a22cf9ad0f802736e68a98a70a1ef71b.ppt
- Количество слайдов: 93
 E LNE C End-of-Life Nursing Education Consortium International Curriculum Pain Management In Palliative Care
E LNE C End-of-Life Nursing Education Consortium International Curriculum Pain Management In Palliative Care
 Pain Is. . . • “An unpleasant sensory and emotional experience associated with actual or potential tissue damage” IASP, 1979 • “What the person says it is…” Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 2
Pain Is. . . • “An unpleasant sensory and emotional experience associated with actual or potential tissue damage” IASP, 1979 • “What the person says it is…” Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 2
 Current Status of Pain • Cancer patients at end-of-life – 54% have pain • AIDS with prognosis <6 months – intense pain APS, 2008; Paice, 2010 E L N E C International Curriculum 3
Current Status of Pain • Cancer patients at end-of-life – 54% have pain • AIDS with prognosis <6 months – intense pain APS, 2008; Paice, 2010 E L N E C International Curriculum 3
 Current Status of Pain (cont. ) • Less research conducted in other chronic illness • Inadequate pain relief hastens death • Pain relief is essential at end of life E L N E C International Curriculum 4
Current Status of Pain (cont. ) • Less research conducted in other chronic illness • Inadequate pain relief hastens death • Pain relief is essential at end of life E L N E C International Curriculum 4
 Pain An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. International Association for the Study of Pain E L N E C International Curriculum
Pain An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. International Association for the Study of Pain E L N E C International Curriculum
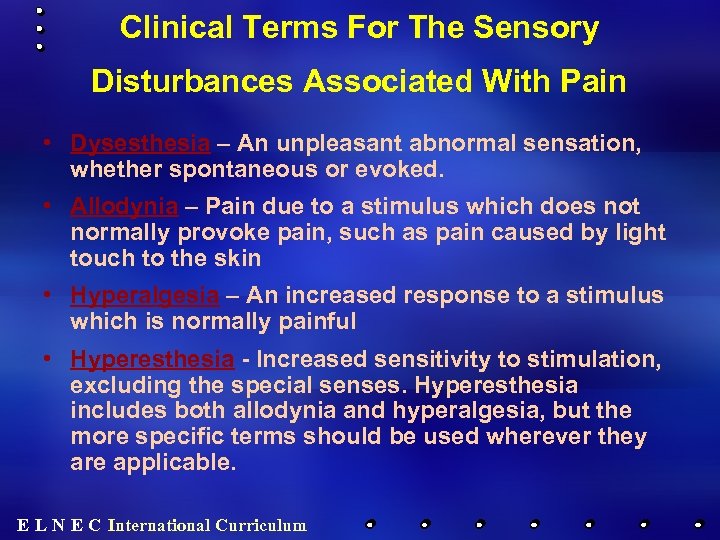 Clinical Terms For The Sensory Disturbances Associated With Pain • Dysesthesia – An unpleasant abnormal sensation, whether spontaneous or evoked. • Allodynia – Pain due to a stimulus which does not normally provoke pain, such as pain caused by light touch to the skin • Hyperalgesia – An increased response to a stimulus which is normally painful • Hyperesthesia - Increased sensitivity to stimulation, excluding the special senses. Hyperesthesia includes both allodynia and hyperalgesia, but the more specific terms should be used wherever they are applicable. E L N E C International Curriculum
Clinical Terms For The Sensory Disturbances Associated With Pain • Dysesthesia – An unpleasant abnormal sensation, whether spontaneous or evoked. • Allodynia – Pain due to a stimulus which does not normally provoke pain, such as pain caused by light touch to the skin • Hyperalgesia – An increased response to a stimulus which is normally painful • Hyperesthesia - Increased sensitivity to stimulation, excluding the special senses. Hyperesthesia includes both allodynia and hyperalgesia, but the more specific terms should be used wherever they are applicable. E L N E C International Curriculum
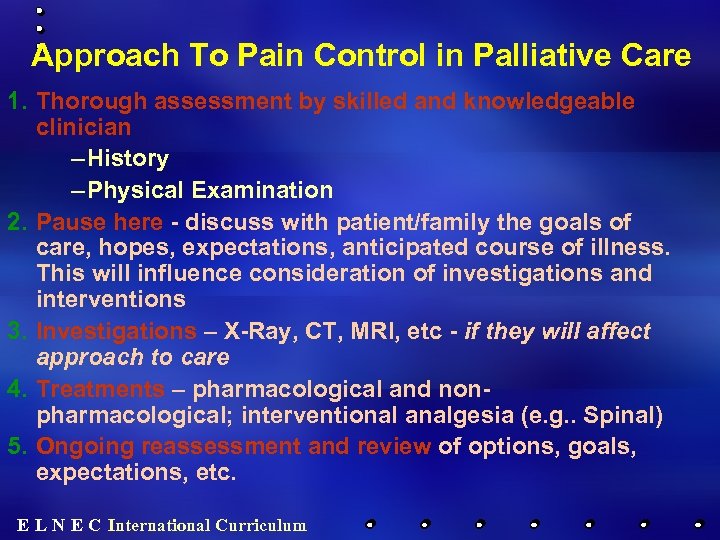 Approach To Pain Control in Palliative Care 1. Thorough assessment by skilled and knowledgeable clinician – History – Physical Examination 2. Pause here - discuss with patient/family the goals of care, hopes, expectations, anticipated course of illness. This will influence consideration of investigations and interventions 3. Investigations – X-Ray, CT, MRI, etc - if they will affect approach to care 4. Treatments – pharmacological and nonpharmacological; interventional analgesia (e. g. . Spinal) 5. Ongoing reassessment and review of options, goals, expectations, etc. E L N E C International Curriculum
Approach To Pain Control in Palliative Care 1. Thorough assessment by skilled and knowledgeable clinician – History – Physical Examination 2. Pause here - discuss with patient/family the goals of care, hopes, expectations, anticipated course of illness. This will influence consideration of investigations and interventions 3. Investigations – X-Ray, CT, MRI, etc - if they will affect approach to care 4. Treatments – pharmacological and nonpharmacological; interventional analgesia (e. g. . Spinal) 5. Ongoing reassessment and review of options, goals, expectations, etc. E L N E C International Curriculum
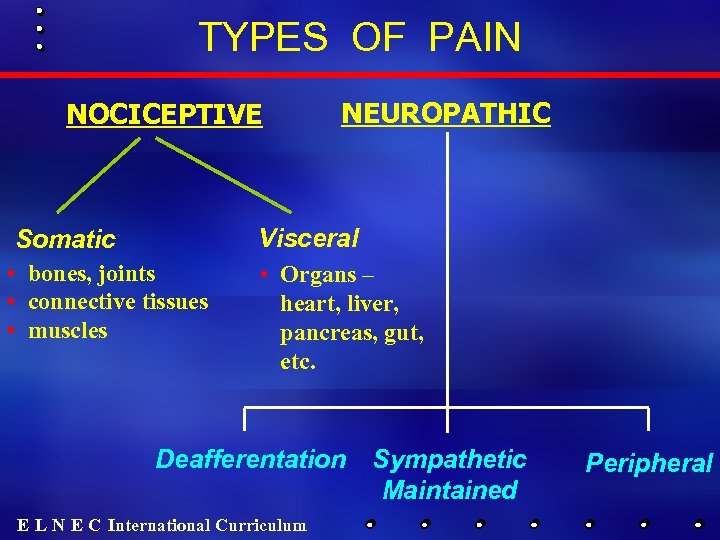 TYPES OF PAIN NOCICEPTIVE NEUROPATHIC Visceral Somatic • bones, joints • connective tissues • muscles • Organs – heart, liver, pancreas, gut, etc. Deafferentation E L N E C International Curriculum Sympathetic Maintained Peripheral
TYPES OF PAIN NOCICEPTIVE NEUROPATHIC Visceral Somatic • bones, joints • connective tissues • muscles • Organs – heart, liver, pancreas, gut, etc. Deafferentation E L N E C International Curriculum Sympathetic Maintained Peripheral
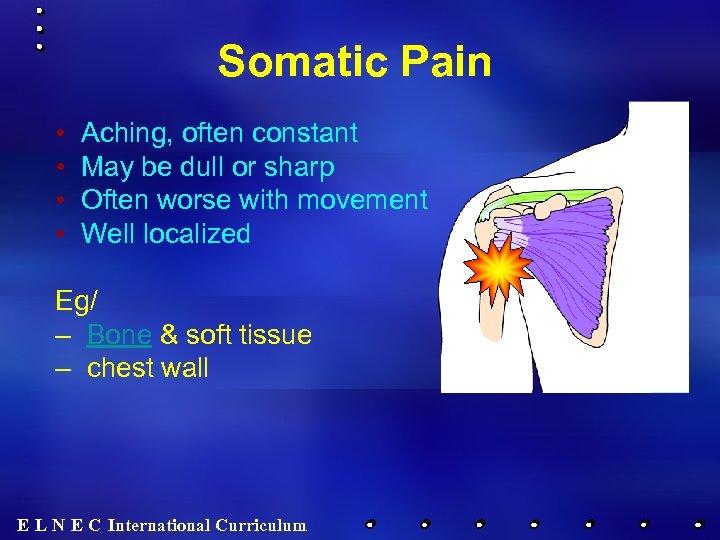 Somatic Pain • • Aching, often constant May be dull or sharp Often worse with movement Well localized Eg/ – Bone & soft tissue – chest wall E L N E C International Curriculum
Somatic Pain • • Aching, often constant May be dull or sharp Often worse with movement Well localized Eg/ – Bone & soft tissue – chest wall E L N E C International Curriculum
