0695a129bfce499c689b4540f1c588d1.ppt
- Количество слайдов: 24
 Endothelial Progenitor Cells, Platelets and PCI Eli I. Lev, MD Director, Cardiac Cathetrization Laboratory Hasharon Hospital, Rabin Medical Center, Tel-Aviv University, Israel
Endothelial Progenitor Cells, Platelets and PCI Eli I. Lev, MD Director, Cardiac Cathetrization Laboratory Hasharon Hospital, Rabin Medical Center, Tel-Aviv University, Israel
 Conflicts of interest • None relevant to the topic of this lecture
Conflicts of interest • None relevant to the topic of this lecture
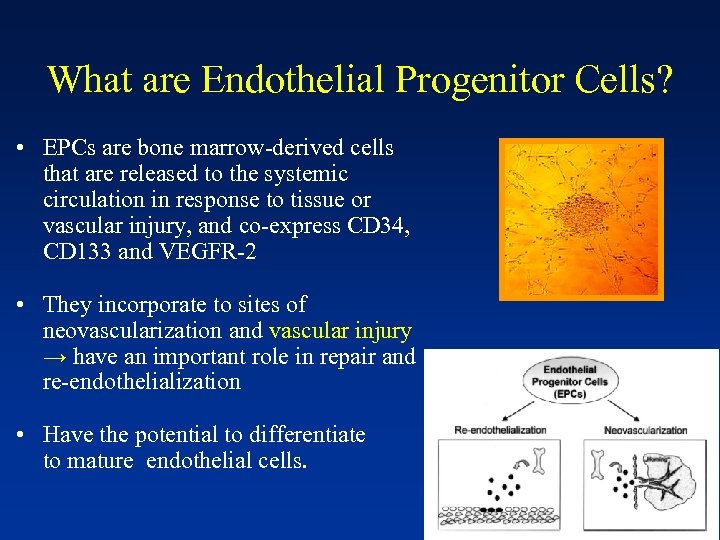 What are Endothelial Progenitor Cells? • EPCs are bone marrow-derived cells that are released to the systemic circulation in response to tissue or vascular injury, and co-express CD 34, CD 133 and VEGFR-2 • They incorporate to sites of neovascularization and vascular injury → have an important role in repair and re-endothelialization • Have the potential to differentiate to mature endothelial cells.
What are Endothelial Progenitor Cells? • EPCs are bone marrow-derived cells that are released to the systemic circulation in response to tissue or vascular injury, and co-express CD 34, CD 133 and VEGFR-2 • They incorporate to sites of neovascularization and vascular injury → have an important role in repair and re-endothelialization • Have the potential to differentiate to mature endothelial cells.
 EPCs and Vascular Injury, Animal Models • Following balloon injury, EPCs mobilize and “home” to denuded parts of the vessel wall accelerate endothelial regeneration (Walter et al, Circ 2002, Werner et al ATVB 2002) • Transplantation of isolated circulating EPCs into balloon-injured arteries leads to rapid reendothelialization of the denuded vessels (Griese et al, Circ 03)
