753d873f77acddf47e8bc04b612dbd61.ppt
- Количество слайдов: 81
Endovascular Management of Aneurysms and Subarachnoid Hemorrhages Lorri Mc. Court-O’Donnell RN, MSN, ACNP, CNRN Advance Practice Nurse Endovascular Neurosurgery/Interventional Neuroradiology Advocate Neurovascular Center March 14, 2015
Disclosures/Thanks • Nothing to disclose • My family for letting me do what I do • The physicians I am privileged to work with • My chauffer for getting me here safely : ) • The Northern Illinois Chapter of AANN
Objectives: • Differentiate treatment for Ruptured and Un-Ruptured Aneurysms • Cerebral circulation and common places for aneurysm development • Epidemiology and risk factors, Morbidity and Mortality • Clinical presentation/diagnostic testing • Nursing care pre/postoperative – Ruptured aneurysm a. SAH – Non ruptured aneurysm • Treatment options • Commonly used grading scales • a. SAH complications
What is Endovascular Neurosurgery? • Treat diseases and pathology involving the vessels of the head, neck and spine using minimally invasive technology • AKA – Interventional Neuroradiology – Interventional Neurovascular – Plus many more…
Disease Treated • Aneurysm – Ruptured – Non ruptured • • Acute Ischemic Stroke AVMs, Dural fistulas, Vein of Galen Carotid and Intracranial stenosis Tumor and epistaxis embolization
• Bi-Plane – real time images – Performed in IR • Conscious Sedation, MAC or General Anesthesia • Femoral Artery Catheterized – 6 French – Catheters and wires are navigated through the anatomy – Right groin access • Interventions performed if indicated – Purely diagnostic • Groin sealed with closure device and or manual pressure
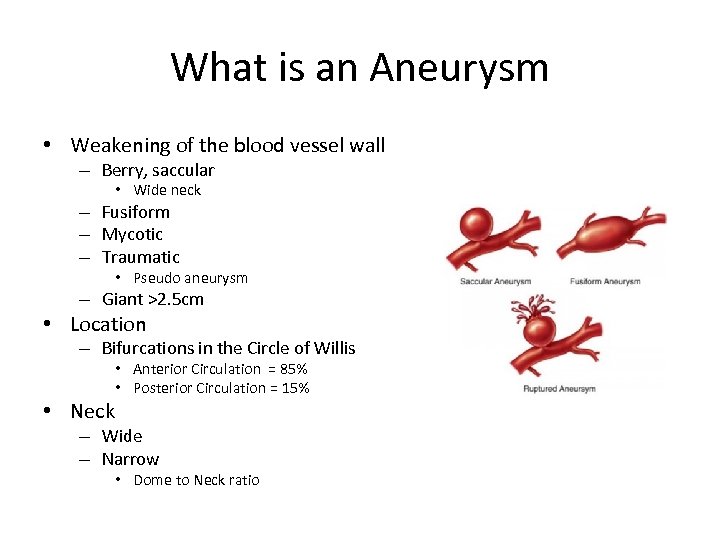
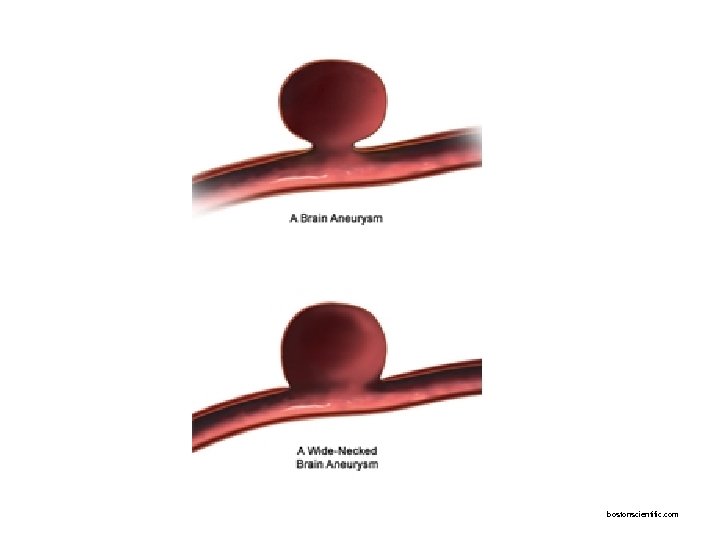
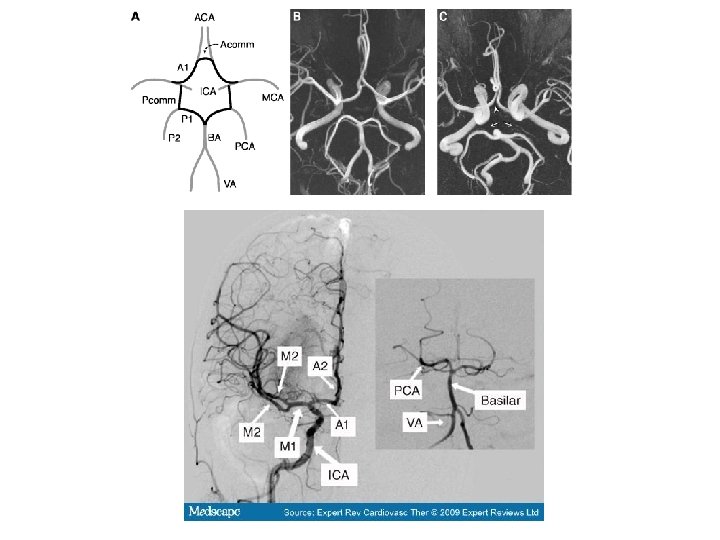
What is an Aneurysm • Weakening of the blood vessel wall – Berry, saccular • Wide neck – Fusiform – Mycotic – Traumatic • Pseudo aneurysm – Giant >2. 5 cm • Location – Bifurcations in the Circle of Willis • Neck • Anterior Circulation = 85% • Posterior Circulation = 15% – Wide – Narrow • Dome to Neck ratio
bostonscientific. com
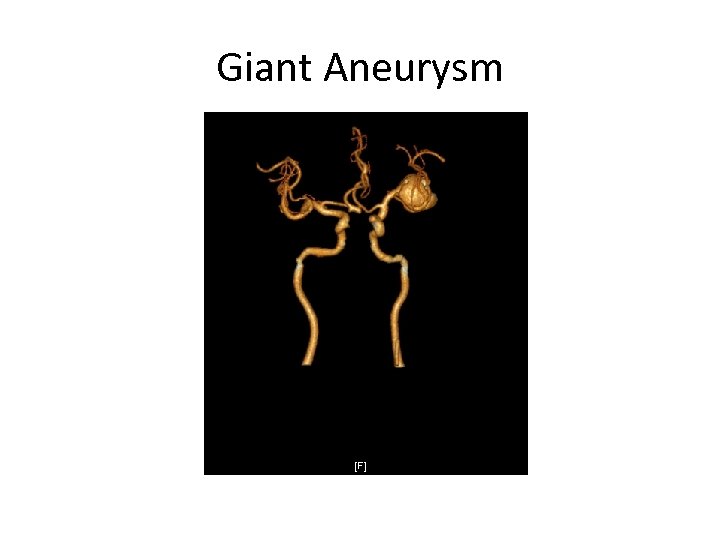
Giant Aneurysm
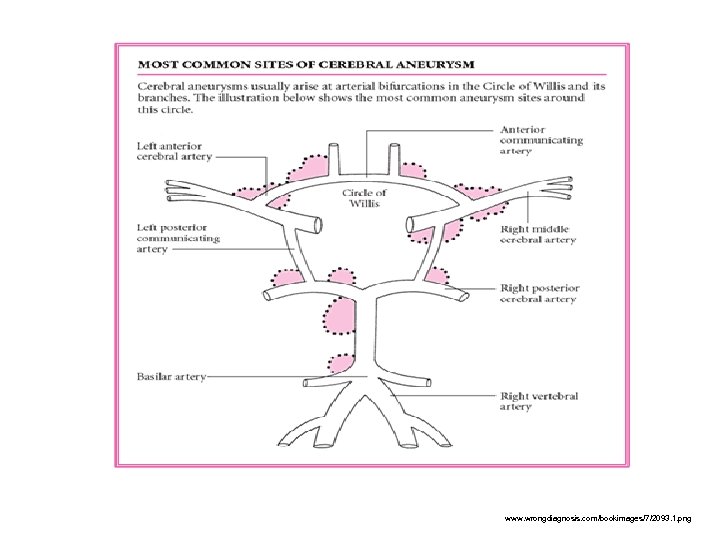
www. wrongdiagnosis. com/bookimages/7/2093. 1. png
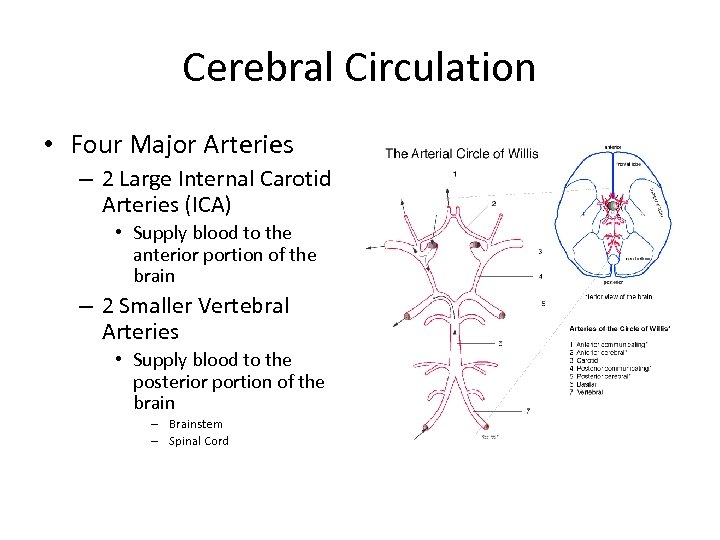
Cerebral Circulation • Four Major Arteries – 2 Large Internal Carotid Arteries (ICA) • Supply blood to the anterior portion of the brain – 2 Smaller Vertebral Arteries • Supply blood to the posterior portion of the brain – Brainstem – Spinal Cord
