f2d180d490407de455df9a19909fbcdf.ppt
- Количество слайдов: 68
 ENTC 4350 Pacemakers
ENTC 4350 Pacemakers
 l A pacemaker is a prosthetic device for the heart, first conceived in 1932 by Albert S. Hymen, an American cardiologist. • In 1952 the pacemaker was used clinically by Paul M. Zoll as an external device.
l A pacemaker is a prosthetic device for the heart, first conceived in 1932 by Albert S. Hymen, an American cardiologist. • In 1952 the pacemaker was used clinically by Paul M. Zoll as an external device.
 l With the advent of solid-state circuitry in the early 1960 s, it was made into a battery-operated prosthesis that was implantable into the patient. • Credit for the implantable pacemaker is given to the American physicians William Chardack and Andrew Gage and to the engineer Wilson Greatbatch.
l With the advent of solid-state circuitry in the early 1960 s, it was made into a battery-operated prosthesis that was implantable into the patient. • Credit for the implantable pacemaker is given to the American physicians William Chardack and Andrew Gage and to the engineer Wilson Greatbatch.
 l Other heart prostheses, or spare parts, include coronary bypass vessels and artificial heart valves. • An especially innovative recent heart prosthesis is the artificial heart, the best known example of which is the Jarvik-7, designed by Robert K. Jarvik and implanted into Barney Clark by William De. Vries in 1982. • Another implantable artificial heart was developed in 1985 at Penn State University by a team headed by William Pierce.
l Other heart prostheses, or spare parts, include coronary bypass vessels and artificial heart valves. • An especially innovative recent heart prosthesis is the artificial heart, the best known example of which is the Jarvik-7, designed by Robert K. Jarvik and implanted into Barney Clark by William De. Vries in 1982. • Another implantable artificial heart was developed in 1985 at Penn State University by a team headed by William Pierce.
 l A pacemaker is a prosthesis specifically for the sinoatrial (SA) node of the heart. • The SA node may become ineffective for several reasons, among them: 1. the SA node tissue or atrium may become diseased; or 2. the path of the heart depolarization—specifically, the atrioventricular (AV) node from the atrium to the ventricles—may become diseased, producing a heart block.
l A pacemaker is a prosthesis specifically for the sinoatrial (SA) node of the heart. • The SA node may become ineffective for several reasons, among them: 1. the SA node tissue or atrium may become diseased; or 2. the path of the heart depolarization—specifically, the atrioventricular (AV) node from the atrium to the ventricles—may become diseased, producing a heart block.
 l Furthermore, bradycardia, a slowing of the heart rate generally to below 50 or 60 beats per minute (bpm), may develop because of aging or other reasons. • These diseases may be treated either with a pacemaker or with medicine, depending upon the case.
l Furthermore, bradycardia, a slowing of the heart rate generally to below 50 or 60 beats per minute (bpm), may develop because of aging or other reasons. • These diseases may be treated either with a pacemaker or with medicine, depending upon the case.
 l In the case that the SA node fails to pace the heart properly, the ventricles may beat at their own self-paced rate, normally about 40 bpm. • At this heart rate, a patient may survive, but may not be able to function normally.
l In the case that the SA node fails to pace the heart properly, the ventricles may beat at their own self-paced rate, normally about 40 bpm. • At this heart rate, a patient may survive, but may not be able to function normally.
 l Because the pacemaker is batteryoperated and surgically implanted, battery lifetime is one of the most important considerations. • The lifetime is determined primarily by the stimulus requirements, as well as the current caused by the pacemaker circuitry.
l Because the pacemaker is batteryoperated and surgically implanted, battery lifetime is one of the most important considerations. • The lifetime is determined primarily by the stimulus requirements, as well as the current caused by the pacemaker circuitry.
 l The use of complementary metal-oxide semiconductor (CMOS) integrated circuits has dramatically reduced the current drain, but the stimulus requirements are determined by physiology and cannot be reduced effectively.
l The use of complementary metal-oxide semiconductor (CMOS) integrated circuits has dramatically reduced the current drain, but the stimulus requirements are determined by physiology and cannot be reduced effectively.
 l As is usually the case with physiological stimuli, there is a curve of stimulus intensity versus duration associated with the physiological response of heart depolarization.
l As is usually the case with physiological stimuli, there is a curve of stimulus intensity versus duration associated with the physiological response of heart depolarization.
