92d9fafa63b52885ce96f60e707ee0b2.ppt
- Количество слайдов: 42

 Entering the ICU: How to do this from the Physiatrist’s Perspective Julie Lanphere DO Assistant Professor Department of Physical Medicine & Rehabilitation Medical Director UPMC Rehabilitation Institute at Montefiore
Entering the ICU: How to do this from the Physiatrist’s Perspective Julie Lanphere DO Assistant Professor Department of Physical Medicine & Rehabilitation Medical Director UPMC Rehabilitation Institute at Montefiore
 • I have no conflicts of interest to report. • I do not endorse any products that may be pictured in any photos.
• I have no conflicts of interest to report. • I do not endorse any products that may be pictured in any photos.
 Objectives • Understand key pearls on how to build an early mobility program in your local institution • Understand how to become comfortable working with ICU patients • Understand the basic concepts and clinical pearls required for critically ill patients using a therapy program in the ICU
Objectives • Understand key pearls on how to build an early mobility program in your local institution • Understand how to become comfortable working with ICU patients • Understand the basic concepts and clinical pearls required for critically ill patients using a therapy program in the ICU
 Physiatry in the ICU • Multidisciplinary team management • Enhance and restore functional ability and quality of life • Critical illness population-vulnerable Cognitive deficits- delirium, agitation, memory, attention Physical deficits- weakness, debility, CIN, CIM Emotional deficits- anxiety, depression, PTSD, paranoia Medical complexity -Cardiopulmonary deconditioning -Respiratory failure, multiorgan system injury • Functional deficits in mobility, endurance, self care/ADL’s, cognition
Physiatry in the ICU • Multidisciplinary team management • Enhance and restore functional ability and quality of life • Critical illness population-vulnerable Cognitive deficits- delirium, agitation, memory, attention Physical deficits- weakness, debility, CIN, CIM Emotional deficits- anxiety, depression, PTSD, paranoia Medical complexity -Cardiopulmonary deconditioning -Respiratory failure, multiorgan system injury • Functional deficits in mobility, endurance, self care/ADL’s, cognition
 Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
 Rehabilitation in the ICU • Current literature supports that early mobility in the critical care unit has a positive effect on cardiopulmonary, neurological, musculoskeletal, and integumentary systems • SAFE and FEASIBLE • Literature supports that detrimental medical complications occur with bed rest and immobility • “You can’t debate the evidence that demonstrates that there’s a benefit to early rehabilitation. It’s like debating the sky is blue. ” Director of Rehabilitation Services
