bc0fbba2c7d26b89c62811e80533084b.ppt
- Количество слайдов: 43
 Dual Impact. Merging Quality Improvement and Resident Curriculum Development: A Family Medicine Inpatient Service Model M. Catherine Murphy MD and Todd A. May MD University of California, San Francisco Family Medicine Inpatient Service San Francisco General Hospital
Dual Impact. Merging Quality Improvement and Resident Curriculum Development: A Family Medicine Inpatient Service Model M. Catherine Murphy MD and Todd A. May MD University of California, San Francisco Family Medicine Inpatient Service San Francisco General Hospital
 Learning Objectives • Review basic components of CQI programs • Identify elements for success with a busy service and limited resources • Describe application of CQI methods in a Family Medicine residency service • Discuss the practical translation of CQI data into targeted curricular interventions
Learning Objectives • Review basic components of CQI programs • Identify elements for success with a busy service and limited resources • Describe application of CQI methods in a Family Medicine residency service • Discuss the practical translation of CQI data into targeted curricular interventions
 Our Inpatient Service • Academic, urban, underserved countyoperated facility • 275 bed acute care hospital • Admissions to our service 2005: 1147 2006: 1114 • Adult medical patients as well as pre- and post-operative surgical patients • Ten faculty members serve as attending physicians in 2 -3 week blocks
Our Inpatient Service • Academic, urban, underserved countyoperated facility • 275 bed acute care hospital • Admissions to our service 2005: 1147 2006: 1114 • Adult medical patients as well as pre- and post-operative surgical patients • Ten faculty members serve as attending physicians in 2 -3 week blocks
 Current Inpatient Service Staff • • • 4 2 2 1 1 -2 1 2 1 PGY-1 All housestaff and MD faculty are FPs PGY-2 PGY-3 PGY-4 Chief Resident Med Student III/IV Pharm Student IV Pharm. D Faculty MD Faculty Ph. D Behavioral Science Faculty (one hr/wk)
Current Inpatient Service Staff • • • 4 2 2 1 1 -2 1 2 1 PGY-1 All housestaff and MD faculty are FPs PGY-2 PGY-3 PGY-4 Chief Resident Med Student III/IV Pharm Student IV Pharm. D Faculty MD Faculty Ph. D Behavioral Science Faculty (one hr/wk)
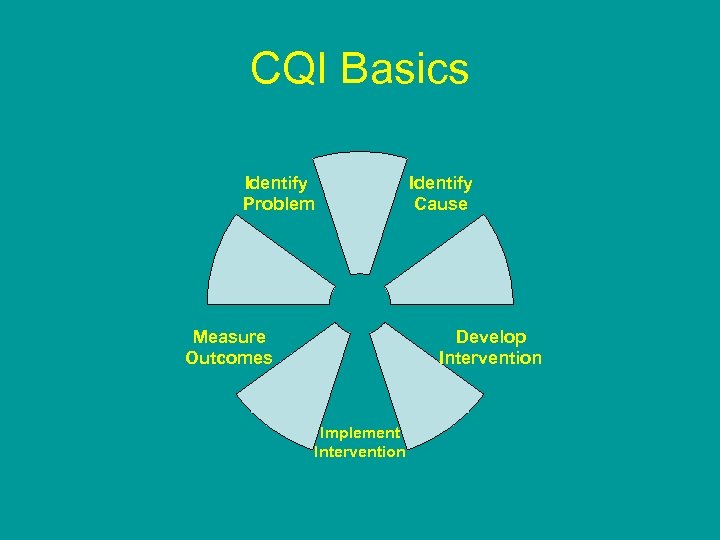 CQI Basics Identify Problem Identify Cause Develop Intervention Measure Outcomes Implement Intervention
