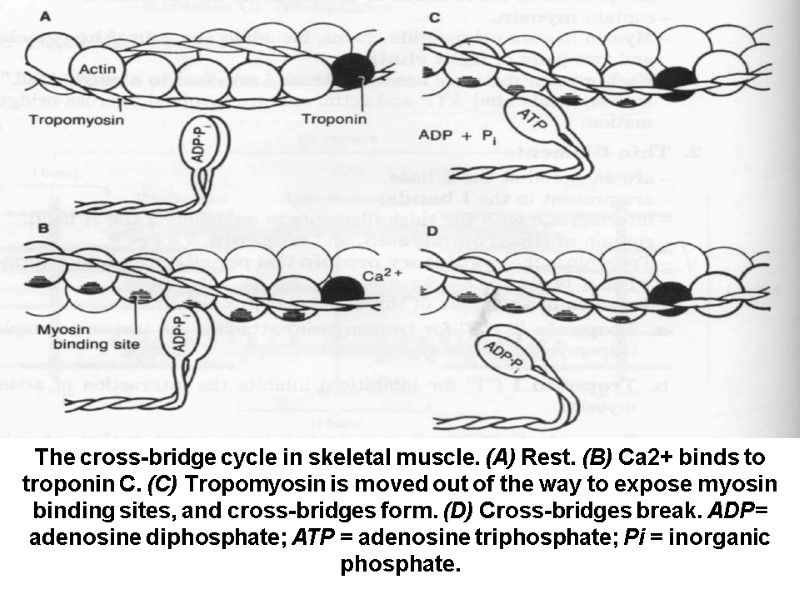
The cross-bridge cycle in skeletal muscle. (A) Rest. (B) Ca2+ binds to troponin C. (C) Tropomyosin is moved out of the way to expose myosin binding sites, and cross-bridges form. (D) Cross-bridges break. ADP= adenosine diphosphate; ATP = adenosine triphosphate; Pi = inorganic phosphate.
![Relationship of the action potential, the increase in intracellular [Ca2+], and muscle contraction in Relationship of the action potential, the increase in intracellular [Ca2+], and muscle contraction in](https://present5.com/presentacii-2/20171208\13532-!!!!!!!!!!!!!!!!!!excitable_tissues_autumn_2014!!!.ppt\13532-!!!!!!!!!!!!!!!!!!excitable_tissues_autumn_2014!!!_179.jpg)
Relationship of the action potential, the increase in intracellular [Ca2+], and muscle contraction in skeletal muscle.
SYNAPSES AND DRUGS
What is a synapse? A synapse is the junction between 2 neurones. There is a very narrow gap of about 20nm between neurones called the synaptic cleft. An action potential cannot cross the synaptic cleft, so nerve impulses are carried by chemicals called neurotransmitters.
