72f24833609d8b64a165479106ea60f9.ppt
- Количество слайдов: 32
 Elective Primary Cesarean Section Paul Wendel, MD Associate Professor Residency Director UAMS Department of Obstetrics & Gynecology
Elective Primary Cesarean Section Paul Wendel, MD Associate Professor Residency Director UAMS Department of Obstetrics & Gynecology
 • Patient choice • Maternal request • On demand All refer to primary cesarean section in the absence of medical/obstetrical indications.
• Patient choice • Maternal request • On demand All refer to primary cesarean section in the absence of medical/obstetrical indications.
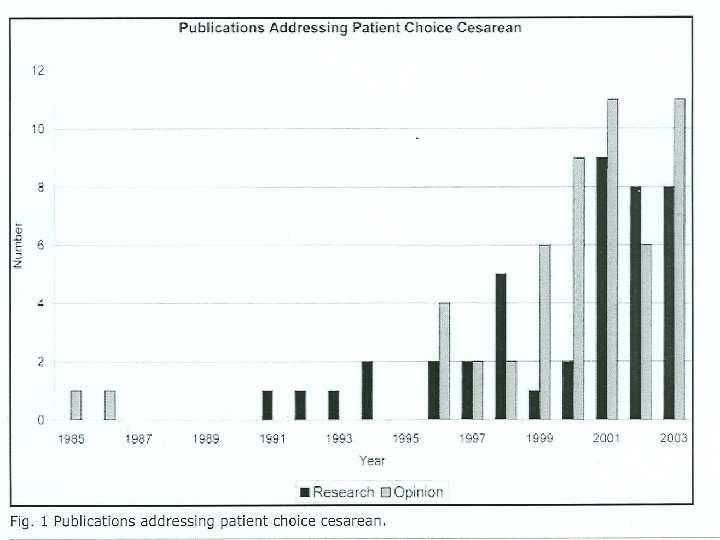
 Concept Origins: Most recently traced to 1985 l Stimulated by medicolegal case involving intrapartum fetal neurologic injury l Authors discussed “prophylactic cesarean section” ‘at term’ l Notion of informed consent for route of delivery was introduced l C-section offered as a means of avoiding the risks associated with vaginal delivery Feldman, GB Prophylactic cesarean at term? NEJM 1985; 312 pp. 1264 -67
Concept Origins: Most recently traced to 1985 l Stimulated by medicolegal case involving intrapartum fetal neurologic injury l Authors discussed “prophylactic cesarean section” ‘at term’ l Notion of informed consent for route of delivery was introduced l C-section offered as a means of avoiding the risks associated with vaginal delivery Feldman, GB Prophylactic cesarean at term? NEJM 1985; 312 pp. 1264 -67
 Patient Perspective Elective cesarean sections currently account for 4 -18% of all c-sections.
Patient Perspective Elective cesarean sections currently account for 4 -18% of all c-sections.
 Why do Women ask for C-Sections? l Extreme tocophobia (fear of childbirth) l Death (patient or baby) l Fetal injury l Genital tract injury
Why do Women ask for C-Sections? l Extreme tocophobia (fear of childbirth) l Death (patient or baby) l Fetal injury l Genital tract injury
 When Psychotherapy was employed by trained professionals to address tocophobia: l 2/3 women ultimately chose vaginal birth These same women… l Ultimately viewed their birth experience as good
When Psychotherapy was employed by trained professionals to address tocophobia: l 2/3 women ultimately chose vaginal birth These same women… l Ultimately viewed their birth experience as good
 Physicians’ Perspective l Several studies have been done in UK, New Zealand, Ireland, Canada, Israel regarding physicians’ and midwives’ attitudes toward “elective c-section” 7 -30% of OB/GYN’s and 4. 4% of midwives preferred csections for themselves if female or their partner if male l 62 -81% reported a willingness to perform c-sections on demand l
Physicians’ Perspective l Several studies have been done in UK, New Zealand, Ireland, Canada, Israel regarding physicians’ and midwives’ attitudes toward “elective c-section” 7 -30% of OB/GYN’s and 4. 4% of midwives preferred csections for themselves if female or their partner if male l 62 -81% reported a willingness to perform c-sections on demand l
 Physicians’ Perspective (con’t) l Similar to their patients, obstetricians cited the following as reasons leading to primary elective c-sections: l Fear of childbirth 27% l Perineal injury 80 -95% l Fetal injury 24 -39% l Anal or urinary incontinence 81 -83% l Sexual dysfunction 58 -59% l Convenience 17 -39% l Control 39% l Pain 7%
Physicians’ Perspective (con’t) l Similar to their patients, obstetricians cited the following as reasons leading to primary elective c-sections: l Fear of childbirth 27% l Perineal injury 80 -95% l Fetal injury 24 -39% l Anal or urinary incontinence 81 -83% l Sexual dysfunction 58 -59% l Convenience 17 -39% l Control 39% l Pain 7%
 Attitudes of Urogynecologist’s & MFM’s to Elective C-sections l Survey was distributed by UNC via web base l 53% of SMFM/AUGS members responded
