ac9177b22beada9d62195e1b0ce6ffdf.ppt
- Количество слайдов: 53
 EMERGING EVIDENCE AROUND SURGICAL PROPHYLAXIS: “the UPSIDES and the DOWNSIDES”
EMERGING EVIDENCE AROUND SURGICAL PROPHYLAXIS: “the UPSIDES and the DOWNSIDES”
 Part 1: EXAMINING CAUSE AND EFFECT Presented by Wendy Runge, RN, BSc. N, CIC Infection Control Practitioner, Calgary AB
Part 1: EXAMINING CAUSE AND EFFECT Presented by Wendy Runge, RN, BSc. N, CIC Infection Control Practitioner, Calgary AB
 HEALTH CARE ASSOCIATED INFECTIONS (HCAI) • THE BIG 3: SSI, CLI, VAP • PREVENTION RESEARCH HAS IDENTIFIED EVIDENCE-BASED INTERVENTIONS (CLASS 1 EVIDENCE) HOWEVER, “NO GOOD DEED GOES UNPUNISHED” (Clare Boothe Luce)
HEALTH CARE ASSOCIATED INFECTIONS (HCAI) • THE BIG 3: SSI, CLI, VAP • PREVENTION RESEARCH HAS IDENTIFIED EVIDENCE-BASED INTERVENTIONS (CLASS 1 EVIDENCE) HOWEVER, “NO GOOD DEED GOES UNPUNISHED” (Clare Boothe Luce)
 1 2 SURGERY: RISKY OUTCOMES? 3? 4?
1 2 SURGERY: RISKY OUTCOMES? 3? 4?
 SSI AND RISK • RISK INCREASED BY: – PATIENT FACTORS – SURGICAL PROCEDURE • RISK MAY BE DECREASED BY: – COMPLIANCE WITH EVIDENCE-BASED PRACTICE
SSI AND RISK • RISK INCREASED BY: – PATIENT FACTORS – SURGICAL PROCEDURE • RISK MAY BE DECREASED BY: – COMPLIANCE WITH EVIDENCE-BASED PRACTICE
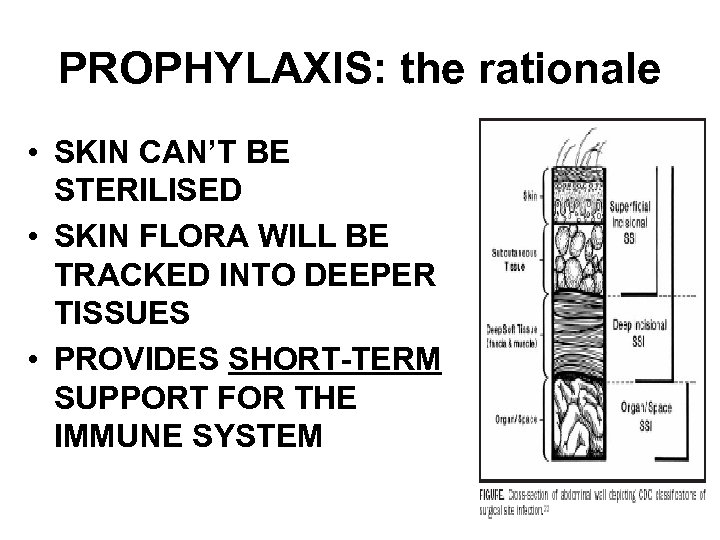 PROPHYLAXIS: the rationale • SKIN CAN’T BE STERILISED • SKIN FLORA WILL BE TRACKED INTO DEEPER TISSUES • PROVIDES SHORT-TERM SUPPORT FOR THE IMMUNE SYSTEM
PROPHYLAXIS: the rationale • SKIN CAN’T BE STERILISED • SKIN FLORA WILL BE TRACKED INTO DEEPER TISSUES • PROVIDES SHORT-TERM SUPPORT FOR THE IMMUNE SYSTEM
 ASSOCIATED RISKS • INCREASED/IMPROPER USE OF ANTIBIOTICS HAS BEEN IMPLICATED IN: – ANTIMICROBIAL RESISTANCE – Clostridium difficile ASSOCIATED DIARRHEA (CDAD)
ASSOCIATED RISKS • INCREASED/IMPROPER USE OF ANTIBIOTICS HAS BEEN IMPLICATED IN: – ANTIMICROBIAL RESISTANCE – Clostridium difficile ASSOCIATED DIARRHEA (CDAD)
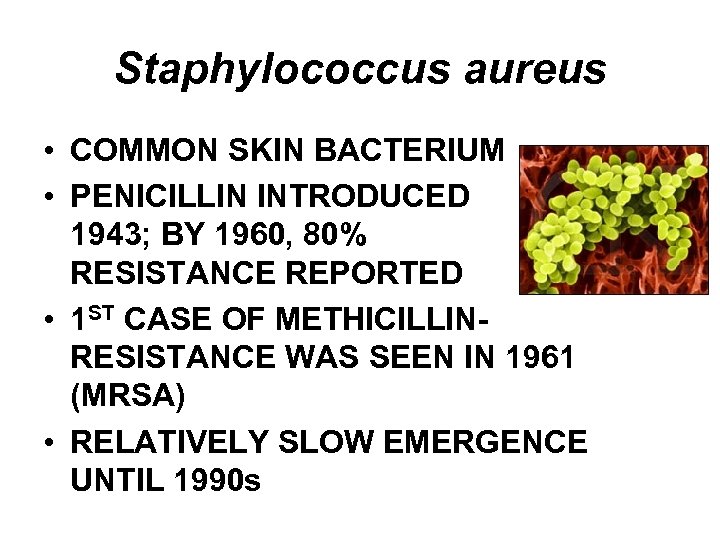 Staphylococcus aureus • COMMON SKIN BACTERIUM • PENICILLIN INTRODUCED 1943; BY 1960, 80% RESISTANCE REPORTED • 1 ST CASE OF METHICILLINRESISTANCE WAS SEEN IN 1961 (MRSA) • RELATIVELY SLOW EMERGENCE UNTIL 1990 s
Staphylococcus aureus • COMMON SKIN BACTERIUM • PENICILLIN INTRODUCED 1943; BY 1960, 80% RESISTANCE REPORTED • 1 ST CASE OF METHICILLINRESISTANCE WAS SEEN IN 1961 (MRSA) • RELATIVELY SLOW EMERGENCE UNTIL 1990 s
 MRSA • ADAPTS AND SHARES GENETIC INFORMATION • ANTIMICROBIAL PRESSURE WILL SELECT FOR RESISTANT STRAINS • RECENT EPIDEMIOLOGY: – COMMUNITY ACQUISITION – POOR ADHERANCE TO HAND HYGIENE IN HEALTH CARE
MRSA • ADAPTS AND SHARES GENETIC INFORMATION • ANTIMICROBIAL PRESSURE WILL SELECT FOR RESISTANT STRAINS • RECENT EPIDEMIOLOGY: – COMMUNITY ACQUISITION – POOR ADHERANCE TO HAND HYGIENE IN HEALTH CARE
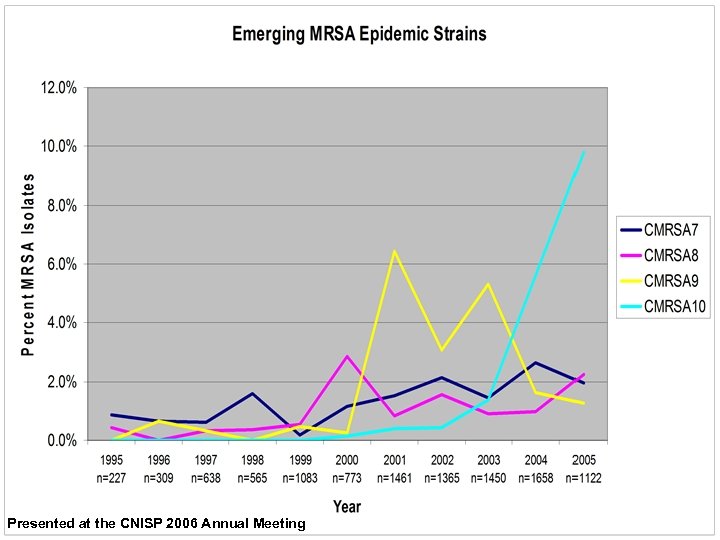 Presented at the CNISP 2006 Annual Meeting
Presented at the CNISP 2006 Annual Meeting
 Clostridium difficile • FOUND IN LOWER BOWEL, CAN BE PART OF RESIDENT FLORA • SPORE-FORMER; SURVIVES FOR EXTENDED PERIODS IN THE ENVIRONMENT • EXCRETES TOXINS WHICH CAN CAUSE TISSUE DAMAGE
Clostridium difficile • FOUND IN LOWER BOWEL, CAN BE PART OF RESIDENT FLORA • SPORE-FORMER; SURVIVES FOR EXTENDED PERIODS IN THE ENVIRONMENT • EXCRETES TOXINS WHICH CAN CAUSE TISSUE DAMAGE
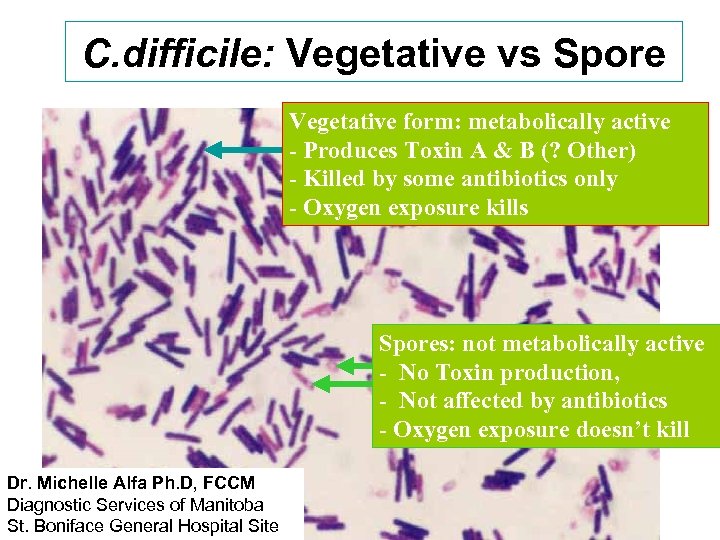 C. difficile: Vegetative vs Spore Vegetative form: metabolically active - Produces Toxin A & B (? Other) - Killed by some antibiotics only - Oxygen exposure kills Spores: not metabolically active - No Toxin production, - Not affected by antibiotics - Oxygen exposure doesn’t kill Dr. Michelle Alfa Ph. D, FCCM Diagnostic Services of Manitoba St. Boniface General Hospital Site
C. difficile: Vegetative vs Spore Vegetative form: metabolically active - Produces Toxin A & B (? Other) - Killed by some antibiotics only - Oxygen exposure kills Spores: not metabolically active - No Toxin production, - Not affected by antibiotics - Oxygen exposure doesn’t kill Dr. Michelle Alfa Ph. D, FCCM Diagnostic Services of Manitoba St. Boniface General Hospital Site
 CDAD (C. difficile associated diarrhea) • ANTIMICROBIAL PRESSURE MAY ALLOW FOR OVERGROWTH • RECOGNIZED AS PRIMARY CAUSE OF ANTIBIOTIC ASSOCIATED DIARRHEA IN 1978 • RECENT EMERGENCE OF NEW STRAINS CAUSING MORE SEVERE DISEASE
