8f0409f6ef199f46e1124aaa0ad48bb8.ppt
- Количество слайдов: 32
e. Prescribing at University Hospitals Birmingham NHS Foundation Trust Ann Slee Director of Pharmacy ann. slee@uhb. nhs. uk
Presentation Outline • • The system System functionality Benefits Ongoing work
The System • Developed by Wolfson Computer Lab ▪ Unit within University Hospital, Birmingham • Continuous development for over 10 years ▪ Always in conjunction with UHB clinical staff • Core design, development, implementation, 7 staff • Currently 12 staff in PICS team
Prescribing Information Communication System
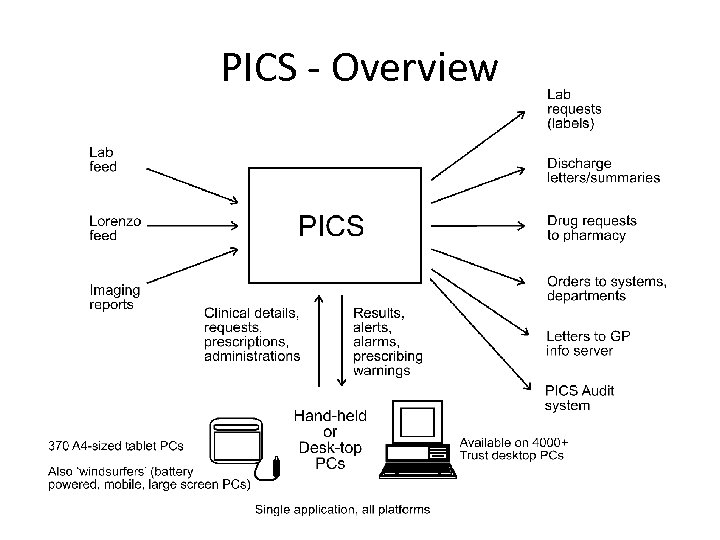
PICS - Overview
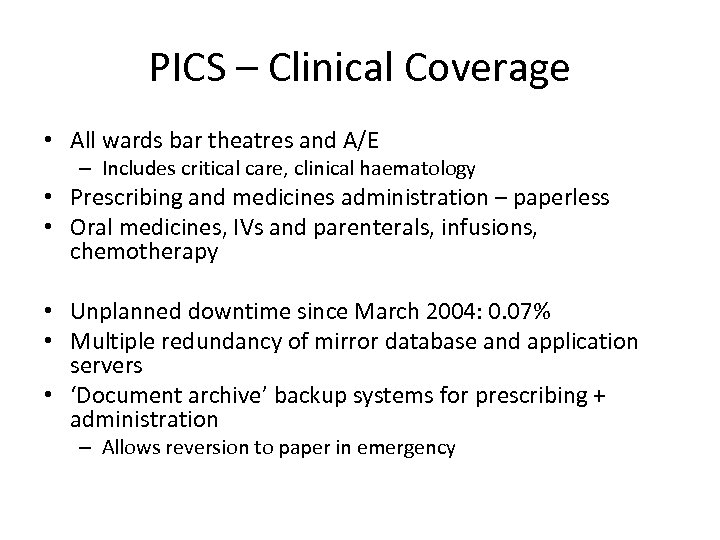
PICS – Clinical Coverage • All wards bar theatres and A/E – Includes critical care, clinical haematology • Prescribing and medicines administration – paperless • Oral medicines, IVs and parenterals, infusions, chemotherapy • Unplanned downtime since March 2004: 0. 07% • Multiple redundancy of mirror database and application servers • ‘Document archive’ backup systems for prescribing + administration – Allows reversion to paper in emergency
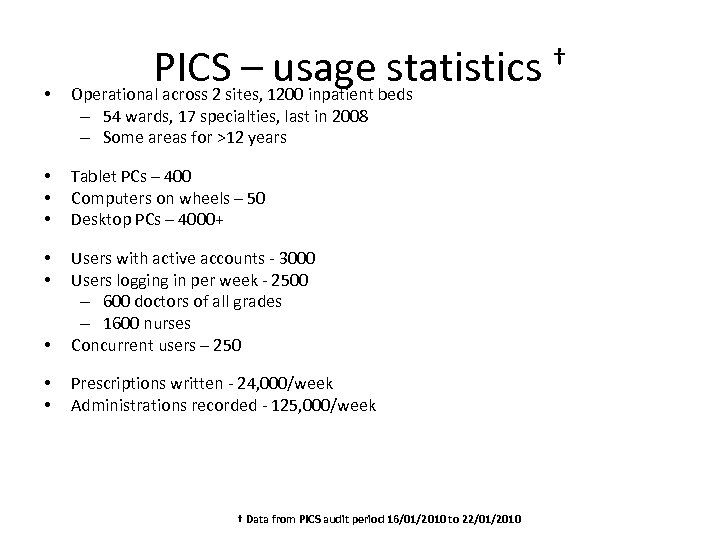
• PICSsites, 1200 inpatient beds – usage statistics † Operational across 2 – 54 wards, 17 specialties, last in 2008 – Some areas for >12 years • • • Tablet PCs – 400 Computers on wheels – 50 Desktop PCs – 4000+ • • • Users with active accounts - 3000 Users logging in per week - 2500 – 600 doctors of all grades – 1600 nurses Concurrent users – 250 • • Prescriptions written - 24, 000/week Administrations recorded - 125, 000/week † Data from PICS audit period 16/01/2010 to 22/01/2010
