e39876c4af4b12d115a54c7a191eff07.ppt
- Количество слайдов: 31
Dynamics in Patient Selection from Inoperable to Moderate Risk: TAVR vs SAVR Alec Vahanian, FESC, FRCP (Edin. ) Bichat Hospital University Paris VII, Paris, France
Alec Vahanian, MD Consulting: Edwards Lifesciences, LLC Honoraria: Abbott Vascular Medtronic, Inc. Valtech
Background • > 60, 000 TAVI procedures since 2002 • Indications – ESC/EACTS/EAPCI Position Statement (Eur Heart J 2008; 29: 1463 -70) – 2012 ACCF/AATS/SCAI/STS Expert Consensus Document on Transcatheter Aortic Valve Replacement (J Am Coll Cardiol 2012; doi: 10. 1016/j. jacc. 2012. 01. 001) – ESC/EACTS Guidelines 2012 (Eur Heart J 2012; doi: 10. 1093/eurheartj/ehs 109 & Eur J Cardiothorac Surg 2012; doi: 10. 1093/ejcts/ezs 455).

European Heart Journal doi: 10. 1093/eurheartj/ehs 109 Guidelines on the management of valvular heart disease (version 2012) The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Authors/Task Force Members: Alec Vahanian (Chairperson) (France), Ottavio Alfieri (Chairperson) (Italy), Felicita Andreotti (Italy), Manuel J. Antunes (Portugal), Gonzalo Barón-Esquivias (Spain), Helmut Baumgartner (Germany), Michael Andrew Borger (Germany), Thierry P. Carrel (Switzerland), Michele De Bonis (Italy), Arturo Evangelista (Spain), Volkmar Falk (Switzerland), Bernard Iung (France), Patrizio Lancellotti (Belgium), Luc Pierard (Belgium), Susanna Price (UK), Hans-Joachim Schäfers (Germany), Gerhard Schuler (Germany), Janina Stepinska (Poland), Karl Swedberg (Sweden), Johanna Takkenberg (The Netherlands), Ulrich Otto Von Oppell (UK), Stephan Windecker (Switzerland), Jose Luis Zamorano (Spain), Marian Zembala (Poland) ESC Committee for Practice Guidelines (CPG): Jeroen J. Bax (Chairperson) (The Netherlands), Helmut Baumgartner (Germany), Claudio Ceconi (Italy), Veronica Dean (France), Christi Deaton (UK), Robert Fagard (Belgium), Christian Funck-Brentano (France), David Hasdai (Israel), Arno Hoes (The Netherlands), Paulus Kirchhof (United Kingdom), Juhani Knuuti (Finland), Philippe Kolh (Belgium), Theresa Mc. Donagh (UK), Cyril Moulin (France), Bogdan A. Popescu (Romania), Željko Reiner (Croatia), Udo Sechtem (Germany), Per Anton Sirnes (Norway), Michal Tendera (Poland), Adam Torbicki (Poland), Alec Vahanian (France), Stephan Windecker (Switzerland) Document Reviewers: Bogdan A. Popescu (ESC CPG Review Coordinator) (Romania), Ludwig Von Segesser (EACTS). Review Coordinator) (Switzerland), Luigi P. Badano (Italy), Matjaž Bunc (Slovenia), Marc J. Claeys (Belgium), Niksa Drinkovic (Croatia), Gerasimos Filippatos (Greece), Gilbert Habib (France), A. Pieter Kappetein (The