0447f0a1ff5a9b1d1dd90c1528da8e65.ppt
- Количество слайдов: 41
Drugs of Toxicology #7 Abuse Huffer Huge thanks to Dr. Sarah Mc. Pherson

Parking Lot
Objectives 1. Understand Demonstrate the Management of an Agitated Patient 1. 2. 3. 4. 2. Review Toxin-Induced Seizures 1. 2. 3. Rapid Assessment Initial Sedation DDx Complications Pathophysiology Management Manage a Patient with an Opiate Toxidrome
Case 1 30 M. Behaving “oddly” Had been out partying with friends – they’re pretty sure he took “something” they didn’t Seems agitated and restless Pt (and his friends) are intoxicated and their contributions to the history are mostly useless
Case 1 On Exam: 37. 8°C, 108, 138/82, 20, 96% Glucose 6. 7 Pupils: large, reactive Skin: diaphoretic Resp: exp. Wheeze
Sympathomimetics Cocaine: Naturally occurring, plant-derived alkaloid Amphetamines: Stimulant agents originally designed as decongestants and dietary aids Popular as recreational drugs around the middle of the 20 th century Collectively, Cocaine, Amphetamines and derivatives are called sympathomimetics As a class, these agents cause CNS stimulation and a cascade of physiologic effects

Anti. Sympathominergic?
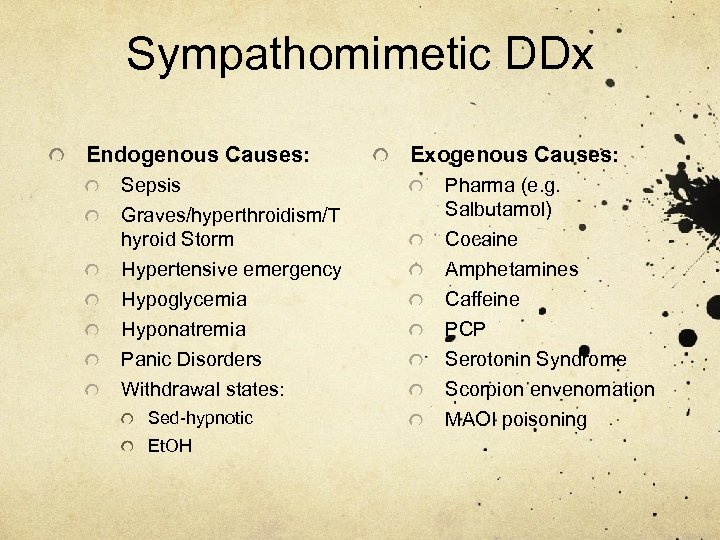
