c739511a45a9c3a1c60748d3adbc2521.ppt
- Количество слайдов: 76
Emergency Department Registration Presented by The Ambulatory Education & Systems Team 1
Table of Contents Emergency Department Registration………………………… 4 -7 Best Practices…………………………………… 8 Non Critical Patient Registration…………………………. . 9 -16 Demographic Information……………………… 9 -10 Disparities Questions………………………… 11 -13 Patient Language……………………………. . . 14 Disparities Questions-General Objections………………. 15 Demographic information………………………. . 16 Fiscal Information…………………………………. . 17 -20 Emergency Department Form…………………………… 21 -23 Special Registrations…………………………………. . 24 -34 Workers Comp………………………………. . 24 -26 Auto Liability……………………………… 27 Worker’s Comp/Auto Liability Scripting…………………. 28 Student Registration……………………………. . 29 RCI Patients………………………………. . . 30 John Doe Patients……………………………. . 31 EU Critical Patient…………………………… 32 -33 Free Care…………………………………. . . 34 2
Table of Contents Mini-Reg……………………………………… 35 -36 Update Mini Reg…………………………………… 37 -40 Has Registration Information Been Reviewed……………………. . . 41 How Will I Know Who Needs Bedside Registration…………………. 42 NEHEN………………………………………. . 43 -57 Edit option………………………………………. . 58 Down Time Procedures………………………………. . 59 -60 UCO Downtime Procedures……………………………. . . 61 -62 Medical Records Merge………………………………. . 63 Emergency Department Portal…………………………… 64 -66 Other Important Functions………………………………. . 67 -68 Limited Access…………………………………… 69 -73 What If? . . . . . . . 74 -75 Resources………………………………………. 76 3
Emergency Department Registration Summary of Procedures for the Emergency Department Registration: • Between the hours of 9 am and 9 pm the mini registration model will be used (or as staffing permits). This model allows the registrar to collect limited information at the point of patient triage to admit the patient to the ED. The rest of the registration information will be collected bedside. To support this effort the following staffing (shift responsibility) changes will take place: 1 Registration Specialist will be assigned to the Triage area to complete “Mini Reg”. 2 Registration Specialists will be assigned to the Core. 1 of these Registration Specialists will wear the Check Out pager and assume responsibility for that function for the shift. • Between the hours of 9 pm and 9 am the full ED “Admit” option will be used to admit and register ED patients. • The Check Out office and associated processes will be open and in effect during the hours of 9 a-9 p (or as staffing permits) 4
Emergency Department Registration • • • Each Registration Specialist will have their own cash bag with which to collect co-payments when assigned to Check Out. These cash bags will be reconciled daily. (Policies and Procedures) New/Updated process for obtaining data elements required to bill Workers Comp and Auto/Liability cases. Integration of NEHEN Eligibility checking into the ED Registration flow as performed by the Registration Specialist (and confirmed by the check out process) Policies and Procedures to support the collection and reconciliation of Copayments/Other Payments (self pay) Please be sure to ask for and check patient’s picture identification!!!! Acceptable forms of ID are drivers license, School ID, Social Security Card with other ID. 5
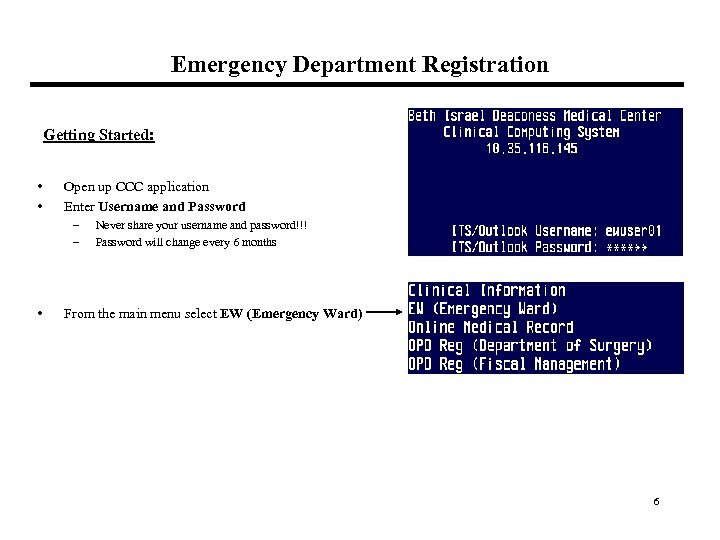
Emergency Department Registration Getting Started: • • Open up CCC application Enter Username and Password – – • Never share your username and password!!! Password will change every 6 months From the main menu select EW (Emergency Ward) 6
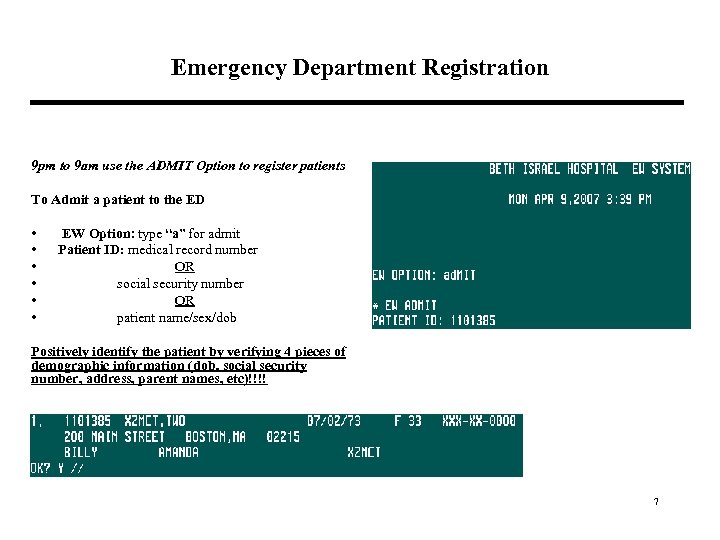
Emergency Department Registration 9 pm to 9 am use the ADMIT Option to register patients To Admit a patient to the ED • • • EW Option: type “a” for admit Patient ID: medical record number OR social security number OR patient name/sex/dob Positively identify the patient by verifying 4 pieces of demographic information (dob, social security number, address, parent names, etc)!!!! 7
BEST PRACTICE GUIDELINES FOR REGISTRATIONS 1. ) Double check ALL registration info. 2. ) Ask for spelling of any information that you are unsure of…. whether that is the patient’s name or street address. 3. ) Do not re-iterate information that is in the system to a patient…For example, ask them what their address is, DO NOT offer them the address that is in the system. If everything matches, except the address, then ask the patient if they lived at the address that is listed in the system in the past. 4. ) If a patient is in the ED and you are asked to change ANYTHING in that registration, the expectation is that you will double check ALL registration fields to ensure that we have not registered the wrong person in error…. and CERTAINLY not alter a registration of an existing patient in the system! If at any point in a patients visit to the ED you are asked to alter the patient name, date of birth, and/or social security number, that should be a RED flag that you may not have the correct patient! 8
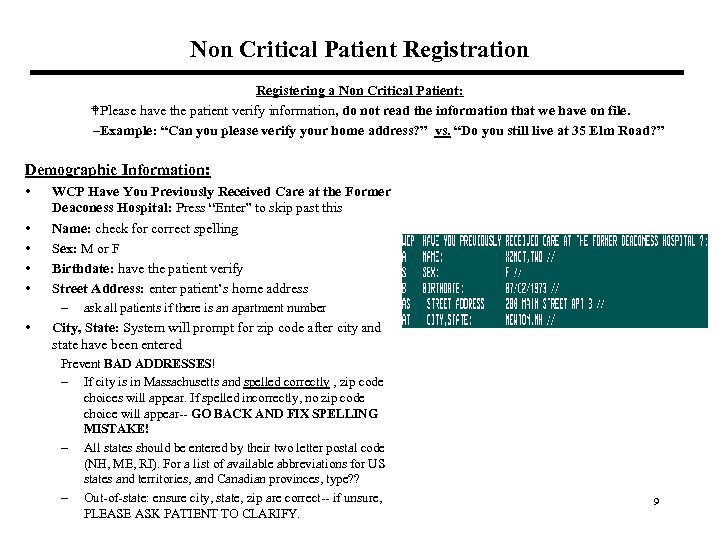
Non Critical Patient Registration Registering a Non Critical Patient: WPlease have the patient verify information, do not read the information that we have on file. –Example: “Can you please verify your home address? ” vs. “Do you still live at 35 Elm Road? ” Demographic Information: • • • WCP Have You Previously Received Care at the Former Deaconess Hospital: Press “Enter” to skip past this Name: check for correct spelling Sex: M or F Birthdate: have the patient verify Street Address: enter patient’s home address – ask all patients if there is an apartment number City, State: System will prompt for zip code after city and state have been entered Prevent BAD ADDRESSES! – If city is in Massachusetts and spelled correctly , zip code choices will appear. If spelled incorrectly, no zip code choice will appear-- GO BACK AND FIX SPELLING MISTAKE! – All states should be entered by their two letter postal code (NH, ME, RI). For a list of available abbreviations for US states and territories, and Canadian provinces, type? ? – Out-of-state: ensure city, state, zip are correct-- if unsure, PLEASE ASK PATIENT TO CLARIFY. 9
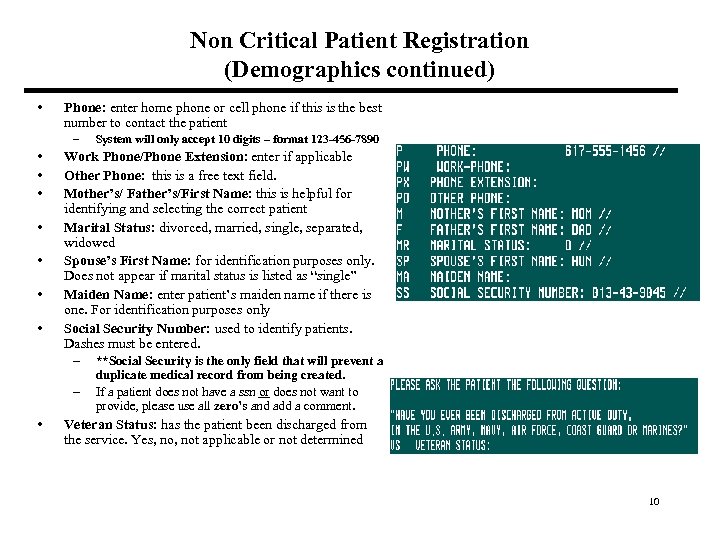
Non Critical Patient Registration (Demographics continued) • Phone: enter home phone or cell phone if this is the best number to contact the patient – • • Work Phone/Phone Extension: enter if applicable Other Phone: this is a free text field. Mother’s/ Father’s/First Name: this is helpful for identifying and selecting the correct patient Marital Status: divorced, married, single, separated, widowed Spouse’s First Name: for identification purposes only. Does not appear if marital status is listed as “single” Maiden Name: enter patient’s maiden name if there is one. For identification purposes only Social Security Number: used to identify patients. Dashes must be entered. – **Social Security is the only field that will prevent a – • System will only accept 10 digits – format 123 -456 -7890 duplicate medical record from being created. If a patient does not have a ssn or does not want to provide, please use all zero’s and add a comment. Veteran Status: has the patient been discharged from the service. Yes, not applicable or not determined 10
Non Critical Patient Registration (Disparities Questions) Introduction: Health disparities are differences between populations in presence of disease, access to health care, use of health care services, and health outcomes Cause of Health Disparities: Health disparities are caused by: • Social, economic and environmental factors (i. e. lower income groups, lead paint, air quality) • Barriers to getting health care (i. e. transportation, language, health insurance) • Differences in quality of health care (i. e. different treatments, discrimination, doctor-patient communication) Data Collection: Getting more information about our patients helps us to understand the type of health disparities that exist at BIDMC and other Boston Hospitals. The following information will be collected: • Race/ethnicity • Primary language • Highest level of education and location it was achieved 11