Epidemiology: • Aneurysms (unruptured) – 5% of US population = 10 -15 million individuals – Brain Aneurysm Foundation • 1: 50 Individuals – 20 -30% have multiple aneurysms • Risk of rupture related to size – 0. 05% risk for <10 mm and no prior a. SAH – 1% risk per year >10 mm – Most aneurysms at time of rupture 4 -7 mm • Risk of rupture is 1 -2% per year
Aneurysmal Subarachnoid Hemorrhage (a. SAH) • 6 -12 cases per 100, 000 – 15, 000 to 30, 000 persons per year – Mean age 55 (40 -60) – Risk of rupture is positively correlated with: • • Aneurysm size Hypertension Smoking Illicit drug use – Cocaine

Risk Factors • a. SAH – – – – Smoking Hypertension Increasing age Alcohol Illicit Drugs AA>Caucasians Females>Males 2 -3: 1 Genetic • Polycystic kidney diseases • Connective tissue diseases • Family history – 1 st degree relative
Morbidity and Mortality • 10 -15% die before reaching the hospital – Overall mortality at 6 months • 40 -50% • Of those who arrive to the hospital – 25% die within 24 hours • Re bleeding is catastrophic – Mortality of 48 -75% • 1/3 of survivors have functional independent lives • Improving outcomes – Being admitted to a Major Medical Center – Interventional Neuroradiology within 7 hours of presentation/bleed
Clinical Picture • Symptoms begin abruptly – ‘Worst headache of life’, ‘Thunderclap’ – 30% lateralized to side of aneurysm – Maybe associated with • • LOC – brief Seizure Nausea, Vomiting Meningeal signs • Sentinel Bleed 10 -43% – 30 -50% minor hemorrhage – a. SAH occur within 6 -20 days
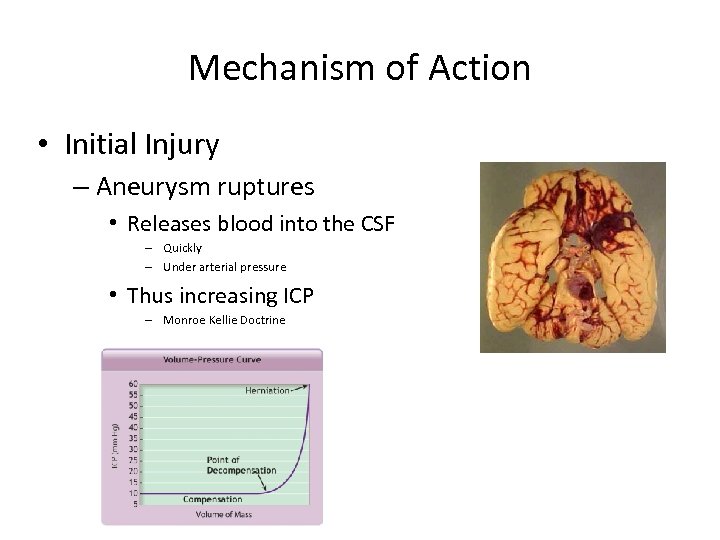
Mechanism of Action • Initial Injury – Aneurysm ruptures • Releases blood into the CSF – Quickly – Under arterial pressure • Thus increasing ICP – Monroe Kellie Doctrine
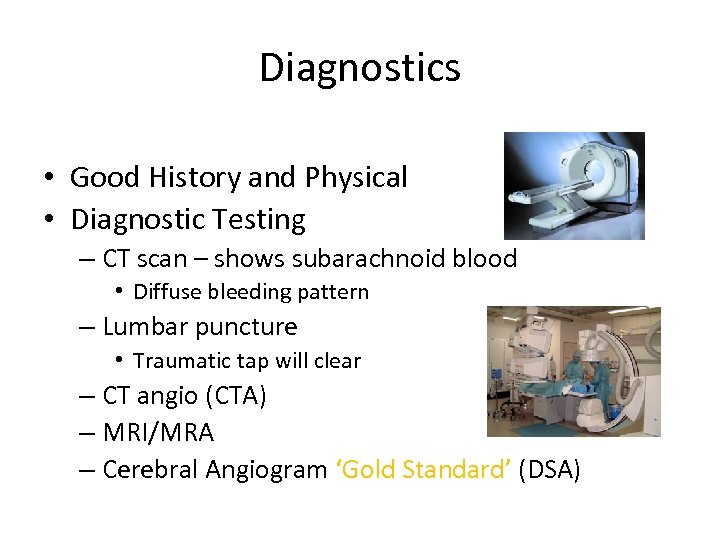
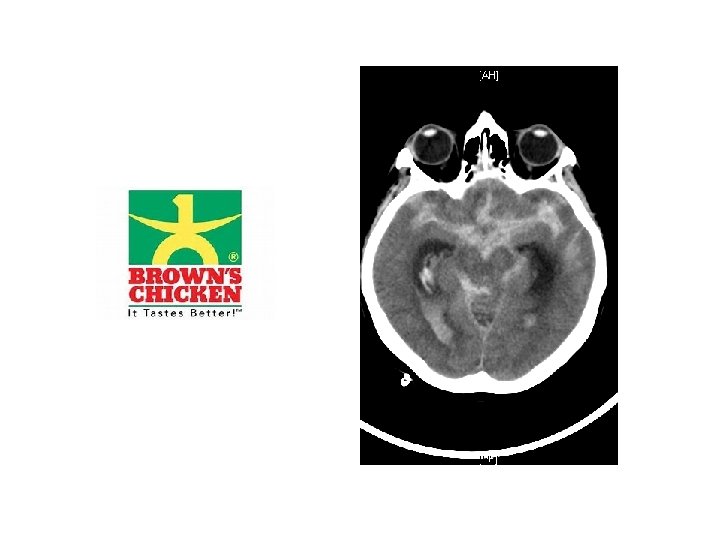
Diagnostics • Good History and Physical • Diagnostic Testing – CT scan – shows subarachnoid blood • Diffuse bleeding pattern – Lumbar puncture • Traumatic tap will clear – CT angio (CTA) – MRI/MRA – Cerebral Angiogram ‘Gold Standard’ (DSA)
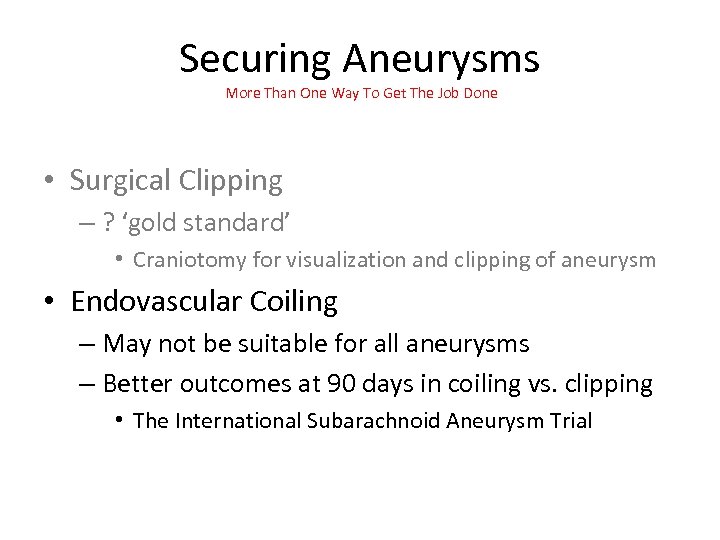
Securing Aneurysms More Than One Way To Get The Job Done • Surgical Clipping – ? ‘gold standard’ • Craniotomy for visualization and clipping of aneurysm • Endovascular Coiling – May not be suitable for all aneurysms – Better outcomes at 90 days in coiling vs. clipping • The International Subarachnoid Aneurysm Trial