EPCs and Vascular Injury, Animal Models • Following balloon injury, EPCs mobilize and “home” to denuded parts of the vessel wall accelerate endothelial regeneration (Walter et al, Circ 2002, Werner et al ATVB 2002) • Transplantation of isolated circulating EPCs into balloon-injured arteries leads to rapid reendothelialization of the denuded vessels (Griese et al, Circ 03)
 EPCs and Vascular Injury, Humans • Circulating EPC levels increase sig. after acute vascular insults (e. g. CABG), and coronary artery stenting → within 6 -12 hours (Lev et al, J Vasc Res 2005, Bonello et al, JTH 2006, etc. ) • Low levels of circulating EPCs have been correlated with CV risk factors and independently with poor CV outcomes in various populations (Hill et al, NEJM 2003, Werner et al NEJM 2005)
EPCs and Vascular Injury, Humans • Circulating EPC levels increase sig. after acute vascular insults (e. g. CABG), and coronary artery stenting → within 6 -12 hours (Lev et al, J Vasc Res 2005, Bonello et al, JTH 2006, etc. ) • Low levels of circulating EPCs have been correlated with CV risk factors and independently with poor CV outcomes in various populations (Hill et al, NEJM 2003, Werner et al NEJM 2005)
 How do EPCs adhere to sites of vascular injury? → Important role of platelets which can interact directly with EPCs
How do EPCs adhere to sites of vascular injury? → Important role of platelets which can interact directly with EPCs
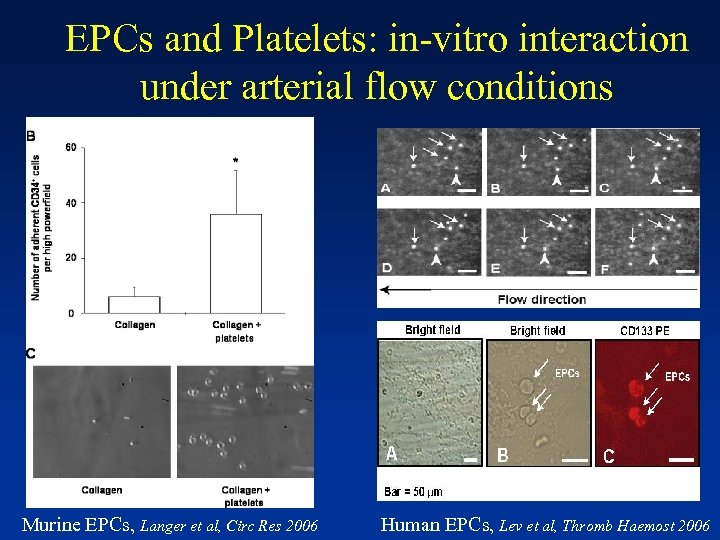 EPCs and Platelets: in-vitro interaction under arterial flow conditions Murine EPCs, Langer et al, Circ Res 2006 Human EPCs, Lev et al, Thromb Haemost 2006