Netherlands), Roland Kassab (Lebanon), Gregory Y. H. Lip (UK), Neil Moat (UK), Georg Nickenig (Germany), Catherine M. Otto (USA), John Pepper, (UK), Nicolo Piazza (Germany), Petronella G. Pieper (The Netherlands), Raphael Rosenhek (Austria), Naltin Shuka (Albania), Ehud Schwammenthal (Israel), Juerg, Schwitter (Switzerland), Pilar Tornos Mas (Spain), Pedro T. Trindade (Switzerland), Thomas Walther (Germany). www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
Why do we need new guidelines on the management of valvular disease? ● New evidence has been accumulated on: – risk stratification, – diagnostic methods, – therapeutic options. ● The importance of the collaborative approach between cardiologists and cardiac surgeons, working as a « heart team » , has emerged. www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
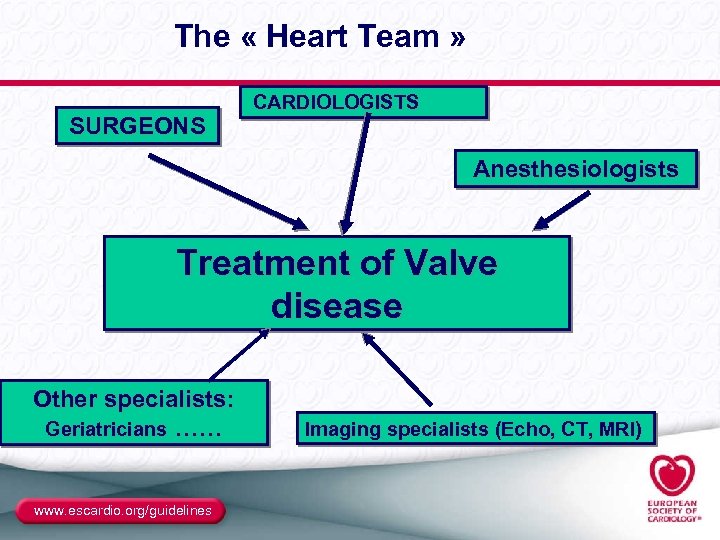
The « Heart Team » SURGEONS CARDIOLOGISTS Anesthesiologists Treatment of Valve disease Other specialists: Geriatricians …… www. escardio. org/guidelines Imaging specialists (Echo, CT, MRI)
Patient Evaluation www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
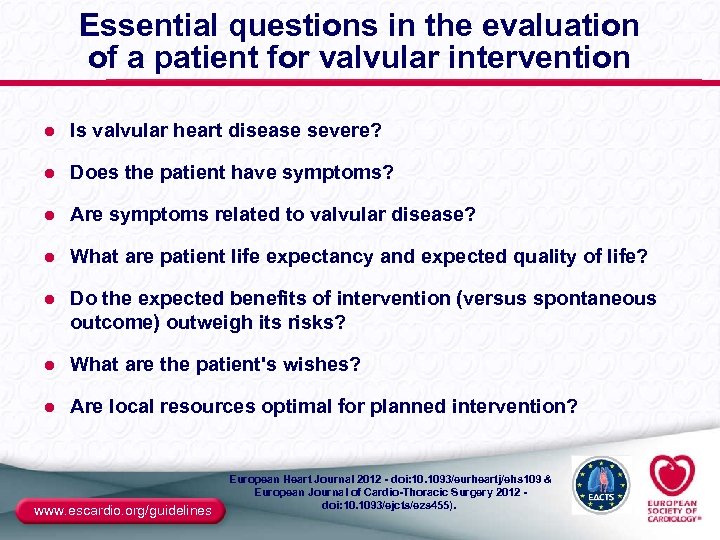
Essential questions in the evaluation of a patient for valvular intervention ● Is valvular heart disease severe? ● Does the patient have symptoms? ● Are symptoms related to valvular disease? ● What are patient life expectancy and expected quality of life? ● Do the expected benefits of intervention (versus spontaneous outcome) outweigh its risks? ● What are the patient's wishes? ● Are local resources optimal for planned intervention? www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
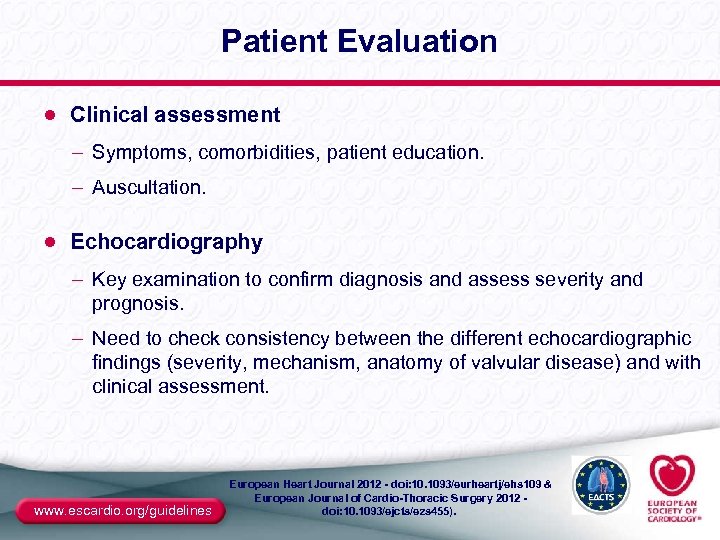
Patient Evaluation ● Clinical assessment – Symptoms, comorbidities, patient education. – Auscultation. ● Echocardiography – Key examination to confirm diagnosis and assess severity and prognosis. – Need to check consistency between the different echocardiographic findings (severity, mechanism, anatomy of valvular disease) and with clinical assessment. www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
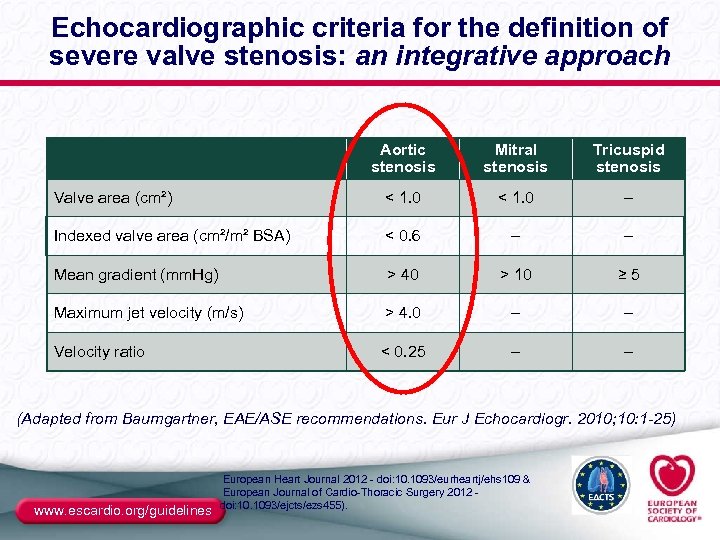
Echocardiographic criteria for the definition of severe valve stenosis: an integrative approach Aortic stenosis Mitral stenosis Tricuspid stenosis Valve area (cm²) < 1. 0 – Indexed valve area (cm²/m² BSA) < 0. 6 – – Mean gradient (mm. Hg) > 40 > 10 ≥ 5 Maximum jet velocity (m/s) > 4. 0 – – Velocity ratio < 0. 25 – – (Adapted from Baumgartner, EAE/ASE recommendations. Eur J Echocardiogr. 2010; 10: 1 -25) www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 doi: 10. 1093/ejcts/ezs 455).