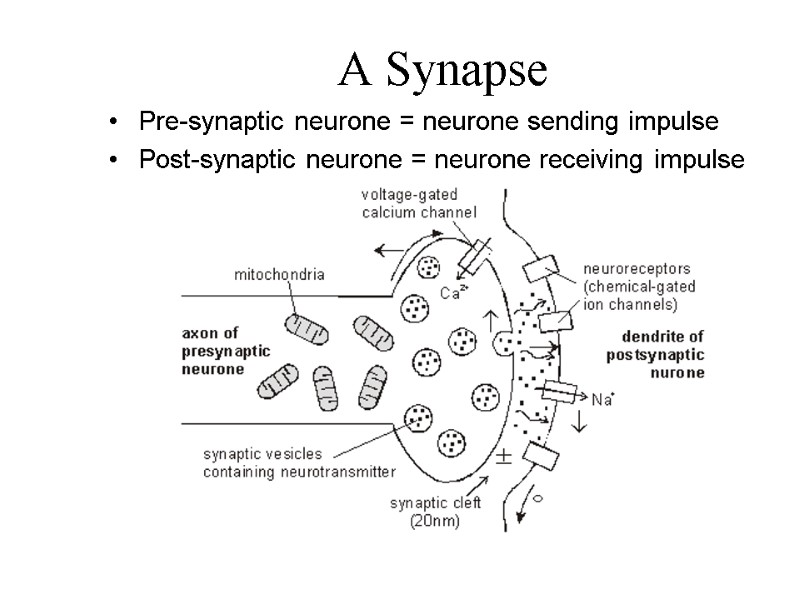
A Synapse Pre-synaptic neurone = neurone sending impulse Post-synaptic neurone = neurone receiving impulse
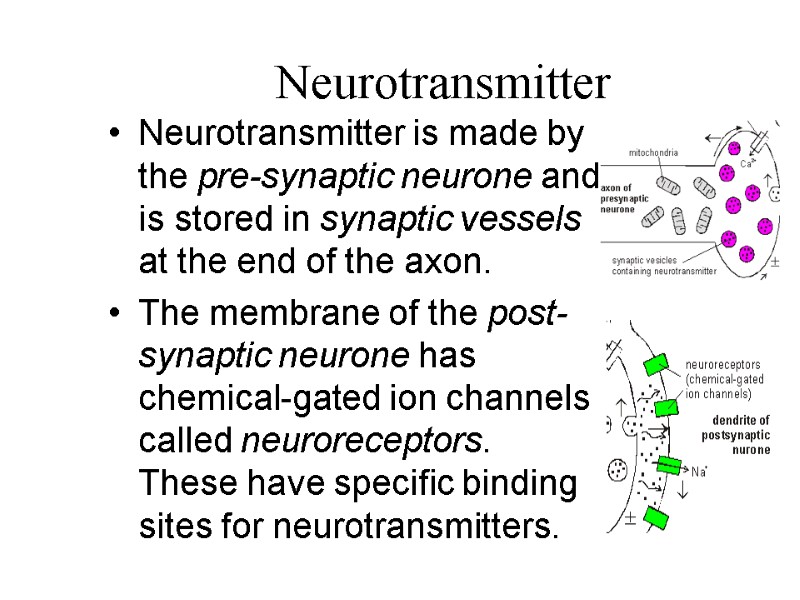
Neurotransmitter Neurotransmitter is made by the pre-synaptic neurone and is stored in synaptic vessels at the end of the axon. The membrane of the post-synaptic neurone has chemical-gated ion channels called neuroreceptors. These have specific binding sites for neurotransmitters.
Cholinergic Synapses Acetylcholine is a common transmitter. Synapses that have acetylcholine transmitter are called cholinergic synapses. Some neurones form more than 1 synapse. This is an electron micrograph of synapses between nerve fibres and a neurone cell body.
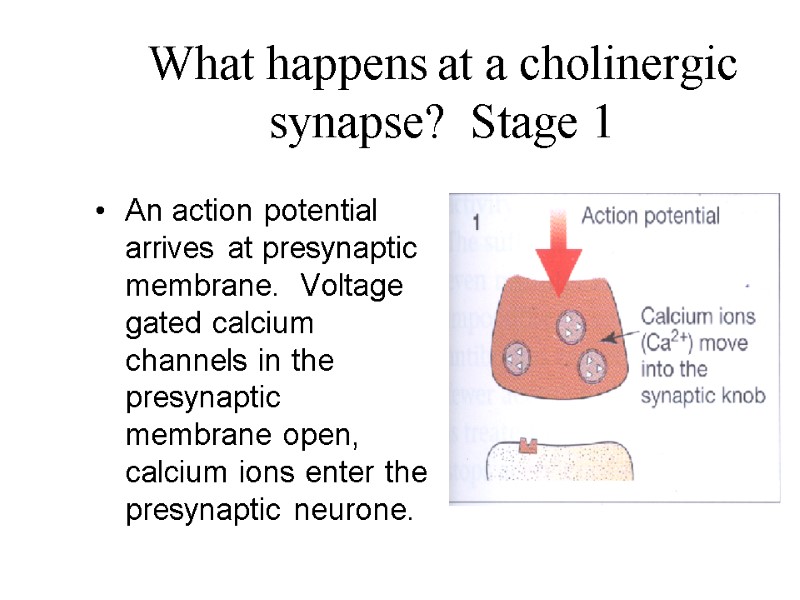
What happens at a cholinergic synapse? Stage 1 An action potential arrives at presynaptic membrane. Voltage gated calcium channels in the presynaptic membrane open, calcium ions enter the presynaptic neurone.