CQI Basics Identify Problem Identify Cause Develop Intervention Measure Outcomes Implement Intervention
 CQI Experiences—Old and New Old—Failure/frustration • Attempted basic outcome monitoring • Primarily manifested as ad hoc M&M conferences for really difficult cases • Barriers – Ineffective leadership – No consistent oversight/championing on service – Low priority New— 2 dynamic Chief Residents • Finally a critical mass of commitment • Consistent promotion/championing, development
CQI Experiences—Old and New Old—Failure/frustration • Attempted basic outcome monitoring • Primarily manifested as ad hoc M&M conferences for really difficult cases • Barriers – Ineffective leadership – No consistent oversight/championing on service – Low priority New— 2 dynamic Chief Residents • Finally a critical mass of commitment • Consistent promotion/championing, development
 Why Initiate a CQI Program? Our Goals • To improve patient care • To improve resident education • To gain a more nuanced understanding of the trends on our service
Why Initiate a CQI Program? Our Goals • To improve patient care • To improve resident education • To gain a more nuanced understanding of the trends on our service
 Starting Point: Defining Our Areas of Interest Deaths: – Anticipated deaths due to terminal chronic diseases (cancer, ESLD, COPD, dementia) versus unanticipated deaths – Potentially preventable? – Importance of communication with PCPs
Starting Point: Defining Our Areas of Interest Deaths: – Anticipated deaths due to terminal chronic diseases (cancer, ESLD, COPD, dementia) versus unanticipated deaths – Potentially preventable? – Importance of communication with PCPs
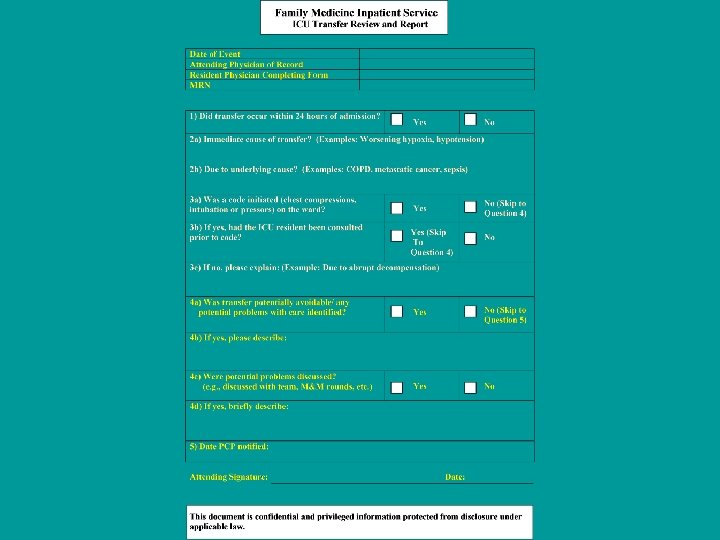
 Starting Point: Defining Our Areas of Interest ICU Transfers: – Which illnesses and organ systems are the causes of our transfers? – Potentially avoidable? – Communicating with PCPs
Starting Point: Defining Our Areas of Interest ICU Transfers: – Which illnesses and organ systems are the causes of our transfers? – Potentially avoidable? – Communicating with PCPs
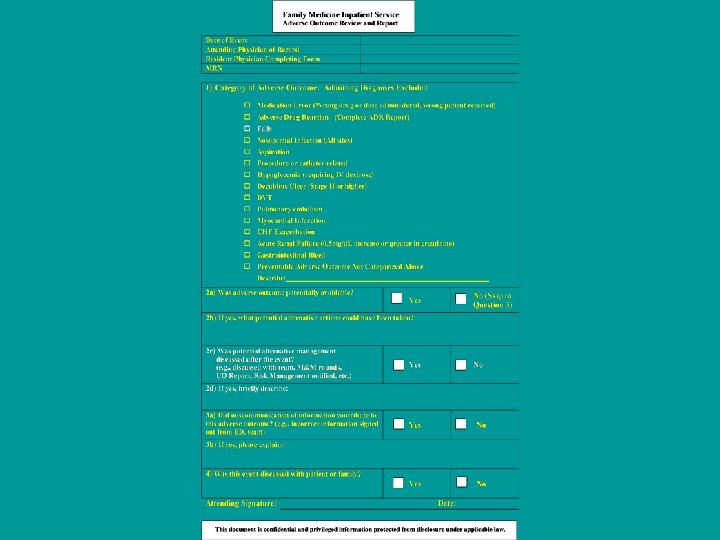
 Starting Point: Defining Our Areas of Interest Adverse Events: – Which events? – Are the AEs on our service possibly preventable? – Are we communicating with patients and families about these events?
Starting Point: Defining Our Areas of Interest Adverse Events: – Which events? – Are the AEs on our service possibly preventable? – Are we communicating with patients and families about these events?
