8768bea483e956ed98dce0828a3cc142.ppt
- Количество слайдов: 47
 Emergency Airway Management Pat Melanson, MD
Emergency Airway Management Pat Melanson, MD
 Safe airway management airway evaluation n identification of the difficult airway n assessment of other clinical factors n selection of the likely most successful plan of action n reasonable alternative plan n
Safe airway management airway evaluation n identification of the difficult airway n assessment of other clinical factors n selection of the likely most successful plan of action n reasonable alternative plan n
 Algorithmic Approach to Airway Management Have a precompiled plan of airway management ready for implementation as clinical airway difficulties are encountered n develop a plan and a back-up plan n Practice guidelines for management of the difficult airway n – ASA taskforce – Anesthesiology 78 : 597 - 602, 1993
Algorithmic Approach to Airway Management Have a precompiled plan of airway management ready for implementation as clinical airway difficulties are encountered n develop a plan and a back-up plan n Practice guidelines for management of the difficult airway n – ASA taskforce – Anesthesiology 78 : 597 - 602, 1993
 Emergency Airway n full stomach n altered level of consciousness n deteriorating cardiorespiratory physiology n abnormal or distorted upper airway anatomy n no time for pre-assessment or plan
Emergency Airway n full stomach n altered level of consciousness n deteriorating cardiorespiratory physiology n abnormal or distorted upper airway anatomy n no time for pre-assessment or plan
 Airway Assessment n compromise or threats n potentially difficult airway
Airway Assessment n compromise or threats n potentially difficult airway
 The Three Pillars of Airway Management n Patency ( airflow integrity ) n Protection against aspiration n Assurance of oxygenation and ventilation
The Three Pillars of Airway Management n Patency ( airflow integrity ) n Protection against aspiration n Assurance of oxygenation and ventilation
 Indications for Active Airway Intervention Patency - relief of obstruction n Protection from aspiration n Hypoxic/ hypercapnic respiratory failure n Airway access for pulmonary toilet, drug delivery, therapeutic hyperventilation n Shock n
Indications for Active Airway Intervention Patency - relief of obstruction n Protection from aspiration n Hypoxic/ hypercapnic respiratory failure n Airway access for pulmonary toilet, drug delivery, therapeutic hyperventilation n Shock n
