117.ppt
- Количество слайдов: 45

Endocarditis Выполнил: Абдиев Ш. Г. Проверила: Факультет: ОМ-043 -01
Goals for Today Recognize the risk factors, signs, and symptoms of infectious endocarditis. Understand the many approaches to diagnosing infectious endocarditis. Appreciate the necessity of rapid treatment. Anticipate possible complications. Bring it all together with an actual patient case!
For Another Day…. . Pediatric infective endocarditis Specifics of nosocomial and prosthetic valve infective endocarditis Specifics of treatment Antibiotic prophylaxis
Definition Infectious Endocarditis (IE): an infection of the heart’s endocardial surface Classified into four groups: – Native Valve IE – Prosthetic Valve IE – Intravenous drug abuse (IVDA) IE – Nosocomial IE
Further Classification Acute – Affects normal heart valves – Rapidly destructive – Metastatic foci – Commonly Staph. – If not treated, usually fatal within 6 weeks Subacute – Often affects damaged heart valves – Indolent nature – If not treated, usually fatal by one year
Pathophysiology 1. Turbulent blood flow disrupts the endocardium making it “sticky” 2. Bacteremia delivers the organisms to the endocardial surface 3. Adherence of the organisms to the endocardial surface 4. Eventual invasion of the valvular leaflets
Epidemiology Incidence difficult to ascertain and varies according to location Much more common in males than in females May occur in persons of any age and increasingly common in elderly Mortality ranges from 20 -30%
Risk Factors Intravenous drug abuse Artificial heart valves and pacemakers Acquired heart defects – Calcific aortic stenosis – Mitral valve prolapse with regurgitation Congenital heart defects Intravascular catheters
