Electrolyte Disorders TJ Berger MS, PA-C
Sodium The main cation (positive ion) that circulates in the body fluids outside the cells
Hyponatremia
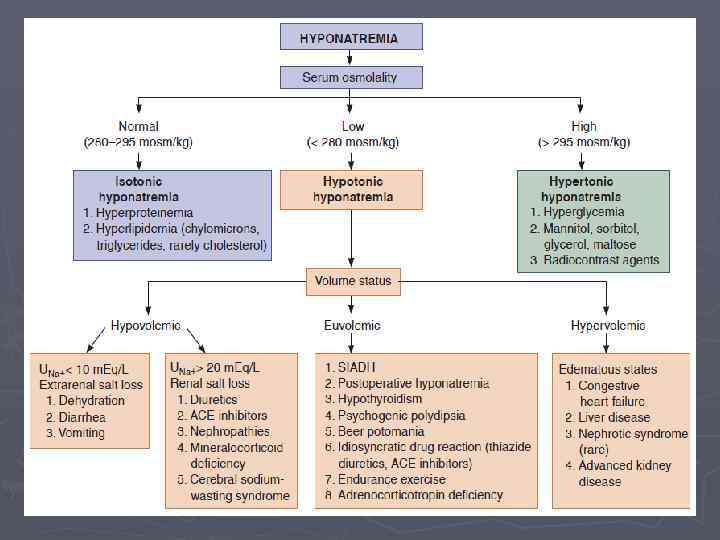
Hyponatremia ► Commonly defined as a serum sodium <135 m. Eq/L ► In virtually all patients, hyponatremia reflects water retention due to an inability to match water excretion with water ingestion ► Most commonly observed electrolyte disturbance (1 -2% of inpatients)
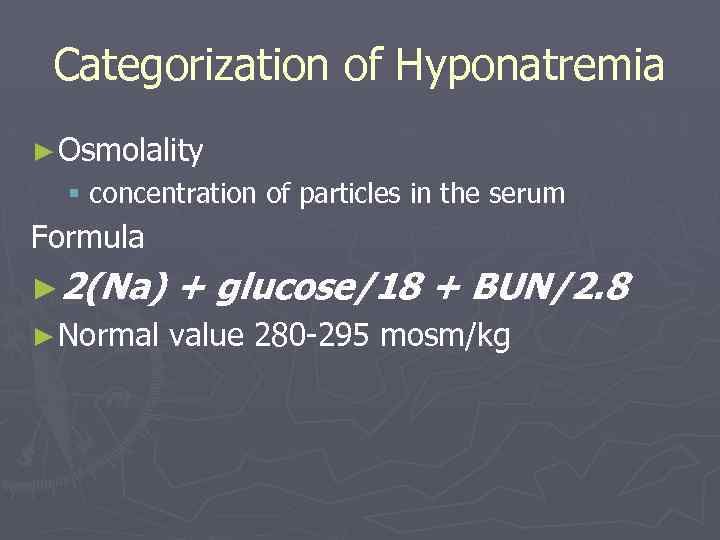
Categorization of Hyponatremia ► Osmolality § concentration of particles in the serum Formula ► 2(Na) + glucose/18 + BUN/2. 8 ► Normal value 280 -295 mosm/kg
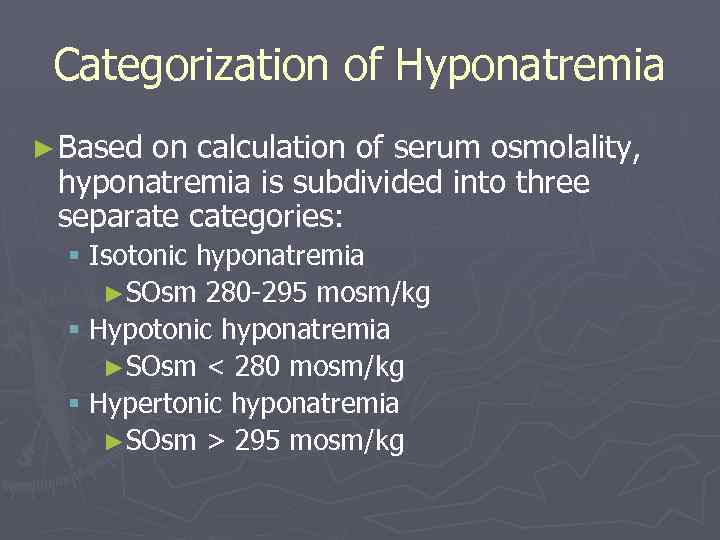
Categorization of Hyponatremia ► Based on calculation of serum osmolality, hyponatremia is subdivided into three separate categories: § Isotonic hyponatremia ►SOsm 280 -295 mosm/kg § Hypotonic hyponatremia ►SOsm < 280 mosm/kg § Hypertonic hyponatremia ►SOsm > 295 mosm/kg
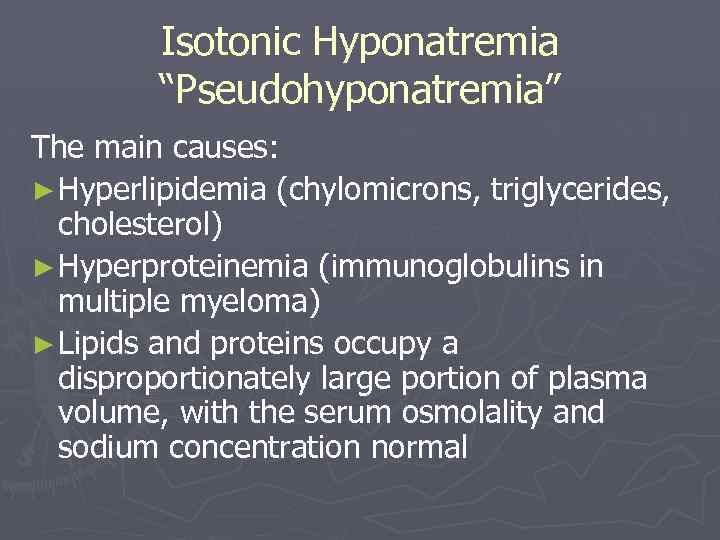
Isotonic Hyponatremia “Pseudohyponatremia” The main causes: ► Hyperlipidemia (chylomicrons, triglycerides, cholesterol) ► Hyperproteinemia (immunoglobulins in multiple myeloma) ► Lipids and proteins occupy a disproportionately large portion of plasma volume, with the serum osmolality and sodium concentration normal
Hypertonic Hyponatremia The main causes: ► Hyperglycemia § Water is drawn from the cells into the extracellular space, diluting the serum sodium ► Mannitol, sorbitol, glycerol, maltose ► Radiocontrast agents
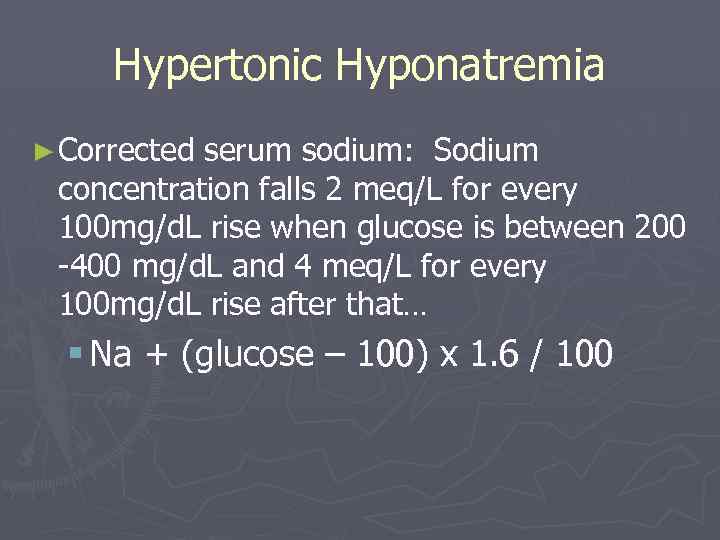
Hypertonic Hyponatremia ► Corrected serum sodium: Sodium concentration falls 2 meq/L for every 100 mg/d. L rise when glucose is between 200 -400 mg/d. L and 4 meq/L for every 100 mg/d. L rise after that… § Na + (glucose – 100) x 1. 6 / 100
Hypotonic Hyponatremia ► True hyponatremia in which water shifts into the cell, resulting in increased ICF ► Usually occurs because of impaired excretion of free water § Renal failure, SIADH ► Diagnosis involves evaluation of the volume status of the ECF § Three categories: hypo-, eu-, and hypervolemic
Hypovolemic Hypotonic Hyponatremia ► Low sodium (total sodium is decreased) ► Decreased extracellular fluid volume ► Setting of renal or extrarenal volume loss § Use of urine Na essential for differentiation ► Physiology § To maintain intravascular volume, ADH secretion increases, and free water is retained at the expense of serum osmolality
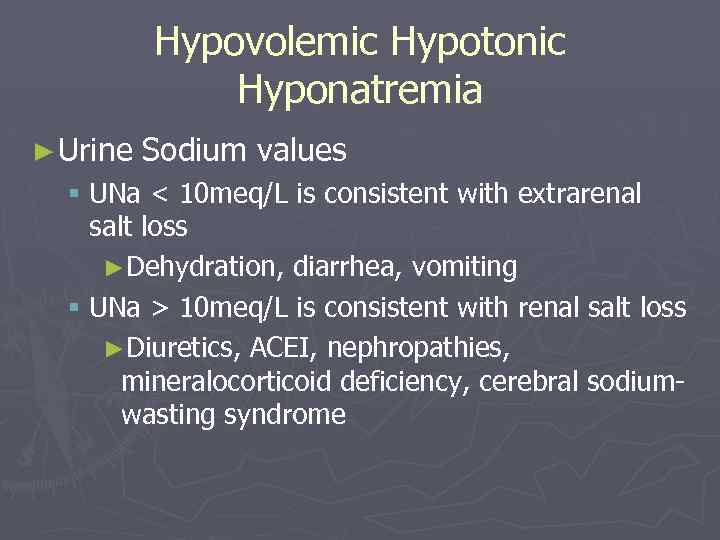
Hypovolemic Hypotonic Hyponatremia ► Urine Sodium values § UNa < 10 meq/L is consistent with extrarenal salt loss ►Dehydration, diarrhea, vomiting § UNa > 10 meq/L is consistent with renal salt loss ►Diuretics, ACEI, nephropathies, mineralocorticoid deficiency, cerebral sodiumwasting syndrome
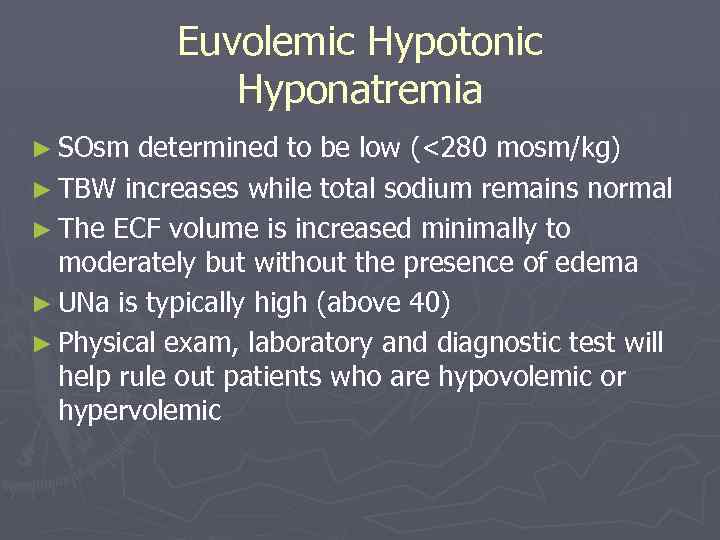
Euvolemic Hypotonic Hyponatremia ► SOsm determined to be low (<280 mosm/kg) ► TBW increases while total sodium remains normal ► The ECF volume is increased minimally to moderately but without the presence of edema ► UNa is typically high (above 40) ► Physical exam, laboratory and diagnostic test will help rule out patients who are hypovolemic or hypervolemic
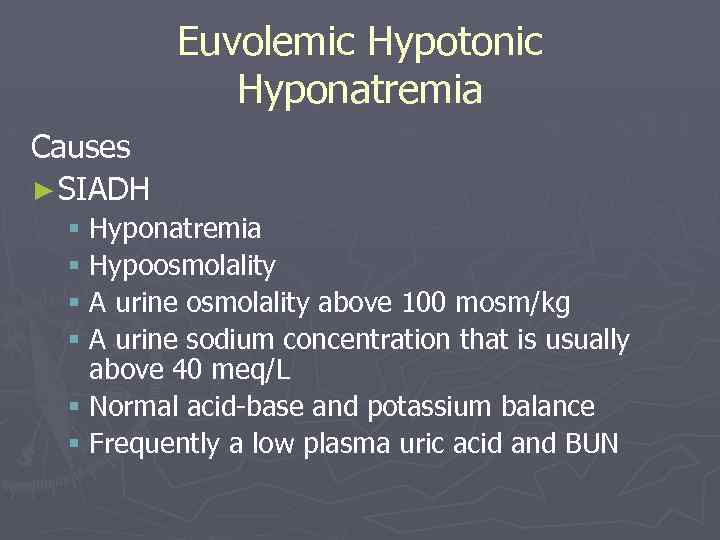
Euvolemic Hypotonic Hyponatremia Causes ► SIADH § Hyponatremia § Hypoosmolality § A urine osmolality above 100 mosm/kg § A urine sodium concentration that is usually above 40 meq/L § Normal acid-base and potassium balance § Frequently a low plasma uric acid and BUN