 Clinical Signs of Airway Compromise : Patency Inspiratory stridor n Snoring ( pharyngeal obstruction ) n Gurgling ( foreign matter/ secretions ) n Drooling ( epiglottitis ) n Hoarseness ( laryngeal edema/ vc paralysis) n Paradoxical chest wall movement n Tracheal tug n
Clinical Signs of Airway Compromise : Patency Inspiratory stridor n Snoring ( pharyngeal obstruction ) n Gurgling ( foreign matter/ secretions ) n Drooling ( epiglottitis ) n Hoarseness ( laryngeal edema/ vc paralysis) n Paradoxical chest wall movement n Tracheal tug n
 Clinical Signs of Airway Compromise : Protection Blood in upper airway n Pus in upper airway n persistant vomiting n n Loss of protective airway reflexes
Clinical Signs of Airway Compromise : Protection Blood in upper airway n Pus in upper airway n persistant vomiting n n Loss of protective airway reflexes
 Clinical Signs of Airway Compromise: Oxygenation and Ventilation Central cyanosis n Obtundation and diaphoresis n rapid shallow respirations n Accessory muscle use n Retractions n Abdominal paradox n
Clinical Signs of Airway Compromise: Oxygenation and Ventilation Central cyanosis n Obtundation and diaphoresis n rapid shallow respirations n Accessory muscle use n Retractions n Abdominal paradox n
 The Difficult Airway n Difficult laryngoscopy n Difficult bag-mask ventilation n Lower airway difficulty
The Difficult Airway n Difficult laryngoscopy n Difficult bag-mask ventilation n Lower airway difficulty
 Techniques for the Compromised Airway Bag-Valve-Mask Ventilation n Endotracheal Intubation n Rapid Sequence Intubation n Alternate techniques for the difficult airway n
Techniques for the Compromised Airway Bag-Valve-Mask Ventilation n Endotracheal Intubation n Rapid Sequence Intubation n Alternate techniques for the difficult airway n
 Golden Rules of Bagging “ Anybody ( almost ) can be oxygenated and ventilated with a bag and a mask “ n The art of bagging should be mastered before the art of intubation n Manual ventilation skill with proper equipment is a fundamental premise of advanced airway management n
Golden Rules of Bagging “ Anybody ( almost ) can be oxygenated and ventilated with a bag and a mask “ n The art of bagging should be mastered before the art of intubation n Manual ventilation skill with proper equipment is a fundamental premise of advanced airway management n
