936bd7126f3eeecafd77c31a905216ae.ppt
- Количество слайдов: 70
 Encephalitis S. Sears, MD
Encephalitis S. Sears, MD
 Herpes simplex virus type 1 Most common cause of fatal sporadic encephalitis HSV infection of the CNS • Immediate CNS invasion – From the trigeminal nerve or olfactory tract – Follows an episode of primary HSV-1 of the oropharynx • CNS invasion after recurrent HSV-1 infection – Represents viral reactivation with subsequent spread • CNS infection without primary or recurrent HSV-1 infection – Represents reactivation of latent HSV in situ within the CNS
Herpes simplex virus type 1 Most common cause of fatal sporadic encephalitis HSV infection of the CNS • Immediate CNS invasion – From the trigeminal nerve or olfactory tract – Follows an episode of primary HSV-1 of the oropharynx • CNS invasion after recurrent HSV-1 infection – Represents viral reactivation with subsequent spread • CNS infection without primary or recurrent HSV-1 infection – Represents reactivation of latent HSV in situ within the CNS
 Pathogenesis Necrosis occurs in the temporal lobe • Direct viral-mediated inflammation – Extent of viral load may be directly related to severity of disease • Indirect immune-mediated CNS damage – Not more common in immunocompromised patients
Pathogenesis Necrosis occurs in the temporal lobe • Direct viral-mediated inflammation – Extent of viral load may be directly related to severity of disease • Indirect immune-mediated CNS damage – Not more common in immunocompromised patients
 Clinical features Focal neurologic findings are acute (< 1 week) • • Altered mentation - level of consciousness Focal cranial nerve deficits Hemiparesis Dysphasia Ataxia Focal seizures Fever Later in the clinical course • • Diminished comprehension Paraphasic (word substitution) spontaneous speech Impaired memory Loss of emotional control
Clinical features Focal neurologic findings are acute (< 1 week) • • Altered mentation - level of consciousness Focal cranial nerve deficits Hemiparesis Dysphasia Ataxia Focal seizures Fever Later in the clinical course • • Diminished comprehension Paraphasic (word substitution) spontaneous speech Impaired memory Loss of emotional control
 Behavioral syndromes Hypomania • • • Inflammation of the temporal - limbic system Elevated mood Excessive animation Decreased need for sleep Inflated self-esteem Hypersexuality Kluver-Bucy syndrome • Psychic blindness • Loss of normal anger and fear responses • Inappropriately oral and sexual States of amnesia
Behavioral syndromes Hypomania • • • Inflammation of the temporal - limbic system Elevated mood Excessive animation Decreased need for sleep Inflated self-esteem Hypersexuality Kluver-Bucy syndrome • Psychic blindness • Loss of normal anger and fear responses • Inappropriately oral and sexual States of amnesia
 Recurrent brainstem encephalitis Upward gaze Facial numbness Signs of involvement • Corticospinal tract • Spinothalamic tract • Cerebrellar pathways
Recurrent brainstem encephalitis Upward gaze Facial numbness Signs of involvement • Corticospinal tract • Spinothalamic tract • Cerebrellar pathways
 Investigations Laboratory • CSF – – – Lymphocytic pleocytosis Increased RBC Elevated protein Normal glucose PCR-diagnostic confirmation Electroencephalogram (EEG) • Nonspecific • Continuous periodic lateralizing epileptiform discharges
Investigations Laboratory • CSF – – – Lymphocytic pleocytosis Increased RBC Elevated protein Normal glucose PCR-diagnostic confirmation Electroencephalogram (EEG) • Nonspecific • Continuous periodic lateralizing epileptiform discharges
 Investigations Imaging • CT – Predominantly unilateral temporal lobe lesions – May be associated with mass effect • MRI – More specific than CT – Brain perfusion studies demonstrate hyperperfusion early in disease
Investigations Imaging • CT – Predominantly unilateral temporal lobe lesions – May be associated with mass effect • MRI – More specific than CT – Brain perfusion studies demonstrate hyperperfusion early in disease
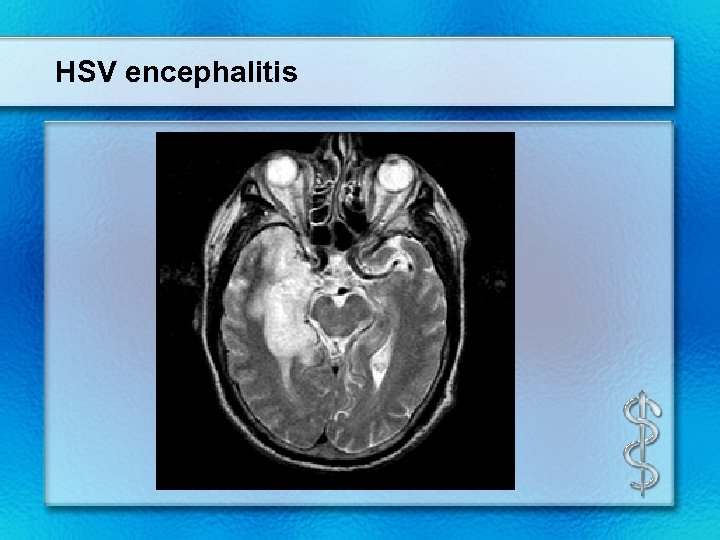 HSV encephalitis
HSV encephalitis
 Differential diagnosis Arthropod viruses Other herpesviruses (CMV, EBV, VZV) Viral Meningitis Brain abscess Post-infectious Reye syndrome Acute disseminated encephalomyelitis Vasculitis Neurosyphilis Primary or secondary malignancy Toxic encephalopathy