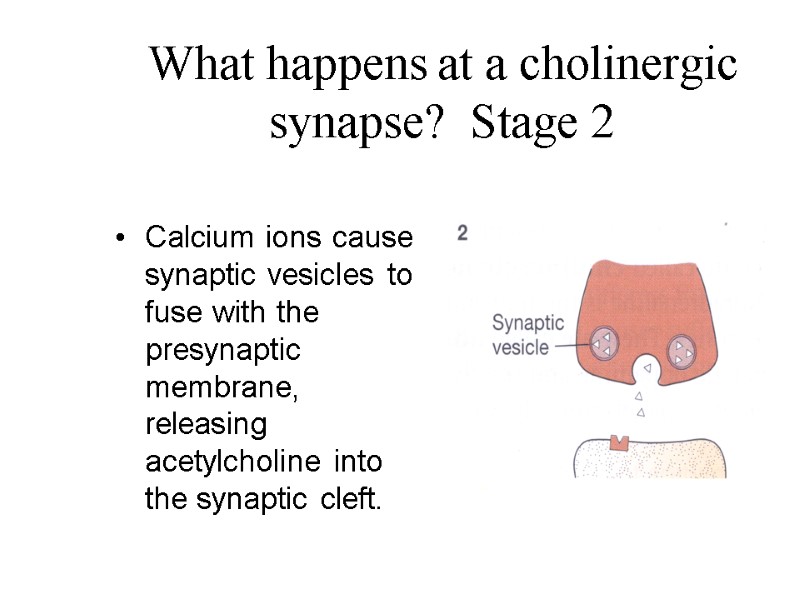
What happens at a cholinergic synapse? Stage 2 Calcium ions cause synaptic vesicles to fuse with the presynaptic membrane, releasing acetylcholine into the synaptic cleft.
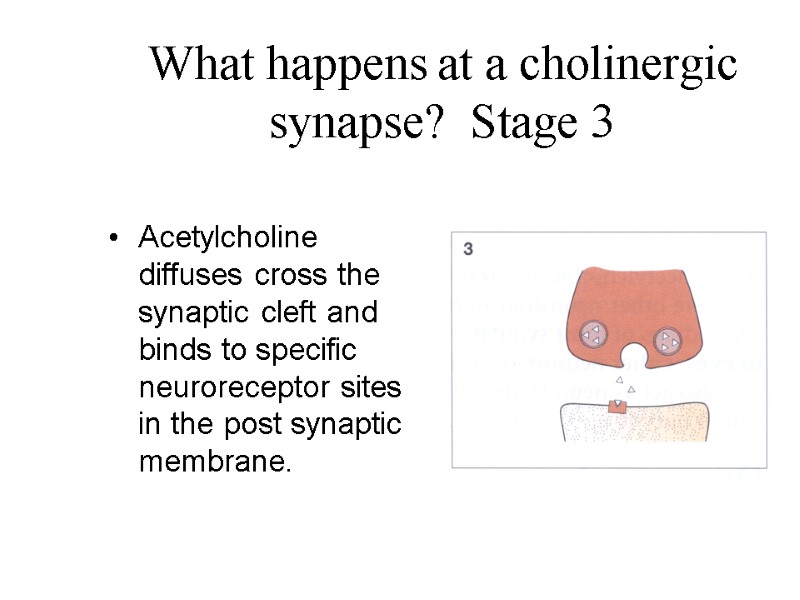
What happens at a cholinergic synapse? Stage 3 Acetylcholine diffuses cross the synaptic cleft and binds to specific neuroreceptor sites in the post synaptic membrane.