Infecting Organisms Common bacteria – S. aureus – Streptococci – Enterococci Not so common bacteria – Fungi – Pseudomonas – HACEK
Symptoms Acute – High grade fever and chills – SOB – Arthralgias/ myalgias – Abdominal pain – Pleuritic chest pain – Back pain Subacute – – – – Low grade fever Anorexia Weight loss Fatigue Arthralgias/ myalgias Abdominal pain N/V The onset of symptoms is usually ~2 weeks or less from the initiating bacteremia
Signs Fever Heart murmur Nonspecific signs – petechiae, subungal or “splinter” hemorrhages, clubbing, splenomegaly, neurologic changes More specific signs - Osler’s Nodes, Janeway lesions, and Roth Spots

Petechiae 1. Nonspecific 2. Often located on extremities or mucous membranes dermatology. about. com/. . . / blpetechiaephoto. htm Photo credit, Josh Fierer, M. D. medicine. ucsd. edu/clinicalimg/ Eye-Petechiae. html Harden Library for the Health Sciences www. lib. uiowa. edu/hardin/md/cdc/3184. html

Splinter Hemorrhages 1. Nonspecific 2. Nonblanching 3. Linear reddish-brown lesions found under the nail bed 4. Usually do NOT extend the entire length of the nail
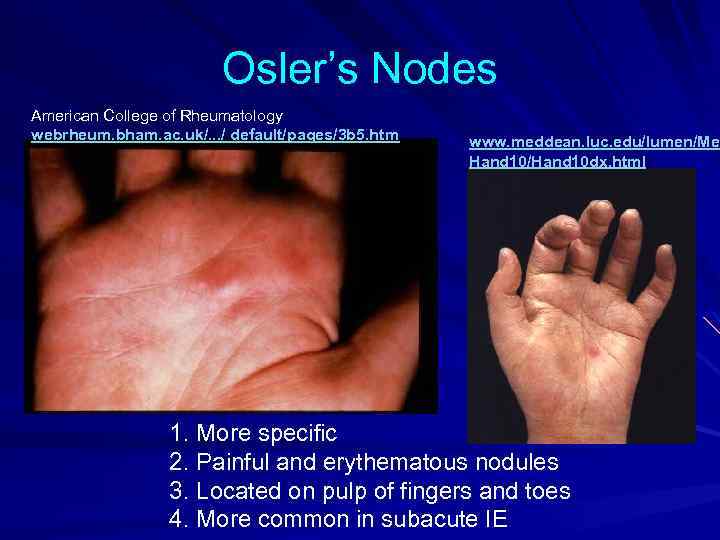
Osler’s Nodes American College of Rheumatology webrheum. bham. ac. uk/. . . / default/pages/3 b 5. htm www. meddean. luc. edu/lumen/Med Hand 10/Hand 10 dx. html 1. More specific 2. Painful and erythematous nodules 3. Located on pulp of fingers and toes 4. More common in subacute IE

Janeway Lesions 1. More specific 2. Erythematous, blanching macules 3. Nonpainful 4. Located on palms and soles
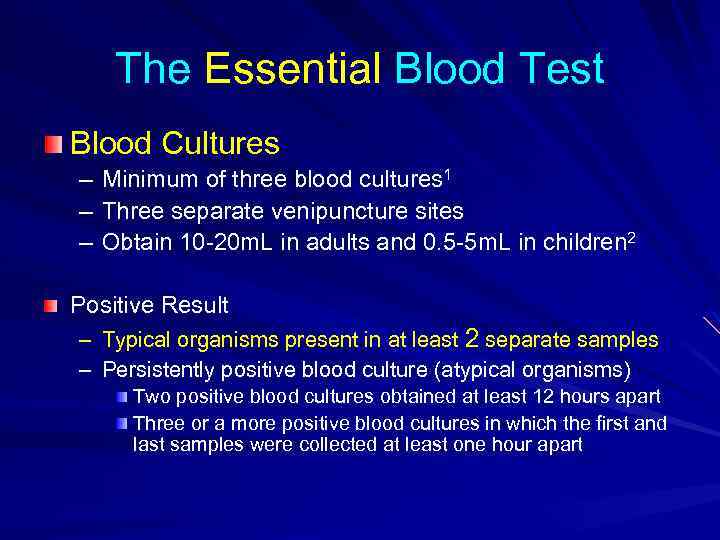