Differential diagnosis Arthropod viruses Other herpesviruses (CMV, EBV, VZV) Viral Meningitis Brain abscess Post-infectious Reye syndrome Acute disseminated encephalomyelitis Vasculitis Neurosyphilis Primary or secondary malignancy Toxic encephalopathy
 Diagnosis Gold standard • • PCR Detects HSV DNA in the CSF Positive early in the course of the disease Detectable 2 -4 weeks after the onset of illness If PCR negative • Patient clinically deteriorates on therapy • Brain biopsy • Still the only accurate way for certain diagnosis CSF antigen and antibody determinations not helpful Viral culture rarely positive
Diagnosis Gold standard • • PCR Detects HSV DNA in the CSF Positive early in the course of the disease Detectable 2 -4 weeks after the onset of illness If PCR negative • Patient clinically deteriorates on therapy • Brain biopsy • Still the only accurate way for certain diagnosis CSF antigen and antibody determinations not helpful Viral culture rarely positive
 Treatment Acyclovir 10 mg/kg IV q 8 hrs for 21 days • Infuse slowly and with fluid to prevent crystalluria and renal failure Shorter courses have been associated with relapse Treat early • • • Before loss of consciousness Within 24 hours onset symptoms Glasgow Coma Scale 9 -15 Discontinue therapy • • • Low probability of encephalitis Normal imaging, CSF, mental status Negative CSF PCR Continue therapy • • • High risk patient Abnormal imaging, CSF, mental status, seizures, abnormal EEG Look for alternative why PCR negative – Early testing, antiviral therapy, PCR inhibitors (bloody CSF)
Treatment Acyclovir 10 mg/kg IV q 8 hrs for 21 days • Infuse slowly and with fluid to prevent crystalluria and renal failure Shorter courses have been associated with relapse Treat early • • • Before loss of consciousness Within 24 hours onset symptoms Glasgow Coma Scale 9 -15 Discontinue therapy • • • Low probability of encephalitis Normal imaging, CSF, mental status Negative CSF PCR Continue therapy • • • High risk patient Abnormal imaging, CSF, mental status, seizures, abnormal EEG Look for alternative why PCR negative – Early testing, antiviral therapy, PCR inhibitors (bloody CSF)
 Prognosis Fatality • 70 percent Survivors • Serious neurologic deficits • Significant neuropsychiatric difficulties • Significant neurobehavioral issues
Prognosis Fatality • 70 percent Survivors • Serious neurologic deficits • Significant neuropsychiatric difficulties • Significant neurobehavioral issues
 Rabies Neurotropic RNA viruses • Belong to the family Rhabdoviridae Human infections • From rabid animals through a bite • In developing countries – Dogs account for 90 percent of reported cases • In the United States – Four major animal reservoirs • • Bats Raccoons Skunks Foxes • Unusual transmission – Organ donor died of encephalitis-unknown cause – All recipients were diagnosed with rabies
Rabies Neurotropic RNA viruses • Belong to the family Rhabdoviridae Human infections • From rabid animals through a bite • In developing countries – Dogs account for 90 percent of reported cases • In the United States – Four major animal reservoirs • • Bats Raccoons Skunks Foxes • Unusual transmission – Organ donor died of encephalitis-unknown cause – All recipients were diagnosed with rabies
 Pathogenesis Viruses deposit in peripheral wounds • Exposed skin vs bite through clothing • Face and head vs peripheral site (distance from CNS) • Amount of virus in the saliva • Degree of innervation at the site of bite • Host immunity
Pathogenesis Viruses deposit in peripheral wounds • Exposed skin vs bite through clothing • Face and head vs peripheral site (distance from CNS) • Amount of virus in the saliva • Degree of innervation at the site of bite • Host immunity
 Pathogenesis Retrograde passage of virus • • • Peripheral nerve Dorsal root ganglia To brain Viral replication in CNS • Localizes – – Brainstem Thalamus Basal ganglia Spinal cord Spread from CNS • Heart • Skin • Salivary glands
Pathogenesis Retrograde passage of virus • • • Peripheral nerve Dorsal root ganglia To brain Viral replication in CNS • Localizes – – Brainstem Thalamus Basal ganglia Spinal cord Spread from CNS • Heart • Skin • Salivary glands
 Clinical manifestations Classic forms • Encephalitic – – Hydrophobia Aerophobia Pharyngeal spasms Hyperactivity • Paralytic – Quadriparesis – Mimics Guillain-Barre – Cerebral involvement is late in the course