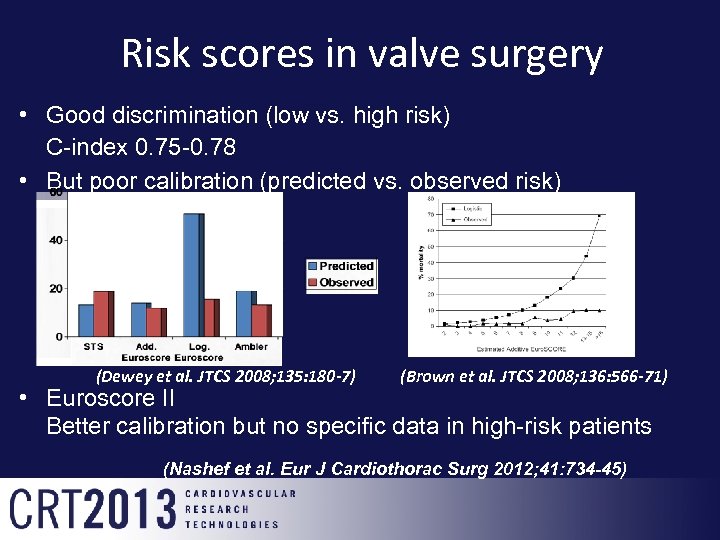
Risk scores in valve surgery • Good discrimination (low vs. high risk) C-index 0. 75 -0. 78 • But poor calibration (predicted vs. observed risk) (Dewey et al. JTCS 2008; 135: 180 -7) (Brown et al. JTCS 2008; 136: 566 -71) • Euroscore II Better calibration but no specific data in high-risk patients (Nashef et al. Eur J Cardiothorac Surg 2012; 41: 734 -45)

Risk factors not Captured in the Traditional Risk Scores • • Liver disease/cirrhosis “Porcelain” aorta Chest irradiation Chest wall deformities Oxygen dependence Neurocognitive dysfunction Frailty ……. .

Subjective assessment of frailty Eye-ball test Severe frailty Flexibility

Objective assessment of frailty Katz Index of Activities of Daily Living How many of these activities do you require help with? • 1. Bathing • 2. Dressing • 3. Toileting • 4. Transfering • 5. Continence • 6. Feeding Score 0 or 1 (Dependence vs. Independence) Total score <4: positive for frailty
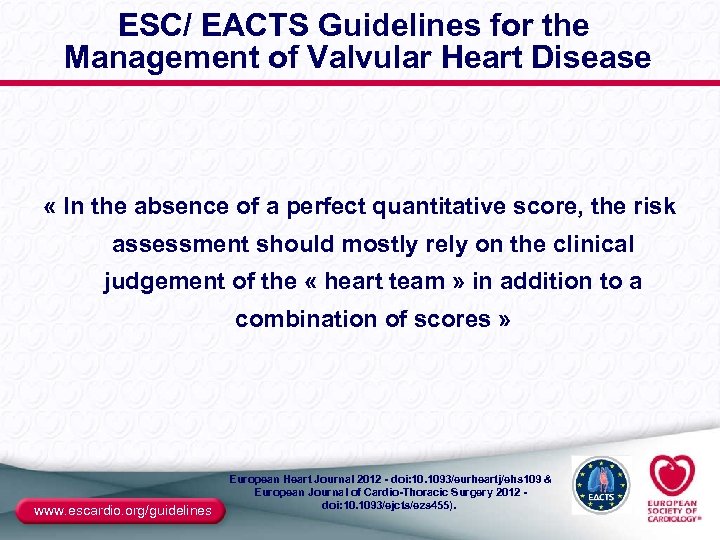
ESC/ EACTS Guidelines for the Management of Valvular Heart Disease « In the absence of a perfect quantitative score, the risk assessment should mostly rely on the clinical judgement of the « heart team » in addition to a combination of scores » www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
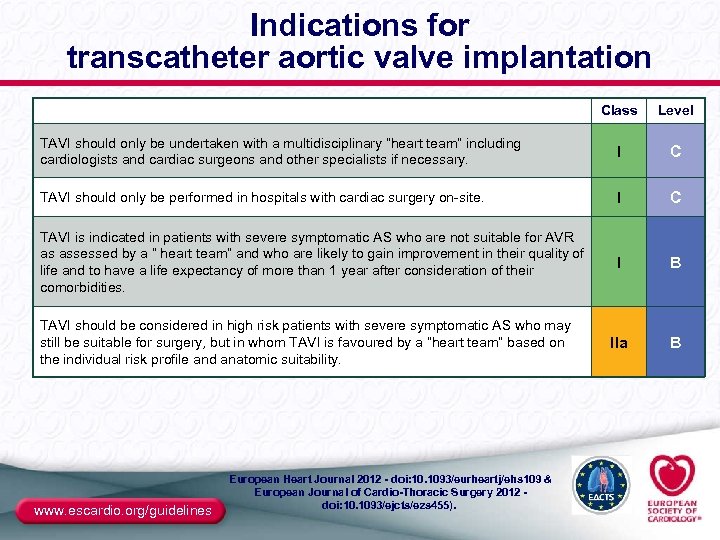
