622ad9a888e2462ca3bc89e32a7a8fcc.ppt
- Количество слайдов: 18
Emergency Department Bypass for ST-Segment Elevation Myocardial Infarction Akshay Bagai MD, MHS St. Michael’s Hospital, Toronto, Canada Washington Hospital Center Cath Conference August 28, 2013
Background • In STEMI, faster reperfusion is associated with lower morbidity and mortality • National guidelines recommend device activation within 90 minutes of first medical contact • Timely reperfusion still remains suboptimal in the U. S. All Rights Reserved, Duke Medicine 2007
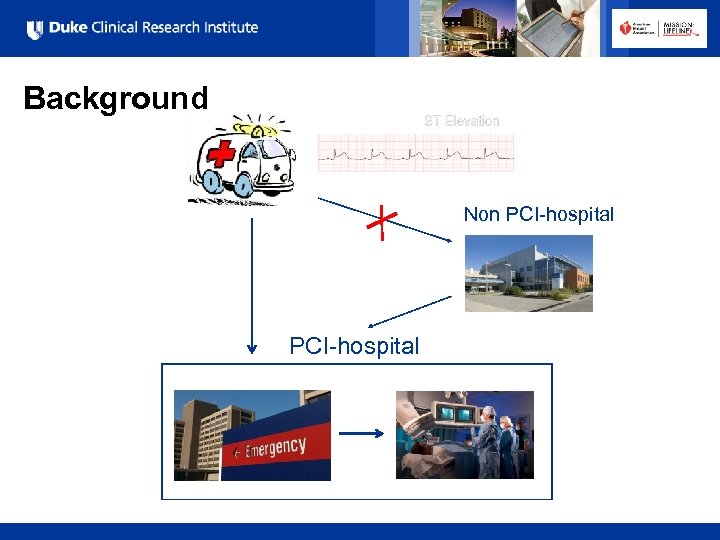
Background Non PCI-hospital All Rights Reserved, Duke Medicine 2007
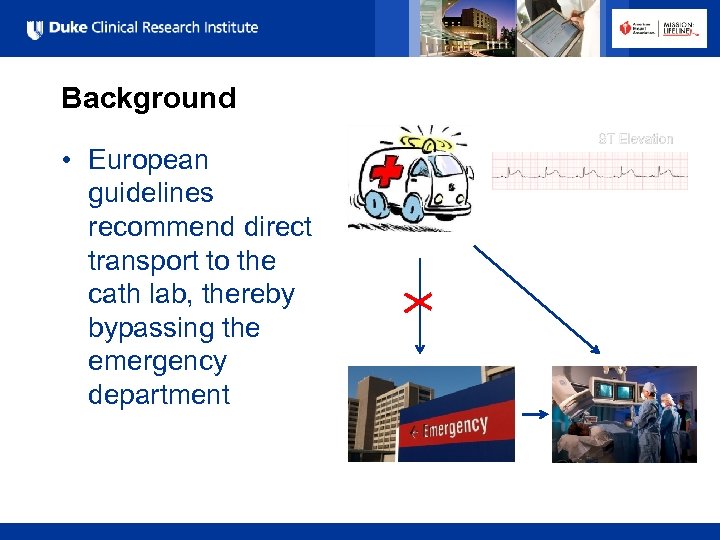
Background • European guidelines recommend direct transport to the cath lab, thereby bypassing the emergency department All Rights Reserved, Duke Medicine 2007
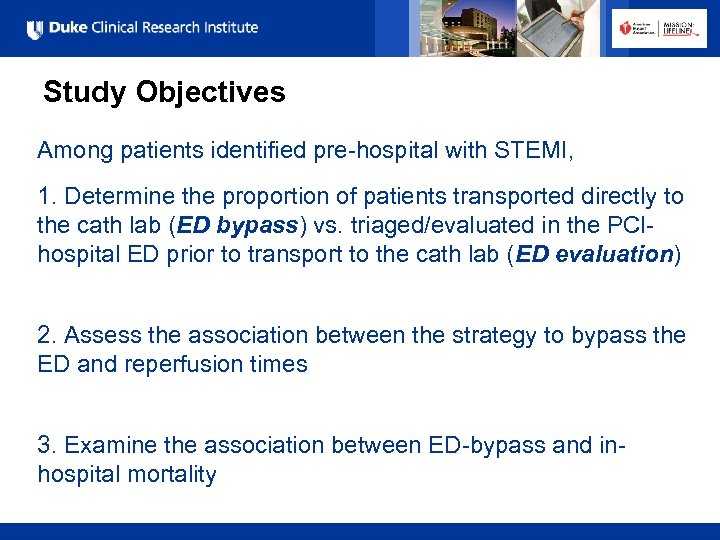