Clinical manifestations Classic forms • Encephalitic – – Hydrophobia Aerophobia Pharyngeal spasms Hyperactivity • Paralytic – Quadriparesis – Mimics Guillain-Barre – Cerebral involvement is late in the course
 Clinical manifestation Non-classic form • Bat-associated rabies • Neuropathic pain • Sensory/motor deficits • Choreiform movements of the bitten limb • Cranial nerve palsies • Myoclonus • Seizures
Clinical manifestation Non-classic form • Bat-associated rabies • Neuropathic pain • Sensory/motor deficits • Choreiform movements of the bitten limb • Cranial nerve palsies • Myoclonus • Seizures
 Clinical manifestation Five general stages • • • Incubation period Prodrome Acute neurologic syndrome Coma Death
Clinical manifestation Five general stages • • • Incubation period Prodrome Acute neurologic syndrome Coma Death
 General stages of disease Incubation period • • One to three months Can be days to one year Prodrome • • Lasts days-not more than a week Flu-like symptoms – – – – • Malaise Anorexia Irritability Low grade fever Sore throat Headache Nausea Vomiting Viral site of entry – – Paresthesias Pain Pruritus Percussion myoedema
General stages of disease Incubation period • • One to three months Can be days to one year Prodrome • • Lasts days-not more than a week Flu-like symptoms – – – – • Malaise Anorexia Irritability Low grade fever Sore throat Headache Nausea Vomiting Viral site of entry – – Paresthesias Pain Pruritus Percussion myoedema
 General stages of the disease Acute neurologic syndrome • Lasts two to seven days after prodrome • Encephalitic rabies • Paralytic rabies • Atypical rabies Coma • Generalized flaccid paralysis • Respiratory failure • Vascular collapse Death • Two weeks after the onset of coma
General stages of the disease Acute neurologic syndrome • Lasts two to seven days after prodrome • Encephalitic rabies • Paralytic rabies • Atypical rabies Coma • Generalized flaccid paralysis • Respiratory failure • Vascular collapse Death • Two weeks after the onset of coma
 Diagnosis Clinical presentation Investigations • Samples – Saliva • Reverse transcriptase PCR • Viral culture – Neck biopsy • Full thickness • At the hairline • Cutaneous nerve • Follicle • RT/PCR • Immunofluorescence staining for viral antigen – Serum and CSF • Antibody titers – Brain biopsy • RT/PCR • Immunofluorescence staining for viral antigen
Diagnosis Clinical presentation Investigations • Samples – Saliva • Reverse transcriptase PCR • Viral culture – Neck biopsy • Full thickness • At the hairline • Cutaneous nerve • Follicle • RT/PCR • Immunofluorescence staining for viral antigen – Serum and CSF • Antibody titers – Brain biopsy • RT/PCR • Immunofluorescence staining for viral antigen
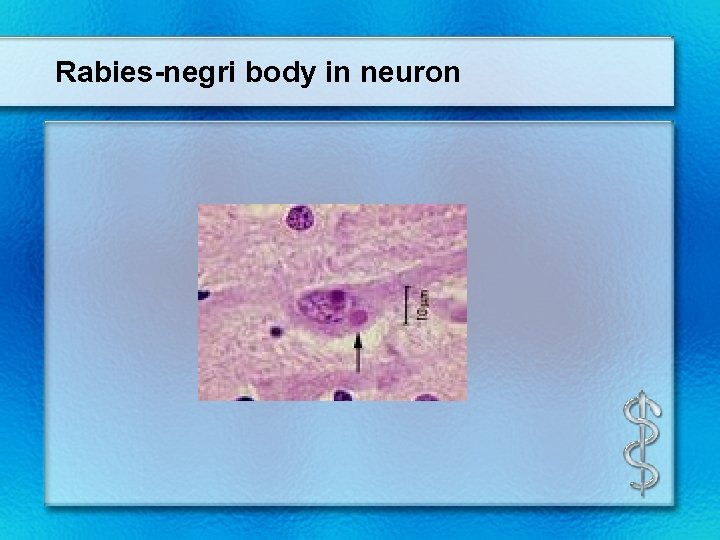 Rabies-negri body in neuron
Rabies-negri body in neuron
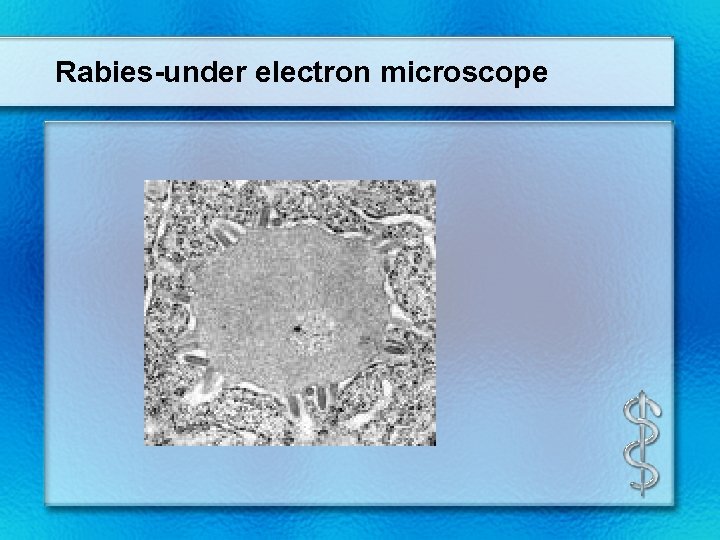 Rabies-under electron microscope
Rabies-under electron microscope
 Treatment Rabies vaccine • • Multiple site intradermal injections To accelerate the immune response Human rabies immune globulin • • Total dose 20 IU/kg Intramuscular Infiltrated around the wound To promote clearance of the infection Ribavirin • Intravenous and intraventricular IFN-alfa • Intravenous and intraventricular Ketamine • • Intravenous infusion Inhibits rabies virus replication Vaccine • For patients not previously vaccinated
Treatment Rabies vaccine • • Multiple site intradermal injections To accelerate the immune response Human rabies immune globulin • • Total dose 20 IU/kg Intramuscular Infiltrated around the wound To promote clearance of the infection Ribavirin • Intravenous and intraventricular IFN-alfa • Intravenous and intraventricular Ketamine • • Intravenous infusion Inhibits rabies virus replication Vaccine • For patients not previously vaccinated
 Prevention Rabies vaccine • Preexposure – – – • Rabies research lab workers Rabies biologics manufacturing workers Veterinarians Animal control workers Wildlife workers Postexposure – Any patient not previously vaccinated
Prevention Rabies vaccine • Preexposure – – – • Rabies research lab workers Rabies biologics manufacturing workers Veterinarians Animal control workers Wildlife workers Postexposure – Any patient not previously vaccinated