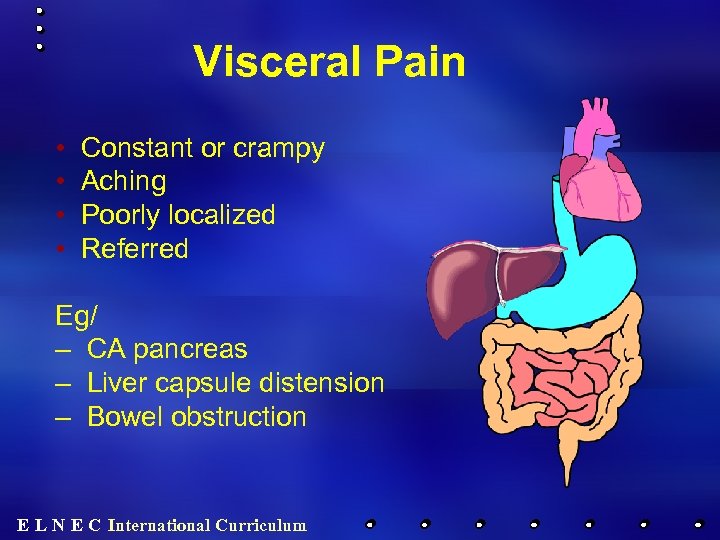 Visceral Pain • • Constant or crampy Aching Poorly localized Referred Eg/ – CA pancreas – Liver capsule distension – Bowel obstruction E L N E C International Curriculum
Visceral Pain • • Constant or crampy Aching Poorly localized Referred Eg/ – CA pancreas – Liver capsule distension – Bowel obstruction E L N E C International Curriculum
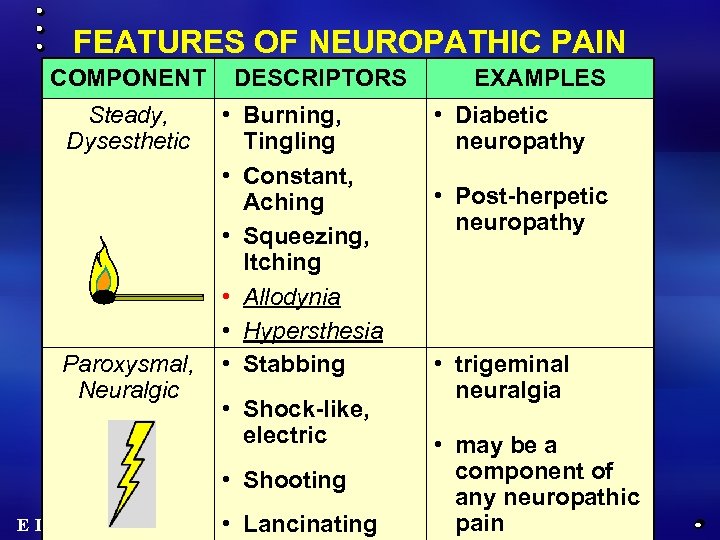 FEATURES OF NEUROPATHIC PAIN COMPONENT Steady, Dysesthetic Paroxysmal, Neuralgic DESCRIPTORS • Burning, Tingling • Constant, Aching • Squeezing, Itching • Allodynia • Hypersthesia • Stabbing • Shock-like, electric • Shooting E L N E C International Curriculum • Lancinating EXAMPLES • Diabetic neuropathy • Post-herpetic neuropathy • trigeminal neuralgia • may be a component of any neuropathic pain
FEATURES OF NEUROPATHIC PAIN COMPONENT Steady, Dysesthetic Paroxysmal, Neuralgic DESCRIPTORS • Burning, Tingling • Constant, Aching • Squeezing, Itching • Allodynia • Hypersthesia • Stabbing • Shock-like, electric • Shooting E L N E C International Curriculum • Lancinating EXAMPLES • Diabetic neuropathy • Post-herpetic neuropathy • trigeminal neuralgia • may be a component of any neuropathic pain
 Pain Assessment E L N E C International Curriculum
Pain Assessment E L N E C International Curriculum
 “Describing pain only in terms of its intensity is like describing music only in terms of its loudness” von Baeyer CL; Pain Research and Management 11(3) 2006; p. 157 -162 E L N E C International Curriculum
“Describing pain only in terms of its intensity is like describing music only in terms of its loudness” von Baeyer CL; Pain Research and Management 11(3) 2006; p. 157 -162 E L N E C International Curriculum
 PAIN HISTORY • Description: severity, quality, location, temporal features, frequency, aggravating & alleviating factors • Previous history • Context: social, cultural, emotional, spiritual factors • Meaning • Interventions: what has been tried? E L N E C International Curriculum
PAIN HISTORY • Description: severity, quality, location, temporal features, frequency, aggravating & alleviating factors • Previous history • Context: social, cultural, emotional, spiritual factors • Meaning • Interventions: what has been tried? E L N E C International Curriculum
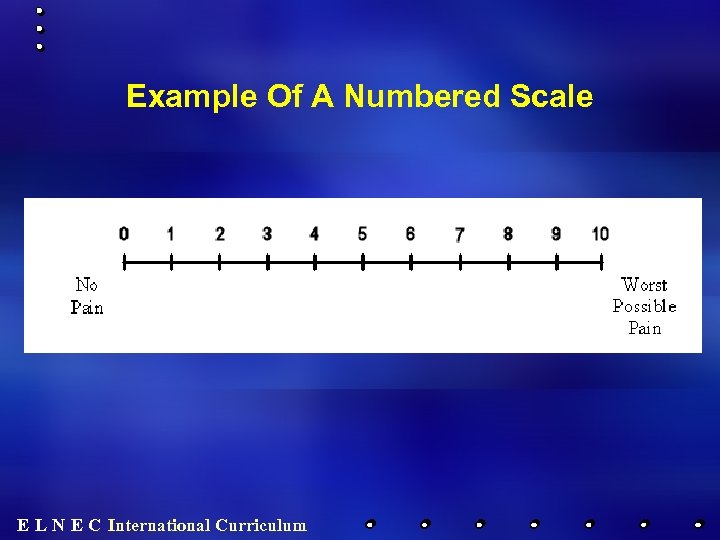 Example Of A Numbered Scale E L N E C International Curriculum
Example Of A Numbered Scale E L N E C International Curriculum
 Medication(s) Taken • • • Dose Route Frequency Duration Efficacy Adverse effects E L N E C International Curriculum
Medication(s) Taken • • • Dose Route Frequency Duration Efficacy Adverse effects E L N E C International Curriculum
 Physical Exam In Pain Assessment Inspection / Observation “You can observe a lot just by watching” • Overall impression… the “gestalt”? Yogi Berra • Facial expression: Grimacing; furrowed brow; appears anxious; flat affect • Body position and spontaneous movement: there may be positioning to protect painful areas, limited movement due to pain • Diaphoresis – can be caused by pain • Areas of redness, swelling • Atrophied muscles • Gait • Myoclonus – possibly indicating opioid-induced neurotoxicity E L N E C International Curriculum
Physical Exam In Pain Assessment Inspection / Observation “You can observe a lot just by watching” • Overall impression… the “gestalt”? Yogi Berra • Facial expression: Grimacing; furrowed brow; appears anxious; flat affect • Body position and spontaneous movement: there may be positioning to protect painful areas, limited movement due to pain • Diaphoresis – can be caused by pain • Areas of redness, swelling • Atrophied muscles • Gait • Myoclonus – possibly indicating opioid-induced neurotoxicity E L N E C International Curriculum
 Physical Exam In Pain Assessment Palpation • Localized tenderness to pressure or percussion • Fullness / mass • Induration / warmth E L N E C International Curriculum
Physical Exam In Pain Assessment Palpation • Localized tenderness to pressure or percussion • Fullness / mass • Induration / warmth E L N E C International Curriculum
 Physical Exam In Pain Assessment Neurological Examination • Important in evaluating pain, due to the possibility of spinal cord compression, and nerve root or peripheral nerve lesions • Sensory examination – Areas of numbness / decreased sensation – Areas of increased sensitivity, such as allodynia or hyperalgesia • Motor (strength) exam - caution if bony metastases (may fracture) • Deep tendon reflexes – intensity, symmetry – Hyperreflexia and clonus: possible upper motor neuron lesion, such as spinal cord compression or cerebral metastases. – Hyoporeflexia - possible lower motor neuron impairment, including lesions of the cauda equina of the spinal cord or leptomeningeal metastases. • Sacral reflexes – diminished rectal tone and absent anal reflexes may indicate cauda equina involvement of by tumour E L N E C International Curriculum