CDAD (C. difficile associated diarrhea) • ANTIMICROBIAL PRESSURE MAY ALLOW FOR OVERGROWTH • RECOGNIZED AS PRIMARY CAUSE OF ANTIBIOTIC ASSOCIATED DIARRHEA IN 1978 • RECENT EMERGENCE OF NEW STRAINS CAUSING MORE SEVERE DISEASE
 CDAD • ANTIMICROBIALS MOST OFTEN IMPLICATED: – CLINDAMYCIN – 2 ND AND 3 RD GENERATION CEPHALOSPORINS – FLUOROQUINOLONES
CDAD • ANTIMICROBIALS MOST OFTEN IMPLICATED: – CLINDAMYCIN – 2 ND AND 3 RD GENERATION CEPHALOSPORINS – FLUOROQUINOLONES
 CDAD: MORE TO THE STORY? • 2000 – 2001: LARGEST MULTICENTRE OUTBREAK TO DATE REPORTED IN CALGARY • INVESTIGATIONAL FINDINGS: – FRAIL ELDERLY WITH MULTIPLE COMORBIDITIES – ENVIRONMENTAL CONTAMINATION – UNRESTRICTED USE OF CLINDAMYCIN
CDAD: MORE TO THE STORY? • 2000 – 2001: LARGEST MULTICENTRE OUTBREAK TO DATE REPORTED IN CALGARY • INVESTIGATIONAL FINDINGS: – FRAIL ELDERLY WITH MULTIPLE COMORBIDITIES – ENVIRONMENTAL CONTAMINATION – UNRESTRICTED USE OF CLINDAMYCIN
 CDAD PREVENTION • ANTIMICROBIAL STEWARDSHIP • ELIMINATING ENVIRONMENTAL RESERVOIRS • CONTACT ISOLATION OF SUSPECT AND CONFIRMED CASES
CDAD PREVENTION • ANTIMICROBIAL STEWARDSHIP • ELIMINATING ENVIRONMENTAL RESERVOIRS • CONTACT ISOLATION OF SUSPECT AND CONFIRMED CASES
 PROPHYLAXIS DONE RIGHT! • TARGETS THE ORGANISMS MOST LIKELY AT THE SURGICAL SITE • DELIVERED AT THE OPTIMAL TIME • PROPHYLAXIS VS TREATMENT • “BUGS & DRUGS 2006 ANTIMICROBIAL REFERENCE BOOK”
PROPHYLAXIS DONE RIGHT! • TARGETS THE ORGANISMS MOST LIKELY AT THE SURGICAL SITE • DELIVERED AT THE OPTIMAL TIME • PROPHYLAXIS VS TREATMENT • “BUGS & DRUGS 2006 ANTIMICROBIAL REFERENCE BOOK”
 Paper K-351 ICAAC 2006 Risk Evaluation of Clostridium difficile-Associated Diarrhea Following Antimicrobial Prophylaxis in Patients Undergoing Cardiac, Vascular or Thoracic Surgery in a Tertiary Care Trauma Center D. J. G. Thirion, M. Sc. , Pharm. D. , BCPS Clinical Assistant Professor, Pharmacist Hôpital du Sacré-Cœur de Montréal Faculty of Pharmacy, Université de Montréal
Paper K-351 ICAAC 2006 Risk Evaluation of Clostridium difficile-Associated Diarrhea Following Antimicrobial Prophylaxis in Patients Undergoing Cardiac, Vascular or Thoracic Surgery in a Tertiary Care Trauma Center D. J. G. Thirion, M. Sc. , Pharm. D. , BCPS Clinical Assistant Professor, Pharmacist Hôpital du Sacré-Cœur de Montréal Faculty of Pharmacy, Université de Montréal
 Background n Antimicrobial prophylaxis (AP) is standard of practice for – Cardiac, thoracic, vascular surgery AP decreases surgical site infections (SSIs) n Risk of C. difficile associated diarrhea (CDAD) has been low historically (1. 2%) Harbarth et al. J Hosp Inf 2001; 48: 93 -97 n
Background n Antimicrobial prophylaxis (AP) is standard of practice for – Cardiac, thoracic, vascular surgery AP decreases surgical site infections (SSIs) n Risk of C. difficile associated diarrhea (CDAD) has been low historically (1. 2%) Harbarth et al. J Hosp Inf 2001; 48: 93 -97 n
 Antibiotic prophylaxis protocol n Promoting rational use of antibiotic prophylaxis in surgery can ê Surgical Site Infections ê length of stay ê therapeutic use of antimicrobials Improve costs Thirion DJG et al. Applied Therapeutics. 2004
Antibiotic prophylaxis protocol n Promoting rational use of antibiotic prophylaxis in surgery can ê Surgical Site Infections ê length of stay ê therapeutic use of antimicrobials Improve costs Thirion DJG et al. Applied Therapeutics. 2004
 Appropriate use to decrease risks (pitfalls!) n Adverse reactions – Allergic or toxic reactions – Clostridium difficile (superinfection) (Spencer RC. AAC 1998) n Development of resistance – Vancomycin resistant enterococci (VRE)
Appropriate use to decrease risks (pitfalls!) n Adverse reactions – Allergic or toxic reactions – Clostridium difficile (superinfection) (Spencer RC. AAC 1998) n Development of resistance – Vancomycin resistant enterococci (VRE)
 CDAD n Outbreak in Quebec, Canada associated with new strain (BI/NAP 1 toxinotype III) – Average rate of up to 20 cases/1000 admissions – Increased mortality, morbidity – Increased severity of disease n n Onset of disease closely related to antimicrobial exposure Outbreak of CDAD may expose pts to higher adverse risk with AP Loo V, et al. N Engl J Med 2005; 353: 2442 -9. Mc. Donald LC, et al. N Engl J Med 2005; 353: 2433 -41.
