753b696ec2db6f34d75deb258e6acd2d.ppt
- Количество слайдов: 57
 Ethical Concerns in Nursing Practice 1
Ethical Concerns in Nursing Practice 1
 Values, Morals, & Ethics • Values: are freely chosen, enduring beliefs or attitudes about the worth of a person, object, idea, or action (e. g. freedom, family, honesty, hard work) • Values frequently derive from a person’s cultural, ethnic, and religious background; from societal traditions; and from the values held by peer group and family • Values form a basic for Behaviour “purposive Behaviour”; The purposive behavior is based on a person’s decisions/choices, and these decisions/choices are based on the person’s underlying values. 2
Values, Morals, & Ethics • Values: are freely chosen, enduring beliefs or attitudes about the worth of a person, object, idea, or action (e. g. freedom, family, honesty, hard work) • Values frequently derive from a person’s cultural, ethnic, and religious background; from societal traditions; and from the values held by peer group and family • Values form a basic for Behaviour “purposive Behaviour”; The purposive behavior is based on a person’s decisions/choices, and these decisions/choices are based on the person’s underlying values. 2
 • Values are learned and are greatly influenced by a person’s sociocultural environment (e. g. demonstrate honesty, folk healer, observation and experience) • People need societal values to feel accepted, and they need personal values to produce a sense of individuality. • Professional values often reflect and expand on personal values • Once a person becomes aware of his/her values, they become an internal control for behavior, thus, a person’s real values are manifested in consistent pattern of behavior 3
• Values are learned and are greatly influenced by a person’s sociocultural environment (e. g. demonstrate honesty, folk healer, observation and experience) • People need societal values to feel accepted, and they need personal values to produce a sense of individuality. • Professional values often reflect and expand on personal values • Once a person becomes aware of his/her values, they become an internal control for behavior, thus, a person’s real values are manifested in consistent pattern of behavior 3
 • Nurses acquire these values during socialization into nursing – from codes of ethics, nursing experiences, teachers, and peers. • Watson (1981) outlined 4 important values of nursing: • Strong commitment to service • Belief in the dignity and worth of each person • Commitment to education • Autonomy • nurses often need to behave in a value-natural way (i. e. being nonjudgmental) 4
• Nurses acquire these values during socialization into nursing – from codes of ethics, nursing experiences, teachers, and peers. • Watson (1981) outlined 4 important values of nursing: • Strong commitment to service • Belief in the dignity and worth of each person • Commitment to education • Autonomy • nurses often need to behave in a value-natural way (i. e. being nonjudgmental) 4
 • Nurses need to understand their own values related to moral matters and to use ethical reasoning to determine and explain their moral positions. • Moral principles are also important, otherwise, they may give emotional responses which often are not helpful. • Although nurses can not and should not ignore or deny their own and the profession’s values, they need to be able to accept a client’s values and beliefs rather than assume their own are the “right ones” This acceptance and nonjudgmental approach requires nurses to be aware of their own values and how they influence behavior 5
• Nurses need to understand their own values related to moral matters and to use ethical reasoning to determine and explain their moral positions. • Moral principles are also important, otherwise, they may give emotional responses which often are not helpful. • Although nurses can not and should not ignore or deny their own and the profession’s values, they need to be able to accept a client’s values and beliefs rather than assume their own are the “right ones” This acceptance and nonjudgmental approach requires nurses to be aware of their own values and how they influence behavior 5
 • What values you hold about life, health, illness, and death. • How do your values influence the nursing care you provide? • We should explore our own values and beliefs regarding such situations as the following: • An individual’s right to make decisions for self when conflicting with medical advice • Abortion • End-of –life issues • Cloning 6
