a52bd922c18836d0b687ed7c57ce687e.ppt
- Количество слайдов: 91
 Emergency Ultrasound in Trauma Anthony J Weekes MD, RDMS Janet G. Alteveer, MD Sarah Stahmer, MD
Emergency Ultrasound in Trauma Anthony J Weekes MD, RDMS Janet G. Alteveer, MD Sarah Stahmer, MD
 Clinical Case l GR is a 62 y male who hit his right torso when he slipped on an icy sidewalk. He denies head trauma, and can walk without a limp. Two hours later the pain in his lower chest has increased he comes to the ED.
Clinical Case l GR is a 62 y male who hit his right torso when he slipped on an icy sidewalk. He denies head trauma, and can walk without a limp. Two hours later the pain in his lower chest has increased he comes to the ED.
 Clinical Case l PE: BP 116/72, pulse 109, RR 24. l There is a minor abrasion to right lateral chest, which is tender to palpation. Diffuse mild abdominal tenderness. l Meds: Coumadin for irregular heartbeat
Clinical Case l PE: BP 116/72, pulse 109, RR 24. l There is a minor abrasion to right lateral chest, which is tender to palpation. Diffuse mild abdominal tenderness. l Meds: Coumadin for irregular heartbeat
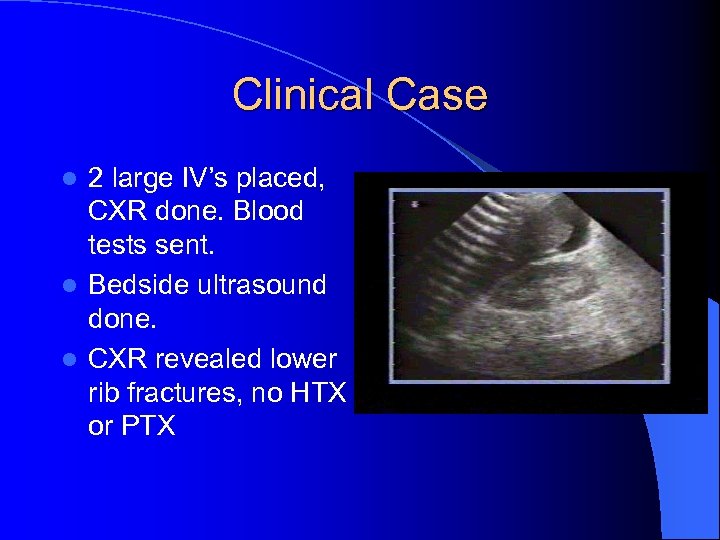 Clinical Case 2 large IV’s placed, CXR done. Blood tests sent. l Bedside ultrasound done. l CXR revealed lower rib fractures, no HTX or PTX l
Clinical Case 2 large IV’s placed, CXR done. Blood tests sent. l Bedside ultrasound done. l CXR revealed lower rib fractures, no HTX or PTX l
 Clinical Case l FFP l He ordered and OR notified. is found to have a liver laceration and 500 cc of blood in the peritoneal cavity.
Clinical Case l FFP l He ordered and OR notified. is found to have a liver laceration and 500 cc of blood in the peritoneal cavity.
 Diagnostic Modalities in Blunt Abdominal Trauma l Diagnostic Peritoneal Lavage (DPL) l CAT Scan l Ultrasound (FAST exam)
Diagnostic Modalities in Blunt Abdominal Trauma l Diagnostic Peritoneal Lavage (DPL) l CAT Scan l Ultrasound (FAST exam)
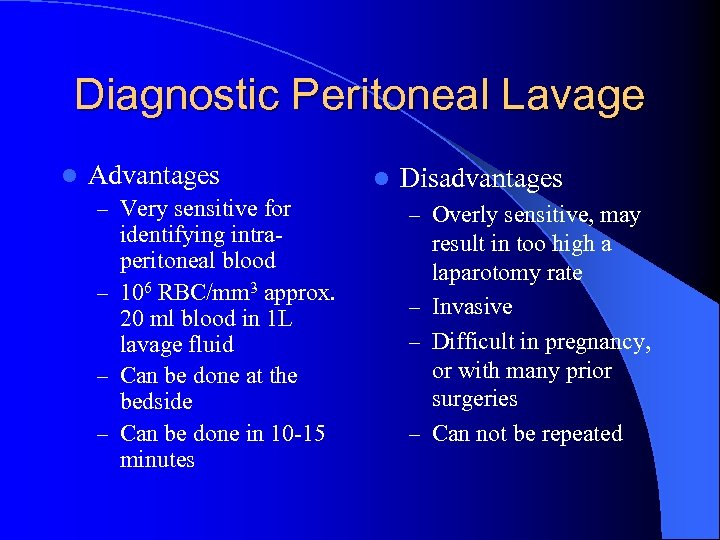 Diagnostic Peritoneal Lavage l Advantages – Very sensitive for identifying intraperitoneal blood – 106 RBC/mm 3 approx. 20 ml blood in 1 L lavage fluid – Can be done at the bedside – Can be done in 10 -15 minutes l Disadvantages – Overly sensitive, may result in too high a laparotomy rate – Invasive – Difficult in pregnancy, or with many prior surgeries – Can not be repeated
Diagnostic Peritoneal Lavage l Advantages – Very sensitive for identifying intraperitoneal blood – 106 RBC/mm 3 approx. 20 ml blood in 1 L lavage fluid – Can be done at the bedside – Can be done in 10 -15 minutes l Disadvantages – Overly sensitive, may result in too high a laparotomy rate – Invasive – Difficult in pregnancy, or with many prior surgeries – Can not be repeated
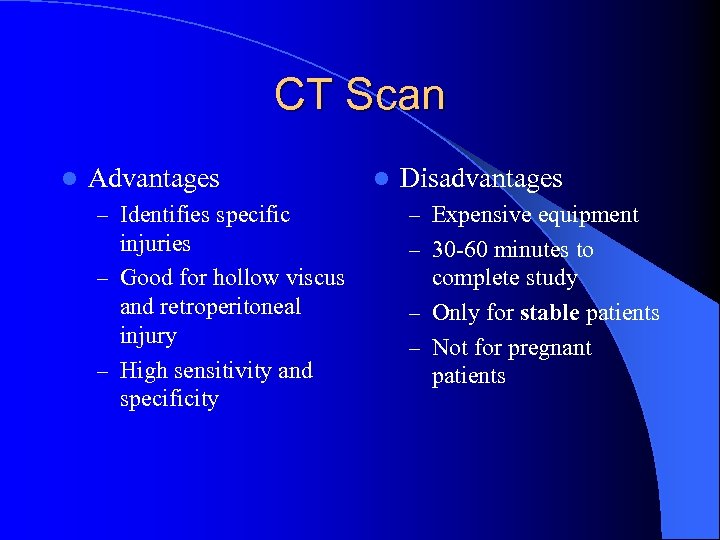 CT Scan l Advantages l Disadvantages – Identifies specific – Expensive equipment injuries – Good for hollow viscus and retroperitoneal injury – High sensitivity and specificity – 30 -60 minutes to complete study – Only for stable patients – Not for pregnant patients
CT Scan l Advantages l Disadvantages – Identifies specific – Expensive equipment injuries – Good for hollow viscus and retroperitoneal injury – High sensitivity and specificity – 30 -60 minutes to complete study – Only for stable patients – Not for pregnant patients
