2ee1b7a56369288fdfac8a94c2c030af.ppt
- Количество слайдов: 46
ENT for General Practice George Vattakuzhiyil MBBS; MS(ENT); FRCS
Objectives l Detailed examination of ENT/H&N l Learn to diagnose & treat common ENT pathology l Recognise serious complication, request additional tests, specialty referral
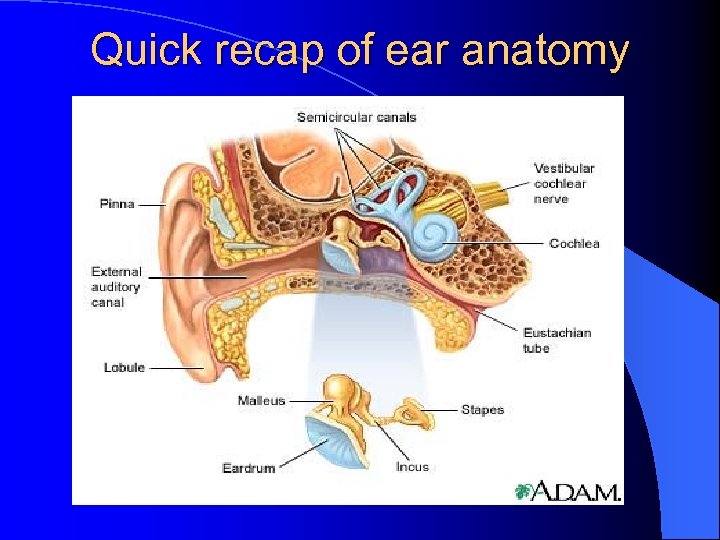
Quick recap of ear anatomy
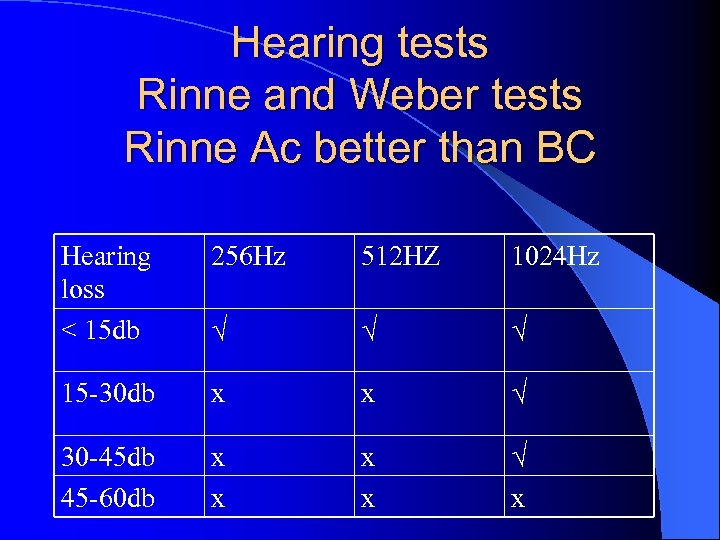
Hearing tests Rinne and Weber tests Rinne Ac better than BC Hearing loss < 15 db 256 Hz 512 HZ 1024 Hz 15 -30 db x x 30 -45 db 45 -60 db x x x
Weber test l Hold the base of the tuning fork in the midline (forehead, incisor teeth) l Laterelising to the left: conductive loss on left or SNHL on right
Otitis Externa l l l Inflammatory disorder of skin lined EAC Acute/Chronic Generelised skin disorder Pathogens: staph, pseudomonas, Fungus Topical antibiotic/steroid Sofradex, otomize spray, otosporin, GHC, locorten- vioform
Otitis externa l Extension to pre/post auricular area l Microsuction/IV antibiotics l Diabetic patient/ Pseudomonas inf l ? Malignant otitis externa
Acute otitis media l l l Common in children otalgia/discharge Unwell/pyrexia TM: red, bulging, oedematous Streptococcus/Haemo philus Amoxycillin 5 -7 days