Attitudes of Urogynecologist’s & MFM’s to Elective C-sections l Survey was distributed by UNC via web base l 53% of SMFM/AUGS members responded
 Survey Results l Overall, 65% of physicians would perform an elective primary cesarean section l Compared with other countries: l 69% England l 67% Australia/New Zealand
Survey Results l Overall, 65% of physicians would perform an elective primary cesarean section l Compared with other countries: l 69% England l 67% Australia/New Zealand
 AUGS / SMFM Survey Comparison l 80% of AUGS members vs. 55% of SMFM members for primary elective c-section l 45% of AUGS and 9. 5% of SMFM members would choose a primary c-section for themselves or their partners
AUGS / SMFM Survey Comparison l 80% of AUGS members vs. 55% of SMFM members for primary elective c-section l 45% of AUGS and 9. 5% of SMFM members would choose a primary c-section for themselves or their partners
 Ethical Principles Can an elective c-section for an uncomplicated pregnancy be ethically justified? l Decision making based on: l Beneficence l Nonmaleficence l Autonomy l Justice l Voracity l
Ethical Principles Can an elective c-section for an uncomplicated pregnancy be ethically justified? l Decision making based on: l Beneficence l Nonmaleficence l Autonomy l Justice l Voracity l
 Ethical Principles l Beneficence: physicians responsibility to promote the patients’ health/welfare l Nonmaleficence: complimentary principle refers to the physician’s obligation to do no harm to the patient l Autonomy: obligates the physician to discuss reasonable alternatives and elicit a decision within the framework of informed consent
Ethical Principles l Beneficence: physicians responsibility to promote the patients’ health/welfare l Nonmaleficence: complimentary principle refers to the physician’s obligation to do no harm to the patient l Autonomy: obligates the physician to discuss reasonable alternatives and elicit a decision within the framework of informed consent
 Ethical Principles Typically, patients retain a “negative right” (right to decline care) but do not hold a “positive right” (the right to demand care that may be unnecessarily risky or medically unproven).
Ethical Principles Typically, patients retain a “negative right” (right to decline care) but do not hold a “positive right” (the right to demand care that may be unnecessarily risky or medically unproven).
 Ethical Principles l Justice: requires that a physician treat patients fairly and make decisions that consider societal good with respect to limited health resources l Voracity: refers to truthfulness in patient counseling
Ethical Principles l Justice: requires that a physician treat patients fairly and make decisions that consider societal good with respect to limited health resources l Voracity: refers to truthfulness in patient counseling
 Committee of the Ethical Aspects of Human Reproduction of the International Federation of Obstetrics and Gynecology (FIGO) in 1999 issued a report regarding c-section for nonmedical reasons: ØC-section was a surgical procedure ØGreater allocation of resources for c-section ØVaginal delivery was safer in long/short term for mother/fetus ØElective c-section was not ethically justified
Committee of the Ethical Aspects of Human Reproduction of the International Federation of Obstetrics and Gynecology (FIGO) in 1999 issued a report regarding c-section for nonmedical reasons: ØC-section was a surgical procedure ØGreater allocation of resources for c-section ØVaginal delivery was safer in long/short term for mother/fetus ØElective c-section was not ethically justified
 American College of OB/GYN Committee on Ethics (2003) If a patient requests cesarean section after informed counseling and the physician believes it will promote the overall health of patient and fetus, “…the elective c-section is ethically justified. ” If the physician disagrees, the patient should be referred to another provider.