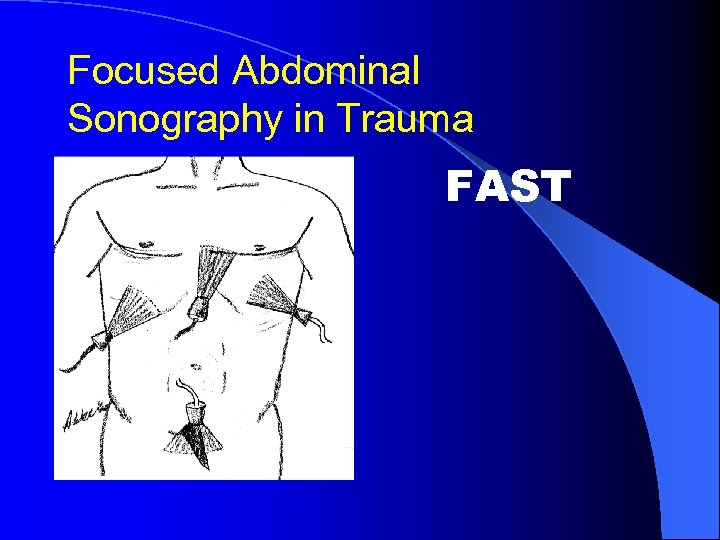 Focused Abdominal Sonography in Trauma FAST
Focused Abdominal Sonography in Trauma FAST
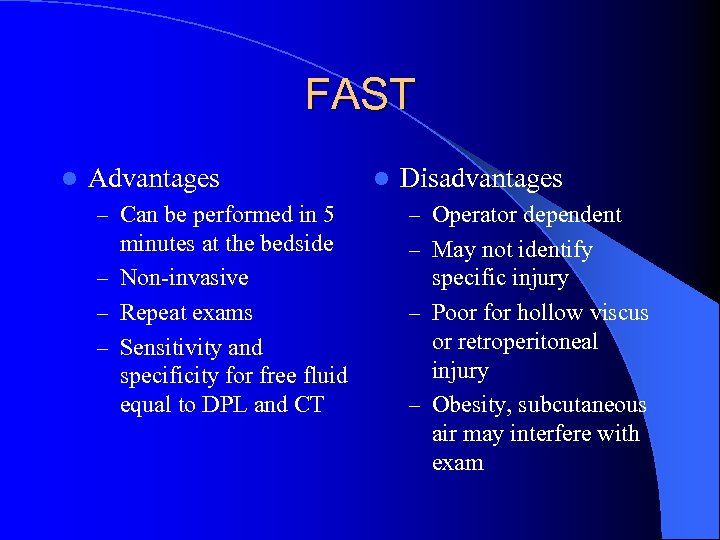 FAST l Advantages l Disadvantages – Can be performed in 5 – Operator dependent minutes at the bedside – Non-invasive – Repeat exams – Sensitivity and specificity for free fluid equal to DPL and CT – May not identify specific injury – Poor for hollow viscus or retroperitoneal injury – Obesity, subcutaneous air may interfere with exam
FAST l Advantages l Disadvantages – Can be performed in 5 – Operator dependent minutes at the bedside – Non-invasive – Repeat exams – Sensitivity and specificity for free fluid equal to DPL and CT – May not identify specific injury – Poor for hollow viscus or retroperitoneal injury – Obesity, subcutaneous air may interfere with exam
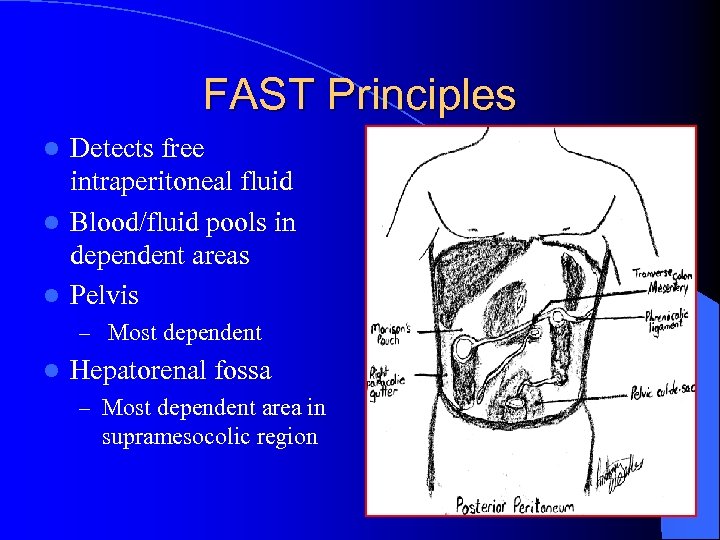 FAST Principles Detects free intraperitoneal fluid l Blood/fluid pools in dependent areas l Pelvis l – Most dependent l Hepatorenal fossa – Most dependent area in supramesocolic region
FAST Principles Detects free intraperitoneal fluid l Blood/fluid pools in dependent areas l Pelvis l – Most dependent l Hepatorenal fossa – Most dependent area in supramesocolic region
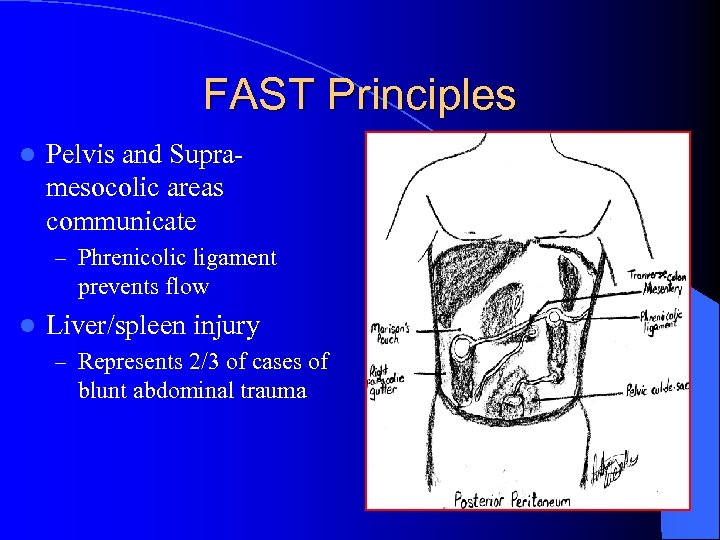 FAST Principles l Pelvis and Supramesocolic areas communicate – Phrenicolic ligament prevents flow l Liver/spleen injury – Represents 2/3 of cases of blunt abdominal trauma
FAST Principles l Pelvis and Supramesocolic areas communicate – Phrenicolic ligament prevents flow l Liver/spleen injury – Represents 2/3 of cases of blunt abdominal trauma
 FAST- principles l Intraperitoneal fluid may be – Blood – Preexisting ascites – Urine – Intestinal contents
FAST- principles l Intraperitoneal fluid may be – Blood – Preexisting ascites – Urine – Intestinal contents
 FAST – limitations l US relatively insensitive for detecting traumatic abdominal organ injury l Fluid may pool at variable rates – Minimum volume for US detection – Multiple views at multiple sites – Serial exams: repeat exam if there is a change in clinical picture l Operator dependent
FAST – limitations l US relatively insensitive for detecting traumatic abdominal organ injury l Fluid may pool at variable rates – Minimum volume for US detection – Multiple views at multiple sites – Serial exams: repeat exam if there is a change in clinical picture l Operator dependent
 Evidence supporting use of FAST l Multiple studies in USA by EM and trauma surgeons l Studies from Europe and Japan l Policy statements by specialty organizations
Evidence supporting use of FAST l Multiple studies in USA by EM and trauma surgeons l Studies from Europe and Japan l Policy statements by specialty organizations
 Emergency department ultrasound in the evaluation of blunt abdominal trauma. Jehle, D. , et al, Am J Emerg Med, 1993 – Single view of Morison’s pouch in 44 patients – Performed by physicians after 2 weeks training – US compared to DPL and laparotomy – Sensitivity 81. 8% – Specificity 93. 9%
Emergency department ultrasound in the evaluation of blunt abdominal trauma. Jehle, D. , et al, Am J Emerg Med, 1993 – Single view of Morison’s pouch in 44 patients – Performed by physicians after 2 weeks training – US compared to DPL and laparotomy – Sensitivity 81. 8% – Specificity 93. 9%