Indications for transcatheter aortic valve implantation Class Level TAVI should only be undertaken with a multidisciplinary “heart team” including cardiologists and cardiac surgeons and other specialists if necessary. I C TAVI should only be performed in hospitals with cardiac surgery on-site. I C TAVI is indicated in patients with severe symptomatic AS who are not suitable for AVR as assessed by a “ heart team” and who are likely to gain improvement in their quality of life and to have a life expectancy of more than 1 year after consideration of their comorbidities. I B IIa B TAVI should be considered in high risk patients with severe symptomatic AS who may still be suitable for surgery, but in whom TAVI is favoured by a “heart team” based on the individual risk profile and anatomic suitability. www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
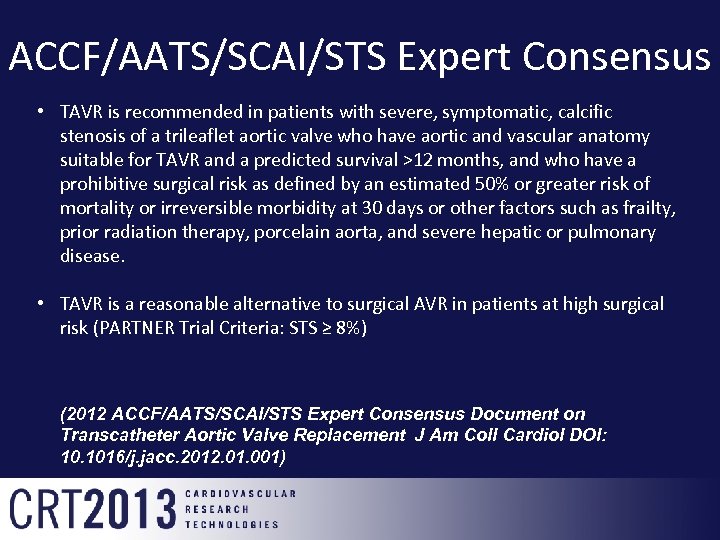
ACCF/AATS/SCAI/STS Expert Consensus • TAVR is recommended in patients with severe, symptomatic, calcific stenosis of a trileaflet aortic valve who have aortic and vascular anatomy suitable for TAVR and a predicted survival >12 months, and who have a prohibitive surgical risk as defined by an estimated 50% or greater risk of mortality or irreversible morbidity at 30 days or other factors such as frailty, prior radiation therapy, porcelain aorta, and severe hepatic or pulmonary disease. • TAVR is a reasonable alternative to surgical AVR in patients at high surgical risk (PARTNER Trial Criteria: STS ≥ 8%) (2012 ACCF/AATS/SCAI/STS Expert Consensus Document on Transcatheter Aortic Valve Replacement J Am Coll Cardiol DOI: 10. 1016/j. jacc. 2012. 01. 001)