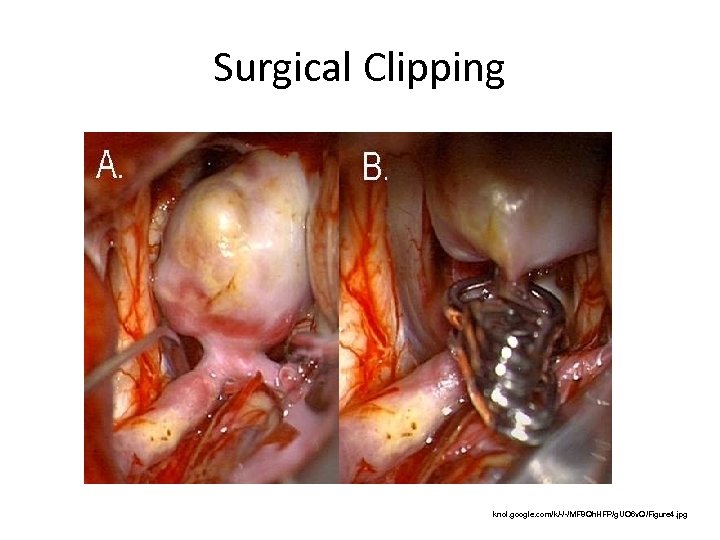
Surgical Clipping knol. google. com/k/-/-/MF 8 Qh. HFP/g. UO 6 v. Q/Figure 4. jpg
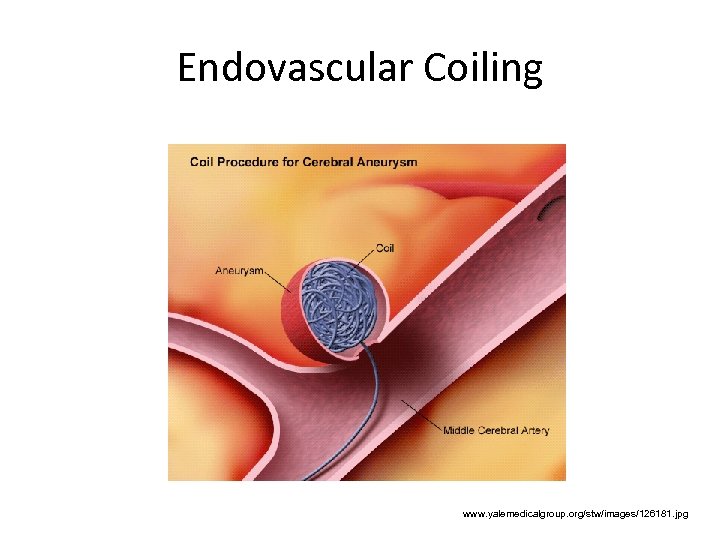
Endovascular Coiling www. yalemedicalgroup. org/stw/images/126181. jpg
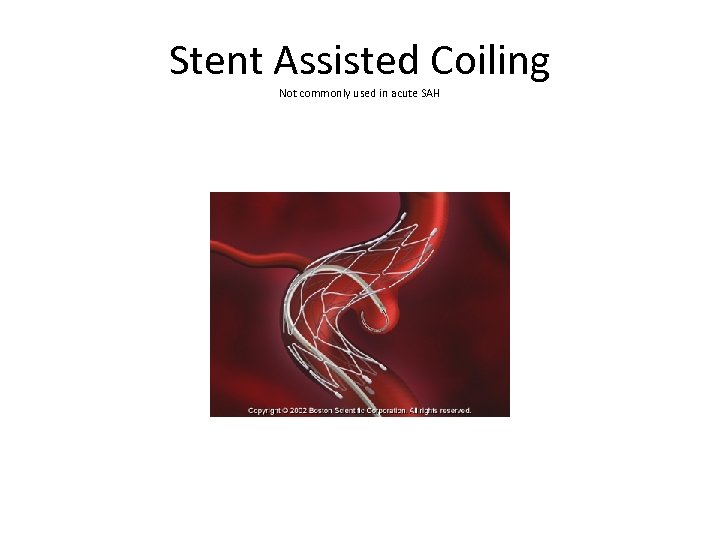
Stent Assisted Coiling Not commonly used in acute SAH
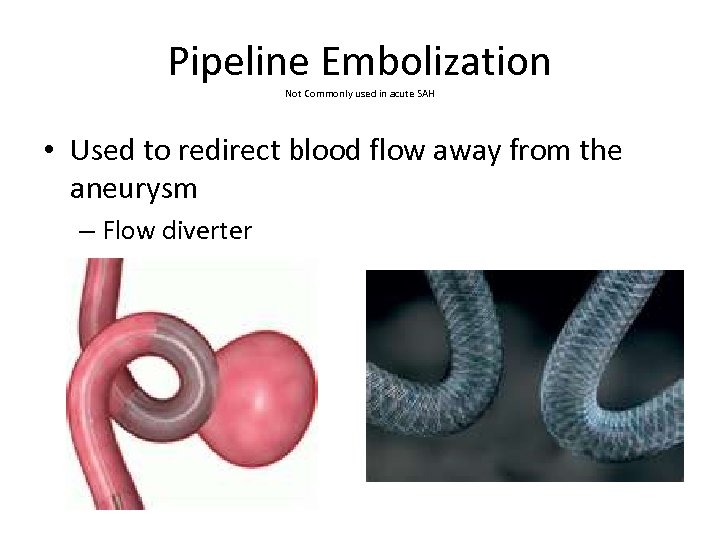
Pipeline Embolization Not Commonly used in acute SAH • Used to redirect blood flow away from the aneurysm – Flow diverter
Nursing care preoperative • ABCs • Neuro Checks • BP management – Systolic between 90 -140 mmhg – AVOID Hypotension • ICP Monitoring – EVD if indicated • Labs – CMP, CBC, Cardiac Enzymes, Coags, T&C, ABGs if intubated, 12 lead EKG, Chest X-Ray
Preoperative Care • NPO • IVF – Maintain euvolemia – 0. 9 NS at 80 -100 ml per hour • Activity – quiet environment, limit visitors • DVT – No anticoagulation until aneurysm securement – Teds, SCDs
Medications • Nimodipine 60 mg Q 4 hrs • Seizure prophylaxis – Phenytoin load 1000 mg then 100 mg Q 8 hrs – 10 -20% of a. SAH have seizures? ? – Side effects of Phenytoin • • Pain Management Antiemetics GI Protection Stool Softeners
Nursing Care Postoperative • ABCs • Frequent Neuro exam Q 1 hr – Or as exams dictate • HOB 30 degrees, neck midline • Reduce stimulation, quiet, dark room – Headaches continue, until blood clears CSF • BP Management – DO NOT TREAT BLOOD PRESSURE ONCE ANEURYSM IS SECURE • Maintain perfusion to the brain • Allow BP to be 200 mmhg systolic • CPP to be >60 to 70 mm. Hg • Fever management • Daily Labs – Electrolytes, CBC, Cardiac Enzymes (1 st 5 days), ABGs, Chest X-Ray, Anticonvulsant levels – Consider baseline 2 D-Echo
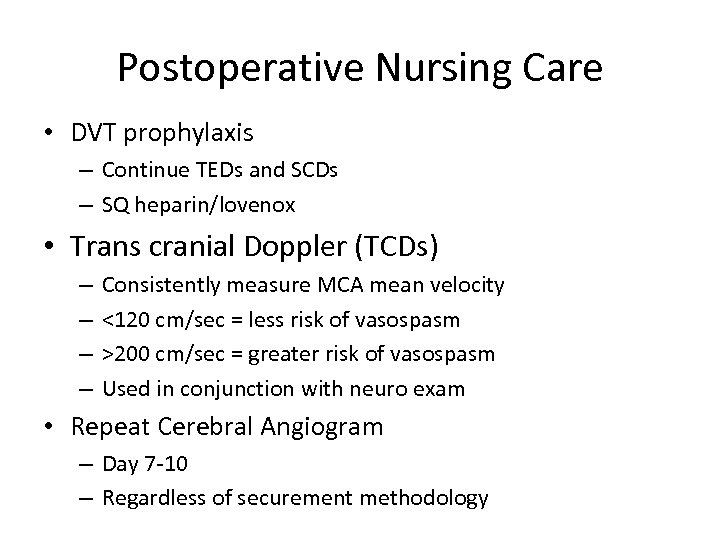
Postoperative Nursing Care • DVT prophylaxis – Continue TEDs and SCDs – SQ heparin/lovenox • Trans cranial Doppler (TCDs) – – Consistently measure MCA mean velocity <120 cm/sec = less risk of vasospasm >200 cm/sec = greater risk of vasospasm Used in conjunction with neuro exam • Repeat Cerebral Angiogram – Day 7 -10 – Regardless of securement methodology
Medications • Nimodipine 60 mg Q 4 hrs – For 21 days • Divided dose 30 mg Q 2 for hypotension • Seizure prophylaxis? ? ? – 100 mg Q 8 hrs – Only 10 -20% of a. SAH have seizures – Side effects of Phenytoin • • Pain Management Antiemetic GI Protection Stool Softeners
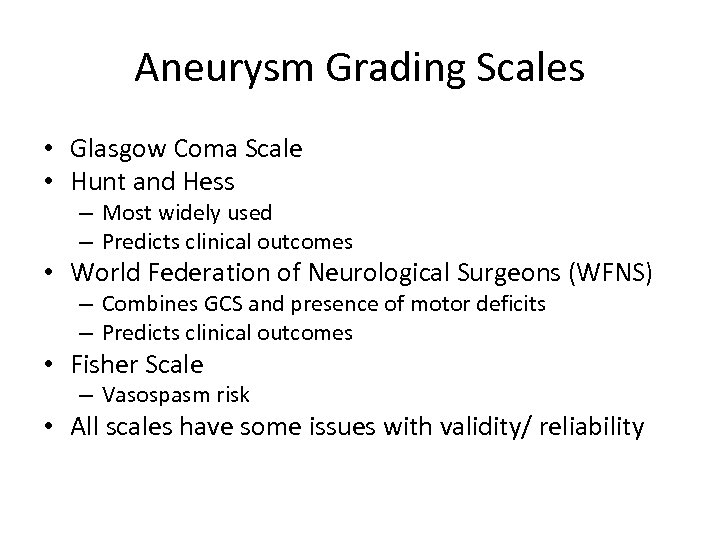