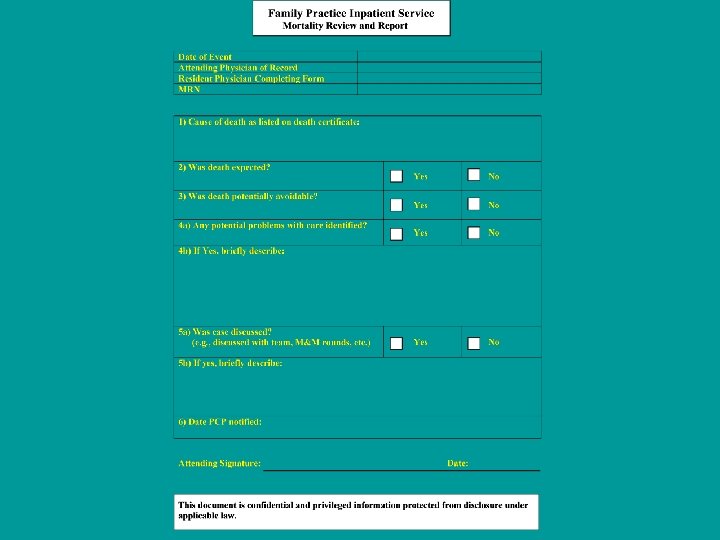
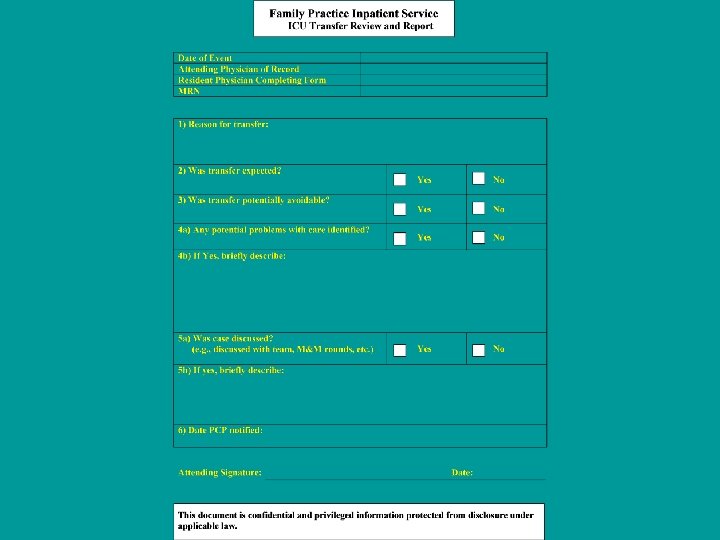
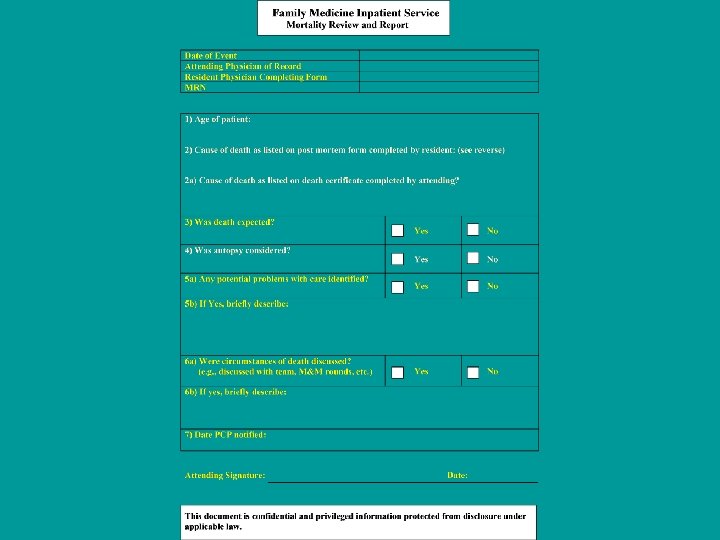
 Creating Our Data Collection Tools • What: A separate form created for each target area of interest – Deaths – ICU transfers – Select adverse events • Priorities – Keep it simple, minimize barriers – Make it useful and educational
Creating Our Data Collection Tools • What: A separate form created for each target area of interest – Deaths – ICU transfers – Select adverse events • Priorities – Keep it simple, minimize barriers – Make it useful and educational
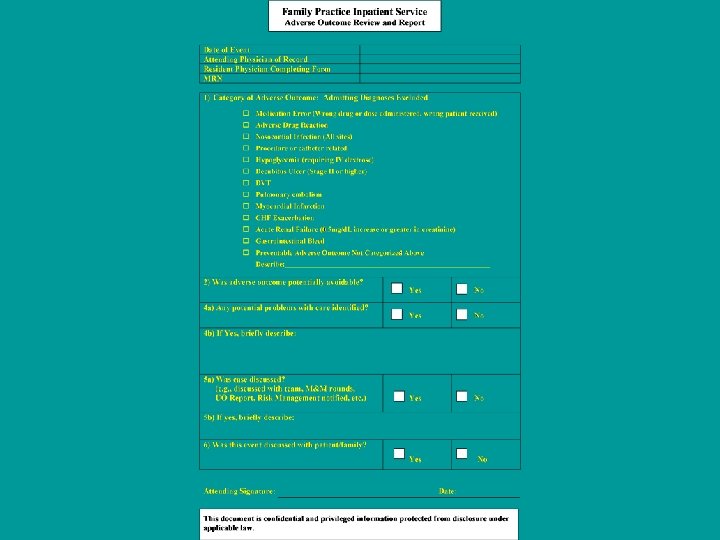
 Adverse Events 1) Category of Adverse Outcome: Admitting Diagnoses Excluded q. Medication Error (Wrong drug or dose administered, wrong patient) q. Adverse Drug Reaction q. Nosocomial Infection (All sites) q. Procedure or catheter related q. Hypoglycemia (requiring IV dextrose) q. Decubitus Ulcer (Stage II or higher) q. DVT q. Pulmonary embolism q. Myocardial Infarction q. CHF Exacerbation q. Acute Renal Failure (0. 5 mg/d. L or greater increase in creatinine) q. Gastrointestinal Bleed q. Preventable Adverse Outcome Not Categorized Above Describe:
Adverse Events 1) Category of Adverse Outcome: Admitting Diagnoses Excluded q. Medication Error (Wrong drug or dose administered, wrong patient) q. Adverse Drug Reaction q. Nosocomial Infection (All sites) q. Procedure or catheter related q. Hypoglycemia (requiring IV dextrose) q. Decubitus Ulcer (Stage II or higher) q. DVT q. Pulmonary embolism q. Myocardial Infarction q. CHF Exacerbation q. Acute Renal Failure (0. 5 mg/d. L or greater increase in creatinine) q. Gastrointestinal Bleed q. Preventable Adverse Outcome Not Categorized Above Describe:
 Defining Our Process • Collect data—reporting component • Immediate case-based feedback/teaching opportunity • Review cumulative data to identify practice trends • Generate curricular interventions based on issues identified
Defining Our Process • Collect data—reporting component • Immediate case-based feedback/teaching opportunity • Review cumulative data to identify practice trends • Generate curricular interventions based on issues identified
 Revising Our Data Collection • CQI Pilot – Assessed after 3 months – Reviewed data and data collection tools • Conclusions – Gained more information about our practice – Some questions were not addressed – Generated new questions