complications Acute mastoiditis l Chronic otitis media l Intracranial complications l
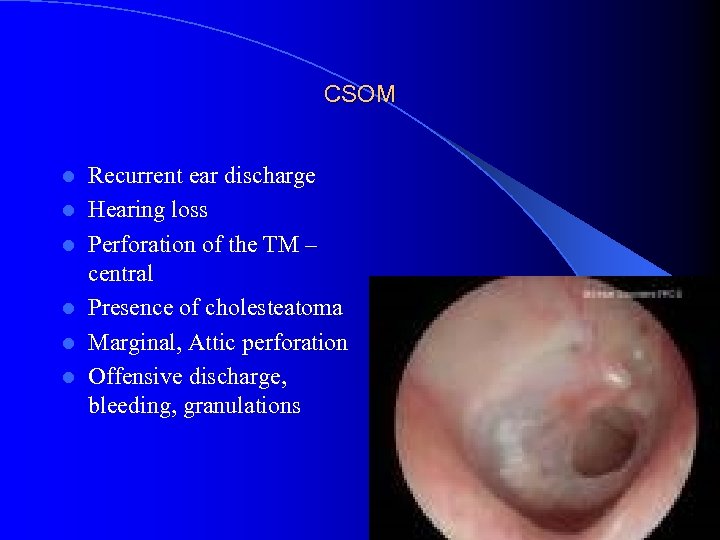
CSOM l l l Recurrent ear discharge Hearing loss Perforation of the TM – central Presence of cholesteatoma Marginal, Attic perforation Offensive discharge, bleeding, granulations
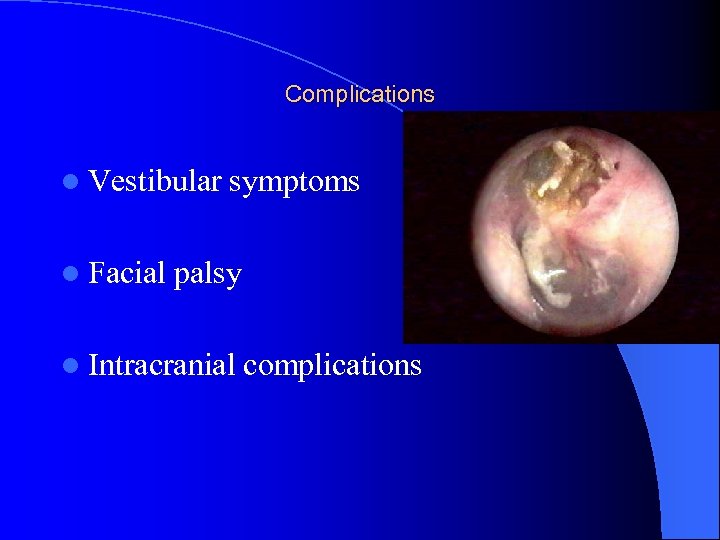
Complications l Vestibular l Facial symptoms palsy l Intracranial complications

Management l Medical: Dry mopping, suction clearance, / Ear drops, rarely systemic antibiotics l Surgical l Myringoplasty/ Tympanoplasty l Combined Mastoidectomy/Tympanoplasty
Otitis media+effusion-Glue ear l Common in children l Reduced hearing noticed by parents/teacher l Recurrent ear infection l Unsteadiness- child falling over l Effusions persist for weeks after AOM l 80% clear at 8 weeks
Signs of OME l Dull retracted TM l May show air-fluid level l Conductive hearing loss(whisper test, Rinne/weber tests) l OME persistant over 3 months ENT referral
Treatment l l l Failed audio Flat tympanograms h/o >3 episodes in 6/12 or >4 in 12/12 Grommet insertion Evaluate adenoids, especially in recurrent grommet insertions
Syringing the ear Which ear needs syringing?