 Frequent Errors with BVM failure to recognize its importance n forget to bag ( focussed on ETT ) n give up on bagging too early n bag but don’t assess efficacy n failure to assign one person to airway management only n
Frequent Errors with BVM failure to recognize its importance n forget to bag ( focussed on ETT ) n give up on bagging too early n bag but don’t assess efficacy n failure to assign one person to airway management only n
 Difficult Airway : BVM Upper airway obstruction n Lack of dentures n Beard n Midfacial smash n facial burns, dressings, scarring n poor lung mechanics n
Difficult Airway : BVM Upper airway obstruction n Lack of dentures n Beard n Midfacial smash n facial burns, dressings, scarring n poor lung mechanics n
 Difficult Airway : BVM degree of difficulty from zero to infinite n zero = no external effort/internal device n one person jaw thrust/ face seal n oropharyngeal or nasopharyngeal AW n two person jaw thrust / face seal – both internal airway devices n infinite -no patency despite maximal external effort and full use of OP/NP n
Difficult Airway : BVM degree of difficulty from zero to infinite n zero = no external effort/internal device n one person jaw thrust/ face seal n oropharyngeal or nasopharyngeal AW n two person jaw thrust / face seal – both internal airway devices n infinite -no patency despite maximal external effort and full use of OP/NP n
 Difficult Airway : BVM Remove FB - Magill forceps n Triple maneuver if c-spine clear – Head tilt, jaw lift, mouth opening n Nasopharyngeal or oropharyngeal airway n two-person, four-hand technique n
Difficult Airway : BVM Remove FB - Magill forceps n Triple maneuver if c-spine clear – Head tilt, jaw lift, mouth opening n Nasopharyngeal or oropharyngeal airway n two-person, four-hand technique n
 Prediction of the difficult airway (Intubation) 1200 prospectively studied patients n of 84 patients predicted to have problem, only 22 (25%) actually had a problem n of 43 actual difficult intubations incurred, only 22 (51%) were predicted n – Latto IP. and Rosen M
Prediction of the difficult airway (Intubation) 1200 prospectively studied patients n of 84 patients predicted to have problem, only 22 (25%) actually had a problem n of 43 actual difficult intubations incurred, only 22 (51%) were predicted n – Latto IP. and Rosen M