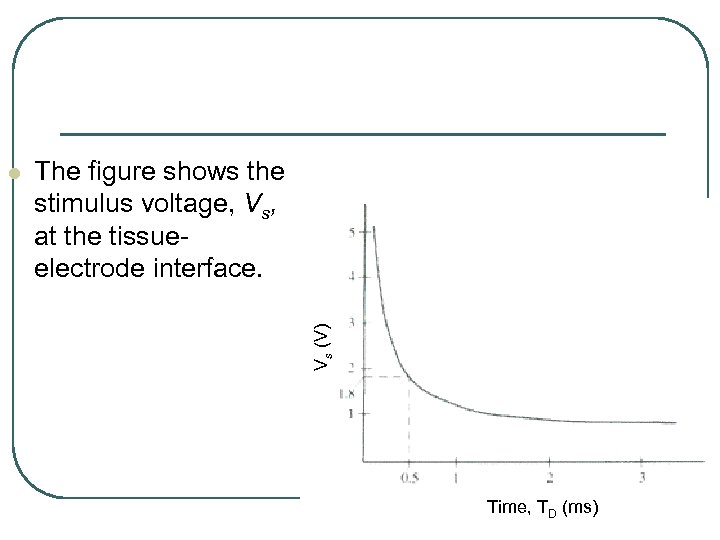 The figure shows the stimulus voltage, Vs, at the tissueelectrode interface. Vs (V) l Time, TD (ms)
The figure shows the stimulus voltage, Vs, at the tissueelectrode interface. Vs (V) l Time, TD (ms)
 l It has a stimulus duration TD, measured in milliseconds. • Such curves depend upon the electrode-heart resistance, RH, which may range from 100 to 1400 W.
l It has a stimulus duration TD, measured in milliseconds. • Such curves depend upon the electrode-heart resistance, RH, which may range from 100 to 1400 W.
 l The value of RH may change over time because of tissue scarring at the electrode-tissue interface. • In order to produce a stimulus pulse, it is necessary to deliver energy to the electrode with a pacemaker circuit.
l The value of RH may change over time because of tissue scarring at the electrode-tissue interface. • In order to produce a stimulus pulse, it is necessary to deliver energy to the electrode with a pacemaker circuit.
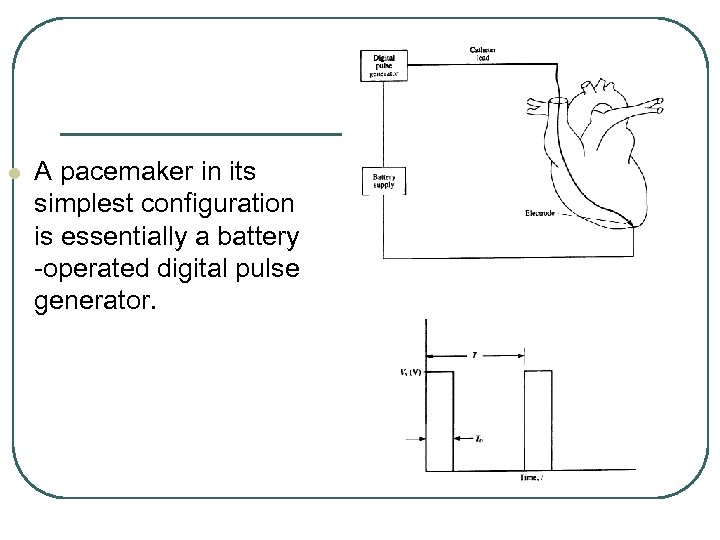 l A pacemaker in its simplest configuration is essentially a battery -operated digital pulse generator.
l A pacemaker in its simplest configuration is essentially a battery -operated digital pulse generator.
 l A digital pulse has a voltage Vs that may be made variable to allow adjustments in the energy, EP, delivered by the pacemaker to the heart during each pulse.
l A digital pulse has a voltage Vs that may be made variable to allow adjustments in the energy, EP, delivered by the pacemaker to the heart during each pulse.
 l During the pulse duration, TD , the stimulus voltage drives energy into the heart. • When the pulse is OFF, it causes an energy drain given by Vs. IDT, where T is the time period between successive pulses, and ID is the current drain on the battery when the pulse is OFF.
l During the pulse duration, TD , the stimulus voltage drives energy into the heart. • When the pulse is OFF, it causes an energy drain given by Vs. IDT, where T is the time period between successive pulses, and ID is the current drain on the battery when the pulse is OFF.
 l Therefore, the energy delivered by the pacemaker during each pulse is given as
l Therefore, the energy delivered by the pacemaker during each pulse is given as
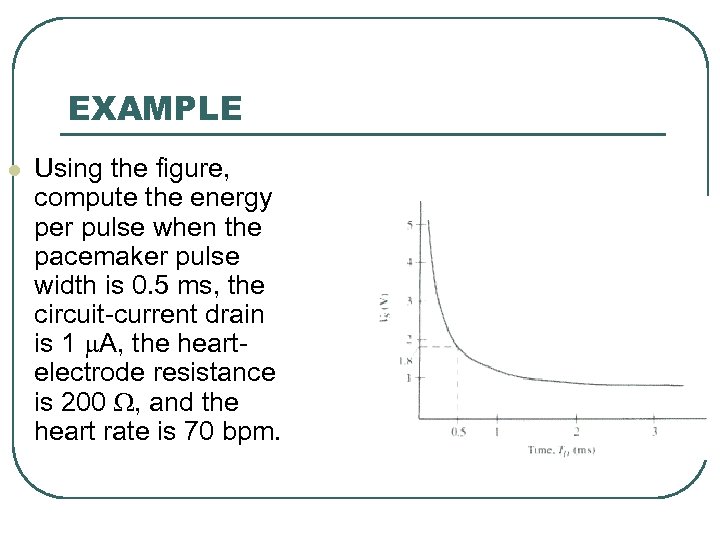 EXAMPLE l Using the figure, compute the energy per pulse when the pacemaker pulse width is 0. 5 ms, the circuit-current drain is 1 m. A, the heartelectrode resistance is 200 W, and the heart rate is 70 bpm.