CDAD n Outbreak in Quebec, Canada associated with new strain (BI/NAP 1 toxinotype III) – Average rate of up to 20 cases/1000 admissions – Increased mortality, morbidity – Increased severity of disease n n Onset of disease closely related to antimicrobial exposure Outbreak of CDAD may expose pts to higher adverse risk with AP Loo V, et al. N Engl J Med 2005; 353: 2442 -9. Mc. Donald LC, et al. N Engl J Med 2005; 353: 2433 -41.
 Assessment Adverse outcomes with CDAD may surpass benefits of AP n Purpose: n – To evaluated the risk of CDAD and its complications – Following AP – In cardiac, thoracic, and vascular surgery
Assessment Adverse outcomes with CDAD may surpass benefits of AP n Purpose: n – To evaluated the risk of CDAD and its complications – Following AP – In cardiac, thoracic, and vascular surgery
 Methodology n n n Retrospective cohort study University affiliated tertiary trauma center Pts who underwent – – – n n Cardiac surgery Thoracic surgery Vascular surgery January 1 st 2002 to December 31 st 2004 AP 4 hours prior to and up to 2 hours after beginning of surgery 2 surgeries in the same patient were considered as separate events Pts who did not receive AP were excluded
Methodology n n n Retrospective cohort study University affiliated tertiary trauma center Pts who underwent – – – n n Cardiac surgery Thoracic surgery Vascular surgery January 1 st 2002 to December 31 st 2004 AP 4 hours prior to and up to 2 hours after beginning of surgery 2 surgeries in the same patient were considered as separate events Pts who did not receive AP were excluded
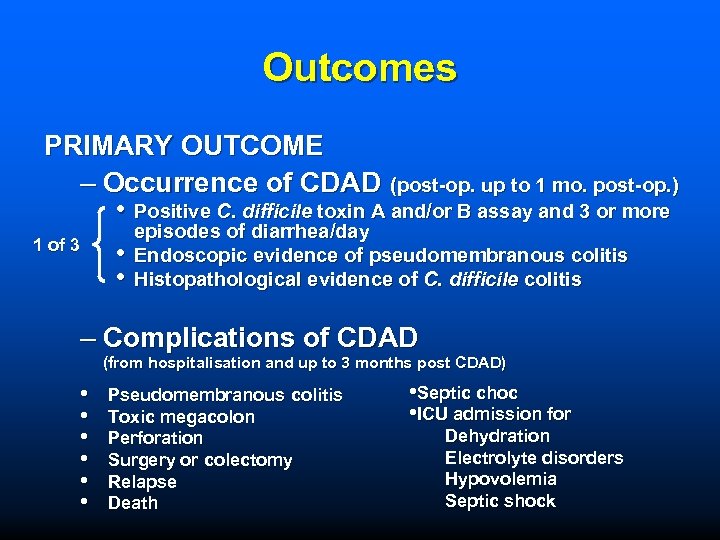 Outcomes PRIMARY OUTCOME – Occurrence of CDAD (post-op. up to 1 mo. post-op. ) • Positive C. difficile toxin A and/or B assay and 3 or more 1 of 3 • • episodes of diarrhea/day Endoscopic evidence of pseudomembranous colitis Histopathological evidence of C. difficile colitis – Complications of CDAD (from hospitalisation and up to 3 months post CDAD) • • • Pseudomembranous colitis Toxic megacolon Perforation Surgery or colectomy Relapse Death • Septic choc • ICU admission for Dehydration Electrolyte disorders Hypovolemia Septic shock
Outcomes PRIMARY OUTCOME – Occurrence of CDAD (post-op. up to 1 mo. post-op. ) • Positive C. difficile toxin A and/or B assay and 3 or more 1 of 3 • • episodes of diarrhea/day Endoscopic evidence of pseudomembranous colitis Histopathological evidence of C. difficile colitis – Complications of CDAD (from hospitalisation and up to 3 months post CDAD) • • • Pseudomembranous colitis Toxic megacolon Perforation Surgery or colectomy Relapse Death • Septic choc • ICU admission for Dehydration Electrolyte disorders Hypovolemia Septic shock
 Outcomes SECONDARY OUTCOME n Risk factors for CDAD n Surgical site infections – Superficial < 30 days post-op – Deep < 30 days post-op < 1 year post-op if material implant
Outcomes SECONDARY OUTCOME n Risk factors for CDAD n Surgical site infections – Superficial < 30 days post-op – Deep < 30 days post-op < 1 year post-op if material implant
 Statistical analysis Rates of CDAD (95% CI) n Risk of complications with CDAD n Rates of SSIs (95% CI) n Logistic regression for influence of different risk factors on the incidence of CDAD (OR, 95% CI) n