Sympathomimetic DDx Endogenous Causes: Sepsis Graves/hyperthroidism/T hyroid Storm Hypertensive emergency Hypoglycemia Hyponatremia Panic Disorders Withdrawal states: Sed-hypnotic Et. OH Exogenous Causes: Pharma (e. g. Salbutamol) Cocaine Amphetamines Caffeine PCP Serotonin Syndrome Scorpion envenomation MAOI poisoning
Pathophysiology 1. Direct action at the α and β adrenergic receptors 2. Indirect release of Norepi from presynaptic cytoplasm 3. Prevention of pre-synaptic reuptake of Norepi 4. Prevention of Norepi metabolism (MAO- I)
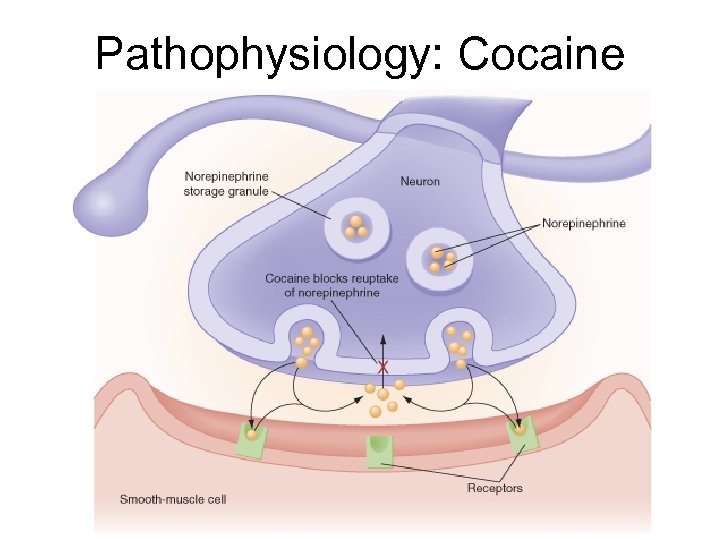
Pathophysiology: Cocaine
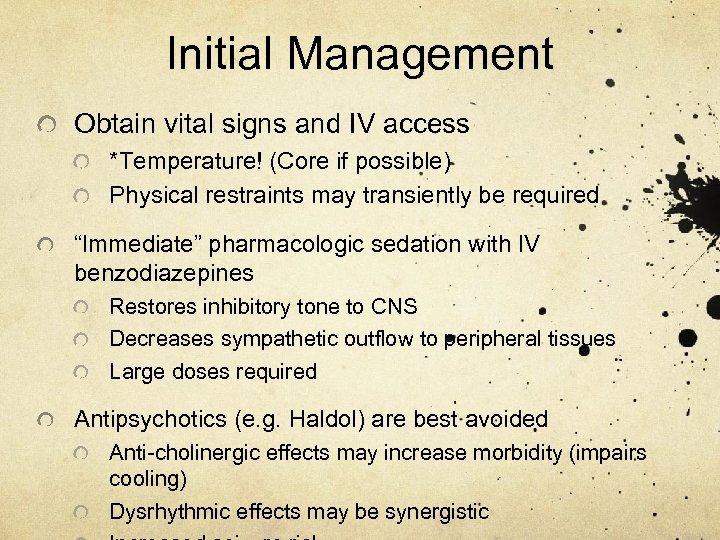
Initial Management Obtain vital signs and IV access *Temperature! (Core if possible) Physical restraints may transiently be required “Immediate” pharmacologic sedation with IV benzodiazepines Restores inhibitory tone to CNS Decreases sympathetic outflow to peripheral tissues Large doses required Antipsychotics (e. g. Haldol) are best avoided Anti-cholinergic effects may increase morbidity (impairs cooling) Dysrhythmic effects may be synergistic
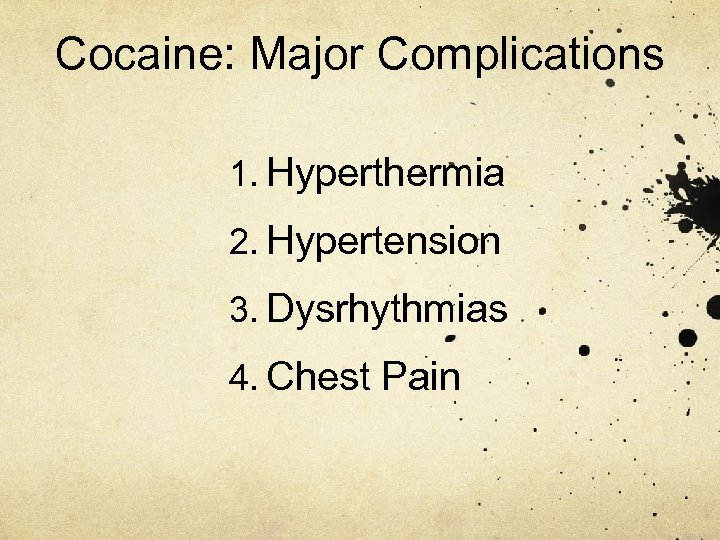
Cocaine: Major Complications 1. Hyperthermia 2. Hypertension 3. Dysrhythmias 4. Chest Pain
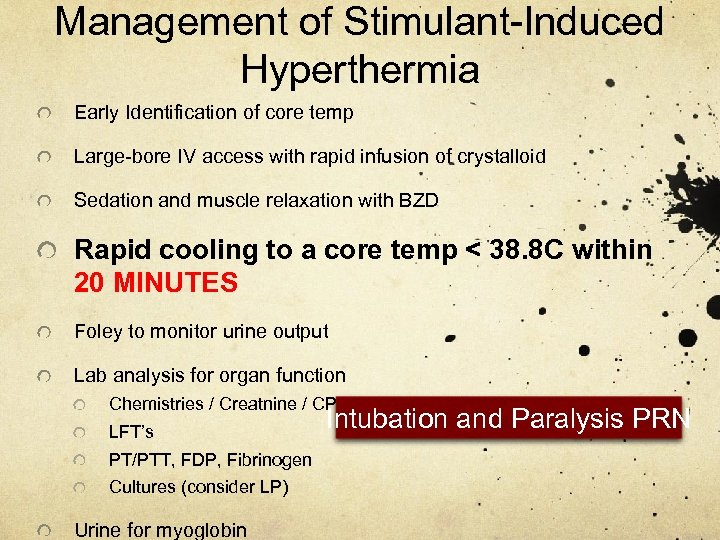
Management of Stimulant-Induced Hyperthermia Early Identification of core temp Large-bore IV access with rapid infusion of crystalloid Sedation and muscle relaxation with BZD Rapid cooling to a core temp < 38. 8 C within 20 MINUTES Foley to monitor urine output Lab analysis for organ function Chemistries / Creatnine / CPK LFT’s PT/PTT, FDP, Fibrinogen Cultures (consider LP) Urine for myoglobin Intubation and Paralysis PRN
