b06b4faefa190ab0511d4083573ad122.ppt
- Количество слайдов: 12
 Eastern Region Housing LIN Overview of the Care Bill Joanna David – Assistant Director Social Care Reform DH/LGA/ADASS Joint Programme Board March 25 th E-mail: Joanna. David@local. gov. uk
Eastern Region Housing LIN Overview of the Care Bill Joanna David – Assistant Director Social Care Reform DH/LGA/ADASS Joint Programme Board March 25 th E-mail: Joanna. David@local. gov. uk
 A critical time for local government • Wide ranging and significant piece of legislation - major opportunity to shape the long term future of adult social care • Core principles have strong sector and stakeholder support – prevention, early intervention, independence and well being • Very substantial change programme – integral links to the wider health and care reforms – BCF, Pioneers, Public Health
A critical time for local government • Wide ranging and significant piece of legislation - major opportunity to shape the long term future of adult social care • Core principles have strong sector and stakeholder support – prevention, early intervention, independence and well being • Very substantial change programme – integral links to the wider health and care reforms – BCF, Pioneers, Public Health
 Programme Board • Joint Programme Board - formal partnership between DH, LGA and ADASS to support implementation of Care Bill - innovative, collaborative - strong buy-in from all Partners • Spirit of engagement and co-production • Legislation that is being shaped in partnership between central and local government, providers and the third sector
Programme Board • Joint Programme Board - formal partnership between DH, LGA and ADASS to support implementation of Care Bill - innovative, collaborative - strong buy-in from all Partners • Spirit of engagement and co-production • Legislation that is being shaped in partnership between central and local government, providers and the third sector
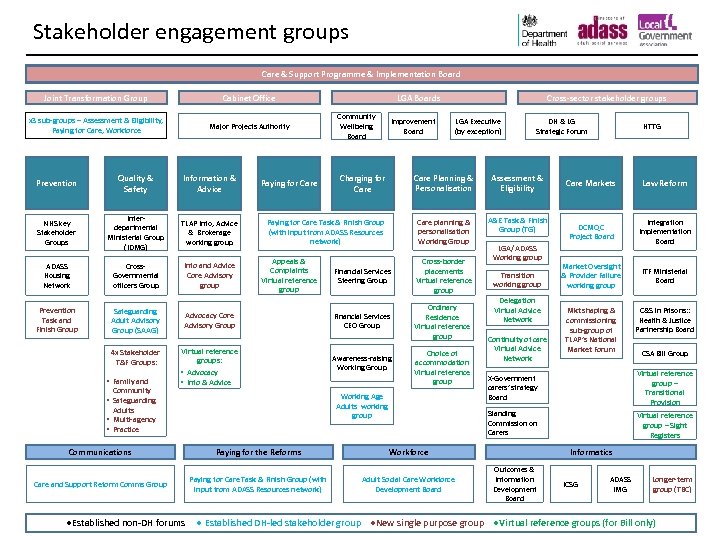 Stakeholder engagement groups Care & Support Programme & Implementation Board Joint Transformation Group Cabinet Office x 3 sub-groups – Assessment & Eligibility, Paying for Care, Workforce Major Projects Authority Prevention Quality & Safety Information & Advice NHS key Stakeholder Groups Interdepartmental Ministerial Group (IDMG) TLAP Info, Advice & Brokerage working group ADASS Housing Network Cross. Governmental officers Group Prevention Task and Finish Group Safeguarding Adult Advisory Group (SAAG) 4 x Stakeholder T&F Groups: • Family and Community Info and Advice Core Advisory group Paying for Care LGA Boards Community Wellbeing Board Improvement Board Advocacy Core Advisory Group Virtual reference groups: • Advocacy • Info & Advice Adults • Multi-agency • Practice DH & LG Strategic Forum Assessment & Eligibility Care planning & personalisation Working Group A&E Task & Finish Group (TG) Financial Services Steering Group Cross-border placements Virtual reference group Financial Services CEO Group Ordinary Residence Virtual reference group Awareness-raising Working Group Choice of accommodation Virtual reference group LGA/ADASS Working group Transition working group Delegation Virtual Advice Network Continuity of care Virtual Advice Network Communications Paying for the Reforms Care Markets Law Reform DCMQC Project Board Integration Implementation Board Market Oversight & Provider Failure working group ITF Ministerial Board Mkt shaping & commissioning sub-group of TLAP’s National Market Forum C&S in Prisons: : Health & Justice Partnership Board CSA Bill Group Care and Support Reform Comms Group Paying for Care Task & Finish Group (with input from ADASS Resources network) Adult Social Care Workforce Development Board X-Government carers’ strategy Board Virtual reference group – Transitional Provision Virtual reference group – Sight Registers Workforce ●Established non-DH forums HTTG Standing Commission on Carers Working Age Adults working group • Safeguarding LGA Executive (by exception) Care Planning & Personalisation Charging for Care Paying for Care Task & Finish Group (with input from ADASS Resources network) Appeals & Complaints Virtual reference group Cross-sector stakeholder groups Informatics Outcomes & Information Development Board ICSG ADASS IMG Longer-term group (TBC) ● Established DH-led stakeholder group ●New single purpose group ●Virtual reference groups (for Bill only)