The Essential Blood Test Blood Cultures – – – Minimum of three blood cultures 1 Three separate venipuncture sites Obtain 10 -20 m. L in adults and 0. 5 -5 m. L in children 2 Positive Result – Typical organisms present in at least 2 separate samples – Persistently positive blood culture (atypical organisms) Two positive blood cultures obtained at least 12 hours apart Three or a more positive blood cultures in which the first and last samples were collected at least one hour apart
Additional Labs CBC ESR and CRP Complement levels (C 3, C 4, CH 50) RF Urinalysis Baseline chemistries and coags
Imaging Chest x-ray – Look for multiple focal infiltrates and calcification of heart valves EKG – Rarely diagnostic – Look for evidence of ischemia, conduction delay, and arrhythmias Echocardiography
Indications for Echocardiography Transthoracic echocardiography (TTE) – First line if suspected IE – Native valves Transesophageal echocardiography (TEE) – Prosthetic valves – Intracardiac complications – Inadequate TTE – Fungal or S. aureus or bacteremia
Making the Diagnosis Pelletier and Petersdorf criteria (1977) – Classification scheme of definite, probable, and possible IE – Reasonably specific but lacked sensitivity Von Reyn criteria (1981) – Added “rejected” as a category – Added more clinical criteria – Improved specificity and clinical utility Duke criteria (1994) – Included the role of echocardiography in diagnosis – Added IVDA as a “predisposing heart condition”
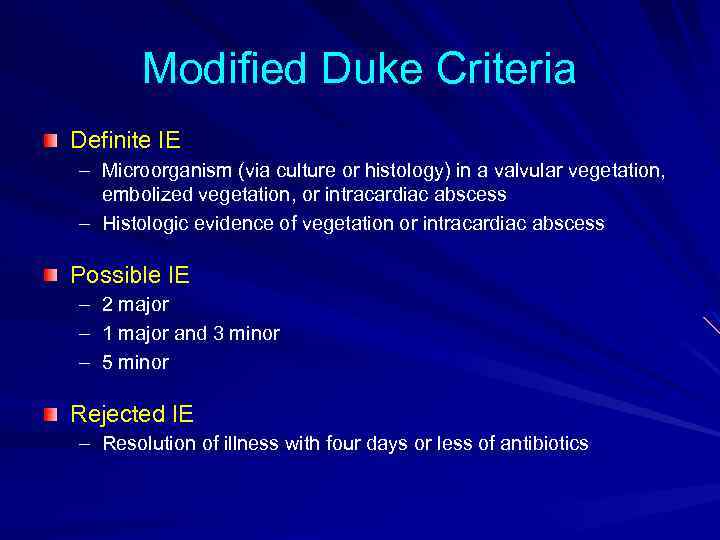
Modified Duke Criteria Definite IE – Microorganism (via culture or histology) in a valvular vegetation, embolized vegetation, or intracardiac abscess – Histologic evidence of vegetation or intracardiac abscess Possible IE – – – 2 major 1 major and 3 minor 5 minor Rejected IE – Resolution of illness with four days or less of antibiotics