Statistical analysis Rates of CDAD (95% CI) n Risk of complications with CDAD n Rates of SSIs (95% CI) n Logistic regression for influence of different risk factors on the incidence of CDAD (OR, 95% CI) n
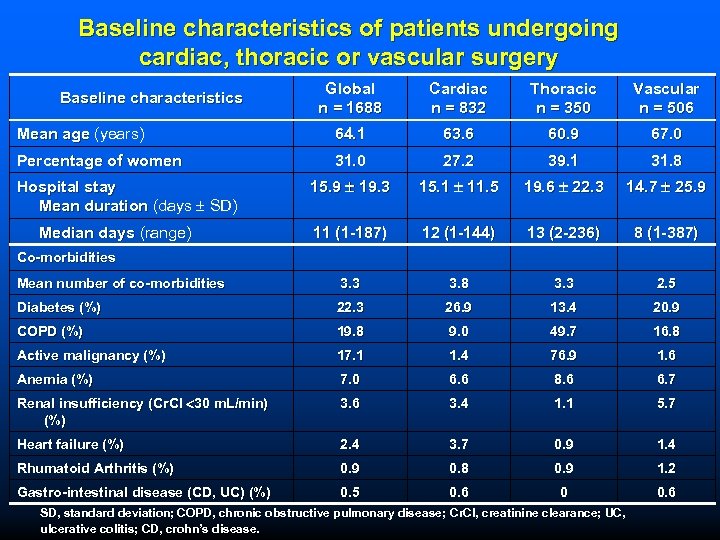 Baseline characteristics of patients undergoing cardiac, thoracic or vascular surgery Global n = 1688 Cardiac n = 832 Thoracic n = 350 Vascular n = 506 Mean age (years) 64. 1 63. 6 60. 9 67. 0 Percentage of women 31. 0 27. 2 39. 1 31. 8 15. 9 19. 3 15. 1 11. 5 19. 6 22. 3 14. 7 25. 9 11 (1 -187) 12 (1 -144) 13 (2 -236) 8 (1 -387) Mean number of co-morbidities 3. 3 3. 8 3. 3 2. 5 Diabetes (%) 22. 3 26. 9 13. 4 20. 9 COPD (%) 19. 8 9. 0 49. 7 16. 8 Active malignancy (%) 17. 1 1. 4 76. 9 1. 6 Anemia (%) 7. 0 6. 6 8. 6 6. 7 Renal insufficiency (Cr. Cl 30 m. L/min) (%) 3. 6 3. 4 1. 1 5. 7 Heart failure (%) 2. 4 3. 7 0. 9 1. 4 Rhumatoid Arthritis (%) 0. 9 0. 8 0. 9 1. 2 Gastro-intestinal disease (CD, UC) (%) 0. 5 0. 6 0 0. 6 Baseline characteristics Hospital stay Mean duration (days SD) Median days (range) Co-morbidities SD, standard deviation; COPD, chronic obstructive pulmonary disease; Cr. Cl, creatinine clearance; UC, Cr. Cl, ulcerative colitis; CD, crohn’s disease.
Baseline characteristics of patients undergoing cardiac, thoracic or vascular surgery Global n = 1688 Cardiac n = 832 Thoracic n = 350 Vascular n = 506 Mean age (years) 64. 1 63. 6 60. 9 67. 0 Percentage of women 31. 0 27. 2 39. 1 31. 8 15. 9 19. 3 15. 1 11. 5 19. 6 22. 3 14. 7 25. 9 11 (1 -187) 12 (1 -144) 13 (2 -236) 8 (1 -387) Mean number of co-morbidities 3. 3 3. 8 3. 3 2. 5 Diabetes (%) 22. 3 26. 9 13. 4 20. 9 COPD (%) 19. 8 9. 0 49. 7 16. 8 Active malignancy (%) 17. 1 1. 4 76. 9 1. 6 Anemia (%) 7. 0 6. 6 8. 6 6. 7 Renal insufficiency (Cr. Cl 30 m. L/min) (%) 3. 6 3. 4 1. 1 5. 7 Heart failure (%) 2. 4 3. 7 0. 9 1. 4 Rhumatoid Arthritis (%) 0. 9 0. 8 0. 9 1. 2 Gastro-intestinal disease (CD, UC) (%) 0. 5 0. 6 0 0. 6 Baseline characteristics Hospital stay Mean duration (days SD) Median days (range) Co-morbidities SD, standard deviation; COPD, chronic obstructive pulmonary disease; Cr. Cl, creatinine clearance; UC, Cr. Cl, ulcerative colitis; CD, crohn’s disease.
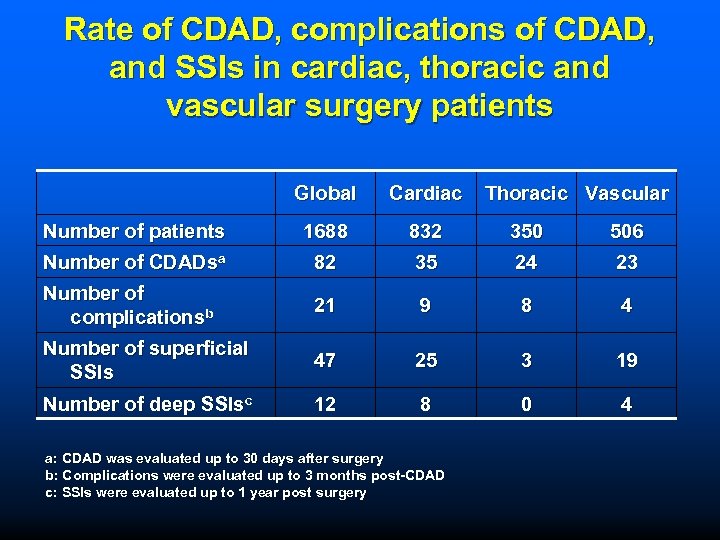 Rate of CDAD, complications of CDAD, and SSIs in cardiac, thoracic and vascular surgery patients Global Cardiac Number of patients 1688 832 350 506 Number of CDADsa 82 35 24 23 Number of complicationsb 21 9 8 4 Number of superficial SSIs 47 25 3 19 Number of deep SSIsc 12 8 0 4 a: CDAD was evaluated up to 30 days after surgery b: Complications were evaluated up to 3 months post-CDAD c: SSIs were evaluated up to 1 year post surgery Thoracic Vascular
Rate of CDAD, complications of CDAD, and SSIs in cardiac, thoracic and vascular surgery patients Global Cardiac Number of patients 1688 832 350 506 Number of CDADsa 82 35 24 23 Number of complicationsb 21 9 8 4 Number of superficial SSIs 47 25 3 19 Number of deep SSIsc 12 8 0 4 a: CDAD was evaluated up to 30 days after surgery b: Complications were evaluated up to 3 months post-CDAD c: SSIs were evaluated up to 1 year post surgery Thoracic Vascular