Rehabilitation in the ICU • Current literature supports that early mobility in the critical care unit has a positive effect on cardiopulmonary, neurological, musculoskeletal, and integumentary systems • SAFE and FEASIBLE • Literature supports that detrimental medical complications occur with bed rest and immobility • “You can’t debate the evidence that demonstrates that there’s a benefit to early rehabilitation. It’s like debating the sky is blue. ” Director of Rehabilitation Services
 ICU Mobility & Immobility: Evidence Based Medicine Suggested Readings v Schweickert, W. D. et al. Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest. December, 2011, Vol 6, 1612 -1617. v Morris, Peter et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Critical Care Medicine, 2008, Vol 36, No 8. v Herridge et al. One Year Outcomes in Survivors of ARDS. 2003; 348(8): 683 -693. v Herridge et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N Engl J Med. 2011; 364; 1293 -304. v Needham et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care Med 2012; 40: 502 -509. v Kress, J. P. , Hall, J. B. , ICU-Acquired Weakness and Recovery from Critical Illness. N Engl J Med. 2014: 1626 -1635
ICU Mobility & Immobility: Evidence Based Medicine Suggested Readings v Schweickert, W. D. et al. Implementing early mobilization interventions in mechanically ventilated patients in the ICU. Chest. December, 2011, Vol 6, 1612 -1617. v Morris, Peter et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Critical Care Medicine, 2008, Vol 36, No 8. v Herridge et al. One Year Outcomes in Survivors of ARDS. 2003; 348(8): 683 -693. v Herridge et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N Engl J Med. 2011; 364; 1293 -304. v Needham et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care Med 2012; 40: 502 -509. v Kress, J. P. , Hall, J. B. , ICU-Acquired Weakness and Recovery from Critical Illness. N Engl J Med. 2014: 1626 -1635
 Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
 Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. GOALS: • Reduce sedation and delirium to allow for mobility • Enforce and increase rehabilitation presence in the Unit • Decrease LOS
Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. GOALS: • Reduce sedation and delirium to allow for mobility • Enforce and increase rehabilitation presence in the Unit • Decrease LOS
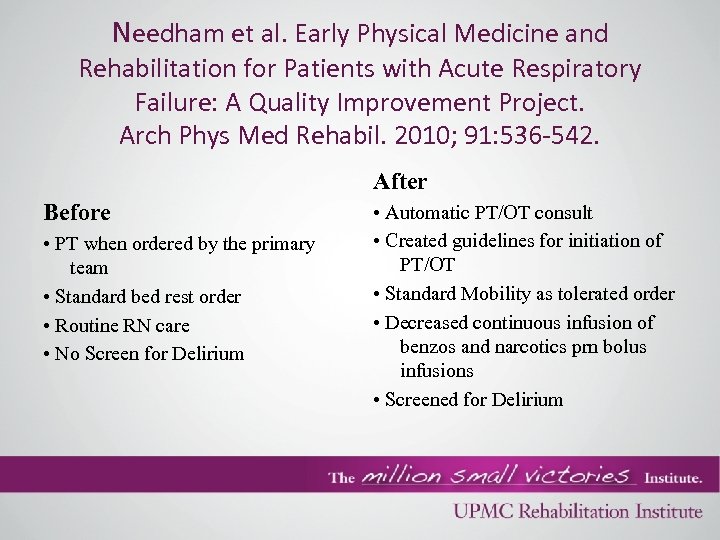 Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. After Before • PT when ordered by the primary team • Standard bed rest order • Routine RN care • No Screen for Delirium • Automatic PT/OT consult • Created guidelines for initiation of PT/OT • Standard Mobility as tolerated order • Decreased continuous infusion of benzos and narcotics prn bolus infusions • Screened for Delirium
Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. After Before • PT when ordered by the primary team • Standard bed rest order • Routine RN care • No Screen for Delirium • Automatic PT/OT consult • Created guidelines for initiation of PT/OT • Standard Mobility as tolerated order • Decreased continuous infusion of benzos and narcotics prn bolus infusions • Screened for Delirium
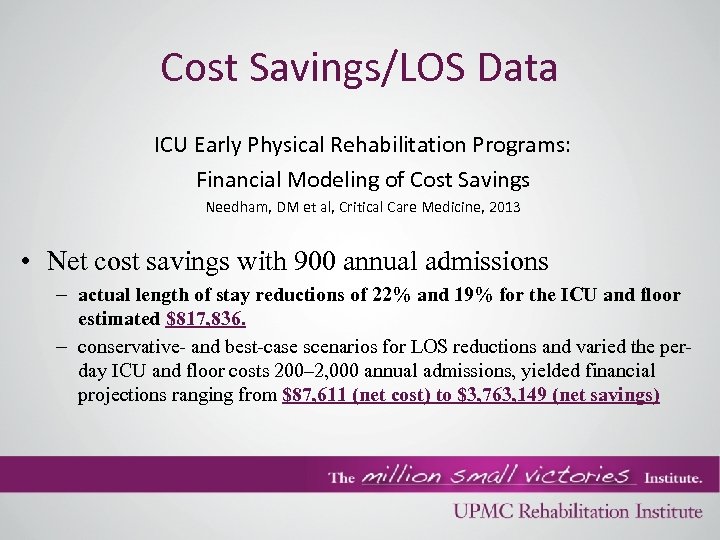 Cost Savings/LOS Data ICU Early Physical Rehabilitation Programs: Financial Modeling of Cost Savings Needham, DM et al, Critical Care Medicine, 2013 • Net cost savings with 900 annual admissions – actual length of stay reductions of 22% and 19% for the ICU and floor estimated $817, 836. – conservative- and best-case scenarios for LOS reductions and varied the perday ICU and floor costs 200– 2, 000 annual admissions, yielded financial projections ranging from $87, 611 (net cost) to $3, 763, 149 (net savings)
Cost Savings/LOS Data ICU Early Physical Rehabilitation Programs: Financial Modeling of Cost Savings Needham, DM et al, Critical Care Medicine, 2013 • Net cost savings with 900 annual admissions – actual length of stay reductions of 22% and 19% for the ICU and floor estimated $817, 836. – conservative- and best-case scenarios for LOS reductions and varied the perday ICU and floor costs 200– 2, 000 annual admissions, yielded financial projections ranging from $87, 611 (net cost) to $3, 763, 149 (net savings)
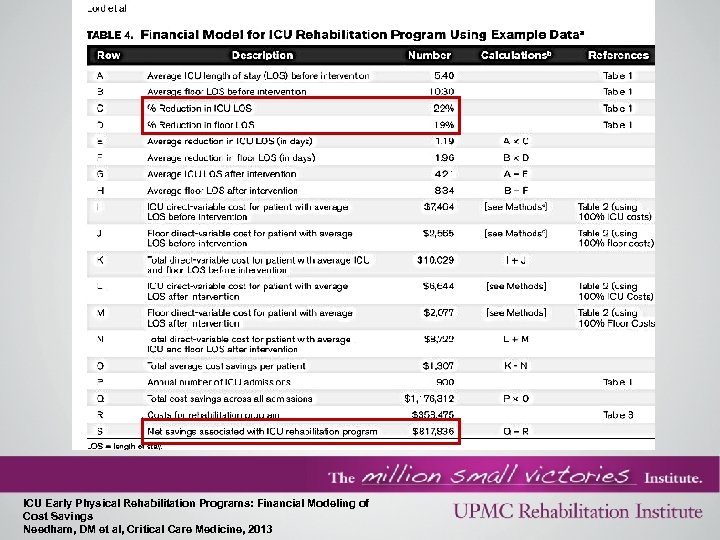 ICU Early Physical Rehabilitation Programs: Financial Modeling of Cost Savings Needham, DM et al, Critical Care Medicine, 2013
ICU Early Physical Rehabilitation Programs: Financial Modeling of Cost Savings Needham, DM et al, Critical Care Medicine, 2013
 Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
Early Mobility Implementation Program • Engage physician leadership for support • Need a critical care physician and RN director champions • Engage therapy and hospital administration leadership to discuss dedicated therapy/RN driven early mobility program • Staff education-sedation protocols, team concept, evidence surrounding feasibility and strengths of ICU early mobility • CQI to assess mobility interactions, HLOS, ICU LOS, HAP/VAP, DVT’s
 Medical Intensive Care Unit: MOBILITY PROJECT
Medical Intensive Care Unit: MOBILITY PROJECT
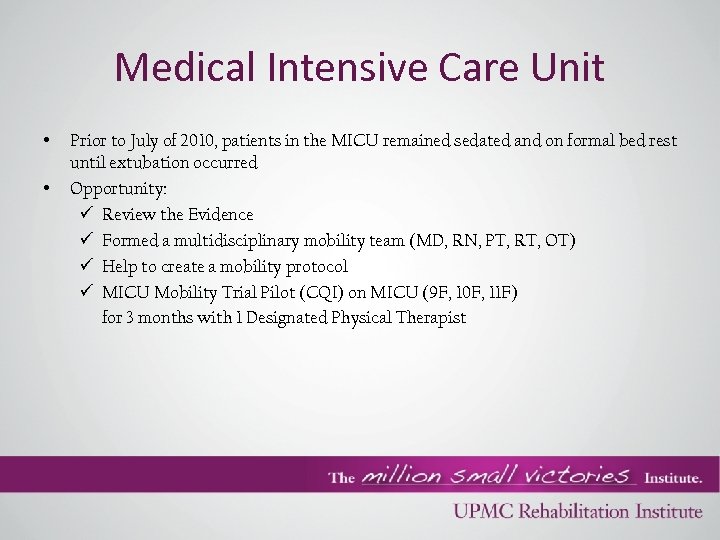 Medical Intensive Care Unit • • Prior to July of 2010, patients in the MICU remained sedated and on formal bed rest until extubation occurred Opportunity: ü Review the Evidence ü Formed a multidisciplinary mobility team (MD, RN, PT, RT, OT) ü Help to create a mobility protocol ü MICU Mobility Trial Pilot (CQI) on MICU (9 F, 10 F, 11 F) for 3 months with 1 Designated Physical Therapist