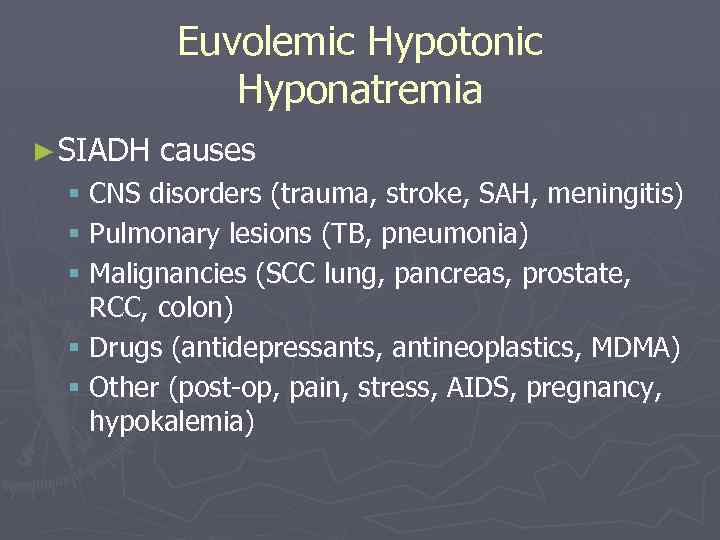
Euvolemic Hypotonic Hyponatremia ► SIADH causes § CNS disorders (trauma, stroke, SAH, meningitis) § Pulmonary lesions (TB, pneumonia) § Malignancies (SCC lung, pancreas, prostate, RCC, colon) § Drugs (antidepressants, antineoplastics, MDMA) § Other (post-op, pain, stress, AIDS, pregnancy, hypokalemia)
Euvolemic Hypotonic Hyponatremia Causes ► Post operative § Secondary to administration of excessive hypotonic fluid in the setting of elevated ADH levels related to pain with continuing excretion of hypertonic urine ► Hypothyroidism § Secondary to H 2 O retention from elevated ADH and non-hormonal alterations in the handling of water by the kidneys
Euvolemic Hypotonic Hyponatremia ► Psychogenic polydipsia § Excess free water intake (>10 L/d) § Euvolemia maintained through the renal excretion of sodium (UNa >20) § Suppressed ADH ► Beer potomania § Nutritional nugget- beer contains <5 meq/L of sodium § Cirrhotic patients often have elevated ADH and decreased GFR
Euvolemic Hypotonic Hyponatremia Causes ► Idiosyncratic drug reaction § Thiazides may cause an excessive renal sodium loss and water retention § ACEI can cause central polydipsia and increased ADH secretion ► Endurance exercise § Excessive fluid overload and continued ADH secretion after reperfusion of the exercise induced ischemic splanchnic bed
Euvolemic Hypotonic Hyponatremia Causes ► Adrenocorticotropin deficiency § Laboratory values may be similar to SIADH § Low plasma bicarbonate (or total CO 2) levels suggest ACTH deficiency
Hypervolemic Hypotonic Hyponatremia ► Total body sodium increases ► TBW increases to a greater extent ► The ECF is increased markedly, with the presence of edema ► UNa is generally < 10 meq/L unless the patient is taking diuretics
Hypervolemic Hypotonic Hyponatremia Causes ► CHF § Total body sodium is increased § Effective circulating volume is sensed as inadequate by baroreceptors stimulating increased ADH and aldosterone ► Liver disease ► Nephrotic syndrome / advanced renal failure
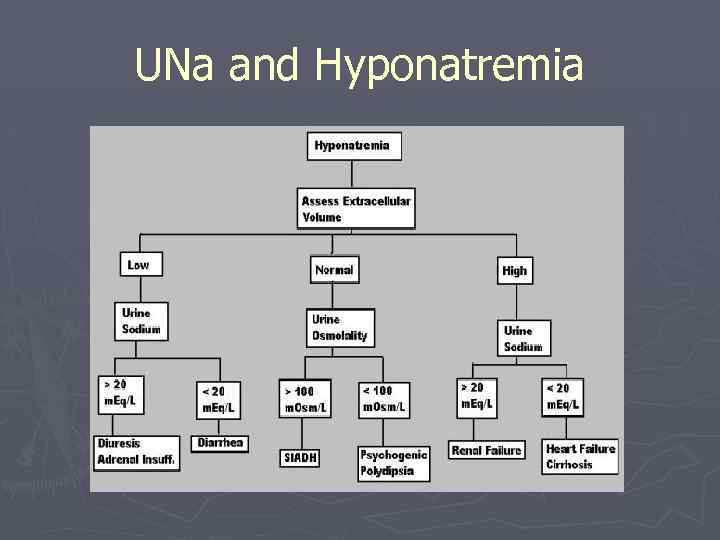
UNa and Hyponatremia
Hyponatremia History ► The number and severity of symptoms increase with the degree of hyponatremia and the rapidity with which it develops ► When the serum sodium level falls gradually, over a period of several days or weeks, sodium levels as low as 110 m. Eq/L may be reached with minimal symptomatology ► In contrast, an equivalent fall in serum sodium level over 24 -48 hours may overwhelm compensatory mechanisms, leading to severe cerebral edema, coma, or brainstem herniation
Hyponatremia Symptoms ► Mild anorexia ► Headache ► Muscle cramps ► Significant alteration in mental status § Obtundation § Coma § Status epilepticus
Hyponatremia ► Physical exam § Dry mucous membranes, tachycardia, diminished skin turgor, and orthostasis suggest hypovolemic hyponatremia due to excessive loss of body fluids and replacement with inappropriately dilute fluids § Pulmonary rales, S 3 gallop, jugular venous distention, peripheral edema, or ascites suggest hypervolemic hyponatremia due to excess retention of sodium and free water § Patients who lack findings of hypovolemia or hypervolemia are considered to have euvolemic hyponatremia