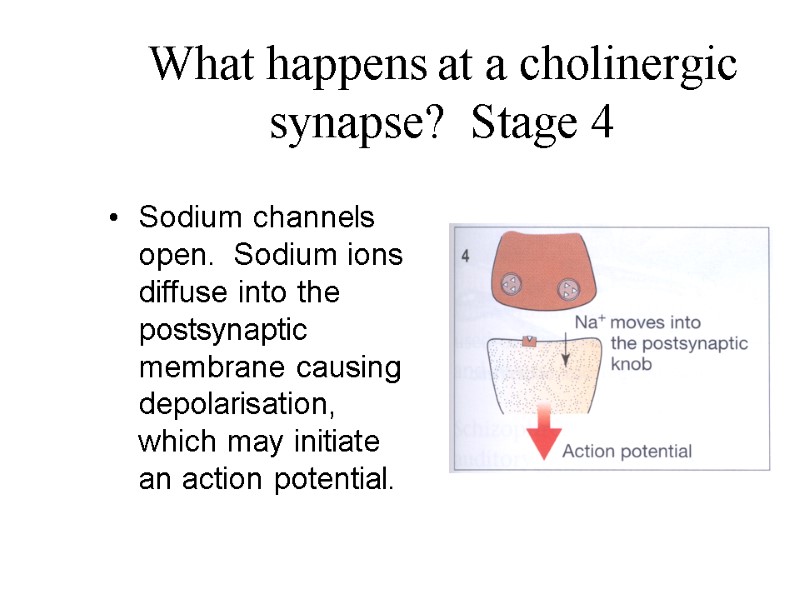
What happens at a cholinergic synapse? Stage 4 Sodium channels open. Sodium ions diffuse into the postsynaptic membrane causing depolarisation, which may initiate an action potential.
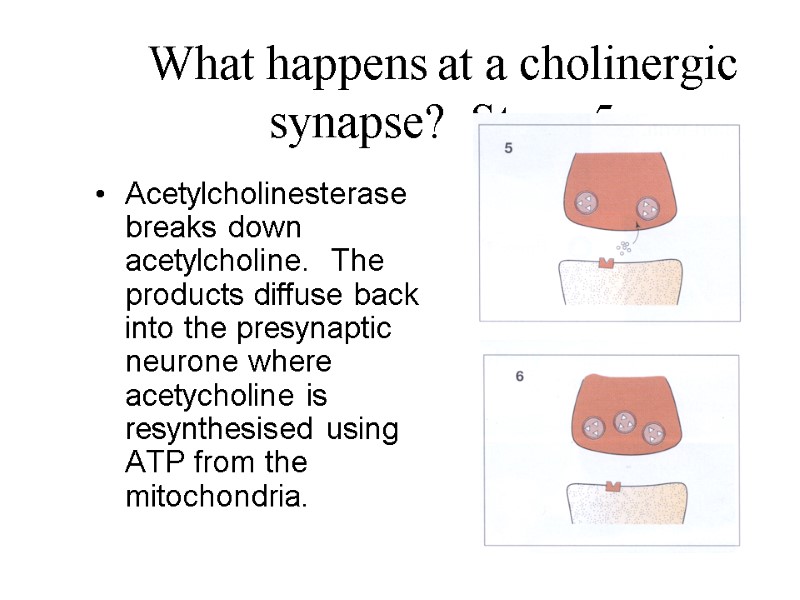
What happens at a cholinergic synapse? Stage 5 Acetylcholinesterase breaks down acetylcholine. The products diffuse back into the presynaptic neurone where acetycholine is resynthesised using ATP from the mitochondria.