Aneurysm Grading Scales • Glasgow Coma Scale • Hunt and Hess – Most widely used – Predicts clinical outcomes • World Federation of Neurological Surgeons (WFNS) – Combines GCS and presence of motor deficits – Predicts clinical outcomes • Fisher Scale – Vasospasm risk • All scales have some issues with validity/ reliability
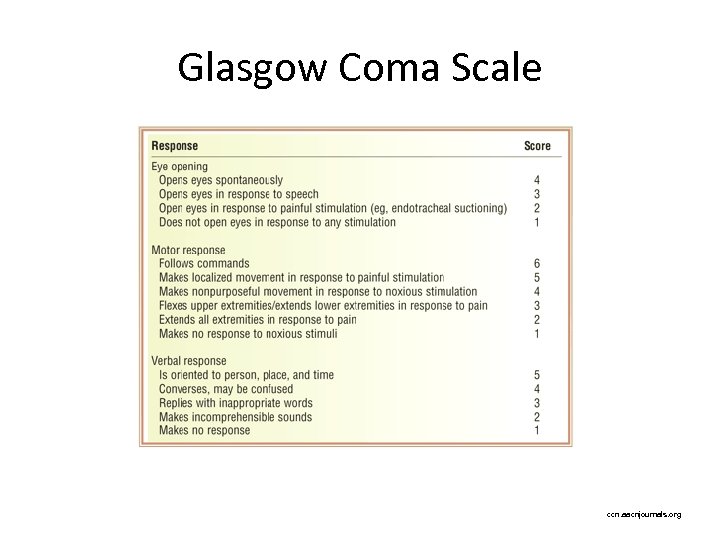
Glasgow Coma Scale ccn. aacnjournals. org
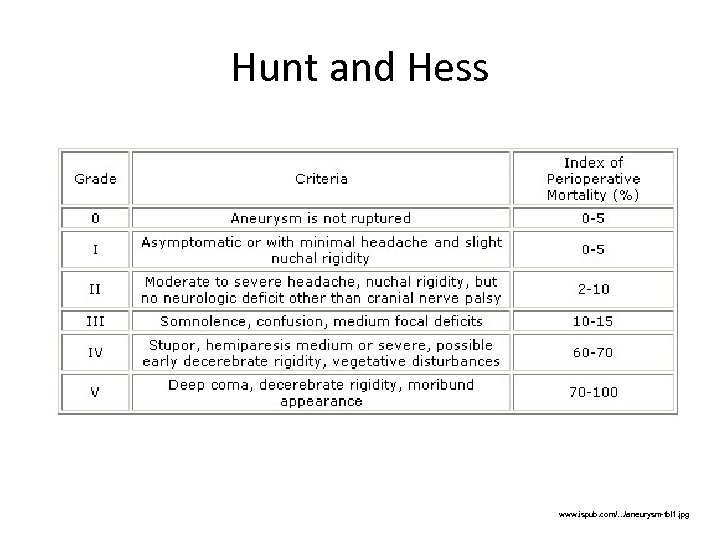
Hunt and Hess www. ispub. com/. . . /aneurysm-tbl 1. jpg
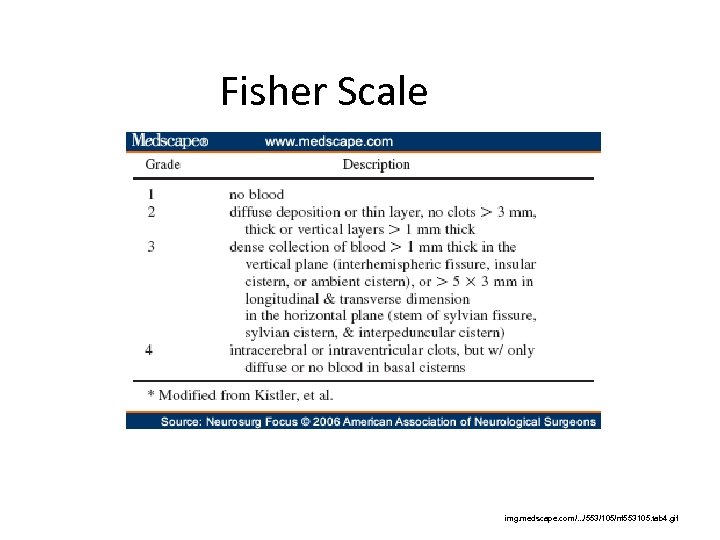
Fisher Scale img. medscape. com/. . . /553/105/nf 553105. tab 4. gif
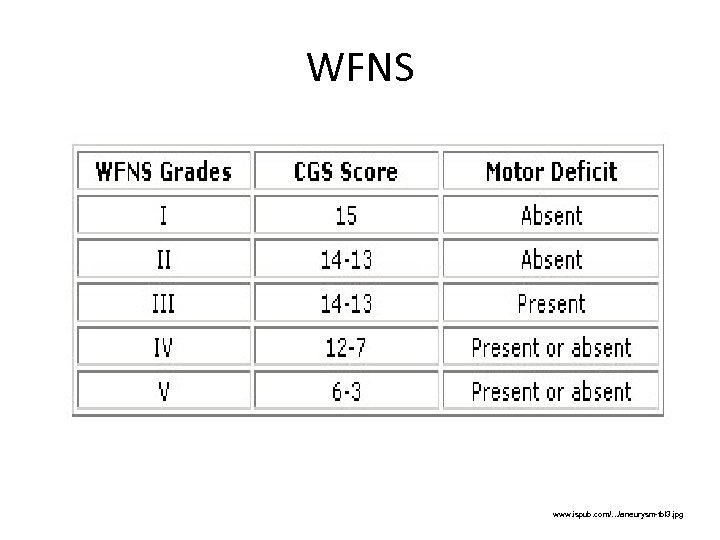
WFNS www. ispub. com/. . . /aneurysm-tbl 3. jpg
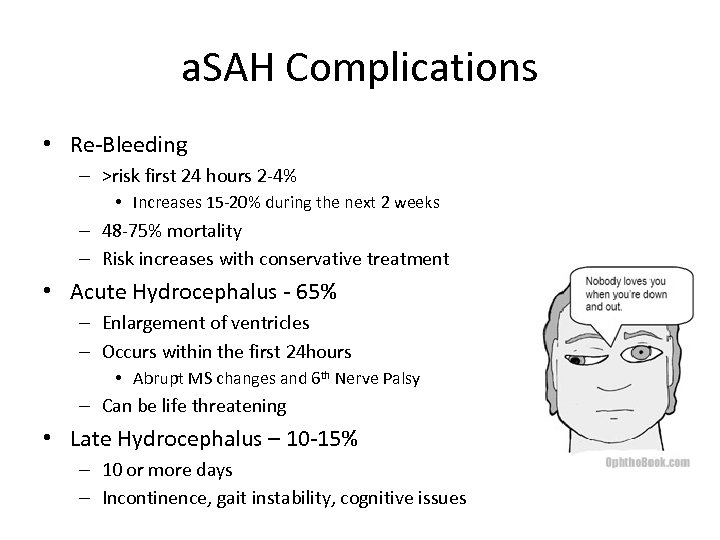
a. SAH Complications • Re-Bleeding – >risk first 24 hours 2 -4% • Increases 15 -20% during the next 2 weeks – 48 -75% mortality – Risk increases with conservative treatment • Acute Hydrocephalus - 65% – Enlargement of ventricles – Occurs within the first 24 hours • Abrupt MS changes and 6 th Nerve Palsy – Can be life threatening • Late Hydrocephalus – 10 -15% – 10 or more days – Incontinence, gait instability, cognitive issues
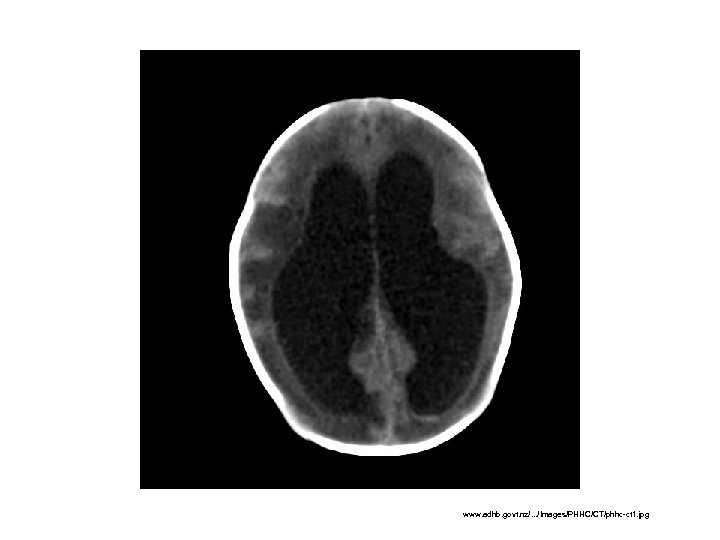
www. adhb. govt. nz/. . . /Images/PHHC/CT/phhc-ct 1. jpg
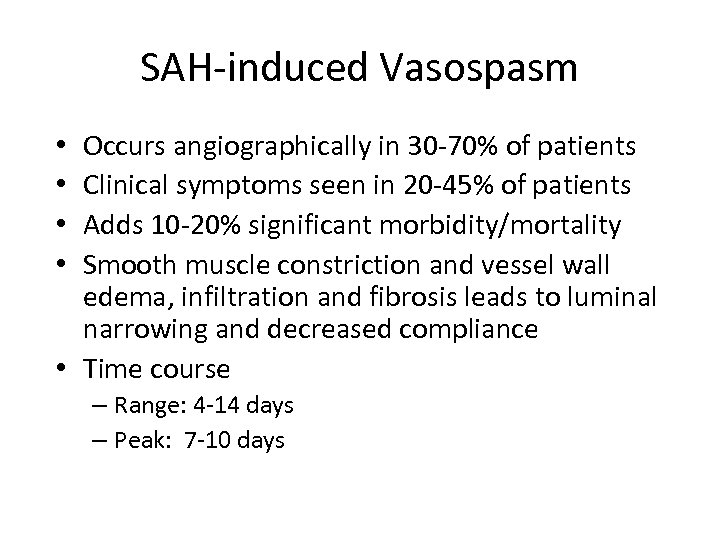
SAH-induced Vasospasm Occurs angiographically in 30 -70% of patients Clinical symptoms seen in 20 -45% of patients Adds 10 -20% significant morbidity/mortality Smooth muscle constriction and vessel wall edema, infiltration and fibrosis leads to luminal narrowing and decreased compliance • Time course • • – Range: 4 -14 days – Peak: 7 -10 days
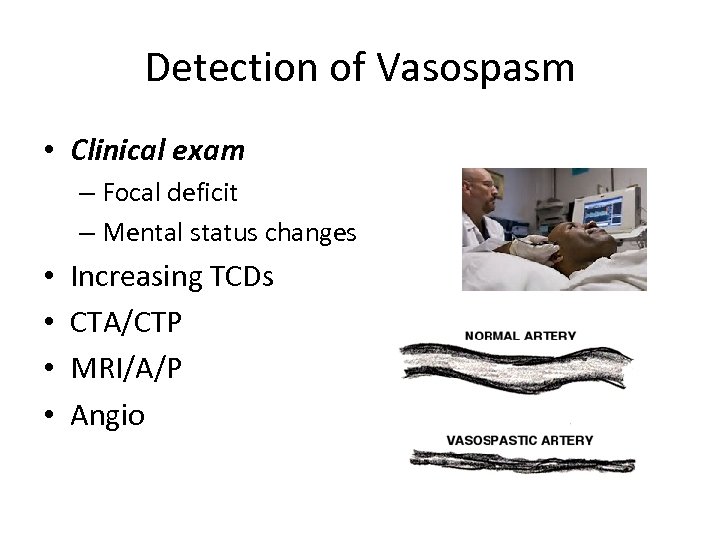
Detection of Vasospasm • Clinical exam – Focal deficit – Mental status changes • • Increasing TCDs CTA/CTP MRI/A/P Angio
Triple H Therapy (Modified) • Hypertensive therapy – SBP >160 mm HG – Don’t treat BP – patients will usually auto regulate • In symptomatic vasospasm vasopressors are used • Hypervolemia – Maintain PCWP at 10 to 16 mm Hg – Urinary output >/= 250 ml per hour • Euvolumia – Using fluids and vasopressors for symptomatic patients • Hemodilution – IV fluids at 100 -150 ml per hour – Hematocrit <0. 40 T
Vasospasm Treatment • Nimodipine – 60 mg Q 4 hr for 21 days • Cerebral Angiogram – Intra arterial calcium channel blockers • Verapamil – Angioplasty – Stent
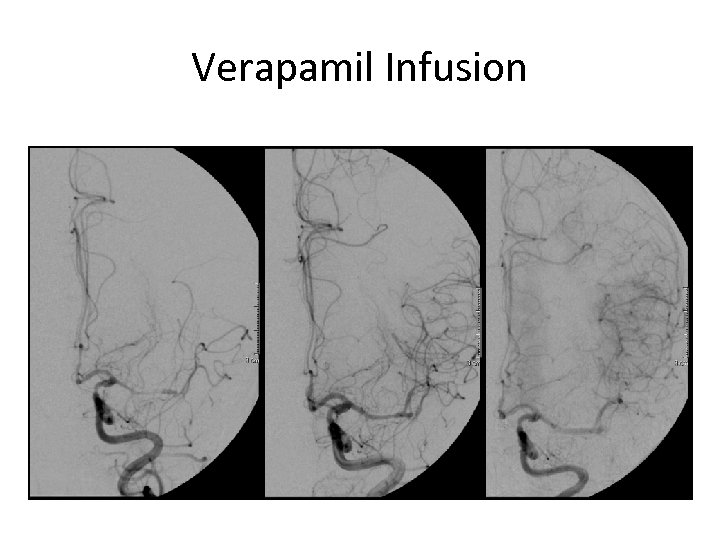
Verapamil Infusion
a. SAH Complications • Hyponatremia – 50% – Associated with poor outcomes – More common in higher grade SAH • Mechanism – Excessive renal secretion of sodium • Cerebral Salt Wasting (CSW) • Leads to cerebral edema • Treatment – Related to volume and salt replacement • Fluid restriction could be detrimental to patients