Hyponatremia Treatment strategies ► Water restriction ► NSS ► Diuretics ► Hypertonic saline
Hyponatremia ► In patients who are treated to raise their serum sodium, use a rate of correction that accounts for the following issues: § The risk of osmotic demyelination (formerly referred to as central pontine myelinolysis) § The risk of brain herniation § The risk of seizures § The severity of symptoms
Hyponatremia ► Goals of therapy: § Raise the serum sodium concentration by 4 to 6 meq/L in a 24 -hour period § In patients who require emergency therapy, this goal should be achieved quickly, over six hours or less; thereafter, the serum sodium can be maintained at a constant level for the remainder of the 24 -hour period to avoid overly rapid correction § Every effort should be made to keep the rise in serum sodium less than 9 meq/L in any 24 -hour period § In general, the same rate of rise can be continued on subsequent days until the sodium is normal or near normal
Hyponatremia Treatment Therapeutic goal is to increase the serum sodium level rapidly by 1 -2 m. Eq/L over the first 2 -3 hours § Total of 12 m. Eq/L over 24 hours ► Eliminate any source of free water ► In symptomatic patients with healthy renal function, the serum sodium level may correct spontaneously without further intervention ► Patients with seizures, severe confusion, coma, or signs of brainstem herniation should receive hypertonic (3%) saline to rapidly correct serum sodium level toward normal but only enough to arrest the progression of symptoms ►
Hyponatremia Treatment ► Overzealous correction of chronic hyponatremia is associated with the development of osmotic dymelination, characterized by focal demyelination in the pons and extrapontine areas ► Symptoms (dysarthria, dysphagia, seizures, altered mental status, quadriparesis, hypotension) typically begin 1 -3 days after correction of serum sodium level ► The condition is often irreversible; slow, cautious correction of serum sodium level and maintenance of adequate oxygenation in these patients is important
Hypovolemic Hyponatremia Treatment ► Patients have decreased total body sodium stores ► If symptoms are mild to moderately severe, treat with isotonic saline ► Monitor serum sodium levels frequently to ensure that serum sodium level increases no faster than 9 m. Eq/L/d
Euvolemic Hyponatremia Treatment ► Implies normal sodium stores and a total body excess of free water ► Free water restriction and correction of the underlying condition ► AVP (vasopressin) receptor antagonists show promise as effective and well-tolerated therapy for SIADH § The vasopressin receptor antagonists produce a selective water diuresis (also called aquaresis) without affecting sodium and potassium excretion § The ensuing loss of free water will tend to correct the hyponatremia § Tolvaptan
Hypervolemic Hyponatremia Treatment ► Patients have increased total body sodium stores ► Treatment consists of sodium and water restriction and attention to the underlying cause
Hypernatremia
Hypernatremia ► Defined as a serum sodium > 145 meq/L ► Represents a relative deficit of water in relation to solute ► Most often due to unreplaced water losses from the GI or respiratory tract ► Urine osmolality helps differentiate renal from nonrenal water loss
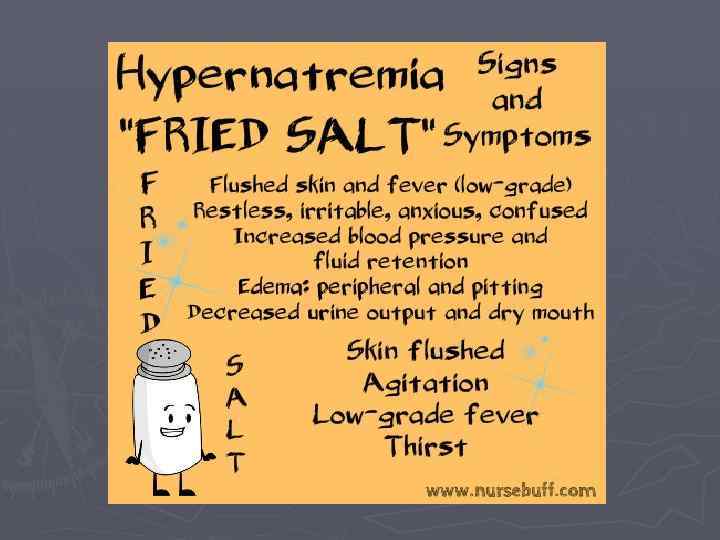
