1476f1bcff927b75dc5dea3365d89a2f.ppt
- Количество слайдов: 15
Evidence-Based Clinical Practice Guidelines in the Veterans Health Administration David Atkins, MD, MPH Health Services Research and Development Quality Enhancement Research Initiative Dept. of Veterans Affairs

Objectives • Briefly review the joint VA/DOD guideline development effort • Describe the role of guidelines in system-wide quality improvement • Reflect on future challenges and implications for guideline development – Guideline development process – Guideline products
Guidelines in The VA Health System • VA is a user and developer of guidelines • Integrated health system serving 5 million Veterans – 200, 000 employees • Collaborates with Dept. of Defense to develop common guidelines for active duty and retired service members
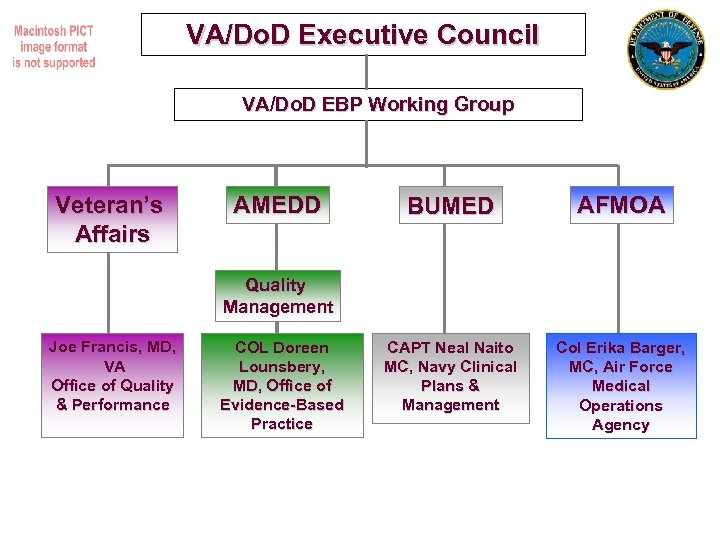
VA/Do. D Executive Council VA/Do. D EBP Working Group Veteran’s Affairs AMEDD BUMED AFMOA CAPT Neal Naito MC, Navy Clinical Plans & Management Col Erika Barger, MC, Air Force Medical Operations Agency Quality Management Joe Francis, MD, VA Office of Quality & Performance COL Doreen Lounsbery, MD, Office of Evidence-Based Practice

Goals of VA/Do. D Evidence-based Guidelines • Summarize evidence and recommendations that can form the basis of clinical policy and delivery system design • Create tools that assist clinicians and managers in implementing evidence into practice • Guide local quality improvement efforts • Reduce waste & inappropriate variation • Enhance population health
Why a VA/Do. D Guideline Development Process? • Allows tailoring to the needs of the current or former service member – may assist seamless transition • • • Provides check on Industry & Professional Group biases Strong adoption of evidentiary standards Focus on primary care Use of algorithms and other tools to assist providers Enhances ability to drive clinical policy

VA/Do. D CPGs Available for Use Posted to www. Guideline. gov (National Guideline Clearing House): • • • • Asthma Amputation Rehabilitation Chronic Heart Failure Chronic Obstructive Pulmonary Disease Diabetes Mellitus Dyslipidemia Dysuria in Women Erectile Dysfunction GERD Hypertension Ischemic Heart Disease Kidney Disease Low Back Pain • • • Major Depressive Disorder Management of Tobacco Use Medically Unexplained Symptoms: Chronic Pain & Fatigue Opioid Therapy for Chronic Pain Obesity Post-Operative Pain Post-Deployment Health – Screening Health Exam Post-Traumatic Stress Disorder Psychosis Stroke Rehabilitation Substance Use Disorder Uncomplicated Pregnancy also Biological, Chemical, and Radiation-Induced Illnesses Pocket Cards
What’s Different About the VA/Do. D? • • • Integrated Health Systems Mission-driven culture Strong emphasis on primary care Wide-spread electronic health record Ten year experience with a robust set of performance metrics
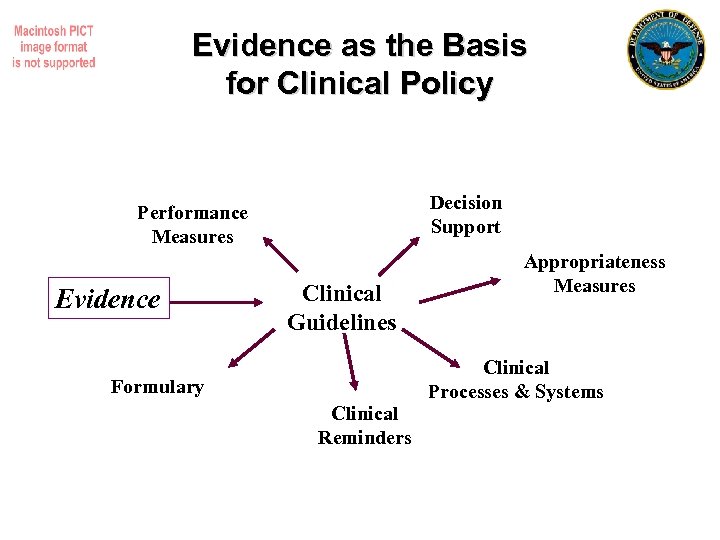
Evidence as the Basis for Clinical Policy Decision Support Performance Measures Evidence Clinical Guidelines Appropriateness Measures Clinical Processes & Systems Formulary Clinical Reminders
What’s Improved • • • Greater use of systematic reviews More explicit presentations of evidence More explicit designation of when evidence is inadequate • ? Multidisciplinary representation
Problems with Guideline Development • Process still too inefficient – Effort not always matched to value; redundancy • Conflict of interest persists – Not solved by disclosure alone • • • Too much effort on less important areas Too little attention to harms, tradeoffs Panels often don’t reflect the targets audience of guidelines – Primary care under-represented – Patient representation challenging


Problems in Guideline Presentation • Is goal to write a textbook or improve care? • Little distinction between recommendations with widely varying health impact • Not written with translation to tools in mind – Computerized decision support – Performance measures – Coverage decisions • Limited attention to costs, feasibility, or patient values • Often contribute to misguided attempts to dichotomize quality of care: good vs. bad
Future Challenges • Tensions between practical guidance vs. individualized care – Benefits of many recommendations depend critically on individual characteristics (e. g. lipids, osteoporosis) – Role of age, co-morbidity, poly-pharmacy • How can guidelines better promote progress towards goal vs. arbitrary goal? • Recognizing system factors and implementation • Are there practical ways to incorporate patient preferences? • Coordination across different groups
Recommendations • Strong policies on conflict of interest • Open peer review • Reduce specialty dominance in developing guidelines aimed at primary care • Address tradeoffs in recommendations – Preferences, costs, feasibility • Consider system and implementation factors – Specific language to identify target population and actions • Avoid black/white definitions of “success”
1476f1bcff927b75dc5dea3365d89a2f.ppt