EXAMPLE l Using the figure, compute the energy per pulse when the pacemaker pulse width is 0. 5 ms, the circuit-current drain is 1 m. A, the heartelectrode resistance is 200 W, and the heart rate is 70 bpm.
 SOLUTION l From the figure, Vs = 1. 8 V. Also, T = (60/70) s. Then, • Thus the energy used for each pulse is EP = 9. 643 m. J/pulse
SOLUTION l From the figure, Vs = 1. 8 V. Also, T = (60/70) s. Then, • Thus the energy used for each pulse is EP = 9. 643 m. J/pulse
 Pacemaker Batteries l Battery-operated equipment is convenient in many applications other than pacemakers because it can be used without a power cord, and it is safer because leakage currents are not usually present. • The disadvantage is that batteries are relatively large and of limited energy-storage capability. • Even so, the energy demand of the pacemaker is such that batteries with lifetimes between five and ten years are available.
Pacemaker Batteries l Battery-operated equipment is convenient in many applications other than pacemakers because it can be used without a power cord, and it is safer because leakage currents are not usually present. • The disadvantage is that batteries are relatively large and of limited energy-storage capability. • Even so, the energy demand of the pacemaker is such that batteries with lifetimes between five and ten years are available.
 l Mercury cells with two-year lifetimes, used in pacemakers in the past, have been made obsolete by lithium iodide cells which can last as long as 15 years before they need to be replaced. • Nuclear pacemaker batteries have been used to extend battery lifetimes to over 20 years, even for dual-chamber pacemakers that use higher amounts of battery power.
l Mercury cells with two-year lifetimes, used in pacemakers in the past, have been made obsolete by lithium iodide cells which can last as long as 15 years before they need to be replaced. • Nuclear pacemaker batteries have been used to extend battery lifetimes to over 20 years, even for dual-chamber pacemakers that use higher amounts of battery power.
 l Nuclear batteries pose an environmental hazard, however, because in an accident the radioactive material could be released into the environment. • Nuclear batteries are being considered for artificial implanted hearts also, because of the potential for high energy storage, but this research is only beginning.
l Nuclear batteries pose an environmental hazard, however, because in an accident the radioactive material could be released into the environment. • Nuclear batteries are being considered for artificial implanted hearts also, because of the potential for high energy storage, but this research is only beginning.
 l Rechargeable batteries are not widely used for low power pacemaker application, since their shelf life is no longer than that of a lithium iodide pacemaker battery in normal use.
l Rechargeable batteries are not widely used for low power pacemaker application, since their shelf life is no longer than that of a lithium iodide pacemaker battery in normal use.
 l The lifetime of a storage battery depends on both its ampere-hour (A-H) rating and its shelf life. • Shelf life is limited self-discharge of the battery due to internal leakage currents, particle migration, formation of insulating layers, and internal shorts.
l The lifetime of a storage battery depends on both its ampere-hour (A-H) rating and its shelf life. • Shelf life is limited self-discharge of the battery due to internal leakage currents, particle migration, formation of insulating layers, and internal shorts.
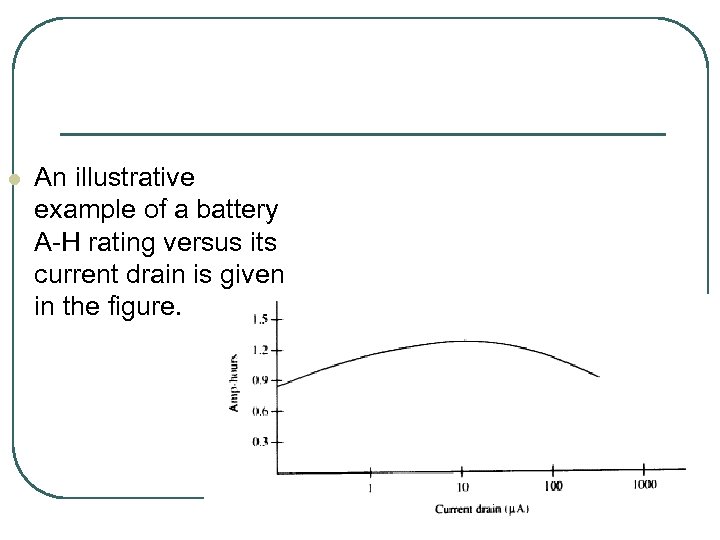 l An illustrative example of a battery A-H rating versus its current drain is given in the figure.
l An illustrative example of a battery A-H rating versus its current drain is given in the figure.
 l At high current drain, polarization of the metal electrolyte boundary increases the internal resistance of the battery and decreases the A-H rating.
l At high current drain, polarization of the metal electrolyte boundary increases the internal resistance of the battery and decreases the A-H rating.
 l Implantable batteries are usually encased in metal. • If they become too hot, such as when shorted, the case may rupture. • Pacemaker design should ensure that the case is strong enough to contain such a rupture and prevent toxic materials from entering the body of the patient.
l Implantable batteries are usually encased in metal. • If they become too hot, such as when shorted, the case may rupture. • Pacemaker design should ensure that the case is strong enough to contain such a rupture and prevent toxic materials from entering the body of the patient.