Non Critical Patient Registration (Disparities Questions) This information must be collected in the same way at all hospitals so that the city will have quality data from which to research and implement programs. This means that patient registration staff need to use similar interview techniques, and respond to patient concerns in the same way How data will be used: Data collected from Boston Hospitals will be used to: • • Identify differences in health care use and health outcomes for patients of different backgrounds Develop programs to address identified disparities It is important to ask patients all of the questions on the following two pages • Users will be prompted with these disparities questions. Responses are required by the system • These questions appear in an edit field for patients that already exist in CCC. It is important that these fields are updated for all patients • Scripts are written in italics next to the field name in this manual. In order to ensure that complete information is obtained, it is important to phrase the questions as shown in the scripts • Use the shift ? to see a list of responses available for each field 12
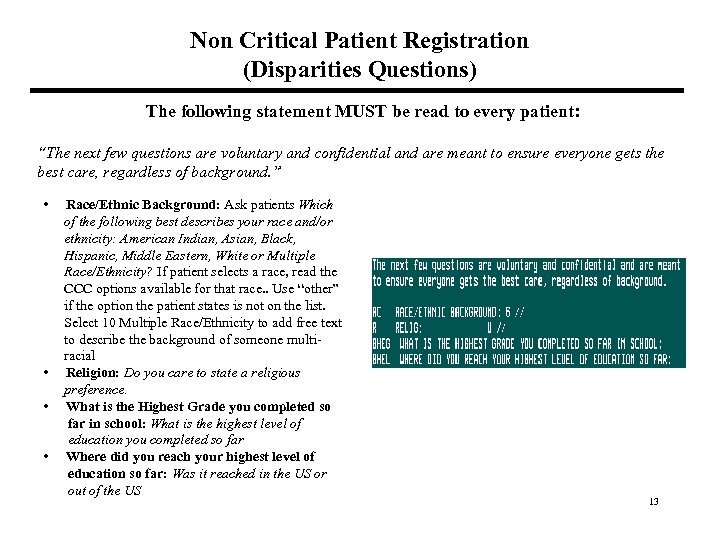
Non Critical Patient Registration (Disparities Questions) The following statement MUST be read to every patient: “The next few questions are voluntary and confidential and are meant to ensure everyone gets the best care, regardless of background. ” • Race/Ethnic Background: Ask patients Which of the following best describes your race and/or ethnicity: American Indian, Asian, Black, Hispanic, Middle Eastern, White or Multiple Race/Ethnicity? If patient selects a race, read the CCC options available for that race. . Use “other” if the option the patient states is not on the list. Select 10 Multiple Race/Ethnicity to add free text to describe the background of someone multi racial • Religion: Do you care to state a religious preference. • What is the Highest Grade you completed so far in school: What is the highest level of education you completed so far • Where did you reach your highest level of education so far: Was it reached in the US or out of the US 13
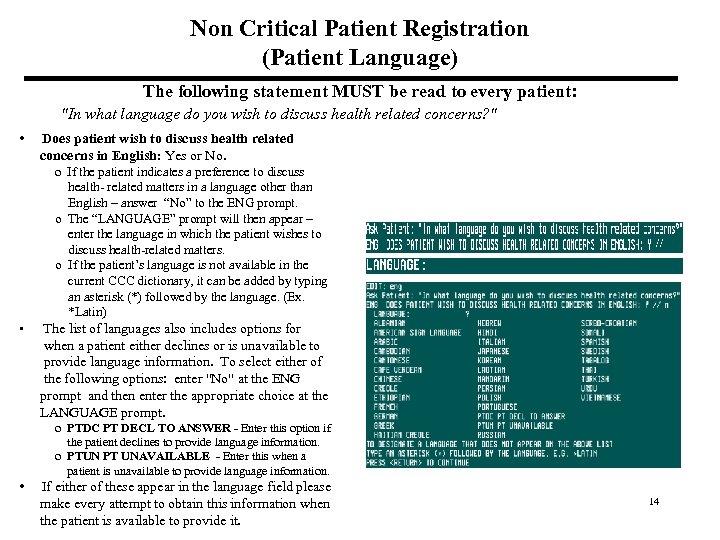
Non Critical Patient Registration (Patient Language) The following statement MUST be read to every patient: "In what language do you wish to discuss health related concerns? " • Does patient wish to discuss health related concerns in English: Yes or No. o If the patient indicates a preference to discuss health- related matters in a language other than English – answer “No” to the ENG prompt. o The “LANGUAGE” prompt will then appear – enter the language in which the patient wishes to discuss health-related matters. o If the patient’s language is not available in the current CCC dictionary, it can be added by typing an asterisk (*) followed by the language. (Ex. *Latin) • The list of languages also includes options for when a patient either declines or is unavailable to provide language information. To select either of the following options: enter "No" at the ENG prompt and then enter the appropriate choice at the LANGUAGE prompt. o PTDC PT DECL TO ANSWER - Enter this option if the patient declines to provide language information. o PTUN PT UNAVAILABLE - Enter this when a patient is unavailable to provide language information. • If either of these appear in the language field please make every attempt to obtain this information when the patient is available to provide it. 14
Non Critical Patient Registration (Disparities Questions) General Objections: There will be times when the patient will object to the questions you are asking. Do the best you can to obtain this information. Here are some tips to get the information • If the patient thinks the answers are obvious then respond with: o I know the answer may seem obvious, but I want to make sure that I record your response • If the patient refuses to answer one of the questions then you can ask: o I understand that this question is sensitive, but your answer helps us improve the healthcare we provide to all If the patient becomes very agitated or combative then select “decline” as your response. 15
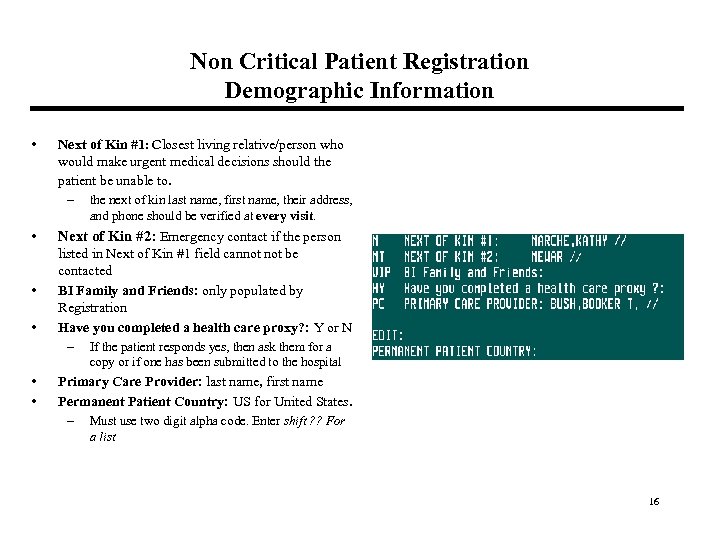
Non Critical Patient Registration Demographic Information • Next of Kin #1: Closest living relative/person who would make urgent medical decisions should the patient be unable to. – the next of kin last name, first name, their address, and phone should be verified at every visit. • • • Next of Kin #2: Emergency contact if the person listed in Next of Kin #1 field cannot be contacted BI Family and Friends: only populated by Registration Have you completed a health care proxy? : Y or N – If the patient responds yes, then ask them for a copy or if one has been submitted to the hospital • • Primary Care Provider: last name, first name Permanent Patient Country: US for United States. – Must use two digit alpha code. Enter shift ? ? For a list 16
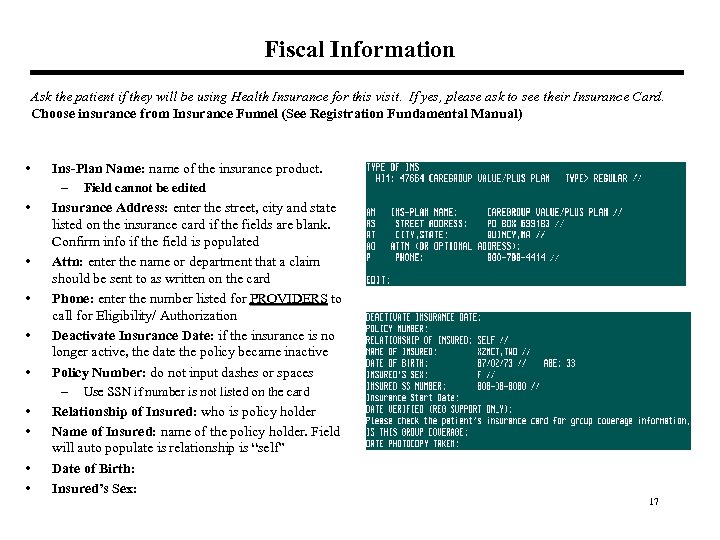
Fiscal Information Ask the patient if they will be using Health Insurance for this visit. If yes, please ask to see their Insurance Card. Choose insurance from Insurance Funnel (See Registration Fundamental Manual) • • • Ins-Plan Name: name of the insurance product. – Field cannot be edited Insurance Address: enter the street, city and state listed on the insurance card if the fields are blank. Confirm info if the field is populated Attn: enter the name or department that a claim should be sent to as written on the card Phone: enter the number listed for PROVIDERS to PROVIDERS call for Eligibility/ Authorization Deactivate Insurance Date: if the insurance is no longer active, the date the policy became inactive Policy Number: do not input dashes or spaces – Use SSN if number is not listed on the card Relationship of Insured: who is policy holder Name of Insured: name of the policy holder. Field will auto populate is relationship is “self” Date of Birth: Insured’s Sex: 17
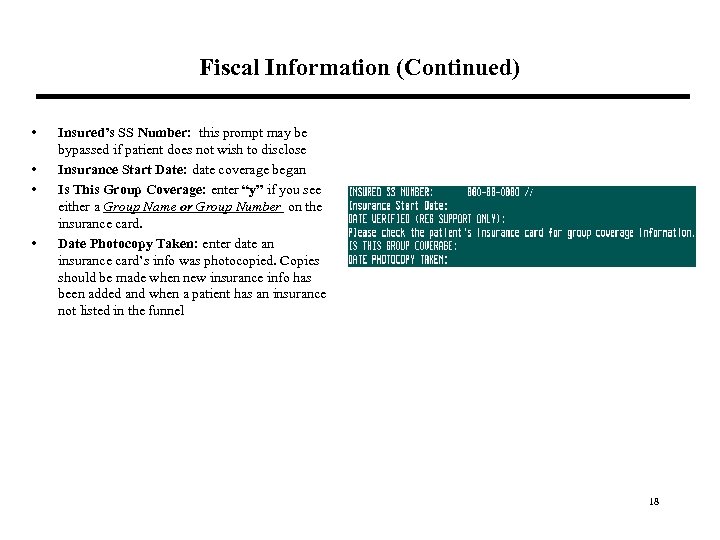
Fiscal Information (Continued) • • Insured’s SS Number: this prompt may be bypassed if patient does not wish to disclose Insurance Start Date: date coverage began Is This Group Coverage: enter “y” if you see either a Group Name or Group Number on the insurance card. Date Photocopy Taken: enter date an insurance card’s info was photocopied. Copies should be made when new insurance info has been added and when a patient has an insurance not listed in the funnel 18
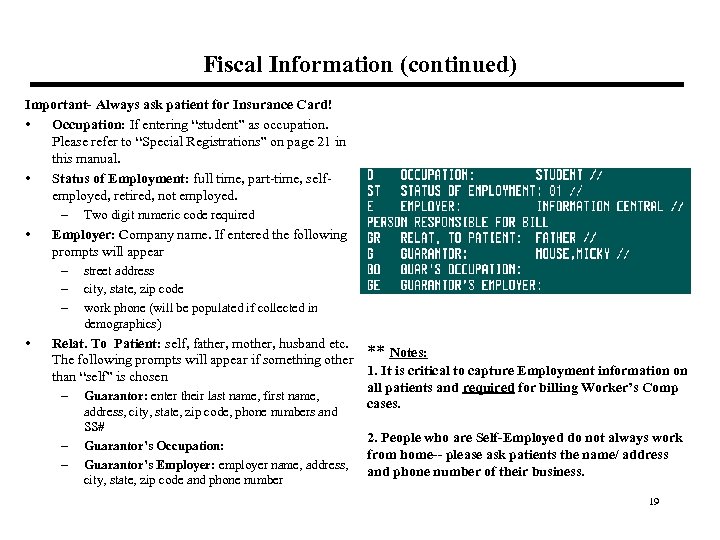
Fiscal Information (continued) Important- Always ask patient for Insurance Card! • Occupation: If entering “student” as occupation. Please refer to “Special Registrations” on page 21 in this manual. • Status of Employment: full time, part-time, selfemployed, retired, not employed. – Two digit numeric code required • Employer: Company name. If entered the following prompts will appear – street address – city, state, zip code – work phone (will be populated if collected in demographics) • Relat. To Patient: self, father, mother, husband etc. ** Notes: The following prompts will appear if something other 1. It is critical to capture Employment information on than “self” is chosen all patients and required for billing Worker’s Comp – Guarantor: enter their last name, first name, cases. – – address, city, state, zip code, phone numbers and SS# Guarantor’s Occupation: Guarantor’s Employer: employer name, address, city, state, zip code and phone number 2. People who are Self-Employed do not always work from home-- please ask patients the name/ address and phone number of their business. 19
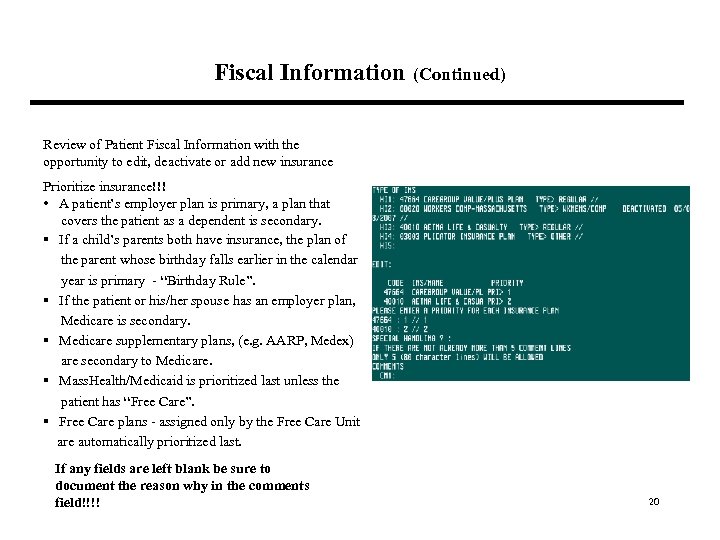
Fiscal Information (Continued) Review of Patient Fiscal Information with the opportunity to edit, deactivate or add new insurance Prioritize insurance!!! • A patient’s employer plan is primary, a plan that covers the patient as a dependent is secondary. § If a child’s parents both have insurance, the plan of the parent whose birthday falls earlier in the calendar year is primary - “Birthday Rule”. § If the patient or his/her spouse has an employer plan, Medicare is secondary. § Medicare supplementary plans, (e. g. AARP, Medex) are secondary to Medicare. § Mass. Health/Medicaid is prioritized last unless the patient has “Free Care”. § Free Care plans - assigned only by the Free Care Unit are automatically prioritized last. If any fields are left blank be sure to document the reason why in the comments field!!!! 20
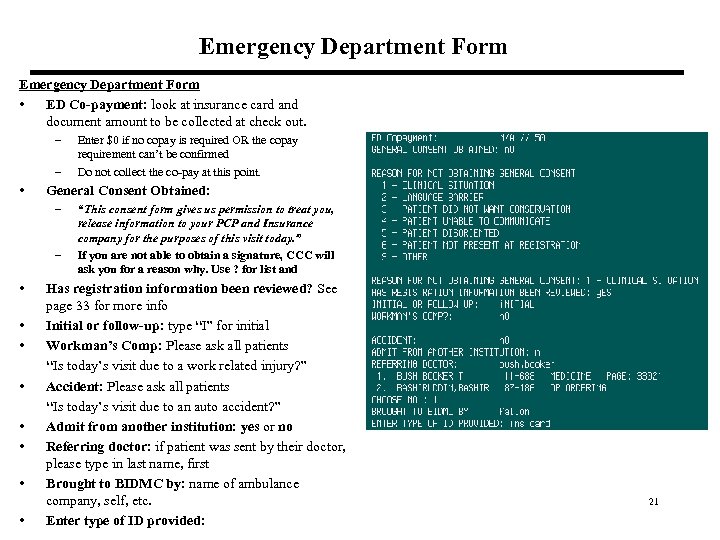