 Trauma surgical study l A prospective study of surgeon- performed ultrasound as the primary adjuvant modality of injured patient assessment. 1994 Rozycki et al. l N=358 patients l Outcomes used: US detection of hemoperitoneum/pericardial effusion
Trauma surgical study l A prospective study of surgeon- performed ultrasound as the primary adjuvant modality of injured patient assessment. 1994 Rozycki et al. l N=358 patients l Outcomes used: US detection of hemoperitoneum/pericardial effusion
 Results l 53/358 (15%) patients w/ free fluid on “gold standard” l All patients: Sens 81. 5%, spec 99. 7% l Blunt trauma: Sens 78. 6%, spec 100% l PPV 98. 1%, NPV 96. 2% l Overall accuracy was 96. 5% for detection of hemoperitoneum or pericardium
Results l 53/358 (15%) patients w/ free fluid on “gold standard” l All patients: Sens 81. 5%, spec 99. 7% l Blunt trauma: Sens 78. 6%, spec 100% l PPV 98. 1%, NPV 96. 2% l Overall accuracy was 96. 5% for detection of hemoperitoneum or pericardium
 Trauma Study l Rozycki G, et al 1998 Surgeon-performed ultrasound for the assessment of truncal injuries. Lessons learned from 1540 patients l FAST exam on patients with precordial or transthoracic wounds or blunt abdominal trauma
Trauma Study l Rozycki G, et al 1998 Surgeon-performed ultrasound for the assessment of truncal injuries. Lessons learned from 1540 patients l FAST exam on patients with precordial or transthoracic wounds or blunt abdominal trauma
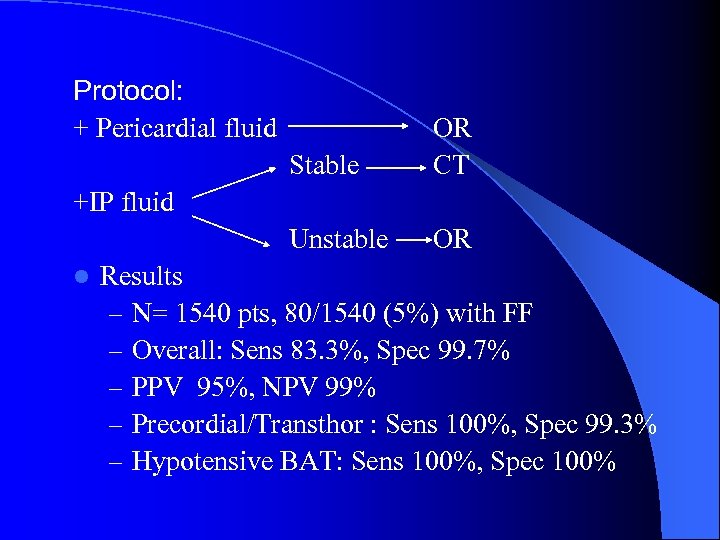 Protocol: + Pericardial fluid Stable OR CT Unstable OR +IP fluid l Results – N= 1540 pts, 80/1540 (5%) with FF – Overall: Sens 83. 3%, Spec 99. 7% – PPV 95%, NPV 99% – Precordial/Transthor : Sens 100%, Spec 99. 3% – Hypotensive BAT: Sens 100%, Spec 100%
Protocol: + Pericardial fluid Stable OR CT Unstable OR +IP fluid l Results – N= 1540 pts, 80/1540 (5%) with FF – Overall: Sens 83. 3%, Spec 99. 7% – PPV 95%, NPV 99% – Precordial/Transthor : Sens 100%, Spec 99. 3% – Hypotensive BAT: Sens 100%, Spec 100%
 FAST – Specialty Societies Established clinical role in Europe, Australia, Japan, Israel l German Surgical Society requires candidates’ proficiency in ultrasound l United States l – US in ATLS – US policies by frontline specialties l l American College of Surgeons ACEP, SAEM & AAEM
FAST – Specialty Societies Established clinical role in Europe, Australia, Japan, Israel l German Surgical Society requires candidates’ proficiency in ultrasound l United States l – US in ATLS – US policies by frontline specialties l l American College of Surgeons ACEP, SAEM & AAEM
 FAST Perform during – Resuscitation – Physical exam – Stabilization
FAST Perform during – Resuscitation – Physical exam – Stabilization
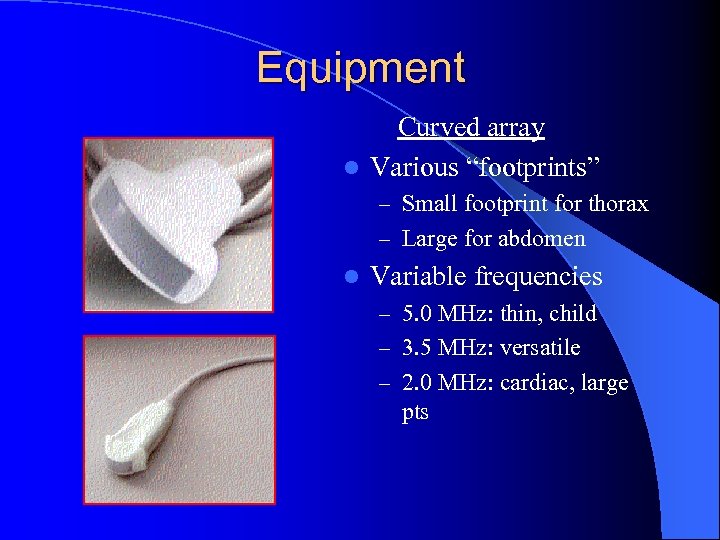 Equipment Curved array l Various “footprints” – Small footprint for thorax – Large for abdomen l Variable frequencies – 5. 0 MHz: thin, child – 3. 5 MHz: versatile – 2. 0 MHz: cardiac, large pts
Equipment Curved array l Various “footprints” – Small footprint for thorax – Large for abdomen l Variable frequencies – 5. 0 MHz: thin, child – 3. 5 MHz: versatile – 2. 0 MHz: cardiac, large pts