 Prediction of the difficult airway history of past airway problems n Careful physical assessment n knowledge and experience to overcome the "unpredicted difficult airway". n learning practical airway management skills in an environment that is not urgent, stressful or life threatening n
Prediction of the difficult airway history of past airway problems n Careful physical assessment n knowledge and experience to overcome the "unpredicted difficult airway". n learning practical airway management skills in an environment that is not urgent, stressful or life threatening n


 Difficult Airway : Laryngoscopy Short thick neck n Receding mandible n Buck teeth n Poor mandibular mobility/ limited jaw opening n Limited head and neck movement n – ( including trauma )
Difficult Airway : Laryngoscopy Short thick neck n Receding mandible n Buck teeth n Poor mandibular mobility/ limited jaw opening n Limited head and neck movement n – ( including trauma )
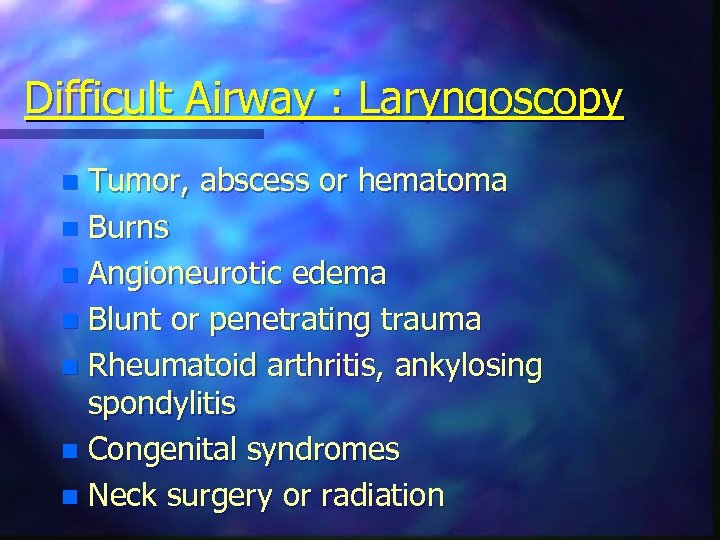 Difficult Airway : Laryngoscopy Tumor, abscess or hematoma n Burns n Angioneurotic edema n Blunt or penetrating trauma n Rheumatoid arthritis, ankylosing spondylitis n Congenital syndromes n Neck surgery or radiation n
Difficult Airway : Laryngoscopy Tumor, abscess or hematoma n Burns n Angioneurotic edema n Blunt or penetrating trauma n Rheumatoid arthritis, ankylosing spondylitis n Congenital syndromes n Neck surgery or radiation n
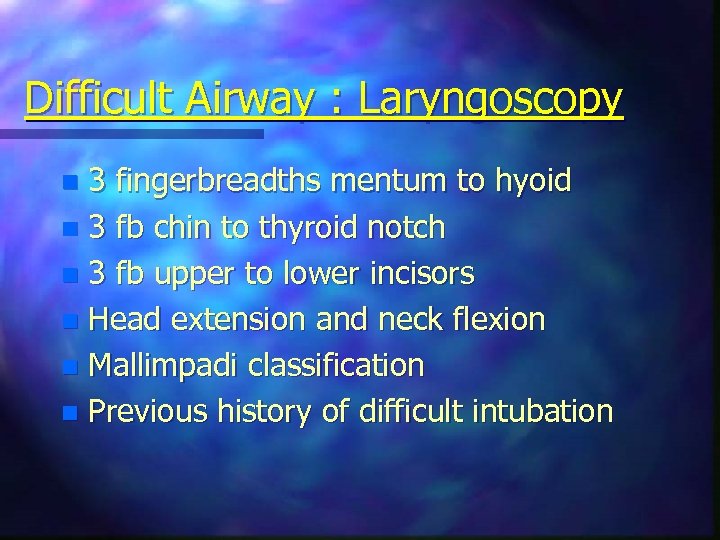 Difficult Airway : Laryngoscopy 3 fingerbreadths mentum to hyoid n 3 fb chin to thyroid notch n 3 fb upper to lower incisors n Head extension and neck flexion n Mallimpadi classification n Previous history of difficult intubation n
Difficult Airway : Laryngoscopy 3 fingerbreadths mentum to hyoid n 3 fb chin to thyroid notch n 3 fb upper to lower incisors n Head extension and neck flexion n Mallimpadi classification n Previous history of difficult intubation n
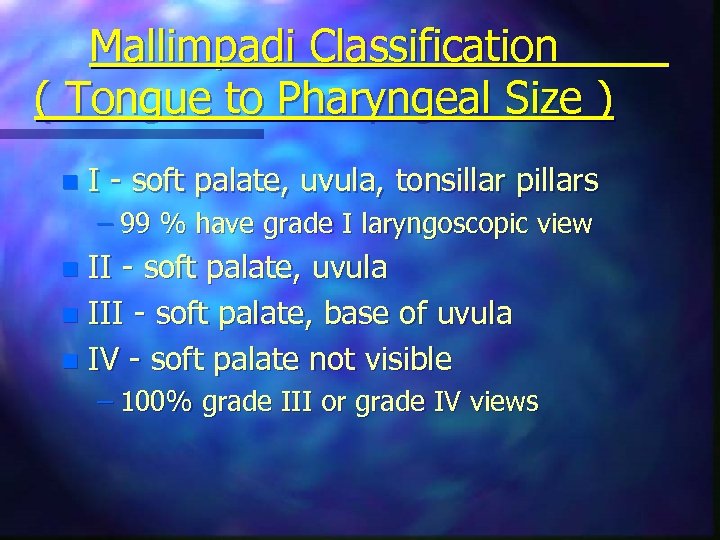 Mallimpadi Classification ( Tongue to Pharyngeal Size ) n I - soft palate, uvula, tonsillar pillars – 99 % have grade I laryngoscopic view II - soft palate, uvula n III - soft palate, base of uvula n IV - soft palate not visible n – 100% grade III or grade IV views
Mallimpadi Classification ( Tongue to Pharyngeal Size ) n I - soft palate, uvula, tonsillar pillars – 99 % have grade I laryngoscopic view II - soft palate, uvula n III - soft palate, base of uvula n IV - soft palate not visible n – 100% grade III or grade IV views