 Illustrative Pacemaker Characteristics l The pacemaker consists of three major components: • the lead wire, • the electronic pulsing circuit, and • the battery.
Illustrative Pacemaker Characteristics l The pacemaker consists of three major components: • the lead wire, • the electronic pulsing circuit, and • the battery.
 l The lead can cause a failure due to metal fatigue, introduced by the motion and beating of the heart. • To avoid such fatigue, the lead may be constructed by winding platinum ribbon around polyester yarn. • Each lead may have three such wires for redundancy.
l The lead can cause a failure due to metal fatigue, introduced by the motion and beating of the heart. • To avoid such fatigue, the lead may be constructed by winding platinum ribbon around polyester yarn. • Each lead may have three such wires for redundancy.
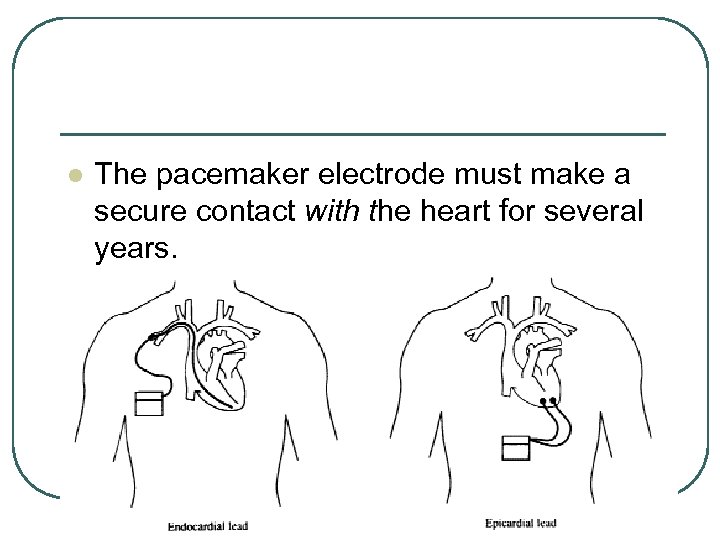 l The pacemaker electrode must make a secure contact with the heart for several years.
l The pacemaker electrode must make a secure contact with the heart for several years.
 l To ensure this, two methods of implantation are used under the following classifications: • (1) endocardial lead, in which the pacemaker • lead is inserted through a major vein through a catheter guide into the right ventricle of the heart; and (2) epicardial lead, in which the pacemaker electrode is sutured to the external wall of the heart during open-heart surgery, and a wire electrode is thereby secured into the tissue.
l To ensure this, two methods of implantation are used under the following classifications: • (1) endocardial lead, in which the pacemaker • lead is inserted through a major vein through a catheter guide into the right ventricle of the heart; and (2) epicardial lead, in which the pacemaker electrode is sutured to the external wall of the heart during open-heart surgery, and a wire electrode is thereby secured into the tissue.
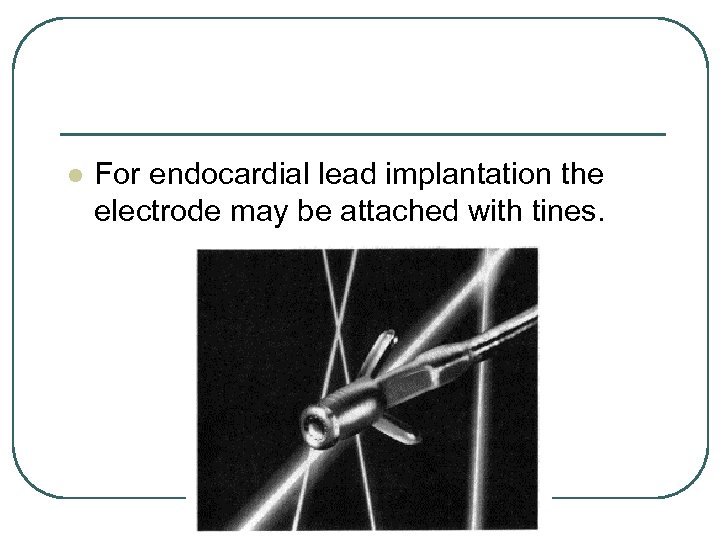 l For endocardial lead implantation the electrode may be attached with tines.
l For endocardial lead implantation the electrode may be attached with tines.
 l The tines are pushed into the Purkinje muscle fibers of the ventricle and latch themselves in place. • The porous electrode tip minimizes motion between the tip and the tissue so as to reduce the scar tissue buildup. • This tends to keep the contact resistance low.
l The tines are pushed into the Purkinje muscle fibers of the ventricle and latch themselves in place. • The porous electrode tip minimizes motion between the tip and the tissue so as to reduce the scar tissue buildup. • This tends to keep the contact resistance low.
 l The electrode may also be held in place with a helical wire that is screwed into the tissues with a twisting motion.
l The electrode may also be held in place with a helical wire that is screwed into the tissues with a twisting motion.