EPCs and Platelets: in-vitro interaction under arterial flow conditions Murine EPCs, Langer et al, Circ Res 2006 Human EPCs, Lev et al, Thromb Haemost 2006
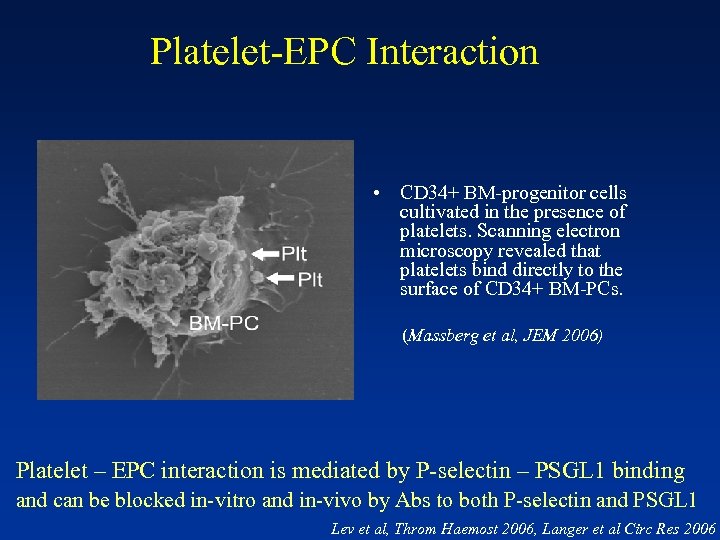 Platelet-EPC Interaction • CD 34+ BM-progenitor cells cultivated in the presence of platelets. Scanning electron microscopy revealed that platelets bind directly to the surface of CD 34+ BM-PCs. (Massberg et al, JEM 2006) Platelet – EPC interaction is mediated by P-selectin – PSGL 1 binding and can be blocked in-vitro and in-vivo by Abs to both P-selectin and PSGL 1 Lev et al, Throm Haemost 2006, Langer et al Circ Res 2006
Platelet-EPC Interaction • CD 34+ BM-progenitor cells cultivated in the presence of platelets. Scanning electron microscopy revealed that platelets bind directly to the surface of CD 34+ BM-PCs. (Massberg et al, JEM 2006) Platelet – EPC interaction is mediated by P-selectin – PSGL 1 binding and can be blocked in-vitro and in-vivo by Abs to both P-selectin and PSGL 1 Lev et al, Throm Haemost 2006, Langer et al Circ Res 2006
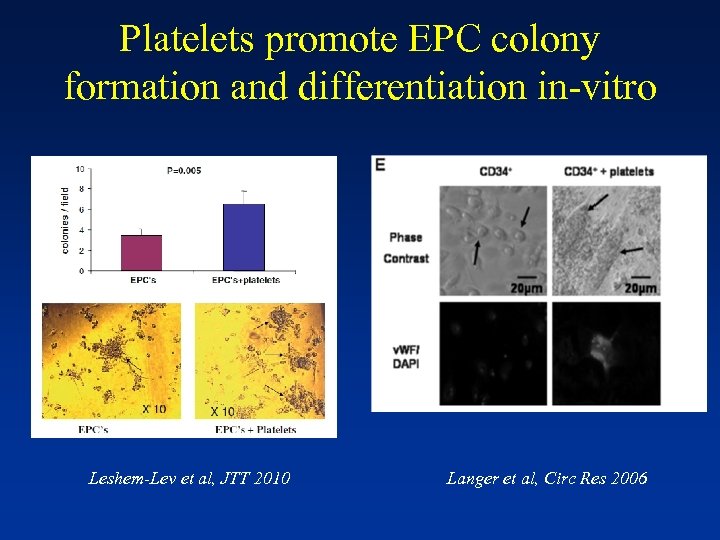 Platelets promote EPC colony formation and differentiation in-vitro Leshem-Lev et al, JTT 2010 Langer et al, Circ Res 2006
Platelets promote EPC colony formation and differentiation in-vitro Leshem-Lev et al, JTT 2010 Langer et al, Circ Res 2006
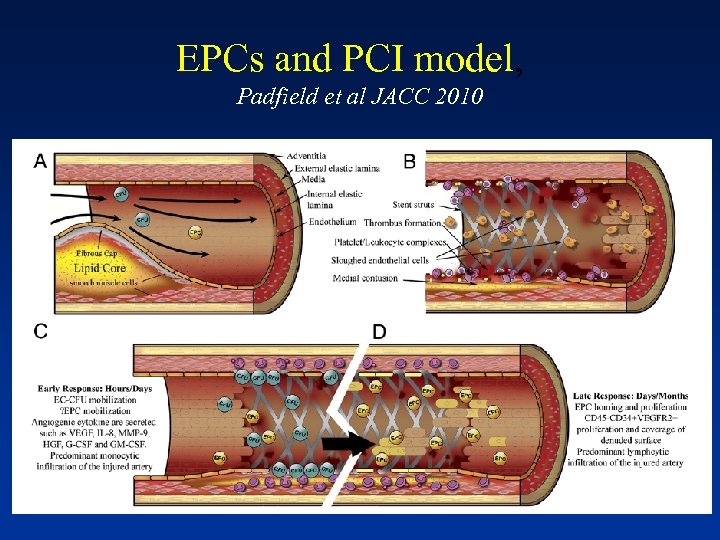 EPCs and PCI model, Padfield et al JACC 2010
EPCs and PCI model, Padfield et al JACC 2010