Occlusive cerumen Causing pain l Hearing loss l Tinnitus l
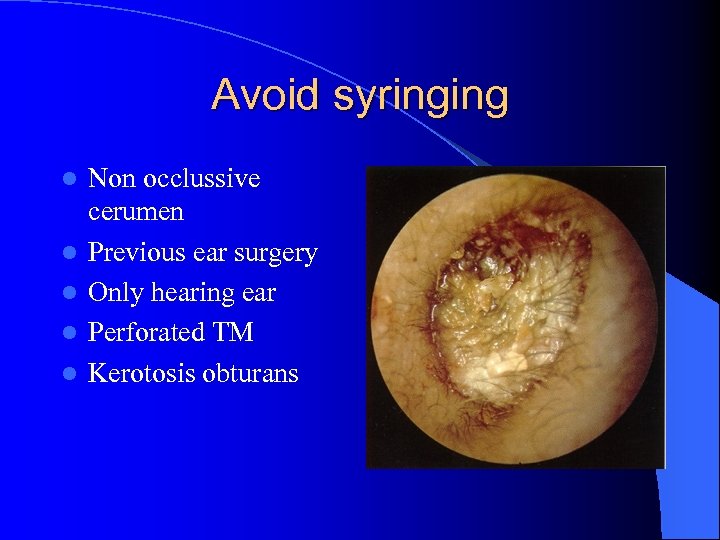
Avoid syringing l l l Non occlussive cerumen Previous ear surgery Only hearing ear Perforated TM Kerotosis obturans
Acute/Chronic tonsillitis l Sorethroat, fever, malaise l Tender cervical lymph nodes l Enlarged congested tonsils with pus l Analgesia l Penicillin l Prolonged course, worsening symptoms consider glandular fever
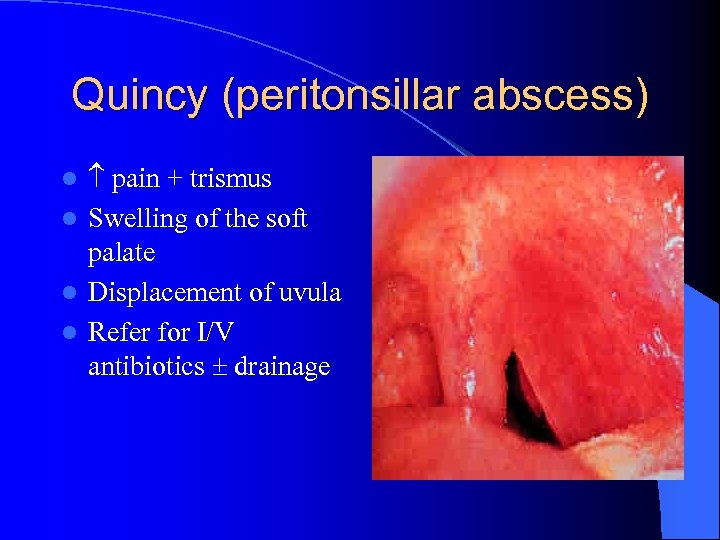
Quincy (peritonsillar abscess) pain + trismus l Swelling of the soft palate l Displacement of uvula l Refer for I/V antibiotics drainage l
Allergic rhinitis l Seasonal : allergen usually outdoor l perennial: indoor dust, mite, cat dander l O/E pale mucosa, boggy turbinate l Avoid allergen, antihistamines, topical vasoconstrictors, steroids l Surgery- SMD, laser, Turbinectomy
sinusitis l Facial pain/ pressure/ fullness l Nasal obstruction/ discharge l Altered smell l Pyrexia in acute sinusitis l Headache, halitosis, dental pain l Minor factors: cough, ear pressure, fatigue
sinusitis l Acute sinusitis < 4/52 l Chronic >4/52 or 4 or more episodes l O/E nasal congestion, polyps, pus in MM l Structural changes: DNS, concha bullosa