Revising Our Data Collection • CQI Pilot – Assessed after 3 months – Reviewed data and data collection tools • Conclusions – Gained more information about our practice – Some questions were not addressed – Generated new questions
 Refining Our Areas of Interest Deaths: – Anticipated deaths due to terminal chronic diseases (cancer, ESLD, COPD, dementia) versus unanticipated deaths – Potentially preventable? – Age of patient relevant (new) – Low rate of autopsy utilization (new) – How well are we educating residents about death certificates? (new) – Importance of communication with PCPs
Refining Our Areas of Interest Deaths: – Anticipated deaths due to terminal chronic diseases (cancer, ESLD, COPD, dementia) versus unanticipated deaths – Potentially preventable? – Age of patient relevant (new) – Low rate of autopsy utilization (new) – How well are we educating residents about death certificates? (new) – Importance of communication with PCPs
 Refining Our Areas of Interest ICU Transfers: – Which illnesses and organ systems are the causes of our transfers? – Define immediate and underlying cause (new) – When in the hospital course are transfers occurring (ED triage issues)? (new) – How well are we communicating with ICU service about our critically ill patients? – Potentially avoidable? – Communicating with PCPs
Refining Our Areas of Interest ICU Transfers: – Which illnesses and organ systems are the causes of our transfers? – Define immediate and underlying cause (new) – When in the hospital course are transfers occurring (ED triage issues)? (new) – How well are we communicating with ICU service about our critically ill patients? – Potentially avoidable? – Communicating with PCPs
 Refining Our Areas of Interest Adverse Events: – Which events? Added falls – Are the AEs on our service possibly preventable? – Are we communicating with patients and families about these events? – Role of miscommunication of information (new)
Refining Our Areas of Interest Adverse Events: – Which events? Added falls – Are the AEs on our service possibly preventable? – Are we communicating with patients and families about these events? – Role of miscommunication of information (new)
 2005 -2007 Summary Data
2005 -2007 Summary Data
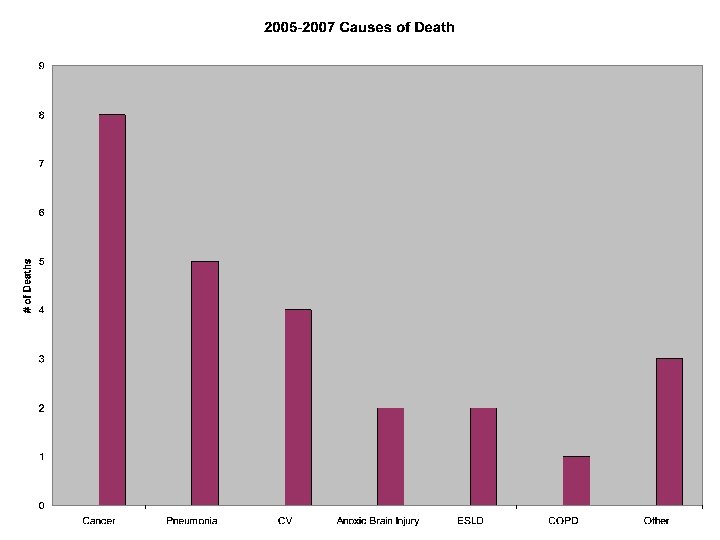
 Mortality Summary • Relatively few deaths on service • Predominately end result of chronic illnesses • More unexpected deaths than anticipated: 6/25 (24%) • Very few deaths with potential problems with care identified (12%) • Limited utility for autopsy?