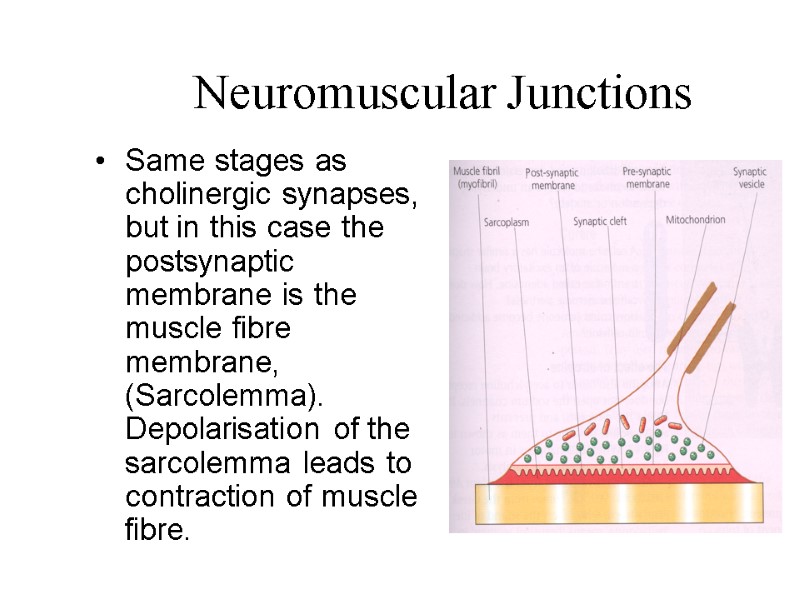
Neuromuscular Junctions Same stages as cholinergic synapses, but in this case the postsynaptic membrane is the muscle fibre membrane, (Sarcolemma). Depolarisation of the sarcolemma leads to contraction of muscle fibre.
Drugs Drugs which have molecules of similar shape to transmitter substances can affect protein receptors in postsynaptic membranes. Drugs that stimulate a nervous system are called AGONISTS Drugs that inhibit a nervous system are called ANTAGONISTS.
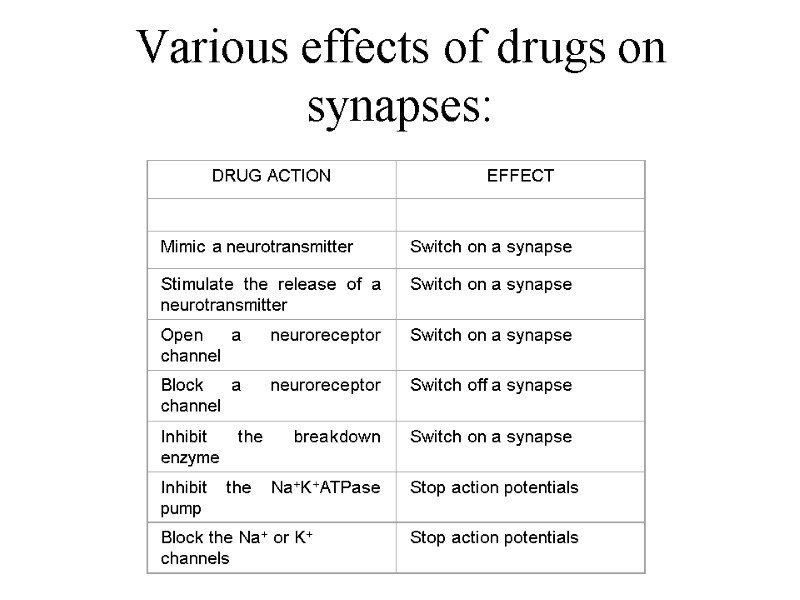
Various effects of drugs on synapses:
Effect of nicotine and atropine
Summary A synapse is the point where 2 nerve cells meet. Tiny gap = synaptic cleft. Chemical transmitter released from presynaptic neurone diffuses across synaptic cleft & fits into receptors on postsynaptic membrane. May cause postsynaptic neurone to depolarise & set up action potential. Neuromuscular junction = motor neurone connects with muscle fibre – similar to a synapse. Many drugs affect synapses.