Presentation Outline • • The system System functionality Benefits Ongoing work
• • • Rules-based clinical management system, configurable by specialty, allowing: ‘Paperless’ management of drug therapy/protocols • In-built real-time checks on drugs, dosages, contra-indications, interactions, etc. Results reporting Automated lab requesting Real-time, event driven alerts Clinical procedures Discharge letters/summaries Order communications Clinical observations Bed state, dependencies, estimated length of stay
Complex rules § Alerts or alarms (rule specifies those groups that can see and can acknowledge) § Abnormal result levels or rates of change § Suggested drug script changes, as a result of: § new results § new clinical information § duration of script, etc. § Reminders, warnings, information, etc. : § arrival of certain report types (e. g. imaging, microbiology) § review of sedation levels § preferred route for drug administration § entry of sedation/ventilation data § suspect on-line blood gas data § compliance with thrombosis guidance
Complex rules cont. (Single rule can generate several actions) § Laboratory investigation proposals, based on: § Clinical classifications § Current drug therapy § Previous results § Inpatient/outpatient status § Drug proposals, e. g. : § On admission scripts § Post-op drugs § Antimicrobial protocols § Drug prescriptions - MRSA protocol
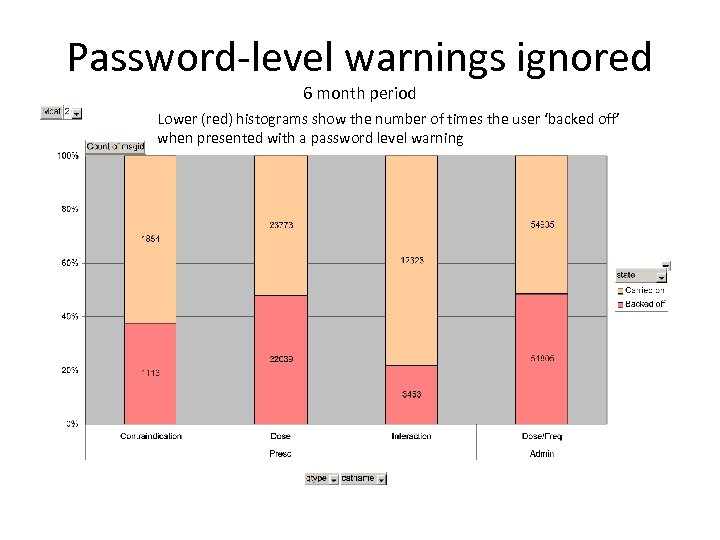
Password-level warnings ignored 6 month period Lower (red) histograms show the number of times the user ‘backed off’ when presented with a password level warning
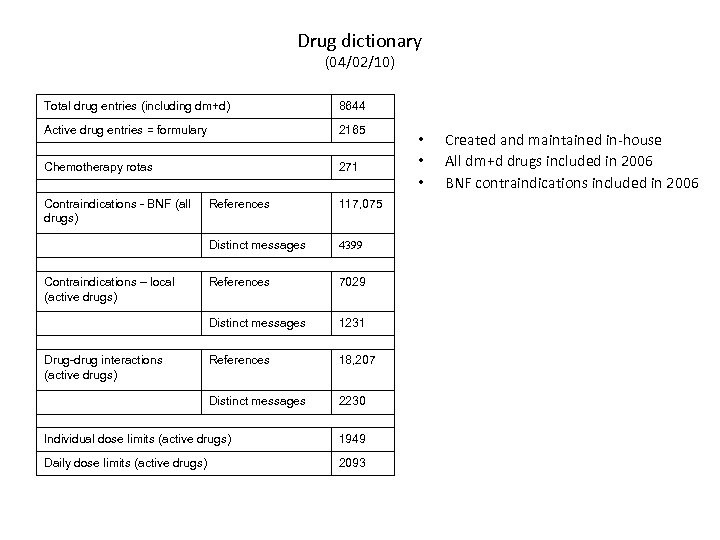
Drug dictionary (04/02/10) Total drug entries (including dm+d) 8644 Active drug entries = formulary 2165 Chemotherapy rotas 271 Contraindications - BNF (all drugs) 4399 References 7029 Distinct messages 1231 References 18, 207 Distinct messages Drug-drug interactions (active drugs) 117, 075 Distinct messages Contraindications – local (active drugs) References 2230 Individual dose limits (active drugs) 1949 Daily dose limits (active drugs) 2093 • • • Created and maintained in-house All dm+d drugs included in 2006 BNF contraindications included in 2006
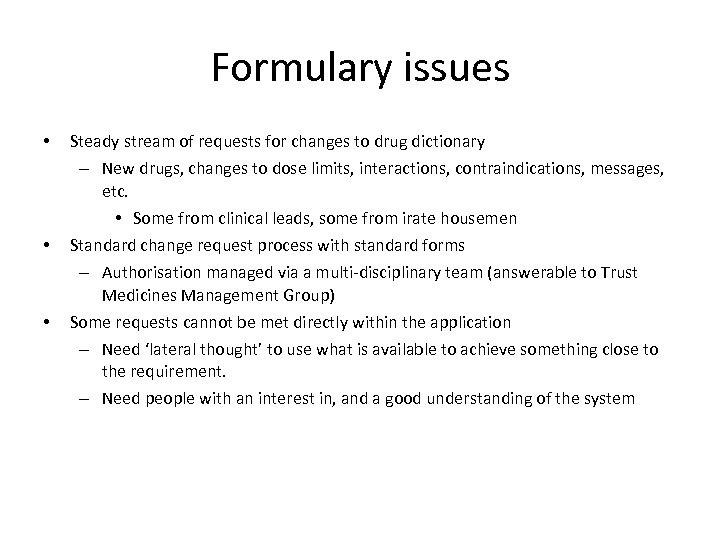
Formulary issues • • • Steady stream of requests for changes to drug dictionary – New drugs, changes to dose limits, interactions, contraindications, messages, etc. • Some from clinical leads, some from irate housemen Standard change request process with standard forms – Authorisation managed via a multi-disciplinary team (answerable to Trust Medicines Management Group) Some requests cannot be met directly within the application – Need ‘lateral thought’ to use what is available to achieve something close to the requirement. – Need people with an interest in, and a good understanding of the system