Emergency Department Form • ED Co-payment: look at insurance card and document amount to be collected at check out. – – • Enter $0 if no copay is required OR the copay requirement can’t be confirmed Do not collect the co-pay at this point. General Consent Obtained: – – “This consent form gives us permission to treat you, release information to your PCP and Insurance company for the purposes of this visit today. ” If you are not able to obtain a signature, CCC will ask you for a reason why. Use ? for list and • Has registration information been reviewed? See page 33 for more info • Initial or follow-up: type “I” for initial • Workman’s Comp: Please ask all patients “Is today’s visit due to a work related injury? ” • Accident: Please ask all patients “Is today’s visit due to an auto accident? ” • Admit from another institution: yes or no • Referring doctor: if patient was sent by their doctor, please type in last name, first • Brought to BIDMC by: name of ambulance company, self, etc. • Enter type of ID provided: 21
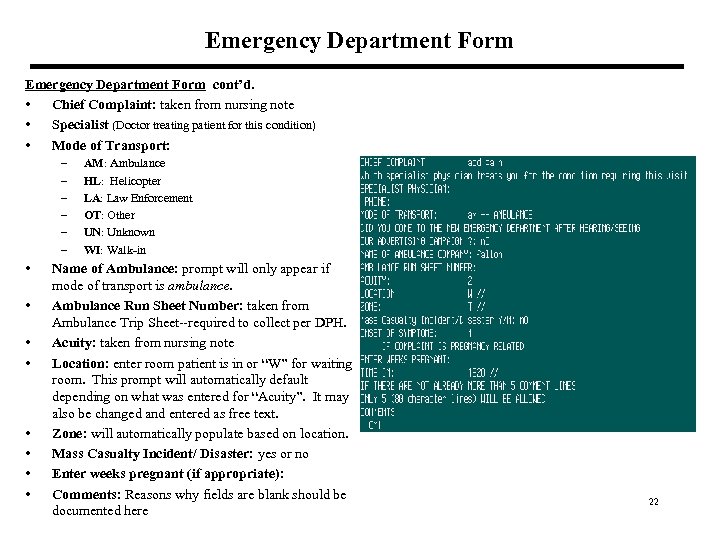
Emergency Department Form cont’d. • Chief Complaint: taken from nursing note • Specialist (Doctor treating patient for this condition) • Mode of Transport: – – – • • AM: Ambulance HL: Helicopter LA: Law Enforcement OT: Other UN: Unknown WI: Walk-in Name of Ambulance: prompt will only appear if mode of transport is ambulance. Ambulance Run Sheet Number: taken from Ambulance Trip Sheet--required to collect per DPH. Acuity: taken from nursing note Location: enter room patient is in or “W” for waiting room. This prompt will automatically default depending on what was entered for “Acuity”. It may also be changed and entered as free text. Zone: will automatically populate based on location. Mass Casualty Incident/ Disaster: yes or no Enter weeks pregnant (if appropriate): Comments: Reasons why fields are blank should be documented here 22
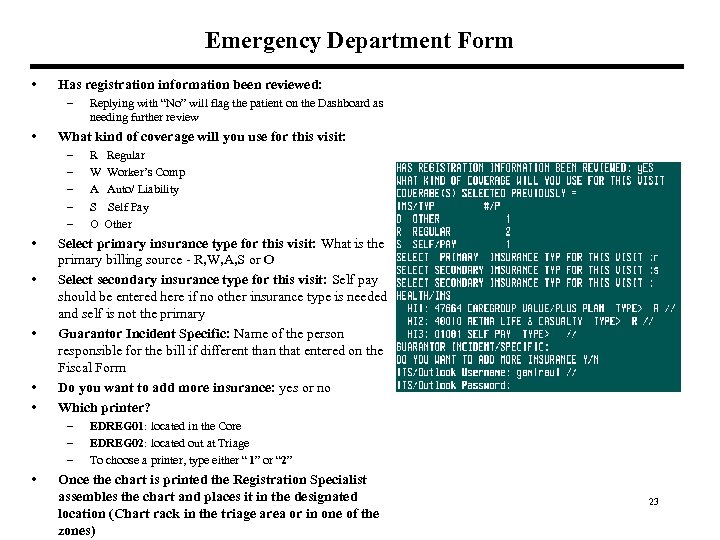
Emergency Department Form • Has registration information been reviewed: – • What kind of coverage will you use for this visit: – – – • • • R Regular W Worker’s Comp A Auto/ Liability S Self Pay O Other Select primary insurance type for this visit: What is the primary billing source - R, W, A, S or O Select secondary insurance type for this visit: Self pay should be entered here if no other insurance type is needed and self is not the primary Guarantor Incident Specific: Name of the person responsible for the bill if different than that entered on the Fiscal Form Do you want to add more insurance: yes or no Which printer? – – – • Replying with “No” will flag the patient on the Dashboard as needing further review EDREG 01: located in the Core EDREG 02: located out at Triage To choose a printer, type either “ 1” or “ 2” Once the chart is printed the Registration Specialist assembles the chart and places it in the designated location (Chart rack in the triage area or in one of the zones) 23
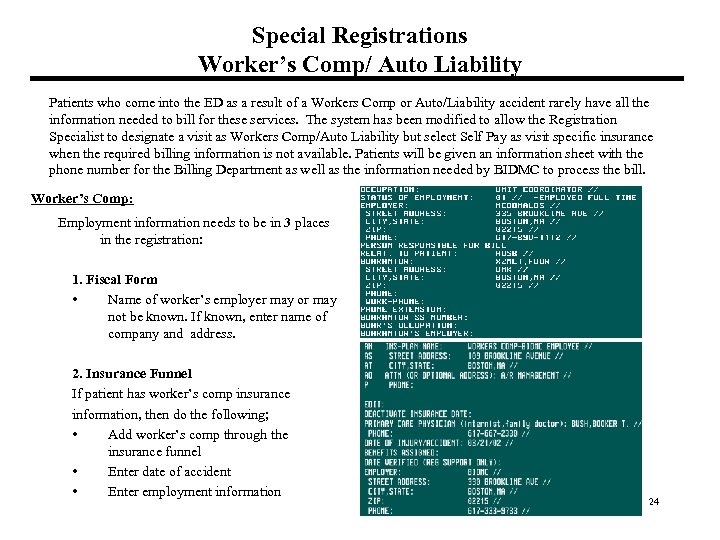
Special Registrations Worker’s Comp/ Auto Liability Patients who come into the ED as a result of a Workers Comp or Auto/Liability accident rarely have all the information needed to bill for these services. The system has been modified to allow the Registration Specialist to designate a visit as Workers Comp/Auto Liability but select Self Pay as visit specific insurance when the required billing information is not available. Patients will be given an information sheet with the phone number for the Billing Department as well as the information needed by BIDMC to process the bill. Worker’s Comp: Employment information needs to be in 3 places in the registration: 1. Fiscal Form • Name of worker’s employer may or may not be known. If known, enter name of company and address. 2. Insurance Funnel If patient has worker’s comp insurance information, then do the following; • Add worker’s comp through the insurance funnel • Enter date of accident • Enter employment information 24
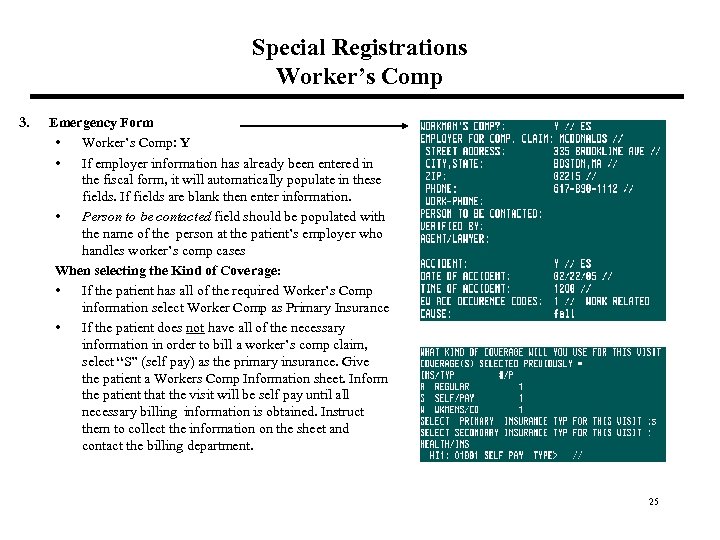
Special Registrations Worker’s Comp 3. Emergency Form • Worker’s Comp: Y • If employer information has already been entered in the fiscal form, it will automatically populate in these fields. If fields are blank then enter information. • Person to be contacted field should be populated with the name of the person at the patient’s employer who handles worker’s comp cases When selecting the Kind of Coverage: • If the patient has all of the required Worker’s Comp information select Worker Comp as Primary Insurance • If the patient does not have all of the necessary information in order to bill a worker’s comp claim, select “S” (self pay) as the primary insurance. Give the patient a Workers Comp Information sheet. Inform the patient that the visit will be self pay until all necessary billing information is obtained. Instruct them to collect the information on the sheet and contact the billing department. 25
Worker’s Comp – BIDMC and Joslin Diabetes Center Employees Effective January 2006, BIDMC and its Employee Occupational Health Department contracted with the Joslin Diabetes Center to provide Employee Occupational Health services to their employees. Effective January 2007, BIDMC and its Employee Occupational Health Department contracted with HMFP to provide Employee Occupational Health services to their employees. BIDMC, Joslin Diabetes and HMFP employees presenting with a work related injury are to be handled as follows: • When a BIDMC employee comes to the ED with a work related injury, they are to be registered using the BIDMC Employee - Workers' Comp Insurance Plan Code (60010). This plan is located under Workers Comp in the insurance funnel. • When an HMFP employee comes to the ED with a work related injury, they are to be registered using the HMFP Worker’s Comp Insurance Plan Code (91033). This plan is located under Workers Comp in the insurance funnel. • When a Joslin Diabetes Center employee comes to the ED with a work related injury, they are to be registered using the Joslin Employee Health Insurance Plan Code (91031). This plan IS NOT located under Workers Comp in the insurance funnel. • Place the Employee Occupational Health sticker on the chart. Placing the sticker on the chart is a VERY important piece of the process since this is a trigger for the Unit Coordinators (UCOs) to copy the chart and send it to Employee Occupational Health. 26
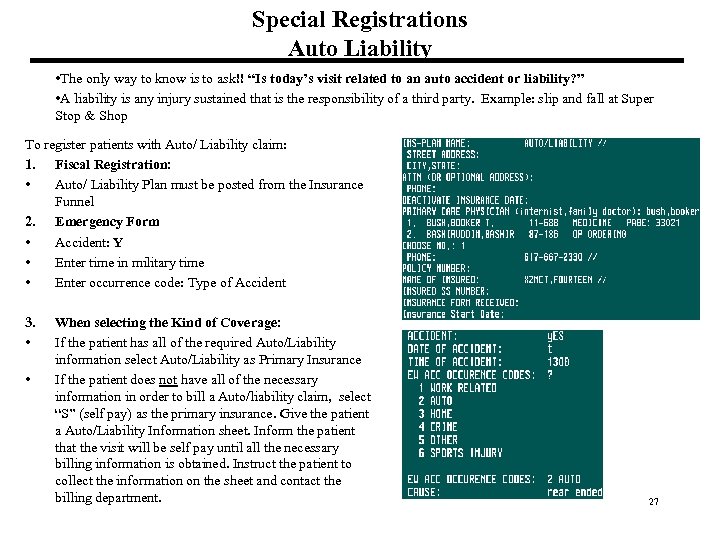
Special Registrations Auto Liability • The only way to know is to ask!! “Is today’s visit related to an auto accident or liability? ” • A liability is any injury sustained that is the responsibility of a third party. Example: slip and fall at Super Stop & Shop To register patients with Auto/ Liability claim: 1. Fiscal Registration: • Auto/ Liability Plan must be posted from the Insurance Funnel 2. Emergency Form • Accident: Y • Enter time in military time • Enter occurrence code: Type of Accident 3. • • When selecting the Kind of Coverage: If the patient has all of the required Auto/Liability information select Auto/Liability as Primary Insurance If the patient does not have all of the necessary information in order to bill a Auto/liability claim, select “S” (self pay) as the primary insurance. Give the patient a Auto/Liability Information sheet. Inform the patient that the visit will be self pay until all the necessary billing information is obtained. Instruct the patient to collect the information on the sheet and contact the billing department. 27
Worker’s Comp/Auto Liability Scripting Ø Script: Workers Comp/Auto Liability • For patients that have some information needed to bill: “I have entered the information that you have provided regarding your workers comp/auto liability information. However, there is additional information needed in order for the billing dept to bill your services correctly. Here is a form with a list of the information required to ensure proper billing. Please contact our Billing office once you have collected all of the information necessary. The phone number is on the form. ” • For patients that have no information: “Since you do not have any of your workers comp/auto liability information, here is a form with a list of the information required to ensure proper billing. Please contact our Billing office once you have collected all of the information necessary. The phone number is on the form. ” 28