Stakeholder engagement groups Care & Support Programme & Implementation Board Joint Transformation Group Cabinet Office x 3 sub-groups – Assessment & Eligibility, Paying for Care, Workforce Major Projects Authority Prevention Quality & Safety Information & Advice NHS key Stakeholder Groups Interdepartmental Ministerial Group (IDMG) TLAP Info, Advice & Brokerage working group ADASS Housing Network Cross. Governmental officers Group Prevention Task and Finish Group Safeguarding Adult Advisory Group (SAAG) 4 x Stakeholder T&F Groups: • Family and Community Info and Advice Core Advisory group Paying for Care LGA Boards Community Wellbeing Board Improvement Board Advocacy Core Advisory Group Virtual reference groups: • Advocacy • Info & Advice Adults • Multi-agency • Practice DH & LG Strategic Forum Assessment & Eligibility Care planning & personalisation Working Group A&E Task & Finish Group (TG) Financial Services Steering Group Cross-border placements Virtual reference group Financial Services CEO Group Ordinary Residence Virtual reference group Awareness-raising Working Group Choice of accommodation Virtual reference group LGA/ADASS Working group Transition working group Delegation Virtual Advice Network Continuity of care Virtual Advice Network Communications Paying for the Reforms Care Markets Law Reform DCMQC Project Board Integration Implementation Board Market Oversight & Provider Failure working group ITF Ministerial Board Mkt shaping & commissioning sub-group of TLAP’s National Market Forum C&S in Prisons: : Health & Justice Partnership Board CSA Bill Group Care and Support Reform Comms Group Paying for Care Task & Finish Group (with input from ADASS Resources network) Adult Social Care Workforce Development Board X-Government carers’ strategy Board Virtual reference group – Transitional Provision Virtual reference group – Sight Registers Workforce ●Established non-DH forums HTTG Standing Commission on Carers Working Age Adults working group • Safeguarding LGA Executive (by exception) Care Planning & Personalisation Charging for Care Paying for Care Task & Finish Group (with input from ADASS Resources network) Appeals & Complaints Virtual reference group Cross-sector stakeholder groups Informatics Outcomes & Information Development Board ICSG ADASS IMG Longer-term group (TBC) ● Established DH-led stakeholder group ●New single purpose group ●Virtual reference groups (for Bill only)
 Key areas of change – Part 1 • National eligibility threshold • Legal right to a personal budget • Carers to have the same rights as those they care for • New duty to prevent / delay the need for care • New duty to provide information and advice to all residents – not just those receiving care
Key areas of change – Part 1 • National eligibility threshold • Legal right to a personal budget • Carers to have the same rights as those they care for • New duty to prevent / delay the need for care • New duty to provide information and advice to all residents – not just those receiving care
 Changes Part 1 • Duty on councils to join up care and support with health and housing where this delivers better care and promotes well being • Duty on councils to ensure there is a wide range of care and support services available that enable local people to choose the care and support services they want (market shaping)
Changes Part 1 • Duty on councils to join up care and support with health and housing where this delivers better care and promotes well being • Duty on councils to ensure there is a wide range of care and support services available that enable local people to choose the care and support services they want (market shaping)