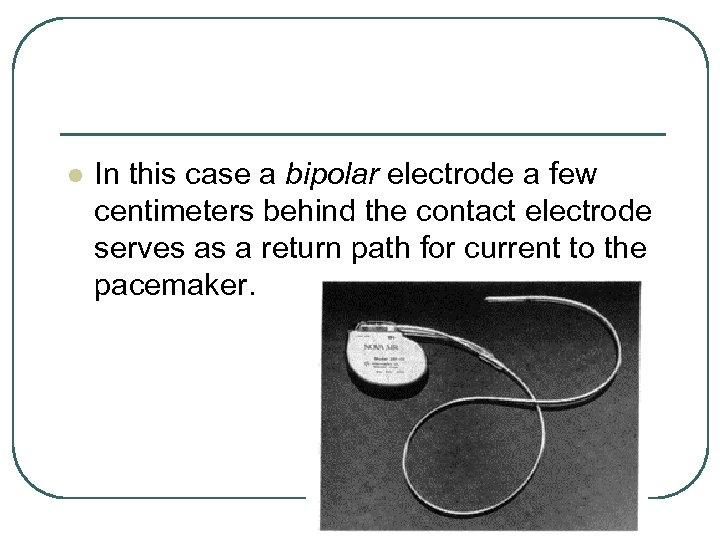 l In this case a bipolar electrode a few centimeters behind the contact electrode serves as a return path for current to the pacemaker.
l In this case a bipolar electrode a few centimeters behind the contact electrode serves as a return path for current to the pacemaker.
 l In the unipolar pacemaker lead, the second electrode is eliminated, and the return conductive path to the pacemaker is made through body fluids. • A unipolar lead electrode may also be held in place by either sutures, tines, or a helical wire.
l In the unipolar pacemaker lead, the second electrode is eliminated, and the return conductive path to the pacemaker is made through body fluids. • A unipolar lead electrode may also be held in place by either sutures, tines, or a helical wire.
 l The electrode-muscle contact can change after a time because of (1) polarization by ionic current flow; (2) tissue and scar growth; or (3) mechanical motion of the heart.
l The electrode-muscle contact can change after a time because of (1) polarization by ionic current flow; (2) tissue and scar growth; or (3) mechanical motion of the heart.
 l A symptom of such change may be an increased electrode impedance. • The problem may be fixed by increasing the pulse voltage from the pacemaker or by lengthening its duration. • Loss of contact altogether may require surgical reimplantation.
l A symptom of such change may be an increased electrode impedance. • The problem may be fixed by increasing the pulse voltage from the pacemaker or by lengthening its duration. • Loss of contact altogether may require surgical reimplantation.
 PROGRAMMABLE PACEMAKERS l The implantable pacemaker is presented as a battery-powered, digital pulse generator, and it may be considered an asynchronous type of unit. • Other types of pacemaker include the R-wave synchronous, R-wave inhibited, and P-wave synchronous pacemakers.
PROGRAMMABLE PACEMAKERS l The implantable pacemaker is presented as a battery-powered, digital pulse generator, and it may be considered an asynchronous type of unit. • Other types of pacemaker include the R-wave synchronous, R-wave inhibited, and P-wave synchronous pacemakers.
 l The asynchronous pacemaker produces a pulse at a preset rate, for example 70 bpm, and delivers pulses to the heart regardless of the heart’s natural beating tendency and independent of the QRS complex. • This pacemaker does not increase the heart rate in response to the body demand for more blood during exertion.
l The asynchronous pacemaker produces a pulse at a preset rate, for example 70 bpm, and delivers pulses to the heart regardless of the heart’s natural beating tendency and independent of the QRS complex. • This pacemaker does not increase the heart rate in response to the body demand for more blood during exertion.
 l However, a P-wave synchronous pacemaker does. • The SA node depolarization responds to body demands through the vagus nerve and hormones transported in the blood.
l However, a P-wave synchronous pacemaker does. • The SA node depolarization responds to body demands through the vagus nerve and hormones transported in the blood.
 l In a P-wave synchronous pacemaker, the SA node triggers the pacer, which in turn drives the ventricle. • It is used when the AV node is blocked because of disease.
l In a P-wave synchronous pacemaker, the SA node triggers the pacer, which in turn drives the ventricle. • It is used when the AV node is blocked because of disease.