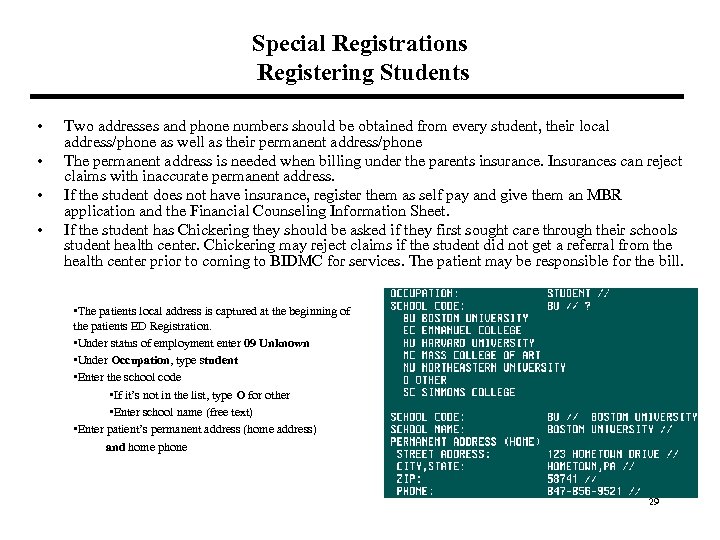
Special Registrations Registering Students • • Two addresses and phone numbers should be obtained from every student, their local address/phone as well as their permanent address/phone The permanent address is needed when billing under the parents insurance. Insurances can reject claims with inaccurate permanent address. If the student does not have insurance, register them as self pay and give them an MBR application and the Financial Counseling Information Sheet. If the student has Chickering they should be asked if they first sought care through their schools student health center. Chickering may reject claims if the student did not get a referral from the health center prior to coming to BIDMC for services. The patient may be responsible for the bill. • The patients local address is captured at the beginning of the patients ED Registration. • Under status of employment enter 09 Unknown • Under Occupation, type student • Enter the school code • If it’s not in the list, type O for other • Enter school name (free text) • Enter patient’s permanent address (home address) and home phone 29
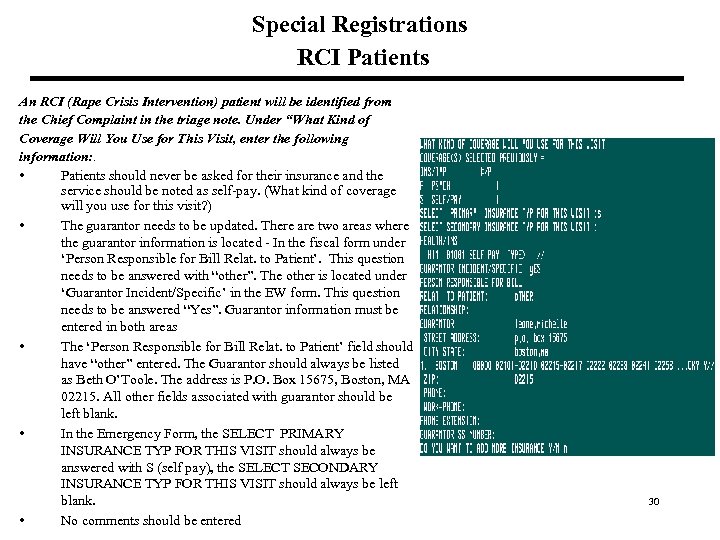
Special Registrations RCI Patients An RCI (Rape Crisis Intervention) patient will be identified from the Chief Complaint in the triage note. Under “What Kind of Coverage Will You Use for This Visit, enter the following information: . • Patients should never be asked for their insurance and the service should be noted as self-pay. (What kind of coverage will you use for this visit? ) • The guarantor needs to be updated. There are two areas where the guarantor information is located - In the fiscal form under ‘Person Responsible for Bill Relat. to Patient’. This question needs to be answered with “other”. The other is located under ‘Guarantor Incident/Specific’ in the EW form. This question needs to be answered “Yes”. Guarantor information must be entered in both areas • The ‘Person Responsible for Bill Relat. to Patient’ field should have “other” entered. The Guarantor should always be listed as Beth O’Toole. The address is P. O. Box 15675, Boston, MA 02215. All other fields associated with guarantor should be left blank. • In the Emergency Form, the SELECT PRIMARY INSURANCE TYP FOR THIS VISIT should always be answered with S (self pay), the SELECT SECONDARY INSURANCE TYP FOR THIS VISIT should always be left blank. • No comments should be entered 30
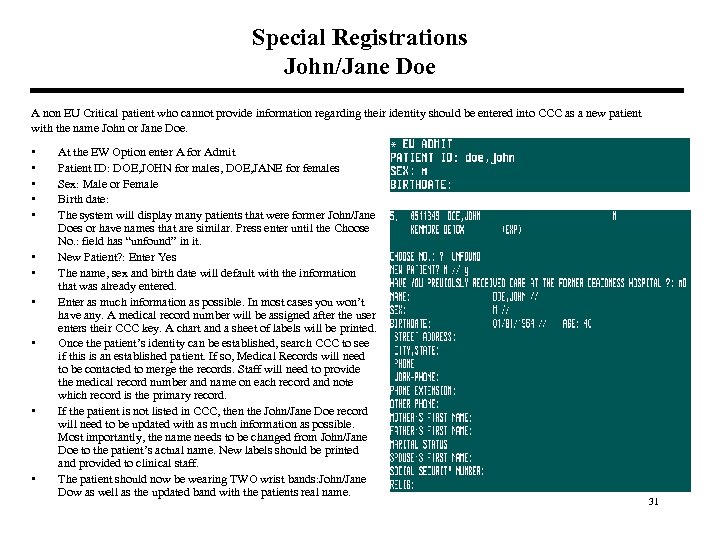
Special Registrations John/Jane Doe A non EU Critical patient who cannot provide information regarding their identity should be entered into CCC as a new patient with the name John or Jane Doe. • • • At the EW Option enter A for Admit Patient ID: DOE, JOHN for males, DOE, JANE for females Sex: Male or Female Birth date: The system will display many patients that were former John/Jane Does or have names that are similar. Press enter until the Choose No. : field has “unfound” in it. New Patient? : Enter Yes The name, sex and birth date will default with the information that was already entered. Enter as much information as possible. In most cases you won’t have any. A medical record number will be assigned after the user enters their CCC key. A chart and a sheet of labels will be printed. Once the patient’s identity can be established, search CCC to see if this is an established patient. If so, Medical Records will need to be contacted to merge the records. Staff will need to provide the medical record number and name on each record and note which record is the primary record. If the patient is not listed in CCC, then the John/Jane Doe record will need to be updated with as much information as possible. Most importantly, the name needs to be changed from John/Jane Doe to the patient’s actual name. New labels should be printed and provided to clinical staff. The patient should now be wearing TWO wrist bands: John/Jane Dow as well as the updated band with the patients real name. 31
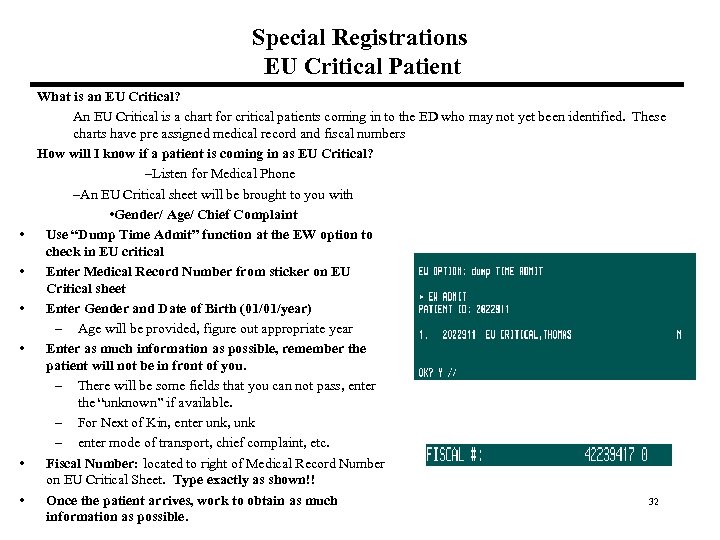
Special Registrations EU Critical Patient • • • What is an EU Critical? An EU Critical is a chart for critical patients coming in to the ED who may not yet been identified. These charts have pre assigned medical record and fiscal numbers How will I know if a patient is coming in as EU Critical? –Listen for Medical Phone –An EU Critical sheet will be brought to you with • Gender/ Age/ Chief Complaint Use “Dump Time Admit” function at the EW option to check in EU critical Enter Medical Record Number from sticker on EU Critical sheet Enter Gender and Date of Birth (01/01/year) – Age will be provided, figure out appropriate year Enter as much information as possible, remember the patient will not be in front of you. – There will be some fields that you can not pass, enter the “unknown” if available. – For Next of Kin, enter unk, unk – enter mode of transport, chief complaint, etc. Fiscal Number: located to right of Medical Record Number on EU Critical Sheet. Type exactly as shown!! Once the patient arrives, work to obtain as much 32 information as possible.
Special Registrations EU Critical Patient (Continued) • Once the patient arrives, work to obtain as much information as possible. – During weekdays a social worker is usually available to follow up with obtaining additional information regarding patient’s identity. – When the social worker is not available it is staff’s responsibility to obtain this information. • If the EU Critical patient can be identified, the staff must check CCC to see if this is an existing patient. • If this is not an existing patient, then staff must use the Edit option to update the EU Critical patient record. It is very important to change the name from EU Critical to the patient’s actual name. All other information available at this time should also be entered. • If this is an existing patient, then staff must immediately contact Medical Records at 7 -3710. (See “Medical Records Merge” in this manual regarding merging medical records). The EU Critical record must be updated with the patient’s name and DOB before contacting Medical Records. • Once the records are merged (usually complete within five minutes of the call) or if a new registration is created by changing the EU Critical name to the patient’s actual name, staff must print a new encounter sheet (face sheet) and labels. If the record is available, the old encounter sheet should be replaced with the new one and all EU Critical sheets should be relabeled with a new label. If the record is NOT available then the encounter sheet and labels should be handed directly to the nurse caring for this patient. • Place a second wristband on the patient. This wristband should contain the patients actual name. Do not remove the EU Critical wristband. • Staff will need to update the old medical record number (which will be used as the primary record) with any insurance information entered in the EU Critical record. The merge will not update the old record with 33 this information
Free Care/Uninsured (Health Safety Net) § Patients who do not have health care insurance should be given a copy of the Health Safety Net Handout sheet. This sheet has information regarding one’s eligibility for financial assistance. § Patients can contact the Financial Counseling Office at 617 667 -5661. They can visit the office which is located on the East Campus in Rabb Building 1 st floor. Their hours are 8 am – 4: 30 pm, Monday – Friday. § Staff should encourage patients to contact Financial Assistance right away because waiting can cause an increase in their cost of care because coverage (depending on what they are eligible for) may be retroactive to as few as ten days. 34
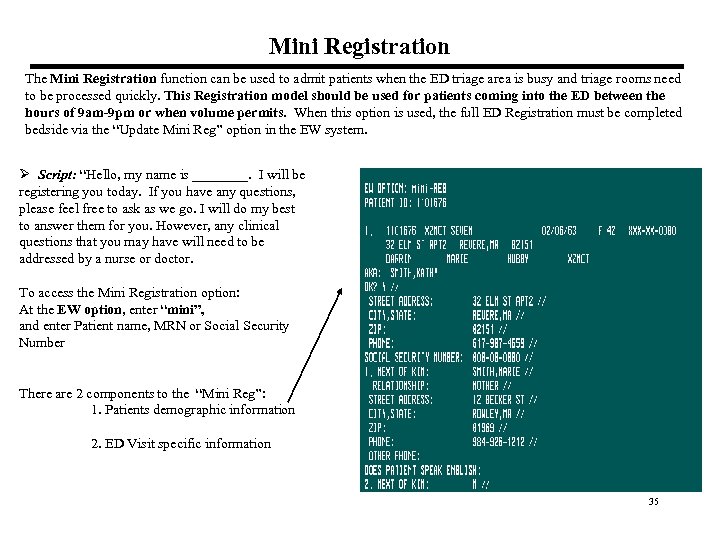
Mini Registration The Mini Registration function can be used to admit patients when the ED triage area is busy and triage rooms need to be processed quickly. This Registration model should be used for patients coming into the ED between the hours of 9 am-9 pm or when volume permits. When this option is used, the full ED Registration must be completed bedside via the “Update Mini Reg” option in the EW system. Ø Script: “Hello, my name is ____. I will be registering you today. If you have any questions, please feel free to ask as we go. I will do my best to answer them for you. However, any clinical questions that you may have will need to be addressed by a nurse or doctor. To access the Mini Registration option: At the EW option, enter “mini”, and enter Patient name, MRN or Social Security Number There are 2 components to the “Mini Reg”: 1. Patients demographic information 2. ED Visit specific information 35