 Time to Complete Scan l Each view: 30 -60 seconds l Number of views dependent on clinical question and findings on initial views l Total exam time usually < 3 -5 minutes l 1988 Armenian earthquake – 400 trauma US scans in 72 hrs
Time to Complete Scan l Each view: 30 -60 seconds l Number of views dependent on clinical question and findings on initial views l Total exam time usually < 3 -5 minutes l 1988 Armenian earthquake – 400 trauma US scans in 72 hrs
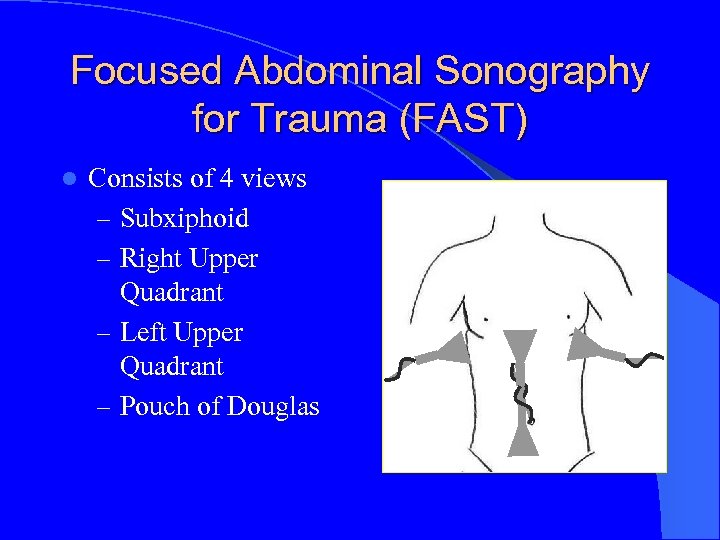 Focused Abdominal Sonography for Trauma (FAST) l Consists of 4 views – Subxiphoid – Right Upper Quadrant – Left Upper Quadrant – Pouch of Douglas
Focused Abdominal Sonography for Trauma (FAST) l Consists of 4 views – Subxiphoid – Right Upper Quadrant – Left Upper Quadrant – Pouch of Douglas
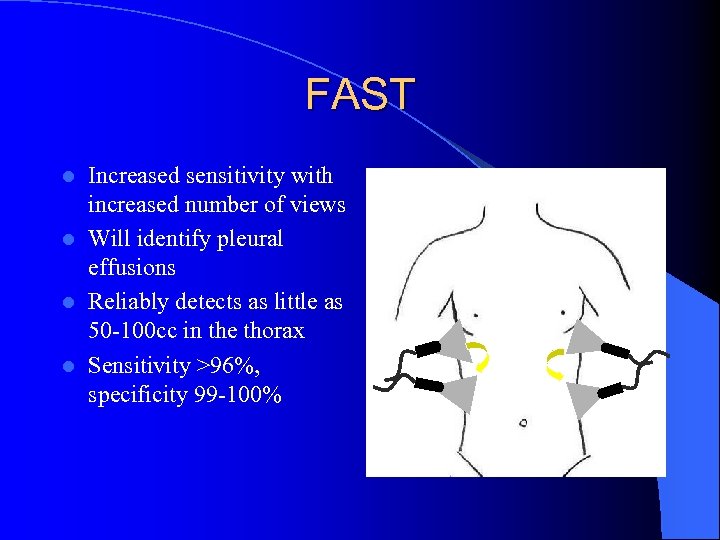 FAST Increased sensitivity with increased number of views l Will identify pleural effusions l Reliably detects as little as 50 -100 cc in the thorax l Sensitivity >96%, specificity 99 -100% l
FAST Increased sensitivity with increased number of views l Will identify pleural effusions l Reliably detects as little as 50 -100 cc in the thorax l Sensitivity >96%, specificity 99 -100% l
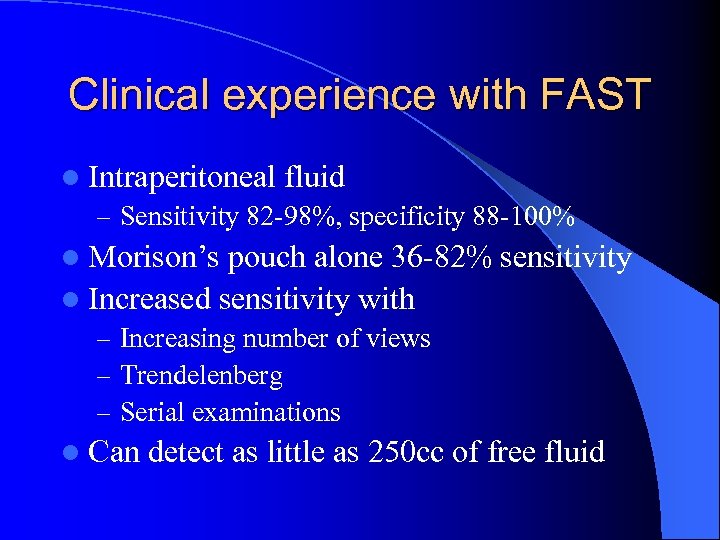 Clinical experience with FAST l Intraperitoneal fluid – Sensitivity 82 -98%, specificity 88 -100% l Morison’s pouch alone 36 -82% sensitivity l Increased sensitivity with – Increasing number of views – Trendelenberg – Serial examinations l Can detect as little as 250 cc of free fluid
Clinical experience with FAST l Intraperitoneal fluid – Sensitivity 82 -98%, specificity 88 -100% l Morison’s pouch alone 36 -82% sensitivity l Increased sensitivity with – Increasing number of views – Trendelenberg – Serial examinations l Can detect as little as 250 cc of free fluid
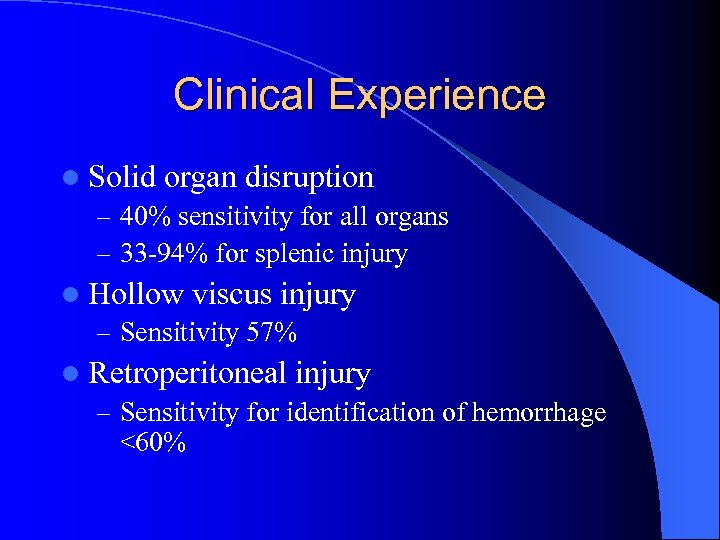 Clinical Experience l Solid organ disruption – 40% sensitivity for all organs – 33 -94% for splenic injury l Hollow viscus injury – Sensitivity 57% l Retroperitoneal injury – Sensitivity for identification of hemorrhage <60%
Clinical Experience l Solid organ disruption – 40% sensitivity for all organs – 33 -94% for splenic injury l Hollow viscus injury – Sensitivity 57% l Retroperitoneal injury – Sensitivity for identification of hemorrhage <60%
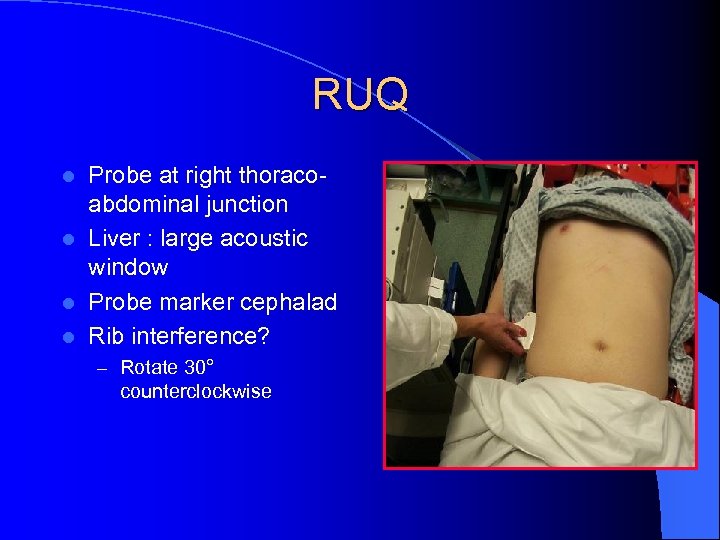 RUQ Probe at right thoracoabdominal junction l Liver : large acoustic window l Probe marker cephalad l Rib interference? l – Rotate 30° counterclockwise
RUQ Probe at right thoracoabdominal junction l Liver : large acoustic window l Probe marker cephalad l Rib interference? l – Rotate 30° counterclockwise
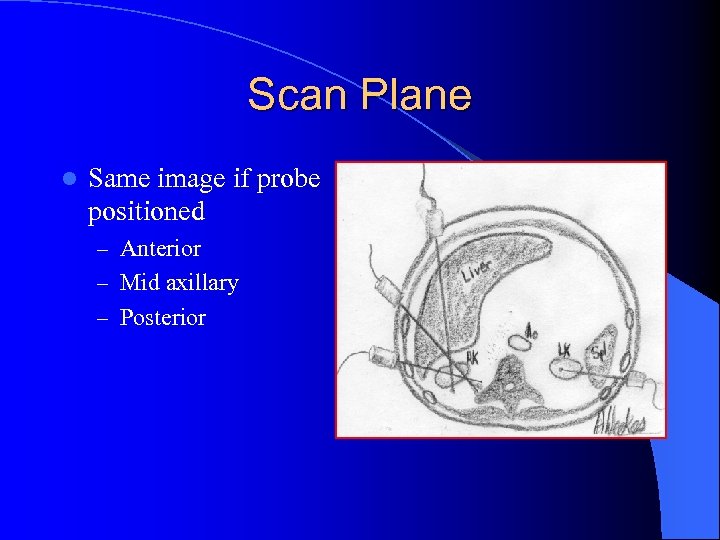 Scan Plane l Same image if probe positioned – Anterior – Mid axillary – Posterior
Scan Plane l Same image if probe positioned – Anterior – Mid axillary – Posterior
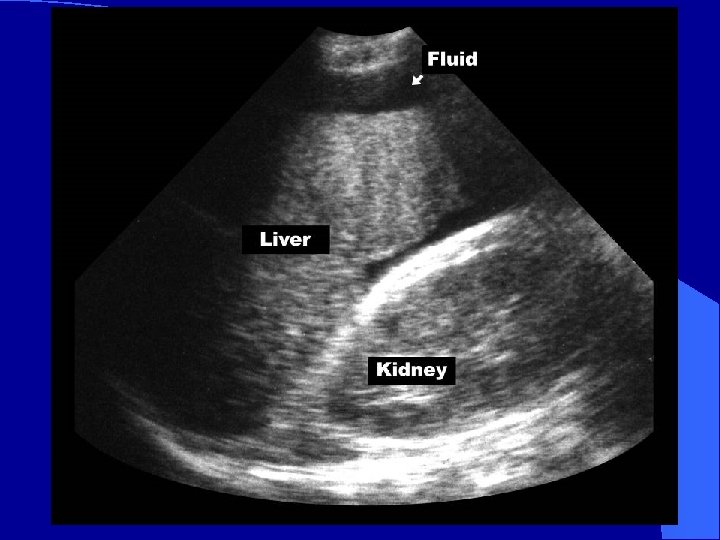
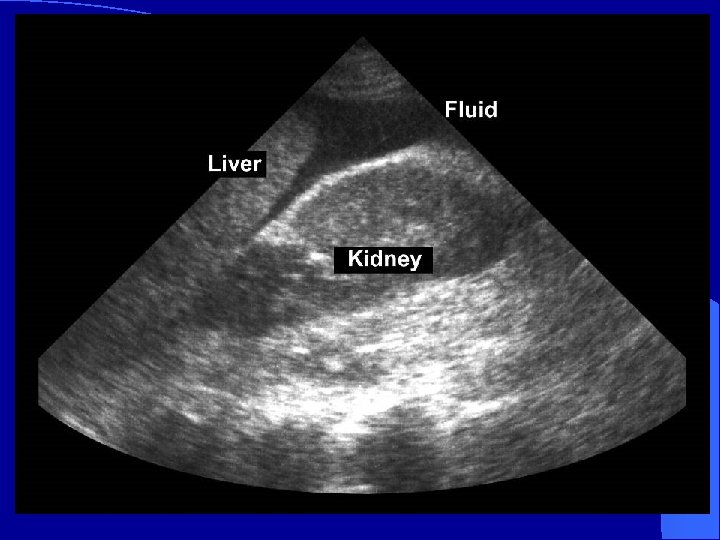
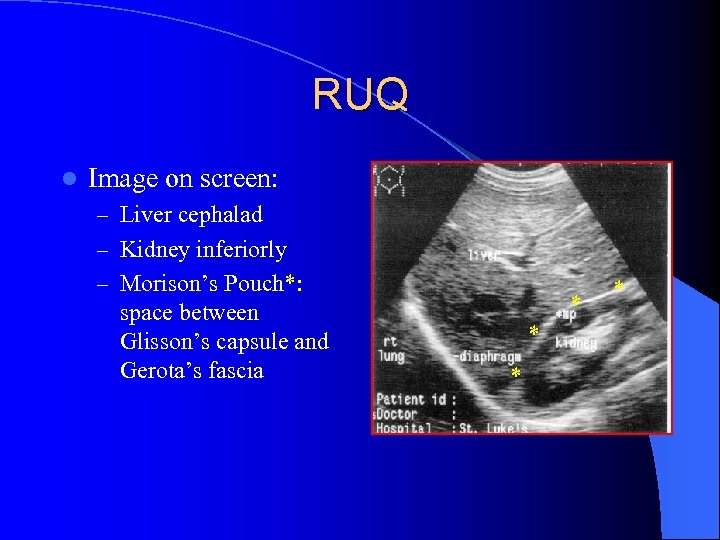 RUQ l Image on screen: – Liver cephalad – Kidney inferiorly – Morison’s Pouch*: space between Glisson’s capsule and Gerota’s fascia * *
RUQ l Image on screen: – Liver cephalad – Kidney inferiorly – Morison’s Pouch*: space between Glisson’s capsule and Gerota’s fascia * *