Medical Intensive Care Unit • • Prior to July of 2010, patients in the MICU remained sedated and on formal bed rest until extubation occurred Opportunity: ü Review the Evidence ü Formed a multidisciplinary mobility team (MD, RN, PT, RT, OT) ü Help to create a mobility protocol ü MICU Mobility Trial Pilot (CQI) on MICU (9 F, 10 F, 11 F) for 3 months with 1 Designated Physical Therapist
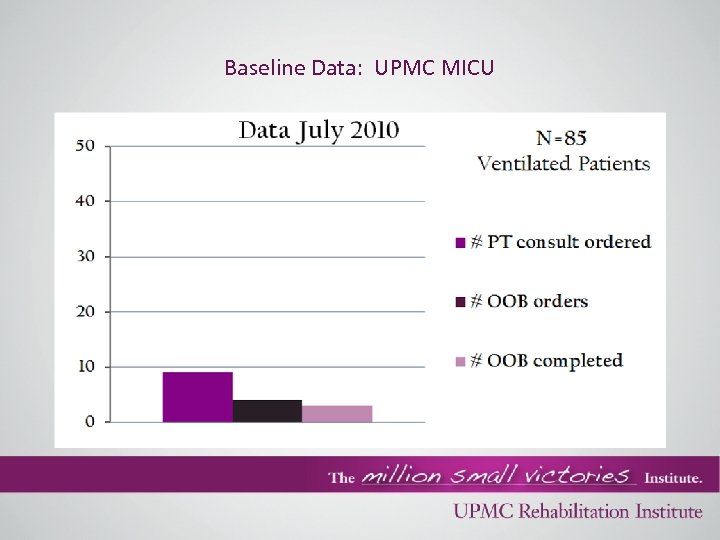 Baseline Data: UPMC MICU
Baseline Data: UPMC MICU
 MICU Mobility Goals • Start with Mobility Protocol /order set – All patients admitted to unit screened by Physical Therapy – Define and redefine relative/absolute contraindications – Sedation Protocol – Delirium screening • Education to nursing staff by therapy (mobility intervention, transfer techniques, body mechanics, safety)
MICU Mobility Goals • Start with Mobility Protocol /order set – All patients admitted to unit screened by Physical Therapy – Define and redefine relative/absolute contraindications – Sedation Protocol – Delirium screening • Education to nursing staff by therapy (mobility intervention, transfer techniques, body mechanics, safety)
 • Education by MD champion to the RN’s, residents, and Fellows (sedation protocols/delirium/pain) • Serve as resource for other ICU’s who wish to implement mobility program
• Education by MD champion to the RN’s, residents, and Fellows (sedation protocols/delirium/pain) • Serve as resource for other ICU’s who wish to implement mobility program
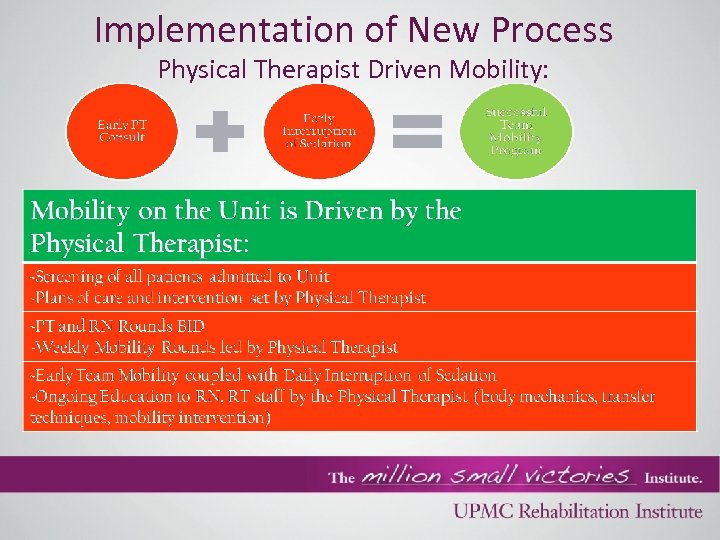 Implementation of New Process Physical Therapist Driven Mobility:
Implementation of New Process Physical Therapist Driven Mobility:
 Mobility Rounds GOAL: Identify barriers to for mobility • Pulmonary/Critical Care – Attending Physician Champion – House staff (residents, fellows) • Physiatrist • PT (+/- PT aide) • Nurse clinician • RN Research Team • Bedside nurses – Presenter • Respiratory therapy
Mobility Rounds GOAL: Identify barriers to for mobility • Pulmonary/Critical Care – Attending Physician Champion – House staff (residents, fellows) • Physiatrist • PT (+/- PT aide) • Nurse clinician • RN Research Team • Bedside nurses – Presenter • Respiratory therapy
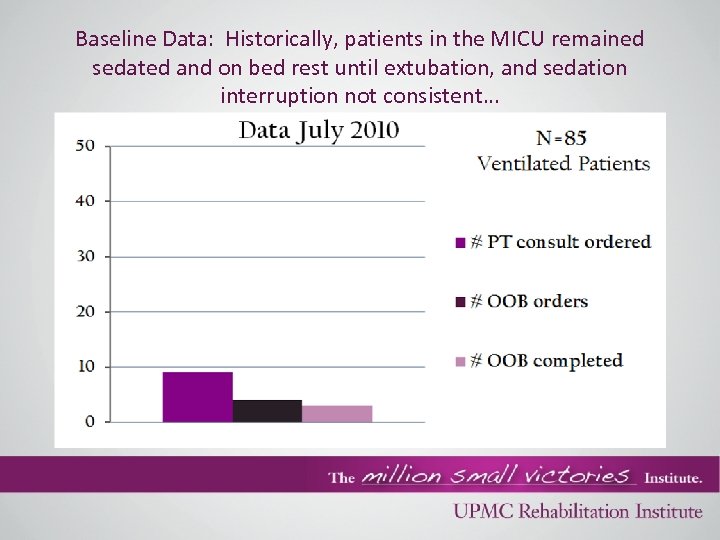 Baseline Data: Historically, patients in the MICU remained sedated and on bed rest until extubation, and sedation interruption not consistent…
Baseline Data: Historically, patients in the MICU remained sedated and on bed rest until extubation, and sedation interruption not consistent…
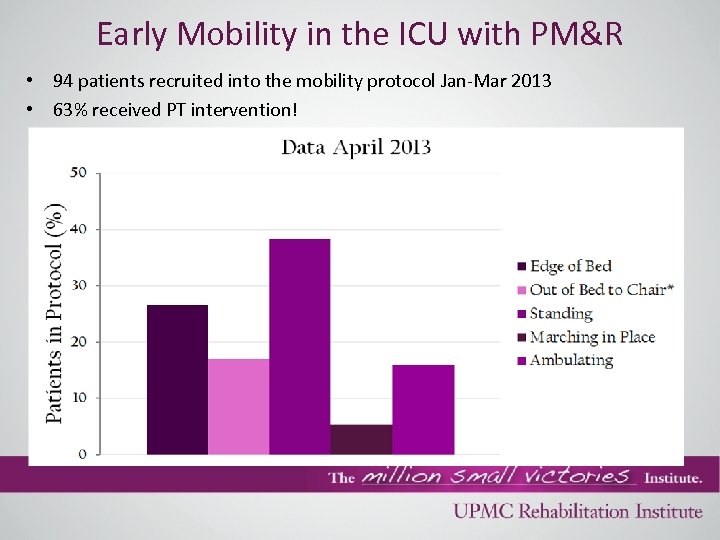 Early Mobility in the ICU with PM&R • 94 patients recruited into the mobility protocol Jan-Mar 2013 • 63% received PT intervention!
Early Mobility in the ICU with PM&R • 94 patients recruited into the mobility protocol Jan-Mar 2013 • 63% received PT intervention!