Hypernatremia Symptoms ► Nonspecific ► Anorexia, restlessness, nausea, and vomiting occur early ► Followed by altered mental status, lethargy or irritability, and, eventually, stupor or coma ► Musculoskeletal symptoms may include twitching, hyperreflexia, ataxia, or tremor ► Neurological symptoms are generally nonfocal (mental status changes, ataxia, seizure), but focal deficits such as hemiparesis have been reported
Hypernatremia Signs ► Assessment of overall fluid status is important ► Note volume status, including mucous membranes, skin turgor, orthostatic vital signs, and neck veins ► As neurological deficits are common, perform a thorough neurological examination ► Significant hypovolemia can result when hypotonic fluid losses cause hypernatremia. The physical findings are those of dehydration or even hypovolemic shock, with tachycardia, orthostasis, and hypotension
Hypernatremia Labs Check serum glucose level to ensure that osmotic diuresis has not occurred ► Basic workup: Uosm and sodium levels § Uosm: extreme range of 50 - 1400 mosm/kg water, but average is about 500 - 800 mosm § Uosm>400 mosm/kg- renal water conserving ability is functioning § Uosm<250 mosm/kg- characteristic of central and nephrogenic diabetes insipidus
Hypernatremia Diagnostic imaging ► Head CT scan or MRI is suggested in all patients with severe hypernatremia § Traction on dural bridging veins and sinuses caused by movement of water from the brain and brain shrinkage can lead to intracranial hemorrhage (SDH) § Hemoconcentration from total body water loss may lead to dural sinus thrombosis § Imaging studies may indicate a central cause for hypernatremia
Hypernatremia Treatment ► Correction § If hypernatremia is too rapidly corrected, the osmotic imbalance may cause water to preferentially enter brain cells, causing cerebral edema and potentially severe neurologic impairment
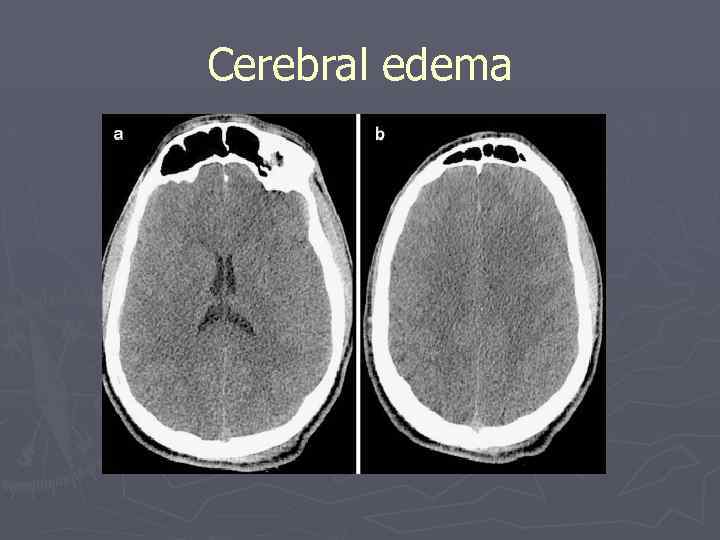
Cerebral edema
Hypernatremia Treatment ► Management of hypernatremia revolves around two tasks § Restoration of normal serum tonicity, and diagnosis and treatment of the underlying etiology § When possible, providing free water to a patient orally is preferred ► Hypernatremia should not be corrected at a rate greater than 1 -2 m. Eq/L per hour
Hypernatremia Treatment ► Hypernatremia with hypovolemia § 0. 9% saline to restore the volume deficit and to treat the hyperosmolarity, since the osmolality of isotonic saline (308 mosm/kg) is often lower than that of the plasma § Followed by 0. 45% saline to replace any remaining free water deficit
Hypernatremia ► Hypernatremia with euvolemia § PO water or D 5 W IV will result in excretion of excess sodium in the urine ► Hypernatremia with hypervolemia § D 5 W to reduce hyperosmolality will also expand vascular volume § Addition of loop diuretic will facilitate sodium excretion § HD may be necessary in renal insufficiency
Hypernatremia ► Calculation of water deficit ► Free water deficit= § TBW (wt. in kg) x (0. 4 -0. 6) x (Na – 140)/140 ► Percentage of TBW should be as follows: § Young men - 0. 6% § Young women and elderly men - 0. 5% § Elderly women - 0. 4%
Case Study 1 ► At precisely 4: 37 am, a telemetry nurse beeps you with some urgent abnormal lab values. He seems particularly concerned about the low sodium level. Please review the labs and offer appropriate orders / likely diagnosis. ► By the way, he also noticed that there was no prn dulcolax order in the computer.