Physical Exam In Pain Assessment Neurological Examination • Important in evaluating pain, due to the possibility of spinal cord compression, and nerve root or peripheral nerve lesions • Sensory examination – Areas of numbness / decreased sensation – Areas of increased sensitivity, such as allodynia or hyperalgesia • Motor (strength) exam - caution if bony metastases (may fracture) • Deep tendon reflexes – intensity, symmetry – Hyperreflexia and clonus: possible upper motor neuron lesion, such as spinal cord compression or cerebral metastases. – Hyoporeflexia - possible lower motor neuron impairment, including lesions of the cauda equina of the spinal cord or leptomeningeal metastases. • Sacral reflexes – diminished rectal tone and absent anal reflexes may indicate cauda equina involvement of by tumour E L N E C International Curriculum
 Physical Exam In Pain Assessment Other Exam Considerations Further areas of focus of the physical examination are determined by the clinical presentation. Eg: evaluation of pleuritic chest pain would involve a detailed respiratory and chest wall examination. E L N E C International Curriculum
Physical Exam In Pain Assessment Other Exam Considerations Further areas of focus of the physical examination are determined by the clinical presentation. Eg: evaluation of pleuritic chest pain would involve a detailed respiratory and chest wall examination. E L N E C International Curriculum
 Pain Treatment E L N E C International Curriculum
Pain Treatment E L N E C International Curriculum
 Non-Pharmacological Pain Management • Acupuncture • Cognitive/behavioral therapy • Meditation/relaxation • Guided imagery • TENS • Therapeutic massage • Others… E L N E C International Curriculum
Non-Pharmacological Pain Management • Acupuncture • Cognitive/behavioral therapy • Meditation/relaxation • Guided imagery • TENS • Therapeutic massage • Others… E L N E C International Curriculum
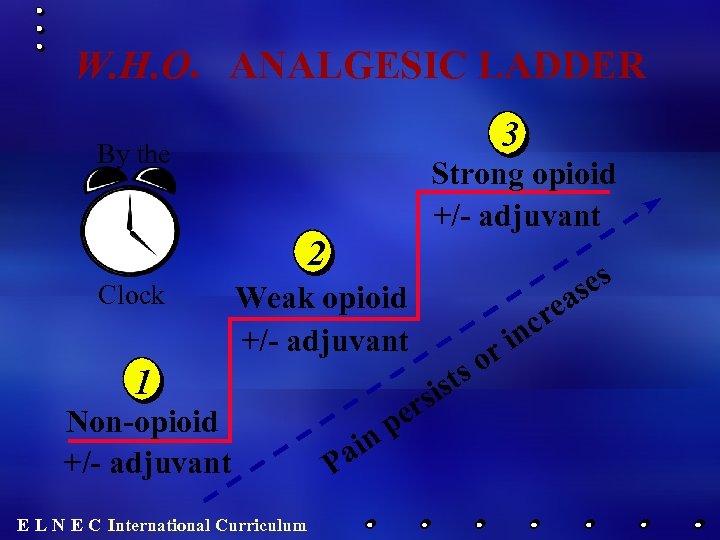 W. H. O. ANALGESIC LADDER 3 By the Strong opioid +/- adjuvant 2 Clock es as Weak opioid +/- adjuvant ist rs 1 Non-opioid +/- adjuvant E L N E C International Curriculum or s ai P pe n re nc i
W. H. O. ANALGESIC LADDER 3 By the Strong opioid +/- adjuvant 2 Clock es as Weak opioid +/- adjuvant ist rs 1 Non-opioid +/- adjuvant E L N E C International Curriculum or s ai P pe n re nc i
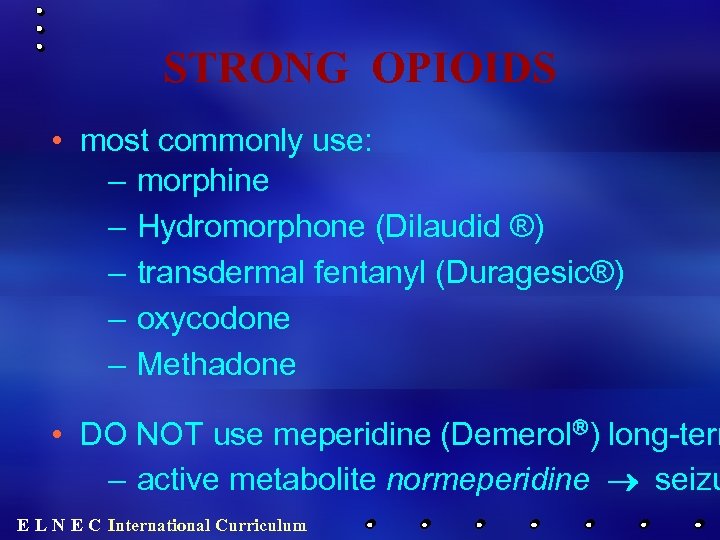 STRONG OPIOIDS • most commonly use: – morphine – Hydromorphone (Dilaudid ®) – transdermal fentanyl (Duragesic®) – oxycodone – Methadone • DO NOT use meperidine (Demerolâ) long-term – active metabolite normeperidine ® seizu E L N E C International Curriculum
STRONG OPIOIDS • most commonly use: – morphine – Hydromorphone (Dilaudid ®) – transdermal fentanyl (Duragesic®) – oxycodone – Methadone • DO NOT use meperidine (Demerolâ) long-term – active metabolite normeperidine ® seizu E L N E C International Curriculum
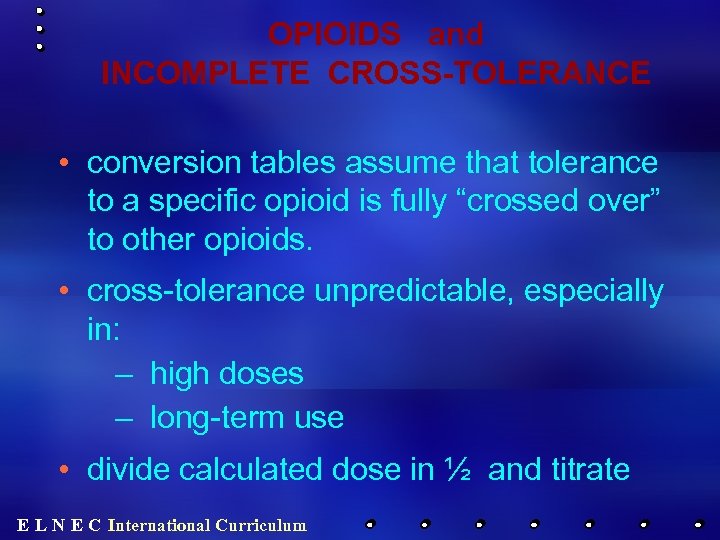 OPIOIDS and INCOMPLETE CROSS-TOLERANCE • conversion tables assume that tolerance to a specific opioid is fully “crossed over” to other opioids. • cross-tolerance unpredictable, especially in: – high doses – long-term use • divide calculated dose in ½ and titrate E L N E C International Curriculum
OPIOIDS and INCOMPLETE CROSS-TOLERANCE • conversion tables assume that tolerance to a specific opioid is fully “crossed over” to other opioids. • cross-tolerance unpredictable, especially in: – high doses – long-term use • divide calculated dose in ½ and titrate E L N E C International Curriculum
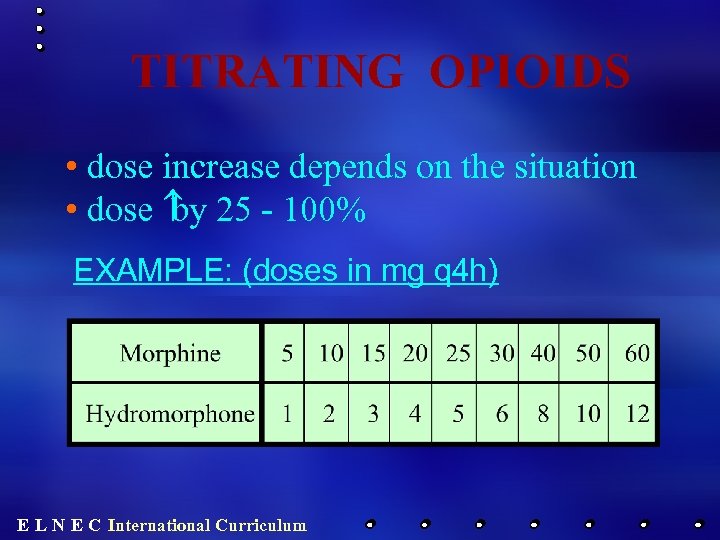 TITRATING OPIOIDS • dose increase depends on the situation • dose 25 - 100% by EXAMPLE: (doses in mg q 4 h) E L N E C International Curriculum
TITRATING OPIOIDS • dose increase depends on the situation • dose 25 - 100% by EXAMPLE: (doses in mg q 4 h) E L N E C International Curriculum
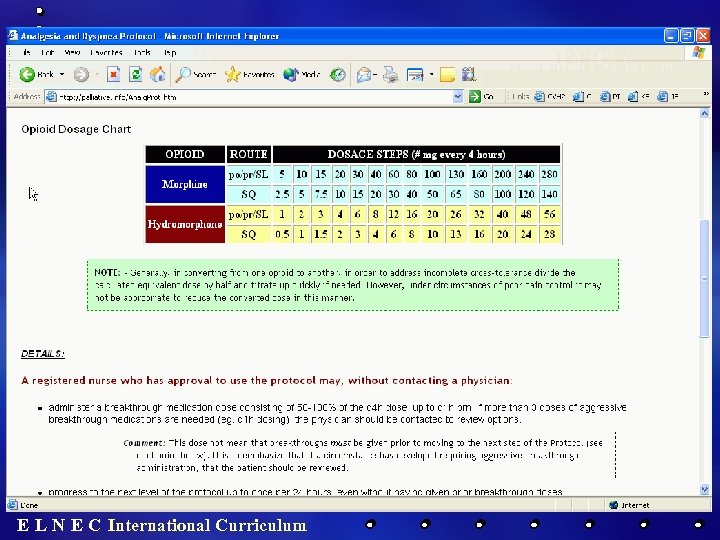
 http: //palliative. info E L N E C International Curriculum
http: //palliative. info E L N E C International Curriculum
 http: //palliative. info E L N E C International Curriculum
http: //palliative. info E L N E C International Curriculum
 E L N E C International Curriculum
E L N E C International Curriculum
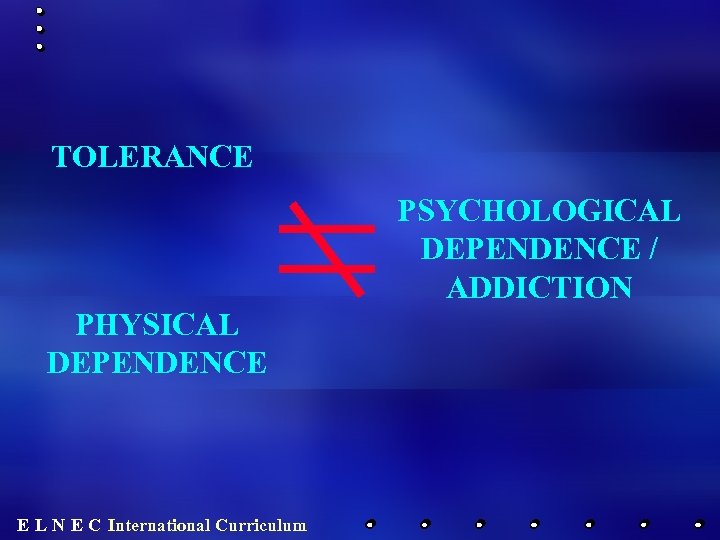 TOLERANCE PSYCHOLOGICAL DEPENDENCE / ADDICTION PHYSICAL DEPENDENCE E L N E C International Curriculum
TOLERANCE PSYCHOLOGICAL DEPENDENCE / ADDICTION PHYSICAL DEPENDENCE E L N E C International Curriculum
 TOLERANCE A normal physiological phenomenon in which increasing doses are required to produce the same effect Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
TOLERANCE A normal physiological phenomenon in which increasing doses are required to produce the same effect Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
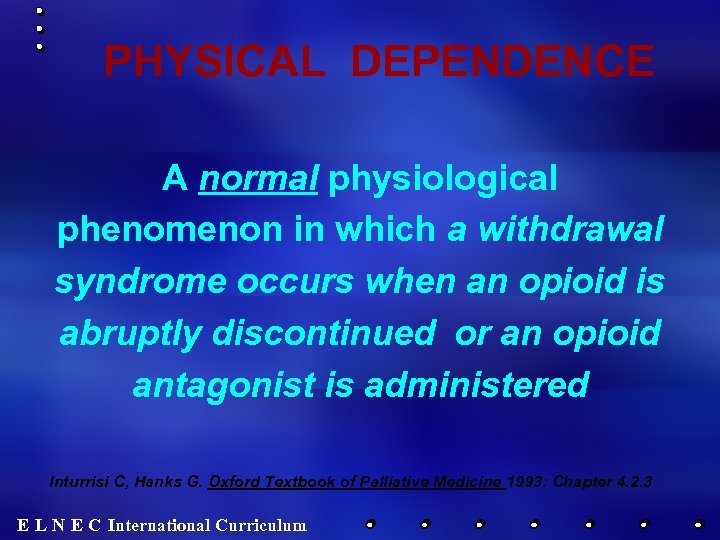 PHYSICAL DEPENDENCE A normal physiological phenomenon in which a withdrawal syndrome occurs when an opioid is abruptly discontinued or an opioid antagonist is administered Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