• What values you hold about life, health, illness, and death. • How do your values influence the nursing care you provide? • We should explore our own values and beliefs regarding such situations as the following: • An individual’s right to make decisions for self when conflicting with medical advice • Abortion • End-of –life issues • Cloning 6
 • The process of becoming more conscious of and naming what one values or considers worthy is known as “value clarification” • In value clarification: we examine what we believe is good, bad, beautiful, worthy, meaningful, …. . and explore the process of determining our personal values. Why? 7
• The process of becoming more conscious of and naming what one values or considers worthy is known as “value clarification” • In value clarification: we examine what we believe is good, bad, beautiful, worthy, meaningful, …. . and explore the process of determining our personal values. Why? 7
 Facts vs. Values: • Factual Statement: scientists often perform painful experiments on animals. • Value Statement: it is morally acceptable (morally required, morally wrong) for us to perform painful experiments on animals. 8
Facts vs. Values: • Factual Statement: scientists often perform painful experiments on animals. • Value Statement: it is morally acceptable (morally required, morally wrong) for us to perform painful experiments on animals. 8
 • Factual Statement: We created and used the atomic bomb. • Value Statement: Creating and using the atomic bomb was morally right (morally wrong). • Factual statement: someday we will have the technology to clone human beings. • Value statement: It is morally acceptable (unacceptable) to clone human beings 9
• Factual Statement: We created and used the atomic bomb. • Value Statement: Creating and using the atomic bomb was morally right (morally wrong). • Factual statement: someday we will have the technology to clone human beings. • Value statement: It is morally acceptable (unacceptable) to clone human beings 9
 • Factual Statement: scientists often perform painful experiments on animals. • Value Statement: it is morally acceptable (morally required, morally wrong) for us to perform painful experiments on animals. 10
• Factual Statement: scientists often perform painful experiments on animals. • Value Statement: it is morally acceptable (morally required, morally wrong) for us to perform painful experiments on animals. 10
 The purposes of value clarifications Ø This increase our self-awareness or understanding of ourselves and assist us in making choices. Ø It facilitates decision-making, because we have a better grasp of our own value system. Ø Consequently, this will be helpful when you are faced with an ethical dilemma • Ethical dilemma occurs when an individual must choose between two unfavorable alternatives “e. g. assisted suicide” 11
The purposes of value clarifications Ø This increase our self-awareness or understanding of ourselves and assist us in making choices. Ø It facilitates decision-making, because we have a better grasp of our own value system. Ø Consequently, this will be helpful when you are faced with an ethical dilemma • Ethical dilemma occurs when an individual must choose between two unfavorable alternatives “e. g. assisted suicide” 11
 • Ethical dilemma usually have no perfect solution and those making decisions may find themselves in the position of having to defend their decisions • Value conflict occurs when we must choose between two things, both of which are important to us. • It’s the nurses’ role to help clients identify values and clarify them…… But How? ? ? 12
• Ethical dilemma usually have no perfect solution and those making decisions may find themselves in the position of having to defend their decisions • Value conflict occurs when we must choose between two things, both of which are important to us. • It’s the nurses’ role to help clients identify values and clarify them…… But How? ? ? 12
 Helping clients identifying their values • List alternatives • Examine possible consequences of choices • Choose freely • Feel good about the choice • Affirm the choice • Act on the choice • Act with a pattern Remember: never impose your personal values never offer an opinion 13
Helping clients identifying their values • List alternatives • Examine possible consequences of choices • Choose freely • Feel good about the choice • Affirm the choice • Act on the choice • Act with a pattern Remember: never impose your personal values never offer an opinion 13
 Morals and Ethics • Morals: is similar to ethics and many people use the two wards interchangeably (closely associated with the concept of ethics) • Derived from the Latin “mores”, means custom or habit. • Morality: usually refers to an individual’s personal standards of what is right and wrong in conduct, character, and attitude. • Morals: are based on religious beliefs and social influence and group norms 14