 West nile virus encephalitis West nile virus Most widely distributed of all the arboviruses • From the group of flavivirus Distribution • • Now North America Was from Africa Middle East Europe Russia South Asia Australia Carried by wild birds Transmitted • • • By the mosquito bite from the Culex species Transfused blood Transplanted organs
West nile virus encephalitis West nile virus Most widely distributed of all the arboviruses • From the group of flavivirus Distribution • • Now North America Was from Africa Middle East Europe Russia South Asia Australia Carried by wild birds Transmitted • • • By the mosquito bite from the Culex species Transfused blood Transplanted organs
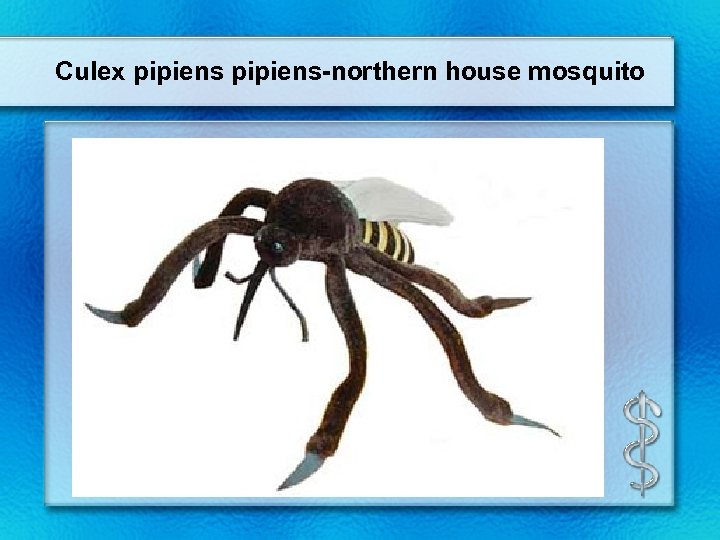 Culex pipiens-northern house mosquito
Culex pipiens-northern house mosquito
 Clinical manifestation Incubation ranges from 2 -14 days West nile fever • • • Fever Malaise Back pain Myalgias Anorexia Persists for 3 -6 days Most frequent symptom • • Maculopapular rash Involves – Chest – Back – arms
Clinical manifestation Incubation ranges from 2 -14 days West nile fever • • • Fever Malaise Back pain Myalgias Anorexia Persists for 3 -6 days Most frequent symptom • • Maculopapular rash Involves – Chest – Back – arms
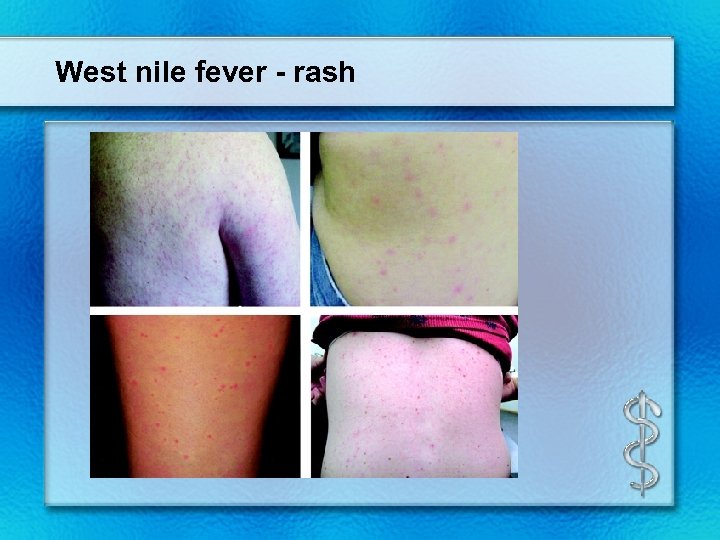 West nile fever - rash
West nile fever - rash
 Neuroinvasive disease Increased risk • • Older age Alcohol abuse Diabetes Immunocompromised Encephalitis • Most common • Presents with – – Headache Fever Nausea Vomiting • Associated with muscle weakness and flaccid paralysis
Neuroinvasive disease Increased risk • • Older age Alcohol abuse Diabetes Immunocompromised Encephalitis • Most common • Presents with – – Headache Fever Nausea Vomiting • Associated with muscle weakness and flaccid paralysis
 Neurologic disease Tremor Myoclonus Parkinsonian features • Rigidity • Postural instability • Bradykinesia Cranial nerve palsies • Facial weakness • Vertigo • Dysarthria • Dysphagia Acute flaccid paralysis syndrome • Anterior horn cell process (like polio) Seizures Cerebellar ataxia Optic neuritis Weakness • Brachial plexopathy • Radiculopathy • Demyelinating peripheral neuropathy
Neurologic disease Tremor Myoclonus Parkinsonian features • Rigidity • Postural instability • Bradykinesia Cranial nerve palsies • Facial weakness • Vertigo • Dysarthria • Dysphagia Acute flaccid paralysis syndrome • Anterior horn cell process (like polio) Seizures Cerebellar ataxia Optic neuritis Weakness • Brachial plexopathy • Radiculopathy • Demyelinating peripheral neuropathy
 Other clinical features Ocular manifestations • Chorioretinitis • Vitritis • Uveitis Rhabdomyolysis Myocarditis Hepatitis Pancreatitis Central diabetes insipidus Palpable purpura
Other clinical features Ocular manifestations • Chorioretinitis • Vitritis • Uveitis Rhabdomyolysis Myocarditis Hepatitis Pancreatitis Central diabetes insipidus Palpable purpura
 Diagnosis Investigations • LP – CSF • • Increased lymphocytes Increased protein Normal glucose Imaging – CT • – Usually normal MRI • Hypertensity – Leptomeninges – Periventricular – Basal ganglia – Thalamus – Caudate nuclei – Brainstem – Spinal cord
Diagnosis Investigations • LP – CSF • • Increased lymphocytes Increased protein Normal glucose Imaging – CT • – Usually normal MRI • Hypertensity – Leptomeninges – Periventricular – Basal ganglia – Thalamus – Caudate nuclei – Brainstem – Spinal cord
 Diagnosis Serology • Ig. M antibody capture enzyme-linked immunosorbent assay • Within first 8 days of illness • Convelescent-phase serum as well • Viral nucleic acid CSF • Ig. M antibody
Diagnosis Serology • Ig. M antibody capture enzyme-linked immunosorbent assay • Within first 8 days of illness • Convelescent-phase serum as well • Viral nucleic acid CSF • Ig. M antibody
 West Nile fever Treatment • Supportive Prognosis • Increased risk – Older age – Immunosuppressed Long-term sequelae
West Nile fever Treatment • Supportive Prognosis • Increased risk – Older age – Immunosuppressed Long-term sequelae
 St. Louis encephalitis Acute mosquito-borne illness Virus is a single-stranded RNA flaviviridae Vector -Culex mosquito Second leading cause of encephalitis after West nile virus Principally occurring • • • Ohio-Mississippi valley Eastern Texas Florida Southeastern Canada Northern Mexico
St. Louis encephalitis Acute mosquito-borne illness Virus is a single-stranded RNA flaviviridae Vector -Culex mosquito Second leading cause of encephalitis after West nile virus Principally occurring • • • Ohio-Mississippi valley Eastern Texas Florida Southeastern Canada Northern Mexico