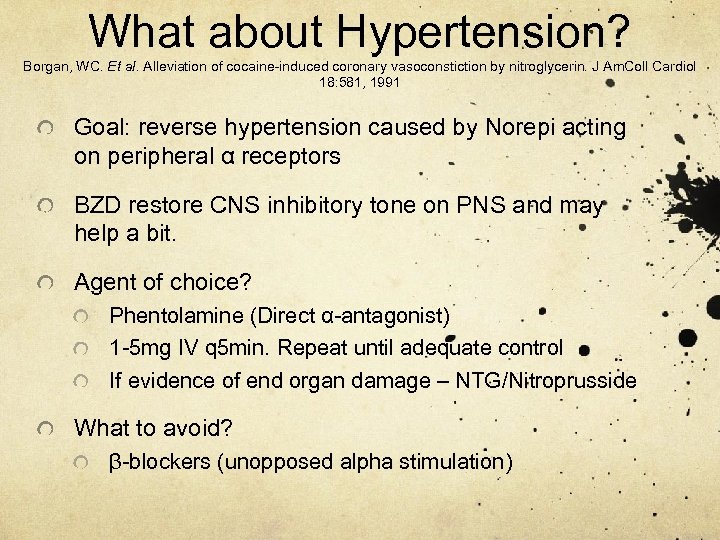
What about Hypertension? Borgan, WC. Et al. Alleviation of cocaine-induced coronary vasoconstiction by nitroglycerin. J Am. Coll Cardiol 18: 581, 1991 Goal: reverse hypertension caused by Norepi acting on peripheral α receptors BZD restore CNS inhibitory tone on PNS and may help a bit. Agent of choice? Phentolamine (Direct α-antagonist) 1 -5 mg IV q 5 min. Repeat until adequate control If evidence of end organ damage – NTG/Nitroprusside What to avoid? β-blockers (unopposed alpha stimulation)
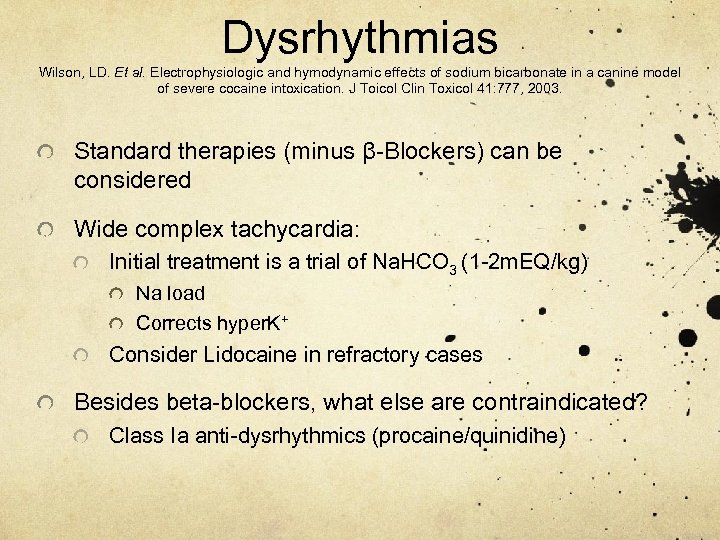
Dysrhythmias Wilson, LD. Et al. Electrophysiologic and hymodynamic effects of sodium bicarbonate in a canine model of severe cocaine intoxication. J Toicol Clin Toxicol 41: 777, 2003. Standard therapies (minus β-Blockers) can be considered Wide complex tachycardia: Initial treatment is a trial of Na. HCO 3 (1 -2 m. EQ/kg) Na load Corrects hyper. K+ Consider Lidocaine in refractory cases Besides beta-blockers, what else are contraindicated? Class Ia anti-dysrhythmics (procaine/quinidine)
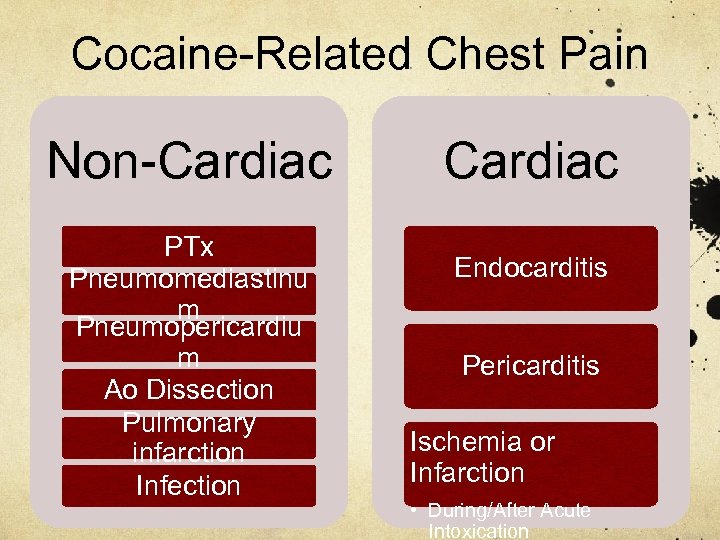