Study Objectives Among patients identified pre-hospital with STEMI, 1. Determine the proportion of patients transported directly to the cath lab (ED bypass) vs. triaged/evaluated in the PCIhospital ED prior to transport to the cath lab (ED evaluation) 2. Assess the association between the strategy to bypass the ED and reperfusion times 3. Examine the association between ED-bypass and inhospital mortality All Rights Reserved, Duke Medicine 2007
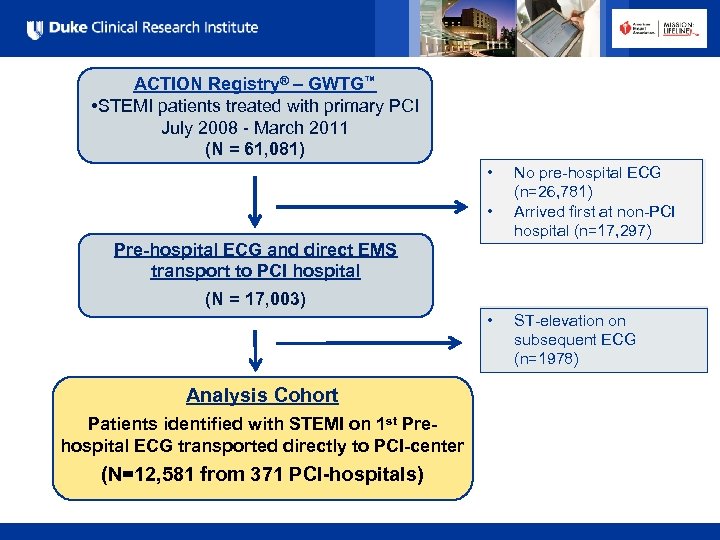
ACTION Registry® – GWTG™ • STEMI patients treated with primary PCI July 2008 - March 2011 (N = 61, 081) • • No pre-hospital ECG (n=26, 781) Arrived first at non-PCI hospital (n=17, 297) Pre-hospital ECG and direct EMS transport to PCI hospital (N = 17, 003) • Analysis Cohort Patients identified with STEMI on 1 st Prehospital ECG transported directly to PCI-center (N=12, 581 from 371 PCI-hospitals) All Rights Reserved, Duke Medicine 2007 ST-elevation on subsequent ECG (n=1978)