PHYSICAL DEPENDENCE A normal physiological phenomenon in which a withdrawal syndrome occurs when an opioid is abruptly discontinued or an opioid antagonist is administered Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
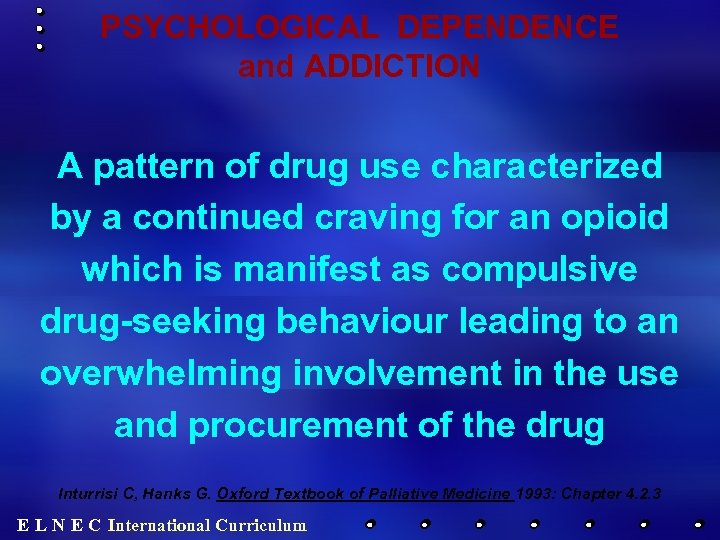 PSYCHOLOGICAL DEPENDENCE and ADDICTION A pattern of drug use characterized by a continued craving for an opioid which is manifest as compulsive drug-seeking behaviour leading to an overwhelming involvement in the use and procurement of the drug Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
PSYCHOLOGICAL DEPENDENCE and ADDICTION A pattern of drug use characterized by a continued craving for an opioid which is manifest as compulsive drug-seeking behaviour leading to an overwhelming involvement in the use and procurement of the drug Inturrisi C, Hanks G. Oxford Textbook of Palliative Medicine 1993: Chapter 4. 2. 3 E L N E C International Curriculum
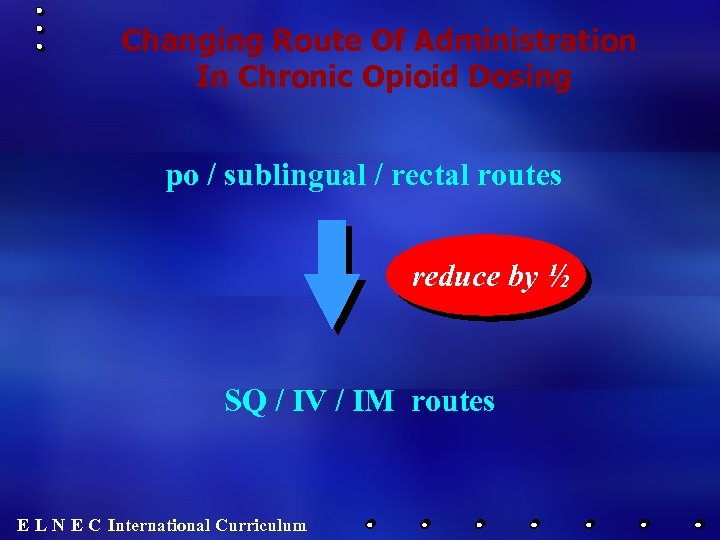 Changing Route Of Administration In Chronic Opioid Dosing po / sublingual / rectal routes reduce by ½ SQ / IV / IM routes E L N E C International Curriculum
Changing Route Of Administration In Chronic Opioid Dosing po / sublingual / rectal routes reduce by ½ SQ / IV / IM routes E L N E C International Curriculum
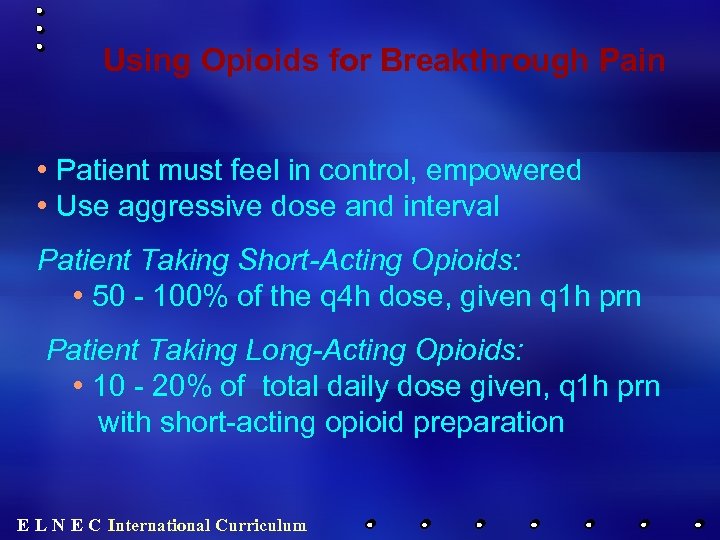 Using Opioids for Breakthrough Pain • Patient must feel in control, empowered • Use aggressive dose and interval Patient Taking Short-Acting Opioids: • 50 - 100% of the q 4 h dose, given q 1 h prn Patient Taking Long-Acting Opioids: • 10 - 20% of total daily dose given, q 1 h prn with short-acting opioid preparation E L N E C International Curriculum
Using Opioids for Breakthrough Pain • Patient must feel in control, empowered • Use aggressive dose and interval Patient Taking Short-Acting Opioids: • 50 - 100% of the q 4 h dose, given q 1 h prn Patient Taking Long-Acting Opioids: • 10 - 20% of total daily dose given, q 1 h prn with short-acting opioid preparation E L N E C International Curriculum
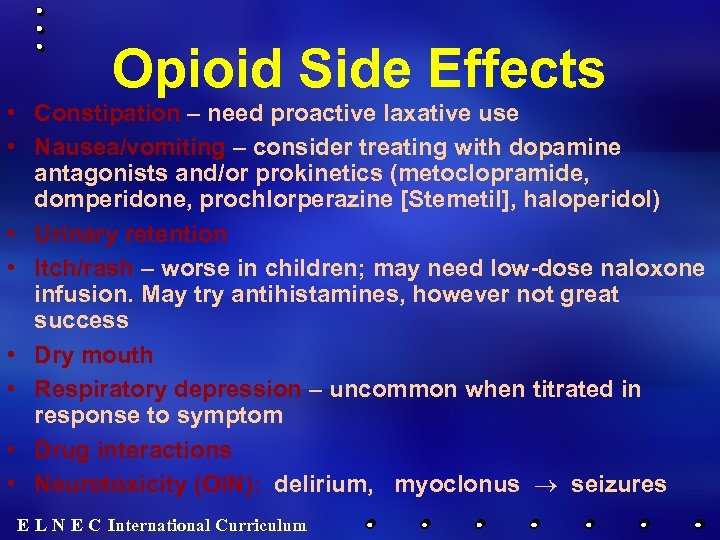 Opioid Side Effects • Constipation – need proactive laxative use • Nausea/vomiting – consider treating with dopamine antagonists and/or prokinetics (metoclopramide, domperidone, prochlorperazine [Stemetil], haloperidol) • Urinary retention • Itch/rash – worse in children; may need low-dose naloxone infusion. May try antihistamines, however not great success • Dry mouth • Respiratory depression – uncommon when titrated in response to symptom • Drug interactions • Neurotoxicity (OIN): delirium, myoclonus ® seizures E L N E C International Curriculum
Opioid Side Effects • Constipation – need proactive laxative use • Nausea/vomiting – consider treating with dopamine antagonists and/or prokinetics (metoclopramide, domperidone, prochlorperazine [Stemetil], haloperidol) • Urinary retention • Itch/rash – worse in children; may need low-dose naloxone infusion. May try antihistamines, however not great success • Dry mouth • Respiratory depression – uncommon when titrated in response to symptom • Drug interactions • Neurotoxicity (OIN): delirium, myoclonus ® seizures E L N E C International Curriculum
 E L N E C International Curriculum
E L N E C International Curriculum
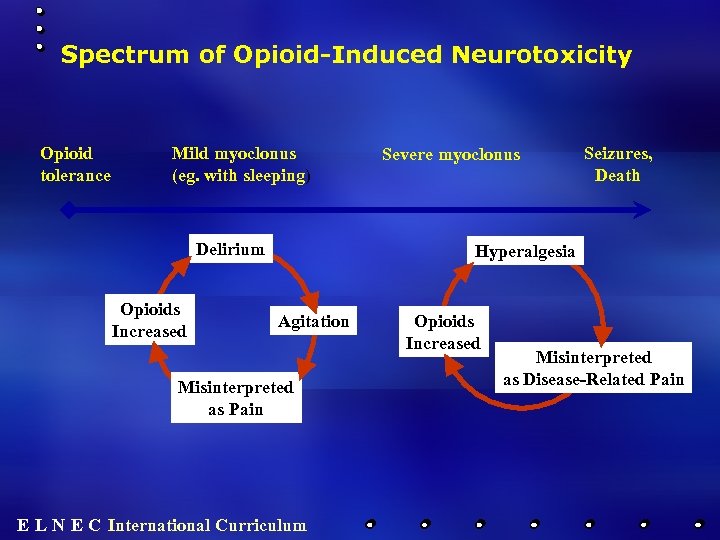 Spectrum of Opioid-Induced Neurotoxicity Opioid tolerance Mild myoclonus (eg. with sleeping) Delirium Opioids Increased Severe myoclonus Seizures, Death Hyperalgesia Agitation Misinterpreted as Pain E L N E C International Curriculum Opioids Increased Misinterpreted as Disease-Related Pain
Spectrum of Opioid-Induced Neurotoxicity Opioid tolerance Mild myoclonus (eg. with sleeping) Delirium Opioids Increased Severe myoclonus Seizures, Death Hyperalgesia Agitation Misinterpreted as Pain E L N E C International Curriculum Opioids Increased Misinterpreted as Disease-Related Pain
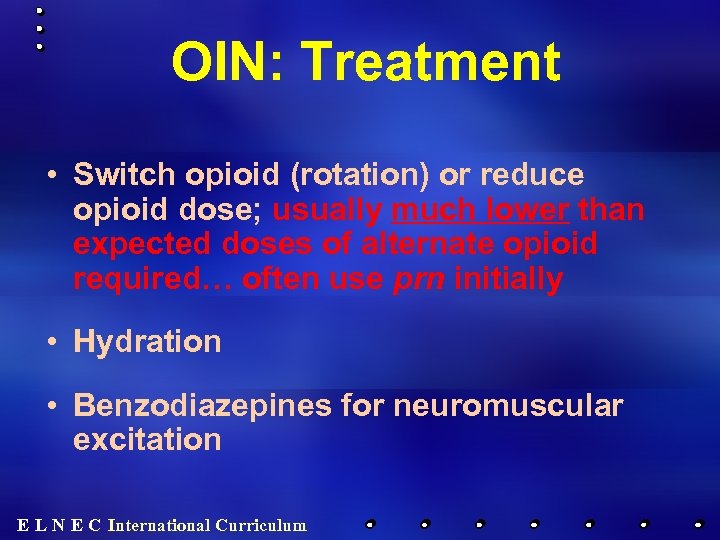 OIN: Treatment • Switch opioid (rotation) or reduce opioid dose; usually much lower than expected doses of alternate opioid required… often use prn initially • Hydration • Benzodiazepines for neuromuscular excitation E L N E C International Curriculum
OIN: Treatment • Switch opioid (rotation) or reduce opioid dose; usually much lower than expected doses of alternate opioid required… often use prn initially • Hydration • Benzodiazepines for neuromuscular excitation E L N E C International Curriculum
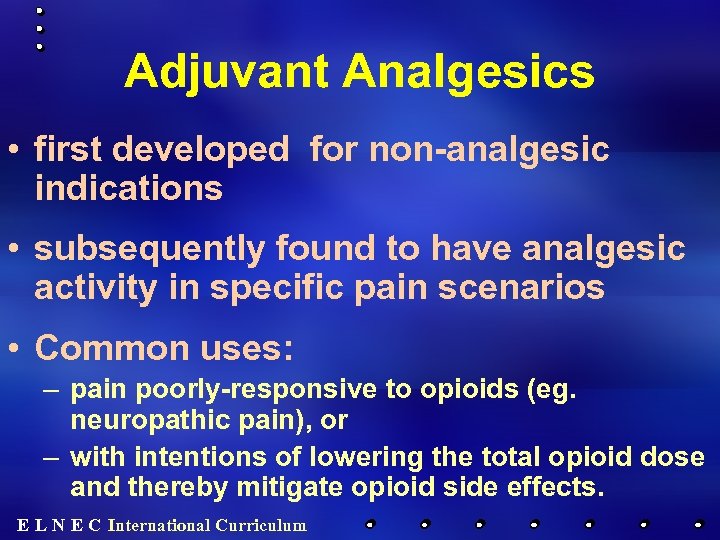 Adjuvant Analgesics • first developed for non-analgesic indications • subsequently found to have analgesic activity in specific pain scenarios • Common uses: – pain poorly-responsive to opioids (eg. neuropathic pain), or – with intentions of lowering the total opioid dose and thereby mitigate opioid side effects. E L N E C International Curriculum
Adjuvant Analgesics • first developed for non-analgesic indications • subsequently found to have analgesic activity in specific pain scenarios • Common uses: – pain poorly-responsive to opioids (eg. neuropathic pain), or – with intentions of lowering the total opioid dose and thereby mitigate opioid side effects. E L N E C International Curriculum