Presentation Outline • • The system System functionality Benefits Ongoing work
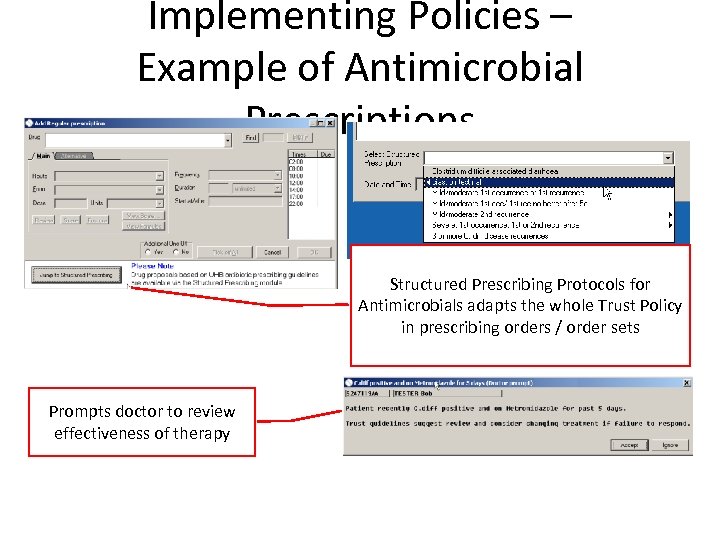
Implementing Policies – Example of Antimicrobial Prescriptions Structured Prescribing Protocols for Antimicrobials adapts the whole Trust Policy in prescribing orders / order sets Prompts doctor to review effectiveness of therapy
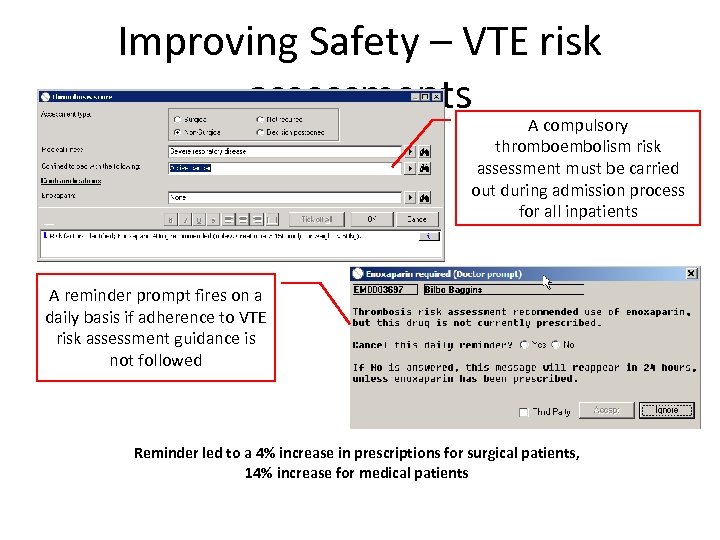
Improving Safety – VTE risk assessments A compulsory thromboembolism risk assessment must be carried out during admission process for all inpatients A reminder prompt fires on a daily basis if adherence to VTE risk assessment guidance is not followed Reminder led to a 4% increase in prescriptions for surgical patients, 14% increase for medical patients
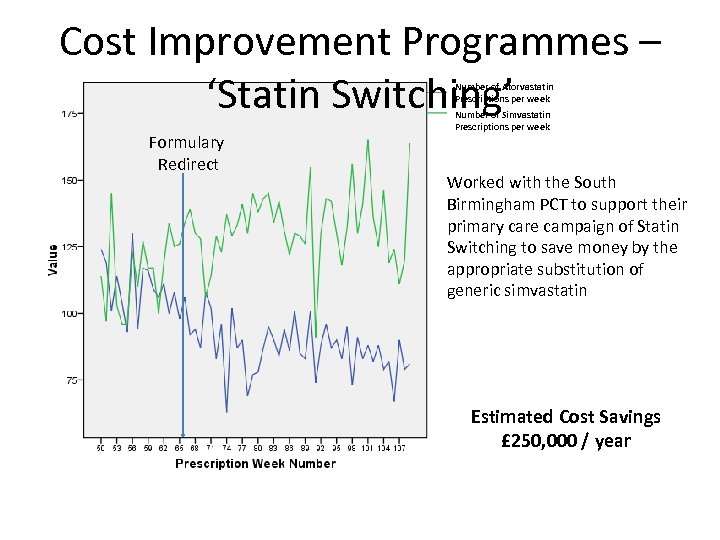
Cost Improvement Programmes – ‘Statin Switching’ Number of Atorvastatin Prescriptions per week Formulary Redirect Number of Simvastatin Prescriptions per week Worked with the South Birmingham PCT to support their primary care campaign of Statin Switching to save money by the appropriate substitution of generic simvastatin Estimated Cost Savings £ 250, 000 / year
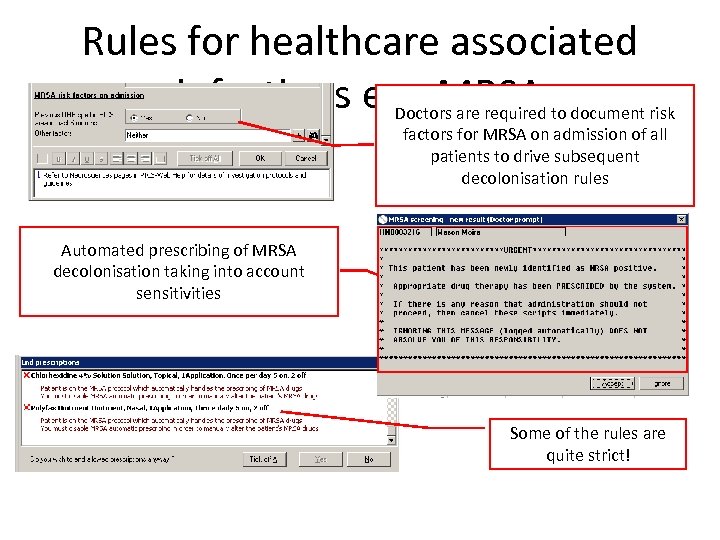
Rules for healthcare associated infections e. g. MRSA to document risk Doctors are required factors for MRSA on admission of all patients to drive subsequent decolonisation rules Automated prescribing of MRSA decolonisation taking into account sensitivities Some of the rules are quite strict!