Morals and Ethics • Morals: is similar to ethics and many people use the two wards interchangeably (closely associated with the concept of ethics) • Derived from the Latin “mores”, means custom or habit. • Morality: usually refers to an individual’s personal standards of what is right and wrong in conduct, character, and attitude. • Morals: are based on religious beliefs and social influence and group norms 14
 Morals and Ethics (continue) • Ethics is a branch of philosophy (the study of beliefs and assumptions) referred to as moral philosophy. • Derived from the Greek word “ethos” which means customs, habitual usage, conduct and character. • Ethics: usually refers to the practices, beliefs, and standards of behavior of a particular group such as nurses. It also refers to the method of inquiry that assists people to understood the morality of human behavior (study of morality) 15
Morals and Ethics (continue) • Ethics is a branch of philosophy (the study of beliefs and assumptions) referred to as moral philosophy. • Derived from the Greek word “ethos” which means customs, habitual usage, conduct and character. • Ethics: usually refers to the practices, beliefs, and standards of behavior of a particular group such as nurses. It also refers to the method of inquiry that assists people to understood the morality of human behavior (study of morality) 15
 Morals and Ethics (continue) • In both, we describe the behavior we observe as good, right, desirable, honorable, fitting or proper or we might describe the behavior as bad, wrong, improper, irresponsible, or evil. [Such perceptions are based on values] • There are times when a differences in values and decisions can be accepted • Differences in values and decisions put people into direct conflict. What to do in such situation? 16
Morals and Ethics (continue) • In both, we describe the behavior we observe as good, right, desirable, honorable, fitting or proper or we might describe the behavior as bad, wrong, improper, irresponsible, or evil. [Such perceptions are based on values] • There are times when a differences in values and decisions can be accepted • Differences in values and decisions put people into direct conflict. What to do in such situation? 16
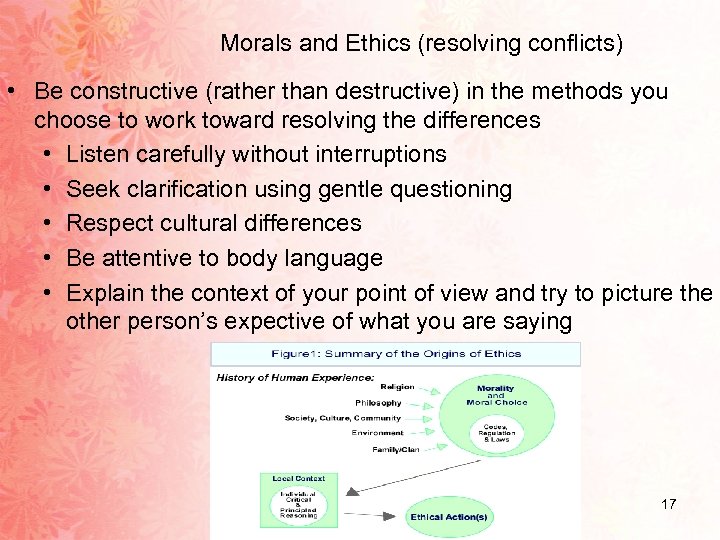 Morals and Ethics (resolving conflicts) • Be constructive (rather than destructive) in the methods you choose to work toward resolving the differences • Listen carefully without interruptions • Seek clarification using gentle questioning • Respect cultural differences • Be attentive to body language • Explain the context of your point of view and try to picture the other person’s expective of what you are saying 17
Morals and Ethics (resolving conflicts) • Be constructive (rather than destructive) in the methods you choose to work toward resolving the differences • Listen carefully without interruptions • Seek clarification using gentle questioning • Respect cultural differences • Be attentive to body language • Explain the context of your point of view and try to picture the other person’s expective of what you are saying 17
 Comparison of morals and ethics Morals • Principles and rules of right conduct • Private, and personal • Commitment to principles and values is usually defended in daily life • • • Ethics Formal responding process used to determine right conduct Professionally and publicly stated Inquiry or study of principles and values Process of questioning, and perhaps changing, one’s morals Speaks to relationships between human beings • Pertain to an individual‘s character 18
Comparison of morals and ethics Morals • Principles and rules of right conduct • Private, and personal • Commitment to principles and values is usually defended in daily life • • • Ethics Formal responding process used to determine right conduct Professionally and publicly stated Inquiry or study of principles and values Process of questioning, and perhaps changing, one’s morals Speaks to relationships between human beings • Pertain to an individual‘s character 18
 19
19
 Moral development • Moral development is a complex process that is not fully understood • It is the process of learning what ought to be done and what ought not to be done • Different approaches to moral development exists: • Kohlberg’s theory • Gilligan 20
Moral development • Moral development is a complex process that is not fully understood • It is the process of learning what ought to be done and what ought not to be done • Different approaches to moral development exists: • Kohlberg’s theory • Gilligan 20