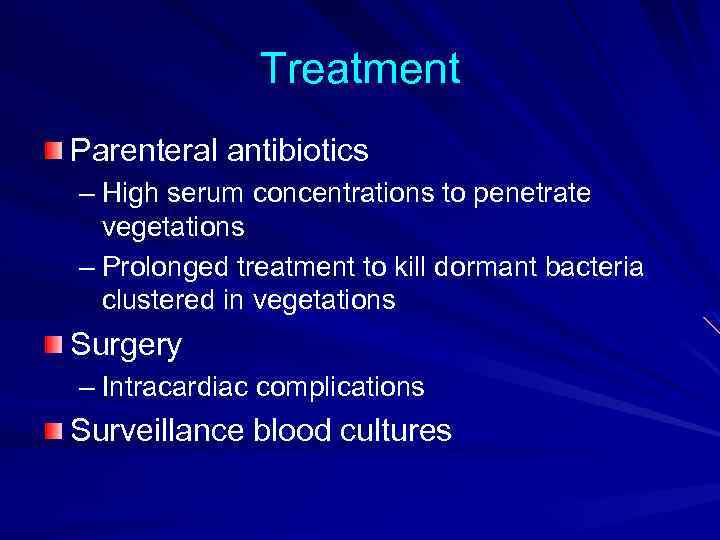
Treatment Parenteral antibiotics – High serum concentrations to penetrate vegetations – Prolonged treatment to kill dormant bacteria clustered in vegetations Surgery – Intracardiac complications Surveillance blood cultures
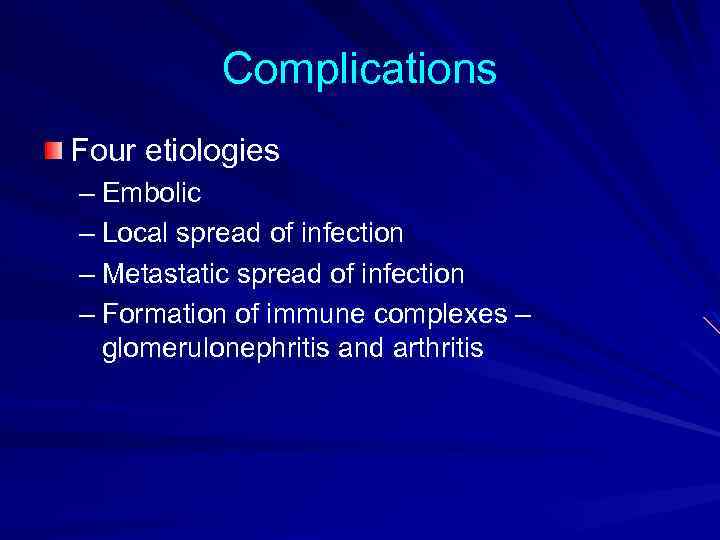
Complications Four etiologies – Embolic – Local spread of infection – Metastatic spread of infection – Formation of immune complexes – glomerulonephritis and arthritis
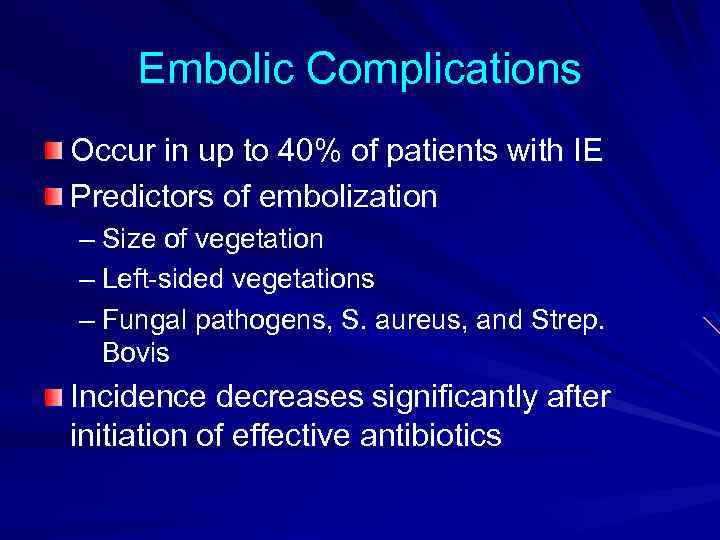
Embolic Complications Occur in up to 40% of patients with IE Predictors of embolization – Size of vegetation – Left-sided vegetations – Fungal pathogens, S. aureus, and Strep. Bovis Incidence decreases significantly after initiation of effective antibiotics
Embolic Complications Stroke Myocardial Infarction – Fragments of valvular vegetation or vegetation -induced stenosis of coronary ostia Ischemic limbs Hypoxia from pulmonary emboli Abdominal pain (splenic or renal infarction)
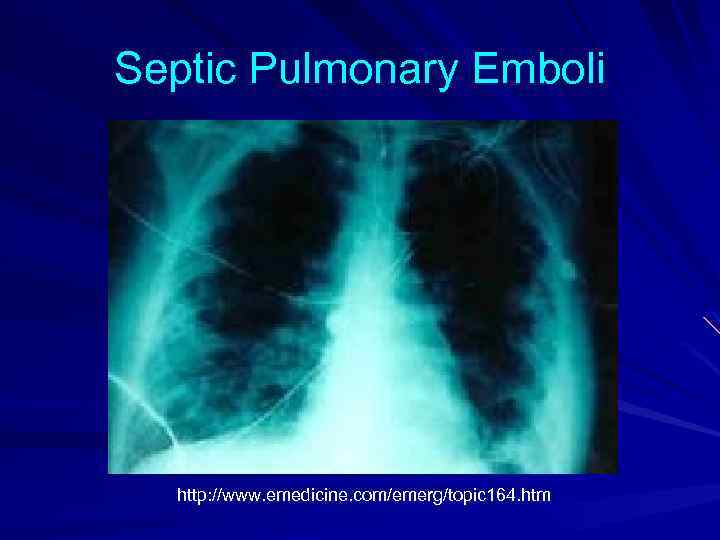
Septic Pulmonary Emboli http: //www. emedicine. com/emerg/topic 164. htm
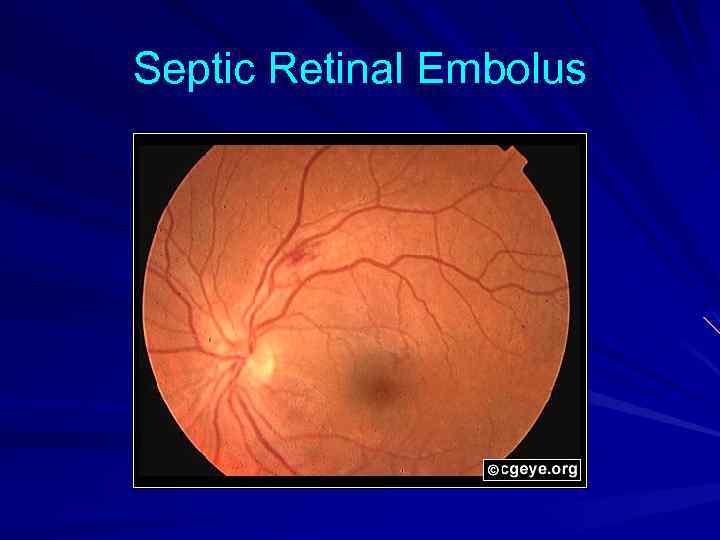
Septic Retinal Embolus
Local Spread of Infection Heart failure – Extensive valvular damage Paravalvular abscess (30 -40%) – Most common in aortic valve, IVDA, and S. aureus – May extend into adjacent conduction tissue causing arrythmias – Higher rates of embolization and mortality Pericarditis Fistulous intracardiac connections
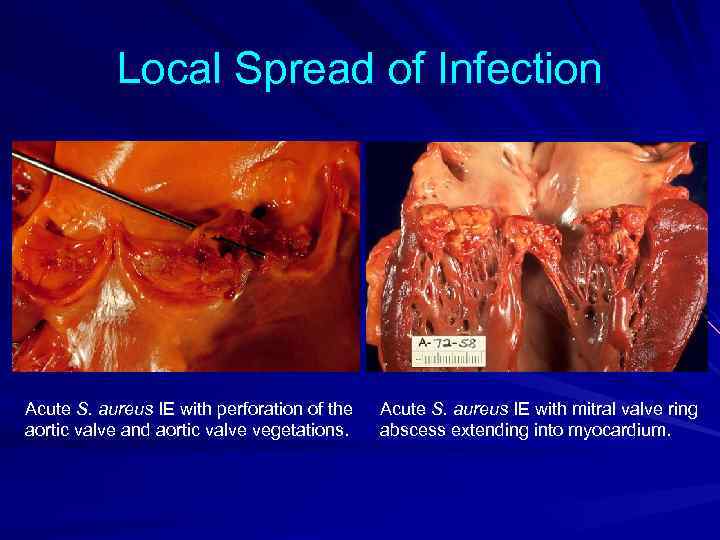
Local Spread of Infection Acute S. aureus IE with perforation of the aortic valve and aortic valve vegetations. Acute S. aureus IE with mitral valve ring abscess extending into myocardium.