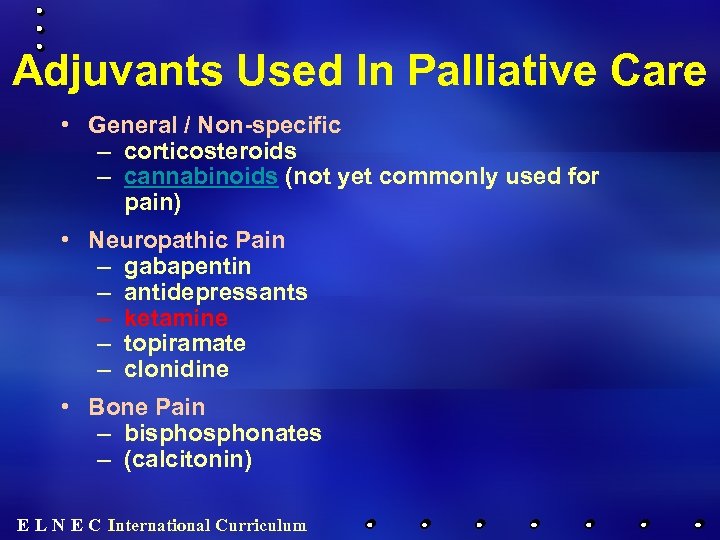 Adjuvants Used In Palliative Care • General / Non-specific – corticosteroids – cannabinoids (not yet commonly used for pain) • Neuropathic Pain – gabapentin – antidepressants – ketamine – topiramate – clonidine • Bone Pain – bisphonates – (calcitonin) E L N E C International Curriculum
Adjuvants Used In Palliative Care • General / Non-specific – corticosteroids – cannabinoids (not yet commonly used for pain) • Neuropathic Pain – gabapentin – antidepressants – ketamine – topiramate – clonidine • Bone Pain – bisphonates – (calcitonin) E L N E C International Curriculum
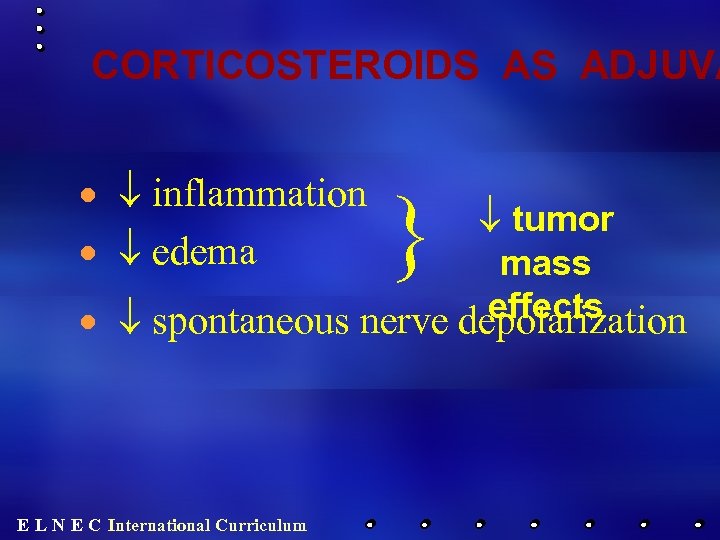 CORTICOSTEROIDS AS ADJUVA · ¯ inflammation · ¯ edema } ¯ tumor mass effects · ¯ spontaneous nerve depolarization E L N E C International Curriculum
CORTICOSTEROIDS AS ADJUVA · ¯ inflammation · ¯ edema } ¯ tumor mass effects · ¯ spontaneous nerve depolarization E L N E C International Curriculum
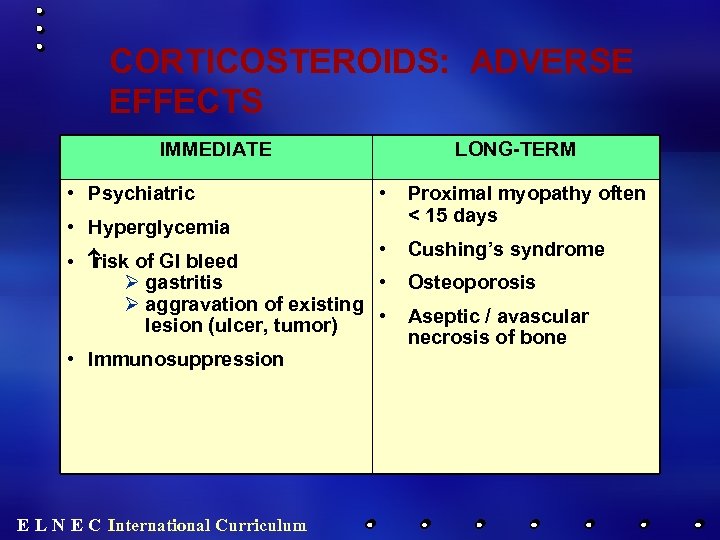 CORTICOSTEROIDS: ADVERSE EFFECTS IMMEDIATE • Psychiatric • Hyperglycemia LONG-TERM • • • risk of GI bleed Ø gastritis • Ø aggravation of existing • lesion (ulcer, tumor) • Immunosuppression E L N E C International Curriculum Proximal myopathy often < 15 days Cushing’s syndrome Osteoporosis Aseptic / avascular necrosis of bone
CORTICOSTEROIDS: ADVERSE EFFECTS IMMEDIATE • Psychiatric • Hyperglycemia LONG-TERM • • • risk of GI bleed Ø gastritis • Ø aggravation of existing • lesion (ulcer, tumor) • Immunosuppression E L N E C International Curriculum Proximal myopathy often < 15 days Cushing’s syndrome Osteoporosis Aseptic / avascular necrosis of bone
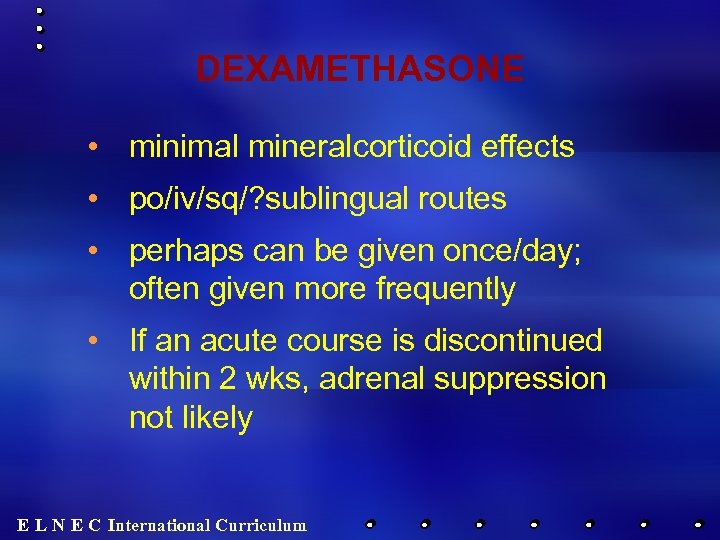 DEXAMETHASONE • minimal mineralcorticoid effects • po/iv/sq/? sublingual routes • perhaps can be given once/day; often given more frequently • If an acute course is discontinued within 2 wks, adrenal suppression not likely E L N E C International Curriculum
DEXAMETHASONE • minimal mineralcorticoid effects • po/iv/sq/? sublingual routes • perhaps can be given once/day; often given more frequently • If an acute course is discontinued within 2 wks, adrenal suppression not likely E L N E C International Curriculum
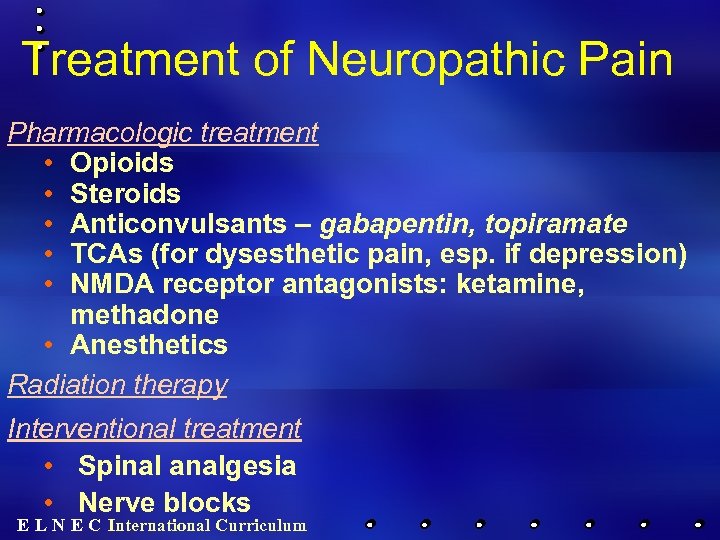 Treatment of Neuropathic Pain Pharmacologic treatment • Opioids • Steroids • Anticonvulsants – gabapentin, topiramate • TCAs (for dysesthetic pain, esp. if depression) • NMDA receptor antagonists: ketamine, methadone • Anesthetics Radiation therapy Interventional treatment • Spinal analgesia • Nerve blocks E L N E C International Curriculum
Treatment of Neuropathic Pain Pharmacologic treatment • Opioids • Steroids • Anticonvulsants – gabapentin, topiramate • TCAs (for dysesthetic pain, esp. if depression) • NMDA receptor antagonists: ketamine, methadone • Anesthetics Radiation therapy Interventional treatment • Spinal analgesia • Nerve blocks E L N E C International Curriculum
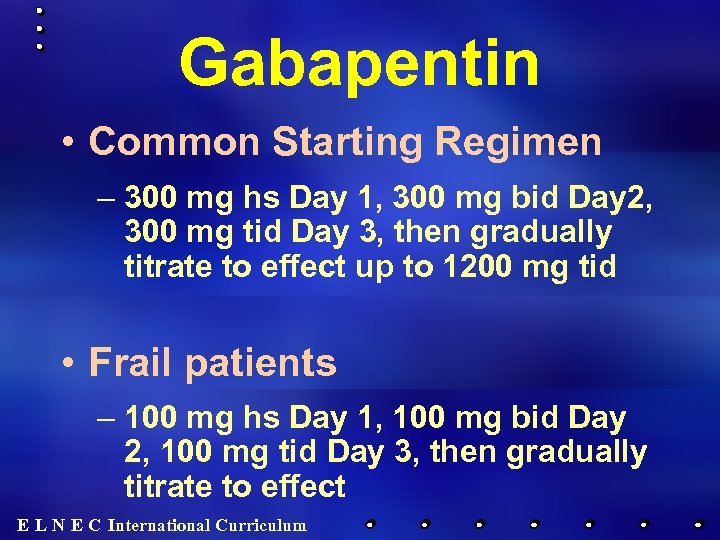 Gabapentin • Common Starting Regimen – 300 mg hs Day 1, 300 mg bid Day 2, 300 mg tid Day 3, then gradually titrate to effect up to 1200 mg tid • Frail patients – 100 mg hs Day 1, 100 mg bid Day 2, 100 mg tid Day 3, then gradually titrate to effect E L N E C International Curriculum
Gabapentin • Common Starting Regimen – 300 mg hs Day 1, 300 mg bid Day 2, 300 mg tid Day 3, then gradually titrate to effect up to 1200 mg tid • Frail patients – 100 mg hs Day 1, 100 mg bid Day 2, 100 mg tid Day 3, then gradually titrate to effect E L N E C International Curriculum
 Incident Pain occurring as a direct and immediate consequence of a movement or activity E L N E C International Curriculum
Incident Pain occurring as a direct and immediate consequence of a movement or activity E L N E C International Curriculum
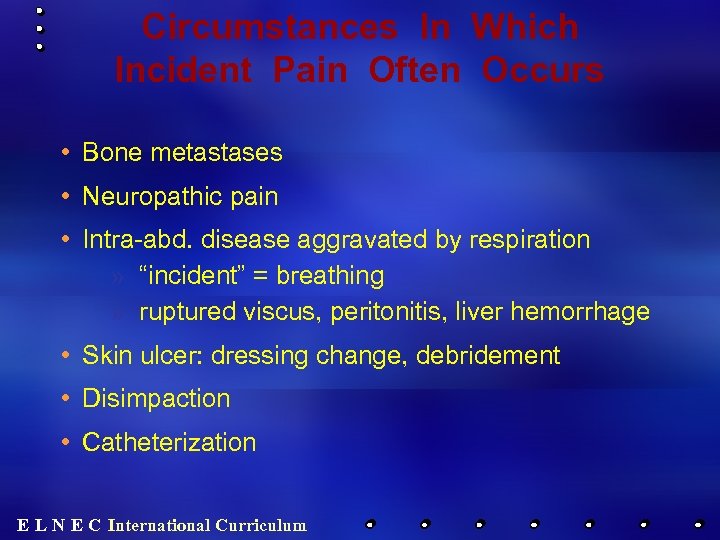 Circumstances In Which Incident Pain Often Occurs • Bone metastases • Neuropathic pain • Intra-abd. disease aggravated by respiration » “incident” = breathing » ruptured viscus, peritonitis, liver hemorrhage • Skin ulcer: dressing change, debridement • Disimpaction • Catheterization E L N E C International Curriculum
Circumstances In Which Incident Pain Often Occurs • Bone metastases • Neuropathic pain • Intra-abd. disease aggravated by respiration » “incident” = breathing » ruptured viscus, peritonitis, liver hemorrhage • Skin ulcer: dressing change, debridement • Disimpaction • Catheterization E L N E C International Curriculum
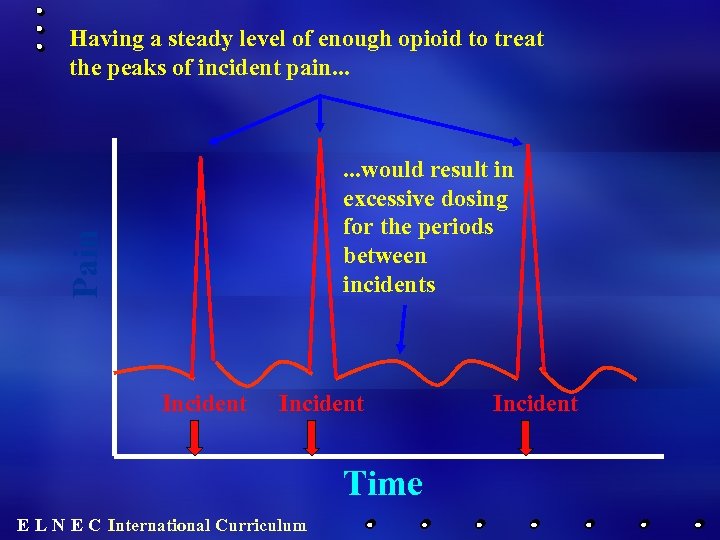 Having a steady level of enough opioid to treat the peaks of incident pain. . . Pain . . . would result in excessive dosing for the periods between incidents Incident Time E L N E C International Curriculum Incident
Having a steady level of enough opioid to treat the peaks of incident pain. . . Pain . . . would result in excessive dosing for the periods between incidents Incident Time E L N E C International Curriculum Incident