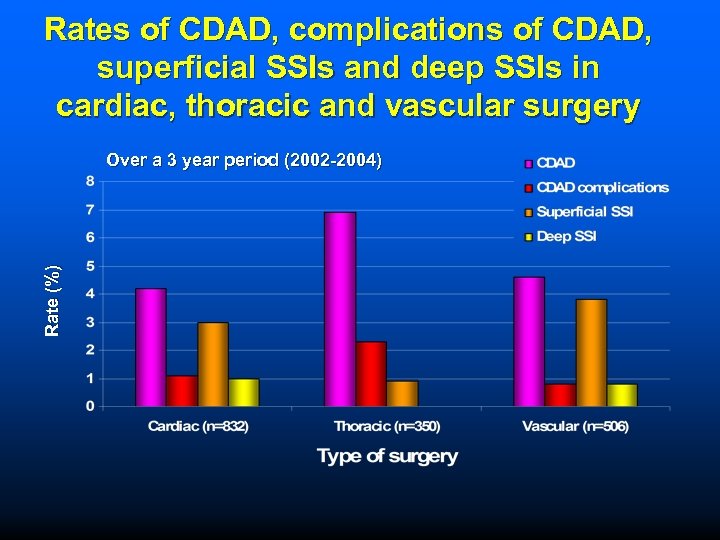 Rates of CDAD, complications of CDAD, superficial SSIs and deep SSIs in cardiac, thoracic and vascular surgery Rate (%) Over a 3 year period (2002 -2004)
Rates of CDAD, complications of CDAD, superficial SSIs and deep SSIs in cardiac, thoracic and vascular surgery Rate (%) Over a 3 year period (2002 -2004)
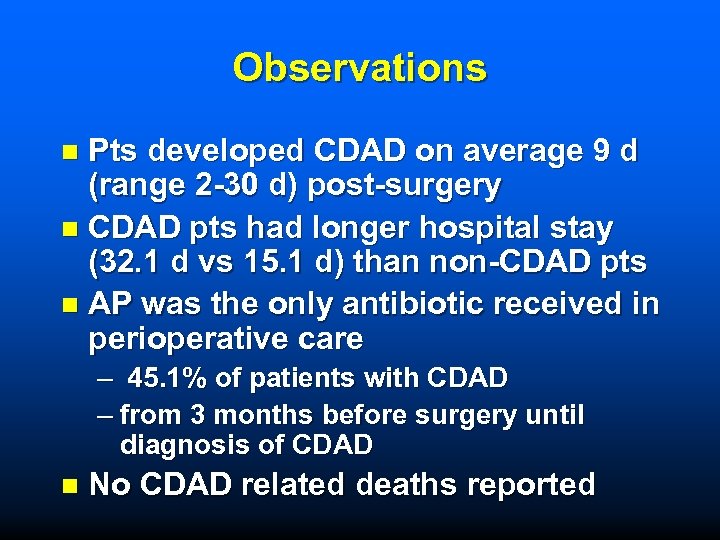 Observations Pts developed CDAD on average 9 d (range 2 -30 d) post-surgery n CDAD pts had longer hospital stay (32. 1 d vs 15. 1 d) than non-CDAD pts n AP was the only antibiotic received in perioperative care n – 45. 1% of patients with CDAD – from 3 months before surgery until diagnosis of CDAD n No CDAD related deaths reported
Observations Pts developed CDAD on average 9 d (range 2 -30 d) post-surgery n CDAD pts had longer hospital stay (32. 1 d vs 15. 1 d) than non-CDAD pts n AP was the only antibiotic received in perioperative care n – 45. 1% of patients with CDAD – from 3 months before surgery until diagnosis of CDAD n No CDAD related deaths reported
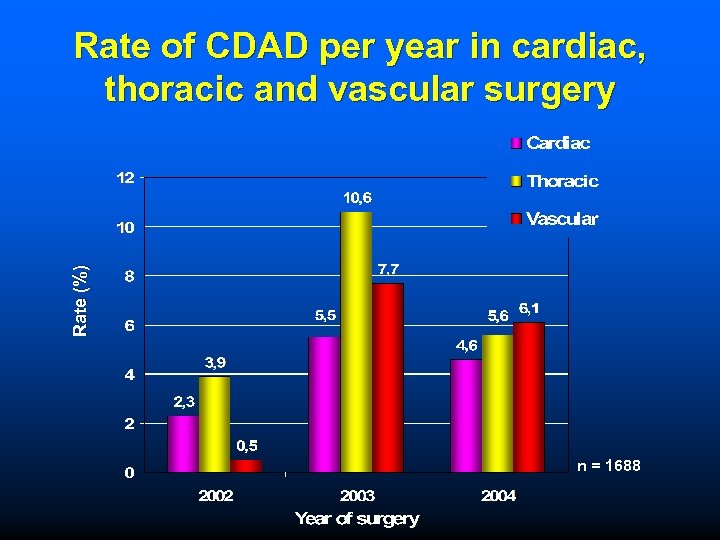 Rate (%) Rate of CDAD per year in cardiac, thoracic and vascular surgery n = 1688
Rate (%) Rate of CDAD per year in cardiac, thoracic and vascular surgery n = 1688
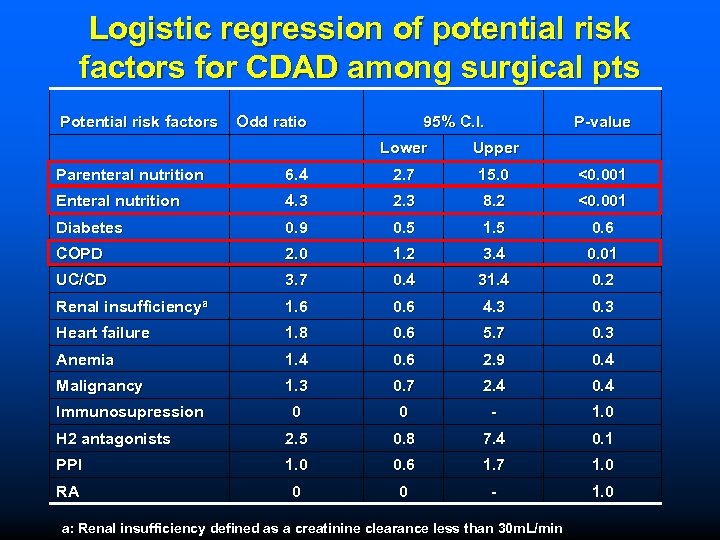 Logistic regression of potential risk factors for CDAD among surgical pts Potential risk factors Odd ratio 95% C. I. P-value Lower Upper Parenteral nutrition 6. 4 2. 7 15. 0 <0. 001 Enteral nutrition 4. 3 2. 3 8. 2 <0. 001 Diabetes 0. 9 0. 5 1. 5 0. 6 COPD 2. 0 1. 2 3. 4 0. 01 UC/CD 3. 7 0. 4 31. 4 0. 2 Renal insufficiencya 1. 6 0. 6 4. 3 0. 3 Heart failure 1. 8 0. 6 5. 7 0. 3 Anemia 1. 4 0. 6 2. 9 0. 4 Malignancy 1. 3 0. 7 2. 4 0 0 - 1. 0 H 2 antagonists 2. 5 0. 8 7. 4 0. 1 PPI 1. 0 0. 6 1. 7 1. 0 RA 0 0 - 1. 0 Immunosupression a: Renal insufficiency defined as a creatinine clearance less than 30 m. L/min
Logistic regression of potential risk factors for CDAD among surgical pts Potential risk factors Odd ratio 95% C. I. P-value Lower Upper Parenteral nutrition 6. 4 2. 7 15. 0 <0. 001 Enteral nutrition 4. 3 2. 3 8. 2 <0. 001 Diabetes 0. 9 0. 5 1. 5 0. 6 COPD 2. 0 1. 2 3. 4 0. 01 UC/CD 3. 7 0. 4 31. 4 0. 2 Renal insufficiencya 1. 6 0. 6 4. 3 0. 3 Heart failure 1. 8 0. 6 5. 7 0. 3 Anemia 1. 4 0. 6 2. 9 0. 4 Malignancy 1. 3 0. 7 2. 4 0 0 - 1. 0 H 2 antagonists 2. 5 0. 8 7. 4 0. 1 PPI 1. 0 0. 6 1. 7 1. 0 RA 0 0 - 1. 0 Immunosupression a: Renal insufficiency defined as a creatinine clearance less than 30 m. L/min
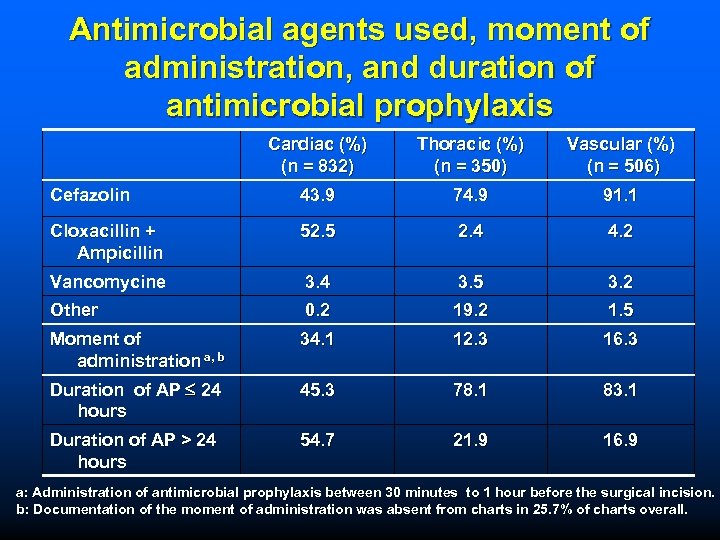 Antimicrobial agents used, moment of administration, and duration of antimicrobial prophylaxis Cardiac (%) (n = 832) Thoracic (%) (n = 350) Vascular (%) (n = 506) Cefazolin 43. 9 74. 9 91. 1 Cloxacillin + Ampicillin 52. 5 2. 4 4. 2 Vancomycine 3. 4 3. 5 3. 2 Other 0. 2 19. 2 1. 5 Moment of administration a, b 34. 1 12. 3 16. 3 Duration of AP 24 hours 45. 3 78. 1 83. 1 Duration of AP > 24 hours 54. 7 21. 9 16. 9 a: Administration of antimicrobial prophylaxis between 30 minutes to 1 hour before the surgical incision. b: Documentation of the moment of administration was absent from charts in 25. 7% of charts overall.