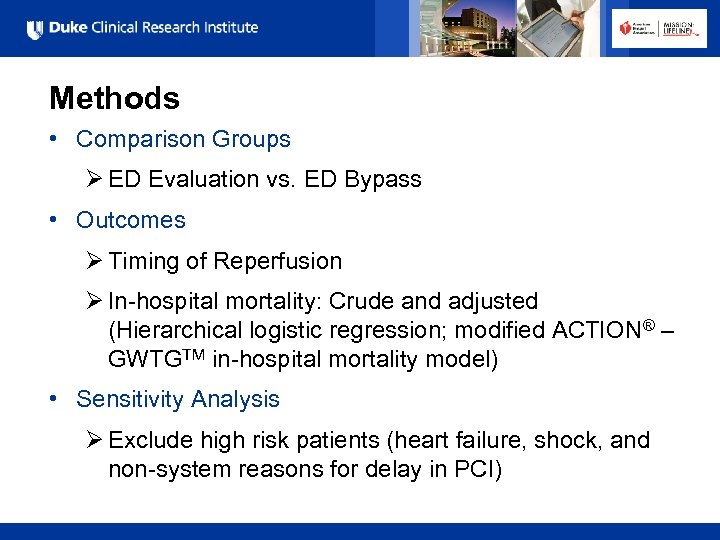
Methods • Comparison Groups Ø ED Evaluation vs. ED Bypass • Outcomes Ø Timing of Reperfusion Ø In-hospital mortality: Crude and adjusted (Hierarchical logistic regression; modified ACTION® – GWTGTM in-hospital mortality model) • Sensitivity Analysis Ø Exclude high risk patients (heart failure, shock, and non-system reasons for delay in PCI) All Rights Reserved, Duke Medicine 2007
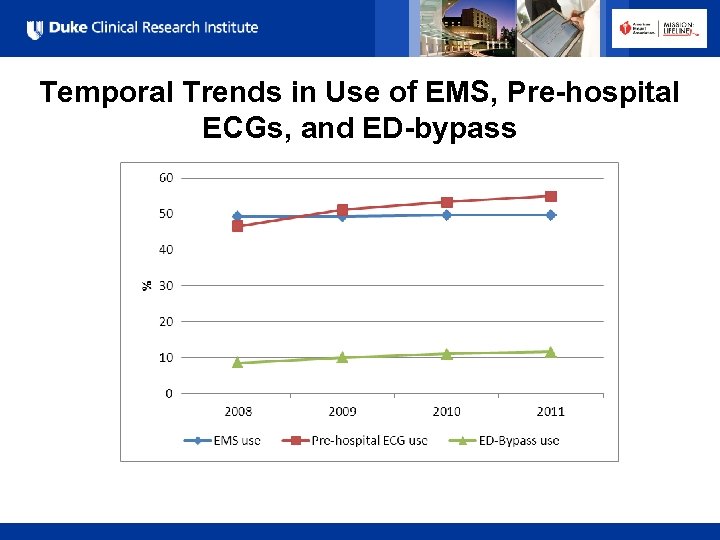
Temporal Trends in Use of EMS, Pre-hospital ECGs, and ED-bypass All Rights Reserved, Duke Medicine 2007
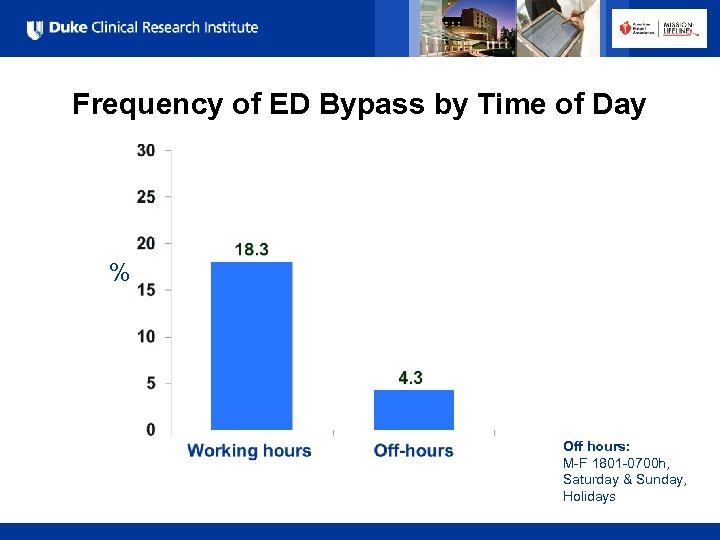
Frequency of ED Bypass by Time of Day % Off hours: M-F 1801 -0700 h, Saturday & Sunday, Holidays All Rights Reserved, Duke Medicine 2007
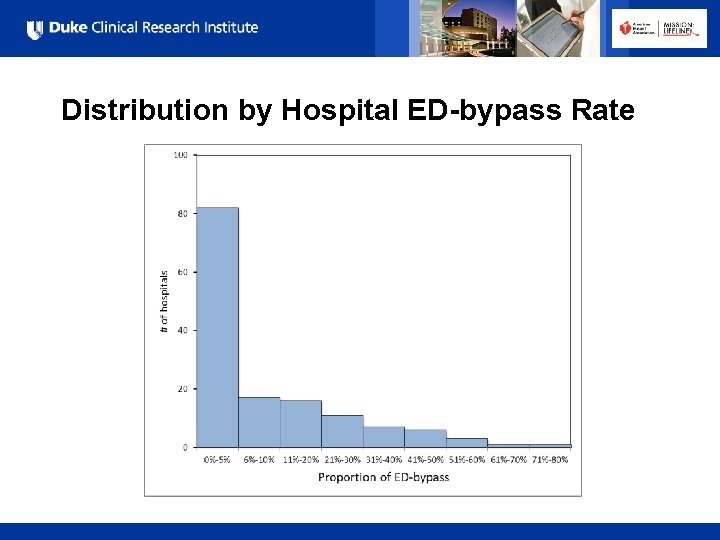
Distribution by Hospital ED-bypass Rate All Rights Reserved, Duke Medicine 2007
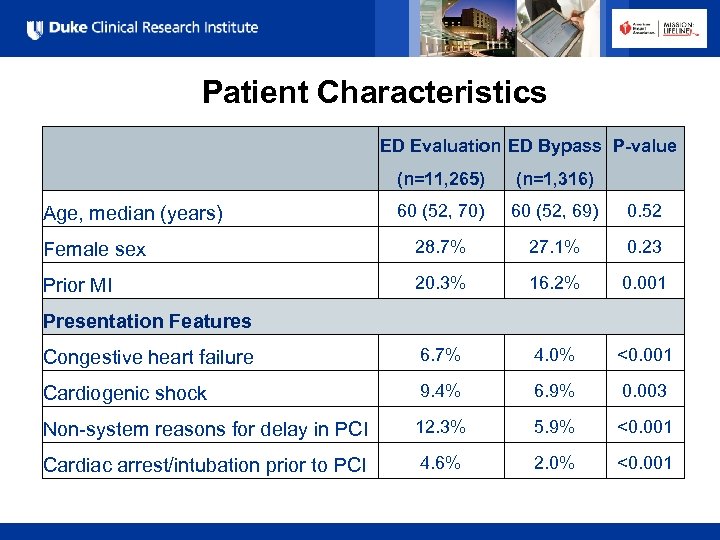