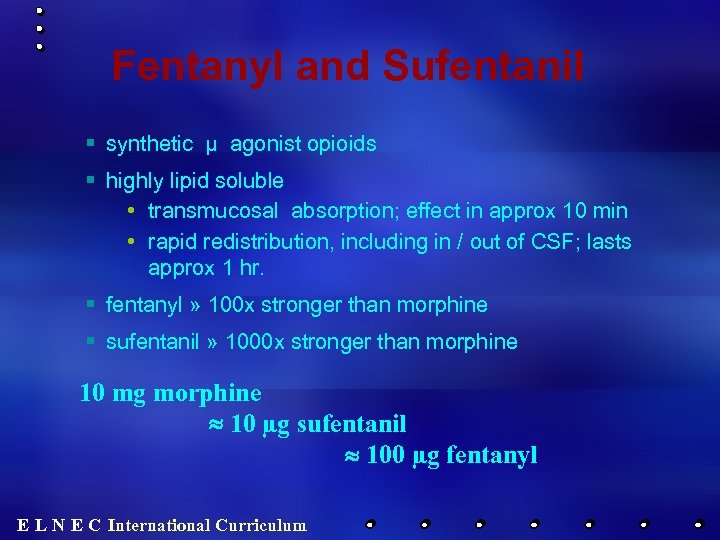 Fentanyl and Sufentanil § synthetic µ agonist opioids § highly lipid soluble • transmucosal absorption; effect in approx 10 min • rapid redistribution, including in / out of CSF; lasts approx 1 hr. § fentanyl » 100 x stronger than morphine § sufentanil » 1000 x stronger than morphine 10 mg morphine » 10 µg sufentanil » 100 µg fentanyl E L N E C International Curriculum
Fentanyl and Sufentanil § synthetic µ agonist opioids § highly lipid soluble • transmucosal absorption; effect in approx 10 min • rapid redistribution, including in / out of CSF; lasts approx 1 hr. § fentanyl » 100 x stronger than morphine § sufentanil » 1000 x stronger than morphine 10 mg morphine » 10 µg sufentanil » 100 µg fentanyl E L N E C International Curriculum
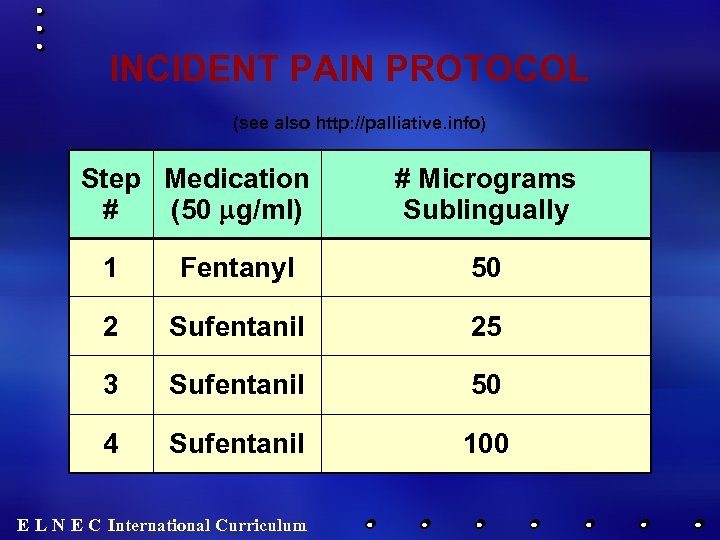 INCIDENT PAIN PROTOCOL (see also http: //palliative. info) Step Medication # (50 mg/ml) # Micrograms Sublingually 1 Fentanyl 50 2 Sufentanil 25 3 Sufentanil 50 4 Sufentanil 100 E L N E C International Curriculum
INCIDENT PAIN PROTOCOL (see also http: //palliative. info) Step Medication # (50 mg/ml) # Micrograms Sublingually 1 Fentanyl 50 2 Sufentanil 25 3 Sufentanil 50 4 Sufentanil 100 E L N E C International Curriculum
 INCIDENT PAIN PROTOCOL ctd. . . • fentanyl or sufentanil is administered SL 10 min. prior to anticipated activity • repeat q 10 min x 2 additional doses if needed • increase to next step if 3 total doses not effective • physician order required to increase to next step if within an hour of last dose • the Incident Pain Protocol may be used up to q 1 h prn E L N E C International Curriculum
INCIDENT PAIN PROTOCOL ctd. . . • fentanyl or sufentanil is administered SL 10 min. prior to anticipated activity • repeat q 10 min x 2 additional doses if needed • increase to next step if 3 total doses not effective • physician order required to increase to next step if within an hour of last dose • the Incident Pain Protocol may be used up to q 1 h prn E L N E C International Curriculum
 Barriers to Pain Relief • Importance of discussing barriers • Specific barriers – Professionals – Health care systems – Patients/families Miaskowski et al. , 2005; Paice, 2010; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 55
Barriers to Pain Relief • Importance of discussing barriers • Specific barriers – Professionals – Health care systems – Patients/families Miaskowski et al. , 2005; Paice, 2010; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 55
 Pain Assessment • Pain history • Pain terms • Acute vs. chronic Fink & Gates, 2010 E L N E C International Curriculum 56
Pain Assessment • Pain history • Pain terms • Acute vs. chronic Fink & Gates, 2010 E L N E C International Curriculum 56
 Pain History • • Location Intensity Quality Temporal pattern E L N E C International Curriculum 57
Pain History • • Location Intensity Quality Temporal pattern E L N E C International Curriculum 57
 Pain History • • Aggravating/alleviating factors Medication history (recent and distant) Meaning of pain Cultural factors E L N E C International Curriculum 58
Pain History • • Aggravating/alleviating factors Medication history (recent and distant) Meaning of pain Cultural factors E L N E C International Curriculum 58
 Physical Examination • • Observation Palpation Auscultation Percussion E L N E C International Curriculum 59
Physical Examination • • Observation Palpation Auscultation Percussion E L N E C International Curriculum 59
 Functional Assessment • Ability to dress self • Walking • Cooking E L N E C International Curriculum 60
Functional Assessment • Ability to dress self • Walking • Cooking E L N E C International Curriculum 60
 Laboratory/Diagnostic Evaluation • Rule out potentially treatable causes • Need for additional laboratory or radiographic evaluation is directed by the goals of care E L N E C International Curriculum 61
Laboratory/Diagnostic Evaluation • Rule out potentially treatable causes • Need for additional laboratory or radiographic evaluation is directed by the goals of care E L N E C International Curriculum 61
 Reassess • Changes in pain • Assess pain relief • Make pain visible E L N E C International Curriculum 62
Reassess • Changes in pain • Assess pain relief • Make pain visible E L N E C International Curriculum 62
 Common Syndromes at the End of Life • Nociceptive – Somatic – Visceral • Neuropathic – – Post herpetic neuropathy Diabetic neuropathy HIV associated neuropathy Chemotherapy related neuropathy E L N E C International Curriculum 63
Common Syndromes at the End of Life • Nociceptive – Somatic – Visceral • Neuropathic – – Post herpetic neuropathy Diabetic neuropathy HIV associated neuropathy Chemotherapy related neuropathy E L N E C International Curriculum 63
 Pain vs. Suffering at the End of Life • Existential distress • Dimensions of quality of life • Requires interdisciplinary approach E L N E C International Curriculum 64
Pain vs. Suffering at the End of Life • Existential distress • Dimensions of quality of life • Requires interdisciplinary approach E L N E C International Curriculum 64