Antimicrobial agents used, moment of administration, and duration of antimicrobial prophylaxis Cardiac (%) (n = 832) Thoracic (%) (n = 350) Vascular (%) (n = 506) Cefazolin 43. 9 74. 9 91. 1 Cloxacillin + Ampicillin 52. 5 2. 4 4. 2 Vancomycine 3. 4 3. 5 3. 2 Other 0. 2 19. 2 1. 5 Moment of administration a, b 34. 1 12. 3 16. 3 Duration of AP 24 hours 45. 3 78. 1 83. 1 Duration of AP > 24 hours 54. 7 21. 9 16. 9 a: Administration of antimicrobial prophylaxis between 30 minutes to 1 hour before the surgical incision. b: Documentation of the moment of administration was absent from charts in 25. 7% of charts overall.
 Discussion n AP is not without risk, especially in epidemic areas of CDAD – AP exposes patients to a high risk of CDAD, which can lead to additional morbidity, length of stay, and hospital costs. – The risk of CDAD with AP use outweighs the benefits in thoracic surgery. n AP in surgeries at low risk of SSIs needs to be reevaluated in the context of CDAD outbreaks. n Confirms other reports that enteral and parenteral nutrition, and COPD are risks for development of CDAD
Discussion n AP is not without risk, especially in epidemic areas of CDAD – AP exposes patients to a high risk of CDAD, which can lead to additional morbidity, length of stay, and hospital costs. – The risk of CDAD with AP use outweighs the benefits in thoracic surgery. n AP in surgeries at low risk of SSIs needs to be reevaluated in the context of CDAD outbreaks. n Confirms other reports that enteral and parenteral nutrition, and COPD are risks for development of CDAD
 Acknowledgements n n n n n David Banon, B. Pharm. 1, 2 Catherine Ferland, B. Pharm. 1, 2 Anik Thibodeau, B. Pharm. 1, 2 Karine Wilhelmy , B. Pharm. 1, 2 Pierre J. Laflamme, MD 1 Gilbert Pichette, MD 1 Thérèse Bigras, M. Sc. Inf. , MBA 1 Anne Filion, B. Pharm. , M. Sc. 1 Lucie Blais, Ph. D. 1, 2 1. 2.
Acknowledgements n n n n n David Banon, B. Pharm. 1, 2 Catherine Ferland, B. Pharm. 1, 2 Anik Thibodeau, B. Pharm. 1, 2 Karine Wilhelmy , B. Pharm. 1, 2 Pierre J. Laflamme, MD 1 Gilbert Pichette, MD 1 Thérèse Bigras, M. Sc. Inf. , MBA 1 Anne Filion, B. Pharm. , M. Sc. 1 Lucie Blais, Ph. D. 1, 2 1. 2.
 Definitions of SSIs n Superficial – < 30 days post-op + – Skin or soft tissue involvment only + – One of the following » Purulent drainage » S/sx of infection and opening of the wound by the surgeon » Diagnosis of superficial surgical site infection » Positive culture from site using aseptic technique
Definitions of SSIs n Superficial – < 30 days post-op + – Skin or soft tissue involvment only + – One of the following » Purulent drainage » S/sx of infection and opening of the wound by the surgeon » Diagnosis of superficial surgical site infection » Positive culture from site using aseptic technique
 Definitions of SSIs n Deep – < 30 days post-op or – < 1 year post-op if material implants + – Infection seems related to surgery + – Affects deep tissue including fascia and muscle + – One of the following » Purulent drainage from deep wound ( but not cavity or organ) » Spontaneous dehiscance opening of the deep wound by the surgeon when T>38°C or localized pain » Abcess or evidence of infection by direct or radiological exam, subsequent surgery, or histopathology » Diagnosis of deep SSI
Definitions of SSIs n Deep – < 30 days post-op or – < 1 year post-op if material implants + – Infection seems related to surgery + – Affects deep tissue including fascia and muscle + – One of the following » Purulent drainage from deep wound ( but not cavity or organ) » Spontaneous dehiscance opening of the deep wound by the surgeon when T>38°C or localized pain » Abcess or evidence of infection by direct or radiological exam, subsequent surgery, or histopathology » Diagnosis of deep SSI