 Moral distress • When the nurses are unable to follow their moral beliefs because of institutional or other restriction. • The distress occurs when the nurse violates a personal moral value and fails to fulfill perceived responsibility. • Moral distress represent practical, rather than ethical dilemmas. 21
Moral distress • When the nurses are unable to follow their moral beliefs because of institutional or other restriction. • The distress occurs when the nurse violates a personal moral value and fails to fulfill perceived responsibility. • Moral distress represent practical, rather than ethical dilemmas. 21
 Moral outrage - Occurs when someone else in the health care setting performs an act the nurse believes to be immoral. - Nurses do not participate in the act. - Nurses not responsible for wrong but perceive that they are powerless to prevent. 22
Moral outrage - Occurs when someone else in the health care setting performs an act the nurse believes to be immoral. - Nurses do not participate in the act. - Nurses not responsible for wrong but perceive that they are powerless to prevent. 22
 Kohlberg Approach • Directly affected by Piaget’s theory of cognitive development • Focuses on the structure of though about moral issues rather than the specific content of moral values. • Emphasizes fairness, rights and autonomy in a justice framework • Moral development progresses through three levels: • Level I: premoral or preconventional level • Level II: conventional level • Level III: post conventional, autonomous or principled level 23
Kohlberg Approach • Directly affected by Piaget’s theory of cognitive development • Focuses on the structure of though about moral issues rather than the specific content of moral values. • Emphasizes fairness, rights and autonomy in a justice framework • Moral development progresses through three levels: • Level I: premoral or preconventional level • Level II: conventional level • Level III: post conventional, autonomous or principled level 23
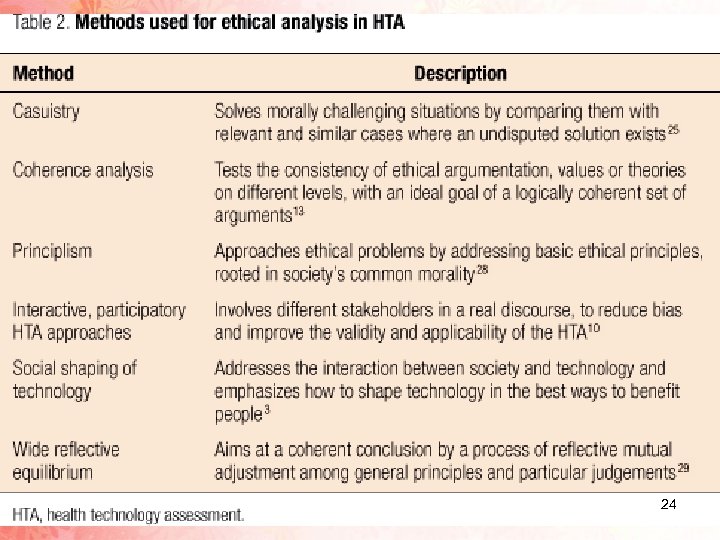 24
24
 Gilligan’s theory • Focuses on a care perspectives • Organized around the notions of responsibility, compassion (care), relationships • The ethics of justice (fairness) is based of the idea of equality “everyone should receive the same treatment”. By contrast, the ethics of care is based on a premise of nonviolence: that no one should be harmed or abandoned 25
Gilligan’s theory • Focuses on a care perspectives • Organized around the notions of responsibility, compassion (care), relationships • The ethics of justice (fairness) is based of the idea of equality “everyone should receive the same treatment”. By contrast, the ethics of care is based on a premise of nonviolence: that no one should be harmed or abandoned 25
 Gilligan’s theory (continue) • Process of developing an “ethics of care” • Stage I: caring for oneself • Stage II: caring for others • Stage III: caring for oneself and others • Each stage ends with a transitional period (a time when the individual recognizes a conflict or discomfort with some present behavior and considers new approaches) 26
Gilligan’s theory (continue) • Process of developing an “ethics of care” • Stage I: caring for oneself • Stage II: caring for others • Stage III: caring for oneself and others • Each stage ends with a transitional period (a time when the individual recognizes a conflict or discomfort with some present behavior and considers new approaches) 26
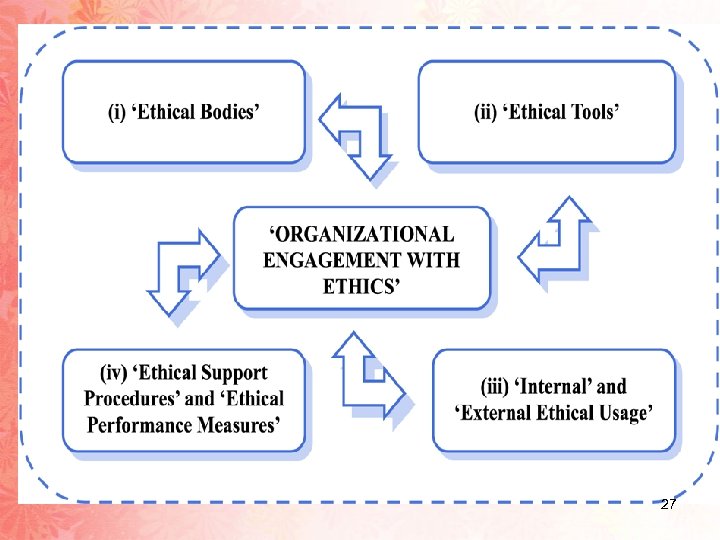 27
27
 Moral/ethical principles (concepts) • Are statements about broad, general philosophic concepts such as autonomy and justice • They provide the foundation for moral values, which are specific prescriptions for actions (e. g. “people should not lie” (rule) is based on the moral principle of respect of autonomy for people. 28
Moral/ethical principles (concepts) • Are statements about broad, general philosophic concepts such as autonomy and justice • They provide the foundation for moral values, which are specific prescriptions for actions (e. g. “people should not lie” (rule) is based on the moral principle of respect of autonomy for people. 28
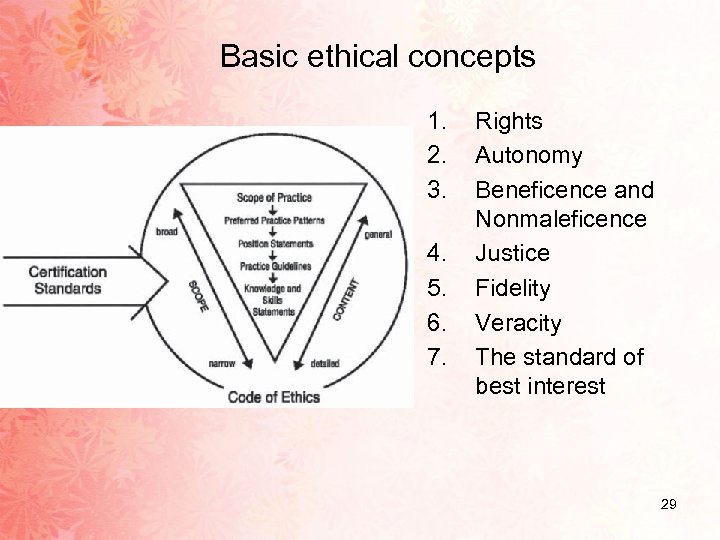 Basic ethical concepts 1. 2. 3. 4. 5. 6. 7. Rights Autonomy Beneficence and Nonmaleficence Justice Fidelity Veracity The standard of best interest 29
Basic ethical concepts 1. 2. 3. 4. 5. 6. 7. Rights Autonomy Beneficence and Nonmaleficence Justice Fidelity Veracity The standard of best interest 29
 Basic ethical concepts Rights • Rights form the basis of most professional codes and legal judgments • Self-determination rights • Rights and cultural relativism • Rights of the unborn • Rights of privacy and confidentiality 30