 St. Louis encephalitis Human infection • • Inoculation of the virus into human host Spread via lymphatics and blood Reaches the choroid plexus Results in lymphocytic encephalitis Most severely affected regions • Hypothalamus • Cerebellum • Cerebral cortex • Basal ganglia • Brainstem • Cervical spinal cord Incubation period • 4 -21 days
St. Louis encephalitis Human infection • • Inoculation of the virus into human host Spread via lymphatics and blood Reaches the choroid plexus Results in lymphocytic encephalitis Most severely affected regions • Hypothalamus • Cerebellum • Cerebral cortex • Basal ganglia • Brainstem • Cervical spinal cord Incubation period • 4 -21 days
 Clinical features Prodromal symptoms • Four to five days • Fever • Severe headache • Photophobia • Nausea • Vomiting • Malaise • Myalgias
Clinical features Prodromal symptoms • Four to five days • Fever • Severe headache • Photophobia • Nausea • Vomiting • Malaise • Myalgias
 Clinical features Neurologic signs • Rapid onset • Alerted sensorium • Tremors – – • Eyelids Tongue Lips Extremities Cranial nerve dysfunction – Unilateral facial motor weakness – Oculomotor dysfunction – Dysarthria • • Myoclonus Opsoclonus Nystagmus Ataxia
Clinical features Neurologic signs • Rapid onset • Alerted sensorium • Tremors – – • Eyelids Tongue Lips Extremities Cranial nerve dysfunction – Unilateral facial motor weakness – Oculomotor dysfunction – Dysarthria • • Myoclonus Opsoclonus Nystagmus Ataxia
 Investigations Laboratory • Increased ALT and CPK • Hyponatremia CSF • Increased lymphocytes • Increased protein • Normal glucose • Negative gram stain Imaging • No specific abnormalities EEG • Diffuse slowing
Investigations Laboratory • Increased ALT and CPK • Hyponatremia CSF • Increased lymphocytes • Increased protein • Normal glucose • Negative gram stain Imaging • No specific abnormalities EEG • Diffuse slowing
 St. Louis encephalitis Diagnosis • Serum • CSF • Ig. M antibodies • Acute and convalescence Treatment • No specific antiviral therapy • Supportive • Interferon alfa-2 B – – Reduced likelihood after first week in hospital Quadriplegia Quadriparesis Respiratory insufficiency
St. Louis encephalitis Diagnosis • Serum • CSF • Ig. M antibodies • Acute and convalescence Treatment • No specific antiviral therapy • Supportive • Interferon alfa-2 B – – Reduced likelihood after first week in hospital Quadriplegia Quadriparesis Respiratory insufficiency
 Outcome Death in the first two weeks • • 20 percent From direct brain injury Poor prognosis • Sustained high fever • Convulsions • Advanced age • Severely depressed state of consciousness Convalescence • Weeks to months • Residual • Headaches • Irritability • Memory deficits • Persistent tremor
Outcome Death in the first two weeks • • 20 percent From direct brain injury Poor prognosis • Sustained high fever • Convulsions • Advanced age • Severely depressed state of consciousness Convalescence • Weeks to months • Residual • Headaches • Irritability • Memory deficits • Persistent tremor
 Prevention No available vaccine Mosquito control
Prevention No available vaccine Mosquito control
 Dengue virus infection Dengue virus • Member of the family flaviviridae • Distribution in every continent • Except Europe and Antarctica Transmitted by • Mosquito-Aedes aegypti • Breed in or close to houses
Dengue virus infection Dengue virus • Member of the family flaviviridae • Distribution in every continent • Except Europe and Antarctica Transmitted by • Mosquito-Aedes aegypti • Breed in or close to houses
 Aedes aegypti mosquito
Aedes aegypti mosquito
 Clinical presentation • Asymptomatic infection • After incubation period 3 -14 days – Self-limited dengue fever – Dengue hemorrhagic fever with shock
Clinical presentation • Asymptomatic infection • After incubation period 3 -14 days – Self-limited dengue fever – Dengue hemorrhagic fever with shock
 Asymptomatic infection • Seen in children under the age of 15 in endemic areas
Asymptomatic infection • Seen in children under the age of 15 in endemic areas
 Dengue fever-classic Acute febrile illness • Headache • Retroorbital pain • Marked muscle and joint pain • Fever-lasts 5 -7 days • Biphasic – Second febrile phase for 1 -2 days Rash- in 2 -5 days after fever Hemorrhagic manifestations • Spontaneous bleeding • Melena • Purpura