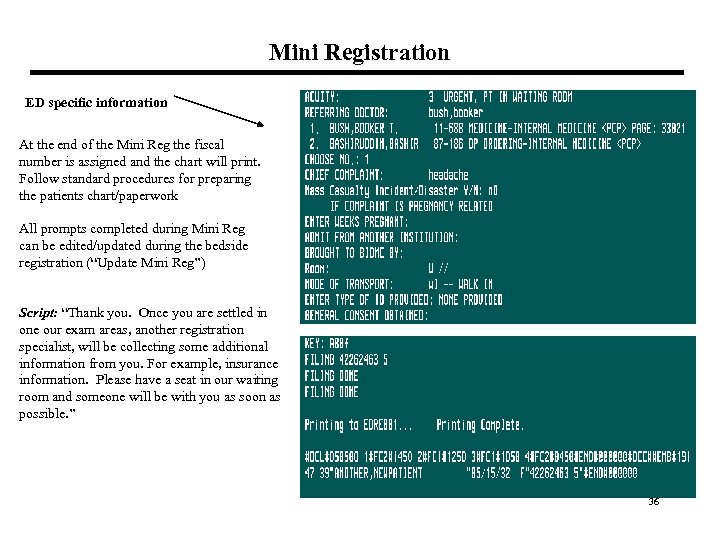
Mini Registration ED specific information At the end of the Mini Reg the fiscal number is assigned and the chart will print. Follow standard procedures for preparing the patients chart/paperwork All prompts completed during Mini Reg can be edited/updated during the bedside registration (“Update Mini Reg”) Script: “Thank you. Once you are settled in one our exam areas, another registration specialist, will be collecting some additional information from you. For example, insurance information. Please have a seat in our waiting room and someone will be with you as soon as possible. ” 36
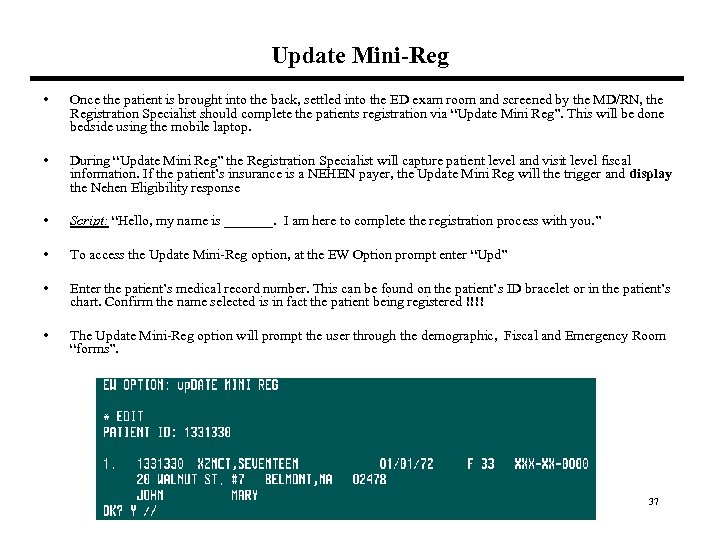
Update Mini-Reg • Once the patient is brought into the back, settled into the ED exam room and screened by the MD/RN, the Registration Specialist should complete the patients registration via “Update Mini Reg”. This will be done bedside using the mobile laptop. • During “Update Mini Reg” the Registration Specialist will capture patient level and visit level fiscal information. If the patient’s insurance is a NEHEN payer, the Update Mini Reg will the trigger and display the Nehen Eligibility response • Script: “Hello, my name is _______. I am here to complete the registration process with you. ” • To access the Update Mini-Reg option, at the EW Option prompt enter “Upd” • Enter the patient’s medical record number. This can be found on the patient’s ID bracelet or in the patient’s chart. Confirm the name selected is in fact the patient being registered !!!! • The Update Mini-Reg option will prompt the user through the demographic, Fiscal and Emergency Room “forms”. 37
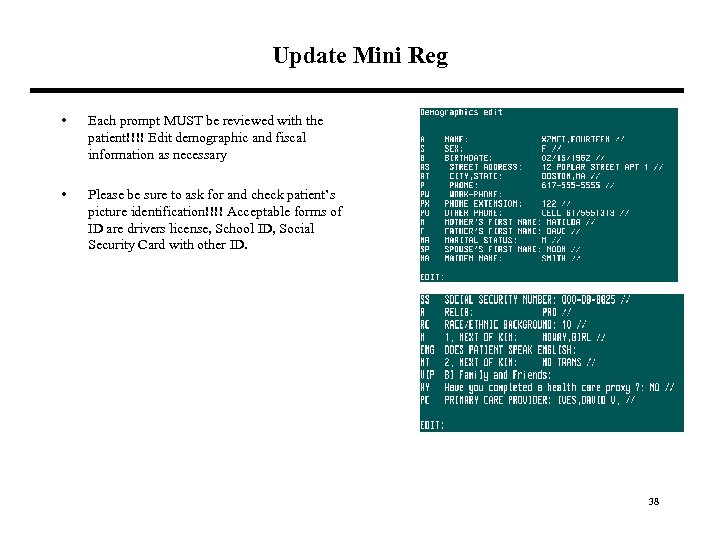
Update Mini Reg • Each prompt MUST be reviewed with the patient!!!! Edit demographic and fiscal information as necessary • Please be sure to ask for and check patient’s picture identification!!!! Acceptable forms of ID are drivers license, School ID, Social Security Card with other ID. 38
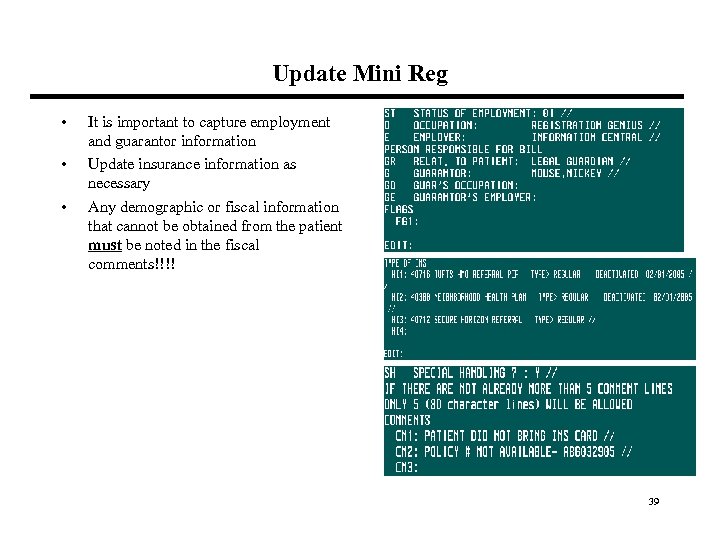
Update Mini Reg • • • It is important to capture employment and guarantor information Update insurance information as necessary Any demographic or fiscal information that cannot be obtained from the patient must be noted in the fiscal comments!!!! 39
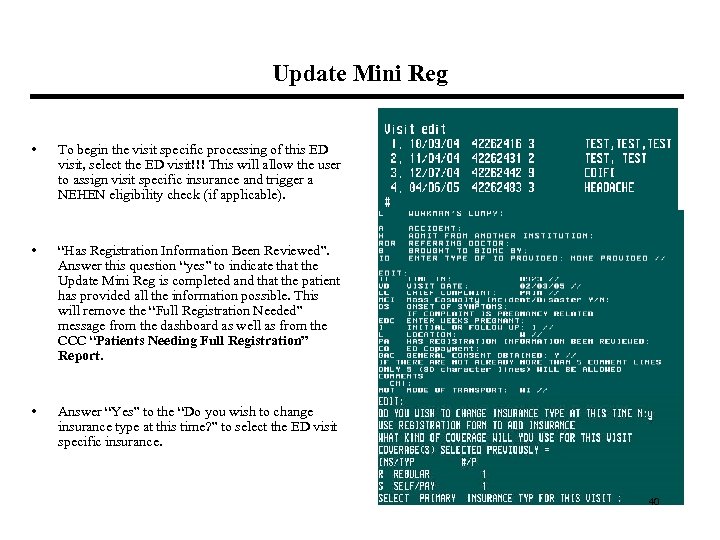
Update Mini Reg • To begin the visit specific processing of this ED visit, select the ED visit!!! This will allow the user to assign visit specific insurance and trigger a NEHEN eligibility check (if applicable). • “Has Registration Information Been Reviewed”. Answer this question “yes” to indicate that the Update Mini Reg is completed and that the patient has provided all the information possible. This will remove the “Full Registration Needed” message from the dashboard as well as from the CCC “Patients Needing Full Registration” Report. • Answer “Yes” to the “Do you wish to change insurance type at this time? ” to select the ED visit specific insurance. 40
Has Registration Information Been Reviewed? • “Has Registration Been Reviewed" will serve as documentation that the Registrar has, to the best of their abilities completed the patient registration. Once this question is answered YES, the registrar becomes accountable for the information captured in the patients registration. Any information that cannot be obtained from the patient should be noted in the fiscal comments and answer this question Yes. • When to answer “no”- Answer No when you are unable to complete the patients registration (and you need to come back at a later time) or if the patient has information to provide, but doesn’t have it at the moment (ie; family member in the waiting room holding their belongings including insurance card) • If Update Mini Reg has not been completed or if the answer to this question is answered “NO’, the patient will appear on the Registration screen of the ED dashboard alerting registrars that bedside registration is required/additional information is needed. (page 52) 41
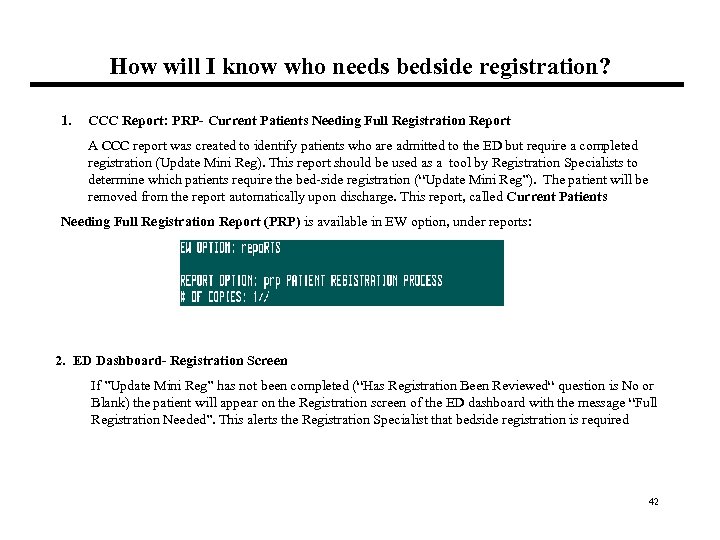
How will I know who needs bedside registration? 1. CCC Report: PRP- Current Patients Needing Full Registration Report A CCC report was created to identify patients who are admitted to the ED but require a completed registration (Update Mini Reg). This report should be used as a tool by Registration Specialists to determine which patients require the bed-side registration (“Update Mini Reg”). The patient will be removed from the report automatically upon discharge. This report, called Current Patients Needing Full Registration Report (PRP) is available in EW option, under reports: 2. ED Dashboard- Registration Screen If ”Update Mini Reg” has not been completed (“Has Registration Been Reviewed“ question is No or Blank) the patient will appear on the Registration screen of the ED dashboard with the message “Full Registration Needed”. This alerts the Registration Specialist that bedside registration is required 42
Integration of NEHEN into the ED Registration Process What is NEHEN? NEHEN is an on line insurance verification tool that is integrated with CCC. It is used to verify insurance eligibility for the following payers: : Harvard Pilgrim, Blue Cross, Tufts, Medicare, Medicaid or NHP. This eligibility check has been inserted into ED Registration flow. The eligibility response will appear at the end of the Registration process in both the “Admit” and “Update Mini Reg” options. In addition, there is a stand alone NEHEN eligibility checking option at the main EW prompt (page 32). IMPORTANT: ALWAYS READ THE RESPONSES!!! It contains important information such as patient insurance eligibility, PCP, ED Co-payment and benefit level. 43
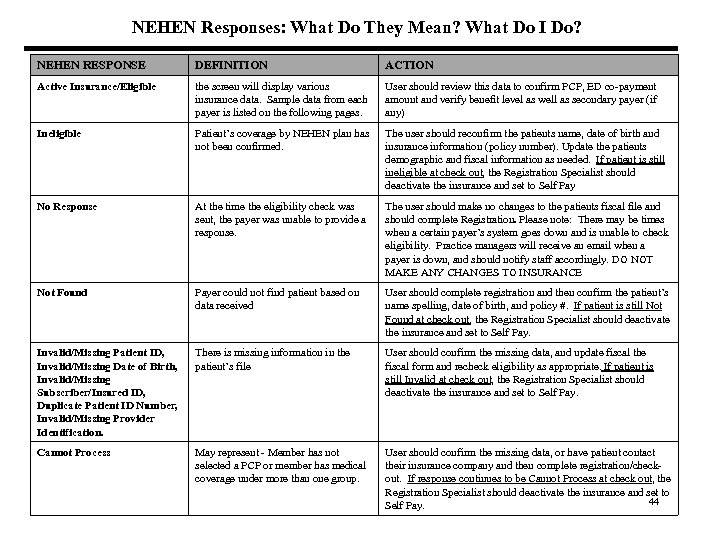
NEHEN Responses: What Do They Mean? What Do I Do? NEHEN RESPONSE DEFINITION ACTION Active Insurance/Eligible the screen will display various insurance data. Sample data from each payer is listed on the following pages. User should review this data to confirm PCP, ED co-payment amount and verify benefit level as well as secondary payer (if any) Ineligible Patient’s coverage by NEHEN plan has not been confirmed. The user should reconfirm the patients name, date of birth and insurance information (policy number). Update the patients demographic and fiscal information as needed. If patient is still ineligible at check out, the Registration Specialist should deactivate the insurance and set to Self Pay No Response At the time the eligibility check was sent, the payer was unable to provide a response. The user should make no changes to the patients fiscal file and should complete Registration. Please note: There may be times when a certain payer’s system goes down and is unable to check eligibility. Practice managers will receive an email when a payer is down, and should notify staff accordingly. DO NOT MAKE ANY CHANGES TO INSURANCE Not Found Payer could not find patient based on data received User should complete registration and then confirm the patient’s name spelling, date of birth, and policy #. If patient is still Not Found at check out, the Registration Specialist should deactivate the insurance and set to Self Pay. Invalid/Missing Patient ID, Invalid/Missing Date of Birth, Invalid/Missing Subscriber/Insured ID, Duplicate Patient ID Number, Invalid/Missing Provider Identification. There is missing information in the patient’s file User should confirm the missing data, and update fiscal the fiscal form and recheck eligibility as appropriate. If patient is still Invalid at check out, the Registration Specialist should deactivate the insurance and set to Self Pay. Cannot Process May represent - Member has not selected a PCP or member has medical coverage under more than one group. User should confirm the missing data, or have patient contact their insurance company and then complete registration/checkout. If response continues to be Cannot Process at check out, the Registration Specialist should deactivate the insurance and set to 44 Self Pay.