Basic ethical concepts Rights • Rights form the basis of most professional codes and legal judgments • Self-determination rights • Rights and cultural relativism • Rights of the unborn • Rights of privacy and confidentiality 30
 Basic ethical concepts Autonomy • • Involves the right of self-determination, independence, and freedom. It refers to the right to make one’s own decisions Respect for autonomy means that nurses recognize the individual’s uniqueness, the right to be what that person is, and the right to choose personal goals Nurses who follow the principle of autonomy respect a client's right to make decisions even when those choices seem not to be in the client’s best interest 31
Basic ethical concepts Autonomy • • Involves the right of self-determination, independence, and freedom. It refers to the right to make one’s own decisions Respect for autonomy means that nurses recognize the individual’s uniqueness, the right to be what that person is, and the right to choose personal goals Nurses who follow the principle of autonomy respect a client's right to make decisions even when those choices seem not to be in the client’s best interest 31
 Basic ethical concepts Autonomy…. . (continue) • • • Respect for people also means treating others with consideration In the clinical setting, this principle is violated when a nurse disregards client's subjective accounts of their symptoms (e. g. pain( Patients should give informed consent before tests and procedures are carried out 32
Basic ethical concepts Autonomy…. . (continue) • • • Respect for people also means treating others with consideration In the clinical setting, this principle is violated when a nurse disregards client's subjective accounts of their symptoms (e. g. pain( Patients should give informed consent before tests and procedures are carried out 32
 Basic ethical concepts Beneficence and Nonmaleficence Beneficence: means “doing good” • Nurses should implement actions that benefit clients and their support persons. However, in an increasing technologic health care system, doing good can also pose a risk of doing harm (e. g. intensive exercise program). Nonmaleficence: means the duty to do no harm. • This is the basic of most codes of nursing ethics. • Harm can mean deliberate harm, risk of harm, and unintentional harm. • In nursing, intentional harm is always unacceptable. • The risk of harm is not always clear • A client may be at risk of harm during a nursing intervention that is intended to be helpful (e. g. medication) 33
Basic ethical concepts Beneficence and Nonmaleficence Beneficence: means “doing good” • Nurses should implement actions that benefit clients and their support persons. However, in an increasing technologic health care system, doing good can also pose a risk of doing harm (e. g. intensive exercise program). Nonmaleficence: means the duty to do no harm. • This is the basic of most codes of nursing ethics. • Harm can mean deliberate harm, risk of harm, and unintentional harm. • In nursing, intentional harm is always unacceptable. • The risk of harm is not always clear • A client may be at risk of harm during a nursing intervention that is intended to be helpful (e. g. medication) 33
 Basic ethical concepts Justice • • • Is often referred to as fairness Nurses frequently face decisions in which a sense of justice should prevail (succeed) E. g. busy unit, new admission 34
Basic ethical concepts Justice • • • Is often referred to as fairness Nurses frequently face decisions in which a sense of justice should prevail (succeed) E. g. busy unit, new admission 34
 Basic ethical concepts Fidelity • • • Means to be faithful to agreements and responsibilities one has undertaken Nurses have responsibilities to clients, employers, government, society, the profession, and themselves Circumstances often affect which responsibilities take precedence at a particular time 35
Basic ethical concepts Fidelity • • • Means to be faithful to agreements and responsibilities one has undertaken Nurses have responsibilities to clients, employers, government, society, the profession, and themselves Circumstances often affect which responsibilities take precedence at a particular time 35
 Basic ethical concepts Verasity • • Refers to telling the truth As a nurse should I tell the truth when it is known that doing so will cause harm? Does tell a lie when it is known that the lie will relieve anxiety and fear? Should I lie to dying people? 36
Basic ethical concepts Verasity • • Refers to telling the truth As a nurse should I tell the truth when it is known that doing so will cause harm? Does tell a lie when it is known that the lie will relieve anxiety and fear? Should I lie to dying people? 36