 Key changes Part 2 – funding reform • Financial protection - everyone will know the maximum they will pay towards the cost of meeting their eligible care needs • People will be protected from having to sell their home in their lifetime to pay for any care home costs • People will be helped to take responsibility for planning and preparing for their care needs in later life
Key changes Part 2 – funding reform • Financial protection - everyone will know the maximum they will pay towards the cost of meeting their eligible care needs • People will be protected from having to sell their home in their lifetime to pay for any care home costs • People will be helped to take responsibility for planning and preparing for their care needs in later life
 Key changes – Part 2 • Cap on costs of meting eligible care needs – to be set at £ 72 k when it is introduced (adjusted annually) • No contribution expected for young people entering adulthood with an eligible care need • Lower cap for adults of working age (level to be determined) • Increase in capital thresholds /extension to the means test providing more support to people with modest wealth • New legal basis for charging covering both residential and non-residential care • Introduction of flat rate contribution towards living costs for people in residential care
Key changes – Part 2 • Cap on costs of meting eligible care needs – to be set at £ 72 k when it is introduced (adjusted annually) • No contribution expected for young people entering adulthood with an eligible care need • Lower cap for adults of working age (level to be determined) • Increase in capital thresholds /extension to the means test providing more support to people with modest wealth • New legal basis for charging covering both residential and non-residential care • Introduction of flat rate contribution towards living costs for people in residential care
 The legislative timetable • The Bill has now had its 3 rd reading in the Commons – Royal Assent expected mid May • Regulations and guidance due to be published mid May – up to 12 weeks consultation • Finalised secondary legislation October 2014 • Part 1 implementation – April 2015 • Part 2 – April 16
The legislative timetable • The Bill has now had its 3 rd reading in the Commons – Royal Assent expected mid May • Regulations and guidance due to be published mid May – up to 12 weeks consultation • Finalised secondary legislation October 2014 • Part 1 implementation – April 2015 • Part 2 – April 16
 Critical areas for implementation • Workforce – ensuring capacity and skills to deliver reforms • IT – care records, new charging, deferred payments • Advice and information - building a comprehensive and accessible service • Understanding how much it is going to cost – financial modelling for the cap plus implementation costs
Critical areas for implementation • Workforce – ensuring capacity and skills to deliver reforms • IT – care records, new charging, deferred payments • Advice and information - building a comprehensive and accessible service • Understanding how much it is going to cost – financial modelling for the cap plus implementation costs
 Building capacity • DH investment in regional structures - seen as pivotal to drive preparation for implementation • Sharing good practice, knowledge and learning – avoiding duplication • Focal point for communication – understanding obstacles, managing risks – surfacing wicked issues
Building capacity • DH investment in regional structures - seen as pivotal to drive preparation for implementation • Sharing good practice, knowledge and learning – avoiding duplication • Focal point for communication – understanding obstacles, managing risks – surfacing wicked issues
 Key risks that are emerging • Still a significant number of policy ‘unknowns’ – working age cap, national eligibility threshold • Uncertainty about total costs of implementation • Context of spending review • State of readiness in adult social care – scale of change
Key risks that are emerging • Still a significant number of policy ‘unknowns’ – working age cap, national eligibility threshold • Uncertainty about total costs of implementation • Context of spending review • State of readiness in adult social care – scale of change