Cocaine-Related Chest Pain Non-Cardiac PTx Pneumomediastinu m Pneumopericardiu m Ao Dissection Pulmonary infarction Infection Cardiac Endocarditis Pericarditis Ischemia or Infarction • During/After Acute Intoxication
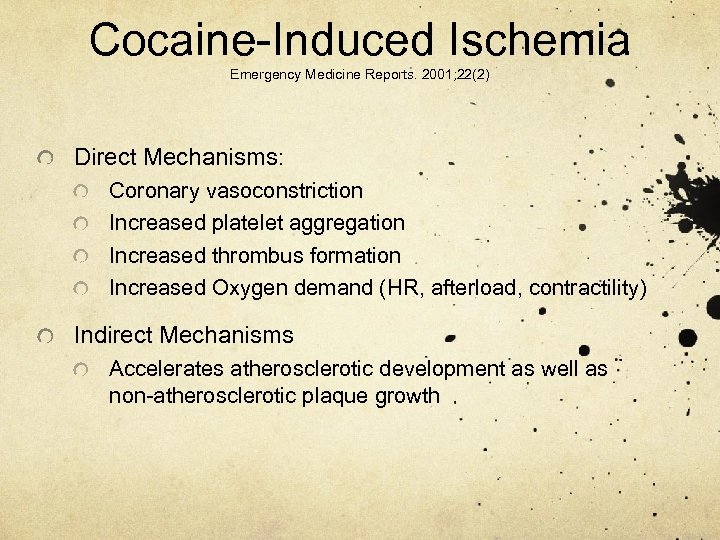
Cocaine-Induced Ischemia Emergency Medicine Reports. 2001; 22(2) Direct Mechanisms: Coronary vasoconstriction Increased platelet aggregation Increased thrombus formation Increased Oxygen demand (HR, afterload, contractility) Indirect Mechanisms Accelerates atherosclerotic development as well as non-atherosclerotic plaque growth
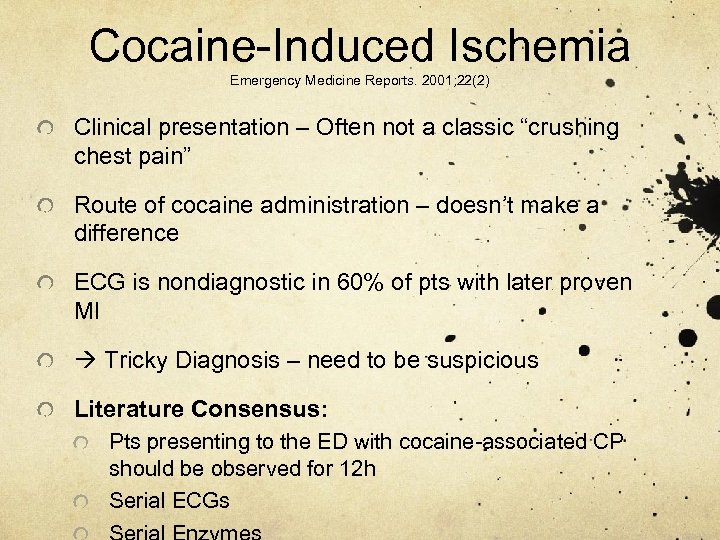
Cocaine-Induced Ischemia Emergency Medicine Reports. 2001; 22(2) Clinical presentation – Often not a classic “crushing chest pain” Route of cocaine administration – doesn’t make a difference ECG is nondiagnostic in 60% of pts with later proven MI Tricky Diagnosis – need to be suspicious Literature Consensus: Pts presenting to the ED with cocaine-associated CP should be observed for 12 h Serial ECGs
Benzos, NTG, or both? Baumann et al. Acad Emerg Med 2000; 7: 878 -885 RCT of diazepam, NTG, or both in patients presenting with chest pain who had used cocaine within past 24 hours Measured time to relief of CP (using a VAS) as well as change in hemodynamic parameters by transthoracic scanning. P set at 0. 007 because of multiple comparisons 40 patients (diazepam = 12, NTG = 13, both = 15) (underpowered) No difference between groups in terms of time to CP improvement or hemodynamic parameters