American College of OB/GYN Committee on Ethics (2003) If a patient requests cesarean section after informed counseling and the physician believes it will promote the overall health of patient and fetus, “…the elective c-section is ethically justified. ” If the physician disagrees, the patient should be referred to another provider.
 Medical Issues Historically, c-sections have a higher risk of maternal mortality than vaginal delivery. However, most studies do not adjust for: èElective vs. emergency c-section èContributing medical/obstetric conditions
Medical Issues Historically, c-sections have a higher risk of maternal mortality than vaginal delivery. However, most studies do not adjust for: èElective vs. emergency c-section èContributing medical/obstetric conditions
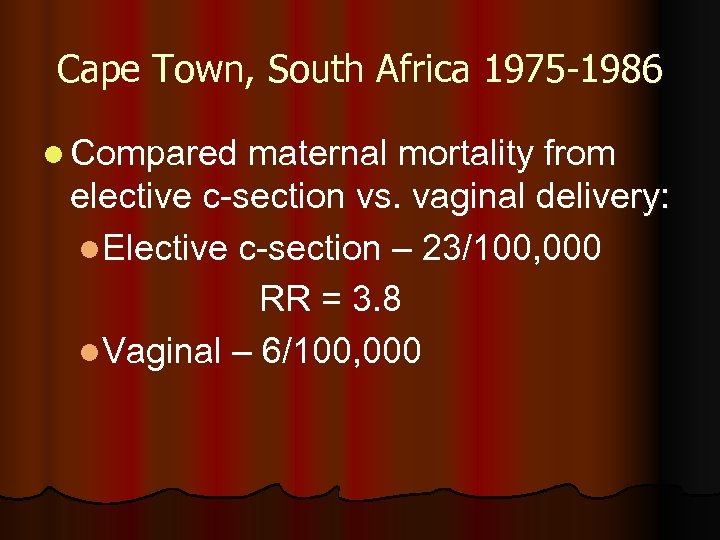 Cape Town, South Africa 1975 -1986 l Compared maternal mortality from elective c-section vs. vaginal delivery: l. Elective c-section – 23/100, 000 RR = 3. 8 l. Vaginal – 6/100, 000
Cape Town, South Africa 1975 -1986 l Compared maternal mortality from elective c-section vs. vaginal delivery: l. Elective c-section – 23/100, 000 RR = 3. 8 l. Vaginal – 6/100, 000
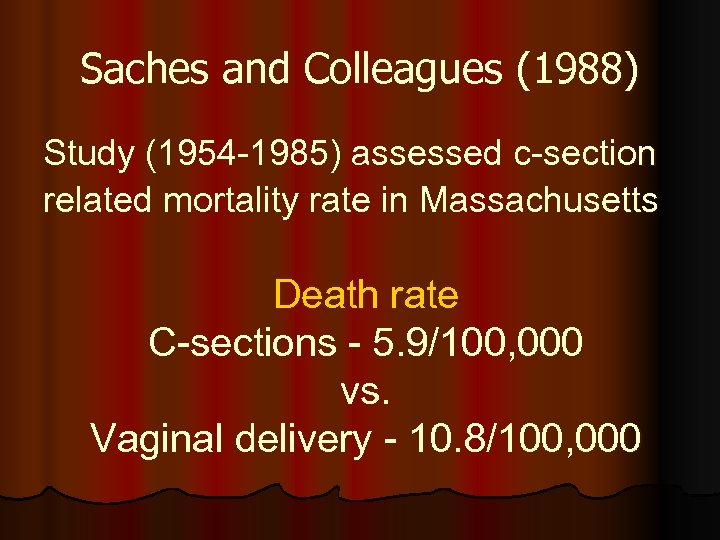 Saches and Colleagues (1988) Study (1954 -1985) assessed c-section related mortality rate in Massachusetts Death rate C-sections - 5. 9/100, 000 vs. Vaginal delivery - 10. 8/100, 000
