a6ff01eeb2ae69c082db3fa7bb1616f0.ppt
- Количество слайдов: 13
Examination of higher cerebral functions
Examination of higher cerebral (mental) functions • It should be a requisite part of standard neurologic examination – at least Mini Mental State Examination should be performed in neurologic pts. • It has to be systematic and hierarchic (level of consciousness directed attention cognition, mood, speech) • Golden neurologic rule „to localize a lesion“ should be applied for mental functions too (neuronal networks). • Extremely important is thorough history taking (changes in pt’s behavior) and focusing on the pt’s behavior during the examination (evaluation of his/her appearance, cooperation, attention, memory, mental flexibility, social adaptability, ability of nonverbal communication, depressive symptomatology, etc. ).
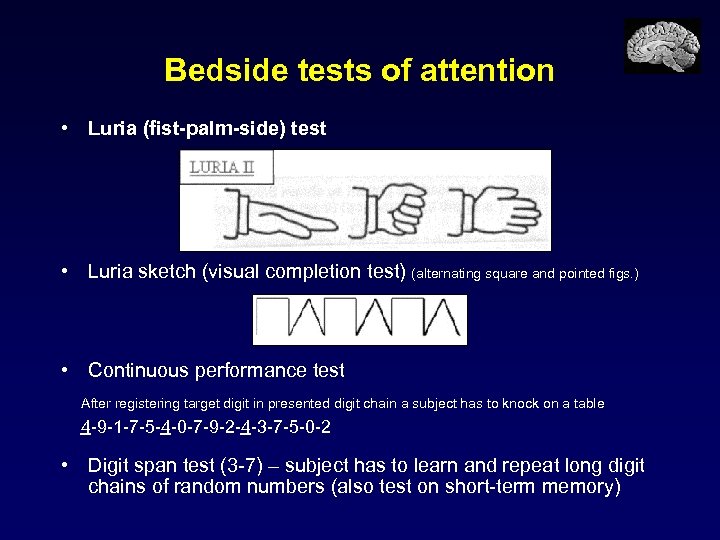
Bedside tests of attention • Luria (fist-palm-side) test • Luria sketch (visual completion test) (alternating square and pointed figs. ) • Continuous performance test After registering target digit in presented digit chain a subject has to knock on a table 4 -9 -1 -7 -5 -4 -0 -7 -9 -2 -4 -3 -7 -5 -0 -2 • Digit span test (3 -7) – subject has to learn and repeat long digit chains of random numbers (also test on short-term memory)
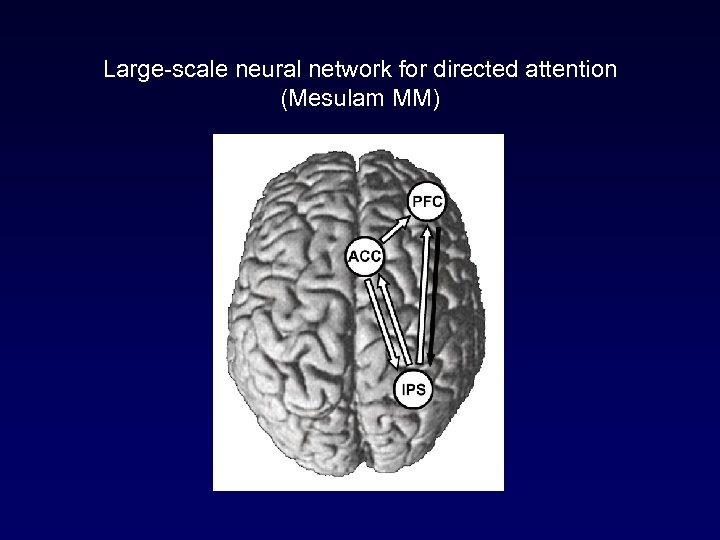
Large-scale neural network for directed attention (Mesulam MM)
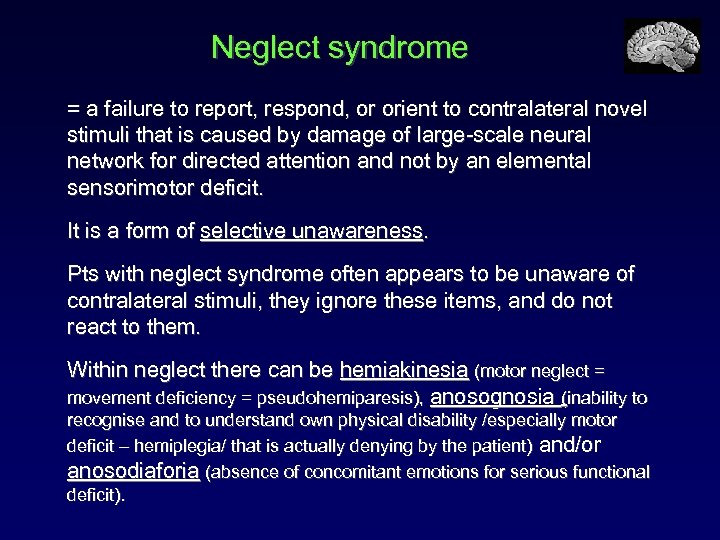
Neglect syndrome = a failure to report, respond, or orient to contralateral novel stimuli that is caused by damage of large-scale neural network for directed attention and not by an elemental sensorimotor deficit. It is a form of selective unawareness. Pts with neglect syndrome often appears to be unaware of contralateral stimuli, they ignore these items, and do not react to them. Within neglect there can be hemiakinesia (motor neglect = movement deficiency = pseudohemiparesis), anosognosia (inability to recognise and to understand own physical disability /especially motor deficit – hemiplegia/ that is actually denying by the patient) and/or anosodiaforia (absence of concomitant emotions for serious functional deficit).