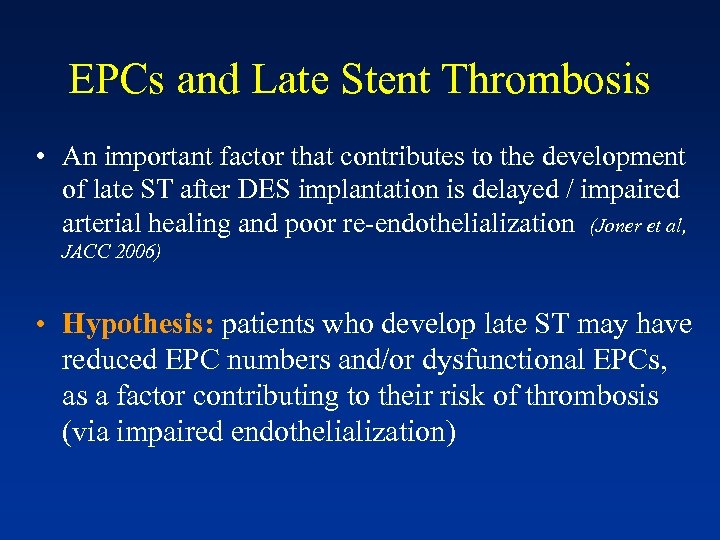 EPCs and Late Stent Thrombosis • An important factor that contributes to the development of late ST after DES implantation is delayed / impaired arterial healing and poor re-endothelialization (Joner et al, JACC 2006) • Hypothesis: patients who develop late ST may have reduced EPC numbers and/or dysfunctional EPCs, as a factor contributing to their risk of thrombosis (via impaired endothelialization)
EPCs and Late Stent Thrombosis • An important factor that contributes to the development of late ST after DES implantation is delayed / impaired arterial healing and poor re-endothelialization (Joner et al, JACC 2006) • Hypothesis: patients who develop late ST may have reduced EPC numbers and/or dysfunctional EPCs, as a factor contributing to their risk of thrombosis (via impaired endothelialization)
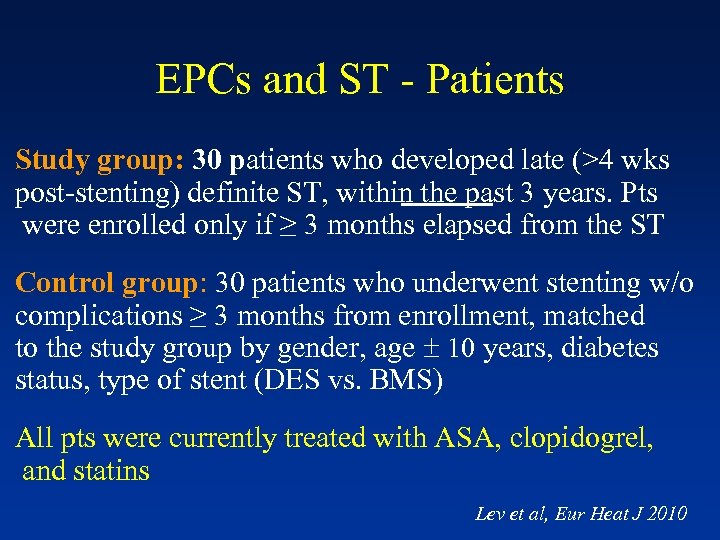 EPCs and ST - Patients Study group: 30 patients who developed late (>4 wks post-stenting) definite ST, within the past 3 years. Pts were enrolled only if ≥ 3 months elapsed from the ST Control group: 30 patients who underwent stenting w/o complications ≥ 3 months from enrollment, matched to the study group by gender, age 10 years, diabetes status, type of stent (DES vs. BMS) All pts were currently treated with ASA, clopidogrel, and statins Lev et al, Eur Heat J 2010
EPCs and ST - Patients Study group: 30 patients who developed late (>4 wks post-stenting) definite ST, within the past 3 years. Pts were enrolled only if ≥ 3 months elapsed from the ST Control group: 30 patients who underwent stenting w/o complications ≥ 3 months from enrollment, matched to the study group by gender, age 10 years, diabetes status, type of stent (DES vs. BMS) All pts were currently treated with ASA, clopidogrel, and statins Lev et al, Eur Heat J 2010