Saches and Colleagues (1988) Study (1954 -1985) assessed c-section related mortality rate in Massachusetts Death rate C-sections - 5. 9/100, 000 vs. Vaginal delivery - 10. 8/100, 000
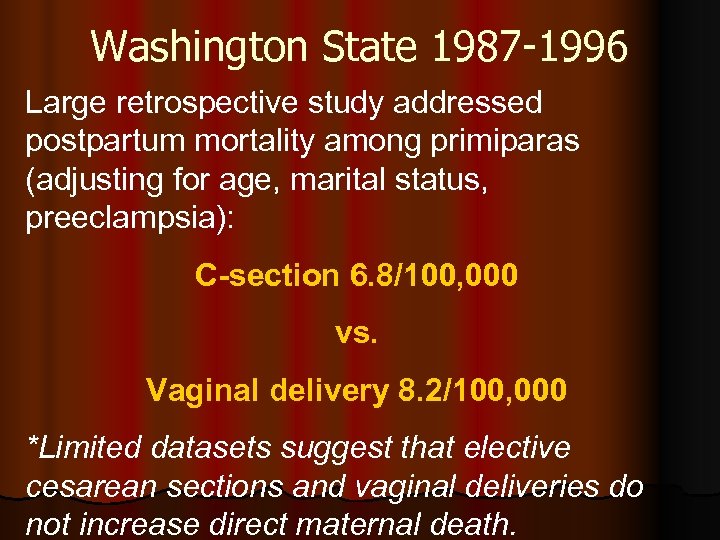 Washington State 1987 -1996 Large retrospective study addressed postpartum mortality among primiparas (adjusting for age, marital status, preeclampsia): C-section 6. 8/100, 000 vs. Vaginal delivery 8. 2/100, 000 *Limited datasets suggest that elective cesarean sections and vaginal deliveries do not increase direct maternal death.
Washington State 1987 -1996 Large retrospective study addressed postpartum mortality among primiparas (adjusting for age, marital status, preeclampsia): C-section 6. 8/100, 000 vs. Vaginal delivery 8. 2/100, 000 *Limited datasets suggest that elective cesarean sections and vaginal deliveries do not increase direct maternal death.
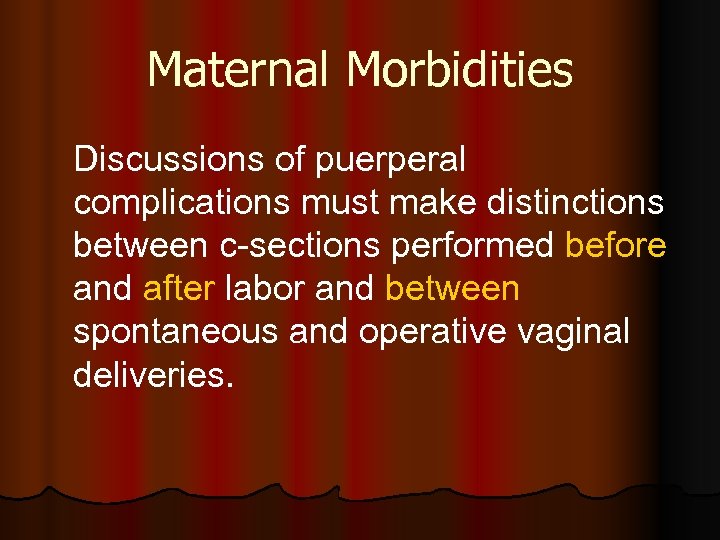 Maternal Morbidities Discussions of puerperal complications must make distinctions between c-sections performed before and after labor and between spontaneous and operative vaginal deliveries.
Maternal Morbidities Discussions of puerperal complications must make distinctions between c-sections performed before and after labor and between spontaneous and operative vaginal deliveries.