 Basic ethical concepts The standard of best interest • Applied when a decision must be made about a patient’s health care and the patient is unable to make an informed decision 37
Basic ethical concepts The standard of best interest • Applied when a decision must be made about a patient’s health care and the patient is unable to make an informed decision 37
 Ethical theory • An ethical theory provides a framework within which agents can reflect on the acceptability of actions and can evaluate moral judgments and moral character 38
Ethical theory • An ethical theory provides a framework within which agents can reflect on the acceptability of actions and can evaluate moral judgments and moral character 38
 Ethical theories 1 - Teleology 2 - Deontology 3 - Institutionism 4 - Ethic of caring 39
Ethical theories 1 - Teleology 2 - Deontology 3 - Institutionism 4 - Ethic of caring 39
 Ethical theories…. (continue ( Teleology: looks to the consequences of an action in judging whether that action is right or wrong Deontology: proposes that the mortality of a decision is not determined by its consequences. It emphasizes duty, rationality, and obedience to rules The difference between Teleology and Deontology can be seen when each approach is applied to the issue of abortion 40
Ethical theories…. (continue ( Teleology: looks to the consequences of an action in judging whether that action is right or wrong Deontology: proposes that the mortality of a decision is not determined by its consequences. It emphasizes duty, rationality, and obedience to rules The difference between Teleology and Deontology can be seen when each approach is applied to the issue of abortion 40
 Ethical theories…. . (continue ( Example: Teleology approach/abortion: saving the mother’s life (the end, or consequence) justifies the abortion (the mean, or act) Deontology approach/abortion: consider any termination of life as a violation of the rule “do not kill” and therefore, would not abort the fetus, regardless of the consequences to the mother 41
Ethical theories…. . (continue ( Example: Teleology approach/abortion: saving the mother’s life (the end, or consequence) justifies the abortion (the mean, or act) Deontology approach/abortion: consider any termination of life as a violation of the rule “do not kill” and therefore, would not abort the fetus, regardless of the consequences to the mother 41
 Ethical theories…. . (continue ( Institutionism: summarized as the notion that people inherently know what is right or wrong; determining what is right is not a matter or rational thought or learning (e. g. the nurse inherently knows it is wrong to strike a client, the nurse does not need to be taught this or to reason it out) The preceding three theories are based on the concept of fairness (justice) Ethic of caring: it is based on relationships. Caring is a force for protecting and enhancing client dignity Caring is of central importance in the client-nurse relationship (e. g. nurses use trust-telling to affirm clients as a persons rather than objects and to assist them to make choices and find meaning in their illness experiences) 42
Ethical theories…. . (continue ( Institutionism: summarized as the notion that people inherently know what is right or wrong; determining what is right is not a matter or rational thought or learning (e. g. the nurse inherently knows it is wrong to strike a client, the nurse does not need to be taught this or to reason it out) The preceding three theories are based on the concept of fairness (justice) Ethic of caring: it is based on relationships. Caring is a force for protecting and enhancing client dignity Caring is of central importance in the client-nurse relationship (e. g. nurses use trust-telling to affirm clients as a persons rather than objects and to assist them to make choices and find meaning in their illness experiences) 42
 Guidelines for Ethical Reasoning Ø Stay open-minded. Challenge your own views. It’s not enough just to hold a position, you must be able to support it with good reasons. Ø Challenge the views of others if you disagree with them, but do so respectfully and considerately. Ø Philosophical discussion loses most of its value if it’s used as a place to dominate or show off. Ø Philosophical discussion is best done as a community enterprise, where all the discussants work together to get closer to the truth. 43
Guidelines for Ethical Reasoning Ø Stay open-minded. Challenge your own views. It’s not enough just to hold a position, you must be able to support it with good reasons. Ø Challenge the views of others if you disagree with them, but do so respectfully and considerately. Ø Philosophical discussion loses most of its value if it’s used as a place to dominate or show off. Ø Philosophical discussion is best done as a community enterprise, where all the discussants work together to get closer to the truth. 43