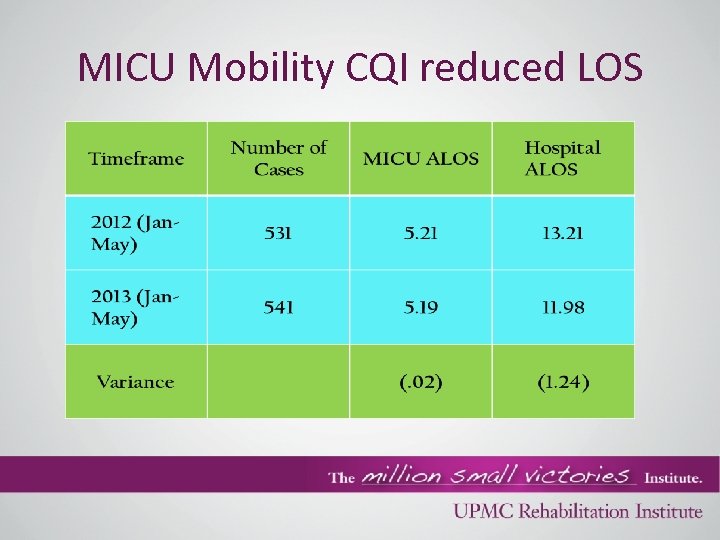 MICU Mobility CQI reduced LOS
MICU Mobility CQI reduced LOS
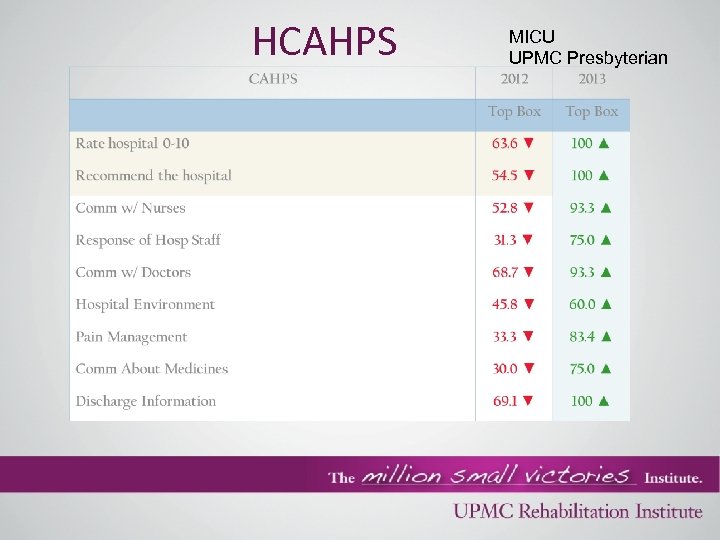 HCAHPS MICU UPMC Presbyterian
HCAHPS MICU UPMC Presbyterian
 MICU Mobility Safety • ~10% of sessions interrupted for safety concern – – – – 26 Majority sustained desaturation Sp. O 2 <90% 1 syncope episode with spontaneous recovery 1 AICD discharge – AF with aberrant conduction and RVR 0 Falls / Assist to floor 0 CVC, feeding tube dislodgement 1 partial ETT dislodgement <10% Rectal tube dislodgement
MICU Mobility Safety • ~10% of sessions interrupted for safety concern – – – – 26 Majority sustained desaturation Sp. O 2 <90% 1 syncope episode with spontaneous recovery 1 AICD discharge – AF with aberrant conduction and RVR 0 Falls / Assist to floor 0 CVC, feeding tube dislodgement 1 partial ETT dislodgement <10% Rectal tube dislodgement
 A Typical Day in the MICU INFORMATION ~ COORDINATION • • ~ TIMING Daily bedside rounds by RN clinician, PT, and bedside nurse Evaluate patient stability & level of functioning Evaluation of new consults Coordination of care with RN based on – Procedures – Sedation interruption – Weaning trials • Mobility protocol implemented based on patient specific needs • Documentation of progress in medical record
A Typical Day in the MICU INFORMATION ~ COORDINATION • • ~ TIMING Daily bedside rounds by RN clinician, PT, and bedside nurse Evaluate patient stability & level of functioning Evaluation of new consults Coordination of care with RN based on – Procedures – Sedation interruption – Weaning trials • Mobility protocol implemented based on patient specific needs • Documentation of progress in medical record
 Getting Comfortable with Critically Ill Patients • Know the evidence • Guidelines to modify therapies • • • Fi. O 2 greater than 60% PEEP greater than 10 cm H 2 O Consistent O 2 Saturations less than 92% Hx of desaturations with positional changes during nursing care Unstable BP on pressors or inotropes Severe Acidosis with p. H less than 7. 30
Getting Comfortable with Critically Ill Patients • Know the evidence • Guidelines to modify therapies • • • Fi. O 2 greater than 60% PEEP greater than 10 cm H 2 O Consistent O 2 Saturations less than 92% Hx of desaturations with positional changes during nursing care Unstable BP on pressors or inotropes Severe Acidosis with p. H less than 7. 30
 Getting Comfortable with Critically Ill Patients Absolute Contraindications TO Stop Therapy 1. 2. 3. 4. Severe CP associated with EKG changes HR above predicted MHR or pre-determined limits set by medical team Hypotension associated with dizziness, lightheadedness, and diaphoresis Intolerable dyspnea, nasal flaring, or cyanosis 5. 6. 7. 8. 9. Unable to recover from or maintain Sp. O 2 of 85% or more despite supplemental oxygen Severe pain despite analgesia Extreme fatigue Patient or Therapist Safety Patient wishes to stop