Mortality Summary • Relatively few deaths on service • Predominately end result of chronic illnesses • More unexpected deaths than anticipated: 6/25 (24%) • Very few deaths with potential problems with care identified (12%) • Limited utility for autopsy?
 ICU Transfers • 76 ICU transfers in 2 years • 17 (22%) potentially avoidable • 13/34 (38%) within 24 hours of admission (data for 06 -07 only) • 14/76 (18%) codes performed prior to transfer • 8/14 (57%) of coded patients discussed with ICU prior to code Opportunities for improvement
ICU Transfers • 76 ICU transfers in 2 years • 17 (22%) potentially avoidable • 13/34 (38%) within 24 hours of admission (data for 06 -07 only) • 14/76 (18%) codes performed prior to transfer • 8/14 (57%) of coded patients discussed with ICU prior to code Opportunities for improvement
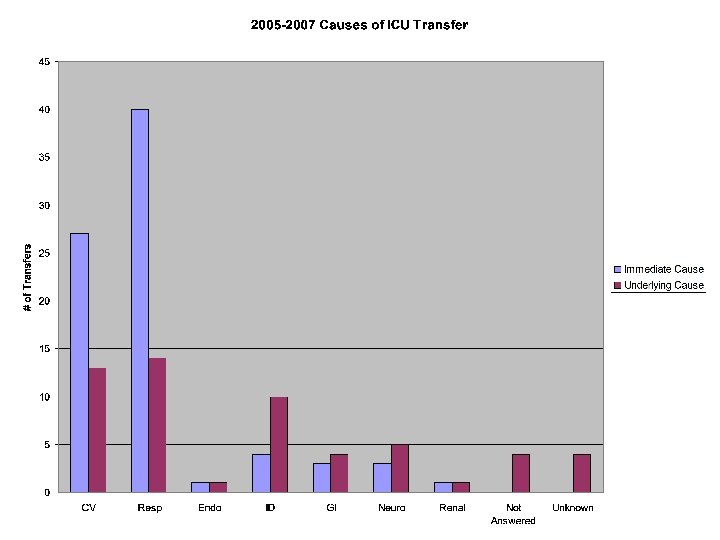
 ICU Transfers • Respiratory and cardiovascular decompensation are most common causes for transfer • Increased attention and education about the initial triage of patients to the appropriate level of care/supervision is required • Limited number of codes performed and appropriate communication with ICU team taking place
ICU Transfers • Respiratory and cardiovascular decompensation are most common causes for transfer • Increased attention and education about the initial triage of patients to the appropriate level of care/supervision is required • Limited number of codes performed and appropriate communication with ICU team taking place
 Adverse Events 05 -07 • 117 total AEs reported • 86 (74%) potentially avoidable – Substantial opportunity for improvement – Possible negative reporting bias • 96 (82%) discussed with patient/family
Adverse Events 05 -07 • 117 total AEs reported • 86 (74%) potentially avoidable – Substantial opportunity for improvement – Possible negative reporting bias • 96 (82%) discussed with patient/family