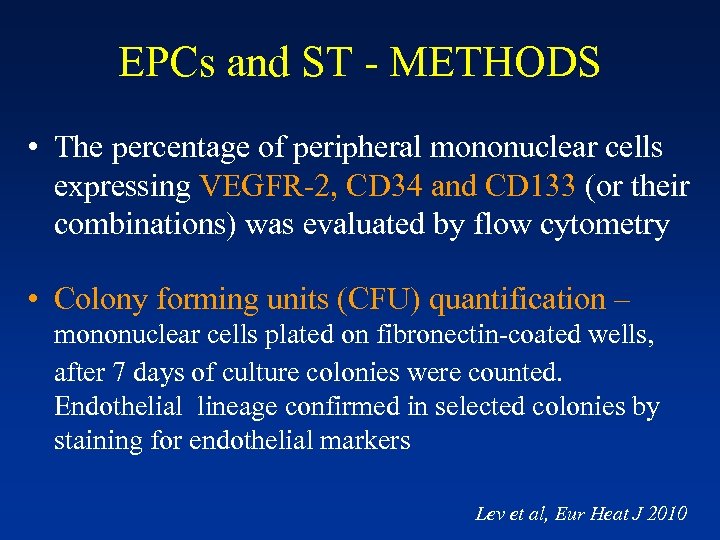 EPCs and ST - METHODS • The percentage of peripheral mononuclear cells expressing VEGFR-2, CD 34 and CD 133 (or their combinations) was evaluated by flow cytometry • Colony forming units (CFU) quantification – mononuclear cells plated on fibronectin-coated wells, after 7 days of culture colonies were counted. Endothelial lineage confirmed in selected colonies by staining for endothelial markers Lev et al, Eur Heat J 2010
EPCs and ST - METHODS • The percentage of peripheral mononuclear cells expressing VEGFR-2, CD 34 and CD 133 (or their combinations) was evaluated by flow cytometry • Colony forming units (CFU) quantification – mononuclear cells plated on fibronectin-coated wells, after 7 days of culture colonies were counted. Endothelial lineage confirmed in selected colonies by staining for endothelial markers Lev et al, Eur Heat J 2010
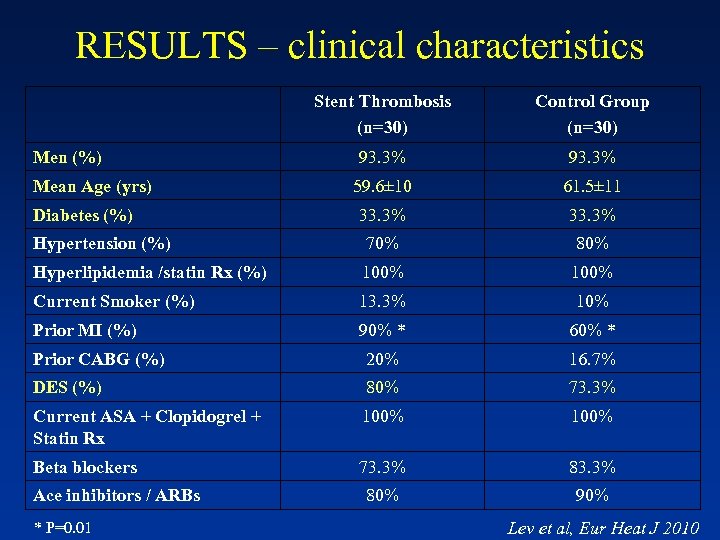 RESULTS – clinical characteristics Stent Thrombosis (n=30) Control Group (n=30) 93. 3% 59. 6± 10 61. 5± 11 33. 3% Hypertension (%) 70% 80% Hyperlipidemia /statin Rx (%) 100% Current Smoker (%) 13. 3% 10% Prior MI (%) 90% * 60% * Prior CABG (%) 20% 16. 7% DES (%) 80% 73. 3% Current ASA + Clopidogrel + Statin Rx 100% Beta blockers 73. 3% 80% 90% Men (%) Mean Age (yrs) Diabetes (%) Ace inhibitors / ARBs * P=0. 01 Lev et al, Eur Heat J 2010
RESULTS – clinical characteristics Stent Thrombosis (n=30) Control Group (n=30) 93. 3% 59. 6± 10 61. 5± 11 33. 3% Hypertension (%) 70% 80% Hyperlipidemia /statin Rx (%) 100% Current Smoker (%) 13. 3% 10% Prior MI (%) 90% * 60% * Prior CABG (%) 20% 16. 7% DES (%) 80% 73. 3% Current ASA + Clopidogrel + Statin Rx 100% Beta blockers 73. 3% 80% 90% Men (%) Mean Age (yrs) Diabetes (%) Ace inhibitors / ARBs * P=0. 01 Lev et al, Eur Heat J 2010