Patient Characteristics ED Evaluation ED Bypass P-value (n=11, 265) (n=1, 316) 60 (52, 70) 60 (52, 69) 0. 52 Female sex 28. 7% 27. 1% 0. 23 Prior MI 20. 3% 16. 2% 0. 001 Congestive heart failure 6. 7% 4. 0% <0. 001 Cardiogenic shock 9. 4% 6. 9% 0. 003 Non-system reasons for delay in PCI 12. 3% 5. 9% <0. 001 Cardiac arrest/intubation prior to PCI 4. 6% 2. 0% <0. 001 Age, median (years) Presentation Features All Rights Reserved, Duke Medicine 2007
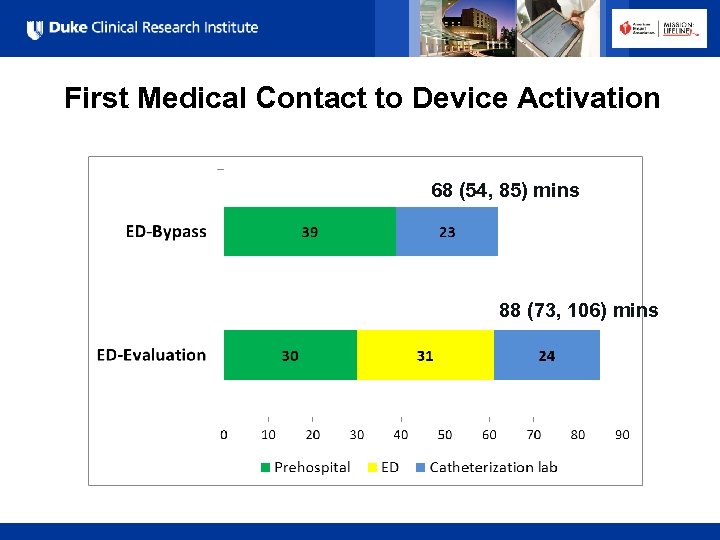
First Medical Contact to Device Activation 68 (54, 85) mins 88 (73, 106) mins All Rights Reserved, Duke Medicine 2007
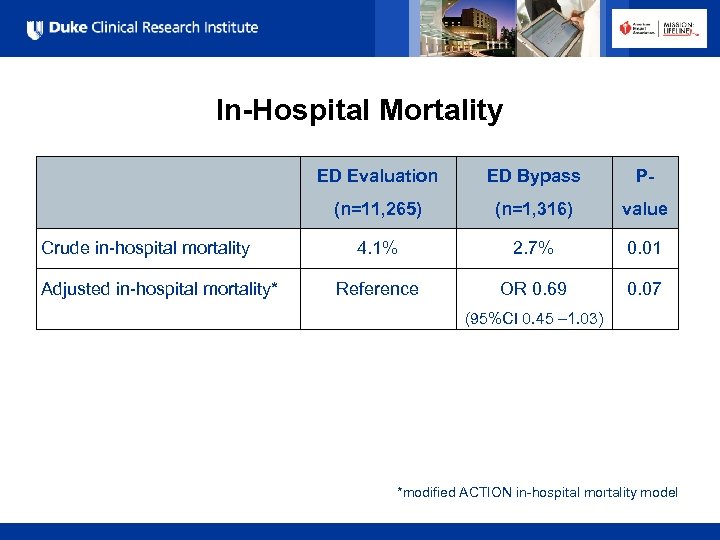
In-Hospital Mortality Adjusted in-hospital mortality* ED Bypass P- (n=11, 265) Crude in-hospital mortality ED Evaluation (n=1, 316) value 4. 1% 2. 7% 0. 01 Reference OR 0. 69 0. 07 (95%CI 0. 45 – 1. 03) *modified ACTION in-hospital mortality model All Rights Reserved, Duke Medicine 2007