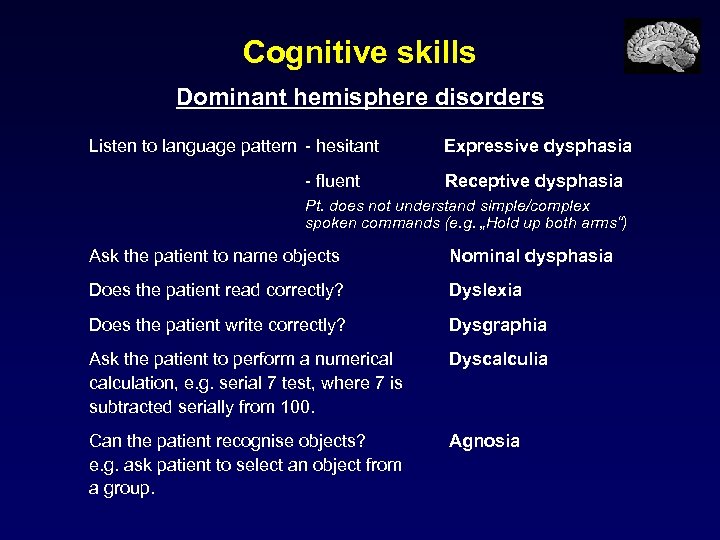
Cognitive skills Dominant hemisphere disorders Listen to language pattern - hesitant - fluent Expressive dysphasia Receptive dysphasia Pt. does not understand simple/complex spoken commands (e. g. „Hold up both arms“) Ask the patient to name objects Nominal dysphasia Does the patient read correctly? Dyslexia Does the patient write correctly? Dysgraphia Ask the patient to perform a numerical calculation, e. g. serial 7 test, where 7 is subtracted serially from 100. Dyscalculia Can the patient recognise objects? e. g. ask patient to select an object from a group. Agnosia
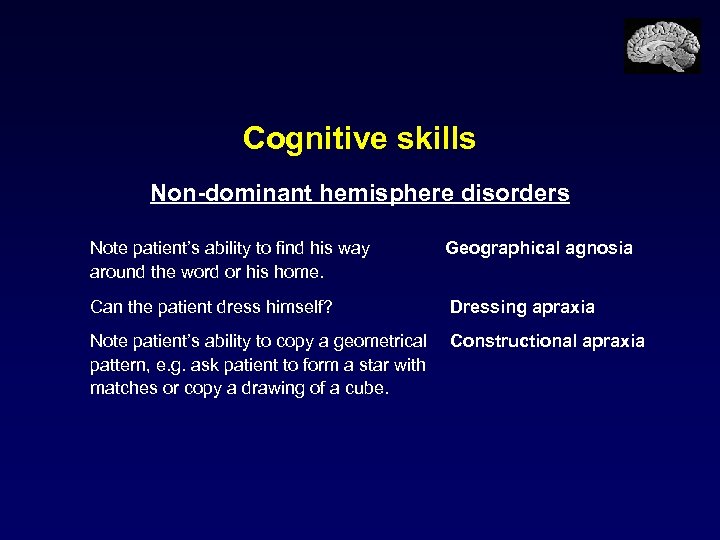
Cognitive skills Non-dominant hemisphere disorders Note patient’s ability to find his way around the word or his home. Geographical agnosia Can the patient dress himself? Dressing apraxia Note patient’s ability to copy a geometrical pattern, e. g. ask patient to form a star with matches or copy a drawing of a cube. Constructional apraxia
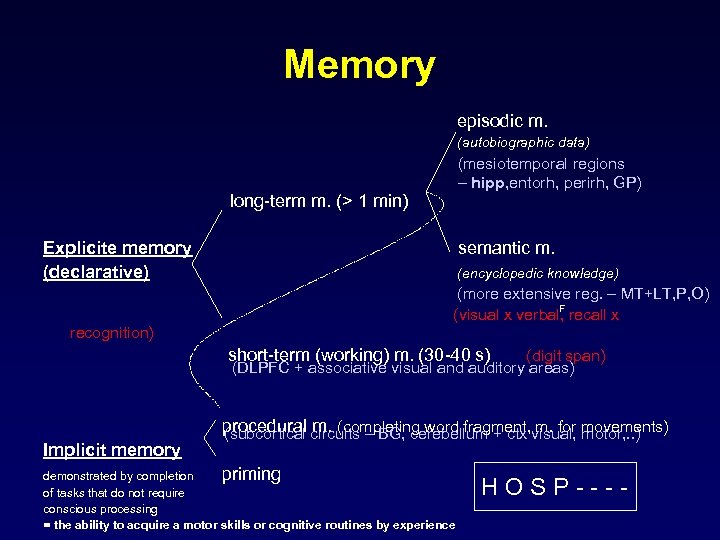
Memory episodic m. (autobiographic data) (mesiotemporal regions – hipp, entorh, perirh, GP) long-term m. (> 1 min) Explicite memory (declarative) recognition) semantic m. (encyclopedic knowledge) (more extensive reg. – MT+LT, P, O) F (visual x verbal, recall x short-term (working) m. (30 -40 s) (digit span) (DLPFC + associative visual and auditory areas) Implicit memory procedural circuits – BG, cerebellum + ctx visual, movements) (subcortical m. (completing word fragment, m. for motor, . . ) demonstrated by completion priming of tasks that do not require conscious processing = the ability to acquire a motor skills or cognitive routines by experience HOSP----