 Patients at Risk for Undertreatment • • Children and older adults Non-verbal or cognitively impaired Patients who deny pain Patients who speak a different language • Different cultures • History of addictive disease E L N E C International Curriculum 65
Patients at Risk for Undertreatment • • Children and older adults Non-verbal or cognitively impaired Patients who deny pain Patients who speak a different language • Different cultures • History of addictive disease E L N E C International Curriculum 65
 Communicating Assessment Findings • Communication improves pain management • Describe intensity, limitations, and response to treatments • Documentation Gordon et al, 2005; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 66
Communicating Assessment Findings • Communication improves pain management • Describe intensity, limitations, and response to treatments • Documentation Gordon et al, 2005; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 66
 Definitions • • Tolerance Physiologic dependence Psychological dependence Opioids and death E L N E C International Curriculum 67
Definitions • • Tolerance Physiologic dependence Psychological dependence Opioids and death E L N E C International Curriculum 67
 Pharmacological Therapies • Nonopioids • Opioids • Adjuvants APS, 2008; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 68
Pharmacological Therapies • Nonopioids • Opioids • Adjuvants APS, 2008; Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 68
 Nonopioids • Paracetamol • NSAIDs APS, 2008; Paice, 2010: Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 69
Nonopioids • Paracetamol • NSAIDs APS, 2008; Paice, 2010: Pasero & Mc. Caffery, 2011 E L N E C International Curriculum 69
 Nonopioids: NSAIDs Adverse Effects E L N E C International Curriculum 70
Nonopioids: NSAIDs Adverse Effects E L N E C International Curriculum 70
 Opioids • • • Morphine Codeine Fentanyl Tramadol Methadone Pethidine E L N E C International Curriculum 71
Opioids • • • Morphine Codeine Fentanyl Tramadol Methadone Pethidine E L N E C International Curriculum 71
 Opioids: Adverse Effects • • • Respiratory depression Constipation Sedation Urinary retention Nausea/vomiting Pruritus E L N E C International Curriculum 72
Opioids: Adverse Effects • • • Respiratory depression Constipation Sedation Urinary retention Nausea/vomiting Pruritus E L N E C International Curriculum 72
 Adjuvant analgesics • • Antidepressants Anticonvulsants Local anesthetics Corticosteroids E L N E C International Curriculum 73
Adjuvant analgesics • • Antidepressants Anticonvulsants Local anesthetics Corticosteroids E L N E C International Curriculum 73
 Antidepressants • Block serotonin and norepinephrine • Administer at bedtime • Side effects • SSRIs have little analgesic effect • Newer agents E L N E C International Curriculum 74
Antidepressants • Block serotonin and norepinephrine • Administer at bedtime • Side effects • SSRIs have little analgesic effect • Newer agents E L N E C International Curriculum 74
 Anticonvulsants/Antiepilepsy Drugs • Older agents have significant adverse effects • Newer agents: – Gabapentin – Pregabalin – Lamotrigine, levetiracetam, oxcarbazepine and others E L N E C International Curriculum 75
Anticonvulsants/Antiepilepsy Drugs • Older agents have significant adverse effects • Newer agents: – Gabapentin – Pregabalin – Lamotrigine, levetiracetam, oxcarbazepine and others E L N E C International Curriculum 75
 Local Anesthetics • Topical: Lidocaine gel or patch (plaster) • Intravenous • Spinal E L N E C International Curriculum 76
Local Anesthetics • Topical: Lidocaine gel or patch (plaster) • Intravenous • Spinal E L N E C International Curriculum 76
 Corticosteroids • Dexamethasone has least mineralocorticoid effect • Psychosis • Proximal muscle wasting • Administer - q am E L N E C International Curriculum 77
Corticosteroids • Dexamethasone has least mineralocorticoid effect • Psychosis • Proximal muscle wasting • Administer - q am E L N E C International Curriculum 77
 Routes of Administration • • • Oral Mucosal Rectal Transdermal Topical E L N E C International Curriculum 78
Routes of Administration • • • Oral Mucosal Rectal Transdermal Topical E L N E C International Curriculum 78
 Routes of Administration (cont. ) • Parenteral – Intravenous – Subcutaneous – Intramuscular E L N E C International Curriculum 79
Routes of Administration (cont. ) • Parenteral – Intravenous – Subcutaneous – Intramuscular E L N E C International Curriculum 79
 Routes of Administration (cont. ) • Spinal – Epidural – Intrathecal E L N E C International Curriculum 80
Routes of Administration (cont. ) • Spinal – Epidural – Intrathecal E L N E C International Curriculum 80
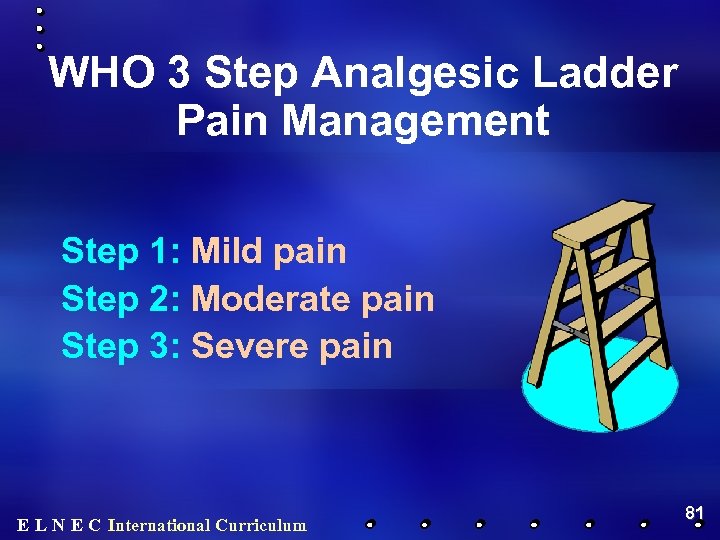 WHO 3 Step Analgesic Ladder Pain Management Step 1: Mild pain Step 2: Moderate pain Step 3: Severe pain E L N E C International Curriculum 81
WHO 3 Step Analgesic Ladder Pain Management Step 1: Mild pain Step 2: Moderate pain Step 3: Severe pain E L N E C International Curriculum 81