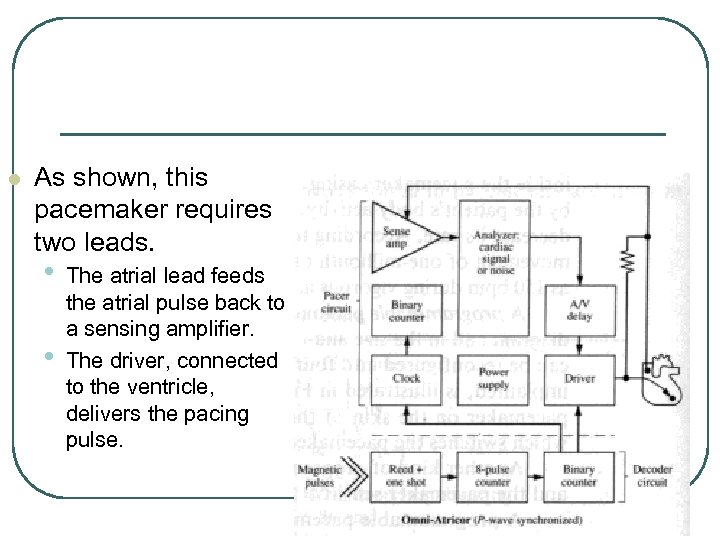 l As shown, this pacemaker requires two leads. • • The atrial lead feeds the atrial pulse back to a sensing amplifier. The driver, connected to the ventricle, delivers the pacing pulse.
l As shown, this pacemaker requires two leads. • • The atrial lead feeds the atrial pulse back to a sensing amplifier. The driver, connected to the ventricle, delivers the pacing pulse.
 l The R-wave inhibited pacemaker also allows the heart to pace at its normal rhythm when it is able to. • However, if the R-wave is missing for a preset period of time, the pacer will supply a stimulus.
l The R-wave inhibited pacemaker also allows the heart to pace at its normal rhythm when it is able to. • However, if the R-wave is missing for a preset period of time, the pacer will supply a stimulus.
 l Therefore, if the pulse rate falls below a predetermined minimum, the pacemaker will turn on and provide the heart a stimulus. • For this reason it is called a demand pacemaker.
l Therefore, if the pulse rate falls below a predetermined minimum, the pacemaker will turn on and provide the heart a stimulus. • For this reason it is called a demand pacemaker.
 l Another type of demand pacemaker uses a piezoelectric sensor shielded inside the pacemaker casing. • When this sensor is slightly stressed or bent by the patient’s body activity, the pacemaker will automatically increase or decrease its rate.
l Another type of demand pacemaker uses a piezoelectric sensor shielded inside the pacemaker casing. • When this sensor is slightly stressed or bent by the patient’s body activity, the pacemaker will automatically increase or decrease its rate.
 l According to Medtronic, Inc. , their model will react to a movement of one-millionth of an inch. • It will change heart rates to as high as 150 bpm during vigorous activity or as low as 60 bpm during rest periods.
l According to Medtronic, Inc. , their model will react to a movement of one-millionth of an inch. • It will change heart rates to as high as 150 bpm during vigorous activity or as low as 60 bpm during rest periods.
 l A programmable pacemaker is one that can be altered both in its block diagram and in the size and rate of the pulse it delivers.
l A programmable pacemaker is one that can be altered both in its block diagram and in the size and rate of the pulse it delivers.
 l A pacemaker that can be reconfigured into four different block diagrams, after having been implanted.
l A pacemaker that can be reconfigured into four different block diagrams, after having been implanted.
 l A magnet may be placed over the pacemaker on the skin of the patient in order to activate a reed switch, which switches the pacemaker into one of the four configurations shown. • Another kind of programming is done to alter the delivered stimulus and the pacemaker sensitivity to feedback signals.
l A magnet may be placed over the pacemaker on the skin of the patient in order to activate a reed switch, which switches the pacemaker into one of the four configurations shown. • Another kind of programming is done to alter the delivered stimulus and the pacemaker sensitivity to feedback signals.
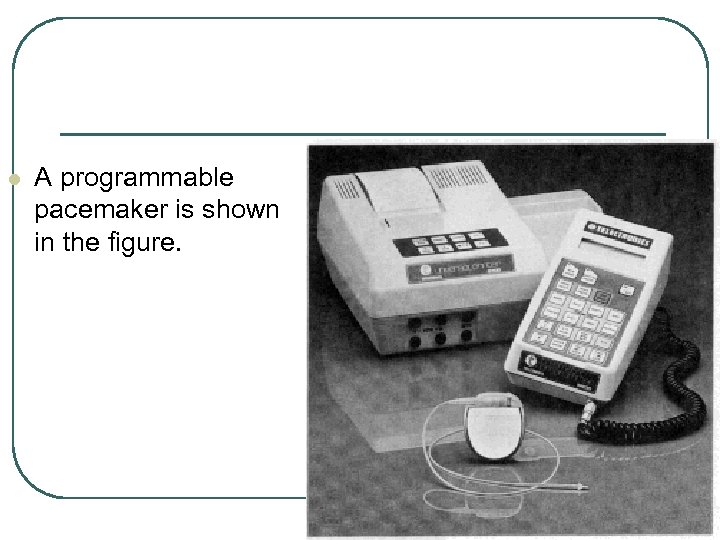 l A programmable pacemaker is shown in the figure.
l A programmable pacemaker is shown in the figure.
 l The telemetric programmer may be placed over the pacemaker to select pulse rates ranging from 30 to 155 bpm, feedback sensitivities from 0. 7 to 4. 5 V, pulse amplitudes from 2. 5 to 10 V, and pulse widths from 0. 25 to 1 ms, among other parameters.
l The telemetric programmer may be placed over the pacemaker to select pulse rates ranging from 30 to 155 bpm, feedback sensitivities from 0. 7 to 4. 5 V, pulse amplitudes from 2. 5 to 10 V, and pulse widths from 0. 25 to 1 ms, among other parameters.
 l A hard copy of the programming record is provided by the printer shown.
l A hard copy of the programming record is provided by the printer shown.