Getting Comfortable with Critically Ill Patients Absolute Contraindications TO Stop Therapy 1. 2. 3. 4. Severe CP associated with EKG changes HR above predicted MHR or pre-determined limits set by medical team Hypotension associated with dizziness, lightheadedness, and diaphoresis Intolerable dyspnea, nasal flaring, or cyanosis 5. 6. 7. 8. 9. Unable to recover from or maintain Sp. O 2 of 85% or more despite supplemental oxygen Severe pain despite analgesia Extreme fatigue Patient or Therapist Safety Patient wishes to stop
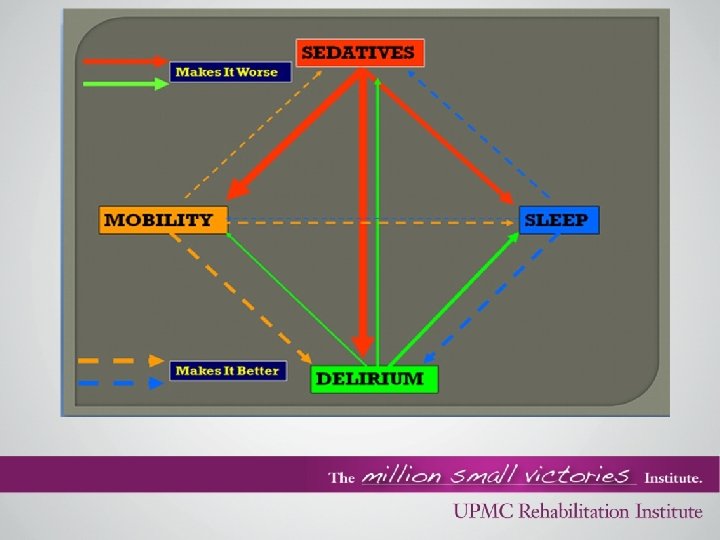
 Sedation Protocols • Understand Sedation Protocols Assess need for & treat pain prior to sedatives Identify & treat delirium Expect agitation as sedation decreased and emphasize nonpharmacological methods to bridge to wakefulness Target cessation of continuous sedative infusion by 48 hours after intubation • Goal: Awake and Breathing at 48 hrs after intubation without using continuous infusions
Sedation Protocols • Understand Sedation Protocols Assess need for & treat pain prior to sedatives Identify & treat delirium Expect agitation as sedation decreased and emphasize nonpharmacological methods to bridge to wakefulness Target cessation of continuous sedative infusion by 48 hours after intubation • Goal: Awake and Breathing at 48 hrs after intubation without using continuous infusions
 ABCDE Bundle Improving Outcomes for Ventilated Patients An Expert Interview With Chandra Alexander RN, CCRN, and Dena Putnam, RN, BA, MBA, Elizabeth Mc. Gann, DNSc, RN, June 14, 2012 A: Awakening trials for ventilated patients.
B: Spontaneous breathing trials.
C: Coordinated effort between the registered nurse and respiratory therapist to perform the spontaneous breathing trial when the patient is awakened by reducing or stopping the patient's sedation. The combination of sedation and analgesics being used are reviewed, and changes or reductions in the doses are considered.
D: A standardized delirium assessment program, including treatment and prevention options.
E: Early mobilization and ambulation of critical care patients.
ABCDE Bundle Improving Outcomes for Ventilated Patients An Expert Interview With Chandra Alexander RN, CCRN, and Dena Putnam, RN, BA, MBA, Elizabeth Mc. Gann, DNSc, RN, June 14, 2012 A: Awakening trials for ventilated patients.
B: Spontaneous breathing trials.
C: Coordinated effort between the registered nurse and respiratory therapist to perform the spontaneous breathing trial when the patient is awakened by reducing or stopping the patient's sedation. The combination of sedation and analgesics being used are reviewed, and changes or reductions in the doses are considered.
D: A standardized delirium assessment program, including treatment and prevention options.
E: Early mobilization and ambulation of critical care patients.