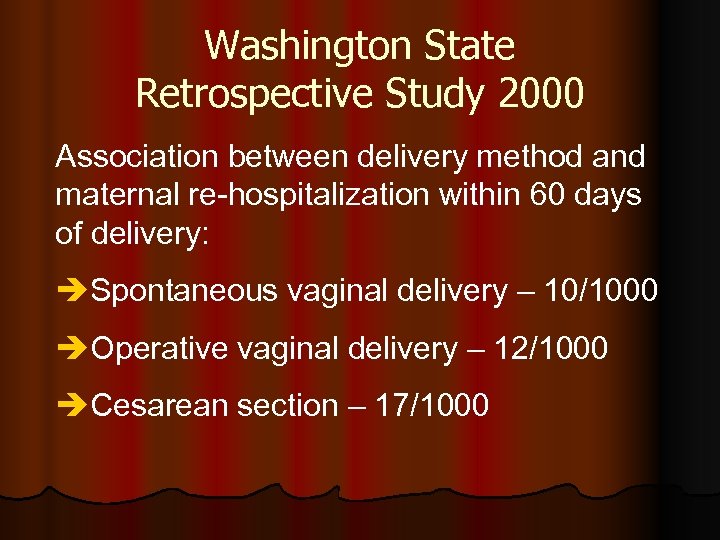 Washington State Retrospective Study 2000 Association between delivery method and maternal re-hospitalization within 60 days of delivery: èSpontaneous vaginal delivery – 10/1000 èOperative vaginal delivery – 12/1000 èCesarean section – 17/1000
Washington State Retrospective Study 2000 Association between delivery method and maternal re-hospitalization within 60 days of delivery: èSpontaneous vaginal delivery – 10/1000 èOperative vaginal delivery – 12/1000 èCesarean section – 17/1000
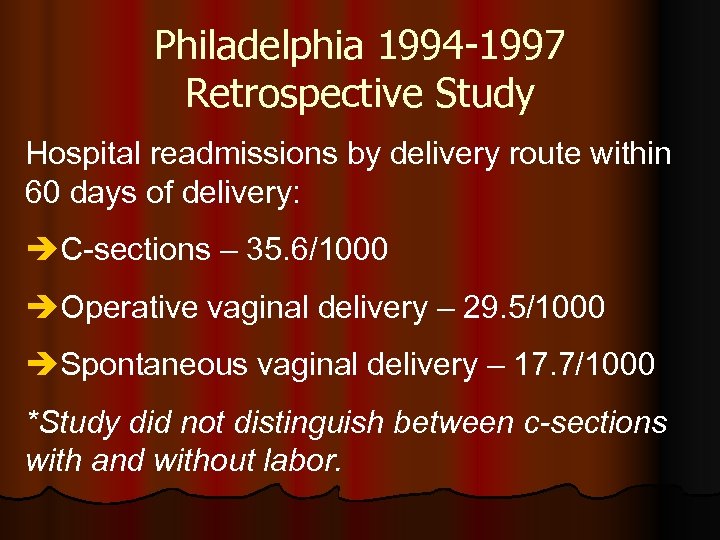 Philadelphia 1994 -1997 Retrospective Study Hospital readmissions by delivery route within 60 days of delivery: èC-sections – 35. 6/1000 èOperative vaginal delivery – 29. 5/1000 èSpontaneous vaginal delivery – 17. 7/1000 *Study did not distinguish between c-sections with and without labor.
Philadelphia 1994 -1997 Retrospective Study Hospital readmissions by delivery route within 60 days of delivery: èC-sections – 35. 6/1000 èOperative vaginal delivery – 29. 5/1000 èSpontaneous vaginal delivery – 17. 7/1000 *Study did not distinguish between c-sections with and without labor.