a. SAH Complications • Cardiac Dysfunction – Tako–tsubo Cardiomyopathy • Neurogenic myocardial stunning • Thought to be related to excessive release of catecholamine • Left Ventricle – Apical ballooning • MUST rule out coronary artery disease first
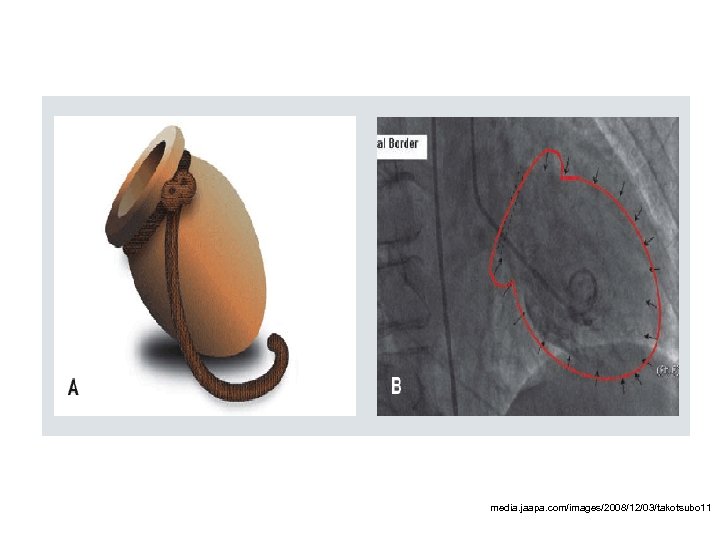
media. jaapa. com/images/2008/12/03/takotsubo 11
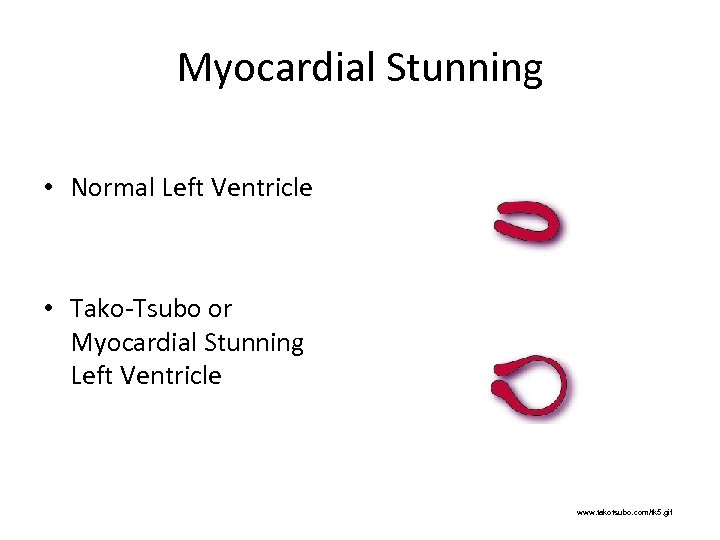
Myocardial Stunning • Normal Left Ventricle • Tako-Tsubo or Myocardial Stunning Left Ventricle www. takotsubo. com/tk 5. gif
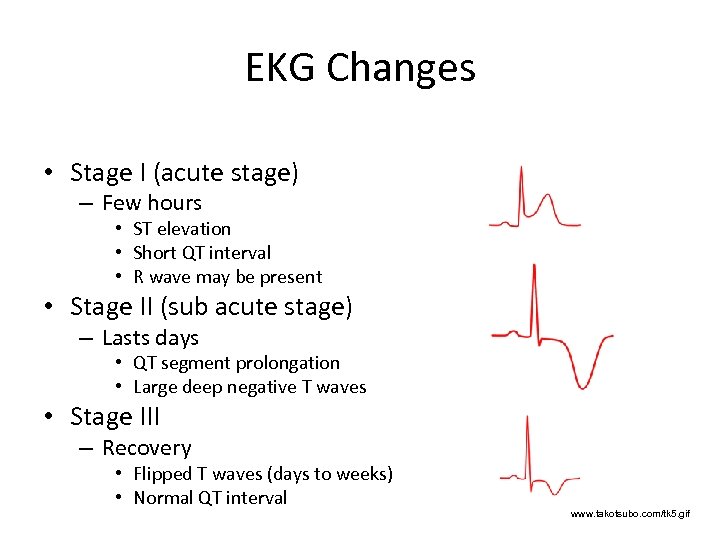
EKG Changes • Stage I (acute stage) – Few hours • ST elevation • Short QT interval • R wave may be present • Stage II (sub acute stage) – Lasts days • QT segment prolongation • Large deep negative T waves • Stage III – Recovery • Flipped T waves (days to weeks) • Normal QT interval www. takotsubo. com/tk 5. gif
Treatment of Myocardial Stunning • Supportive – Unload the left ventricle – Reduce vasopressors • Started due to low BP – Results in increased SVR and afterload – Contractility Agents • Dobutamine – Address Pulmonary Edema • Lasix
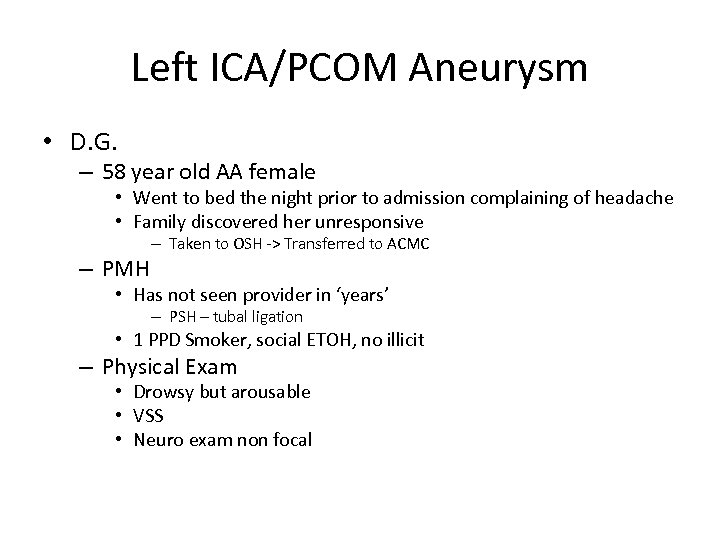
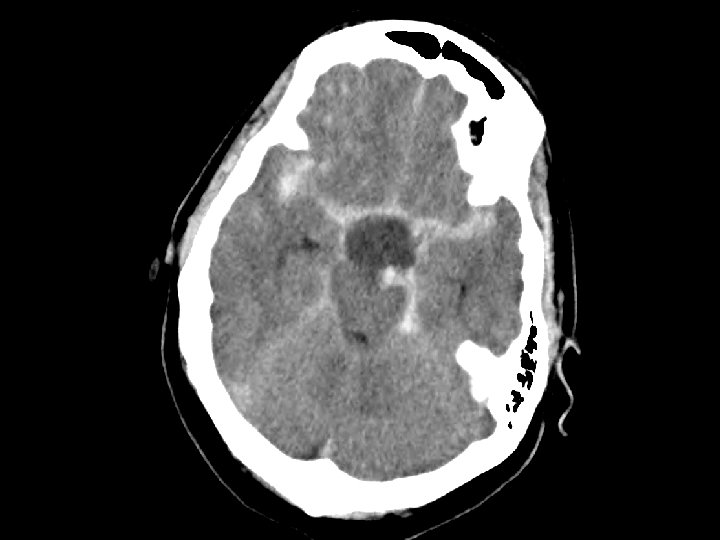
Left ICA/PCOM Aneurysm • D. G. – 58 year old AA female • Went to bed the night prior to admission complaining of headache • Family discovered her unresponsive – PMH – Taken to OSH -> Transferred to ACMC • Has not seen provider in ‘years’ – PSH – tubal ligation • 1 PPD Smoker, social ETOH, no illicit – Physical Exam • Drowsy but arousable • VSS • Neuro exam non focal
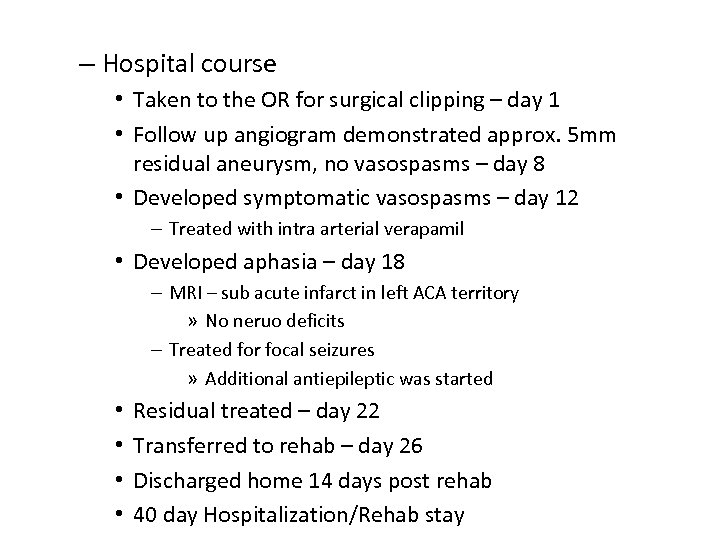
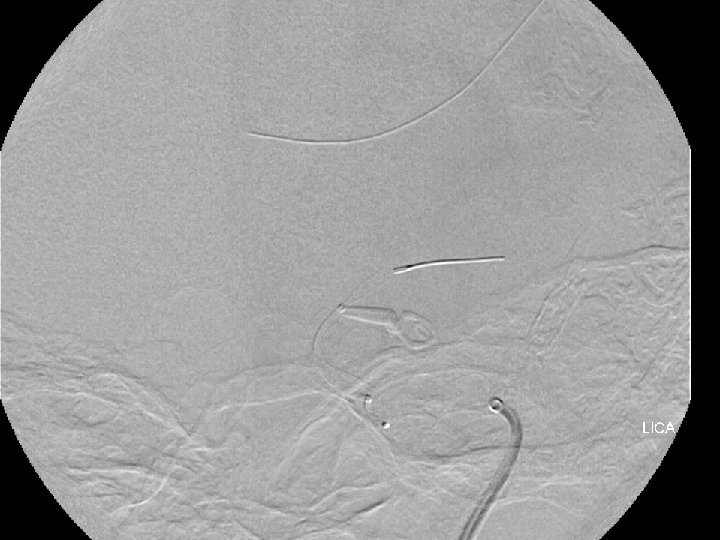
– Hospital course • Taken to the OR for surgical clipping – day 1 • Follow up angiogram demonstrated approx. 5 mm residual aneurysm, no vasospasms – day 8 • Developed symptomatic vasospasms – day 12 – Treated with intra arterial verapamil • Developed aphasia – day 18 – MRI – sub acute infarct in left ACA territory » No neruo deficits – Treated for focal seizures » Additional antiepileptic was started • • Residual treated – day 22 Transferred to rehab – day 26 Discharged home 14 days post rehab 40 day Hospitalization/Rehab stay




Unruptured Aneurysms • To Treat or not To Treat? – That is the question? • Patient Counseling – Family history • Strong family history of aneurysms or first degree relative with a. SAH – Medical history • Polycystic kidneys • Hypertension • Lifestyle – Discussion regarding natural history of aneurysms • Rate of rupture