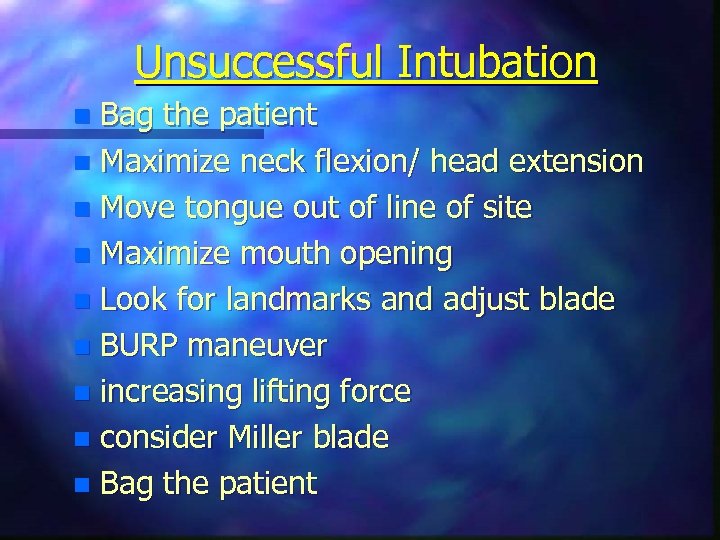 Unsuccessful Intubation Bag the patient n Maximize neck flexion/ head extension n Move tongue out of line of site n Maximize mouth opening n Look for landmarks and adjust blade n BURP maneuver n increasing lifting force n consider Miller blade n Bag the patient n
Unsuccessful Intubation Bag the patient n Maximize neck flexion/ head extension n Move tongue out of line of site n Maximize mouth opening n Look for landmarks and adjust blade n BURP maneuver n increasing lifting force n consider Miller blade n Bag the patient n
 Dilemmas: Awake or Asleep n Oral or Nasal n Laryngoscopy or Blind Intubation n To Paralyze or Not n
Dilemmas: Awake or Asleep n Oral or Nasal n Laryngoscopy or Blind Intubation n To Paralyze or Not n
 Case #1 43 year old female, day 12 post SAH n 5 unclipped cerebral aneurysms n vasospasm with left hemiparesis n hydrocephalus with clotted IV drain n rising ICP and BP n decreasing LOC n ate breakfast n
Case #1 43 year old female, day 12 post SAH n 5 unclipped cerebral aneurysms n vasospasm with left hemiparesis n hydrocephalus with clotted IV drain n rising ICP and BP n decreasing LOC n ate breakfast n
 Techniques DL without pharmacologic aids n Awake Direct Laryngoscopy n Awake Blind Nasal n Rapid Sequence Intubation (RSI) n Fiberoptic n Surgical Cricothyroidotomy n
Techniques DL without pharmacologic aids n Awake Direct Laryngoscopy n Awake Blind Nasal n Rapid Sequence Intubation (RSI) n Fiberoptic n Surgical Cricothyroidotomy n
 Anesthesia Airway Maxims the awake airway is the safest to manage n spontaneous breathing is generally safer than paralysis with PPV by mask n have a low threshold to wake the patient up and cancel the case n call for help early n
Anesthesia Airway Maxims the awake airway is the safest to manage n spontaneous breathing is generally safer than paralysis with PPV by mask n have a low threshold to wake the patient up and cancel the case n call for help early n
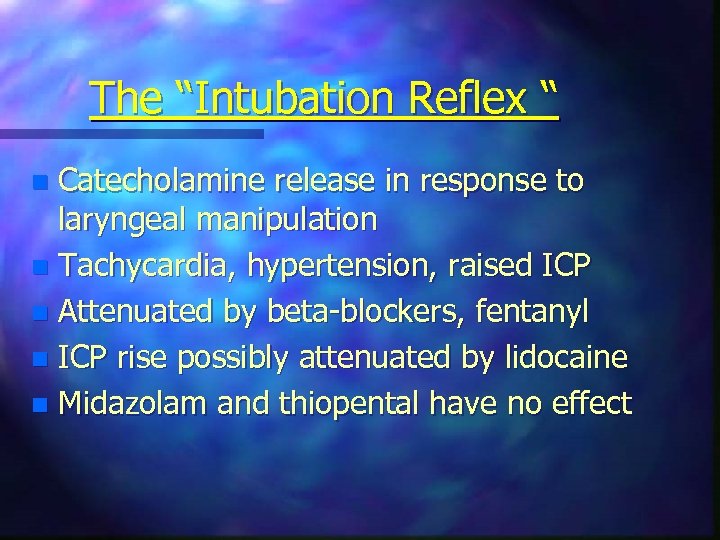 The “Intubation Reflex “ Catecholamine release in response to laryngeal manipulation n Tachycardia, hypertension, raised ICP n Attenuated by beta-blockers, fentanyl n ICP rise possibly attenuated by lidocaine n Midazolam and thiopental have no effect n
The “Intubation Reflex “ Catecholamine release in response to laryngeal manipulation n Tachycardia, hypertension, raised ICP n Attenuated by beta-blockers, fentanyl n ICP rise possibly attenuated by lidocaine n Midazolam and thiopental have no effect n