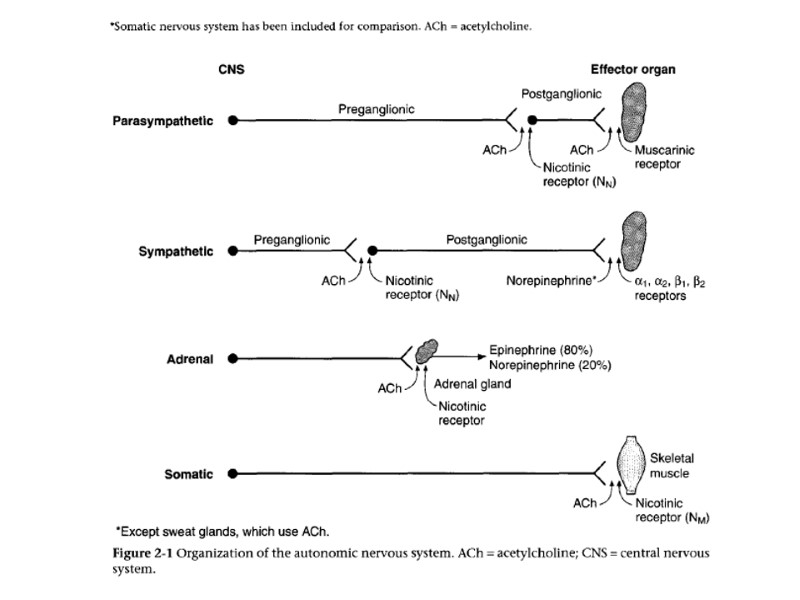
COMMON PROPERTIES OF SYNAPSES: (1)The one-way transmission. (2)Synaptic delay (is required to transmit excitation across the synapse) 0.2-0.5 msec. (3)Fatigue (diminution of the storage of mediator under stimulation with high frequency for a long time). (4)Low lability (100-120 imp/sec). (5)Special substances can blockade neuromuscular junction: Curare: blockade cholinoreceptors at the postsynaptic membrane Botulinum toxin: blockade release acetylcholine through the presynaptic membrane. Chemical inhibitors of enzyme (cholinesterase) cause accumulation of large quantities of mediator, long depolarization of the postsynaptic membrane and then inactivation of Na-channels at adjacent portions of the muscle fiber membrane.
PHYSIOLOGY OF NERVE AND SYNAPSE. PROPAGATION OF ACTION POTENTIAL ELECTRICAL MECHANISM OF PROPAGATION: 1-The excited area of the membrane has an opposite charge in comparison with adjacent resting areas. 2-Some difference of potential appears between excited and resting areas along the membrane: from -80 mV (resting) to +30 mV (excited) = 110 mV in all. 3-Local current flow switches on immediately along the membrane [arrows from (+) to (-) in our picture]. Ohm law: I=(U1-U2)/R (the more potential difference, the more current flow arises). 4-Local current flow goes out (till zero) very soon. Its propagation is electrotonic and has very little distance (about 100 mcm). 5-New action potential will be generated in each point of the cell membrane, for which local current is threshold and super-threshold. 6-(Look through 1 to 5) Process will last along the membrane repeating again and again. Every time AP becomes irritator for adjacent resting portion of the membrane. It is strong irritator: the ratio of AP to threshold is 8:1 (about 8-fold). It is a safety-factor of AP.
NEUROMUSCULAR TRANSMISSION TRANSMISSION OF IMPULSES FROM NERVES TO SKELETAL MUSCLE FIBERS. Skeletal muscle fibers are innervated by large myelinated nerve fibers that originate in the large motoneurons of the anterior horns of the spinal cord. The nerve ending makes junction with the muscle fiber (the neuromuscular synapse). There is only one junction per muscle fiber in the skeletal masculature. Nerve ending (nerve terminal) invaginates into the muscle fiber but lie on the outside. This entire structure is called “motor end plate”. Neuromuscular synapse consists of presynaptic membrane, postsynaptic membrane, and synaptic cleft.