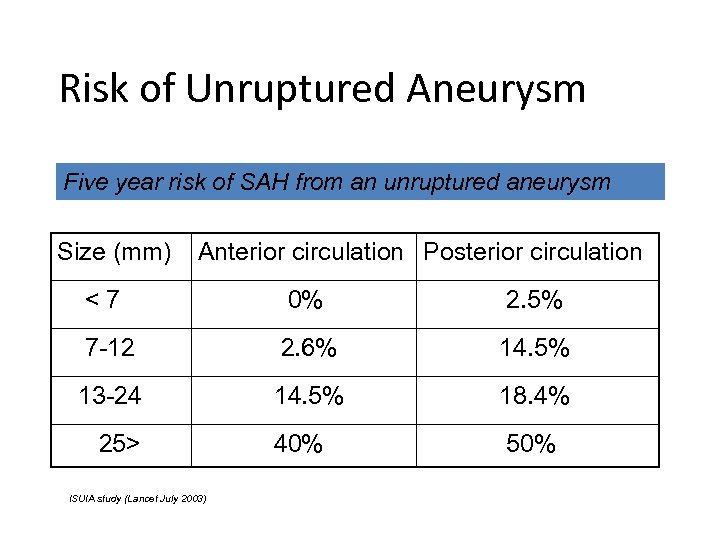
Risk of Unruptured Aneurysm Five year risk of SAH from an unruptured aneurysm Size (mm) Anterior circulation Posterior circulation <7 0% 2. 5% 7 -12 2. 6% 14. 5% 13 -24 14. 5% 18. 4% 40% 50% 25> ISUIA study (Lancet July 2003)
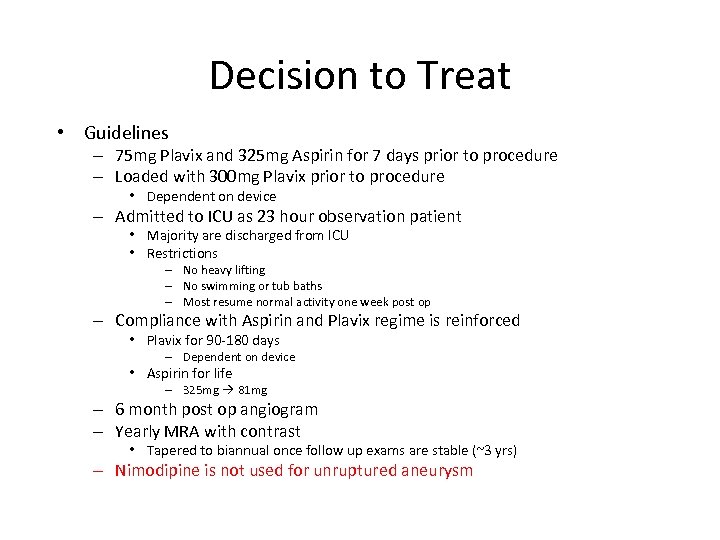
Decision to Treat • Guidelines – 75 mg Plavix and 325 mg Aspirin for 7 days prior to procedure – Loaded with 300 mg Plavix prior to procedure • Dependent on device – Admitted to ICU as 23 hour observation patient • Majority are discharged from ICU • Restrictions – No heavy lifting – No swimming or tub baths – Most resume normal activity one week post op – Compliance with Aspirin and Plavix regime is reinforced • Plavix for 90 -180 days – Dependent on device • Aspirin for life – 325 mg 81 mg – 6 month post op angiogram – Yearly MRA with contrast • Tapered to biannual once follow up exams are stable (~3 yrs) – Nimodipine is not used for unruptured aneurysm
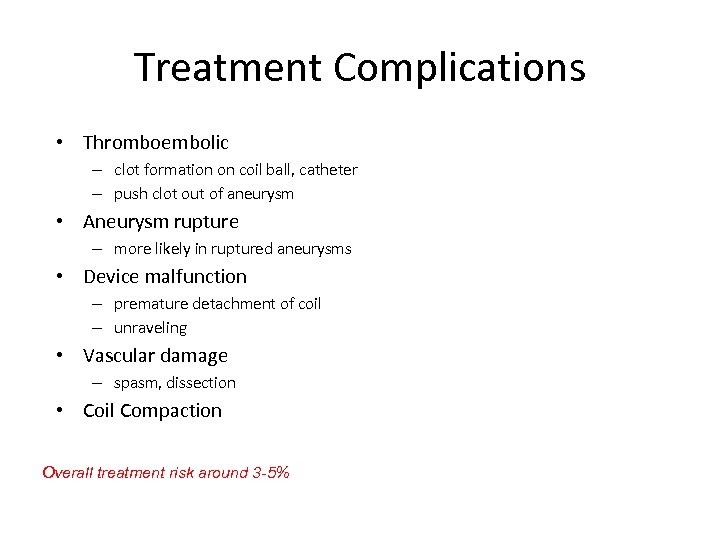
Treatment Complications • Thromboembolic – clot formation on coil ball, catheter – push clot out of aneurysm • Aneurysm rupture – more likely in ruptured aneurysms • Device malfunction – premature detachment of coil – unraveling • Vascular damage – spasm, dissection • Coil Compaction Overall treatment risk around 3 -5%
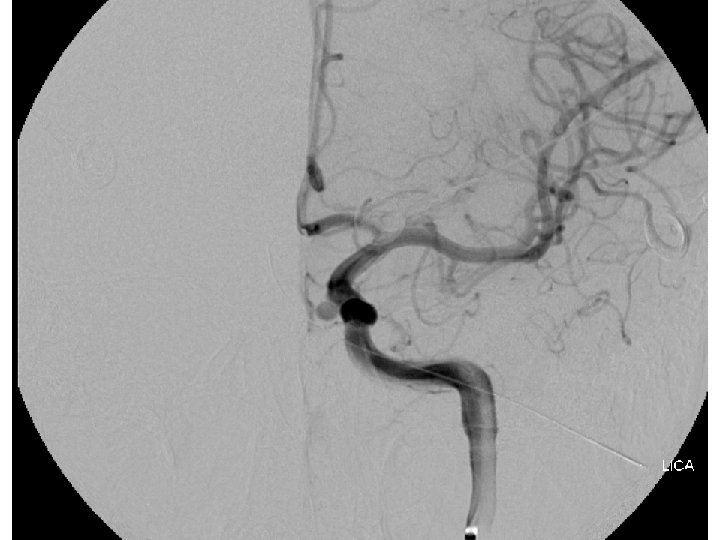
Elective Aneurysm Embolization • KM, 45 y/o female – PMH/PSH • Chari Malformation repair, Migraines, Fibromyalgia, Tubal ligation – PFH • Mother, Sister(multiple) aneurysms • Grandmother deceased from subarachnoid hemorrhage – Known ICA aneurysm being followed for years by Neurosurgery • Recent interval growth • Sent by Neurosurgeon for evaluation – PE • Non focal exam – Scheduled for Pipeline Embolization of aneurysm

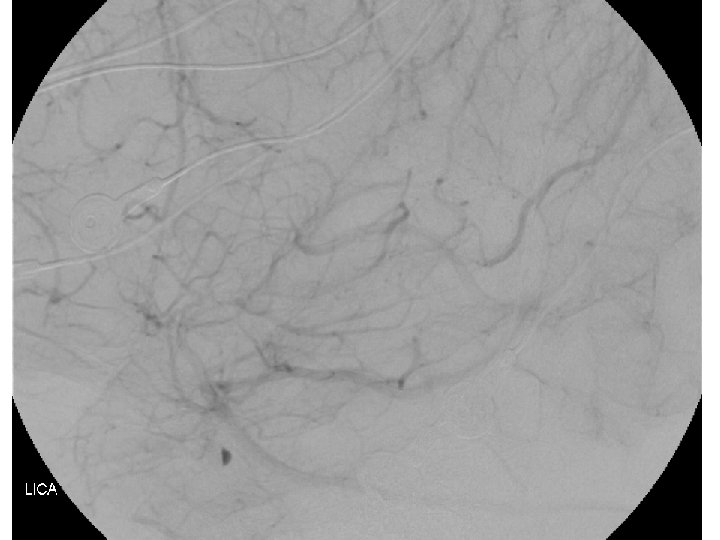
Endovascular follow up Guidelines • Initial treatment – SAH • 1 week follow angiogram – Evaluate for vasospasm • 6 month follow up angiogram • Yearly MRAs with contrast – Elective • 6 month follow up angiogram • Yearly MRAs with contrast – Once stable for several years Q 2 year MRAs
Evidence Based Care
Treatment Outcomes • ISAT trial – Comparative study of coiling vs. clipping • 2143 patients enrolled – – 1070 Clipping 1055 1073 Coiling 1063 • WFNS Grade 1 -2 – Outcomes at 1 years • m. RS of greater than 2 (dependent or dead) – – 326 or 30. 9% clipping 250 or 23. 5% coiling • Risk reduction of 7. 4% • Lower risk of post SAH epilepsy – Rebleeding at 1 year • • 7 coiling 2 clipping – Advantage followed out for 7 years