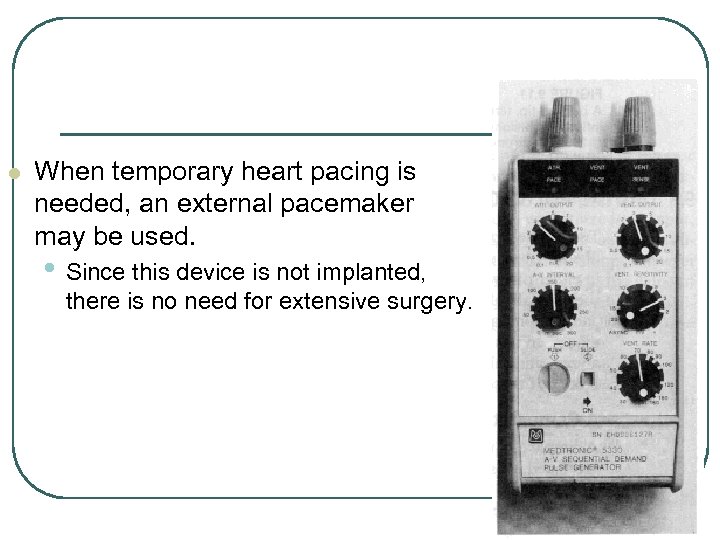 l When temporary heart pacing is needed, an external pacemaker may be used. • Since this device is not implanted, there is no need for extensive surgery.
l When temporary heart pacing is needed, an external pacemaker may be used. • Since this device is not implanted, there is no need for extensive surgery.
 l A temporary pacing lead uses a balloon tip, so that the flow of blood will carry the pacing electrode into the heart when the balloon is inflated.
l A temporary pacing lead uses a balloon tip, so that the flow of blood will carry the pacing electrode into the heart when the balloon is inflated.
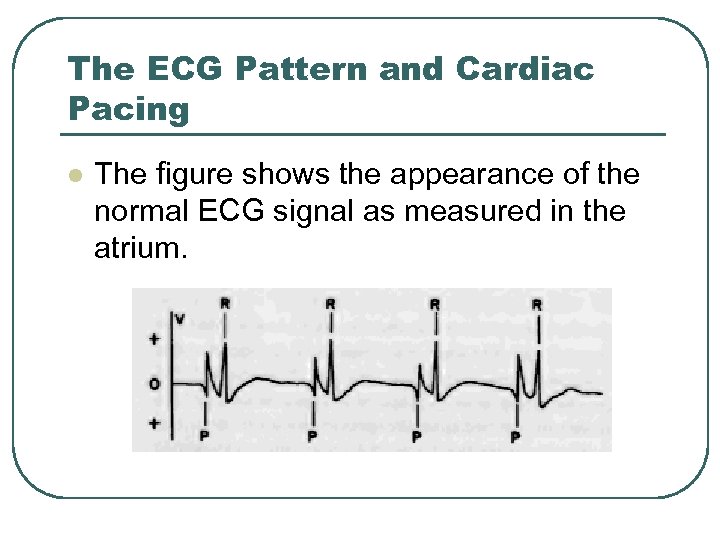 The ECG Pattern and Cardiac Pacing l The figure shows the appearance of the normal ECG signal as measured in the atrium.
The ECG Pattern and Cardiac Pacing l The figure shows the appearance of the normal ECG signal as measured in the atrium.
 l Notice the large P wave, which is almost as high as the normal QRS complex.
l Notice the large P wave, which is almost as high as the normal QRS complex.
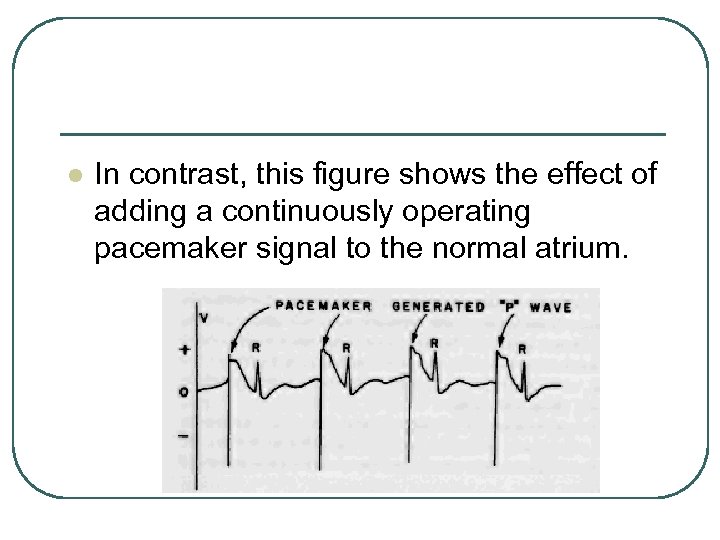 l In contrast, this figure shows the effect of adding a continuously operating pacemaker signal to the normal atrium.