Benzos, NTG, or both? Honderick et al. Am J Emerg Med 2003; 21: 39 -42 RCT of NTG vs. NTG and lorazepam in patients presenting with chest pain who had used cocaine within past 72 hours Measured time to relief of CP using an ordinal pain scale 27 patients (15 NTG, 12 both) Significant improvement in pain scores in the LOR + NTG group vs. NTG alone
Cocaine-Induced Ischemia: ED Treatment ABC’s Nitroglycerin Benzodiazepines No beta blockers Aspirin/Heparin no studies to support efficacy but their use is generally accepted if no contraindications
Lytics or cath lab? Low mortality rate from cocaine-associated MI (close to 0%) Risk of treating a false positive ECG with lytics Thrombosis may not be the cause of the MI Patients may present with seizures, head trauma, or hypertension. If BP severe (> 180/110) and unable to control contraindication to lytics THEREFORE, CATH LAB PREFERABLE IF AVAILABLE If no cath lab available and objective evidence of acute transmural MI (ECG and positive
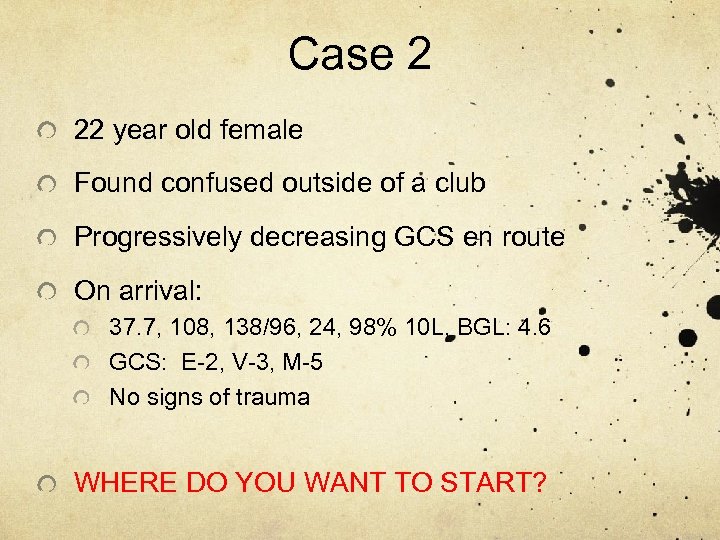
Case 2 22 year old female Found confused outside of a club Progressively decreasing GCS en route On arrival: 37. 7, 108, 138/96, 24, 98% 10 L, BGL: 4. 6 GCS: E-2, V-3, M-5 No signs of trauma WHERE DO YOU WANT TO START?