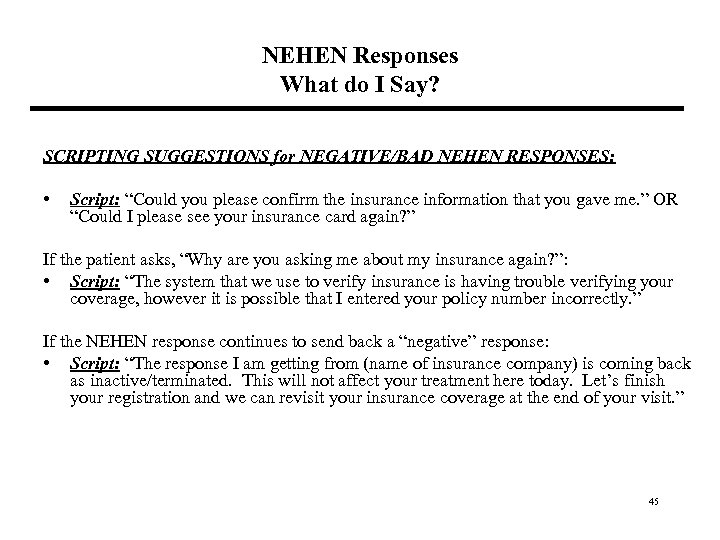
NEHEN Responses What do I Say? SCRIPTING SUGGESTIONS for NEGATIVE/BAD NEHEN RESPONSES: • Script: “Could you please confirm the insurance information that you gave me. ” OR “Could I please see your insurance card again? ” If the patient asks, “Why are you asking me about my insurance again? ”: • Script: “The system that we use to verify insurance is having trouble verifying your coverage, however it is possible that I entered your policy number incorrectly. ” If the NEHEN response continues to send back a “negative” response: • Script: “The response I am getting from (name of insurance company) is coming back as inactive/terminated. This will not affect your treatment here today. Let’s finish your registration and we can revisit your insurance coverage at the end of your visit. ” 45
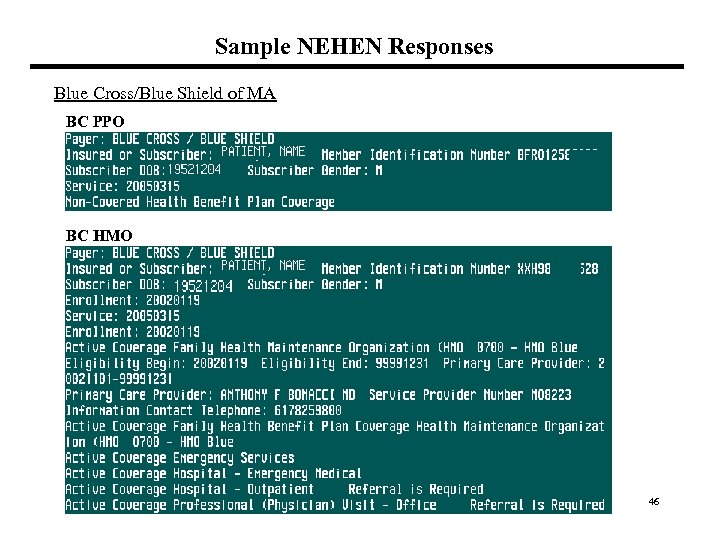
Sample NEHEN Responses Blue Cross/Blue Shield of MA BC PPO BC HMO 46
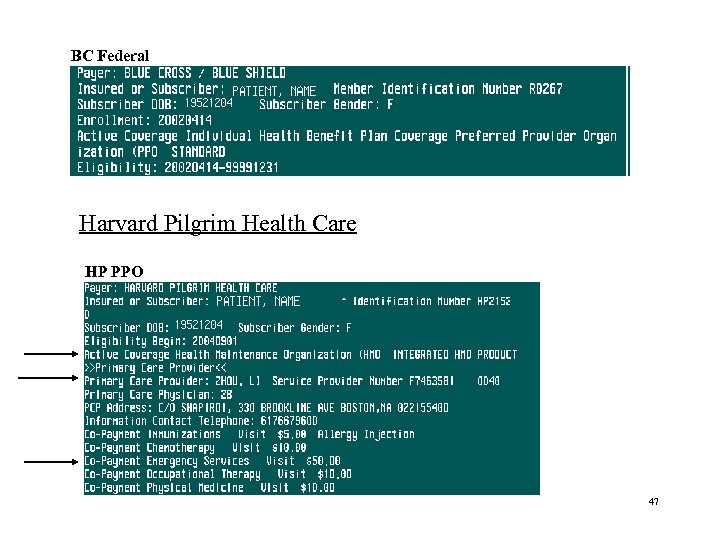
BC Federal Harvard Pilgrim Health Care HP PPO 47
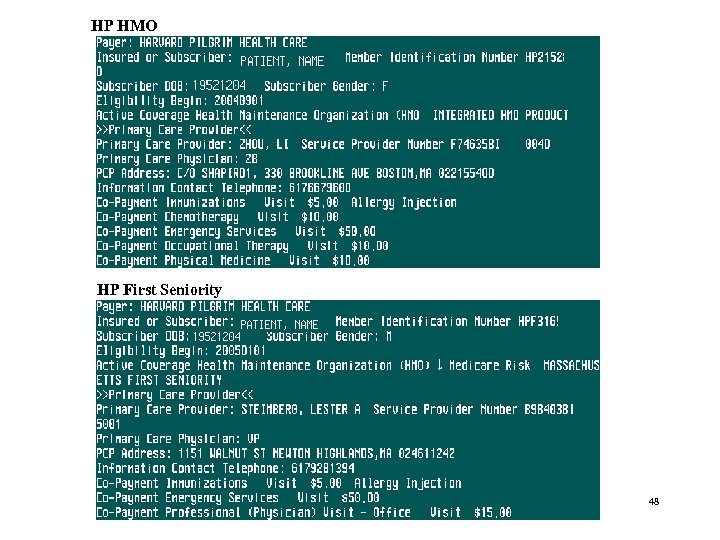
HP HMO HP First Seniority 48
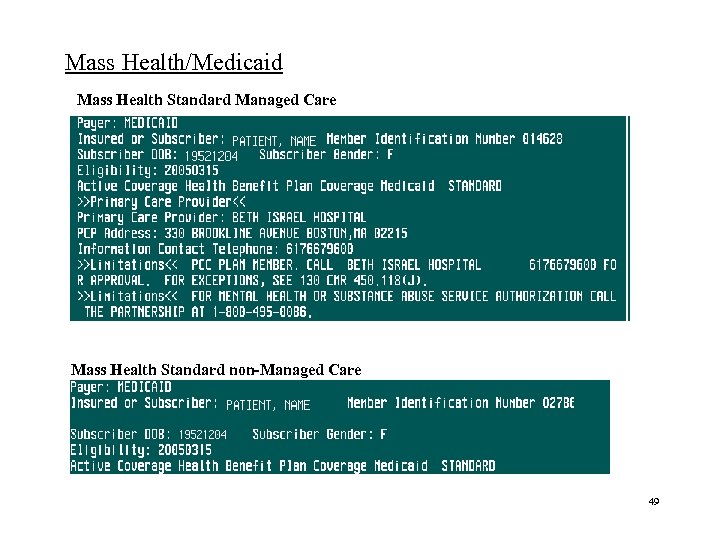
Mass Health/Medicaid Mass Health Standard Managed Care Mass Health Standard non-Managed Care 49
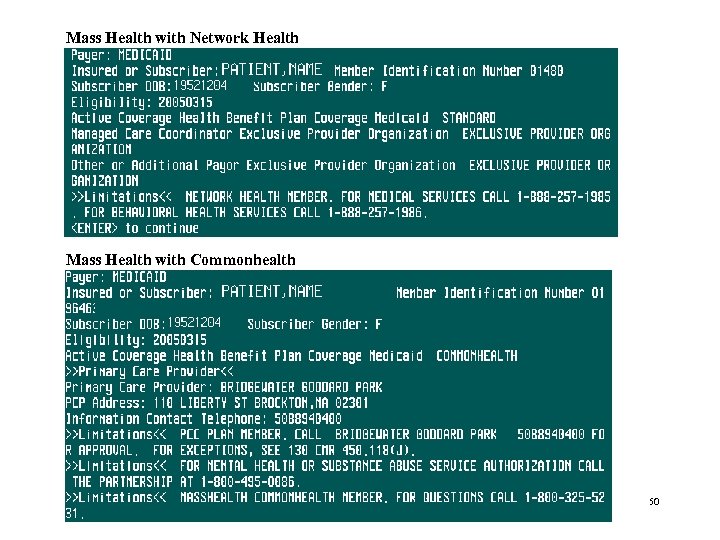
Mass Health with Network Health Mass Health with Commonhealth 50
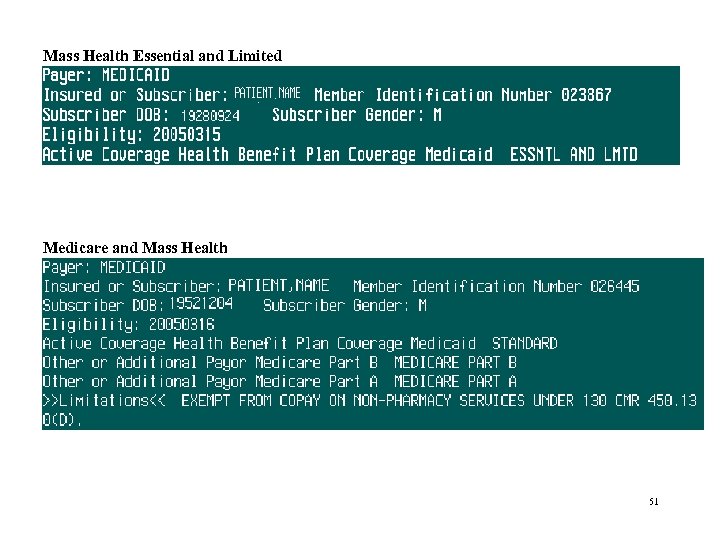
Mass Health Essential and Limited Medicare and Mass Health 51
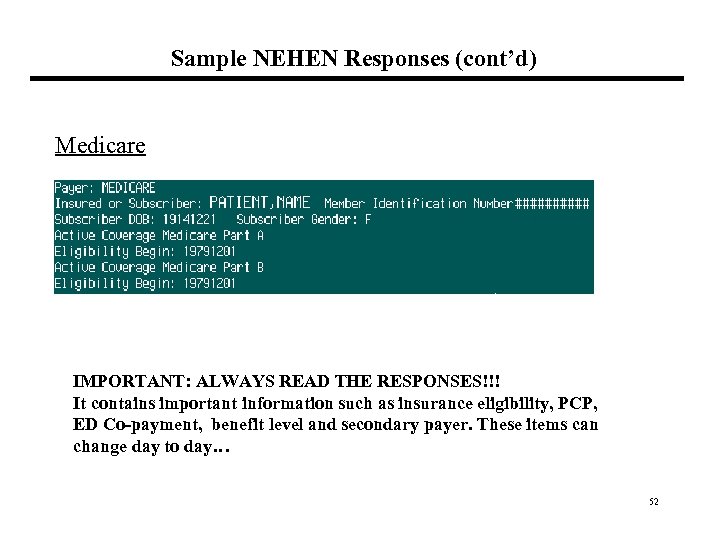
Sample NEHEN Responses (cont’d) Medicare IMPORTANT: ALWAYS READ THE RESPONSES!!! It contains important information such as insurance eligibility, PCP, ED Co-payment, benefit level and secondary payer. These items can change day to day… 52
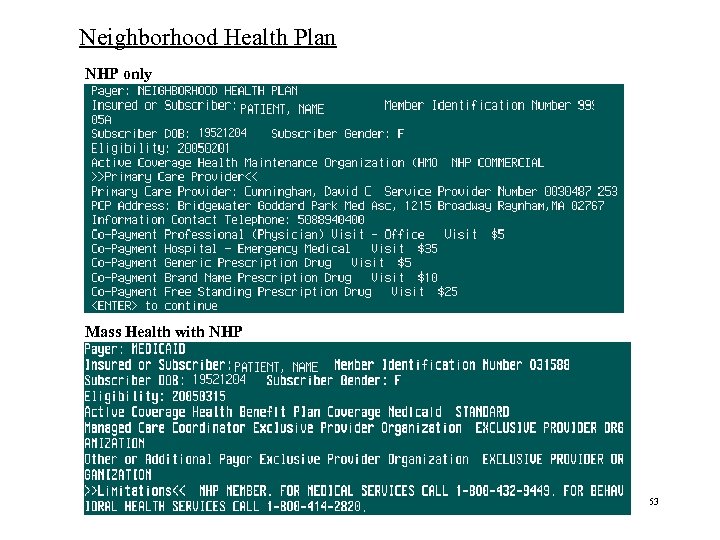
Neighborhood Health Plan NHP only Mass Health with NHP 53
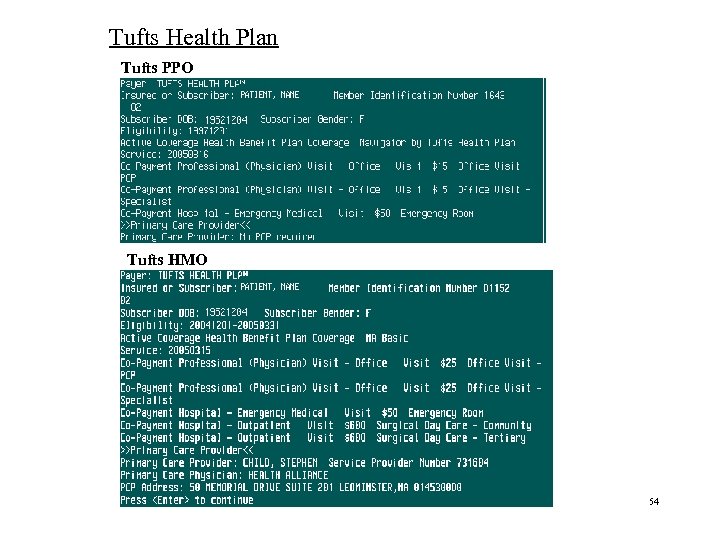
Tufts Health Plan Tufts PPO Tufts HMO 54
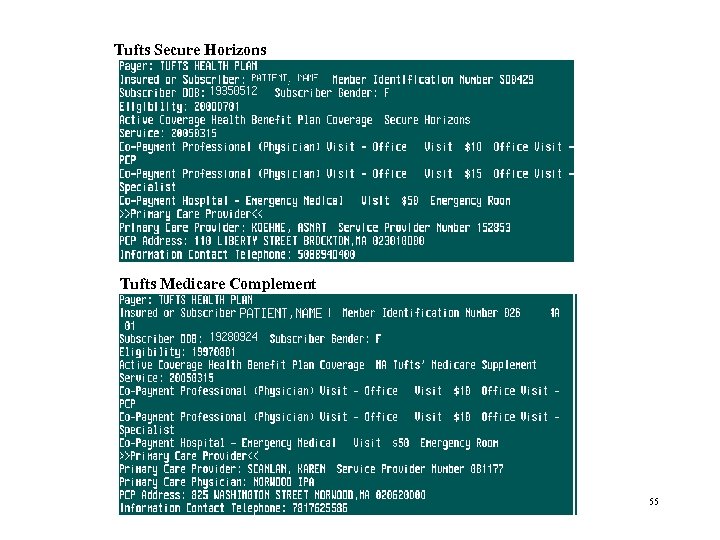
Tufts Secure Horizons Tufts Medicare Complement 55
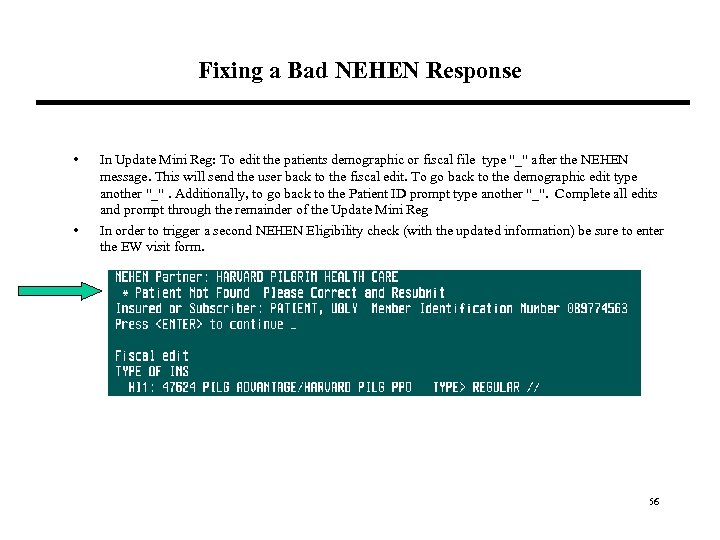
Fixing a Bad NEHEN Response • • In Update Mini Reg: To edit the patients demographic or fiscal file type "_" after the NEHEN message. This will send the user back to the fiscal edit. To go back to the demographic edit type another "_". Additionally, to go back to the Patient ID prompt type another "_". Complete all edits and prompt through the remainder of the Update Mini Reg In order to trigger a second NEHEN Eligibility check (with the updated information) be sure to enter the EW visit form. 56
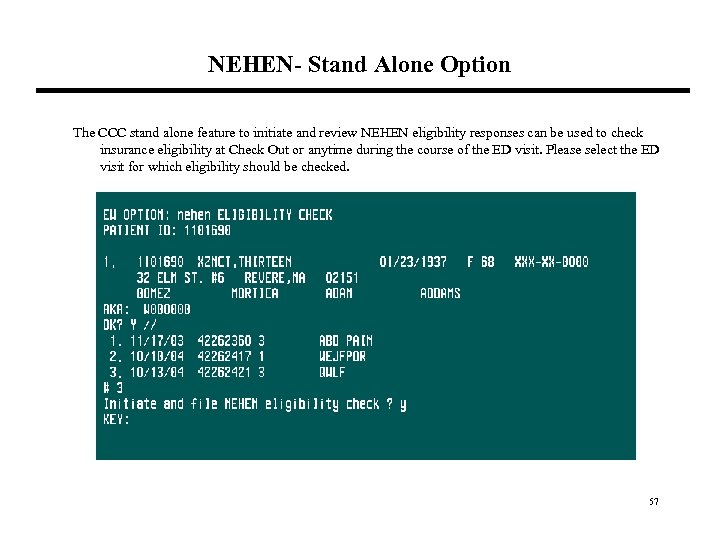
NEHEN- Stand Alone Option The CCC stand alone feature to initiate and review NEHEN eligibility responses can be used to check insurance eligibility at Check Out or anytime during the course of the ED visit. Please select the ED visit for which eligibility should be checked. 57
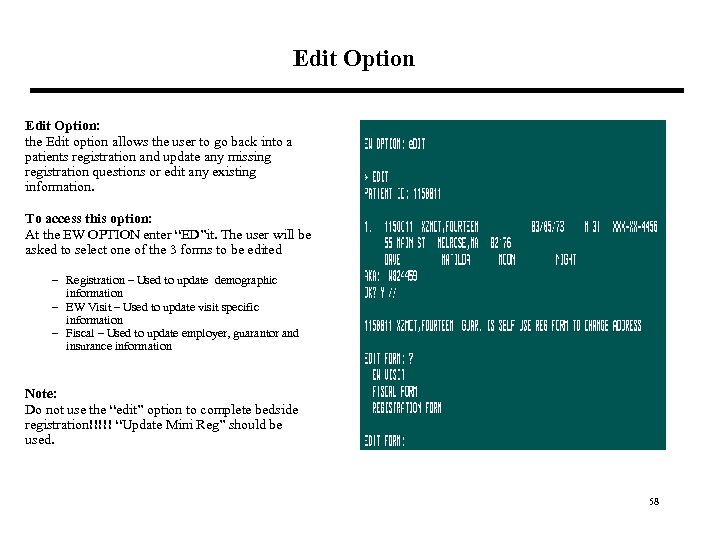
Edit Option: the Edit option allows the user to go back into a patients registration and update any missing registration questions or edit any existing information. To access this option: At the EW OPTION enter “ED”it. The user will be asked to select one of the 3 forms to be edited – Registration – Used to update demographic information – EW Visit – Used to update visit specific information – Fiscal – Used to update employer, guarantor and insurance information Note: Do not use the “edit” option to complete bedside registration!!!!! “Update Mini Reg” should be used. 58
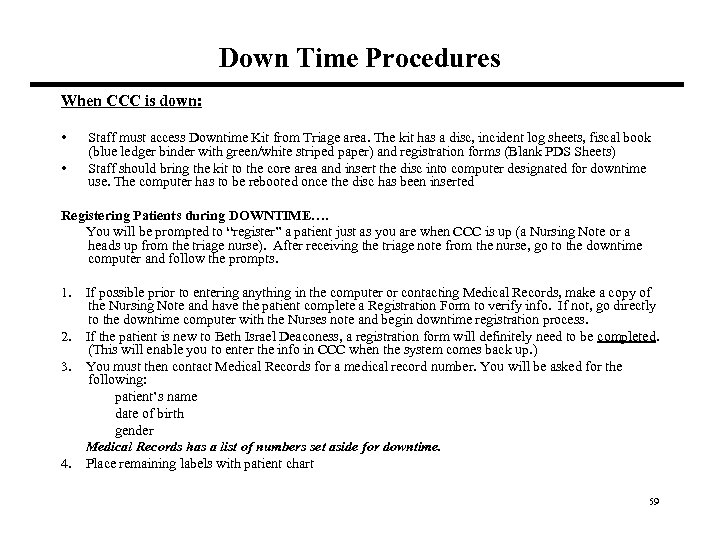
Down Time Procedures When CCC is down: • • Staff must access Downtime Kit from Triage area. The kit has a disc, incident log sheets, fiscal book (blue ledger binder with green/white striped paper) and registration forms (Blank PDS Sheets) Staff should bring the kit to the core area and insert the disc into computer designated for downtime use. The computer has to be rebooted once the disc has been inserted Registering Patients during DOWNTIME…. You will be prompted to “register” a patient just as you are when CCC is up (a Nursing Note or a heads up from the triage nurse). After receiving the triage note from the nurse, go to the downtime computer and follow the prompts. 1. If possible prior to entering anything in the computer or contacting Medical Records, make a copy of the Nursing Note and have the patient complete a Registration Form to verify info. If not, go directly to the downtime computer with the Nurses note and begin downtime registration process. 2. If the patient is new to Beth Israel Deaconess, a registration form will definitely need to be completed. (This will enable you to enter the info in CCC when the system comes back up. ) 3. You must then contact Medical Records for a medical record number. You will be asked for the following: patient’s name date of birth gender Medical Records has a list of numbers set aside for downtime. 4. Place remaining labels with patient chart 59
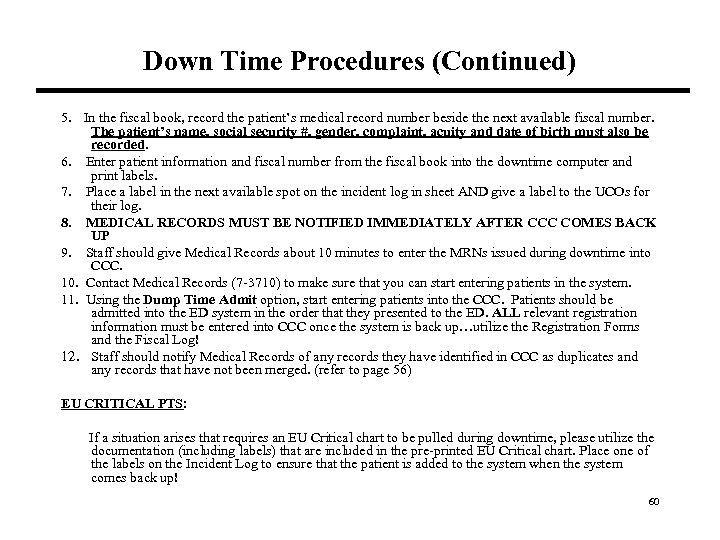
Down Time Procedures (Continued) 5. In the fiscal book, record the patient’s medical record number beside the next available fiscal number. The patient’s name, social security #, gender, complaint, acuity and date of birth must also be recorded. 6. Enter patient information and fiscal number from the fiscal book into the downtime computer and print labels. 7. Place a label in the next available spot on the incident log in sheet AND give a label to the UCOs for their log. 8. MEDICAL RECORDS MUST BE NOTIFIED IMMEDIATELY AFTER CCC COMES BACK UP 9. Staff should give Medical Records about 10 minutes to enter the MRNs issued during downtime into CCC. 10. Contact Medical Records (7 -3710) to make sure that you can start entering patients in the system. 11. Using the Dump Time Admit option, start entering patients into the CCC. Patients should be admitted into the ED system in the order that they presented to the ED. ALL relevant registration information must be entered into CCC once the system is back up…utilize the Registration Forms and the Fiscal Log! 12. Staff should notify Medical Records of any records they have identified in CCC as duplicates and any records that have not been merged. (refer to page 56) EU CRITICAL PTS: If a situation arises that requires an EU Critical chart to be pulled during downtime, please utilize the documentation (including labels) that are included in the pre-printed EU Critical chart. Place one of the labels on the Incident Log to ensure that the patient is added to the system when the system comes back up! 60