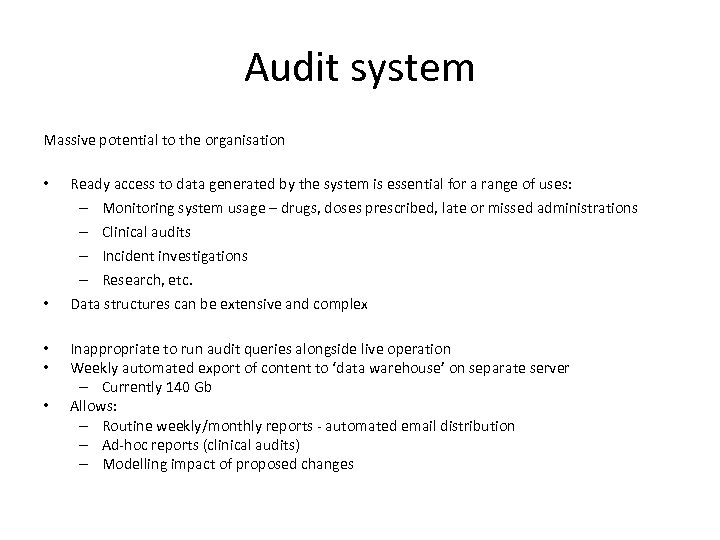
Audit system Massive potential to the organisation • • • Ready access to data generated by the system is essential for a range of uses: – Monitoring system usage – drugs, doses prescribed, late or missed administrations – Clinical audits – Incident investigations – Research, etc. Data structures can be extensive and complex Inappropriate to run audit queries alongside live operation Weekly automated export of content to ‘data warehouse’ on separate server – Currently 140 Gb Allows: – Routine weekly/monthly reports - automated email distribution – Ad-hoc reports (clinical audits) – Modelling impact of proposed changes
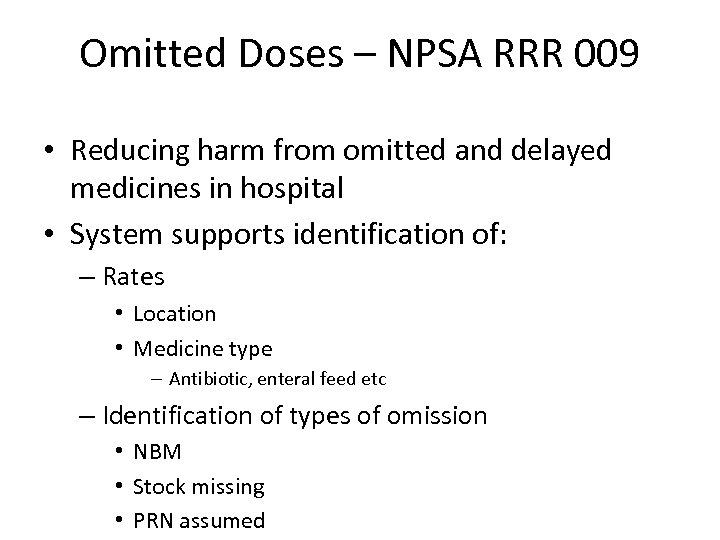
Omitted Doses – NPSA RRR 009 • Reducing harm from omitted and delayed medicines in hospital • System supports identification of: – Rates • Location • Medicine type – Antibiotic, enteral feed etc – Identification of types of omission • NBM • Stock missing • PRN assumed
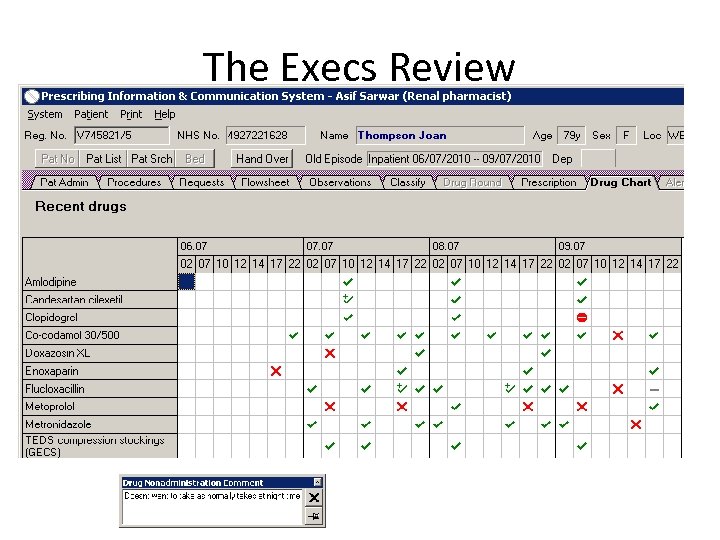
The Execs Review