sinusitis l Sinus X ray usually unhelpful l CT sinuses l Acute: amoxicillin clavulonate, oxymetazoline l Chronic: Pus c/s, augmentin+metronidazole, Treat the cause: allergy, surgery(FESS)
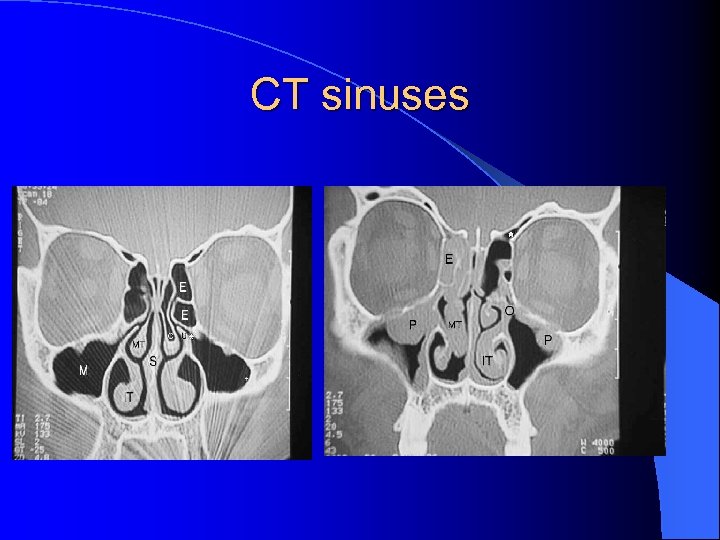
CT sinuses
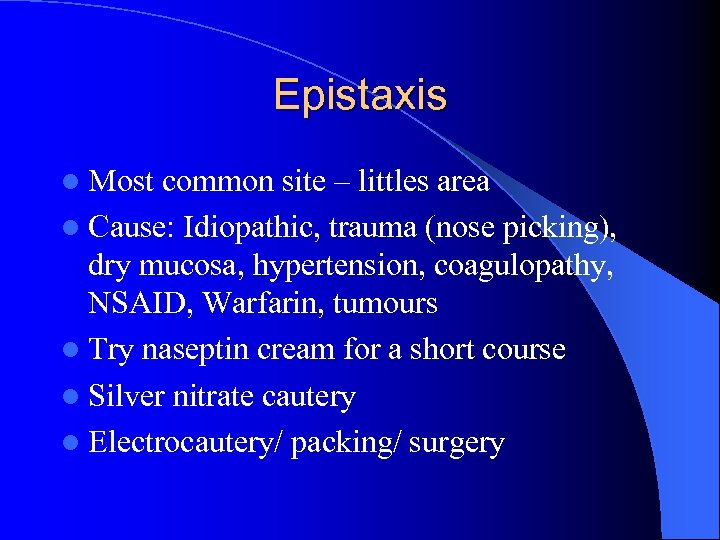
Epistaxis l Most common site – littles area l Cause: Idiopathic, trauma (nose picking), dry mucosa, hypertension, coagulopathy, NSAID, Warfarin, tumours l Try naseptin cream for a short course l Silver nitrate cautery l Electrocautery/ packing/ surgery
Common Pathology Viral laryngitis Viral URTI preceding aphonia § Hx sorethroat § B/L V. c. oedema/erythema § voice rest, antibiotics §
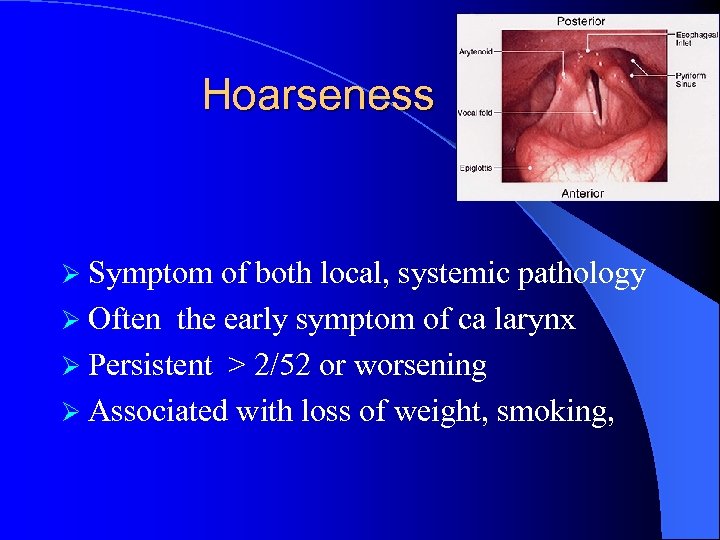
Hoarseness Ø Symptom of both local, systemic pathology Ø Often the early symptom of ca larynx Ø Persistent > 2/52 or worsening Ø Associated with loss of weight, smoking,
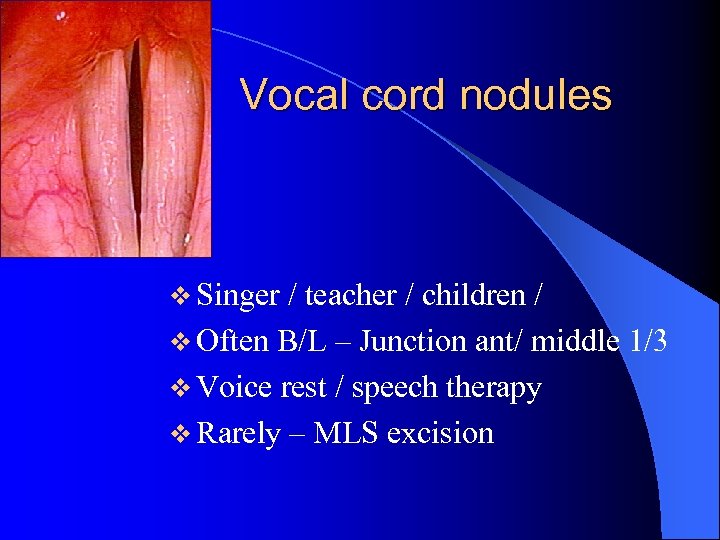
Vocal cord nodules v Singer / teacher / children / v Often B/L – Junction ant/ middle 1/3 v Voice rest / speech therapy v Rarely – MLS excision