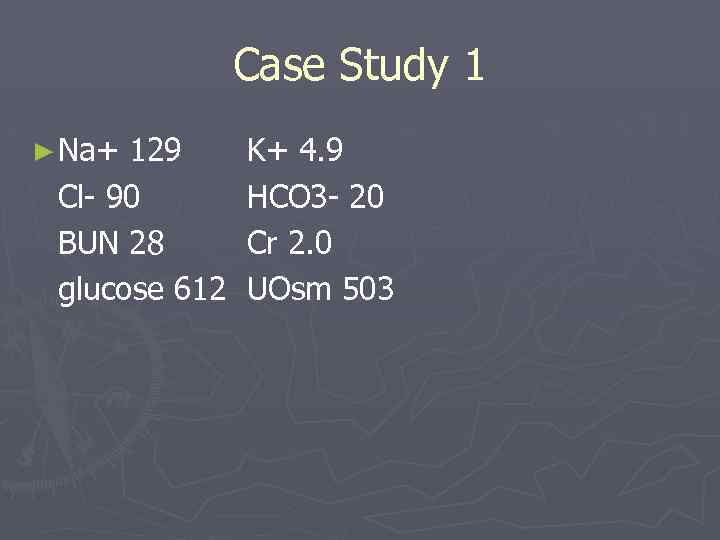
Case Study 1 ► Na+ 129 K+ 4. 9 Cl- 90 HCO 3 - 20 BUN 28 Cr 2. 0 glucose 612 UOsm 503
Case Study 1 ► What is the corrected Na+? ► What are some possible treatment strategies? ► What is the likely diagnosis? ► Enter prn dulcolax
Case Study 2 ► A 92 year old, 50 kg NH resident is brought to the ED by ambulance; paramedics were quickly dispatched to another call. ► You are asked to evaluate the patient with no further history available at this time, as the patient has advanced Alzheimer’s. ► Significant PE findings include tachycardia, orthostasis, and decreased skin turgor.
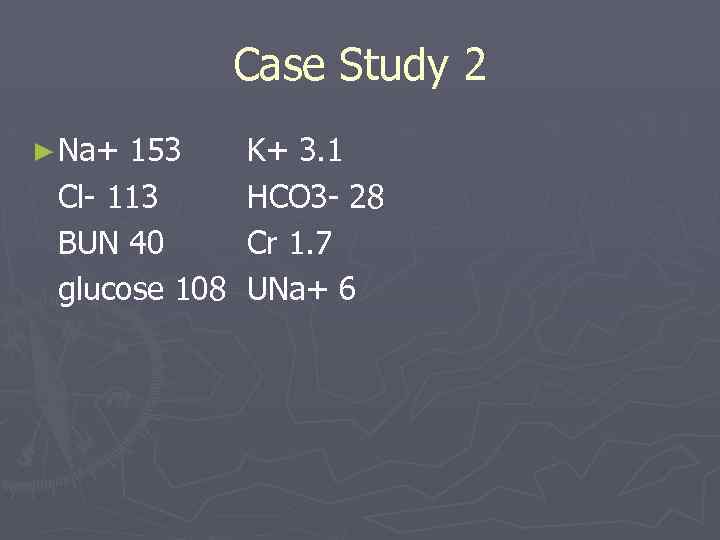
Case Study 2 ► Na+ 153 K+ 3. 1 Cl- 113 HCO 3 - 28 BUN 40 Cr 1. 7 glucose 108 UNa+ 6
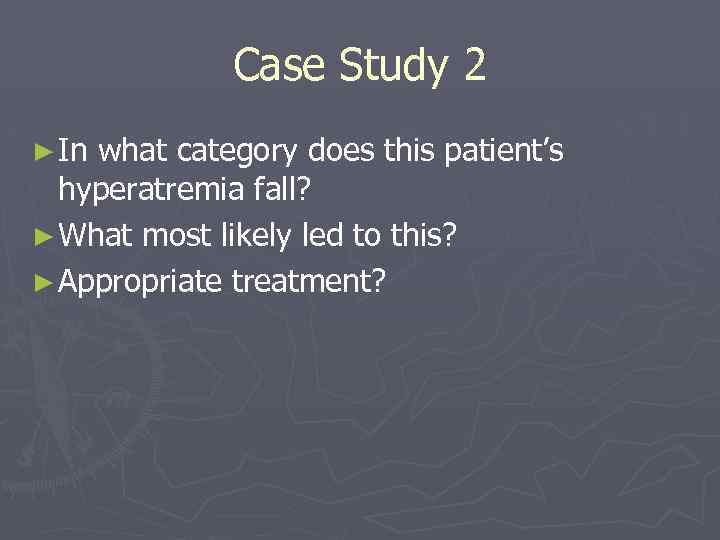
Case Study 2 ► In what category does this patient’s hyperatremia fall? ► What most likely led to this? ► Appropriate treatment?