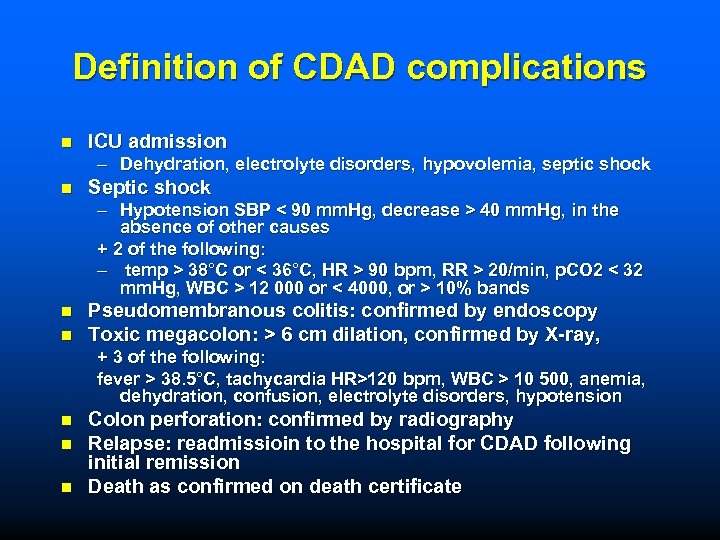 Definition of CDAD complications n ICU admission – Dehydration, electrolyte disorders, hypovolemia, septic shock n Septic shock – Hypotension SBP < 90 mm. Hg, decrease > 40 mm. Hg, in the absence of other causes + 2 of the following: – temp > 38°C or < 36°C, HR > 90 bpm, RR > 20/min, p. CO 2 < 32 mm. Hg, WBC > 12 000 or < 4000, or > 10% bands n n Pseudomembranous colitis: confirmed by endoscopy Toxic megacolon: > 6 cm dilation, confirmed by X-ray, + 3 of the following: fever > 38. 5°C, tachycardia HR>120 bpm, WBC > 10 500, anemia, dehydration, confusion, electrolyte disorders, hypotension n Colon perforation: confirmed by radiography Relapse: readmissioin to the hospital for CDAD following initial remission Death as confirmed on death certificate
Definition of CDAD complications n ICU admission – Dehydration, electrolyte disorders, hypovolemia, septic shock n Septic shock – Hypotension SBP < 90 mm. Hg, decrease > 40 mm. Hg, in the absence of other causes + 2 of the following: – temp > 38°C or < 36°C, HR > 90 bpm, RR > 20/min, p. CO 2 < 32 mm. Hg, WBC > 12 000 or < 4000, or > 10% bands n n Pseudomembranous colitis: confirmed by endoscopy Toxic megacolon: > 6 cm dilation, confirmed by X-ray, + 3 of the following: fever > 38. 5°C, tachycardia HR>120 bpm, WBC > 10 500, anemia, dehydration, confusion, electrolyte disorders, hypotension n Colon perforation: confirmed by radiography Relapse: readmissioin to the hospital for CDAD following initial remission Death as confirmed on death certificate
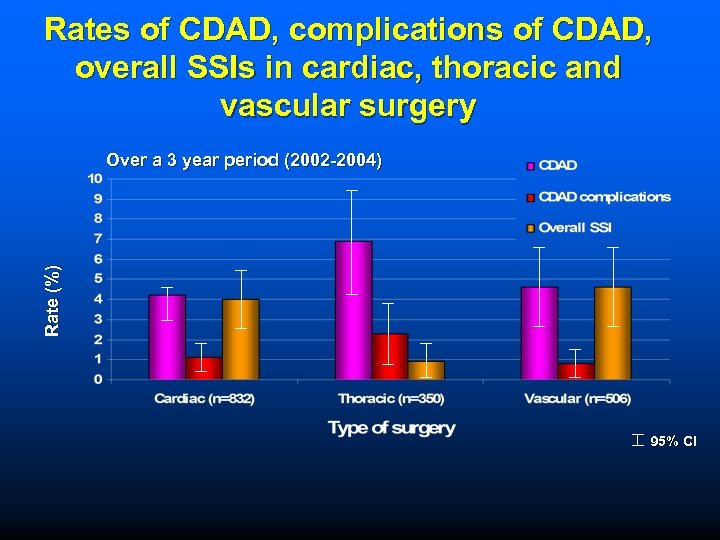 Rates of CDAD, complications of CDAD, overall SSIs in cardiac, thoracic and vascular surgery Rate (%) Over a 3 year period (2002 -2004) 95% CI
Rates of CDAD, complications of CDAD, overall SSIs in cardiac, thoracic and vascular surgery Rate (%) Over a 3 year period (2002 -2004) 95% CI
 Prevention and Change
Prevention and Change
 Questions to consider in Prevention What is the burden of disease Is there any proven benefit from the intervention? If there is, how great is it ? Are there any adverse effects of the intervention? If there are, what are they, how serious are they, and how frequently do they occur? Informed consent.
Questions to consider in Prevention What is the burden of disease Is there any proven benefit from the intervention? If there is, how great is it ? Are there any adverse effects of the intervention? If there are, what are they, how serious are they, and how frequently do they occur? Informed consent.
 Size of benefit Multiple studies actual results varied however OR in ranges of 0. 30 to 0. 5 in antibiotic vs placebo trials Number needed to treat (NNT) approximately 6
Size of benefit Multiple studies actual results varied however OR in ranges of 0. 30 to 0. 5 in antibiotic vs placebo trials Number needed to treat (NNT) approximately 6
 Adverse events - frequency Gillespie 2000 - Cochrane collaboration RR 1. 83 (0. 96 -3. 5) Crabtree TD, et al. Am Surg. 1999. 65: 507 -511. In 16% of post surgical patients with C. difficile colitis the antibiotics were prophylactic. Antibiotic resistance - associated with antibiotic use - ? relevance to a single dose regimen
Adverse events - frequency Gillespie 2000 - Cochrane collaboration RR 1. 83 (0. 96 -3. 5) Crabtree TD, et al. Am Surg. 1999. 65: 507 -511. In 16% of post surgical patients with C. difficile colitis the antibiotics were prophylactic. Antibiotic resistance - associated with antibiotic use - ? relevance to a single dose regimen
 Summary Evidence supports the use of prophylactic antibiotics. the current benefit : harm ratio is favorable However:
Summary Evidence supports the use of prophylactic antibiotics. the current benefit : harm ratio is favorable However:
 Microorganisms are not boring-change is constant The healthcare system should not be boring - change needs to be constant.
Microorganisms are not boring-change is constant The healthcare system should not be boring - change needs to be constant.