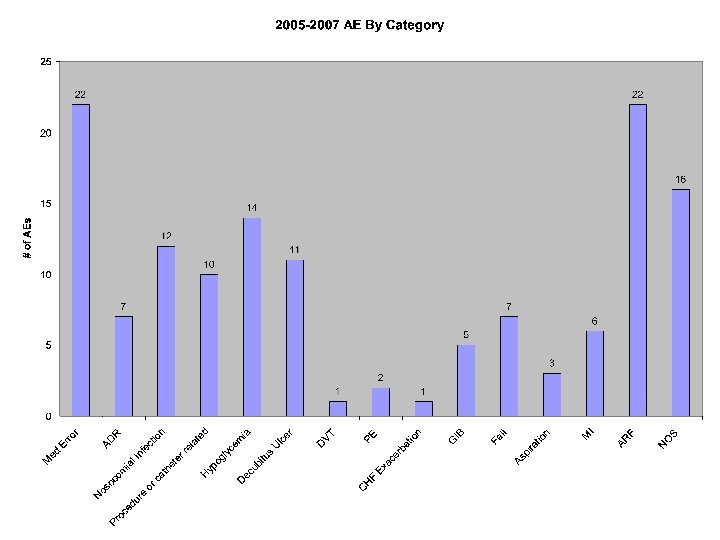
 Adverse Events 05 -07 Most common: • • • ARF Medication errors Hypoglycemia Nosocomial Procedure/catheter 19% 12% 10% 8%
Adverse Events 05 -07 Most common: • • • ARF Medication errors Hypoglycemia Nosocomial Procedure/catheter 19% 12% 10% 8%
 Next Step: Using Data for Curriculum Development In reviewing our 2005 -2006 data, we identified several important topics that were not part of our formal inpatient curriculum: – Decubitus Ulcer prevention – Death certificate completion
Next Step: Using Data for Curriculum Development In reviewing our 2005 -2006 data, we identified several important topics that were not part of our formal inpatient curriculum: – Decubitus Ulcer prevention – Death certificate completion
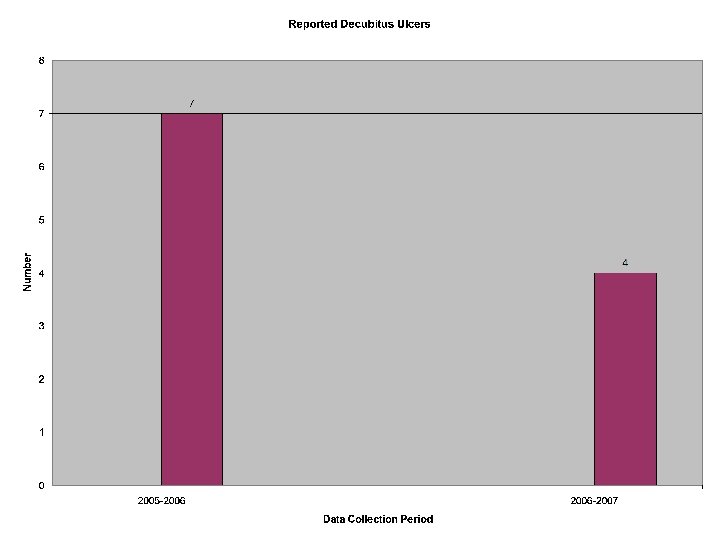
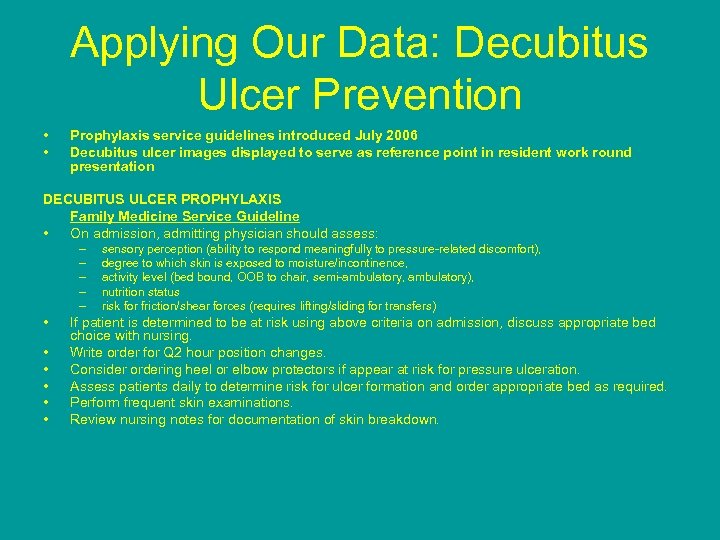 Applying Our Data: Decubitus Ulcer Prevention • • Prophylaxis service guidelines introduced July 2006 Decubitus ulcer images displayed to serve as reference point in resident work round presentation DECUBITUS ULCER PROPHYLAXIS Family Medicine Service Guideline • On admission, admitting physician should assess: – – – • • • sensory perception (ability to respond meaningfully to pressure-related discomfort), degree to which skin is exposed to moisture/incontinence, activity level (bed bound, OOB to chair, semi-ambulatory, ambulatory), nutrition status risk for friction/shear forces (requires lifting/sliding for transfers) If patient is determined to be at risk using above criteria on admission, discuss appropriate bed choice with nursing. Write order for Q 2 hour position changes. Consider ordering heel or elbow protectors if appear at risk for pressure ulceration. Assess patients daily to determine risk for ulcer formation and order appropriate bed as required. Perform frequent skin examinations. Review nursing notes for documentation of skin breakdown.