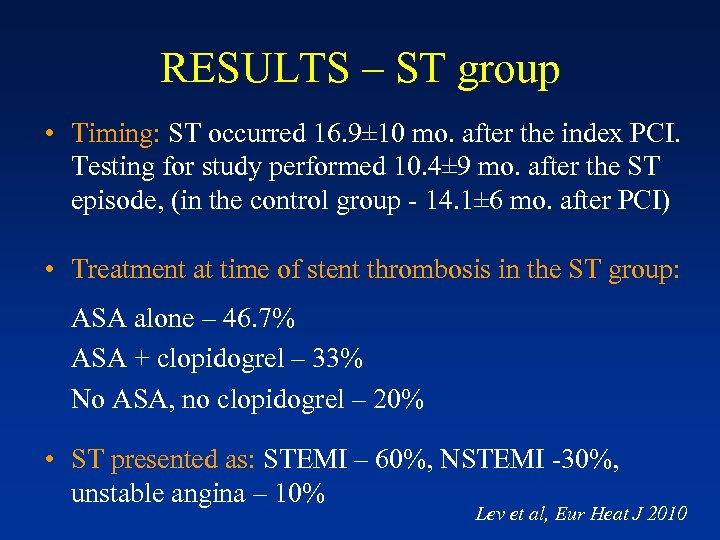 RESULTS – ST group • Timing: ST occurred 16. 9± 10 mo. after the index PCI. Testing for study performed 10. 4± 9 mo. after the ST episode, (in the control group - 14. 1± 6 mo. after PCI) • Treatment at time of stent thrombosis in the ST group: ASA alone – 46. 7% ASA + clopidogrel – 33% No ASA, no clopidogrel – 20% • ST presented as: STEMI – 60%, NSTEMI -30%, unstable angina – 10% Lev et al, Eur Heat J 2010
RESULTS – ST group • Timing: ST occurred 16. 9± 10 mo. after the index PCI. Testing for study performed 10. 4± 9 mo. after the ST episode, (in the control group - 14. 1± 6 mo. after PCI) • Treatment at time of stent thrombosis in the ST group: ASA alone – 46. 7% ASA + clopidogrel – 33% No ASA, no clopidogrel – 20% • ST presented as: STEMI – 60%, NSTEMI -30%, unstable angina – 10% Lev et al, Eur Heat J 2010
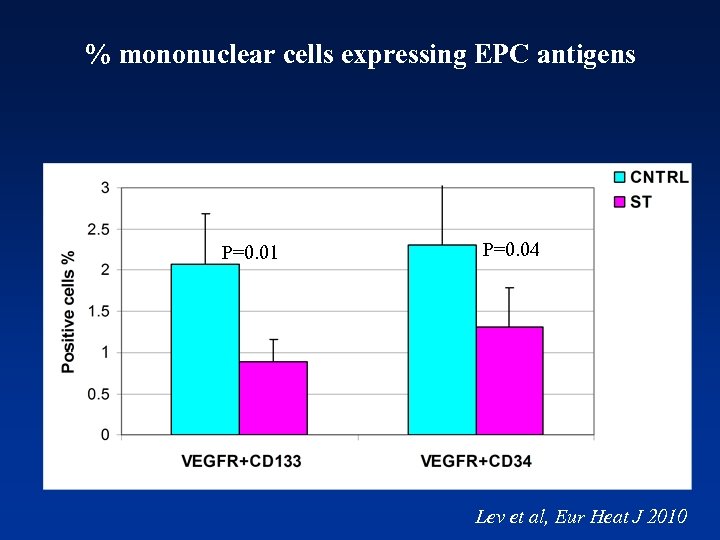 % mononuclear cells expressing EPC antigens P=0. 01 P=0. 04 Lev et al, Eur Heat J 2010
% mononuclear cells expressing EPC antigens P=0. 01 P=0. 04 Lev et al, Eur Heat J 2010
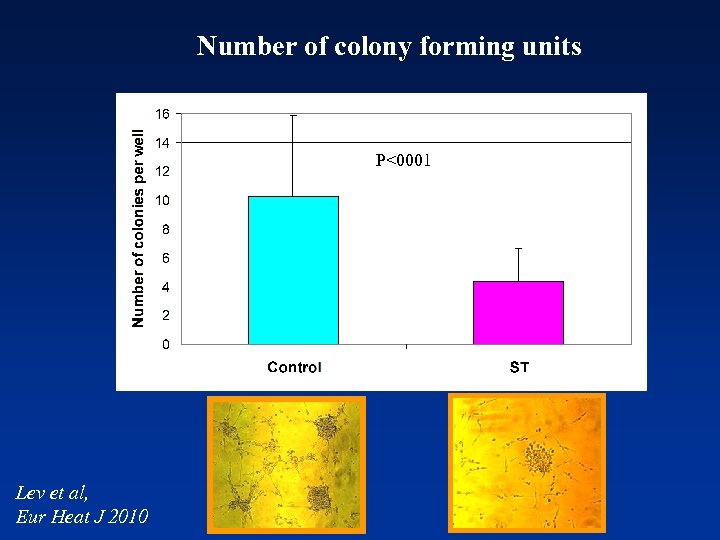 Number of colony forming units P<0001 Lev et al, Eur Heat J 2010
Number of colony forming units P<0001 Lev et al, Eur Heat J 2010
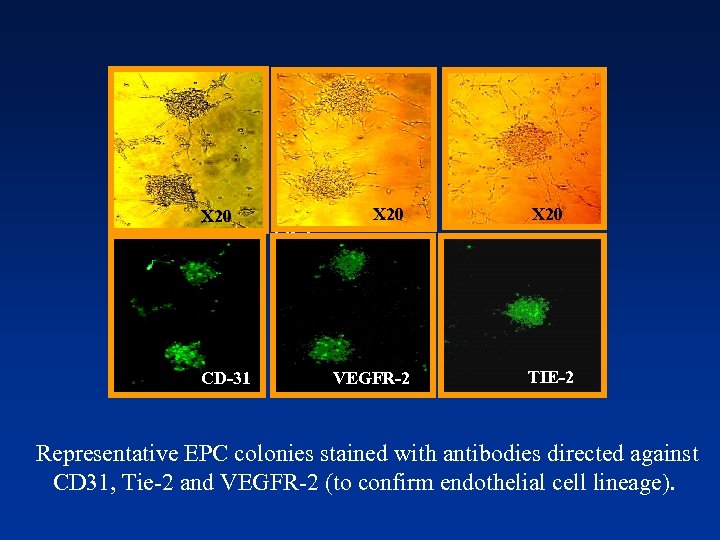 X 20 CD-31 X 20 Tei-2 VEGFR-2 TIE-2 Representative EPC colonies stained with antibodies directed against CD 31, Tie-2 and VEGFR-2 (to confirm endothelial cell lineage).