Barrow Ruptured Aneurysm Trial • Eligible patients assigned in an alternating fashion to surgical aneurysm clipping or endovascular coil therapy – 239 clipping – 233 coiling • Not all aneurysms were amenable to coiling – Cross over from coiling to clipping – Cross over patients did worse, but no worse than those randomized to clipping • Overall 1 year results (defined as m. RS >2) – 33. 7% of clipped – 23. 2% of coiling
Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage -Stroke 2012 • For patients with ruptured aneurysms judged to be technically amenable to both endovascular coiling and neurosurgical clipping, endovascular coiling should be considered (Class I; Level of Evidence B). • Microsurgical clipping may receive increased consideration in patients presenting with large (>50 m. L) intraparenchymal hematomas and middle cerebral artery aneurysms. • Endovascular coiling may receive increased consideration in the elderly (>70 years of age), in those presenting with poor-grade and in those with aneurysms of the basilar apex (Class IIb; Level of evidence C). Should patients be offered the option of coiling vs. clipping in the acute setting?
Future Research • Magnesium – Cerebral vasodilatory effects • Ability to penetrate CNS – Readily available, inexpensive – Recent research • DNI – 12/54 in the Magnesium Group = 22% – 27/53 in the Control Group = 51% • Mortality – 6/54 in the Magnesium Group = 11% – 10/53 in the control Group = 19% – Recommendations • Do not induce hypermagnesaemia • Avoid hypomagnesaemia • Further research is needed
Future Research • Statins – Several small randomized clinical trials • Shown to reduce vasospasms and DNI • Reactivation of the Stash Study – Multicenter study on the use of statins in a. SAH – Recommendation • If patient is taking statin continue • May consider in statin naive patients • More research is recommended
Future Research • Phenytoin Prophylaxis – Three day course of Phenytoin • 1. 9% of patients had seizures with 3 day prophylaxis – 1. 3% in retrospective group • 80% treated with craniotomy – Drug Reaction • 8. 8% to 0. 5% with three day course • Hospital length of stay 14. 2 to 13. 1 – Recommendations • Use of anticonvulsants is not recommended • If anticonvulsant prophylaxis is used – 3 -7 days • If patient presents with history of seizure – Institution’s protocol