Laryngitis - GORD l Hx of GORD l Inflammation of Post larynx l Treatment for reflux l Raising head end of cot
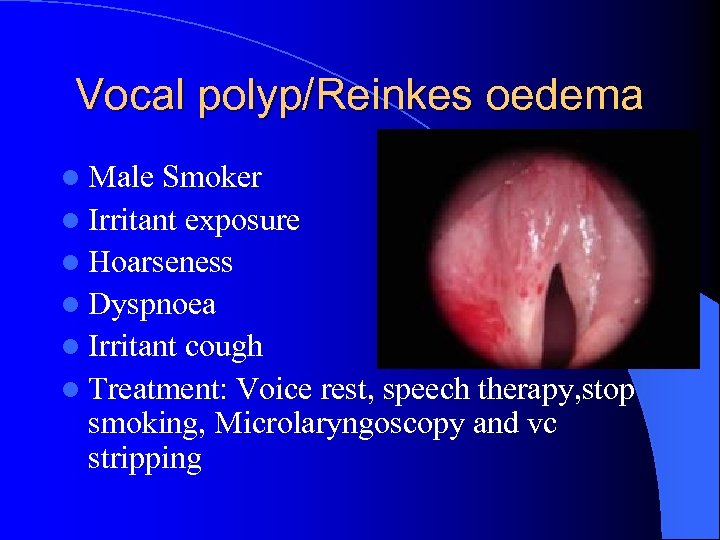
Vocal polyp/Reinkes oedema l Male Smoker l Irritant exposure l Hoarseness l Dyspnoea l Irritant cough l Treatment: Voice rest, speech therapy, stop smoking, Microlaryngoscopy and vc stripping
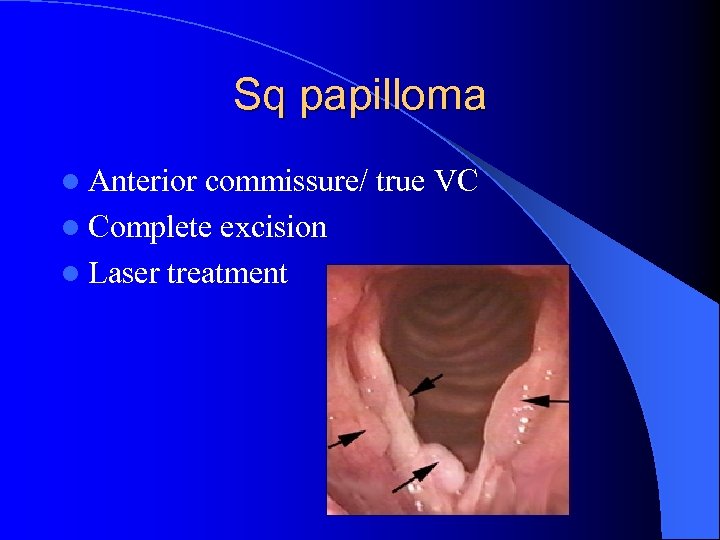
Sq papilloma l Anterior commissure/ true VC l Complete excision l Laser treatment

Laryngeal Malignancy l Risk factors l Smoking l Alcohol l Radiation exposure l HPV l Nickel exposure
Symptoms l Hoareseness associated with l Dysphagia l Odynophagia l Otalgia l Haemoptysis
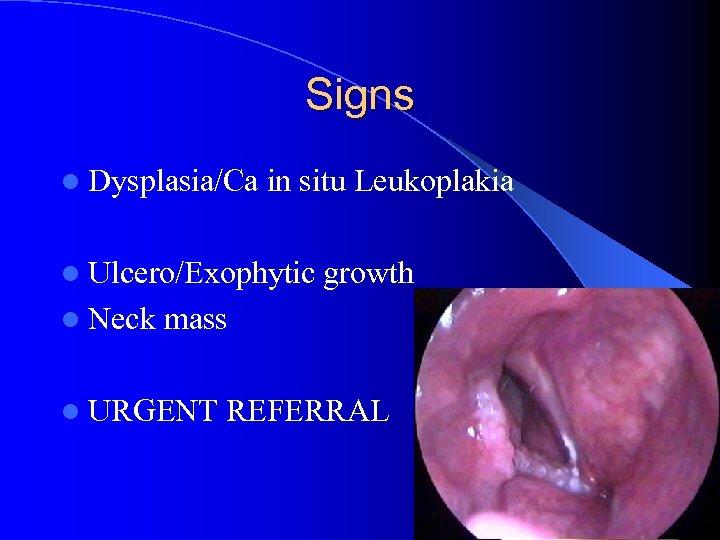
Signs l Dysplasia/Ca in situ Leukoplakia l Ulcero/Exophytic l Neck growth mass l URGENT REFERRAL
Cord paralysis l Breathy voice (air escape) l B/L airway compromise l P/H of thyroid, cardiovascular Sx l Cord in paramedian position l Refer for investigations and treatment
Functional aphonia l Psychogenic Only able to speak in forced whisper l Normal cough l Spastic dysphonia strained/strangled voice l Onset related to major life stress l Hyperadduction of true/false cord l Speech therapy, ? Botulinum toxin inj