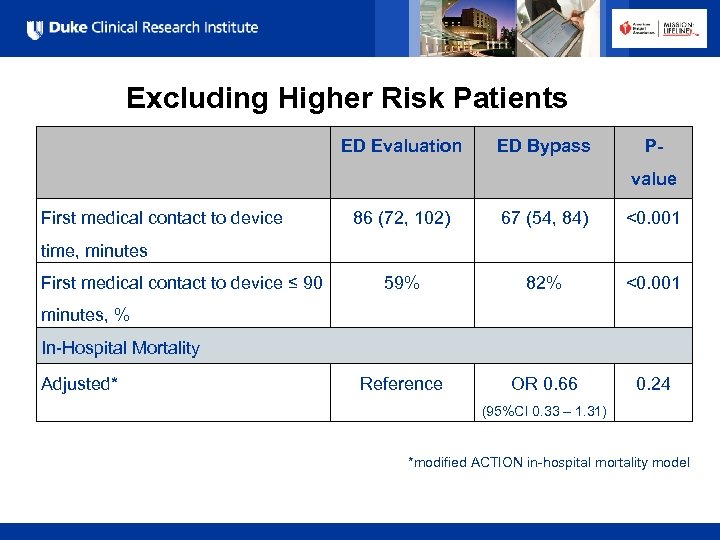
Excluding Higher Risk Patients ED Evaluation ED Bypass P- value First medical contact to device 86 (72, 102) 67 (54, 84) <0. 001 59% 82% <0. 001 Reference OR 0. 66 0. 24 time, minutes First medical contact to device ≤ 90 minutes, % In-Hospital Mortality Adjusted* (95%CI 0. 33 – 1. 31) *modified ACTION in-hospital mortality model All Rights Reserved, Duke Medicine 2007
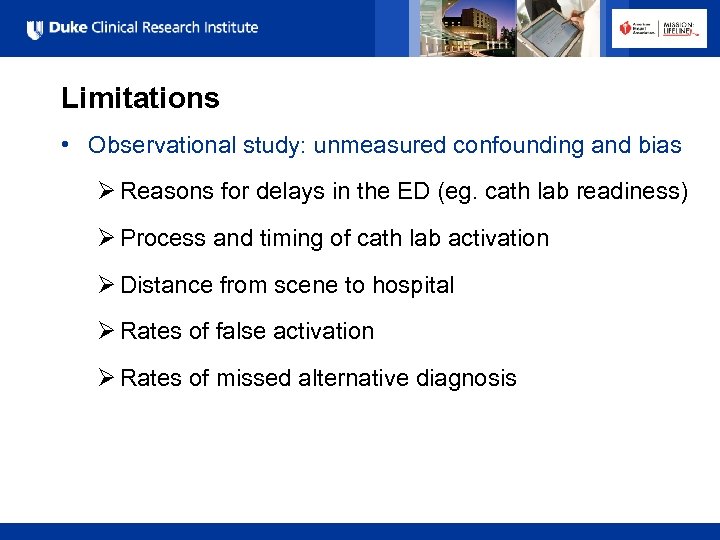
Limitations • Observational study: unmeasured confounding and bias Ø Reasons for delays in the ED (eg. cath lab readiness) Ø Process and timing of cath lab activation Ø Distance from scene to hospital Ø Rates of false activation Ø Rates of missed alternative diagnosis All Rights Reserved, Duke Medicine 2007
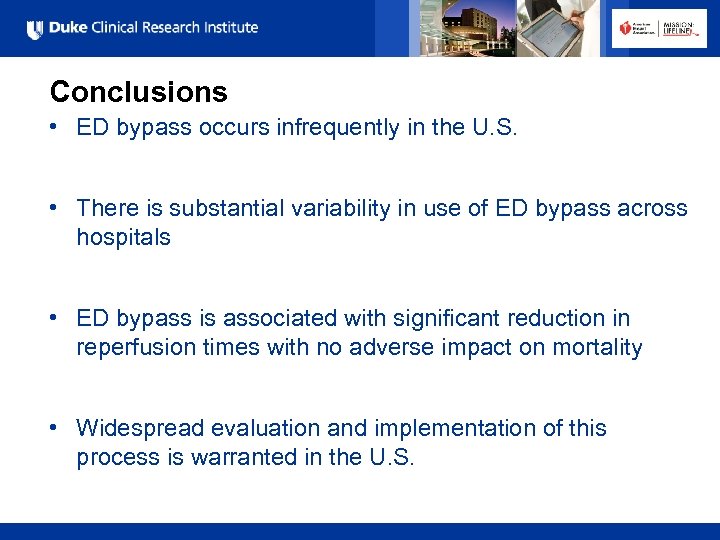
Conclusions • ED bypass occurs infrequently in the U. S. • There is substantial variability in use of ED bypass across hospitals • ED bypass is associated with significant reduction in reperfusion times with no adverse impact on mortality • Widespread evaluation and implementation of this process is warranted in the U. S. All Rights Reserved, Duke Medicine 2007
Implementation of ED Bypass Protocols 1. Triage protocols for unstable patients Ø Cardiac arrest, cardiogenic shock, respiratory failure 2. Confirm diagnosis/minimize false activation Ø Paramedic training, computer ECG interpretation, wireless ECG transmission for consultation 3. Off-hours holding area until cath lab ready Ø In-house team of CCU nurse, CCU fellow, Cardiologist Ø Expectation: start case within 30 mins of being paged All Rights Reserved, Duke Medicine 2007
Collaborators Dr. Matthew Roe Dr. Christopher Granger Dr. Jamie Jollis Dr. Harold Dauerman Dr. Ivan Rokos Dr. Eric Bates Dr. William French Andrew Peng All Rights Reserved, Duke Medicine 2007 PCI-hospital
622ad9a888e2462ca3bc89e32a7a8fcc.ppt