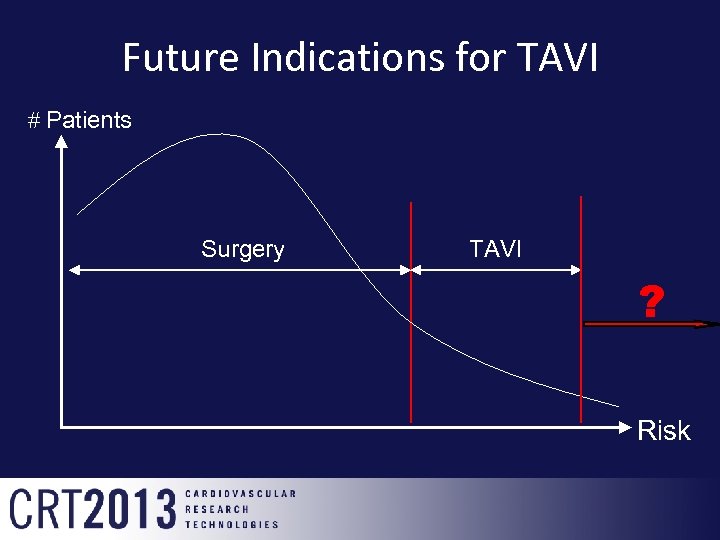
Future Indications for TAVI # Patients Surgery TAVI ? Risk
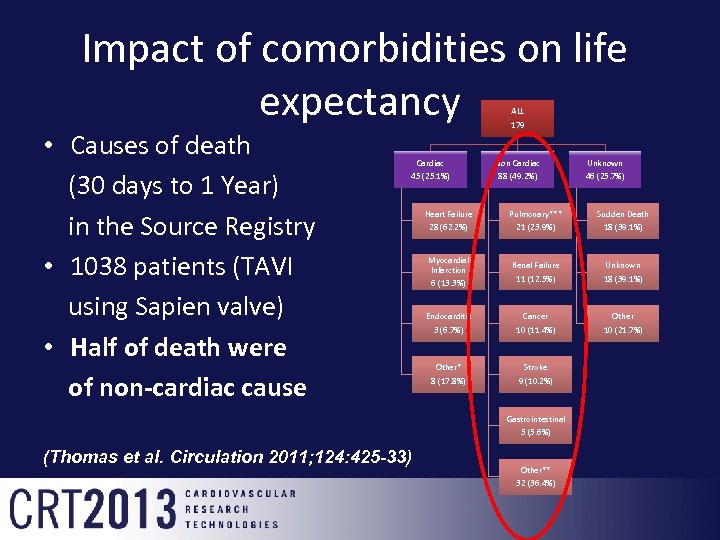
Impact of comorbidities on life expectancy ALL • Causes of death (30 days to 1 Year) in the Source Registry • 1038 patients (TAVI using Sapien valve) • Half of death were of non-cardiac cause 179 Cardiac Non Cardiac Unknown 45 (25. 1%) 88 (49. 2%) 46 (25. 7%) Heart Failure Pulmonary*** Sudden Death 28 (62. 2%) 21 (23. 9%) 18 (39. 1%) Myocardial Infarction 6 (13. 3%) Renal Failure Unknown 11 (12. 5%) 18 (39. 1%) Endocarditis Cancer Other 3 (6. 7%) 10 (11. 4%) 10 (21. 7%) Other* Stroke 8 (17. 8%) 9 (10. 2%) Gastrointestinal 5 (5. 6%) (Thomas et al. Circulation 2011; 124: 425 -33) Other** 32 (36. 4%)
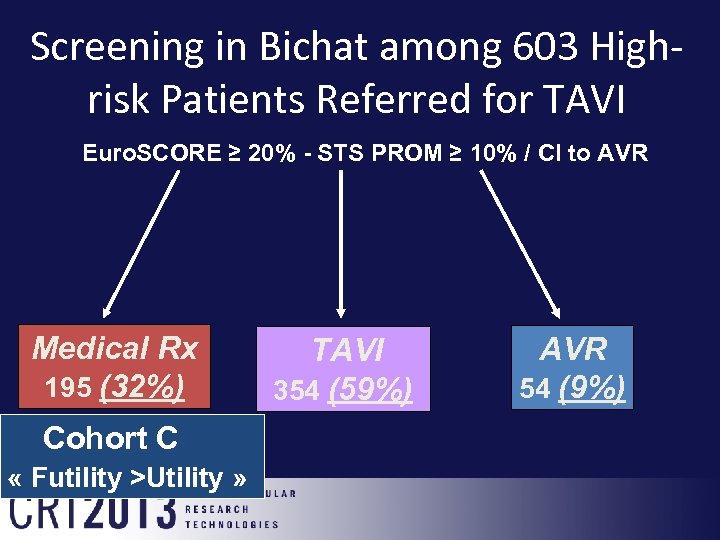
Screening in Bichat among 603 Highrisk Patients Referred for TAVI Euro. SCORE ≥ 20% - STS PROM ≥ 10% / CI to AVR Medical Rx 195 (32%) Cohort C « Futility >Utility » TAVI 354 (59%) AVR 54 (9%)
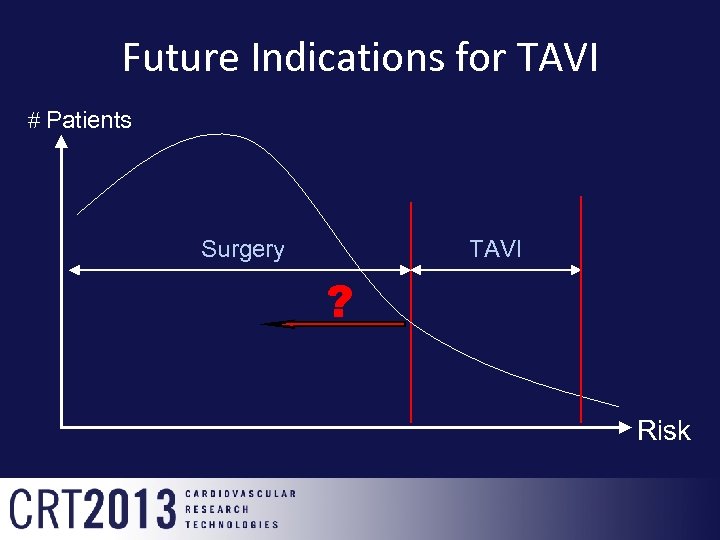
Future Indications for TAVI # Patients Surgery TAVI ? Risk
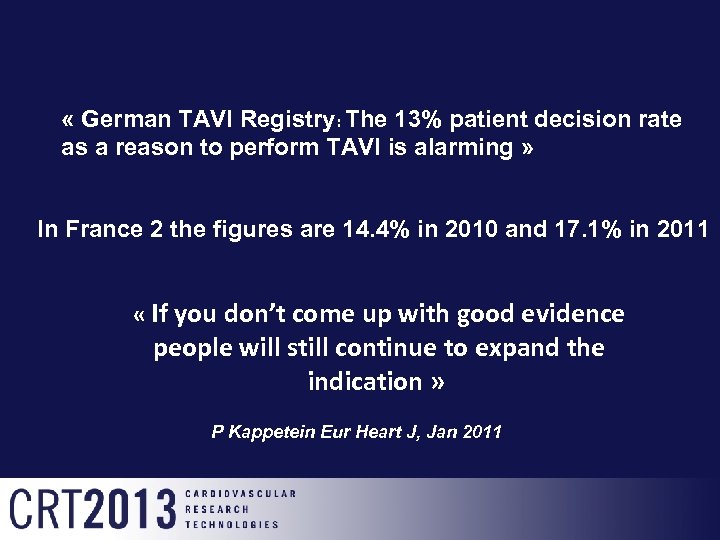
« German TAVI Registry: The 13% patient decision rate as a reason to perform TAVI is alarming » In France 2 the figures are 14. 4% in 2010 and 17. 1% in 2011 « If you don’t come up with good evidence people will still continue to expand the indication » P Kappetein Eur Heart J, Jan 2011