Mechanism of neuromuscular transmission is chemical, using special neurotransmitter – mediator (acetylcholine). Acetylcholine stores in the nerve ending in form of synaptic vesicles. Synthesis of mediator: (a) in the body of motoneuron and (b) in the nerve ending itself. Successive stages of transmission: 1.Generation of AP in the nerve ending (inversion of potential) 2.Permeability of the membrane of the nerve ending to calcium (Ca2+) increases (opening of potential-sensitive Ca-channels). 3.Calcium current flow into nerve ending. 4.Ca-ions are necessary to release mediator through the membrane of the nerve ending (by exocytosis: vesicles fuse with the membrane and empty their acetylcholine into synaptic cleft). 5.Diffusion of mediator toward postsynaptic membrane. 6.Interaction between acetylcholine and molecular cholinoreceptors, which are situated in the postsynaptic membrane.
Mechanism of neuromuscular transmission is chemical, using special neurotransmitter – mediator (acetylcholine). 7.Cholinoreceptor plays role of chemical-sensitive ion channel. The channel remains closed until two acetylcholine molecules attach to this protein-receptor and open the channel. The more numbers of mediator, the more numbers of opened channels appear in the membrane. 8.Ions current flow through the postsynaptic membrane: Na-ion current inward and K-ion current outward simultaneously (chemical-sensitive channels have low selectivity). 9.Generation of postsynaptic potential (“end plate potential”). End plate potential is the change of the membrane potential in the positive direction; its amplitude is 50 to 75 mV. End plate potential has properties of local potential: its amplitude depends on numbers of acetylcholine molecules; it can be summated. End plate potential is super-threshold (it has 3-fold “safety factor”). It initiates an AR at the muscle fiber membrane (by electrical mechanism) and thus causes muscle contraction in response to each nerve impulse. 10.The acetylcholine is destroyed by the enzyme cholinesterase that is present in the synaptic space. Choline returns into presynaptic nerve ending (by active reabsorption) and new portions of mediator form.
GENERAL MECHANISM OF MUSCLE CONTRACTION 1-Action potential travels along a motor nerve to its ending on muscle fiber. 2-At each ending the nerve secretes the transmitter – acetylcholine. 3-Transmitter acts on a postsynaptic membrane (its molecular cholinoreceptors) and open acetylcholine-gated channels there. 4-Large quantities of Na-ions flow to the interior of the muscle fiber. End plate potential (local potential) forms on the postsynaptic membrane and it initiates generation of AP in the surrounding muscle fiber membrane (note: end plate potential is always threshold!). 5-The AP travels along the muscle fiber membrane and also travels deeply within the muscle fiber (along transverse tubules). 6-Depolarization of the membrane causes the sarcoplasmatic reticulum to release large quantities of Ca-ions into sarcoplasma. 7-The Ca-ions initiate attractive forces between the actin and myosin filaments. They slide together, which is contractile process. 8-After a fraction of a second the Ca-ions are pumped back into reticulum, where they remain stored, and muscle contraction ceases.