Applying Our Data: Decubitus Ulcer Prevention • • Prophylaxis service guidelines introduced July 2006 Decubitus ulcer images displayed to serve as reference point in resident work round presentation DECUBITUS ULCER PROPHYLAXIS Family Medicine Service Guideline • On admission, admitting physician should assess: – – – • • • sensory perception (ability to respond meaningfully to pressure-related discomfort), degree to which skin is exposed to moisture/incontinence, activity level (bed bound, OOB to chair, semi-ambulatory, ambulatory), nutrition status risk for friction/shear forces (requires lifting/sliding for transfers) If patient is determined to be at risk using above criteria on admission, discuss appropriate bed choice with nursing. Write order for Q 2 hour position changes. Consider ordering heel or elbow protectors if appear at risk for pressure ulceration. Assess patients daily to determine risk for ulcer formation and order appropriate bed as required. Perform frequent skin examinations. Review nursing notes for documentation of skin breakdown.
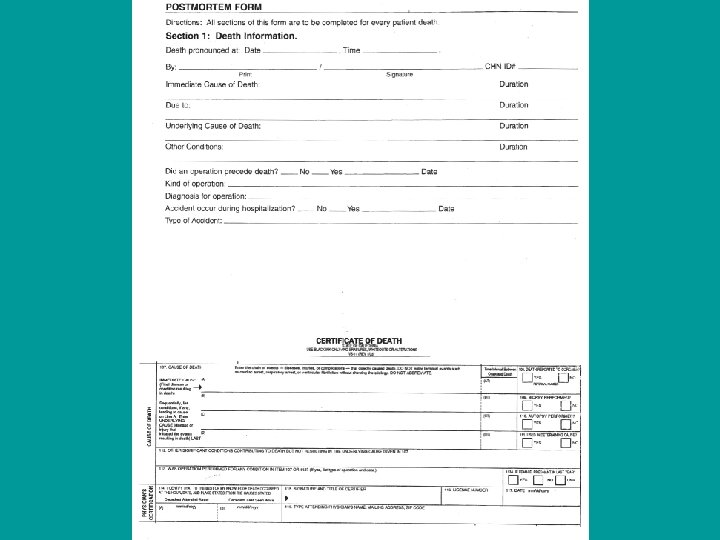
 Applying Our Data: Death Certificate Curriculum • 2005 -2006 data revealed poor accuracy in completing death certificate worksheets by our residents – Respiratory failure or arrest listed as cause of death on 25% of forms completed by residents • We introduced a 20 minute case-based presentation on death certificate completion in our inpatient curriculum series
Applying Our Data: Death Certificate Curriculum • 2005 -2006 data revealed poor accuracy in completing death certificate worksheets by our residents – Respiratory failure or arrest listed as cause of death on 25% of forms completed by residents • We introduced a 20 minute case-based presentation on death certificate completion in our inpatient curriculum series
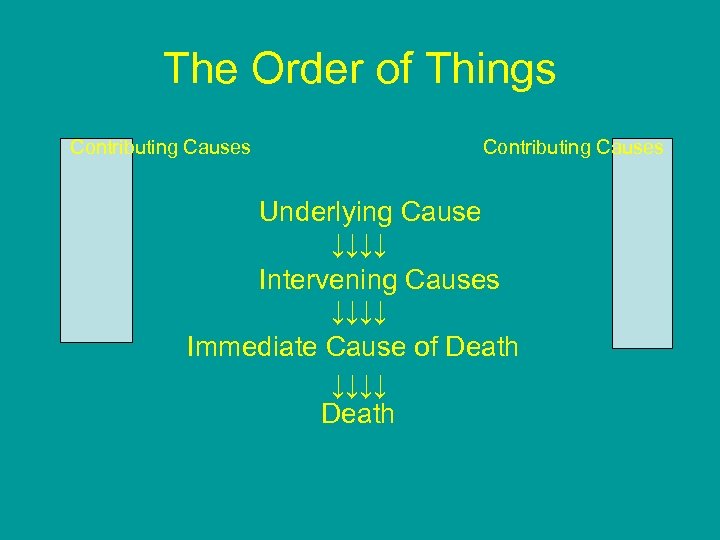 The Order of Things Contributing Causes Underlying Cause ↓↓↓↓ Intervening Causes ↓↓↓↓ Immediate Cause of Death ↓↓↓↓ Death
The Order of Things Contributing Causes Underlying Cause ↓↓↓↓ Intervening Causes ↓↓↓↓ Immediate Cause of Death ↓↓↓↓ Death
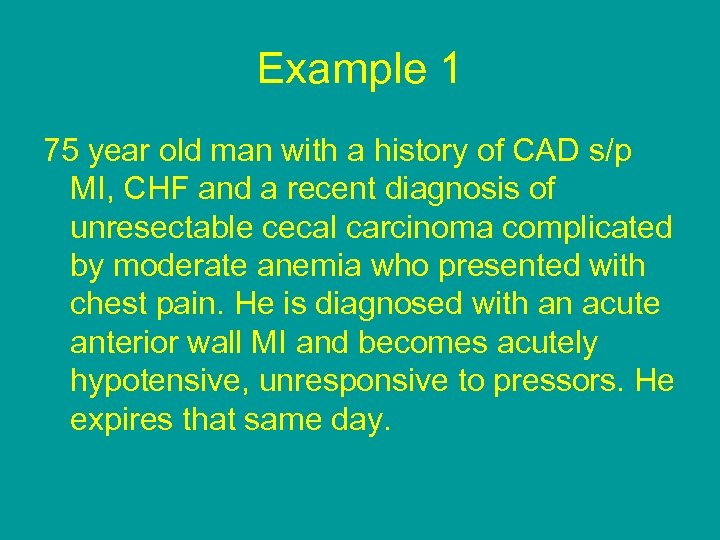 Example 1 75 year old man with a history of CAD s/p MI, CHF and a recent diagnosis of unresectable cecal carcinoma complicated by moderate anemia who presented with chest pain. He is diagnosed with an acute anterior wall MI and becomes acutely hypotensive, unresponsive to pressors. He expires that same day.