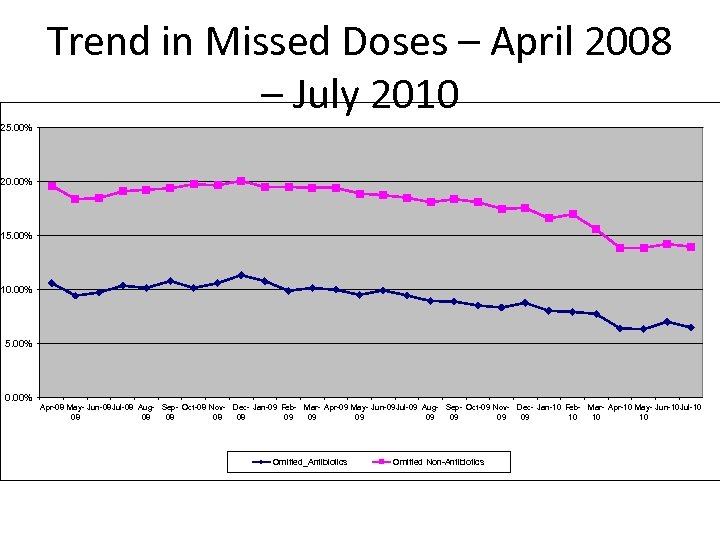
Trend in Missed Doses – April 2008 – July 2010 25. 00% 20. 00% 15. 00% 10. 00% 5. 00% 0. 00% Apr-08 May- Jun-08 Jul-08 Aug- Sep- Oct-08 Nov- Dec- Jan-09 Feb- Mar- Apr-09 May- Jun-09 Jul-09 Aug- Sep- Oct-09 Nov- Dec- Jan-10 Feb- Mar- Apr-10 May- Jun-10 Jul-10 08 08 08 09 09 10 10 10 Omitted_Antibiotics Omitted Non-Antibiotics
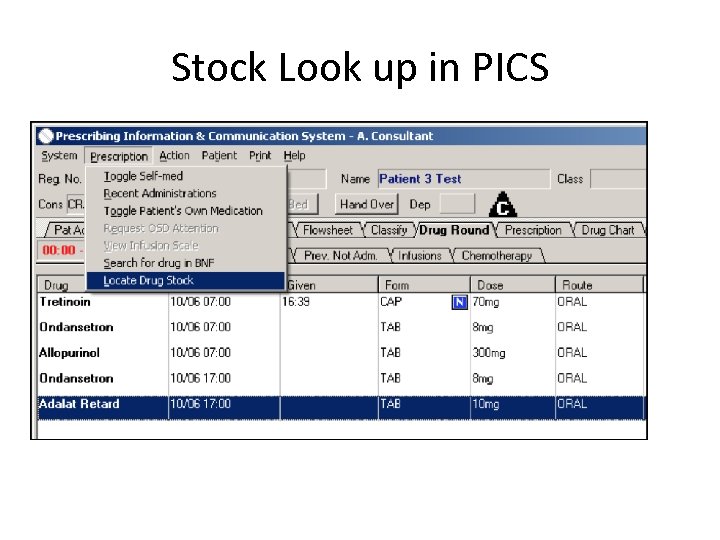
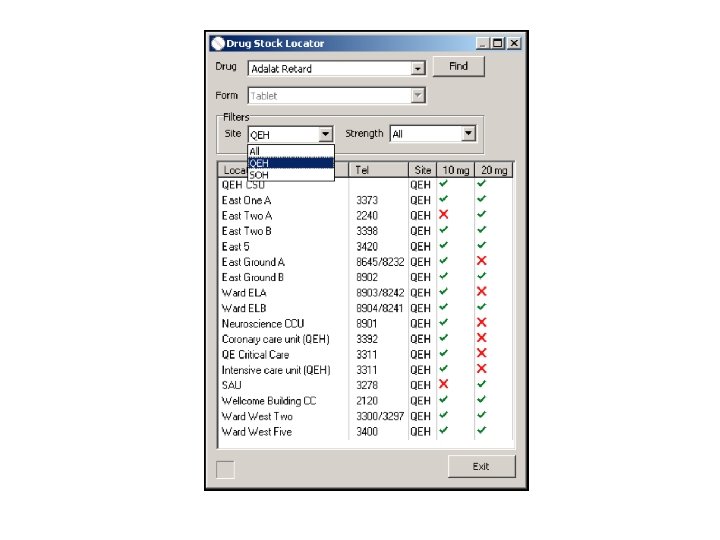
Stock Look up in PICS
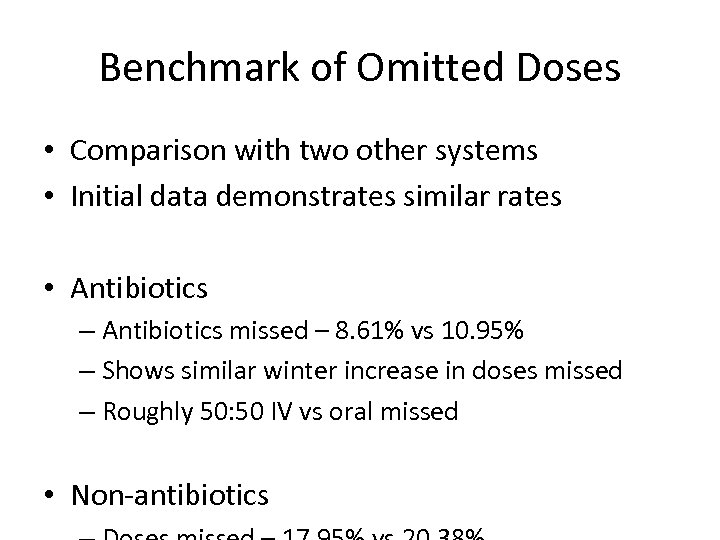
Benchmark of Omitted Doses • Comparison with two other systems • Initial data demonstrates similar rates • Antibiotics – Antibiotics missed – 8. 61% vs 10. 95% – Shows similar winter increase in doses missed – Roughly 50: 50 IV vs oral missed • Non-antibiotics
Presentation Outline • • The system System functionality Benefits Ongoing work
Ongoing Work • Increased use of data – for example – DDDs for antibiotics – NPSA warfarin requirements • Counselling • Monitoring Rx verification • Renal injury
Ongoing Work – Functionality • • • Outpatients Anaesthetics A&E Handover Clinical pharmacy support Recording of ward based testing Formulary support Indication driven Rx and increased use of order sets Rules development
Ongoing Work • System being marketed - CSE – UK specific functionality – UK specific rules and policy interpretation • Ongoing benchmarking – Cleveland clinic – Other English Trusts with systems • Research to demonstrate benefits
Summary - Benefits to the Organisation • Generic Learning – System Longevity and Systematic Implementation means already learned the lessons other Trusts still have to face – Clinical Decision Support requires extensive clinical backing • Improving Quality – Many wider benefits to the Trust beyond paperless prescribing – e. g. VTE Assessment, Infection Control, Indicators, Cost Improvement Programmes, • Integration is key – Using PICS as clinical cornerstone – can ‘connect rather than replace’ – Enhancing and continuing to build informatics capability
8f0409f6ef199f46e1124aaa0ad48bb8.ppt