CHARACTERISTICS OF WHOLE MUSCLE CONTRACTION (I) SINGLE CONTRACTION Single contraction is response of muscle to single stimulus. It has three phases: (a) latent period of contraction; (b) the contraction phase; (c) the relaxation phase. During latent period there is generation of AP in the muscle fiber. Spike of AP coincides with the refractory period (about 1-5 msec). Therefore, when skeletal muscle is contracted, its excitability is already normal. Strength of single muscle contraction depends on strength of stimulus (directly). Muscle consists of a large number of fibers, each of which reacts to stimulation according to “all-or-none” law. But individual fibers have different excitability. The stronger the stimulus, the larger is the number of excited (and contracted) fibers. With a maximum contraction all muscle fibers are contracted. Strength of contraction of individual muscle fiber depends on its ability to form a larger number of actin-myosin bridges: (1) The larger number of myofibrils (with their actin and myosin filaments) the more is strength of contraction. This can be observed, when hypertrophia of the skeletal muscle develops. (2) Interrelation between initial length of the sarcomere and strength of following contraction (Frank-Starling law):
(II) SUMMATION OF CONTRACTION This phenomenon demonstrates interrelation between the strength of muscle contraction and the frequency of rhythmic stimulation. (1) Summation in response to pair of stimulus. If interval of time between two stimuli is shorter than duration of single contraction, muscle contraction will be summated. Summated contraction has more strength and more duration than single response. Incomplete summation will be, if the second stimulus is applied during the relaxation phase. Complete summation will be, if the second stimulus is applied during the contraction phase. (2) Summation in response to rhythmic stimulation. Under the rhythmic stimulation an intense and continuous muscle contraction forms. This continuous contraction is called tetanus. Dental tetanus (clonus) forms as a result from incomplete summation (if each successive stimulus is applied to the muscle during the relaxation phase, when relaxation began). Smooth tetanus forms as a result from complete summation (if each successive stimulus is applied to the muscle during the contraction phase, when relaxation didn’t begin). The more frequency of stimulation, the more strength of tetanic contraction is. Explanation: (1) Ca-ions concentration increases in the sarcoplasma under rhythmic stimulation; (2) the larger number of muscle fibers participate in the contraction (because of summation of local subthreshold potential under rhythmic stimulation).
MOTOR UNITS OF THE SKELETAL MUSCLE Each motoneuron innervates many different muscle fibers. All number of the muscle fibers innervated by a single motoneuron is called a motor unit. Small muscles that react rapidly and exactly have a few muscle fibers in each motor unit (2 to 10). These are laryngeal muscles, ocular muscles, muscles of the fingers. Large muscles, which support the body against gravity, have several hundreds muscle fibers in each motor units. MOTOR UNITS can be of two types: tonic and phasic (tonic units are contracted continuously, and phasic units contract with two successive phases – contraction and relaxation). Phasic units can be of two types: fast units and slow units. Fast muscle fibers are much larger and much stronger. They have more extensive sarcoplasmic reticulum but fewer mitochondria and myoglobin molecules, and less degree of blood supply (so-called “white muscle”). They have mainly glycolitic processes for energy releasing (oxidative processes is of secondary importance). That is way they usually fatigue soon. Fast muscle fibers are innervated by large alpha-1-motoneurons (with lower excitability). They provide locomotion and manipulation.
Fast muscle fibers are much larger and much stronger. They have more extensive sarcoplasmic reticulum but fewer mitochondria and myoglobin molecules, and less degree of blood supply (so-called “white muscle”). They have mainly glycolitic processes for energy releasing (oxidative processes is of secondary importance). That is way they usually fatigue soon. Fast muscle fibers are innervated by large alpha-1-motoneurons (with lower excitability). They provide locomotion and manipulation. Slow muscle fibers are smaller and weaker. They have a large number of mitochondria, large amount of myoglobin (iron-containing protein) and more extensive blood supply (so-called “red muscle”). They have mainly oxidative processes for energy releasing and don’t fatigue soon. Slow muscle fibers are innervated by smaller alpha-2-motoneurons (with high excitability). They provide continuous muscle tone. Each skeletal muscle in the human being is mixed (it contains either fast or slow motor units). TWO MECHANISM OF TETANUS FORMATION IN THE BODY (1)-High frequency of nerve impulses and synchronic contraction of a large number of skeletal muscle fibers (mainly of fast motor units) give us smooth tetanus with maximum strength (very seldom, under strong emotional state). (2)-Low frequency of nerve impulses and asynchronic contraction of a large number of skeletal muscle fibers (mainly of slow motor units) give us weak continuous muscle tone.


13532-!!!!!!!!!!!!!!!!!!excitable_tissues_autumn_2014!!!.ppt
- Количество слайдов: 210