Potassium The main cation (positive ion) found inside the cells (95%)
Hypokalemia
Hypokalemia ► The reference range for serum potassium level is 3. 5 -5 m. Eq/L, with total body potassium stores of approximately 50 m. Eq/kg (approximately 3500 m. Eq in a 70 kg person) ► Hypokalemia is defined as a potassium level less than 3. 5 m. Eq/L ► Moderate hypokalemia § 2. 5 -3 m. Eq/L ► Severe hypokalemia § <2. 5 m. Eq/L
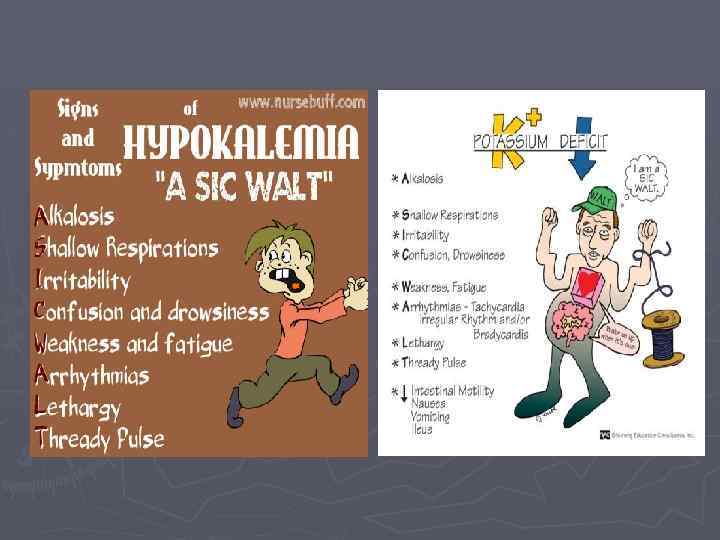
Hypokalemia Symptoms ► Palpitations ► Skeletal muscle weakness or cramping ► Paralysis, paresthesias ► Constipation ► Nausea or vomiting ► Abdominal cramping ► Polyuria, nocturia, or polydipsia ► Psychosis, delirium, or hallucinations ► Depression
Hypokalemia Signs ► Ileus ► Hypotension ► PVCs, PACs, bradycardia, tachycardia ► Cardiac arrest ► Hypoventilation, respiratory distress / failure ► Lethargy or other mental status changes ► Decreased muscle strength, fasciculations, tetany ► Decreased tendon reflexes ► Cushingoid appearance
Hypokalemia Lab Studies: ► Serum potassium level <3. 5 m. Eq/L ► BUN and creatinine ► Glucose, magnesium, calcium, and/or phosphorous if coexistent electrolyte disturbances are suspected ► Consider digoxin level if the patient is on a digitalis preparation; hypokalemia can potentiate digitalisinduced arrhythmias ► Consider arterial blood gases (ABG): Alkalosis can cause potassium to shift from extracellular to intracellular
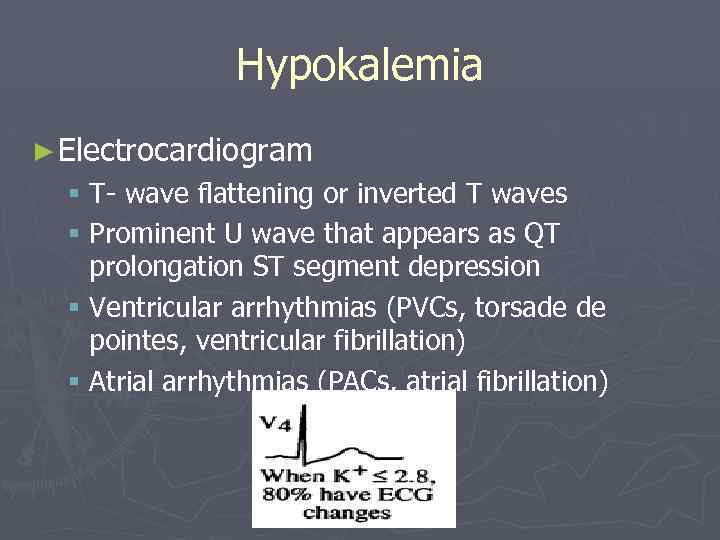
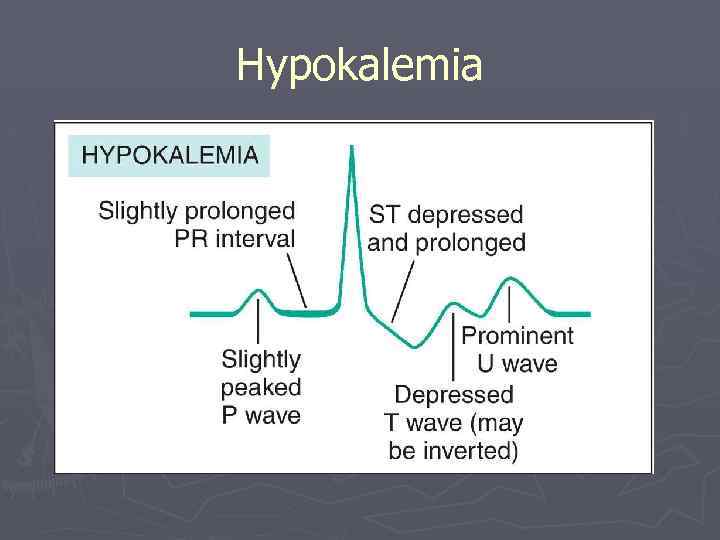
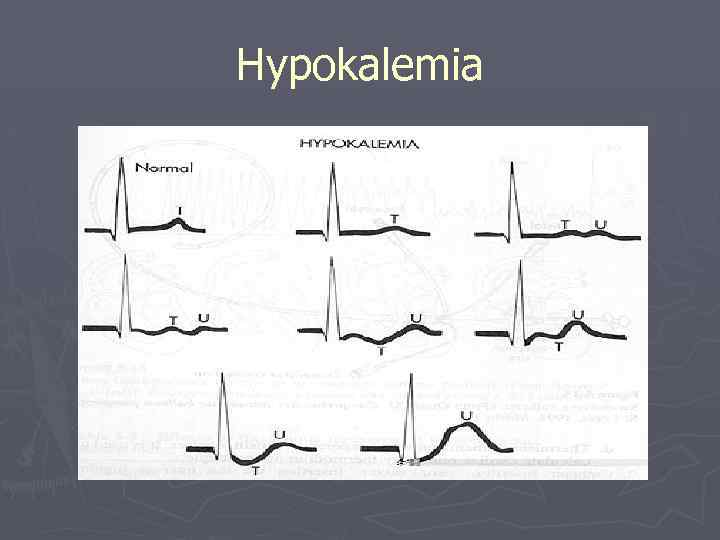
Hypokalemia ► Electrocardiogram § T- wave flattening or inverted T waves § Prominent U wave that appears as QT prolongation ST segment depression § Ventricular arrhythmias (PVCs, torsade de pointes, ventricular fibrillation) § Atrial arrhythmias (PACs, atrial fibrillation)
Hypokalemia
Hypokalemia
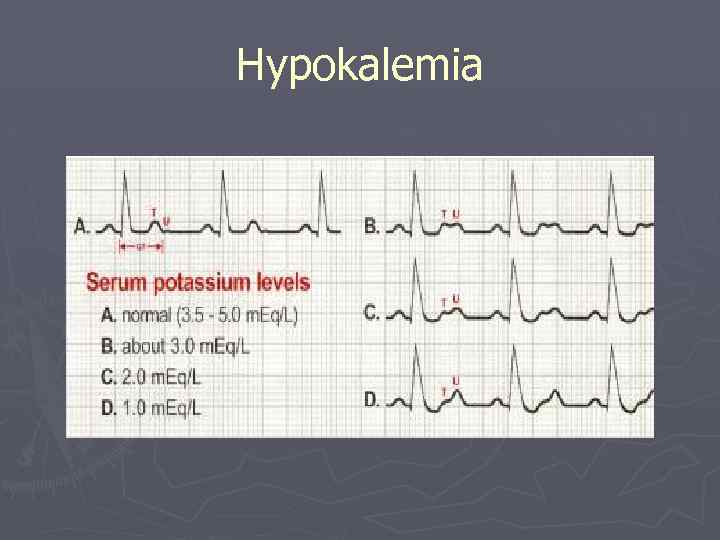
Hypokalemia