Example 1 75 year old man with a history of CAD s/p MI, CHF and a recent diagnosis of unresectable cecal carcinoma complicated by moderate anemia who presented with chest pain. He is diagnosed with an acute anterior wall MI and becomes acutely hypotensive, unresponsive to pressors. He expires that same day.
 Limitations of Our Project • Small numbers • Under-reporting and variable adherence – Uncertain true incidence of events over time – Limits assessment of trends and effectiveness of interventions • Limited resources—must rely on physician staff and manual data collection • Self-evaluation by team rather than independent review (potential bias)
Limitations of Our Project • Small numbers • Under-reporting and variable adherence – Uncertain true incidence of events over time – Limits assessment of trends and effectiveness of interventions • Limited resources—must rely on physician staff and manual data collection • Self-evaluation by team rather than independent review (potential bias)
 Future Directions • Next curricular interventions: – Hypoglycemia (in progress) – Procedure/catheter – Medication errors • Sustainability: – Major challenge—constant tilling and prodding – Role of Chief Residents • Maintaining our gains: – Continuing education on the inpatient service – Monitoring results
Future Directions • Next curricular interventions: – Hypoglycemia (in progress) – Procedure/catheter – Medication errors • Sustainability: – Major challenge—constant tilling and prodding – Role of Chief Residents • Maintaining our gains: – Continuing education on the inpatient service – Monitoring results
 Where to Find Our Forms http: //intmedschool. ucsf. edu/sfghres/ info_residents. aspx
Where to Find Our Forms http: //intmedschool. ucsf. edu/sfghres/ info_residents. aspx
 Faculty Opportunity UCSF/SFGH Core Faculty Position • Inpatient/Urgent Care focus – Curriculum development – Practice guideline development – CQI programs • Ample resident and student teaching – Hospital, clinic, seminars, small groups • Continuity practice • OB practice optional • Scholarly activities supported/encouraged
Faculty Opportunity UCSF/SFGH Core Faculty Position • Inpatient/Urgent Care focus – Curriculum development – Practice guideline development – CQI programs • Ample resident and student teaching – Hospital, clinic, seminars, small groups • Continuity practice • OB practice optional • Scholarly activities supported/encouraged