 Nursing Codes of Ethics • A code of ethics is a formal statement of a group’s ideals and values. • It is a set of ethical principles that is shared by members of the group, reflects their moral judgments over time and serves as a standard for their professional actions. • Codes of Ethics are usually higher than legal standards • International, state nursing associations have established codes of ethics 44
Nursing Codes of Ethics • A code of ethics is a formal statement of a group’s ideals and values. • It is a set of ethical principles that is shared by members of the group, reflects their moral judgments over time and serves as a standard for their professional actions. • Codes of Ethics are usually higher than legal standards • International, state nursing associations have established codes of ethics 44
 Nursing Codes of Ethics (purposes) 1. 2. 3. 4. 5. 6. To inform the public about the minimum standards of the profession and to help them understand professional nursing conducts To provide a sign of the profession’s commitment to the public it serves To outline the major ethical considerations of the profession To provide general guidelines for professional behavior To guide the profession in self-regulation To remind nurses of the special responsibility they assume when caring for clients. 45
Nursing Codes of Ethics (purposes) 1. 2. 3. 4. 5. 6. To inform the public about the minimum standards of the profession and to help them understand professional nursing conducts To provide a sign of the profession’s commitment to the public it serves To outline the major ethical considerations of the profession To provide general guidelines for professional behavior To guide the profession in self-regulation To remind nurses of the special responsibility they assume when caring for clients. 45
 Nursing Codes of Ethics (elements) • Nurses have four fundamental responsibilities: to promote health, to prevent illness, to restore health, and alleviate suffering. • Nurses and people • Nurses and practice • Nurses and the profession • Nurses and the coworkers 46
Nursing Codes of Ethics (elements) • Nurses have four fundamental responsibilities: to promote health, to prevent illness, to restore health, and alleviate suffering. • Nurses and people • Nurses and practice • Nurses and the profession • Nurses and the coworkers 46
 What is Ethical Decision Making? • When faced with an ethical dilemma the objective is to make a judgment based on well-reasoned, defensible ethical principles. • The risk is poor judgment i. e. a low-quality decision • A low-quality decision can have a wide range of negative consequences 47
What is Ethical Decision Making? • When faced with an ethical dilemma the objective is to make a judgment based on well-reasoned, defensible ethical principles. • The risk is poor judgment i. e. a low-quality decision • A low-quality decision can have a wide range of negative consequences 47
 Two Types of Ethical Choices • Right vs wrong: choosing right from wrong is the easiest • Right vs right • Situation contains shades of gray i. e. all alternative have desirable and undesirable results • Choosing “the lesser of two evils” • Objective: make a defensible decision 48
Two Types of Ethical Choices • Right vs wrong: choosing right from wrong is the easiest • Right vs right • Situation contains shades of gray i. e. all alternative have desirable and undesirable results • Choosing “the lesser of two evils” • Objective: make a defensible decision 48
 Factors that influence EDM 1. 2. 3. 4. 5. 6. 7. 8. Codes for Nurses The patient’s rights Social and cultural attitudes Science and technology Legislation Judicial decisions Funding Personal religious and philosophic viewpoint 49
Factors that influence EDM 1. 2. 3. 4. 5. 6. 7. 8. Codes for Nurses The patient’s rights Social and cultural attitudes Science and technology Legislation Judicial decisions Funding Personal religious and philosophic viewpoint 49
 Factors in the work environment that affect EDM 1. 2. 3. 4. 5. 6. Status as an employment Collective bargaining contracts Collegial relationships Authoritarian and paternalistic background Ethics committees in health care Consumer involvement in health care 50
Factors in the work environment that affect EDM 1. 2. 3. 4. 5. 6. Status as an employment Collective bargaining contracts Collegial relationships Authoritarian and paternalistic background Ethics committees in health care Consumer involvement in health care 50