Hypokalemia Treatment ► Cardiac monitor, IV access, assessment of respiratory status ► Mild or moderate hypokalemia (potassium of 2. 53. 5 m. Eq/L) § Oral potassium replacement therapy § If cardiac arrhythmias or significant symptoms are present, then more aggressive therapy is warranted ► Severe hypokalemia (<2. 5 m. Eq/L) § IV potassium should be given ► Serum potassium is difficult to replenish if serum magnesium is low
Hyperkalemia
Hyperkalemia ► A potassium level greater than 5. 5 m. Eq/L Ranges are as follows: § 5. 5 -6. 0 m. Eq/L - Mild condition § 6. 1 -7. 0 m. Eq/L - Moderate condition § 7. 0 m. Eq/L and greater - Severe condition
Hyperkalemia Causes ► Decreased or impaired potassium excretion § acute or chronic renal failure (most common) § Potassium-sparing diuretics § Urinary obstruction § Sickle cell disease § Addison disease § SLE ► Additions of potassium into extracellular space § Potassium supplements (PO/IV, salt substitutes) § Rhabdomyolysis § Hemolysis (venipuncture, blood transfusions, burns, tumor lysis)
Hyperkalemia Causes ► Transmembrane shifts (from the intracellular to extracellular space) ►As observed with acidosis § Medication effects (acute digitalis toxicity, beta-blockers, succinylcholine) ► Factitious or pseudohyperkalemia § Improper blood collection (ischemic blood draw from venipuncture technique) § laboratory error § leukocytosis, thrombocytosis
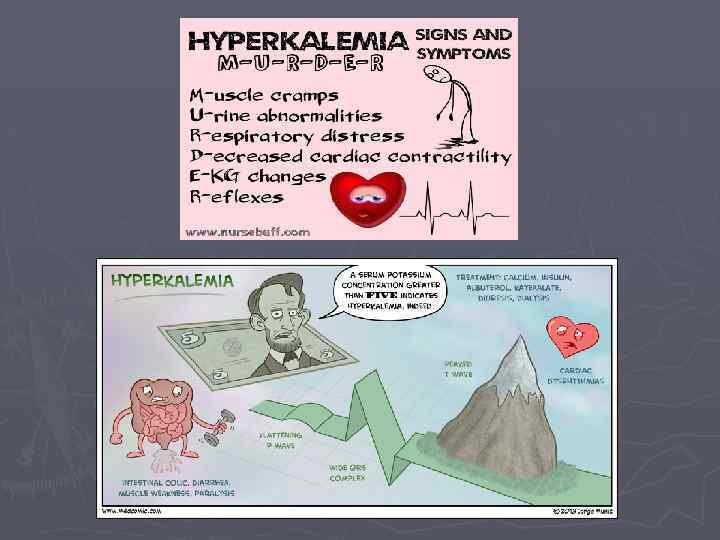
Hyperkalemia ► Signs and Symptoms § Fatigue § Weakness § Tingling, numbness, or other unusual sensations § Paralysis § Palpitations § Difficulty breathing
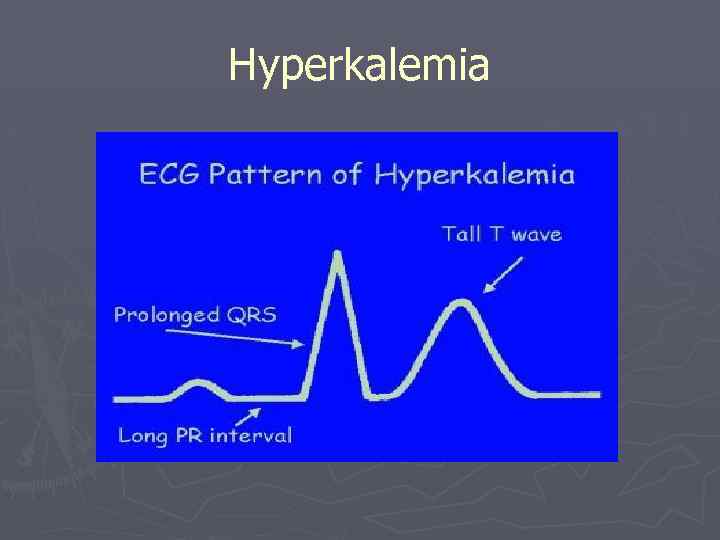
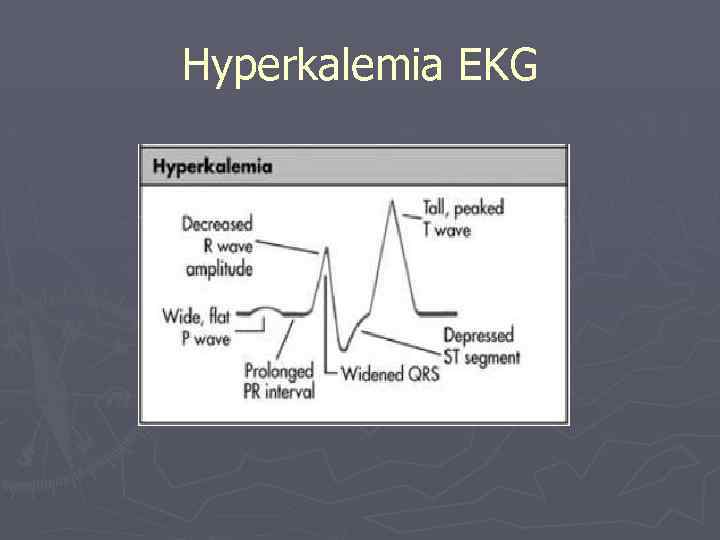
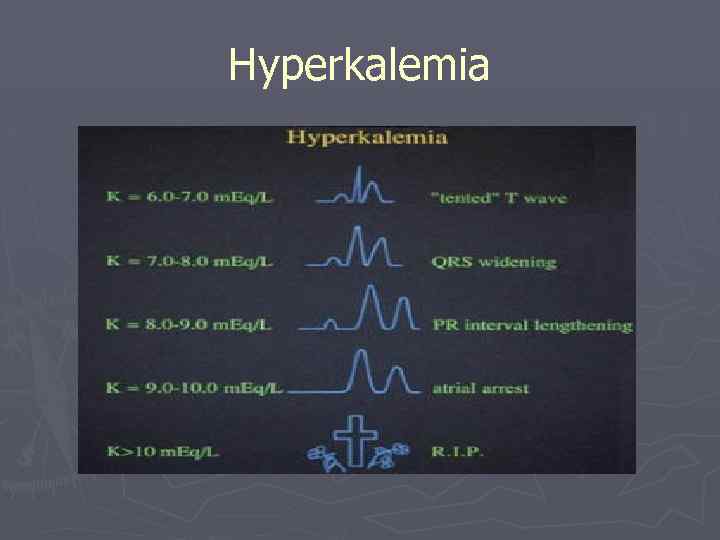
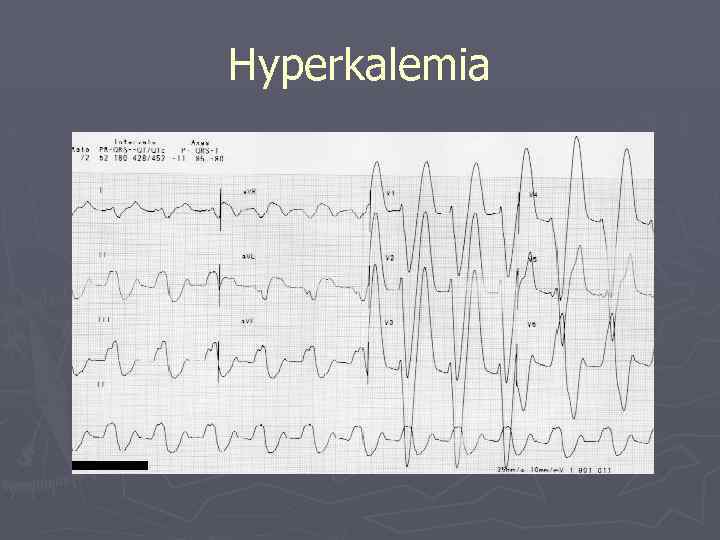
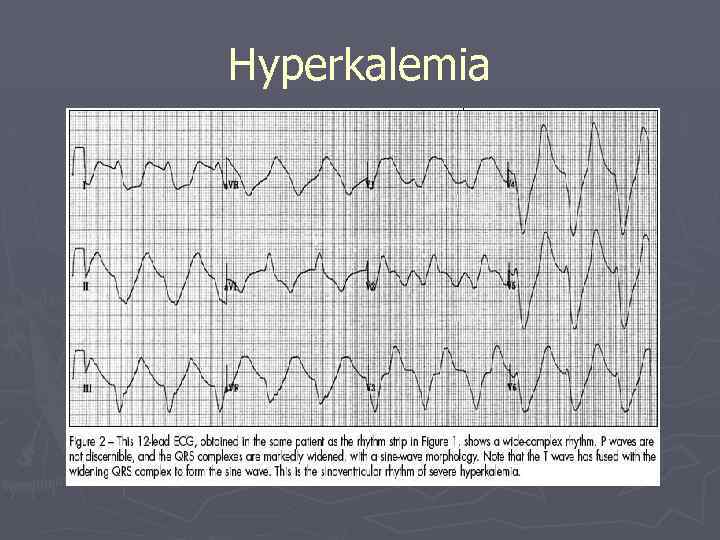
Hyperkalemia ► Electrocardiogram § Prolonged PR interval § Flattened P waves § Tall, peaked T waves § ST depression § S and T wave merging § Widened QRS…sine wave