Dengue fever-classic Acute febrile illness • Headache • Retroorbital pain • Marked muscle and joint pain • Fever-lasts 5 -7 days • Biphasic – Second febrile phase for 1 -2 days Rash- in 2 -5 days after fever Hemorrhagic manifestations • Spontaneous bleeding • Melena • Purpura
 Classic dengue Physical exam • • • Conjunctival injection Pharyngeal erythema Lymphadenopathy Hepatomegaly Maculopapular rash Laboratory • • Leukopenia Thrombocytopenia Serum aspartate transaminase elevated Virus often found in high concentration in the liver
Classic dengue Physical exam • • • Conjunctival injection Pharyngeal erythema Lymphadenopathy Hepatomegaly Maculopapular rash Laboratory • • Leukopenia Thrombocytopenia Serum aspartate transaminase elevated Virus often found in high concentration in the liver
 Dengue hemorrhagic fever Defined by the World Health Organization Four cardinal features • Fever lasting 2 -7 days • Marked thrombocytopenia (dec platelets) • Increased vascular permeability – – – Plasma leak syndrome Preceded by abdominal pain hypothermia Hemoconcentration Pleural effusion Ascites • Hemorrhagic tendency – – Positive tourniquet test (greater than 20 petechiae) Hematemsis Melena epistaxis
Dengue hemorrhagic fever Defined by the World Health Organization Four cardinal features • Fever lasting 2 -7 days • Marked thrombocytopenia (dec platelets) • Increased vascular permeability – – – Plasma leak syndrome Preceded by abdominal pain hypothermia Hemoconcentration Pleural effusion Ascites • Hemorrhagic tendency – – Positive tourniquet test (greater than 20 petechiae) Hematemsis Melena epistaxis
 Positive tourniquet test
Positive tourniquet test
 Uncommon syndromes Liver failure Encephalopathy Encephalitis Seizures Motor weakness • Mononeuropathies • Polyneuropathies • Guillain-Barre syndrome • Transverse myelitis Myocarditis Cholecystitis Retinal vasculitis
Uncommon syndromes Liver failure Encephalopathy Encephalitis Seizures Motor weakness • Mononeuropathies • Polyneuropathies • Guillain-Barre syndrome • Transverse myelitis Myocarditis Cholecystitis Retinal vasculitis
 Diagnosis Provisional diagnosis can be made on clinical basis Laboratory testing • Acute phase serum plasma for Ig. M immunoassay • If negative repeat in 6 days • At least 10 -14 days later convalescent serum • Both specimens analyzed together • By hemagglutination inhibition Viral detection • Direct culture Detection of plasma leakage • Ultrasound
Diagnosis Provisional diagnosis can be made on clinical basis Laboratory testing • Acute phase serum plasma for Ig. M immunoassay • If negative repeat in 6 days • At least 10 -14 days later convalescent serum • Both specimens analyzed together • By hemagglutination inhibition Viral detection • Direct culture Detection of plasma leakage • Ultrasound
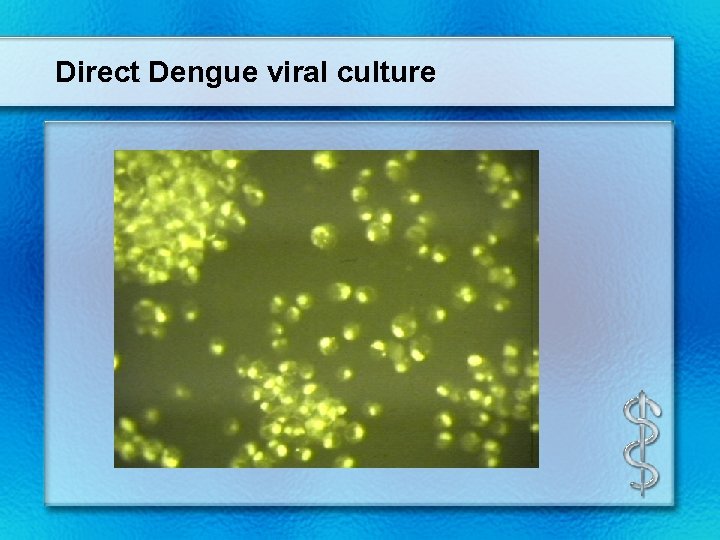 Direct Dengue viral culture
Direct Dengue viral culture
 Treatment No specific therapy-mortality dependent on severity of disease and is variable Directed at Fever • Acetaminophen Bleeding • Transfusion – Red blood cells – Platelets Reversal of hypovolemic shock • IV fluids • Prevention of end organ damage
Treatment No specific therapy-mortality dependent on severity of disease and is variable Directed at Fever • Acetaminophen Bleeding • Transfusion – Red blood cells – Platelets Reversal of hypovolemic shock • IV fluids • Prevention of end organ damage
 Arthropod-borne encephalitides Similarities • All viruses • Family – – Togaviridae Flaviviridae Bunyaviridae Reoviridae • Transmitted to humans via a vector – Mosquito-Culex – Tick • Incubation time after inoculation – From 3 days to two weeks
Arthropod-borne encephalitides Similarities • All viruses • Family – – Togaviridae Flaviviridae Bunyaviridae Reoviridae • Transmitted to humans via a vector – Mosquito-Culex – Tick • Incubation time after inoculation – From 3 days to two weeks
 Arthropod-borne encephalitides Similarities • Prodrome – Flu-like illness • Results in encephalitis • Diagnosis – CSF • • • Lymphocytosis Increased protein Normal glucose Gram stain negative – Ig. M antibody by capture immunoassay in CSF – Demonstrate viral antigen or genome in tissue Treatment – Supportive Prevention – Arthropod • Control • Avoidance