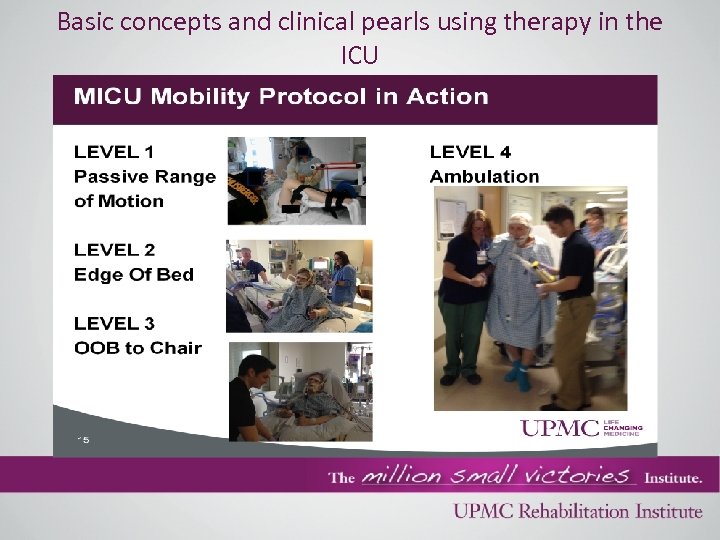 Basic concepts and clinical pearls using therapy in the ICU
Basic concepts and clinical pearls using therapy in the ICU
 Basic concepts and clinical pearls using therapy in the ICU • Remember the basics to mobility *Edge of bed sitting (CORE/RESPIRATORY MUSCLES/CARDIOPULM) *Transfers/standing/sit in chair (Likolift, power standers, wheeled walkers, hand held assist) (CORE/RESPIRATORY MUSCLES/CARDIOPULM + PERIPHERAL MUSCLE/NERVE STIMULATION, STRENGTHENING) *Ambulation (speaks for itself)-Wheeled Walkers *Stationary Bikes, therabands, Nustep *PT, OT, SLP, Neuro Psych, Inpatient rehab if indicated/Outpatient therapies at DC (don’t forget these!) SLEEP/WAKE CYCLES
Basic concepts and clinical pearls using therapy in the ICU • Remember the basics to mobility *Edge of bed sitting (CORE/RESPIRATORY MUSCLES/CARDIOPULM) *Transfers/standing/sit in chair (Likolift, power standers, wheeled walkers, hand held assist) (CORE/RESPIRATORY MUSCLES/CARDIOPULM + PERIPHERAL MUSCLE/NERVE STIMULATION, STRENGTHENING) *Ambulation (speaks for itself)-Wheeled Walkers *Stationary Bikes, therabands, Nustep *PT, OT, SLP, Neuro Psych, Inpatient rehab if indicated/Outpatient therapies at DC (don’t forget these!) SLEEP/WAKE CYCLES
 Family Presence Advocate/motivator/help mood Less sedation Hygiene care Advocacy-prevents complications, med error prevention, unnecessary procedures • Invested in the patient • •
Family Presence Advocate/motivator/help mood Less sedation Hygiene care Advocacy-prevents complications, med error prevention, unnecessary procedures • Invested in the patient • •
 Mobility-A Docs Perspective as a Patient • Huge impact on delirium and when you get home (1700) • Issues after DC do not get addressed by PCP, other medical providers • “The four steps to get into my house are my biggest physical barriers when I leave the ICU. ” • “As a critical care doc, I didn’t get a lot of training about assistive devices patients can use at discharge. I just don’t think about it in my daily practice, about how I can make it easier for my patient when they get home. Not a lot of my primary care physicians and specialists address this. Until I saw my rehab specialists at discharge, these issues did not get addressed.
Mobility-A Docs Perspective as a Patient • Huge impact on delirium and when you get home (1700) • Issues after DC do not get addressed by PCP, other medical providers • “The four steps to get into my house are my biggest physical barriers when I leave the ICU. ” • “As a critical care doc, I didn’t get a lot of training about assistive devices patients can use at discharge. I just don’t think about it in my daily practice, about how I can make it easier for my patient when they get home. Not a lot of my primary care physicians and specialists address this. Until I saw my rehab specialists at discharge, these issues did not get addressed.
 Mobility-A Docs Perspective as a Patient • Sleep issues-big problem! “IF YOU CAN’T SLEEP, YOU CAN’T COPE. ” PTSD exaggerated, becomes a vicious cycle • Fear of getting sick again (lack of resources, seeking care post ICU DC, who do you call? ? ) • Depression-family members and patients • Set expectations on how to get better
Mobility-A Docs Perspective as a Patient • Sleep issues-big problem! “IF YOU CAN’T SLEEP, YOU CAN’T COPE. ” PTSD exaggerated, becomes a vicious cycle • Fear of getting sick again (lack of resources, seeking care post ICU DC, who do you call? ? ) • Depression-family members and patients • Set expectations on how to get better

 Educational and Tutorial Videos Dale Neeham MD-Into • http: //www. youtube. com/watch? v=D 53 gyg. WRh. LM Phyllis-ICU REHAB COURSE-Short version • http: //www. youtube. com/watch? v=woofpnw-u 74 ICU Delirium • http: //www. youtube. com/watch? v=30 sbef. Bcj. EU&feature=you tu. be
Educational and Tutorial Videos Dale Neeham MD-Into • http: //www. youtube. com/watch? v=D 53 gyg. WRh. LM Phyllis-ICU REHAB COURSE-Short version • http: //www. youtube. com/watch? v=woofpnw-u 74 ICU Delirium • http: //www. youtube. com/watch? v=30 sbef. Bcj. EU&feature=you tu. be