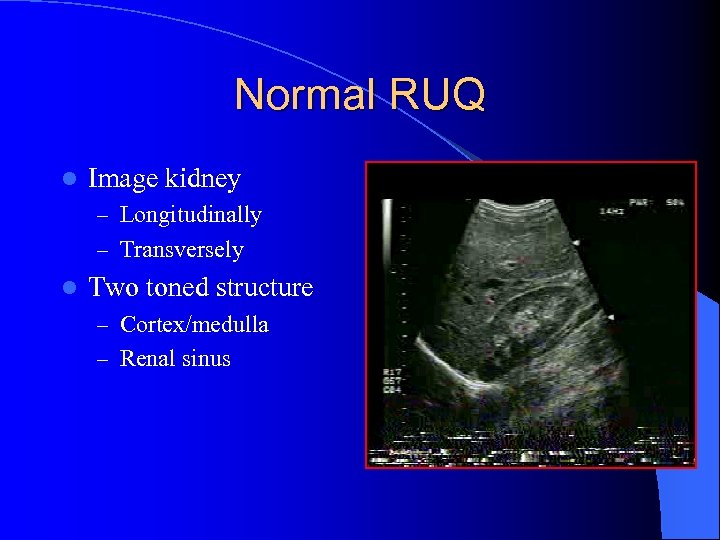 Normal RUQ l Image kidney – Longitudinally – Transversely l Two toned structure – Cortex/medulla – Renal sinus
Normal RUQ l Image kidney – Longitudinally – Transversely l Two toned structure – Cortex/medulla – Renal sinus
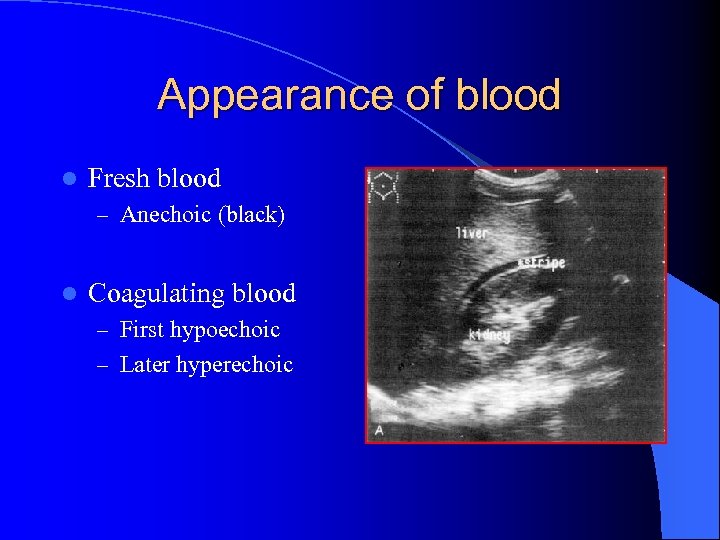 Appearance of blood l Fresh blood – Anechoic (black) l Coagulating blood – First hypoechoic – Later hyperechoic
Appearance of blood l Fresh blood – Anechoic (black) l Coagulating blood – First hypoechoic – Later hyperechoic
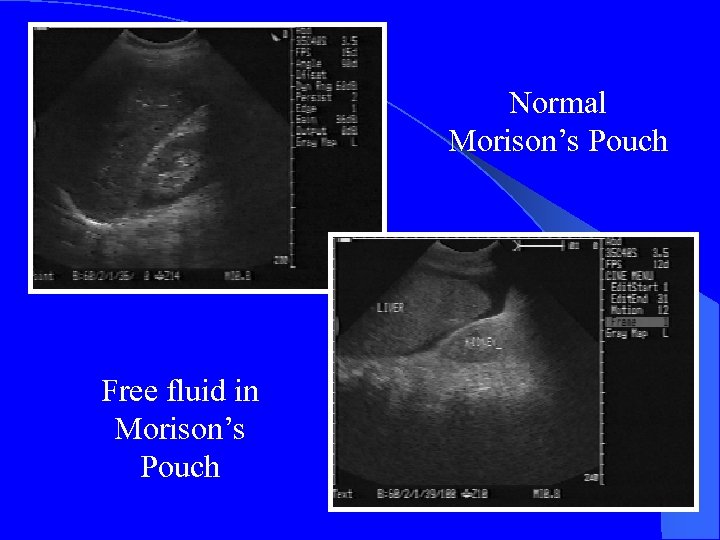 Normal Morison’s Pouch Free fluid in Morison’s Pouch
Normal Morison’s Pouch Free fluid in Morison’s Pouch


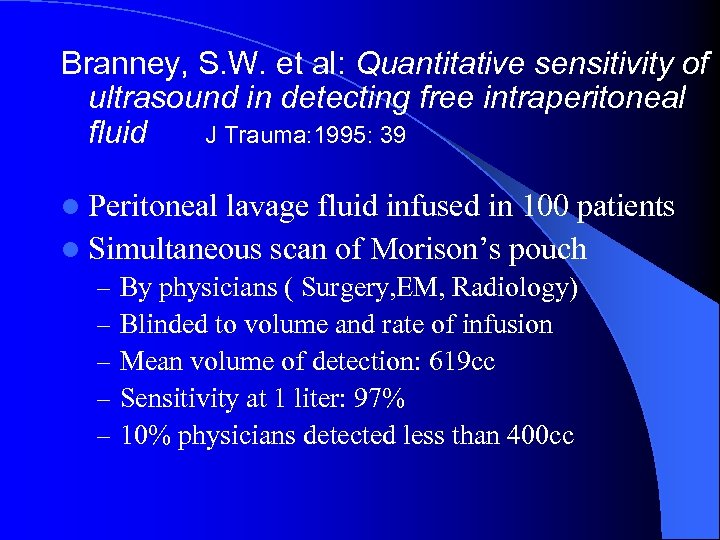 Branney, S. W. et al: Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid J Trauma: 1995: 39 l Peritoneal lavage fluid infused in 100 patients l Simultaneous scan of Morison’s pouch – By physicians ( Surgery, EM, Radiology) – Blinded to volume and rate of infusion – Mean volume of detection: 619 cc – Sensitivity at 1 liter: 97% – 10% physicians detected less than 400 cc
Branney, S. W. et al: Quantitative sensitivity of ultrasound in detecting free intraperitoneal fluid J Trauma: 1995: 39 l Peritoneal lavage fluid infused in 100 patients l Simultaneous scan of Morison’s pouch – By physicians ( Surgery, EM, Radiology) – Blinded to volume and rate of infusion – Mean volume of detection: 619 cc – Sensitivity at 1 liter: 97% – 10% physicians detected less than 400 cc
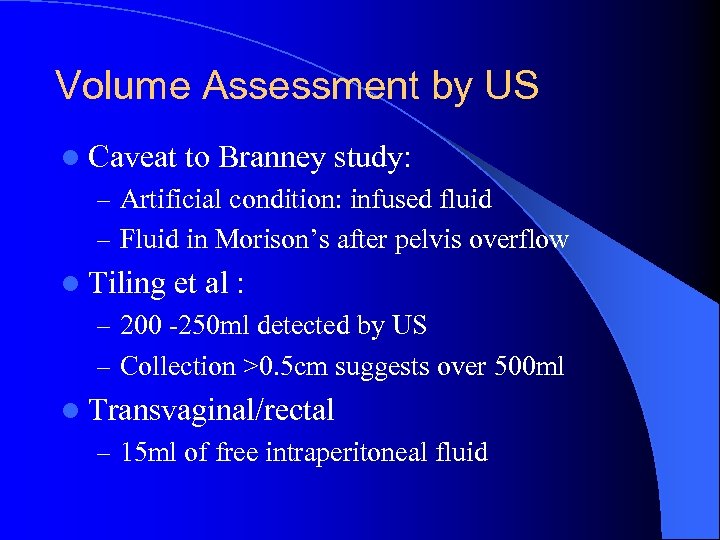 Volume Assessment by US l Caveat to Branney study: – Artificial condition: infused fluid – Fluid in Morison’s after pelvis overflow l Tiling et al : – 200 -250 ml detected by US – Collection >0. 5 cm suggests over 500 ml l Transvaginal/rectal – 15 ml of free intraperitoneal fluid
Volume Assessment by US l Caveat to Branney study: – Artificial condition: infused fluid – Fluid in Morison’s after pelvis overflow l Tiling et al : – 200 -250 ml detected by US – Collection >0. 5 cm suggests over 500 ml l Transvaginal/rectal – 15 ml of free intraperitoneal fluid
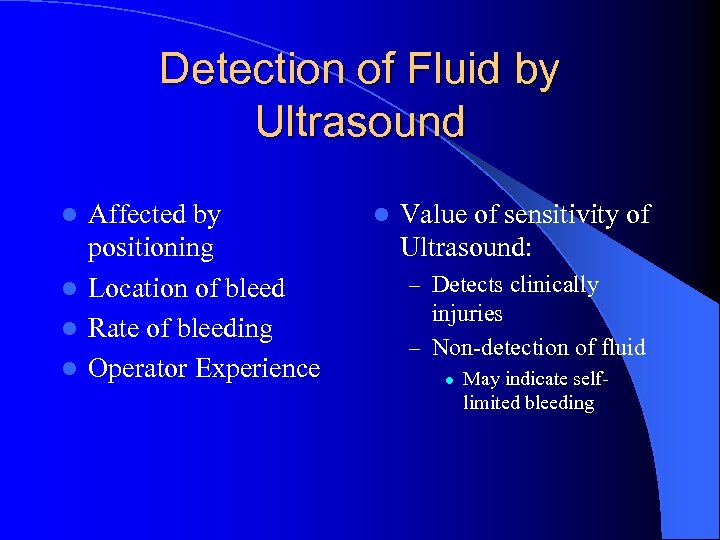 Detection of Fluid by Ultrasound Affected by positioning l Location of bleed l Rate of bleeding l Operator Experience l l Value of sensitivity of Ultrasound: – Detects clinically injuries – Non-detection of fluid l May indicate self- limited bleeding
Detection of Fluid by Ultrasound Affected by positioning l Location of bleed l Rate of bleeding l Operator Experience l l Value of sensitivity of Ultrasound: – Detects clinically injuries – Non-detection of fluid l May indicate self- limited bleeding
 All Fluid is not Blood l Ascites l Ruptured Ovarian Cyst l Lavage fluid l Urine from ruptured bladder
All Fluid is not Blood l Ascites l Ruptured Ovarian Cyst l Lavage fluid l Urine from ruptured bladder
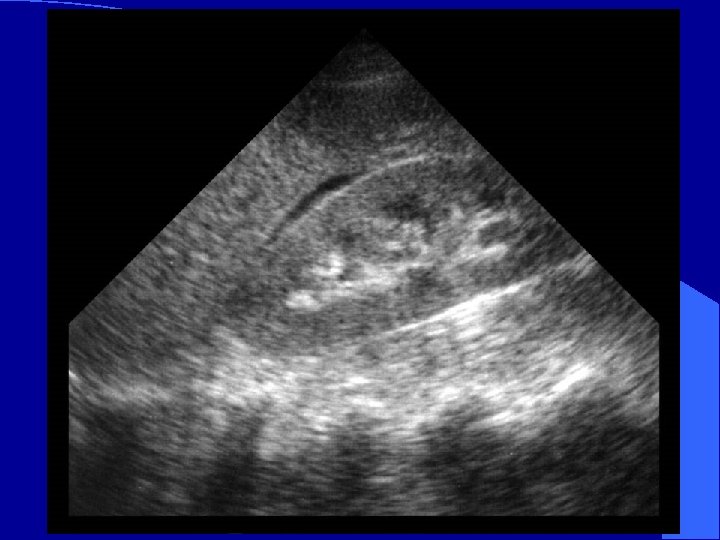
 Mimics of Fluid in RUQ l Perinephric fat – May be hypoechoic like blood – Usually evenly layered along kidney – If in doubt, compare to left kidney l Abdominal inflammation – Widened extra-renal space – Echogenicity of kidney becomes more like the liver parenchyma
Mimics of Fluid in RUQ l Perinephric fat – May be hypoechoic like blood – Usually evenly layered along kidney – If in doubt, compare to left kidney l Abdominal inflammation – Widened extra-renal space – Echogenicity of kidney becomes more like the liver parenchyma