Bedside memory testing is limited! Testing requires alertness and is not possible in a confused or dysphasic patient! • Short-term memory – DIGIT SPAN TEST – ask the patient to repeat a sequence of 5, 6, or 7 random numbers. • Long-term memory – ask the patient to describe present illness, duration of hospital stay or recent events in the news (RECENT MEMORY), ask about events and circumstances occuring more than five years previously (REMOTE MEMORY). • Verbal memory – ask the patient to remember a sentence or a short story and test after 15 minutes. • Visual memory – ask the patient to remember objects on a tray and test after 15 minutes
Reasoning and problem solving • Test patient with two-step calculation, e. g. ‘I wish to buy 12 articles at 7 cent each. How much change will I receive from € 1? ’. • Ask patient to reverse 3 or 4 random numbers. • Ask patient to explain proverbs. The examiner must compare patient’s present reasoning ability with expected abilities based on job history and/or school work!
Affect Note the patient’s affect! • Does the patient seem depressed? • Loss of interest, euphoria, or social disinhibition may be signs of frontal lobe dysfunction. Emotional behavior such as aggression and anger may arise from damage to the limbic system. • Emotional lability should prompt further examination to look for upper motor neuron signs and a pseudobulbar palsy.
Determination of hemispheric dominance Interview about writing, eating with spoon, throwing a ball, kicking, step; tapping – domin. hand 50/min, nondomin. hand 45/min. Left hemisphere is dominant in 95% right-handers and 60% lefthanders! Left hemisphere – dominant for speech and motor functions, reading, writing, counting, recognition of colors, verbal memory, important for linguistic thinking, . . . Right hemisphere – dominant for attentional functions, prosopognosia, prosodia (affective component of speech), nonverbal communication (ability to „read from face“), visuo-spatial perception, visual and topographical memory, recognition of music, …
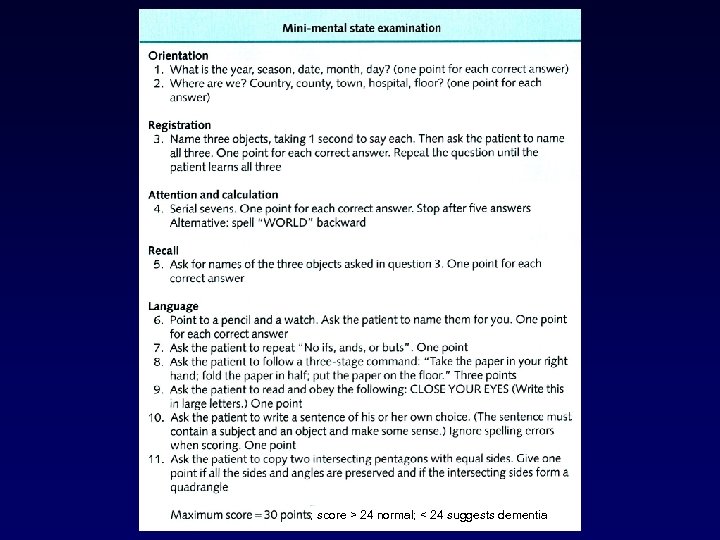
; score > 24 normal; < 24 suggests dementia
a6ff01eeb2ae69c082db3fa7bb1616f0.ppt