l In contrast, this figure shows the effect of adding a continuously operating pacemaker signal to the normal atrium.
 l Now the heart is responding only to the pacemaker, and the pacemaker is said to have “captured” the heart rate. • Note that the QRS wave follows the pacemaker-generated P wave at a fixed interval, and that there are no beats generated sinoatrial (SA) node.
l Now the heart is responding only to the pacemaker, and the pacemaker is said to have “captured” the heart rate. • Note that the QRS wave follows the pacemaker-generated P wave at a fixed interval, and that there are no beats generated sinoatrial (SA) node.
 l The pacemaker signal is large enough and occurs at a high enough rate to keep the SA node in the depolarized condition so that it cannot fire. • This is important, because an occasional, ectopic, SA-node beat would be entirely out of synchronization with the regularly occurring pacemaker beat.
l The pacemaker signal is large enough and occurs at a high enough rate to keep the SA node in the depolarized condition so that it cannot fire. • This is important, because an occasional, ectopic, SA-node beat would be entirely out of synchronization with the regularly occurring pacemaker beat.
 l Eventually, a pacemaker-induced pulse would occur during the latter part of the QRS complex or during the T wave from the ectopic SA-node beat, and this would be trouble. • It turns out that disease-weakened hearts are more sensitive than healthy hearts to any signal that arrive during the latter part of the QRS complex or the T wave, and such a weakened heart will go into fibrillation if a pacemaker beat and either of these signals happen to coincide.
l Eventually, a pacemaker-induced pulse would occur during the latter part of the QRS complex or during the T wave from the ectopic SA-node beat, and this would be trouble. • It turns out that disease-weakened hearts are more sensitive than healthy hearts to any signal that arrive during the latter part of the QRS complex or the T wave, and such a weakened heart will go into fibrillation if a pacemaker beat and either of these signals happen to coincide.
 l To avoid this hazard, the pacemaker signal is set large enough to preclude the occurrence of any inadvertent SA-node beats.
l To avoid this hazard, the pacemaker signal is set large enough to preclude the occurrence of any inadvertent SA-node beats.
 l The above mode of pacemaker operation was always used when pacemakers were first invented, and it is still used if the P or QRS waves are weak, very irregular, or entirely absent. • This mode has its problems in that no adjustment can be made for the normal change in heart rate from resting to exercise.
l The above mode of pacemaker operation was always used when pacemakers were first invented, and it is still used if the P or QRS waves are weak, very irregular, or entirely absent. • This mode has its problems in that no adjustment can be made for the normal change in heart rate from resting to exercise.
 l Usually a rate of 70 heats per minute is used as a compromise. • The requirement for continuous operation is reflected in reduced battery life, and the pacemaker has to be changed more often.
l Usually a rate of 70 heats per minute is used as a compromise. • The requirement for continuous operation is reflected in reduced battery life, and the pacemaker has to be changed more often.
 l If a patient has a more nearly normal heart, there may be no need for continuous pacing, and the unit is set in the “demand” mode. • In this mode, the pacemaker detects the peak of the QRS wave and begins “counting. ”
l If a patient has a more nearly normal heart, there may be no need for continuous pacing, and the unit is set in the “demand” mode. • In this mode, the pacemaker detects the peak of the QRS wave and begins “counting. ”
 l If the next QRS wave occurs within what is called the “capture interval, ” the pacemaker does nothing. • If the QRS wave is late or absent, the pacemaker stimulates the heart. • Here again, the locus of can be in the atrium or in the right ventricle, as necessary.
l If the next QRS wave occurs within what is called the “capture interval, ” the pacemaker does nothing. • If the QRS wave is late or absent, the pacemaker stimulates the heart. • Here again, the locus of can be in the atrium or in the right ventricle, as necessary.
 l If the QRS wave stops entirely, the pacemaker will stimulate the heart at about 70 beats per minute; • One might say that it switches from the “demand” mode to the “continuous” mode.
l If the QRS wave stops entirely, the pacemaker will stimulate the heart at about 70 beats per minute; • One might say that it switches from the “demand” mode to the “continuous” mode.
 l Demand operation results in longer battery life and allows the patient to benefit from the normal heart-rate control system that adjusts the beat to the demands of the body. • The pacemaker is available for action if and when the patient’s own heart-rate control system should fail.
l Demand operation results in longer battery life and allows the patient to benefit from the normal heart-rate control system that adjusts the beat to the demands of the body. • The pacemaker is available for action if and when the patient’s own heart-rate control system should fail.