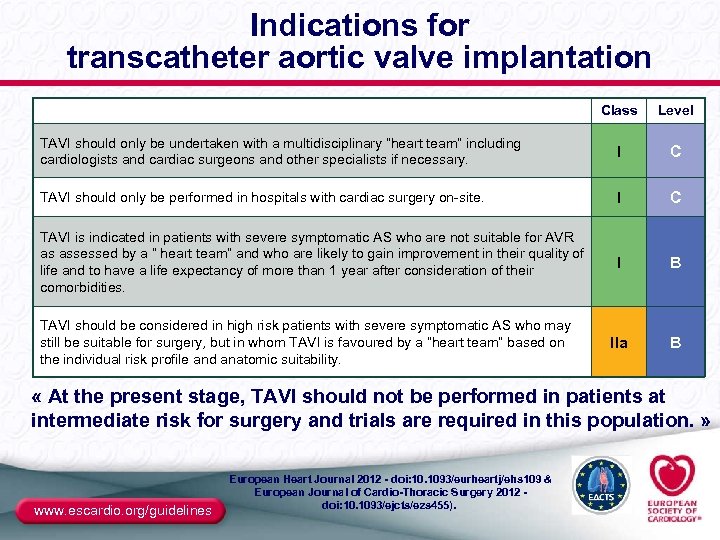
Indications for transcatheter aortic valve implantation Class Level TAVI should only be undertaken with a multidisciplinary “heart team” including cardiologists and cardiac surgeons and other specialists if necessary. I C TAVI should only be performed in hospitals with cardiac surgery on-site. I C TAVI is indicated in patients with severe symptomatic AS who are not suitable for AVR as assessed by a “ heart team” and who are likely to gain improvement in their quality of life and to have a life expectancy of more than 1 year after consideration of their comorbidities. I B IIa B TAVI should be considered in high risk patients with severe symptomatic AS who may still be suitable for surgery, but in whom TAVI is favoured by a “heart team” based on the individual risk profile and anatomic suitability. « At the present stage, TAVI should not be performed in patients at intermediate risk for surgery and trials are required in this population. » www. escardio. org/guidelines European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
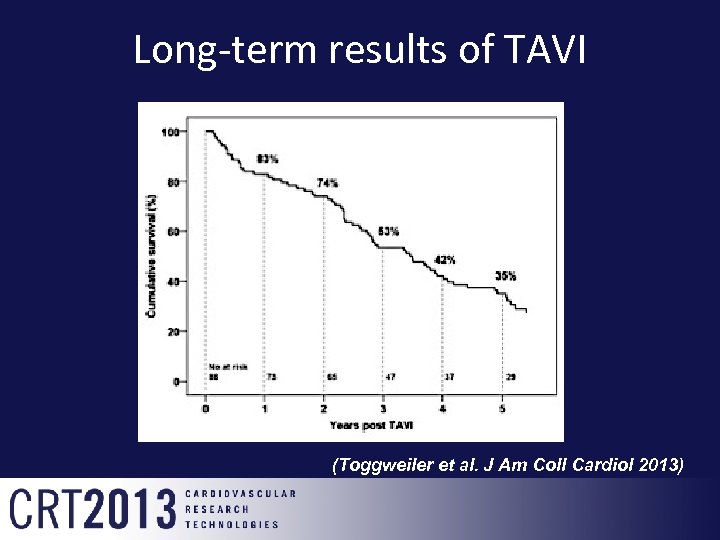
Long-term results of TAVI (Toggweiler et al. J Am Coll Cardiol 2013)

Early calcific degeneration of a Core. Valve bioprosthesis (5 years) • (Ong. Eur Heart J. Online August 2011)
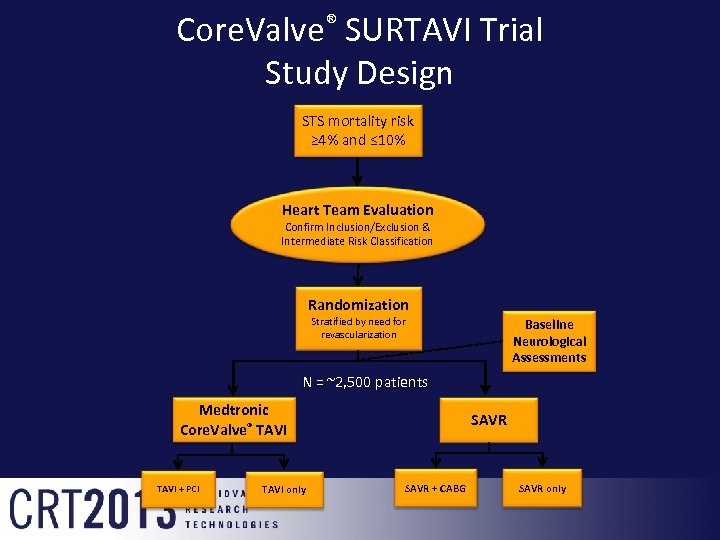