Arthropod-borne encephalitides Similarities • Prodrome – Flu-like illness • Results in encephalitis • Diagnosis – CSF • • • Lymphocytosis Increased protein Normal glucose Gram stain negative – Ig. M antibody by capture immunoassay in CSF – Demonstrate viral antigen or genome in tissue Treatment – Supportive Prevention – Arthropod • Control • Avoidance
 Family-Togaviridae • Eastern equine encephalitis virus • Western equine encephalitis virus • Venezuelan equine encephalitis virus
Family-Togaviridae • Eastern equine encephalitis virus • Western equine encephalitis virus • Venezuelan equine encephalitis virus
 Eastern equine encephalitis virus • Virus distributed North, Central, South America and Caribbean • Virus transmitted by mosquito found in swamp areas • Peak incidence in August and September • Outbreaks along the Atlantic and Gulf coasts • Neurologic deterioration is rapid once symptoms begin • Common – Seizures – Focal neurologic signs • Sequelae – Convulsions – Paralysis – Mental retardation • Mortality is 30%
Eastern equine encephalitis virus • Virus distributed North, Central, South America and Caribbean • Virus transmitted by mosquito found in swamp areas • Peak incidence in August and September • Outbreaks along the Atlantic and Gulf coasts • Neurologic deterioration is rapid once symptoms begin • Common – Seizures – Focal neurologic signs • Sequelae – Convulsions – Paralysis – Mental retardation • Mortality is 30%
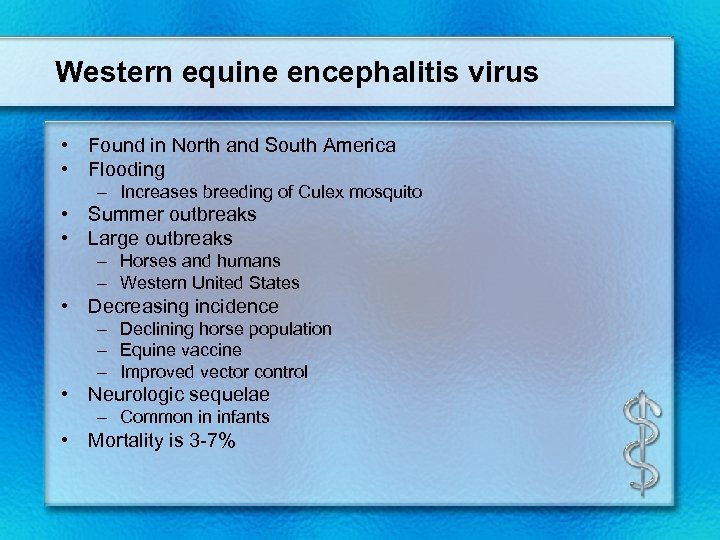 Western equine encephalitis virus • Found in North and South America • Flooding – Increases breeding of Culex mosquito • Summer outbreaks • Large outbreaks – Horses and humans – Western United States • Decreasing incidence – Declining horse population – Equine vaccine – Improved vector control • Neurologic sequelae – Common in infants • Mortality is 3 -7%
Western equine encephalitis virus • Found in North and South America • Flooding – Increases breeding of Culex mosquito • Summer outbreaks • Large outbreaks – Horses and humans – Western United States • Decreasing incidence – Declining horse population – Equine vaccine – Improved vector control • Neurologic sequelae – Common in infants • Mortality is 3 -7%
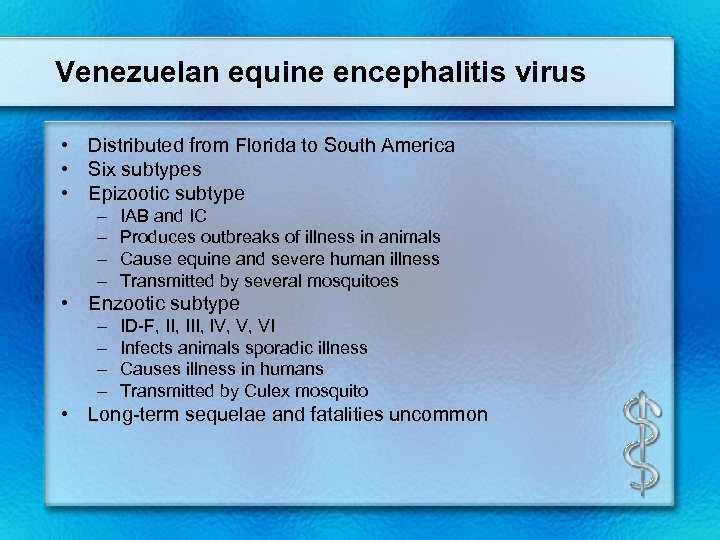 Venezuelan equine encephalitis virus • Distributed from Florida to South America • Six subtypes • Epizootic subtype – – IAB and IC Produces outbreaks of illness in animals Cause equine and severe human illness Transmitted by several mosquitoes • Enzootic subtype – – ID-F, III, IV, V, VI Infects animals sporadic illness Causes illness in humans Transmitted by Culex mosquito • Long-term sequelae and fatalities uncommon
Venezuelan equine encephalitis virus • Distributed from Florida to South America • Six subtypes • Epizootic subtype – – IAB and IC Produces outbreaks of illness in animals Cause equine and severe human illness Transmitted by several mosquitoes • Enzootic subtype – – ID-F, III, IV, V, VI Infects animals sporadic illness Causes illness in humans Transmitted by Culex mosquito • Long-term sequelae and fatalities uncommon
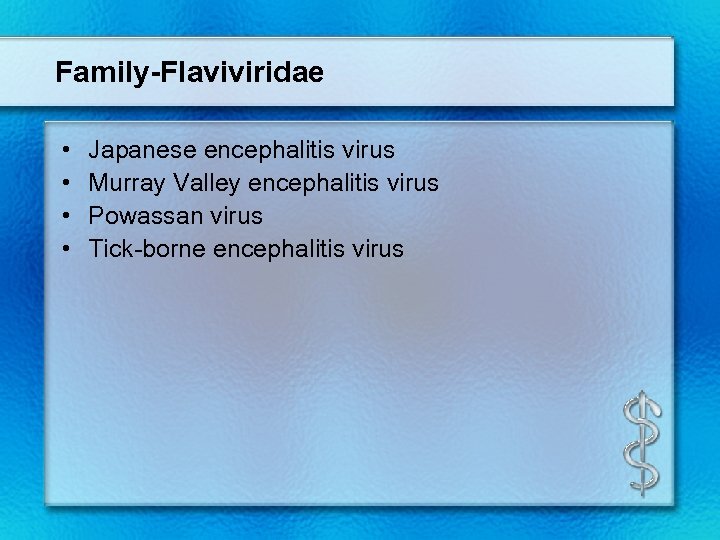 Family-Flaviviridae • • Japanese encephalitis virus Murray Valley encephalitis virus Powassan virus Tick-borne encephalitis virus
Family-Flaviviridae • • Japanese encephalitis virus Murray Valley encephalitis virus Powassan virus Tick-borne encephalitis virus
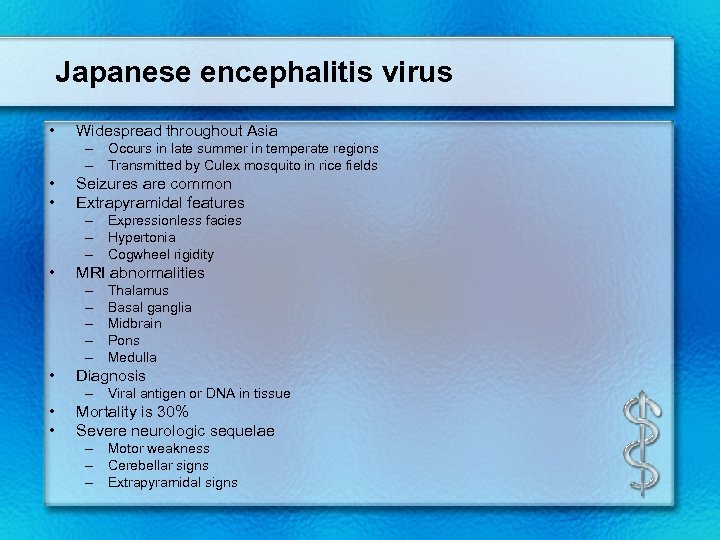 Japanese encephalitis virus • Widespread throughout Asia – Occurs in late summer in temperate regions – Transmitted by Culex mosquito in rice fields • • Seizures are common Extrapyramidal features – Expressionless facies – Hypertonia – Cogwheel rigidity • MRI abnormalities – – – • Thalamus Basal ganglia Midbrain Pons Medulla Diagnosis – Viral antigen or DNA in tissue • • Mortality is 30% Severe neurologic sequelae – Motor weakness – Cerebellar signs – Extrapyramidal signs
Japanese encephalitis virus • Widespread throughout Asia – Occurs in late summer in temperate regions – Transmitted by Culex mosquito in rice fields • • Seizures are common Extrapyramidal features – Expressionless facies – Hypertonia – Cogwheel rigidity • MRI abnormalities – – – • Thalamus Basal ganglia Midbrain Pons Medulla Diagnosis – Viral antigen or DNA in tissue • • Mortality is 30% Severe neurologic sequelae – Motor weakness – Cerebellar signs – Extrapyramidal signs