Hyperkalemia
Hyperkalemia EKG
Hyperkalemia
Hyperkalemia
Hyperkalemia
Hyperkalemia Treatment ► Directed at antagonizing the membrane effects of potassium ► Driving extracellular potassium into the cells ► Removing excess potassium from the body
Hyperkalemia Treatment ► Calcium § Hyperkalemia induces repolarization of the resting membrane potential and leads to inactivation of NA+ channels § Calcium antagonizes this effect and is protective within minutes § Gluconate / chloride
Hyperkalemia Treatment ► Insulin and glucose § Increasing the availability of insulin lowers the plasma K+ concentration by driving K+ into the cells by enhancing the activity of the Na-KATPase pump in skeletal muscle § Effect begins in 15 minutes, peaks at one hour and lasts for several hours § 10 Units IV insulin followed by 50 m. L D 50
Hyperkalemia Treatment ► Sodium bicarbonate § Raising the p. H results in hydrogen ion release from the cells which drives potassium intracellularly § Effect begins within 30 -60 minutes and persists for several hours § 1 amp (45 meq) infused over 5 minutes
Hyperkalemia Treatment ► Beta 2 -adrenergic agonists § Drives K+ into the cells by increasing the Na-KATPase activity § Lowers K+ by 0. 5 -1. 5 meq/L § 10 -20 mg in 4 m. L of saline nebulized § Peak onset is about 90 minutes
Hyperkalemia Treatment ► Loop or thiazide diuretics § Only transiently lower the plasma K+ concentration § Patients with renal disease are unlikely to have a good response to this therapy
Hyperkalemia Treatment ► Cation exchange resin (Kayexalate) § In the gut, this resin takes up K+ and releases Na+ § Each gram of resin may bind as much as 1 meq of K+ and release 1 -2 meq of Na+ § Given either orally or as a retention enema ► 15 -30 grams provided in 60 -120 m. L of 70% sorbitol
Hyperkalemia Treatment ► Hemodialysis § Used if more conservative measures previously listed are ineffective § Can remove 25 -50 meq of K+ per hour