Metastatic Spread of Infection Metastatic abscess – Kidneys, spleen, brain, soft tissues Meningitis and/or encephalitis Vertebral osteomyelitis Septic arthritis
Poor Prognostic Factors Female S. aureus Vegetation size Aortic valve Prosthetic valve Older age Diabetes mellitus Low serum albumen Apache II score Heart failure Paravalvular abscess Embolic events
What do these patients have in common? Pt. A: 65 y/o female with PMH of esophageal cancer who presents to clinic with deyhdration, cough, SOB, and “oozing” near her mediport site. Pt. B: 30 y/o male IVDA with a several weeks of fatigue and low grade fevers. Pt. C: 24 y/o female IVDA with severe N/V/abd pain and fevers up to 104 for two weeks. Pt also c/o cough with DOE.

All these patients have MRSA endocarditis!
Patients A, B, and C Try to classify each patient’s IE. Which of these patients likely has acute IE? Which has subacute IE? What was the likely etiology of each patient’s bacteremia?
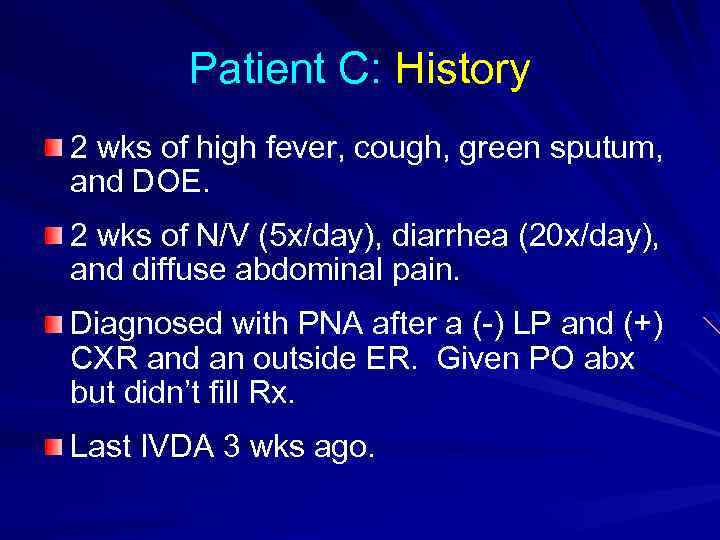
Patient C: History 2 wks of high fever, cough, green sputum, and DOE. 2 wks of N/V (5 x/day), diarrhea (20 x/day), and diffuse abdominal pain. Diagnosed with PNA after a (-) LP and (+) CXR and an outside ER. Given PO abx but didn’t fill Rx. Last IVDA 3 wks ago.
Patient C: History Which symptoms does Patient C have that suggest IE? Does Patient C have any symptoms you can’t explain?
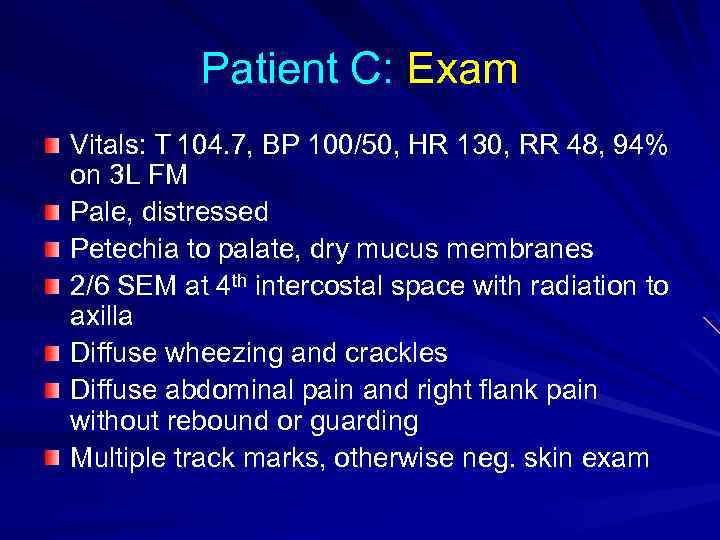
Patient C: Exam Vitals: T 104. 7, BP 100/50, HR 130, RR 48, 94% on 3 L FM Pale, distressed Petechia to palate, dry mucus membranes 2/6 SEM at 4 th intercostal space with radiation to axilla Diffuse wheezing and crackles Diffuse abdominal pain and right flank pain without rebound or guarding Multiple track marks, otherwise neg. skin exam
Patient C: Exam Which signs does Patient C exhibit that suggest IE? Does Patient C have any signs you can’t explain?