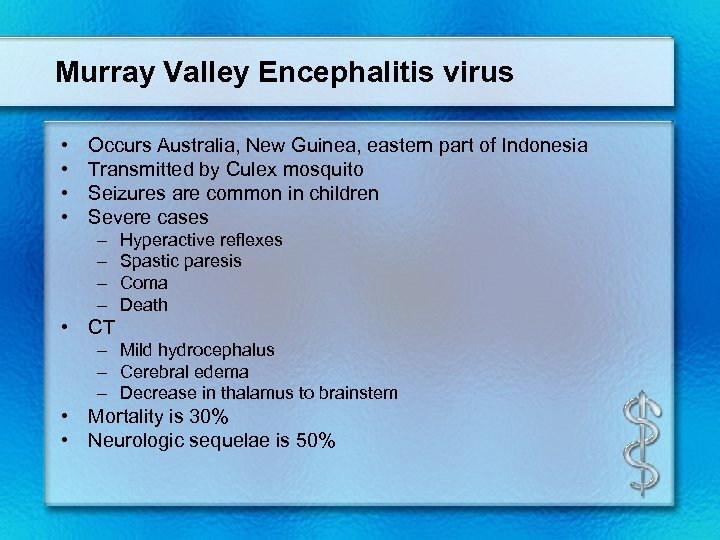 Murray Valley Encephalitis virus • • Occurs Australia, New Guinea, eastern part of Indonesia Transmitted by Culex mosquito Seizures are common in children Severe cases – – Hyperactive reflexes Spastic paresis Coma Death • CT – Mild hydrocephalus – Cerebral edema – Decrease in thalamus to brainstem • Mortality is 30% • Neurologic sequelae is 50%
Murray Valley Encephalitis virus • • Occurs Australia, New Guinea, eastern part of Indonesia Transmitted by Culex mosquito Seizures are common in children Severe cases – – Hyperactive reflexes Spastic paresis Coma Death • CT – Mild hydrocephalus – Cerebral edema – Decrease in thalamus to brainstem • Mortality is 30% • Neurologic sequelae is 50%
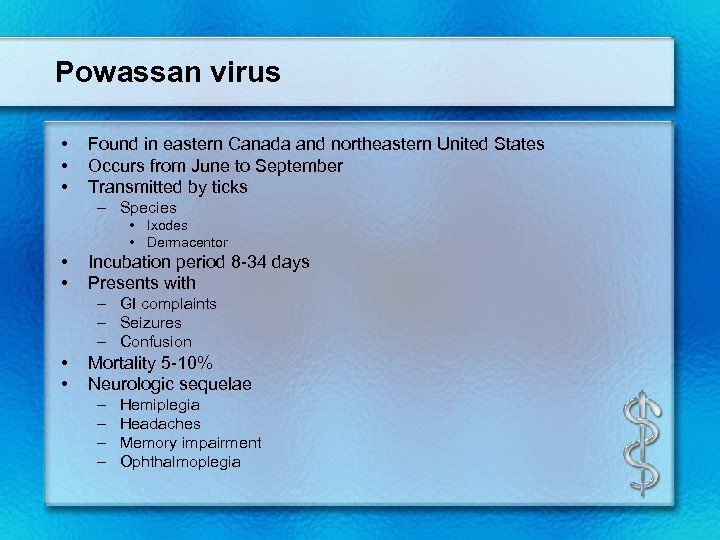 Powassan virus • • • Found in eastern Canada and northeastern United States Occurs from June to September Transmitted by ticks – Species • Ixodes • Dermacentor • • Incubation period 8 -34 days Presents with – GI complaints – Seizures – Confusion • • Mortality 5 -10% Neurologic sequelae – – Hemiplegia Headaches Memory impairment Ophthalmoplegia
Powassan virus • • • Found in eastern Canada and northeastern United States Occurs from June to September Transmitted by ticks – Species • Ixodes • Dermacentor • • Incubation period 8 -34 days Presents with – GI complaints – Seizures – Confusion • • Mortality 5 -10% Neurologic sequelae – – Hemiplegia Headaches Memory impairment Ophthalmoplegia
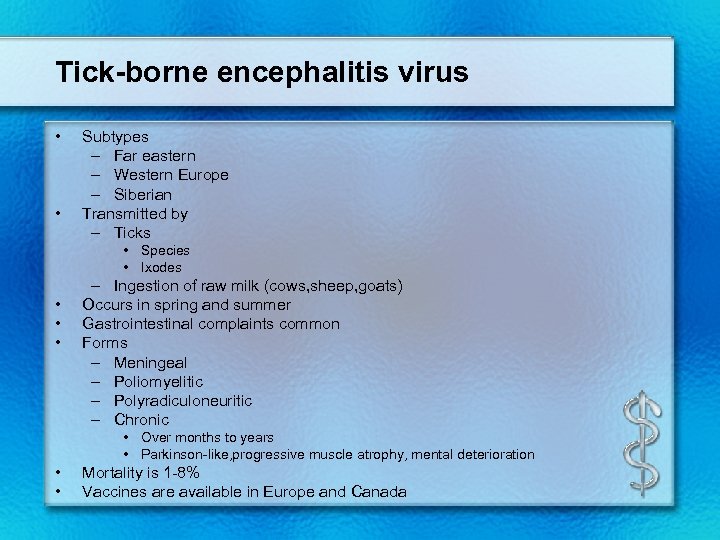 Tick-borne encephalitis virus • • Subtypes – Far eastern – Western Europe – Siberian Transmitted by – Ticks • Species • Ixodes • • • – Ingestion of raw milk (cows, sheep, goats) Occurs in spring and summer Gastrointestinal complaints common Forms – Meningeal – Poliomyelitic – Polyradiculoneuritic – Chronic • Over months to years • Parkinson-like, progressive muscle atrophy, mental deterioration • • Mortality is 1 -8% Vaccines are available in Europe and Canada
Tick-borne encephalitis virus • • Subtypes – Far eastern – Western Europe – Siberian Transmitted by – Ticks • Species • Ixodes • • • – Ingestion of raw milk (cows, sheep, goats) Occurs in spring and summer Gastrointestinal complaints common Forms – Meningeal – Poliomyelitic – Polyradiculoneuritic – Chronic • Over months to years • Parkinson-like, progressive muscle atrophy, mental deterioration • • Mortality is 1 -8% Vaccines are available in Europe and Canada
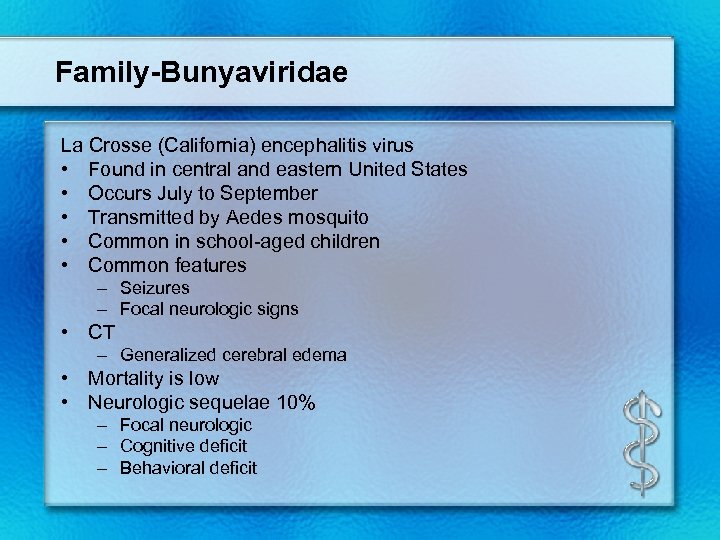 Family-Bunyaviridae La Crosse (California) encephalitis virus • Found in central and eastern United States • Occurs July to September • Transmitted by Aedes mosquito • Common in school-aged children • Common features – Seizures – Focal neurologic signs • CT – Generalized cerebral edema • Mortality is low • Neurologic sequelae 10% – Focal neurologic – Cognitive deficit – Behavioral deficit
Family-Bunyaviridae La Crosse (California) encephalitis virus • Found in central and eastern United States • Occurs July to September • Transmitted by Aedes mosquito • Common in school-aged children • Common features – Seizures – Focal neurologic signs • CT – Generalized cerebral edema • Mortality is low • Neurologic sequelae 10% – Focal neurologic – Cognitive deficit – Behavioral deficit
 Family-Reoviridae Colorado tick fever virus • Found in western United States and Canada • Transmitted by the wood tick • Occurs from March to September • Peaks April to June • Clinical features – Petechial rash – Increasing fatigue • Virus infects bone marrow – Leukopenia common • Prognosis is favorable
Family-Reoviridae Colorado tick fever virus • Found in western United States and Canada • Transmitted by the wood tick • Occurs from March to September • Peaks April to June • Clinical features – Petechial rash – Increasing fatigue • Virus infects bone marrow – Leukopenia common • Prognosis is favorable
 Chandipura virus • • Found in India Transmitted by the sandfly Occurs mostly in children Identified – Electron microscopy – Complement fixation – Neutralizing tests • Rapid onset – Vomiting – Altered mental status – Seizures • Progressive encephalitis • Mortality rate 50%
Chandipura virus • • Found in India Transmitted by the sandfly Occurs mostly in children Identified – Electron microscopy – Complement fixation – Neutralizing tests • Rapid onset – Vomiting – Altered mental status – Seizures • Progressive encephalitis • Mortality rate 50%