 Pitfalls l RUQ – Not attempting multiple probe placements – Not placing the probe cephalad enough to use the acoustic window of the liver Scanning too soon before enough blood has accumulated l Not repeating the scan l
Pitfalls l RUQ – Not attempting multiple probe placements – Not placing the probe cephalad enough to use the acoustic window of the liver Scanning too soon before enough blood has accumulated l Not repeating the scan l
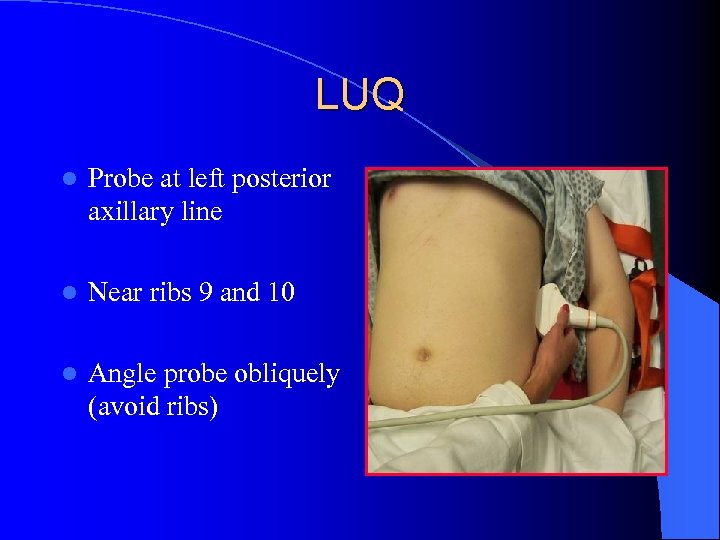 LUQ l Probe at left posterior axillary line l Near ribs 9 and 10 l Angle probe obliquely (avoid ribs)
LUQ l Probe at left posterior axillary line l Near ribs 9 and 10 l Angle probe obliquely (avoid ribs)
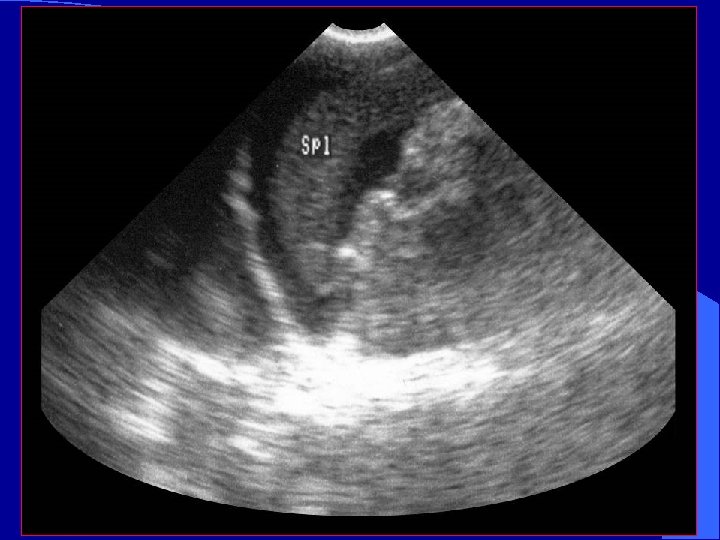
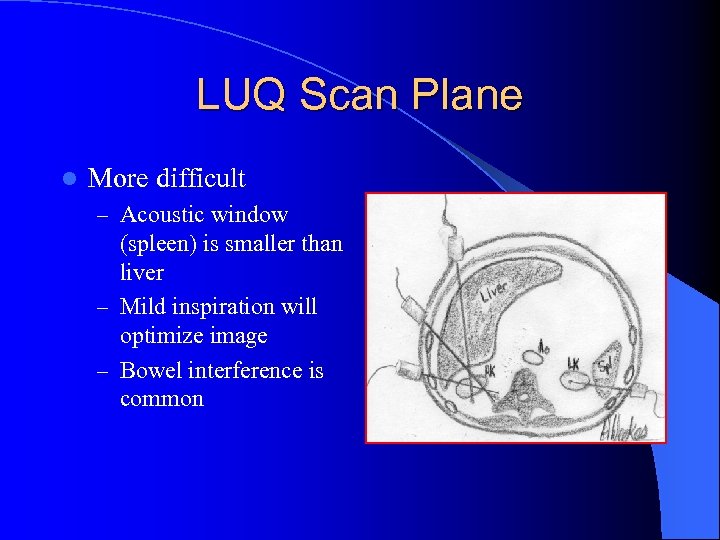 LUQ Scan Plane l More difficult – Acoustic window (spleen) is smaller than liver – Mild inspiration will optimize image – Bowel interference is common
LUQ Scan Plane l More difficult – Acoustic window (spleen) is smaller than liver – Mild inspiration will optimize image – Bowel interference is common
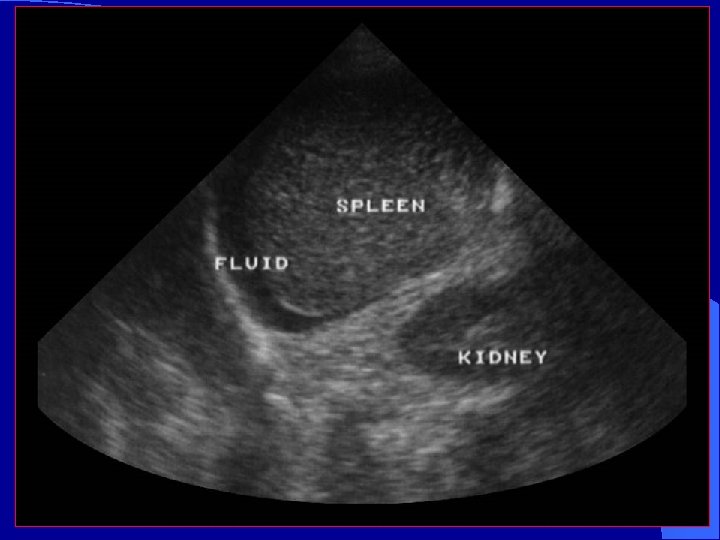
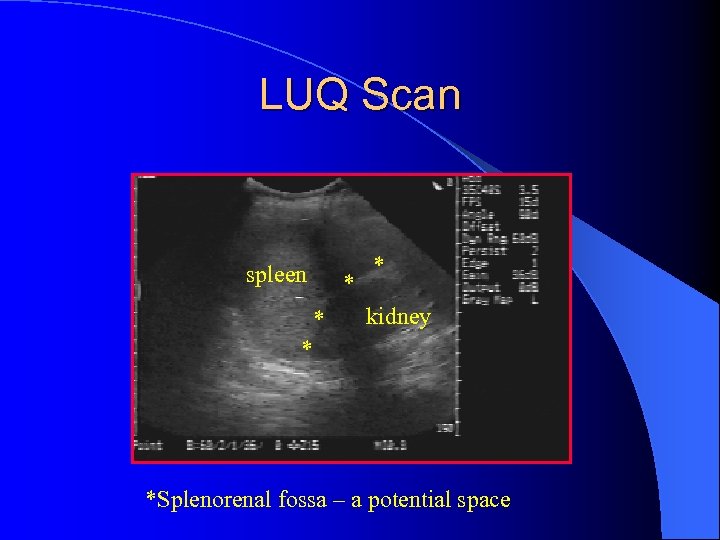 LUQ Scan spleen * * * kidney * *Splenorenal fossa – a potential space
LUQ Scan spleen * * * kidney * *Splenorenal fossa – a potential space
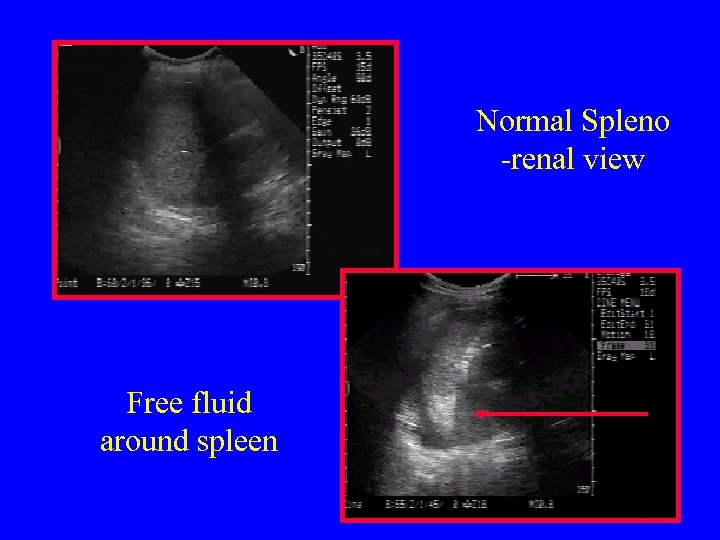 Normal Spleno -renal view Free fluid around spleen
Normal Spleno -renal view Free fluid around spleen
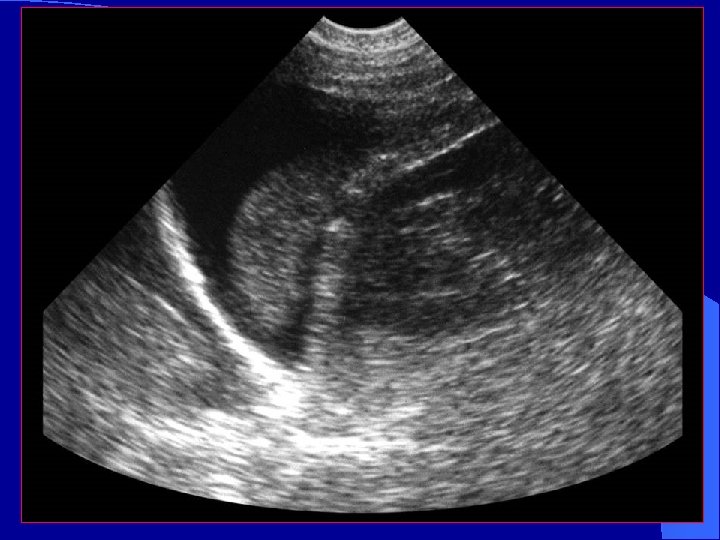

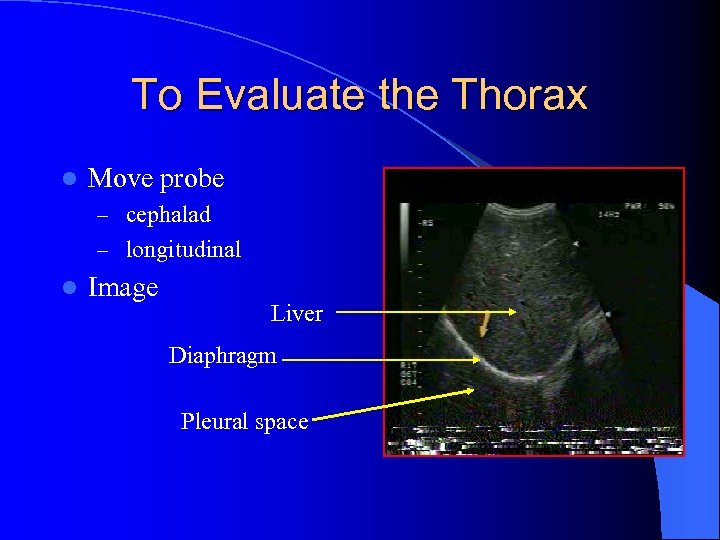 To Evaluate the Thorax l Move probe – cephalad – longitudinal l Image Liver Diaphragm Pleural space
To Evaluate the Thorax l Move probe – cephalad – longitudinal l Image Liver Diaphragm Pleural space
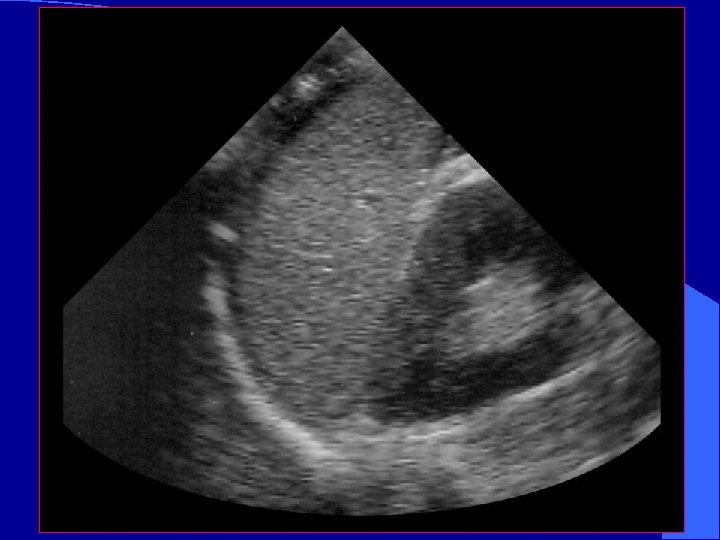
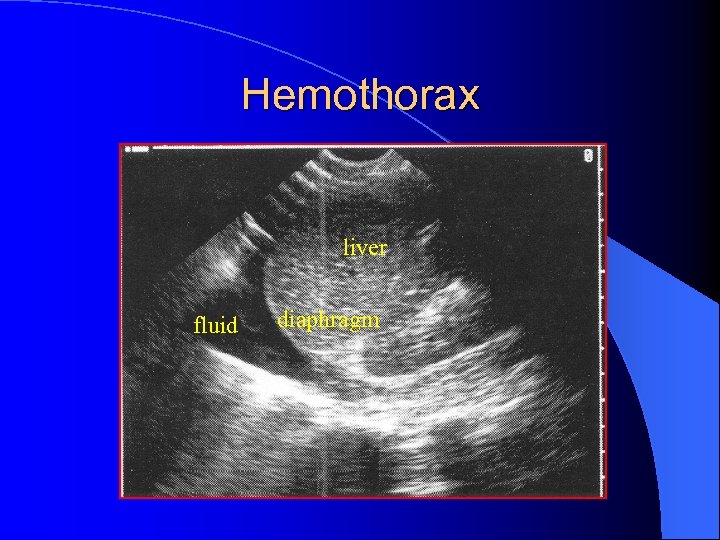 Hemothorax liver fluid diaphragm
Hemothorax liver fluid diaphragm
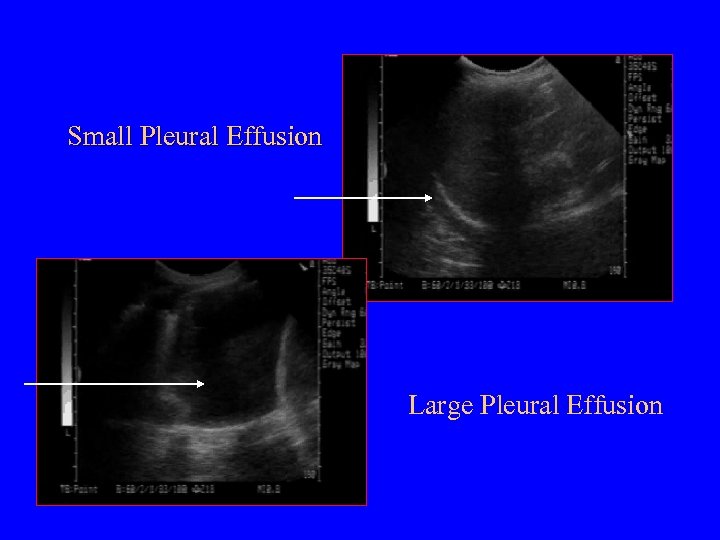 Small Pleural Effusion Large Pleural Effusion
Small Pleural Effusion Large Pleural Effusion
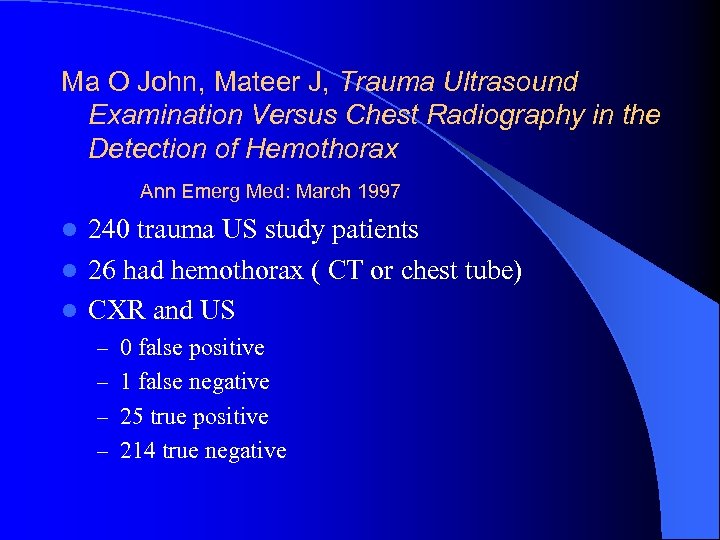 Ma O John, Mateer J, Trauma Ultrasound Examination Versus Chest Radiography in the Detection of Hemothorax Ann Emerg Med: March 1997 l 240 trauma US study patients l 26 had hemothorax ( CT or chest tube) l CXR and US – 0 false positive – 1 false negative – 25 true positive – 214 true negative
Ma O John, Mateer J, Trauma Ultrasound Examination Versus Chest Radiography in the Detection of Hemothorax Ann Emerg Med: March 1997 l 240 trauma US study patients l 26 had hemothorax ( CT or chest tube) l CXR and US – 0 false positive – 1 false negative – 25 true positive – 214 true negative
 Pelvic View Probe should be placed in the suprapubic position l Either can be transverse or longitudinal l Helpful to image before placement of a Foley catheter l
Pelvic View Probe should be placed in the suprapubic position l Either can be transverse or longitudinal l Helpful to image before placement of a Foley catheter l
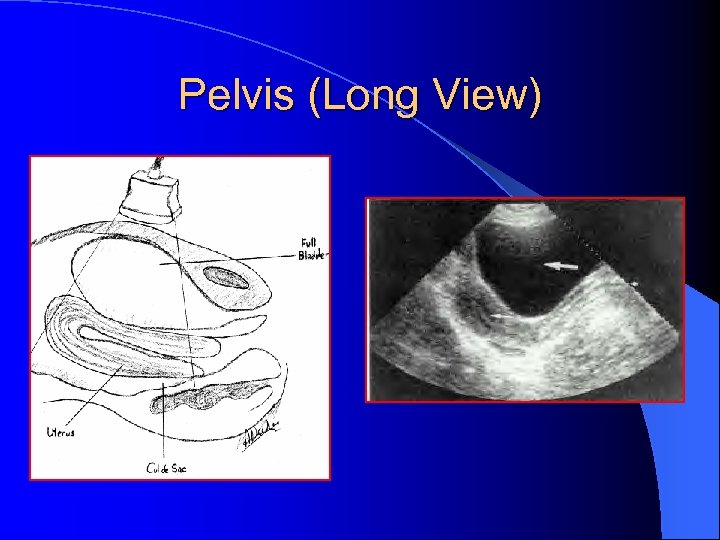 Pelvis (Long View)
Pelvis (Long View)
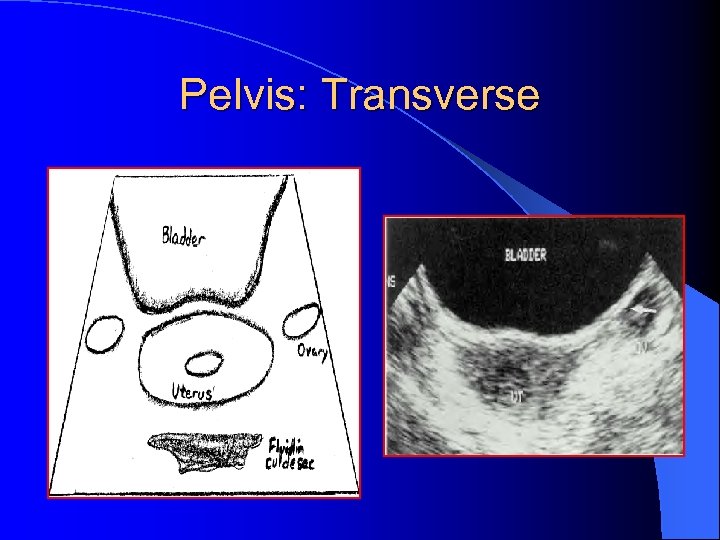 Pelvis: Transverse
Pelvis: Transverse
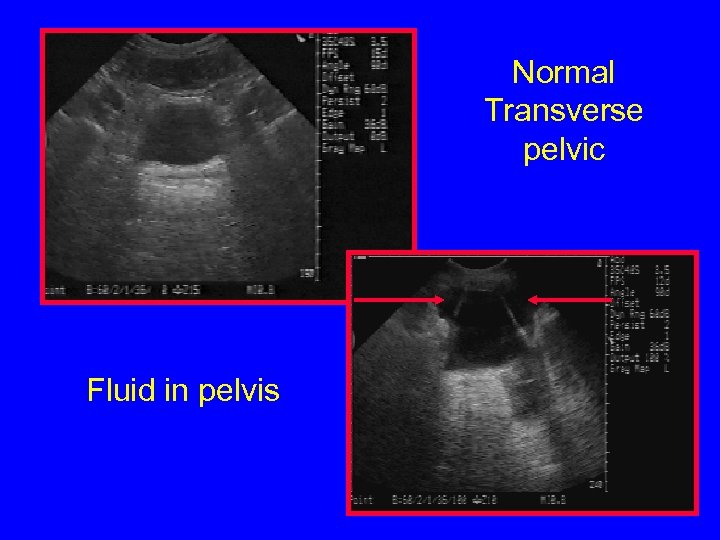 Normal Transverse pelvic Fluid in pelvis