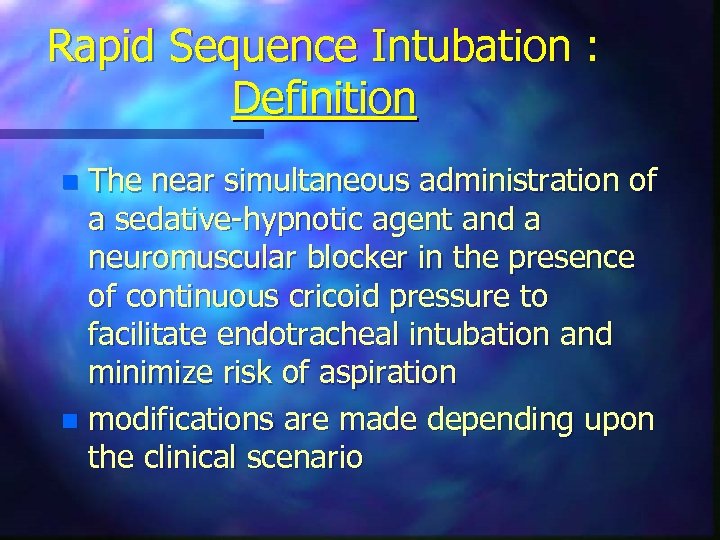 Rapid Sequence Intubation : Definition The near simultaneous administration of a sedative-hypnotic agent and a neuromuscular blocker in the presence of continuous cricoid pressure to facilitate endotracheal intubation and minimize risk of aspiration n modifications are made depending upon the clinical scenario n
Rapid Sequence Intubation : Definition The near simultaneous administration of a sedative-hypnotic agent and a neuromuscular blocker in the presence of continuous cricoid pressure to facilitate endotracheal intubation and minimize risk of aspiration n modifications are made depending upon the clinical scenario n
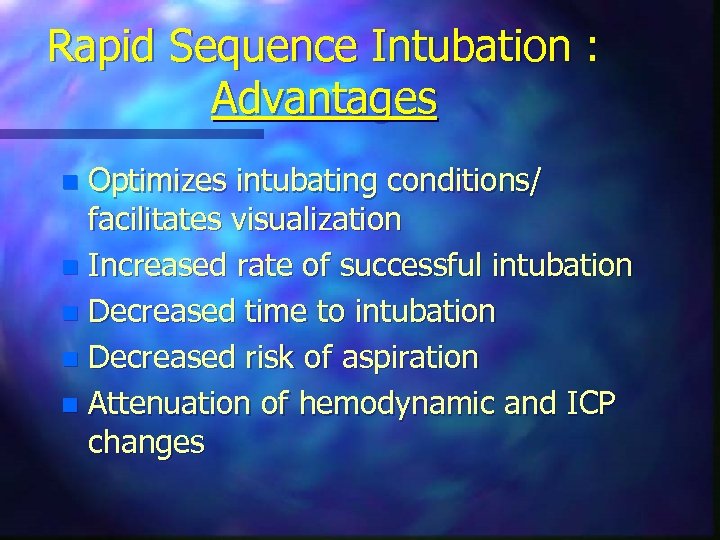 Rapid Sequence Intubation : Advantages Optimizes intubating conditions/ facilitates visualization n Increased rate of successful intubation n Decreased time to intubation n Decreased risk of aspiration n Attenuation of hemodynamic and ICP changes n
Rapid Sequence Intubation : Advantages Optimizes intubating conditions/ facilitates visualization n Increased rate of successful intubation n Decreased time to intubation n Decreased risk of aspiration n Attenuation of hemodynamic and ICP changes n
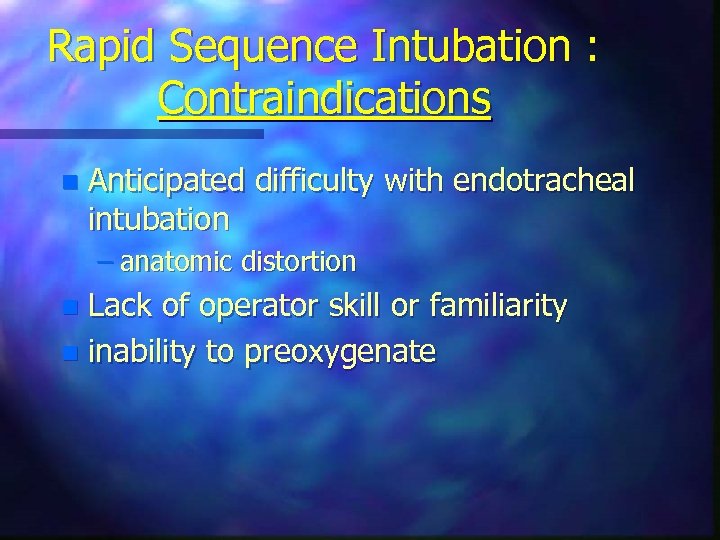 Rapid Sequence Intubation : Contraindications n Anticipated difficulty with endotracheal intubation – anatomic distortion Lack of operator skill or familiarity n inability to preoxygenate n
Rapid Sequence Intubation : Contraindications n Anticipated difficulty with endotracheal intubation – anatomic distortion Lack of operator skill or familiarity n inability to preoxygenate n
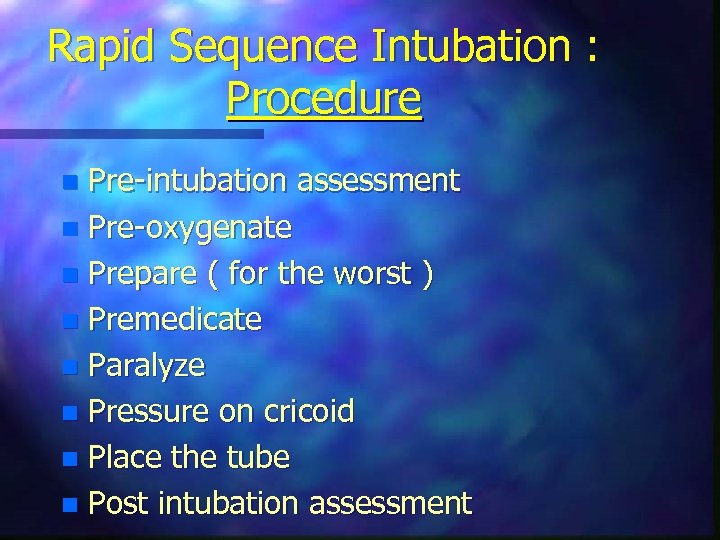 Rapid Sequence Intubation : Procedure Pre-intubation assessment n Pre-oxygenate n Prepare ( for the worst ) n Premedicate n Paralyze n Pressure on cricoid n Place the tube n Post intubation assessment n
Rapid Sequence Intubation : Procedure Pre-intubation assessment n Pre-oxygenate n Prepare ( for the worst ) n Premedicate n Paralyze n Pressure on cricoid n Place the tube n Post intubation assessment n
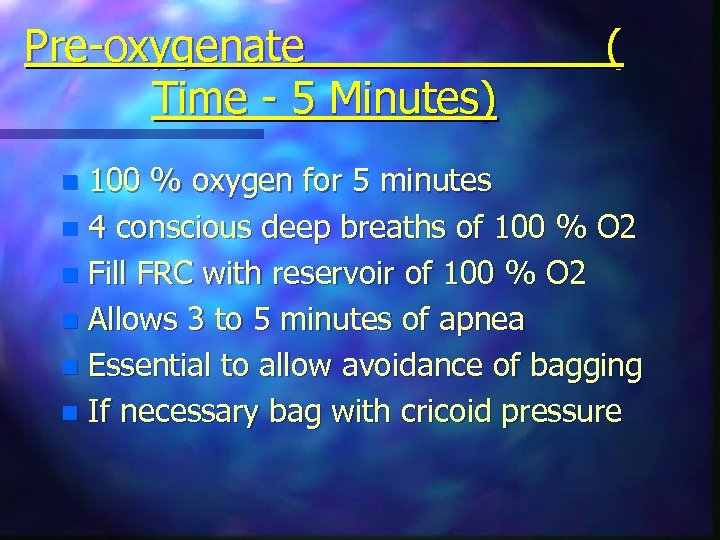 Pre-oxygenate Time - 5 Minutes) ( 100 % oxygen for 5 minutes n 4 conscious deep breaths of 100 % O 2 n Fill FRC with reservoir of 100 % O 2 n Allows 3 to 5 minutes of apnea n Essential to allow avoidance of bagging n If necessary bag with cricoid pressure n