UCO DOWNTIME STEPS The following procedures are to be followed by the ED Unit Coordinators. These steps are listed here so that Registrars understand the relationship between their roles and those of the Unit Coordinators during computer downtime. 1. Get a Downtime Disposition Log from the Downtime Binder. (Downtime Binder is kept on the back counter behind the Core UCO desk) 2. After a patient is registered you should get a sticker from the Registration Specialist and ask the Registration Specialist for the time the patient came into the department. Place the sticker on the Downtime Disposition Log. Make sure to write down the time the patient came into the dept on the downtime log. 3. When a patient is discharged during downtime the nurse is responsible for informing the UCOs about the time of discharge. If the patient was in the system prior to downtime, the nurse needs to provide you with a patient sticker to add to the downtime log. In the Downtime Disposition Log, in the Disposition column, write “A” for admit or “D/C” for discharged, or “TX” for transfer. You must also find out from the RN what time the patient left the department, and write it down on the downtime log. 4. When CCC comes back up, double check with registration to see if they have entered the patients into the system. We then need to edit the time in for the patients that were registered during the downtime. Also we need to make sure that when we are timing out the patients we use the time on the downtime log. As for patients that were here prior to downtime we need to review our log to determine if any patients were discharged. If there were patients discharged during the downtime, we need to time out the patient according to the info on the downtime log. 61
UCO DOWNTIME STEPS (Continued) To edit the time a patient came into the department in CCC these are the steps you would follow once CCC is back up and registration has done there part: a. Find the patients name on the ENT Log in CCC and pick the number to the left of the patients name and hit enter. b. At the edit prompt you would type TI (for Time In) then hit enter. When the prompt for time in comes up you should take the time from the downtime log and input it there then hit enter. c. Step 3: Timing Patients Out If the patient is still in the ED continue hitting enter after you have edited the TI (Time In) until the computer prompts you to input your username and password. If the patient has been discharged from the ED continue hitting enter until you get to the prompt for Time Out and then input the time from the downtime log. 5. If a test (for example CT or MRI) is necessary for a patient’s treatment, it is possible that the physicians will notify the UCOs. The expectation is that the UCO would contact the appropriate department (for example, radiology). The completed test requisition will be picked up by with the patient for the test. 6. During downtime if a resident gives you a bed request for a patient all you need to do is look it over and make sure that it’s filled out correctly and then fax it over to admitting. There fax number is 42224. Please note: If a patient label is NOT on the Bed Request, you must add the patient’s date of birth. 62
Medical Records Merge • • Any time a patient has more than one record in CCC, they need to be merged into one record. A duplicate record may be created if staff creates a new record for a patient either as a new patient, John/Jane Doe or EU Critical. If the patient has an established record in CCC, medical records needs to be contacted to merge the records. Staff must provide medical records with the name, DOB, sex and medical record number on each record as well as identifying which record should be the primary. Check CCC periodically to see if the records have been merged. Once merged, staff should print new labels and provide them to the clinical staff Staff must review the old medical record number (the one used as the primary record) to ensure information is updated. Edit fields as necessary. Insurance information entered in the new record will not appear in the primary record after the merge has been completed. This information will have to be added to the old medical record number. Medical Records should be notified of a merge requirement well in advance of an admission, because records cannot be merged once a patient is admitted. Medical Records Phone Number is: 7 -3710 63
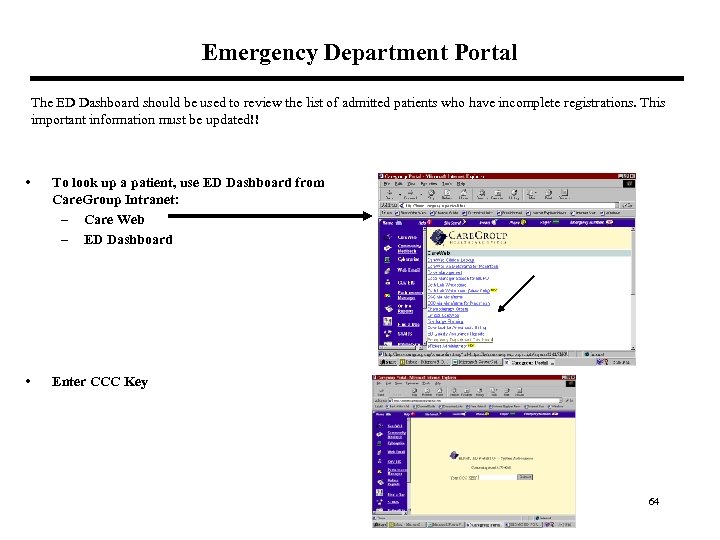
Emergency Department Portal The ED Dashboard should be used to review the list of admitted patients who have incomplete registrations. This important information must be updated!! • To look up a patient, use ED Dashboard from Care. Group Intranet: – Care Web – ED Dashboard • Enter CCC Key 64
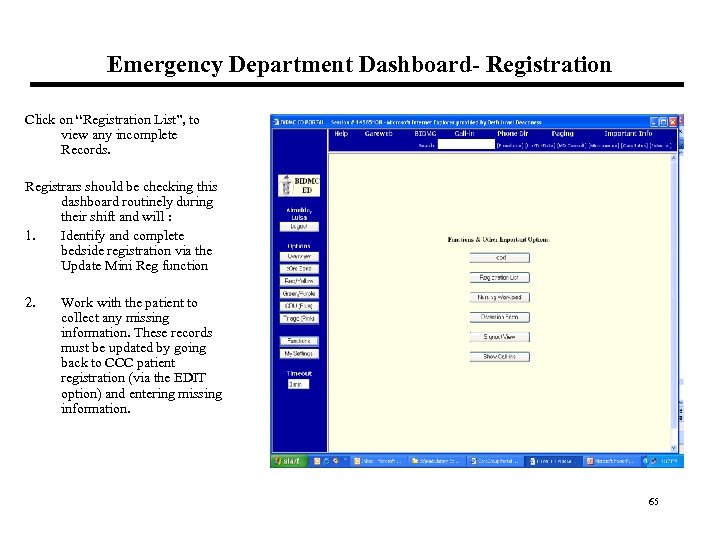
Emergency Department Dashboard- Registration Click on “Registration List”, to view any incomplete Records. Registrars should be checking this dashboard routinely during their shift and will : 1. Identify and complete bedside registration via the Update Mini Reg function 2. New screen print Work with the patient to collect any missing information. These records must be updated by going back to CCC patient registration (via the EDIT option) and entering missing information. 65
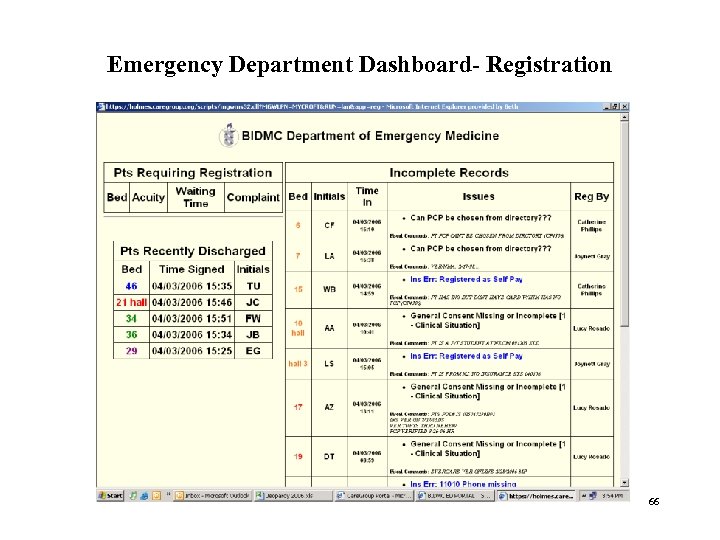
Emergency Department Dashboard- Registration 66
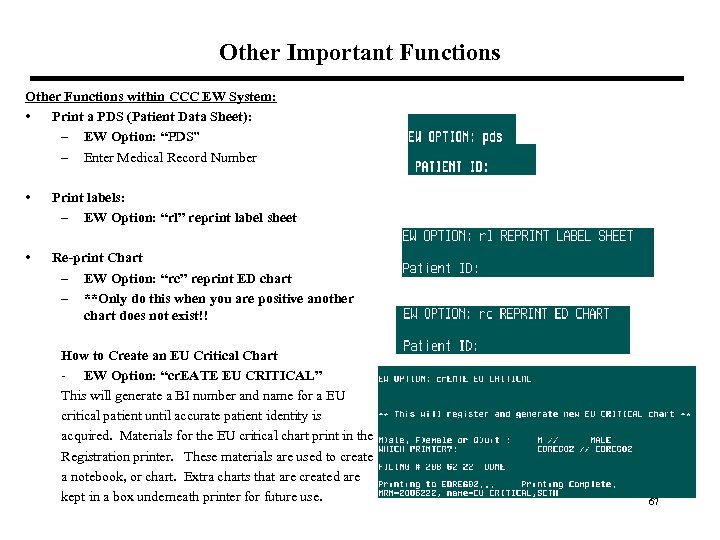
Other Important Functions Other Functions within CCC EW System: • Print a PDS (Patient Data Sheet): – EW Option: “PDS” – Enter Medical Record Number • Print labels: – EW Option: “rl” reprint label sheet • Re-print Chart – EW Option: “rc” reprint ED chart – **Only do this when you are positive another chart does not exist!! How to Create an EU Critical Chart - EW Option: “cr. EATE EU CRITICAL” This will generate a BI number and name for a EU critical patient until accurate patient identity is acquired. Materials for the EU critical chart print in the Registration printer. These materials are used to create a notebook, or chart. Extra charts that are created are kept in a box underneath printer for future use. 67
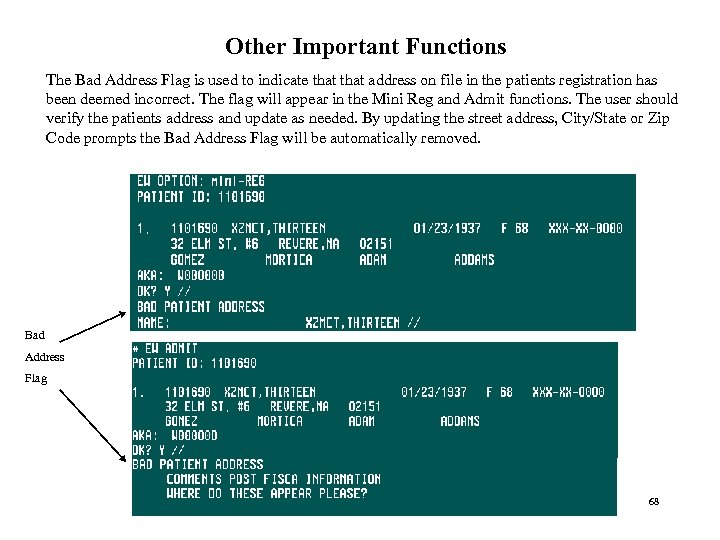
Other Important Functions The Bad Address Flag is used to indicate that address on file in the patients registration has been deemed incorrect. The flag will appear in the Mini Reg and Admit functions. The user should verify the patients address and update as needed. By updating the street address, City/State or Zip Code prompts the Bad Address Flag will be automatically removed. Bad Address Flag 68
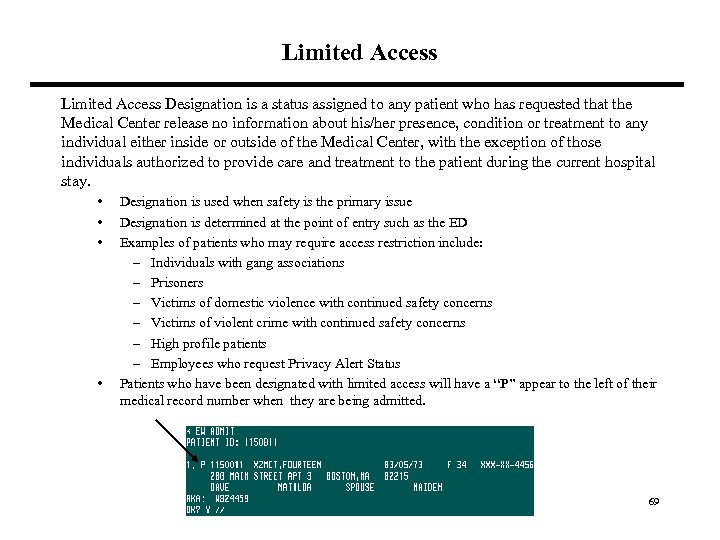
Limited Access Designation is a status assigned to any patient who has requested that the Medical Center release no information about his/her presence, condition or treatment to any individual either inside or outside of the Medical Center, with the exception of those individuals authorized to provide care and treatment to the patient during the current hospital stay. • • Designation is used when safety is the primary issue Designation is determined at the point of entry such as the ED Examples of patients who may require access restriction include: – Individuals with gang associations – Prisoners – Victims of domestic violence with continued safety concerns – Victims of violent crime with continued safety concerns – High profile patients – Employees who request Privacy Alert Status Patients who have been designated with limited access will have a “P” appear to the left of their medical record number when they are being admitted. 69