Dysphagia l Progressive dysphagia for solids structural lesion l Dysphagia for liquids Neurological l Painful swallow spasm of cricopharynx, ulcer l Signs of reflux l Signs of aspiration
Examination-key points l Oral cavity Tongue, gag reflex, soft palate l Pharynx pooling, lesions l larynx Elevation of larynx, scopy l Neck masses

Investigations l Ba meal l Video fluroscopy l Oesophagoscopy l Imaging CT/MRI
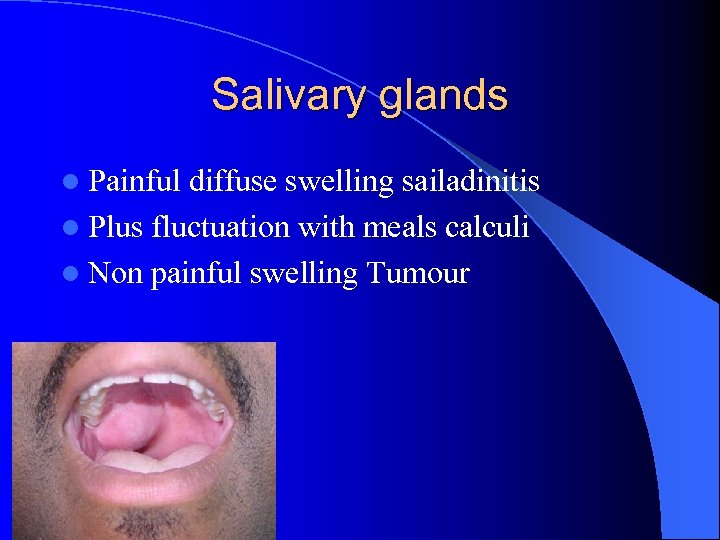
Salivary glands l Painful diffuse swelling sailadinitis l Plus fluctuation with meals calculi l Non painful swelling Tumour
Examination l l l Unilateral/bilateral ? Diffuse/well circumscribed? Is it tender? Any discharge from the ducts? Enlarged nodes? Palpable calculi?
Investigations Plain X-ray lateral view l FNAC l CT scan l Sialogram l
Tinnitus l SNHL l Drugs-NSAID, Aminoglycosides, Antidepressants l Tumors- Acoustic neuroma, Temporal lobe tumor l Anxiety/ Depression
Tinnitus l If unilateral refer: MRI l Serology: FTA l Haematocrit l Lipids l Audiogram/ ABR l Consider hearing therapy referral councilling/ tinnitus masker

2ee1b7a56369288fdfac8a94c2c030af.ppt