Take Home Points • Sentinel leak is often overlooked • Aneurysmal rebleeding is fatal in 75% of patients • Neurogenic Pulmonary Edema occurs independent of cardiac dysfunction • Cerebral Salt Wasting is real and important
• • • Phenytoin Prophylaxis in a. SAH causes more problems then it solves Symptoms of Vasospasm and Hydrocephalus are similar Angiographic signature of vasospasm does not explain patient findings Vascular Treatments for vasospasms are inadequate Treatments for High Grade Patients remain poor
www. newyorker. com/. . . /071210_r 16884_p 465. jpg


The End
? ? ? Questions? ? ?
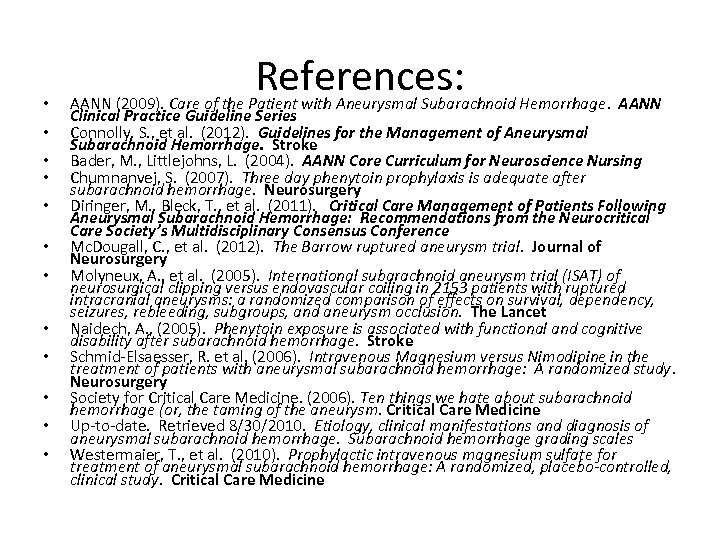
• • • References: AANN (2009). Care of the Patient with Aneurysmal Subarachnoid Hemorrhage. AANN Clinical Practice Guideline Series Connolly, S. , et al. (2012). Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage. Stroke Bader, M. , Littlejohns, L. (2004). AANN Core Curriculum for Neuroscience Nursing Chumnanvej, S. (2007). Three day phenytoin prophylaxis is adequate after subarachnoid hemorrhage. Neurosurgery Diringer, M. , Bleck, T. , et al. (2011). Critical Care Management of Patients Following Aneurysmal Subarachnoid Hemorrhage: Recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference Mc. Dougall, C. , et al. (2012). The Barrow ruptured aneurysm trial. Journal of Neurosurgery Molyneux, A. , et al. (2005). International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2153 patients with ruptured intracranial aneurysms: a randomized comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. The Lancet Naidech, A. , (2005). Phenytoin exposure is associated with functional and cognitive disability after subarachnoid hemorrhage. Stroke Schmid-Elsaesser, R. et al. (2006). Intravenous Magnesium versus Nimodipine in the treatment of patients with aneurysmal subarachnoid hemorrhage: A randomized study. Neurosurgery Society for Critical Care Medicine. (2006). Ten things we hate about subarachnoid hemorrhage (or, the taming of the aneurysm. Critical Care Medicine Up-to-date. Retrieved 8/30/2010. Etiology, clinical manifestations and diagnosis of aneurysmal subarachnoid hemorrhage. Subarachnoid hemorrhage grading scales Westermaier, T. , et al. (2010). Prophylactic intravenous magnesium sulfate for treatment of aneurysmal subarachnoid hemorrhage: A randomized, placebo-controlled, clinical study. Critical Care Medicine
753d873f77acddf47e8bc04b612dbd61.ppt