 Principles: Prevent and Treat Side Effects • Anticipate • Prevent • Treat E L N E C International Curriculum 82
Principles: Prevent and Treat Side Effects • Anticipate • Prevent • Treat E L N E C International Curriculum 82
 Principles: Long Acting Medications • Sustained release medications • Immediate release for breakthrough pain • Distinguish types of breakthrough pain –Episodic –Idiopathic –End of dose failure E L N E C International Curriculum 83
Principles: Long Acting Medications • Sustained release medications • Immediate release for breakthrough pain • Distinguish types of breakthrough pain –Episodic –Idiopathic –End of dose failure E L N E C International Curriculum 83
 Principles of Equianalgesia • Determine equal doses when changing drugs or routes of administration • Oral to parenteral morphine 3: 1 ratio • Reduce by 25% when changing drugs • Use of morphine equivalents E L N E C International Curriculum 84
Principles of Equianalgesia • Determine equal doses when changing drugs or routes of administration • Oral to parenteral morphine 3: 1 ratio • Reduce by 25% when changing drugs • Use of morphine equivalents E L N E C International Curriculum 84
 Principles: Use of Opioid Rotation • Use when one opioid is ineffective even with adequate titration • Use when adverse effects are unmanageable E L N E C International Curriculum 85
Principles: Use of Opioid Rotation • Use when one opioid is ineffective even with adequate titration • Use when adverse effects are unmanageable E L N E C International Curriculum 85
 Placebos • Not diagnostic • Causes mistrust • Never ethical E L N E C International Curriculum 86
Placebos • Not diagnostic • Causes mistrust • Never ethical E L N E C International Curriculum 86
 Cancer Therapies to Relieve Pain • • • Radiation Surgery Chemotherapy Hormonal therapy Others Doyle et al. , 2001; Janjan et al. , 2003; Jeremic, 2001 E L N E C International Curriculum 87
Cancer Therapies to Relieve Pain • • • Radiation Surgery Chemotherapy Hormonal therapy Others Doyle et al. , 2001; Janjan et al. , 2003; Jeremic, 2001 E L N E C International Curriculum 87
 Interventional Therapies • Neurolytic blocks • Neuroablative procedures • Vertebroplasty Furlan et al. , 2001; Mathias et al. , 2001; Swarm et al. , 2010 E L N E C International Curriculum 88
Interventional Therapies • Neurolytic blocks • Neuroablative procedures • Vertebroplasty Furlan et al. , 2001; Mathias et al. , 2001; Swarm et al. , 2010 E L N E C International Curriculum 88
 Non-Pharmacologic Techniques • Cognitive - behavioral therapies – Relaxation – Imagery – Distraction – Support groups – Pastoral counseling E L N E C International Curriculum 89
Non-Pharmacologic Techniques • Cognitive - behavioral therapies – Relaxation – Imagery – Distraction – Support groups – Pastoral counseling E L N E C International Curriculum 89
 Non-Pharmacologic Techniques (cont. ) • Physical measures (heat, cold, massage) • Complementary therapies • Repositioning/ bracing Ernst, 2004; Kravits & Berenson, 2010; Smith et al. , 2002 E L N E C International Curriculum 90
Non-Pharmacologic Techniques (cont. ) • Physical measures (heat, cold, massage) • Complementary therapies • Repositioning/ bracing Ernst, 2004; Kravits & Berenson, 2010; Smith et al. , 2002 E L N E C International Curriculum 90
 Pain in HIV • • • Abdominal pain Headache Musculosketal pain Neuropathy Oral lesions E L N E C International Curriculum 91
Pain in HIV • • • Abdominal pain Headache Musculosketal pain Neuropathy Oral lesions E L N E C International Curriculum 91
 Roles of the Healthcare Team • • Direct clinical care Patient/family teaching Education of colleagues Identify system barriers a work to correct E L N E C International Curriculum 92
Roles of the Healthcare Team • • Direct clinical care Patient/family teaching Education of colleagues Identify system barriers a work to correct E L N E C International Curriculum 92
 Conclusion • Pain relief is contingent on adequate assessment and use of both drug and non-drug therapies • Pain extends beyond physical causes to other causes of suffering and existential distress • Interdisciplinary care E L N E C International Curriculum 93
Conclusion • Pain relief is contingent on adequate assessment and use of both drug and non-drug therapies • Pain extends beyond physical causes to other causes of suffering and existential distress • Interdisciplinary care E L N E C International Curriculum 93
 Freedom 94
Freedom 94
 Give the answers to the following questions please: 1. The definitions of Dysesthesia, Allodynia, Hyperalgesia, Hyperesthesia 2. Compare the nociceptive and neuropathic pain. What are the difference? 3. What are the main opioids used in palliative care? E L N E C International Curriculum
Give the answers to the following questions please: 1. The definitions of Dysesthesia, Allodynia, Hyperalgesia, Hyperesthesia 2. Compare the nociceptive and neuropathic pain. What are the difference? 3. What are the main opioids used in palliative care? E L N E C International Curriculum