Core. Valve® SURTAVI Trial Study Design STS mortality risk ≥ 4% and ≤ 10% Heart Team Evaluation Confirm Inclusion/Exclusion & Intermediate Risk Classification Randomization Stratified by need for revascularization Baseline Neurological Assessments N = ~2, 500 patients Medtronic Core. Valve® TAVI + PCI TAVI only SAVR + CABG SAVR only
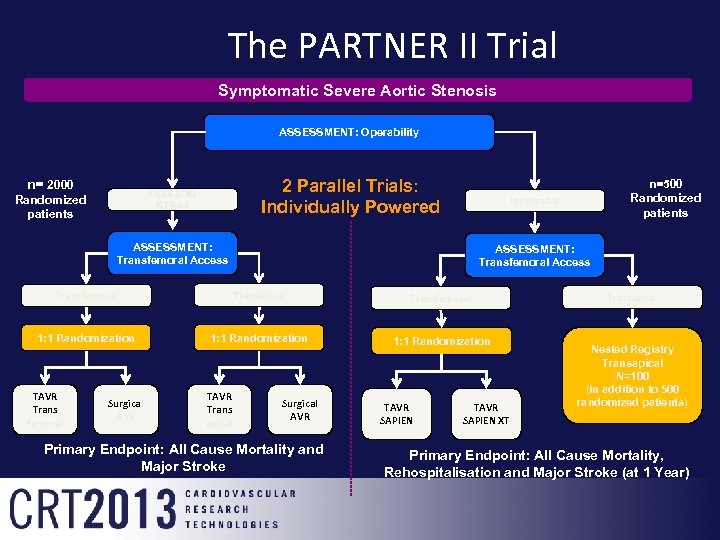
The PARTNER II Trial Symptomatic Severe Aortic Stenosis ASSESSMENT: Operability n= 2000 2 Parallel Trials: Individually Powered Operable STS>4 Randomized patients Inoperable ASSESSMENT: Transfemoral Access Transfemoral Transapical Transfemoral 1: 1 Randomization TAVR Trans femoral Surgical AVR Trans apical n=500 Randomized patients Surgical AVR Primary Endpoint: All Cause Mortality and Major Stroke TAVR SAPIEN XT Transapical Nested Registry Transapical N=100 (in addition to 500 randomized patients) Primary Endpoint: All Cause Mortality, Rehospitalisation and Major Stroke (at 1 Year)
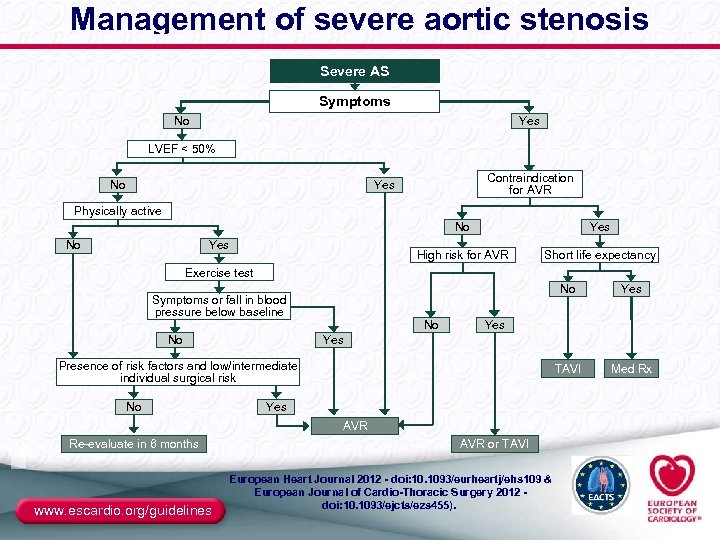
Management of severe aortic stenosis Severe AS Symptoms No Yes LVEF < 50% Contraindication for AVR Yes No Physically active No No High risk for AVR Yes Short life expectancy Exercise test No No No Yes AVR Re-evaluate in 6 months www. escardio. org/guidelines Med Rx Yes Presence of risk factors and low/intermediate individual surgical risk No Yes TAVI Symptoms or fall in blood pressure below baseline AVR or TAVI European Heart Journal 2012 - doi: 10. 1093/eurheartj/ehs 109 & European Journal of Cardio-Thoracic Surgery 2012 - doi: 10. 1093/ejcts/ezs 455).