X 20 CD-31 X 20 Tei-2 VEGFR-2 TIE-2 Representative EPC colonies stained with antibodies directed against CD 31, Tie-2 and VEGFR-2 (to confirm endothelial cell lineage).
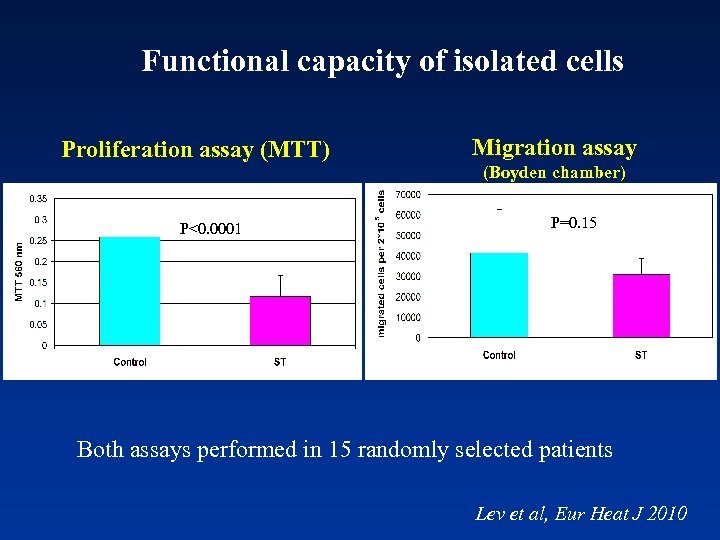 Functional capacity of isolated cells Proliferation assay (MTT) Migration assay (Boyden chamber) P<0. 0001 P=0. 15 Both assays performed in 15 randomly selected patients Lev et al, Eur Heat J 2010
Functional capacity of isolated cells Proliferation assay (MTT) Migration assay (Boyden chamber) P<0. 0001 P=0. 15 Both assays performed in 15 randomly selected patients Lev et al, Eur Heat J 2010
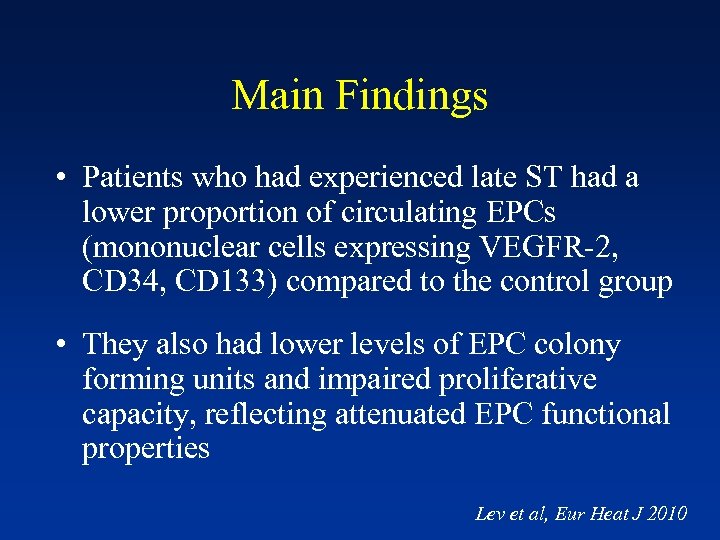 Main Findings • Patients who had experienced late ST had a lower proportion of circulating EPCs (mononuclear cells expressing VEGFR-2, CD 34, CD 133) compared to the control group • They also had lower levels of EPC colony forming units and impaired proliferative capacity, reflecting attenuated EPC functional properties Lev et al, Eur Heat J 2010
Main Findings • Patients who had experienced late ST had a lower proportion of circulating EPCs (mononuclear cells expressing VEGFR-2, CD 34, CD 133) compared to the control group • They also had lower levels of EPC colony forming units and impaired proliferative capacity, reflecting attenuated EPC functional properties Lev et al, Eur Heat J 2010
 Conclusions • Patients who underwent late ST had reduced levels and function of EPCs compared with matched control group • Limitations of case-control design, one blood sample → findings require validation by further studies, but may contribute to understanding the mechanism of late ST • Clinical implications: If indeed EPCs have an essential role in stent endothel. and attenuated EPC status contributes to ST development, augmenting EPCs may reduce the risk of ST → statins, PE, locally by “EPC capturing” stents