Limited Access (continued) For those patients who require or request Patient Privacy Alert Status the following measures will be implemented: • The patient will agree to limit their communication to immediate family. The patient is the only one who can disclose their room and/or phone number • Staff will not acknowledge that the patient is in the hospital (whether inquiry is made in person, telephone or in writing) • Staff will not accept gifts, calls, or visitors on behalf of the patient 70
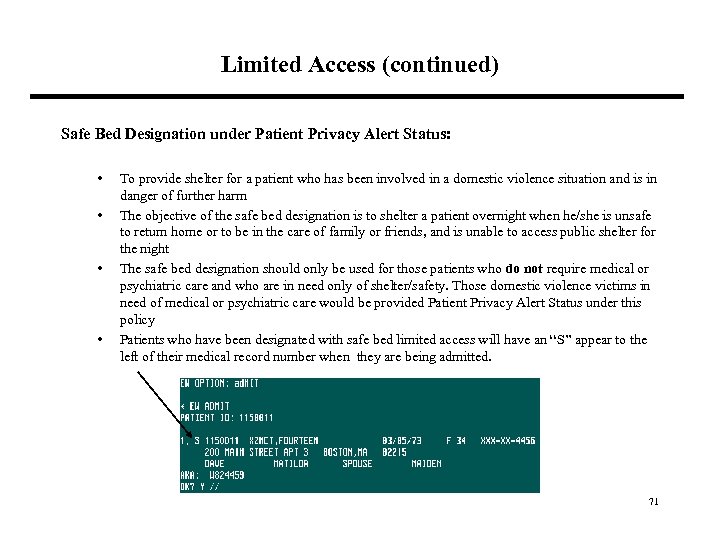
Limited Access (continued) Safe Bed Designation under Patient Privacy Alert Status: • • To provide shelter for a patient who has been involved in a domestic violence situation and is in danger of further harm The objective of the safe bed designation is to shelter a patient overnight when he/she is unsafe to return home or to be in the care of family or friends, and is unable to access public shelter for the night The safe bed designation should only be used for those patients who do not require medical or psychiatric care and who are in need only of shelter/safety. Those domestic violence victims in need of medical or psychiatric care would be provided Patient Privacy Alert Status under this policy Patients who have been designated with safe bed limited access will have an “S” appear to the left of their medical record number when they are being admitted. 71
Emergency Department (ED) Procedures for Limited Access 1. Patients requiring Limited Access Restrictions may be identified in a variety of ways: Notification to Registration, Public Safety Consultation, Clinical Provider Assessment, Patient/Family request, BIDMC policy (i. e. All prisoners should have Limited Access status)or Other 2. Once it is determined that a patient requires Limited Access Restrictions, the ED Resource Nurse must be notified by the staff member who makes that determination. 3. The Resource nurse informs the Registration Specialist or Unit Coordinator of the designation. The Registration Specialist or UCO sets the Limited Access Flag in CCC. In addition to the Limited access category, enter any special instructions given to him/her by the resource nurse regarding release of information as agreed upon by the patient, clinicians, Police and Public Safety, etc. Setting of the Limited Access Flag in CCC removes patient name from the ED Dashboard. 4. The Resource nurse notifies Public Safety as appropriate to the situation (2 -9111) 5. Public Safety will respond assist in determining the Limited Access Restriction in collaboration with the patient, family, clinicians, and/or others. 6. Before giving any information, ED staff that answer the phone or provide reception services must check the patient’s record for the Limited Access Flag and any special instructions. Limited Access flags will appear on the display of the “Enter EU Log”. 7. The limited access flag and special instructions appear on the Admission/Bed Request form and thus serves to alert Admitting Department staff of Limited Access Restrictions for patients being admitted. 8. For admitted patients requiring Public Safety measures, Public Safety must notify and discuss the plan with the patient care unit to which the patient is being admitted. Bed assignment can be obtained from the ED UCO or the Admitting Department. 72
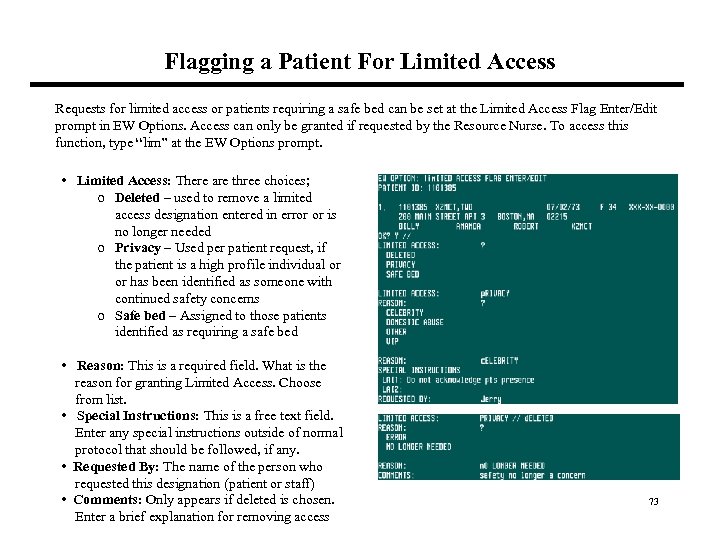
Flagging a Patient For Limited Access Requests for limited access or patients requiring a safe bed can be set at the Limited Access Flag Enter/Edit prompt in EW Options. Access can only be granted if requested by the Resource Nurse. To access this function, type “lim” at the EW Options prompt. • Limited Access: There are three choices; o Deleted – used to remove a limited access designation entered in error or is no longer needed o Privacy – Used per patient request, if the patient is a high profile individual or has been identified as someone with continued safety concerns o Safe bed – Assigned to those patients identified as requiring a safe bed • Reason: This is a required field. What is the reason for granting Limited Access. Choose from list. • Special Instructions: This is a free text field. Enter any special instructions outside of normal protocol that should be followed, if any. • Requested By: The name of the person who requested this designation (patient or staff) • Comments: Only appears if deleted is chosen. Enter a brief explanation for removing access 73
What if? 1. What if a patient comes in for a psych related issue? Which insurance should I list? Answer: Patients regular insurance should be listed. ED staff should NOT select or add a Psych insurance for any ED visit. The Psych plan will be added, if appropriate, by Inpatient Accounts staff if patient becomes admitted. 2. What if a patient has free care at another BIDMC site and they present at BIDMC Boston for treatment? Answer: NEHEN can be used to verify that the patient is Free Care eligible. • If you have been trained and have access to assign Free Care, enter the information onto the patients Registration. • If you have not been trained (and do not have access) select self pay, enter a note in comments and send an e-mail to the Registration Support team ( email “Registration Support“). Registration Support will assign Free Care. 3. What if the triage sheet does not have the chief complaint filled out. ? What should staff enter at the “Chief complaint prompt” during registration? Answer: The field should never be left blank or populated with inaccurate information. It is the responsibility of staff to get this information from the nurse at bedside if needed. 74
What if? 4. What if a patient comes in to the ED as a result of a auto/liability accident? Which insurance should be chosen? Answer: If the auto/liability information is not available, self-pay is the best choice. This ensures that the bill is sent to the patient at home and their immediate involvement is needed. 5. What if a patient comes in as a Student? Which steps should be taken? 6. Answer: ED Registration staff should try to obtain both local and permanent address for student. If the student does not have insurance, they will need to be registered as self-pay. They should then be referred to free care. If student has Chickering as their insurance they should be asked if they first sought care at their student health center, since in many cases Chickering my not pay for visit if they do not have a referral from the center. 75
Resources Ambulatory Educations and Systems Team: Amy Goldman 617 -667 -1590 Jerry Amirault 617 -667 -1593 Patricia Cox 617 -667 -1585 Irene Jordan 617 -667 -1592 Geoff O’Hara 617 -667 -1594 Julie Rockwell 617 -667 -1599 Charmaine Massey 617 -667 -1557 Policy Questions: Your Supervisor 76
c739511a45a9c3a1c60748d3adbc2521.ppt