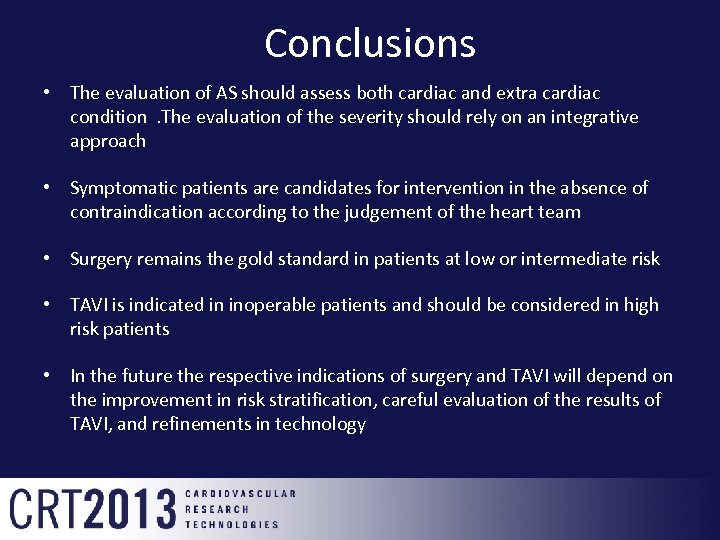
Conclusions • The evaluation of AS should assess both cardiac and extra cardiac condition. The evaluation of the severity should rely on an integrative approach • Symptomatic patients are candidates for intervention in the absence of contraindication according to the judgement of the heart team • Surgery remains the gold standard in patients at low or intermediate risk • TAVI is indicated in inoperable patients and should be considered in high risk patients • In the future the respective indications of surgery and TAVI will depend on the improvement in risk stratification, careful evaluation of the results of TAVI, and refinements in technology
stop
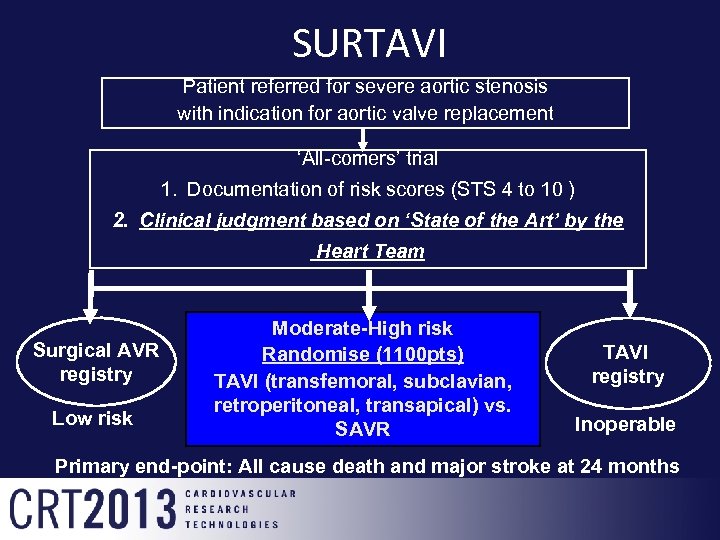
SURTAVI Patient referred for severe aortic stenosis with indication for aortic valve replacement ‘All-comers’ trial 1. Documentation of risk scores (STS 4 to 10 ) 2. Clinical judgment based on ‘State of the Art’ by the Heart Team Surgical AVR registry Low risk Moderate-High risk Randomise (1100 pts) TAVI (transfemoral, subclavian, retroperitoneal, transapical) vs. SAVR TAVI registry Inoperable Primary end-point: All cause death and major stroke at 24 months
e39876c4af4b12d115a54c7a191eff07.ppt