Conclusions • Patients who underwent late ST had reduced levels and function of EPCs compared with matched control group • Limitations of case-control design, one blood sample → findings require validation by further studies, but may contribute to understanding the mechanism of late ST • Clinical implications: If indeed EPCs have an essential role in stent endothel. and attenuated EPC status contributes to ST development, augmenting EPCs may reduce the risk of ST → statins, PE, locally by “EPC capturing” stents
 THANK YOU
THANK YOU
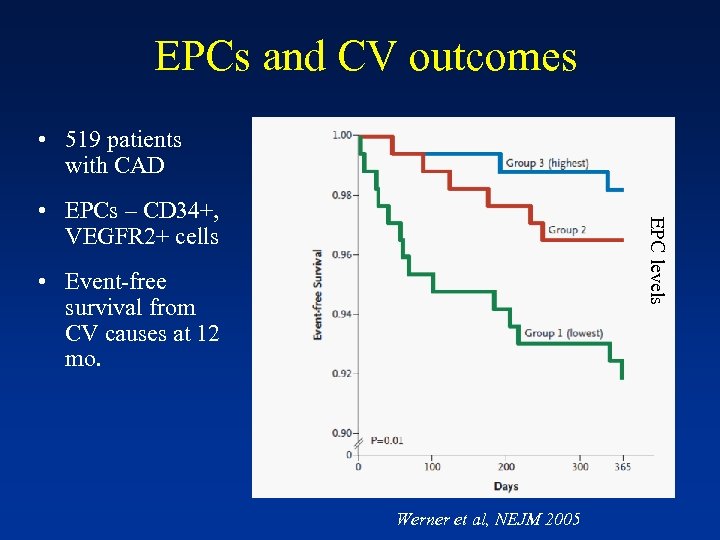 EPCs and CV outcomes • 519 patients with CAD EPC levels • EPCs – CD 34+, VEGFR 2+ cells • Event-free survival from CV causes at 12 mo. Werner et al, NEJM 2005
EPCs and CV outcomes • 519 patients with CAD EPC levels • EPCs – CD 34+, VEGFR 2+ cells • Event-free survival from CV causes at 12 mo. Werner et al, NEJM 2005
 BACKGROUND • Stent thrombosis (ST) is a rare but life-threatening complication of coronary stent implantation • Early ST can occur following implantation of either BMS or DES, whereas late (> 30 days) and very late (> 1 year) ST occur more commonly with DES • Research of possible mechanisms of ST has focused on 2 main areas: procedure and stent-related factors (e. g. stent under-expansion, bifurcation stenting), and plateletrelated factors (d/c or low response to clopidogrel, ASA)
BACKGROUND • Stent thrombosis (ST) is a rare but life-threatening complication of coronary stent implantation • Early ST can occur following implantation of either BMS or DES, whereas late (> 30 days) and very late (> 1 year) ST occur more commonly with DES • Research of possible mechanisms of ST has focused on 2 main areas: procedure and stent-related factors (e. g. stent under-expansion, bifurcation stenting), and plateletrelated factors (d/c or low response to clopidogrel, ASA)