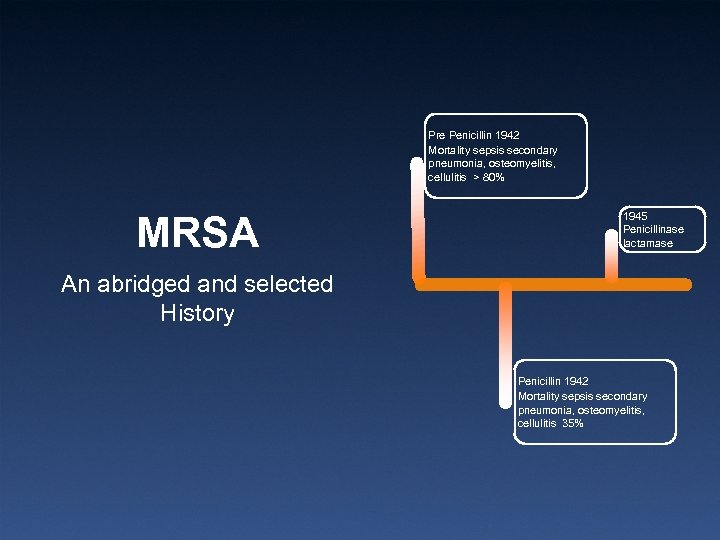 Pre Penicillin 1942 Mortality sepsis secondary pneumonia, osteomyelitis, cellulitis > 80% MRSA 1945 Penicillinase lactamase An abridged and selected History Penicillin 1942 Mortality sepsis secondary pneumonia, osteomyelitis, cellulitis 35%
Pre Penicillin 1942 Mortality sepsis secondary pneumonia, osteomyelitis, cellulitis > 80% MRSA 1945 Penicillinase lactamase An abridged and selected History Penicillin 1942 Mortality sepsis secondary pneumonia, osteomyelitis, cellulitis 35%
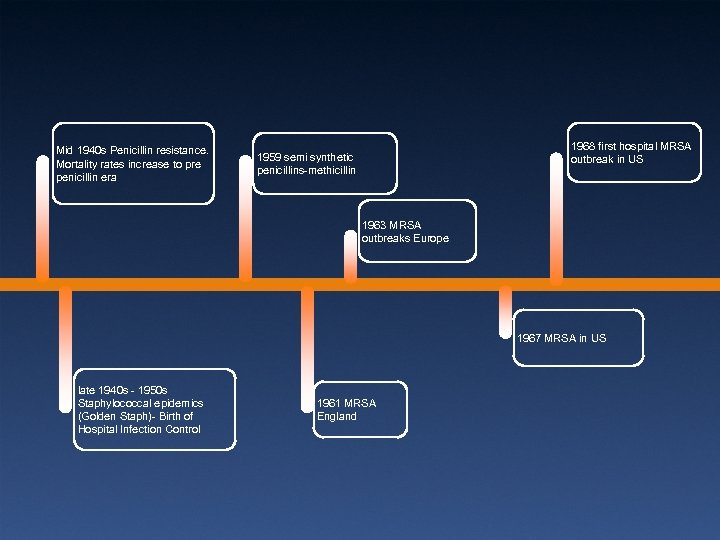 Mid 1940 s Penicillin resistance. Mortality rates increase to pre penicillin era 1968 first hospital MRSA outbreak in US 1959 semi synthetic penicillins-methicillin 1963 MRSA outbreaks Europe 1967 MRSA in US late 1940 s - 1950 s Staphylococcal epidemics (Golden Staph)- Birth of Hospital Infection Control 1961 MRSA England
Mid 1940 s Penicillin resistance. Mortality rates increase to pre penicillin era 1968 first hospital MRSA outbreak in US 1959 semi synthetic penicillins-methicillin 1963 MRSA outbreaks Europe 1967 MRSA in US late 1940 s - 1950 s Staphylococcal epidemics (Golden Staph)- Birth of Hospital Infection Control 1961 MRSA England
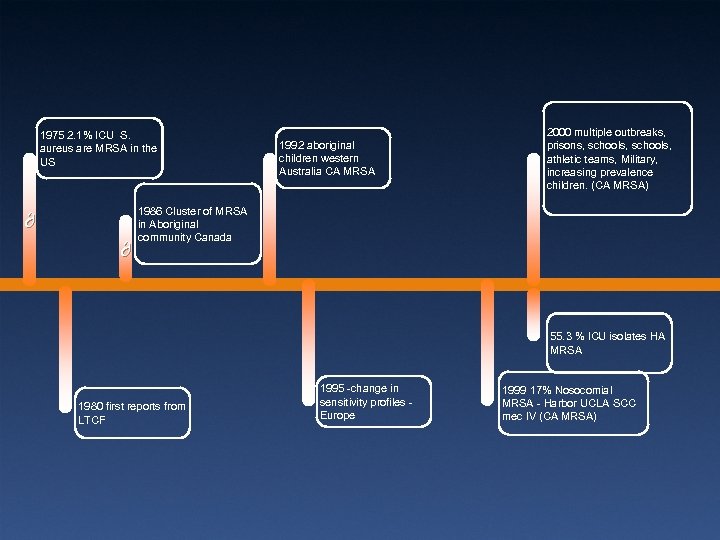 1975 2. 1% ICU S. aureus are MRSA in the US ∂ ∂ 1992 aboriginal children western Australia CA MRSA 2000 multiple outbreaks, prisons, schools, athletic teams, Military, increasing prevalence children. (CA MRSA) 1986 Cluster of MRSA in Aboriginal community Canada 55. 3 % ICU isolates HA MRSA 1980 first reports from LTCF 1995 -change in sensitivity profiles Europe 1999 17% Nosocomial MRSA - Harbor UCLA SCC mec IV (CA MRSA)
1975 2. 1% ICU S. aureus are MRSA in the US ∂ ∂ 1992 aboriginal children western Australia CA MRSA 2000 multiple outbreaks, prisons, schools, athletic teams, Military, increasing prevalence children. (CA MRSA) 1986 Cluster of MRSA in Aboriginal community Canada 55. 3 % ICU isolates HA MRSA 1980 first reports from LTCF 1995 -change in sensitivity profiles Europe 1999 17% Nosocomial MRSA - Harbor UCLA SCC mec IV (CA MRSA)
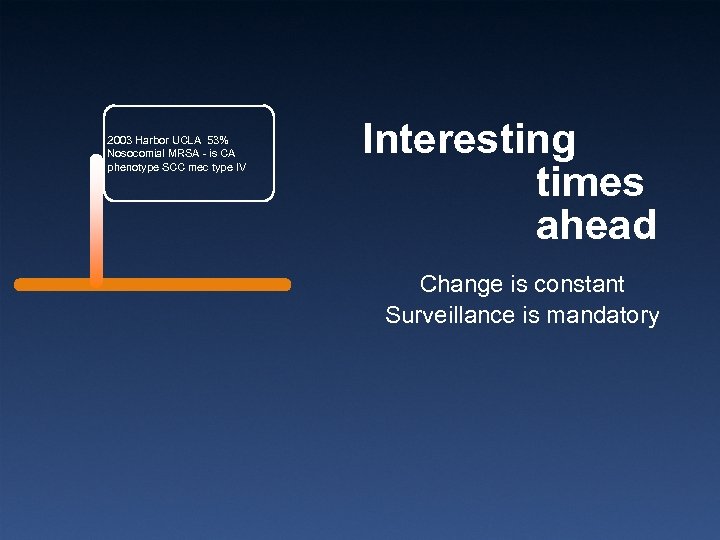 2003 Harbor UCLA 53% Nosocomial MRSA - is CA phenotype SCC mec type IV Interesting times ahead Change is constant Surveillance is mandatory
2003 Harbor UCLA 53% Nosocomial MRSA - is CA phenotype SCC mec type IV Interesting times ahead Change is constant Surveillance is mandatory
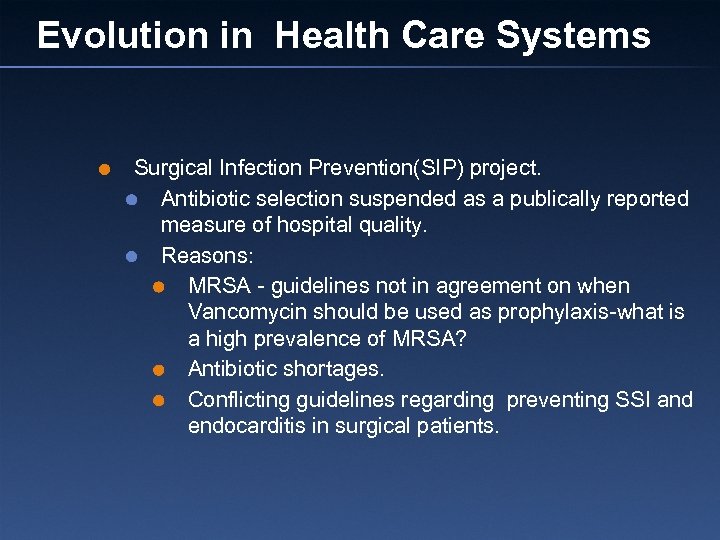 Evolution in Health Care Systems Surgical Infection Prevention(SIP) project. Antibiotic selection suspended as a publically reported measure of hospital quality. Reasons: MRSA - guidelines not in agreement on when Vancomycin should be used as prophylaxis-what is a high prevalence of MRSA? Antibiotic shortages. Conflicting guidelines regarding preventing SSI and endocarditis in surgical patients.
Evolution in Health Care Systems Surgical Infection Prevention(SIP) project. Antibiotic selection suspended as a publically reported measure of hospital quality. Reasons: MRSA - guidelines not in agreement on when Vancomycin should be used as prophylaxis-what is a high prevalence of MRSA? Antibiotic shortages. Conflicting guidelines regarding preventing SSI and endocarditis in surgical patients.
 Remember Organisms change. New knowledge is accumulating. There is an absolute need to monitor what is happening in your institution. There is a need for organizations such as Safer Healthcare Now to regularly review the recommendations in their guidelines.
Remember Organisms change. New knowledge is accumulating. There is an absolute need to monitor what is happening in your institution. There is a need for organizations such as Safer Healthcare Now to regularly review the recommendations in their guidelines.
 Thank you and have a good day
Thank you and have a good day