Pre-oxygenate Time - 5 Minutes) ( 100 % oxygen for 5 minutes n 4 conscious deep breaths of 100 % O 2 n Fill FRC with reservoir of 100 % O 2 n Allows 3 to 5 minutes of apnea n Essential to allow avoidance of bagging n If necessary bag with cricoid pressure n
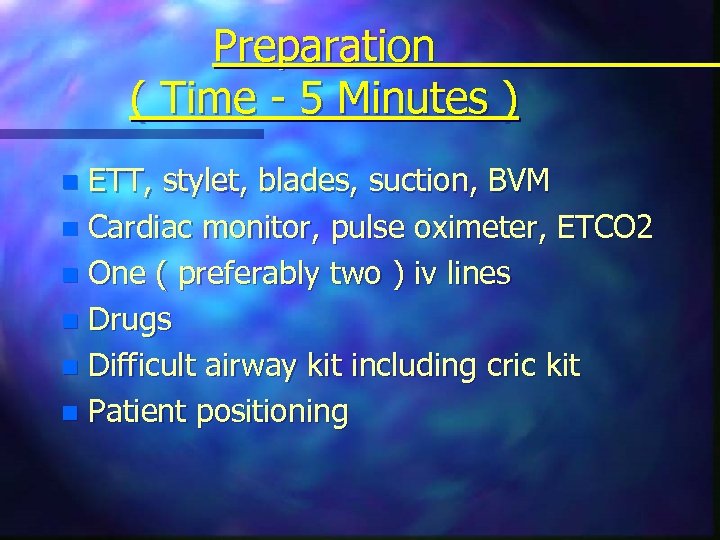 Preparation ( Time - 5 Minutes ) ETT, stylet, blades, suction, BVM n Cardiac monitor, pulse oximeter, ETCO 2 n One ( preferably two ) iv lines n Drugs n Difficult airway kit including cric kit n Patient positioning n
Preparation ( Time - 5 Minutes ) ETT, stylet, blades, suction, BVM n Cardiac monitor, pulse oximeter, ETCO 2 n One ( preferably two ) iv lines n Drugs n Difficult airway kit including cric kit n Patient positioning n
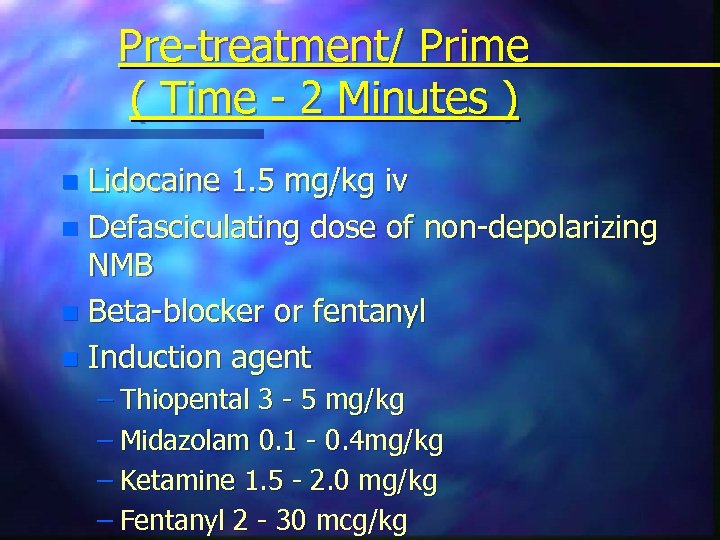 Pre-treatment/ Prime ( Time - 2 Minutes ) Lidocaine 1. 5 mg/kg iv n Defasciculating dose of non-depolarizing NMB n Beta-blocker or fentanyl n Induction agent n – Thiopental 3 - 5 mg/kg – Midazolam 0. 1 - 0. 4 mg/kg – Ketamine 1. 5 - 2. 0 mg/kg – Fentanyl 2 - 30 mcg/kg
Pre-treatment/ Prime ( Time - 2 Minutes ) Lidocaine 1. 5 mg/kg iv n Defasciculating dose of non-depolarizing NMB n Beta-blocker or fentanyl n Induction agent n – Thiopental 3 - 5 mg/kg – Midazolam 0. 1 - 0. 4 mg/kg – Ketamine 1. 5 - 2. 0 mg/kg – Fentanyl 2 - 30 mcg/kg
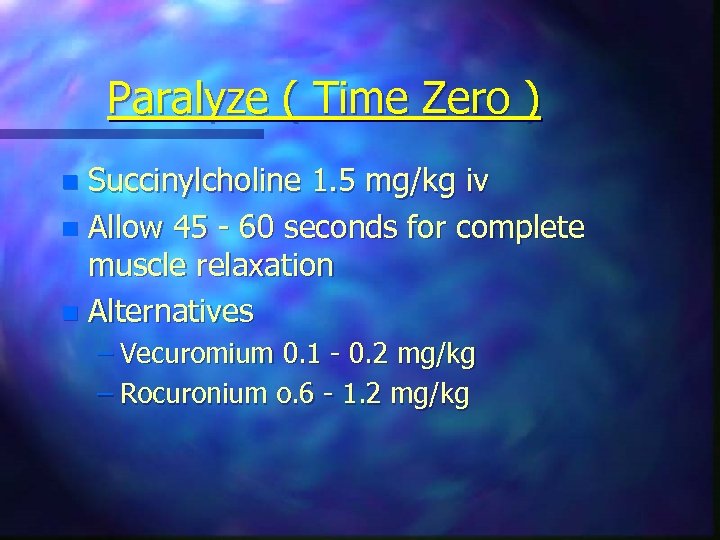 Paralyze ( Time Zero ) Succinylcholine 1. 5 mg/kg iv n Allow 45 - 60 seconds for complete muscle relaxation n Alternatives n – Vecuromium 0. 1 - 0. 2 mg/kg – Rocuronium o. 6 - 1. 2 mg/kg
Paralyze ( Time Zero ) Succinylcholine 1. 5 mg/kg iv n Allow 45 - 60 seconds for complete muscle relaxation n Alternatives n – Vecuromium 0. 1 - 0. 2 mg/kg – Rocuronium o. 6 - 1. 2 mg/kg
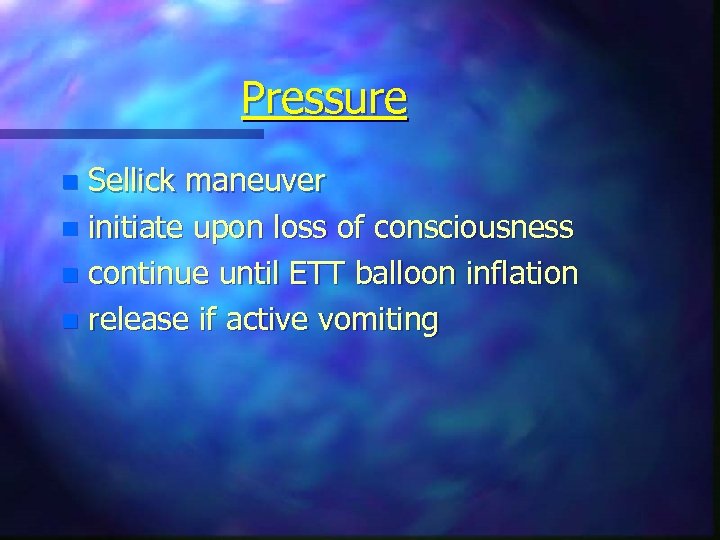 Pressure Sellick maneuver n initiate upon loss of consciousness n continue until ETT balloon inflation n release if active vomiting n
Pressure Sellick maneuver n initiate upon loss of consciousness n continue until ETT balloon inflation n release if active vomiting n
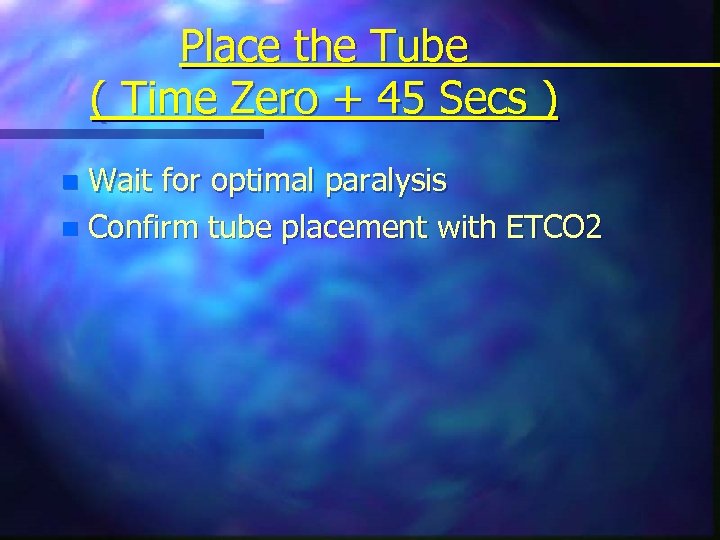 Place the Tube ( Time Zero + 45 Secs ) Wait for optimal paralysis n Confirm tube placement with ETCO 2 n
Place the Tube ( Time Zero + 45 Secs ) Wait for optimal paralysis n Confirm tube placement with ETCO 2 n
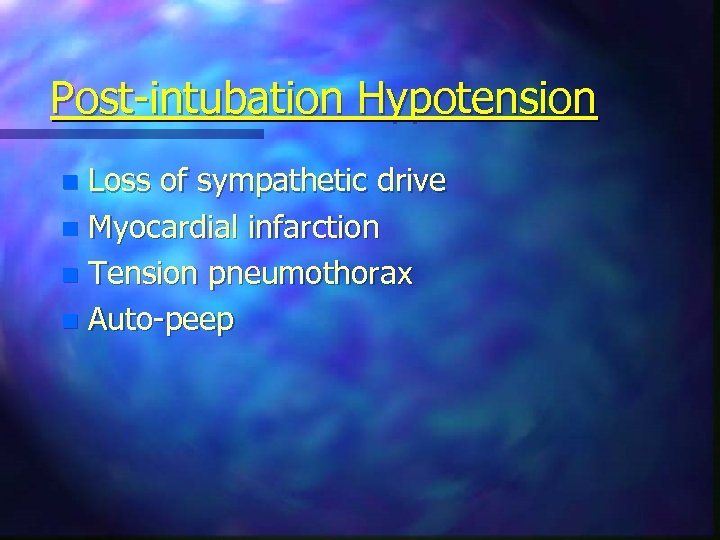 Post-intubation Hypotension Loss of sympathetic drive n Myocardial infarction n Tension pneumothorax n Auto-peep n