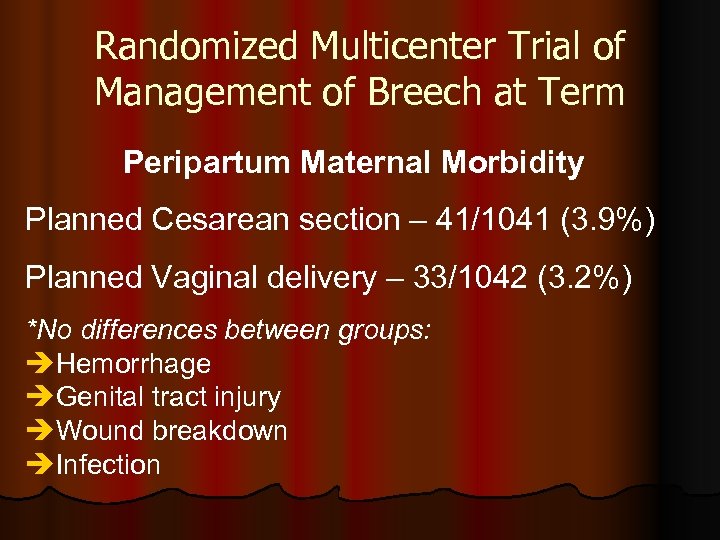 Randomized Multicenter Trial of Management of Breech at Term Peripartum Maternal Morbidity Planned Cesarean section – 41/1041 (3. 9%) Planned Vaginal delivery – 33/1042 (3. 2%) *No differences between groups: èHemorrhage èGenital tract injury èWound breakdown èInfection
Randomized Multicenter Trial of Management of Breech at Term Peripartum Maternal Morbidity Planned Cesarean section – 41/1041 (3. 9%) Planned Vaginal delivery – 33/1042 (3. 2%) *No differences between groups: èHemorrhage èGenital tract injury èWound breakdown èInfection
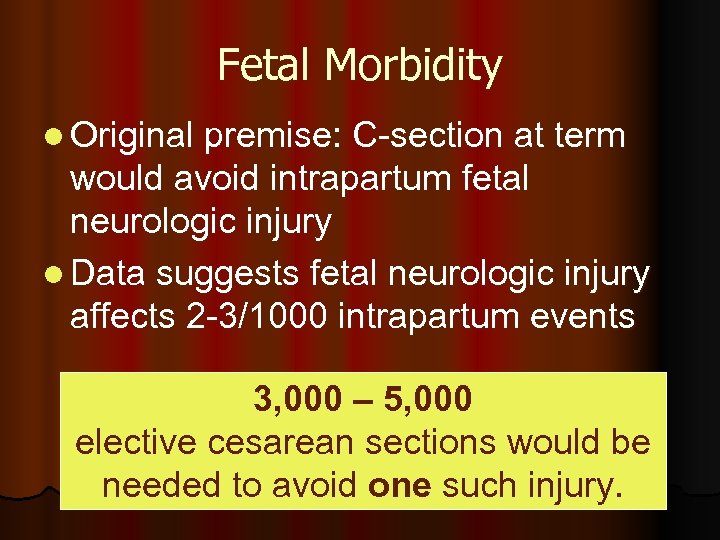 Fetal Morbidity l Original premise: C-section at term would avoid intrapartum fetal neurologic injury l Data suggests fetal neurologic injury affects 2 -3/1000 intrapartum events 3, 000 – 5, 000 elective cesarean sections would be needed to avoid one such injury.
Fetal Morbidity l Original premise: C-section at term would avoid intrapartum fetal neurologic injury l Data suggests fetal neurologic injury affects 2 -3/1000 intrapartum events 3, 000 – 5, 000 elective cesarean sections would be needed to avoid one such injury.
 C-section Rate (mid 1970’s – present) Pooled data from these countries have shown significant rise of c-section rates: Sweden Canada England Ireland Australia Denmark Norway U. S. è Cerebral palsy rates have remained stable internationally è C-section is not neuroprotective for the fetus
C-section Rate (mid 1970’s – present) Pooled data from these countries have shown significant rise of c-section rates: Sweden Canada England Ireland Australia Denmark Norway U. S. è Cerebral palsy rates have remained stable internationally è C-section is not neuroprotective for the fetus
 Birth Injury Available data suggests that “pre-labor” cesarean section does not offer a clear fetal benefit with respect to intracranial, brachial plexus, or fracture injury. May increase the risk of laceration injury in the infant.
Birth Injury Available data suggests that “pre-labor” cesarean section does not offer a clear fetal benefit with respect to intracranial, brachial plexus, or fracture injury. May increase the risk of laceration injury in the infant.
 Conclusion l The debate over elective c-sections is growing. l Obstetrician should be aware of the issues and their colleagues’ beliefs. l No adequate study has compared elective c-sections and planned SVD. l In the absence of data, professional organizations will have different opinions on ethical acceptability.
Conclusion l The debate over elective c-sections is growing. l Obstetrician should be aware of the issues and their colleagues’ beliefs. l No adequate study has compared elective c-sections and planned SVD. l In the absence of data, professional organizations will have different opinions on ethical acceptability.
 Conclusion Available data, though not robust, suggests that overall maternal and perinatal mortality, short- and long-term maternal and neonatal morbidity favor a vaginal delivery.
Conclusion Available data, though not robust, suggests that overall maternal and perinatal mortality, short- and long-term maternal and neonatal morbidity favor a vaginal delivery.