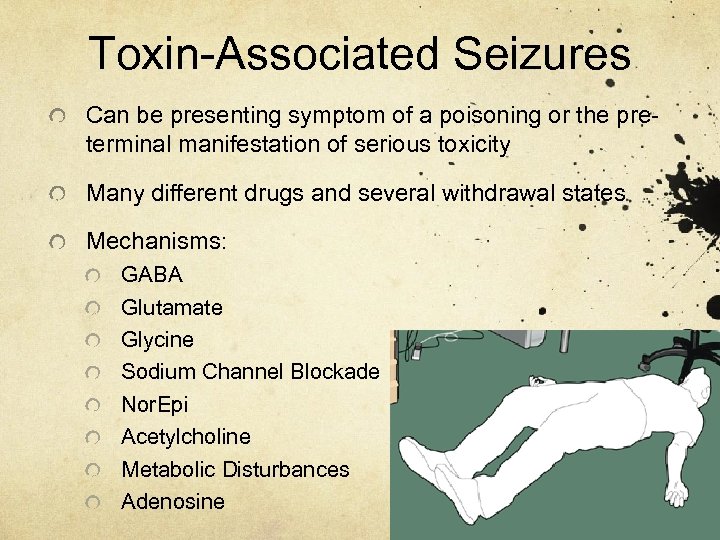
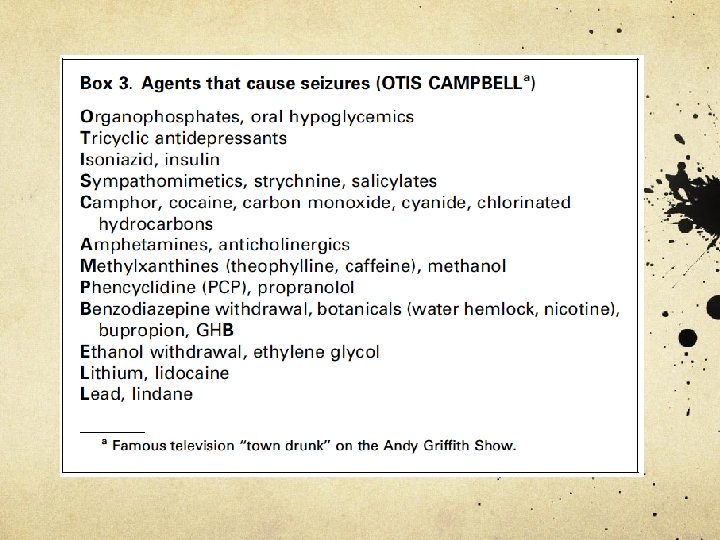
Toxin-Associated Seizures Can be presenting symptom of a poisoning or the preterminal manifestation of serious toxicity Many different drugs and several withdrawal states Mechanisms: GABA Glutamate Glycine Sodium Channel Blockade Nor. Epi Acetylcholine Metabolic Disturbances Adenosine
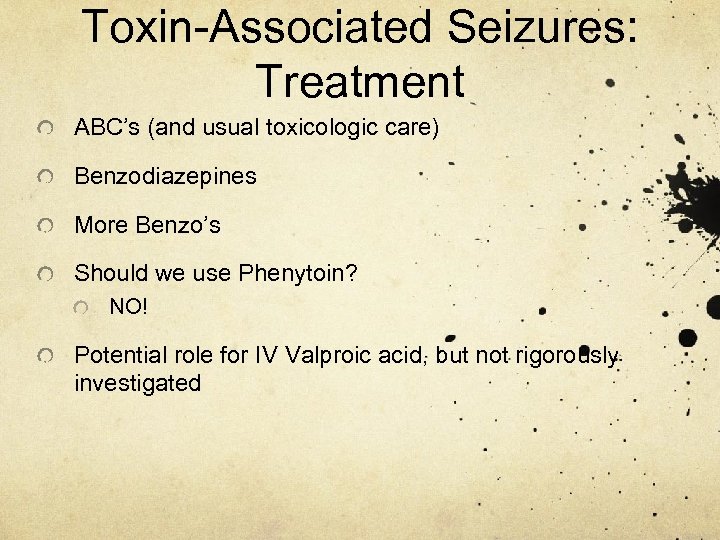
Toxin-Associated Seizures: Treatment ABC’s (and usual toxicologic care) Benzodiazepines More Benzo’s Should we use Phenytoin? NO! Potential role for IV Valproic acid, but not rigorously investigated
Pathophysiology: Amphetamines increase circulating norepinephrine, dopamine, and serotonin by: Increasing release of Norepi from nerve terminals Inhibiting NE reuptake into presynaptic nerve terminals This is minimal compared to cocaine Preventing NE breakdown
Methamphetamine Abused by all routes (PO, IV, inhaled) Peak 30 mins via IV, 2 -3 hrs po Half life 10 -20 hours Duration of action > 24 hours Compared to cocaine, methamphetamine Is easier to make and buy Is cheaper Lasts longer (> 24 hours vs. 6 hours)
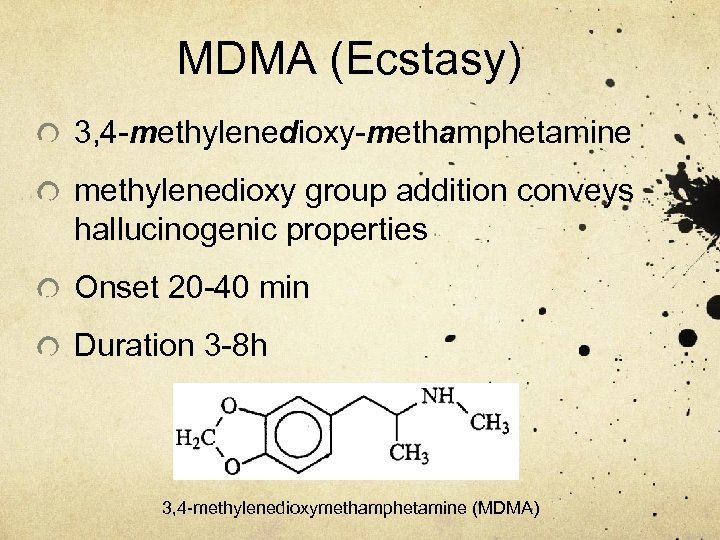