Post-intubation Hypotension Loss of sympathetic drive n Myocardial infarction n Tension pneumothorax n Auto-peep n
 Succinylcholine : Contraindications Hyperkalemia - renal failure n Active neuromuscular disease with functional denervation ( 6 days to 6 months) n Extensive burns or crush injuries n Malignant hyperthermia n Pseudocholinesterase deficiency n Organophosphate poisoning n
Succinylcholine : Contraindications Hyperkalemia - renal failure n Active neuromuscular disease with functional denervation ( 6 days to 6 months) n Extensive burns or crush injuries n Malignant hyperthermia n Pseudocholinesterase deficiency n Organophosphate poisoning n
 Succinylcholine : Complications Inability to secure airway n Increased vagal tone ( second dose ) n Histamine release ( rare ) n Increased ICP/ IOP/ intragastric pressure n Myalgias n Hyperkalemia with burns, NM disease n malignant hyperthermia n
Succinylcholine : Complications Inability to secure airway n Increased vagal tone ( second dose ) n Histamine release ( rare ) n Increased ICP/ IOP/ intragastric pressure n Myalgias n Hyperkalemia with burns, NM disease n malignant hyperthermia n
 Difficult Airway Kit Multiple blades and ETTs n ETT guides ( stylets, bougé, light wand) n Emergency nonsurgical ventilation ( LMA, combitube, TTJV ) n Emergency surgical airway access ( cricothyroidotomy kit, cricotomes ) n ETT placement verification n Fiberoptic and retrograde intubation n
Difficult Airway Kit Multiple blades and ETTs n ETT guides ( stylets, bougé, light wand) n Emergency nonsurgical ventilation ( LMA, combitube, TTJV ) n Emergency surgical airway access ( cricothyroidotomy kit, cricotomes ) n ETT placement verification n Fiberoptic and retrograde intubation n
 Emergency Surgical Airway Maxims they are usually a bloody mess, but. . . n a bloody surgical airway is better than an arrested patient with a nice looking neck n
Emergency Surgical Airway Maxims they are usually a bloody mess, but. . . n a bloody surgical airway is better than an arrested patient with a nice looking neck n
 Case # 2 42 year old female n right Pancoast tumor n RUL, RML, RLL collapse n ARDS on left n hypoxemic respiratory failure n cord compression C 7 - T 4 n
Case # 2 42 year old female n right Pancoast tumor n RUL, RML, RLL collapse n ARDS on left n hypoxemic respiratory failure n cord compression C 7 - T 4 n