 A framework for Ethical Decision Making (EDM) 1. 2. 3. 4. 5. Identify and clarify the ethical problem Gather data Identify options Make a decision Act and assess 51
A framework for Ethical Decision Making (EDM) 1. 2. 3. 4. 5. Identify and clarify the ethical problem Gather data Identify options Make a decision Act and assess 51
 Making Moral Decisions--Some Inappropriate Ways: • Appeal to Authority • Appeal to Law • Appeal exclusively to self-interest 52
Making Moral Decisions--Some Inappropriate Ways: • Appeal to Authority • Appeal to Law • Appeal exclusively to self-interest 52
 Some Guidelines for Making Ethical Decisions 1. Choose correct moral language. (Often, the way in which you initially conceptualize a situation will affect what moral conclusions you will make) 2. Be as clear as you can about the facts, both empirical and philosophical 3. Consider the relevant moral principles and rules, and make your best judgment. 53
Some Guidelines for Making Ethical Decisions 1. Choose correct moral language. (Often, the way in which you initially conceptualize a situation will affect what moral conclusions you will make) 2. Be as clear as you can about the facts, both empirical and philosophical 3. Consider the relevant moral principles and rules, and make your best judgment. 53
 Ethics Committees With the increasing complexity of ethical issues in health care, ethics committees have been created to assist in making ethical decisions in clinical settings. Ethical committees can: 1. Provide structure and guidelines for potential problems. 2. Serve as an open forum for discussion and debate. 3. Function as a patient advocate by placing the patient at the core of the committee’s deliberations. 54
Ethics Committees With the increasing complexity of ethical issues in health care, ethics committees have been created to assist in making ethical decisions in clinical settings. Ethical committees can: 1. Provide structure and guidelines for potential problems. 2. Serve as an open forum for discussion and debate. 3. Function as a patient advocate by placing the patient at the core of the committee’s deliberations. 54
 Discussion Questions • Is the patient’s decision a rational one? • What is the difference between withholding and withdrawing life-sustaining treatment? • In view of the fact that a potent sedative such as morphine may produce respiratory depression, should this be given prior to discontinuing the respirator? Would this constitute active euthanasia? • Would the situation be different if Mrs. C. had a living will? • What role could the nurse play in addressing the ethical issues in this case? 55
Discussion Questions • Is the patient’s decision a rational one? • What is the difference between withholding and withdrawing life-sustaining treatment? • In view of the fact that a potent sedative such as morphine may produce respiratory depression, should this be given prior to discontinuing the respirator? Would this constitute active euthanasia? • Would the situation be different if Mrs. C. had a living will? • What role could the nurse play in addressing the ethical issues in this case? 55
 notes • Euthanasia Greek words meaning “easy death”. Euthanasia is an act by which the causative agent of death is administered by another with the intent to end life. Killing an innocent person, even at his or her request is not ethical. “Code for Nurses (1985) and the ANA position statement (1994) states that the nurse should not participate in euthanasia but be vigilant advocates for the delivery of 56 dignified and human care.
notes • Euthanasia Greek words meaning “easy death”. Euthanasia is an act by which the causative agent of death is administered by another with the intent to end life. Killing an innocent person, even at his or her request is not ethical. “Code for Nurses (1985) and the ANA position statement (1994) states that the nurse should not participate in euthanasia but be vigilant advocates for the delivery of 56 dignified and human care.
 • Living Wills Prepared while patient has decisional capacity Describes patient preferences in the event they become incapable of making decisions or communicating decisions. Usually describes what type of life prolonging procedures the patient would or would not want and circumstances under which they would want these procedures carried out, withheld, or withdrawn 57
• Living Wills Prepared while patient has decisional capacity Describes patient preferences in the event they become incapable of making decisions or communicating decisions. Usually describes what type of life prolonging procedures the patient would or would not want and circumstances under which they would want these procedures carried out, withheld, or withdrawn 57