 • Recovering from the ICU: An MD Survivor's Story/Perspective: http: //www. youtube. com/watch? v=bvm 6_6 vt. Ga 4 • University of Chicago PT/OT mobilization Video of patient https: //www. youtube. com/watch? v=6 xe. Hvr 9 Wax. Q&feature= youtu. be&a • Hopkins Early Mobility Resource website http: //www. hopkinsmedicine. org/pulmonary/research/outco mes_after_critical_illness_surgery/oacis_videos_news. html
• Recovering from the ICU: An MD Survivor's Story/Perspective: http: //www. youtube. com/watch? v=bvm 6_6 vt. Ga 4 • University of Chicago PT/OT mobilization Video of patient https: //www. youtube. com/watch? v=6 xe. Hvr 9 Wax. Q&feature= youtu. be&a • Hopkins Early Mobility Resource website http: //www. hopkinsmedicine. org/pulmonary/research/outco mes_after_critical_illness_surgery/oacis_videos_news. html
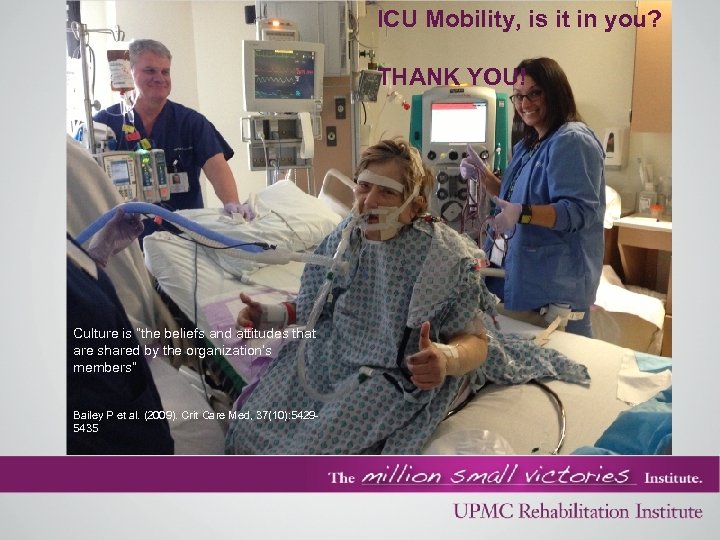 ICU Mobility, is it in you? THANK YOU! Culture is “the beliefs and attitudes that are shared by the organization’s members” Bailey P et al. (2009). Crit Care Med, 37(10): 54295435
ICU Mobility, is it in you? THANK YOU! Culture is “the beliefs and attitudes that are shared by the organization’s members” Bailey P et al. (2009). Crit Care Med, 37(10): 54295435
 References Herridge et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N Engl J Med 2011; 364; 1293 -304 Needham et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care. Med 2012; 40: 502 -509. Morris et al. Early Intensive Care Unit Mobility Therapy in the treatment of Acute Respiratory Failure. Crit Care Med. 2008; 36(8): 2238 -2243 Schweickert WD et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet. 2009; 373: 1874 -82. Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. An Expert Interview With Chandra Alexander RN, CCRN, and Dena Putnam, RN, BA, MBA, Elizabeth Mc. Gann, DNSc, RN, Improving Outcomes for Ventilated Patients. June 14, 2012 Pohlman M C, Schweickert W D, Pohlman A S, Nigos C, Pawlik A J, Esbrook C L, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt G A, Bowman A, Barr R, Mc. Callister K, Hall J B, Kress J P. Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Critical Care Medicine. 2010; Vol 38, Number 11: 2089 -2094. Kress, J. P. , Hall, J. B. , ICU-Acquired Weakness and Recovery from Critical Illness. NEJM 2014: 1626 -1635 http: //www. aacn. org/WD/practice/docs/practicealerts/delirium-practice-alert-2011. pdf Motomed CQI Powerpoint Sept 2012 MICU Team MICU Mobility Magnet Presentation 2014 UPMC MICU Mobility Pilot Data UPMC MICU Mobility Patient Photos UPMC MICU Mobility Patient Video
References Herridge et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N Engl J Med 2011; 364; 1293 -304 Needham et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit Care. Med 2012; 40: 502 -509. Morris et al. Early Intensive Care Unit Mobility Therapy in the treatment of Acute Respiratory Failure. Crit Care Med. 2008; 36(8): 2238 -2243 Schweickert WD et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet. 2009; 373: 1874 -82. Needham et al. Early Physical Medicine and Rehabilitation for Patients with Acute Respiratory Failure: A Quality Improvement Project. Arch Phys Med Rehabil. 2010; 91: 536 -542. An Expert Interview With Chandra Alexander RN, CCRN, and Dena Putnam, RN, BA, MBA, Elizabeth Mc. Gann, DNSc, RN, Improving Outcomes for Ventilated Patients. June 14, 2012 Pohlman M C, Schweickert W D, Pohlman A S, Nigos C, Pawlik A J, Esbrook C L, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt G A, Bowman A, Barr R, Mc. Callister K, Hall J B, Kress J P. Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Critical Care Medicine. 2010; Vol 38, Number 11: 2089 -2094. Kress, J. P. , Hall, J. B. , ICU-Acquired Weakness and Recovery from Critical Illness. NEJM 2014: 1626 -1635 http: //www. aacn. org/WD/practice/docs/practicealerts/delirium-practice-alert-2011. pdf Motomed CQI Powerpoint Sept 2012 MICU Team MICU Mobility Magnet Presentation 2014 UPMC MICU Mobility Pilot Data UPMC MICU Mobility Patient Photos UPMC MICU Mobility Patient Video