Normal Transverse pelvic Fluid in pelvis
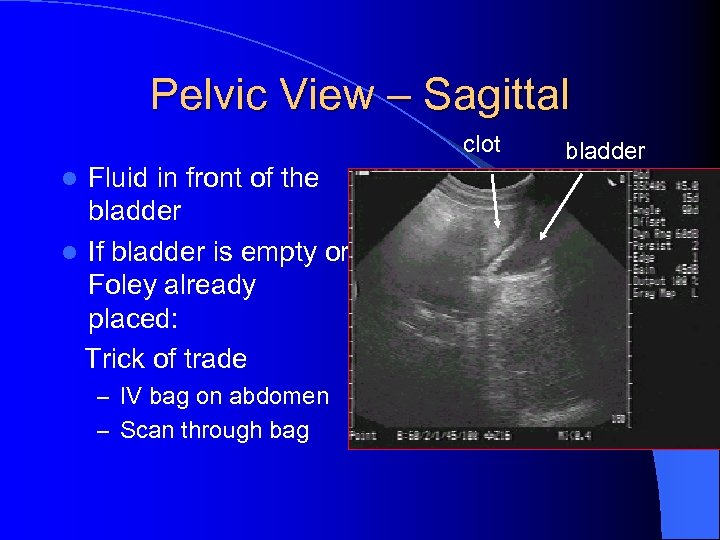 Pelvic View – Sagittal clot Fluid in front of the bladder l If bladder is empty or Foley already placed: Trick of trade l – IV bag on abdomen – Scan through bag bladder
Pelvic View – Sagittal clot Fluid in front of the bladder l If bladder is empty or Foley already placed: Trick of trade l – IV bag on abdomen – Scan through bag bladder
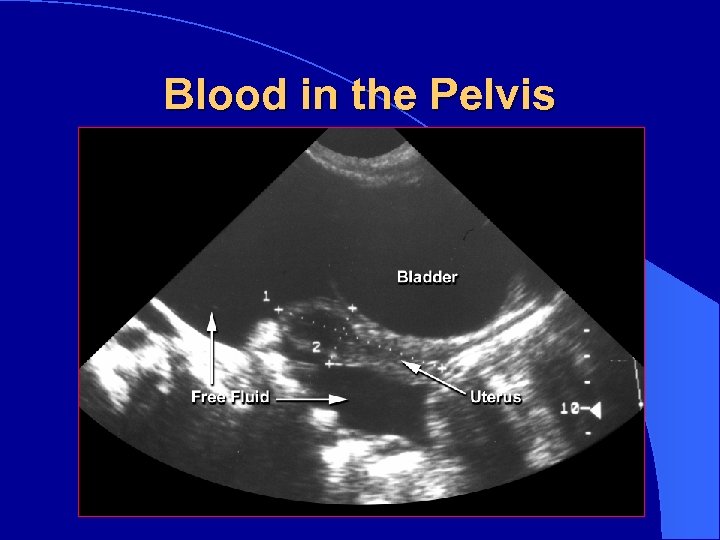 Blood in the Pelvis
Blood in the Pelvis

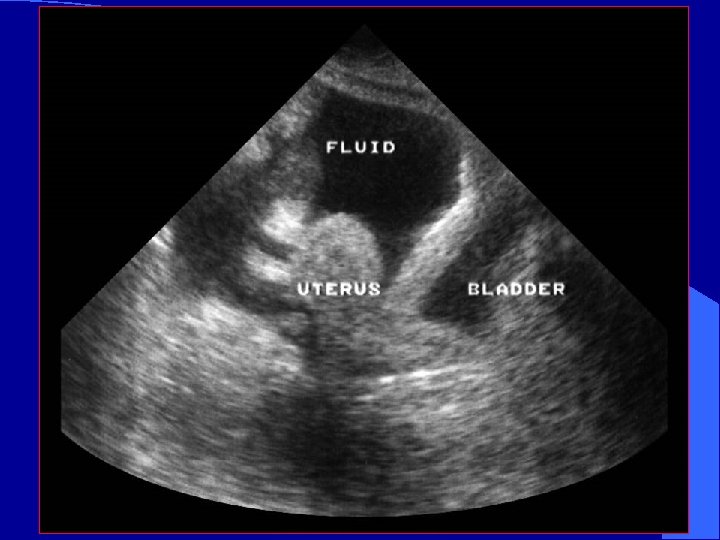
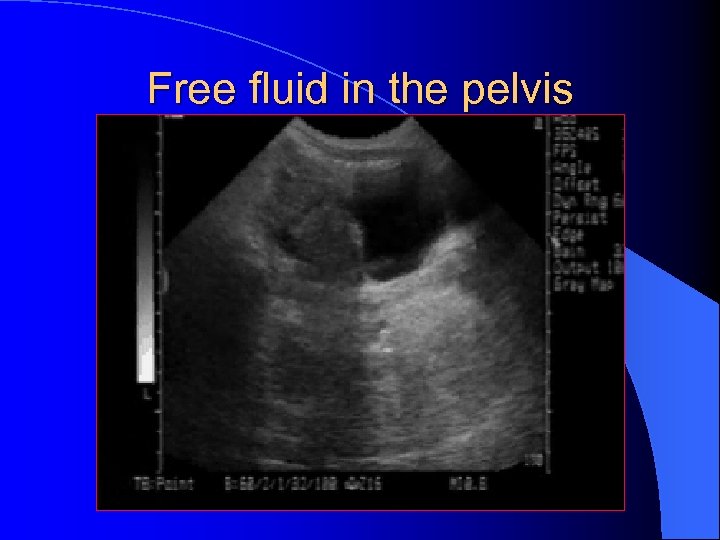 Free fluid in the pelvis
Free fluid in the pelvis
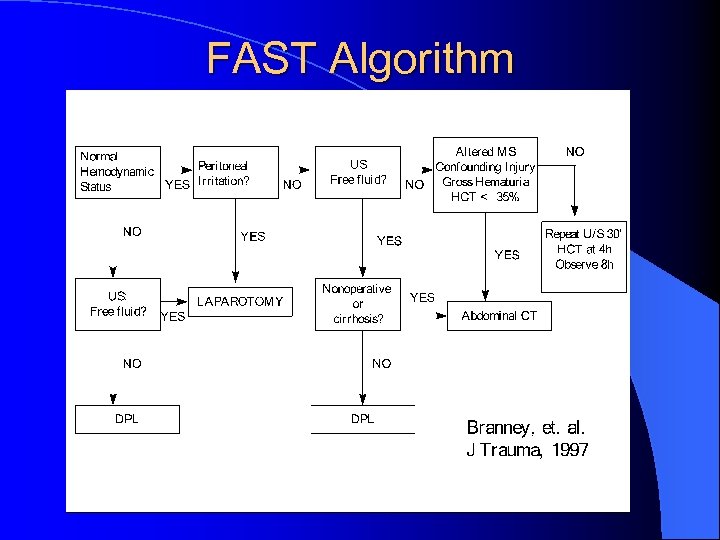 FAST Algorithm
FAST Algorithm
 Ultrasound in the Detection of Injury From Blunt or Penetrating Thoracic Trauma
Ultrasound in the Detection of Injury From Blunt or Penetrating Thoracic Trauma
 Penetrating Thoracic Injury l Clinical challenge – Where is the penetration? – What was the weapon? – What was the trajectory? – What organ(s) have been injured? – Improved outcomes in patients with normal or near-normal vital signs
Penetrating Thoracic Injury l Clinical challenge – Where is the penetration? – What was the weapon? – What was the trajectory? – What organ(s) have been injured? – Improved outcomes in patients with normal or near-normal vital signs
 Penetrating Cardiac Trauma l Pericardial effusion – May develop suddenly or surreptitiously – May exist before clinical signs develop l Salvage rates better if detected before hypotension develops
Penetrating Cardiac Trauma l Pericardial effusion – May develop suddenly or surreptitiously – May exist before clinical signs develop l Salvage rates better if detected before hypotension develops
 Clinical Case l QD is 37 year old male brought in by EMS for ingesting entire bottle of unidentified red and white pills. In the ambulance bay he pulls out a knife and stabs himself in the left nipple.
Clinical Case l QD is 37 year old male brought in by EMS for ingesting entire bottle of unidentified red and white pills. In the ambulance bay he pulls out a knife and stabs himself in the left nipple.
 Clinical Case l Initial BP 116/72, pulse 109 RR 24. IV’s placed. l No JVD, Clear breath sounds, non tender abdomen l As CXR is about to be done, pulse increases to 134. l Bedside ultrasound is done while cartridge is developed.
Clinical Case l Initial BP 116/72, pulse 109 RR 24. IV’s placed. l No JVD, Clear breath sounds, non tender abdomen l As CXR is about to be done, pulse increases to 134. l Bedside ultrasound is done while cartridge is developed.
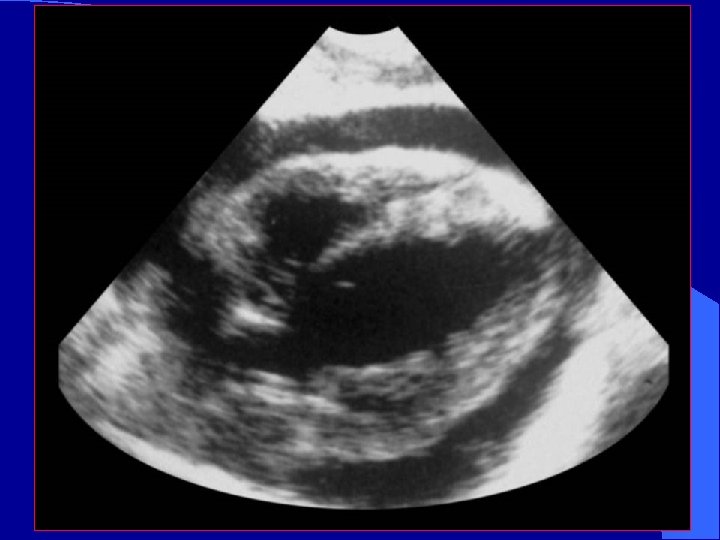
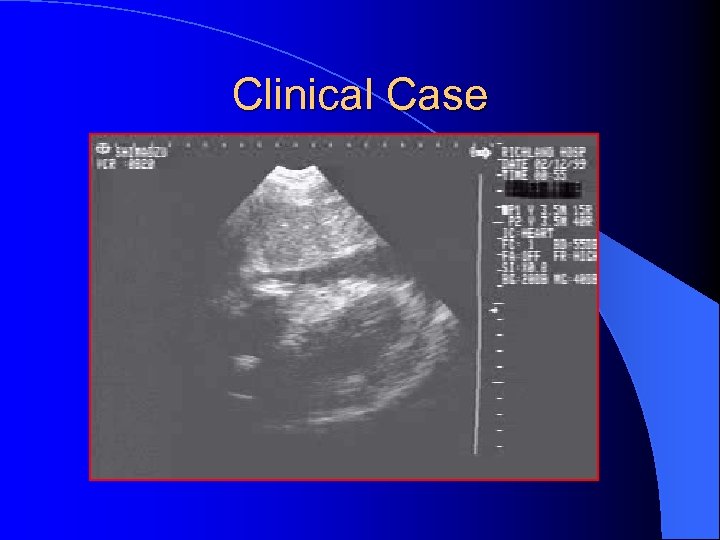 Clinical Case
Clinical Case
 Clinical Case l Patient is taken to the OR l Penetrating cardiac wound is repaired
Clinical Case l Patient is taken to the OR l Penetrating cardiac wound is repaired
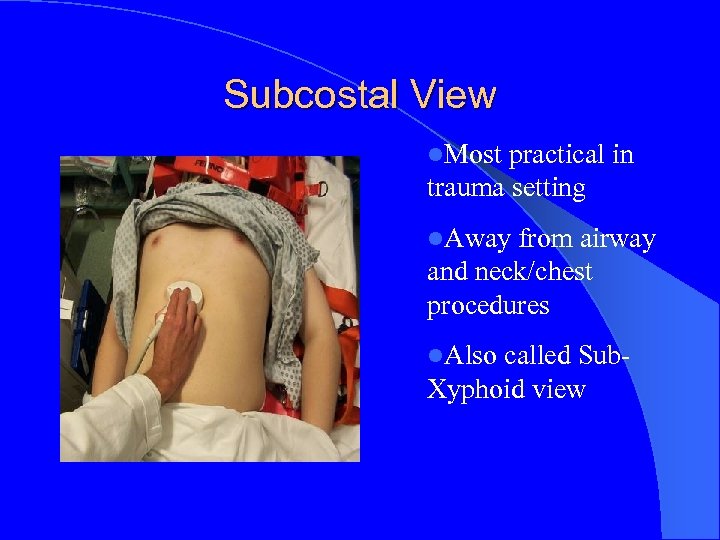 Subcostal View l. Most practical in trauma setting l. Away from airway and neck/chest procedures l. Also called Sub- Xyphoid view
Subcostal View l. Most practical in trauma setting l. Away from airway and neck/chest procedures l. Also called Sub- Xyphoid view
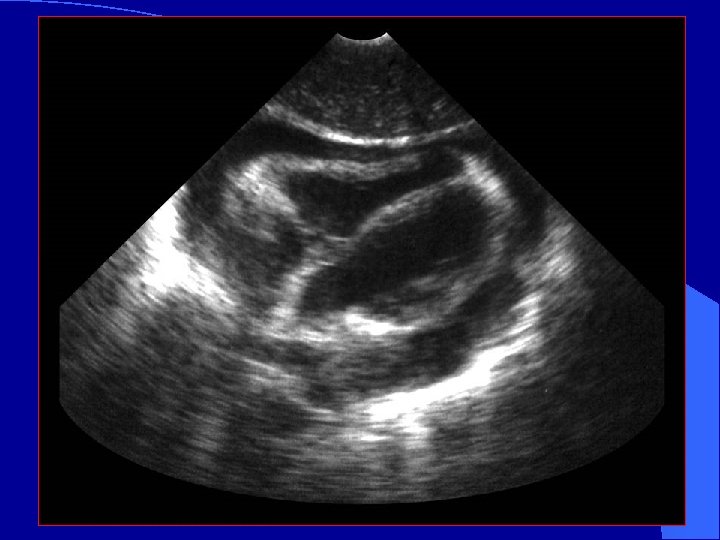
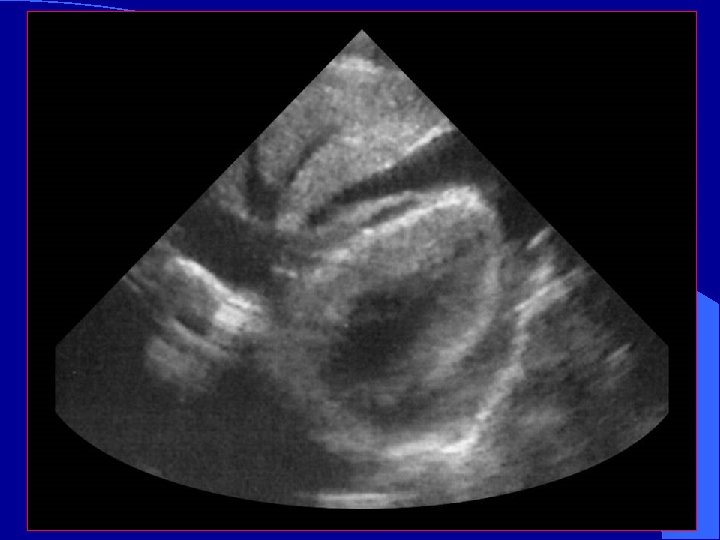