Patient C: Labs WBC 20, H/H of 9/27, Platelets 66 p. H 7. 45, p. O 2 54, p. CO 2 27 Albumen 1. 7 UA: 2+ protein, 3+ blood EKG: WNL except sinus tachycardia CXR: enlarged right heart, bilateral infiltrates with nodularity Chest CT: multiple pulmonary abscesses
Patient C: Labs Can you explain these results? Are there other lab values you would like to know?
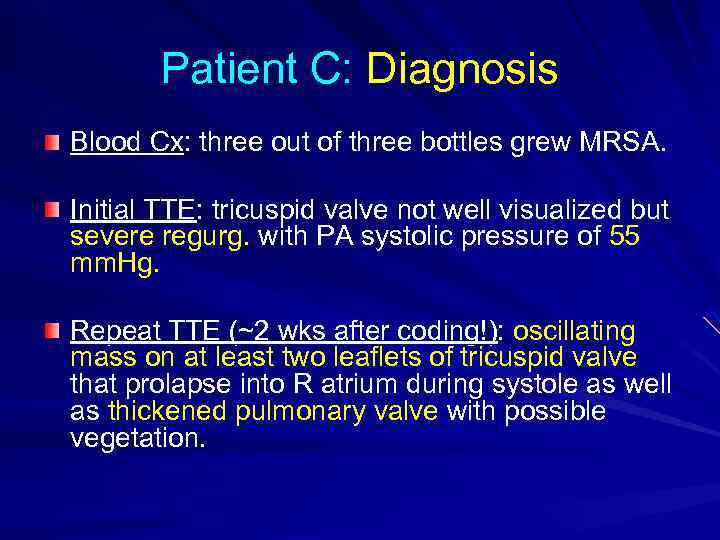
Patient C: Diagnosis Blood Cx: three out of three bottles grew MRSA. Initial TTE: tricuspid valve not well visualized but severe regurg. with PA systolic pressure of 55 mm. Hg. Repeat TTE (~2 wks after coding!): oscillating mass on at least two leaflets of tricuspid valve that prolapse into R atrium during systole as well as thickened pulmonary valve with possible vegetation.
Patient C: Diagnosis What major Duke criteria does Patient C meet? What minor Duke criteria does Patient C meet?
Patient C: Today s/p chest tube with removal 2 separate episodes of respiratory failure with intubation (now extubated) 1 episode of V. fib with cardioversion and a lidocaine gtt. (now weaned off after 1 episode of lidocaine toxicity) CT surgery evaluated the pt and felt she wasn’t a surgical candidate. She is currently still requiring 3 L oxygen and c/o N/V and SOB on telemetry.
Summary IVDA and the elderly are at greatest risk of developing IE. The signs and symptoms of IE are nonspecific and varied. A thorough but timely evaluation (including serial blood cultures, adjunct labs, and an echo) is crucial to accurately diagnose and treat IE. Beware of life-threatening complications.
References Sexton, D. J. , Infective endocarditis: Epidemiology and risk factors. Up To Date (updated September 2, 2005) Brusch, J. L. , Infective Endocarditis. e. Medincine (updated August 15, 2005) www. emedicine. com. Sexton, D. J. , Diagnostic approach to infective endocarditis. Up To Date (updated September 7, 2005) www. uptodate. com. Sexton, D. J. , Corey, G. F. , Infective endocarditis: Historical and Duke Criteria. Up To Date (updated August 29, 2005) www. uptodate. com. Spelman, D. , Sexton D. J. , Complications of infective endocarditis. Up To Date (updated September 7, 2005) Cohen & Powderly: Infectious Diseases, 2 nd ed. , Copyright © 2004 Mosby; pp. 653 -665. Zipes: Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 7 th ed. , Copyright © 2005 Saunders, pp. 1633 -1654.
117.ppt