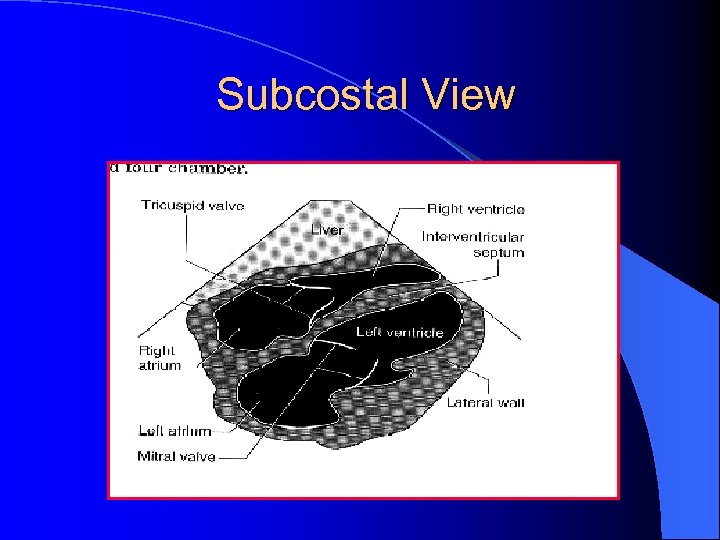 Subcostal View
Subcostal View
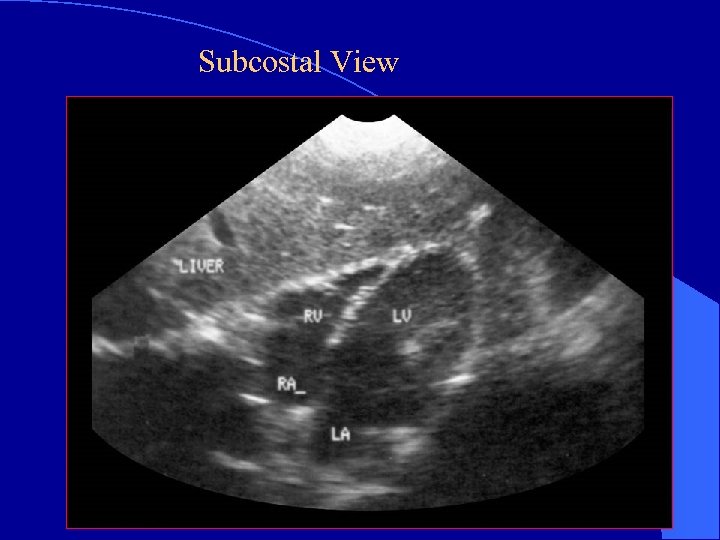 Subcostal View
Subcostal View
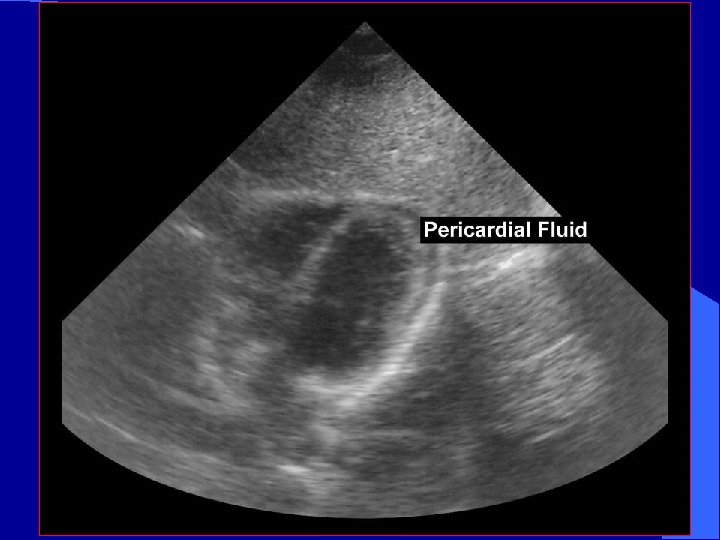
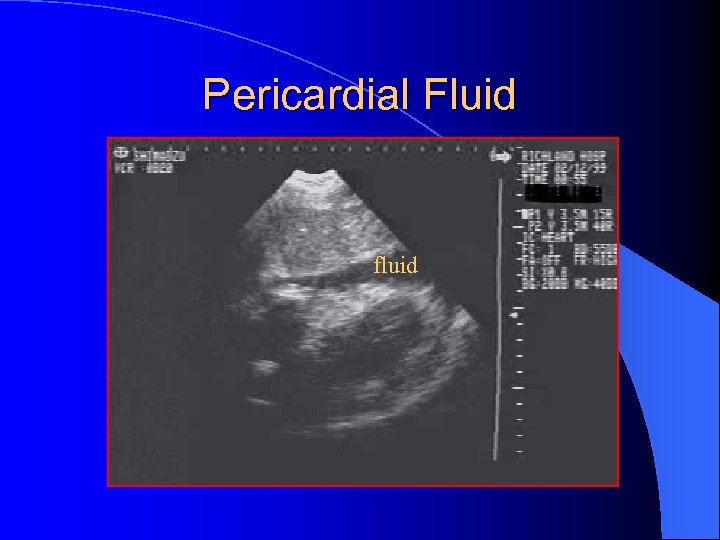 Pericardial Fluid fluid
Pericardial Fluid fluid

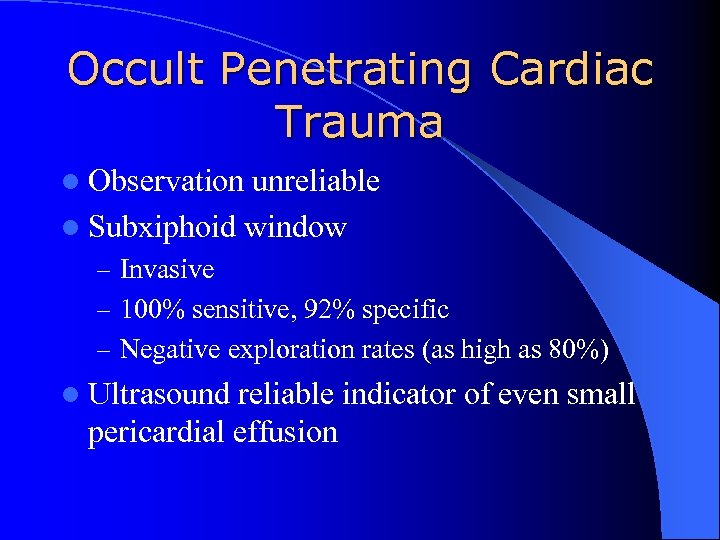 Occult Penetrating Cardiac Trauma l Observation unreliable l Subxiphoid window – Invasive – 100% sensitive, 92% specific – Negative exploration rates (as high as 80%) l Ultrasound reliable indicator of even small pericardial effusion
Occult Penetrating Cardiac Trauma l Observation unreliable l Subxiphoid window – Invasive – 100% sensitive, 92% specific – Negative exploration rates (as high as 80%) l Ultrasound reliable indicator of even small pericardial effusion
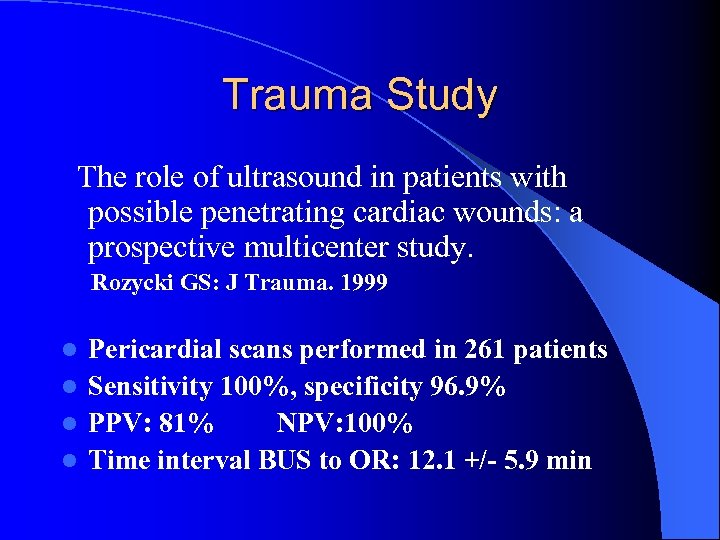 Trauma Study The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. Rozycki GS: J Trauma. 1999 Pericardial scans performed in 261 patients l Sensitivity 100%, specificity 96. 9% l PPV: 81% NPV: 100% l Time interval BUS to OR: 12. 1 +/- 5. 9 min l
Trauma Study The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. Rozycki GS: J Trauma. 1999 Pericardial scans performed in 261 patients l Sensitivity 100%, specificity 96. 9% l PPV: 81% NPV: 100% l Time interval BUS to OR: 12. 1 +/- 5. 9 min l
 Avoid Pitfalls l Normal echo does not definitively rule out major pericardial injury l Repeat echo with clinical picture l Epicardial fat pad may easily be misinterpreted as “clot” l Hemothorax may be confused with pericardial effusion
Avoid Pitfalls l Normal echo does not definitively rule out major pericardial injury l Repeat echo with clinical picture l Epicardial fat pad may easily be misinterpreted as “clot” l Hemothorax may be confused with pericardial effusion
 Blunt Cardiac Trauma l Basic Assessments – Pericardial effusion – Assess for wall motion abnormality – RV: l l closest to anterior chest wall Most likely to be injured l Advanced Assessments – Assess thoracic aorta – may need TEE to see all of thoracic aorta l l l Hematoma Intimal flap Abnormal contour – Valvular dysfunction or septal rupture
Blunt Cardiac Trauma l Basic Assessments – Pericardial effusion – Assess for wall motion abnormality – RV: l l closest to anterior chest wall Most likely to be injured l Advanced Assessments – Assess thoracic aorta – may need TEE to see all of thoracic aorta l l l Hematoma Intimal flap Abnormal contour – Valvular dysfunction or septal rupture
 Blunt cardiac trauma l Injuries difficult to assess by FAST – Valvular incompetence – Myocardial rupture – Intracardiac thrombosis – Ventricular aneurysm – Coronary Thrombosis – Intra-cardiac Thrombosis
Blunt cardiac trauma l Injuries difficult to assess by FAST – Valvular incompetence – Myocardial rupture – Intracardiac thrombosis – Ventricular aneurysm – Coronary Thrombosis – Intra-cardiac Thrombosis
 “ The most important preoperative objective in the management of the patient with trauma is to ascertain whether or not laparotomy is needed, and not the diagnosis of a specific organ injury”
“ The most important preoperative objective in the management of the patient with trauma is to ascertain whether or not laparotomy is needed, and not the diagnosis of a specific organ injury”