MDMA (Ecstasy) 3, 4 -methylenedioxy-methamphetamine methylenedioxy group addition conveys hallucinogenic properties Onset 20 -40 min Duration 3 -8 h 3, 4 -methylenedioxymethamphetamine (MDMA)
Guess what I’m thinking: MDMA Name a potentially life-threatening electrolyte disturbance precipitated by MDMA intoxication. HYPONATREMIA Treatment? FLUID RESTRICTION (UNLESS SEIZING) HYPERTONIC SALINE SEE JAY’S LECTURE FROM THIS SPRING 2009!
Case 3 You’re on your ICU rotation and hear your first code blue called! Sweet – you’re the boss! Wait…Yikes! You’re the boss! 24 F on the antepartum ward, not responsive. Nurse came in for vital check and found her with a GCS of 7, resp rate of 6/min and sats of 86%. What do you do?
Case 3 You successfully intubate the patient and bring her down to the ICU to examine her. 37. 3 C, 88, 6, 98/64, 98% on 50%FIO 2 AC BGL=6. 3 Pupils 2 mm, GCS E 1, V 2 M 4 = 7 Skin: pink, moist Chest clear Peripherally – nil
Opiods Term applies to all agents with morphine-like actions As a class have been around for thousands of years Heroin first synthesized from morphine in 1874 Pharmacologic actions involve the GI, CVS, Pulm, and CNS systems 3 receptors: OP 1 (formally called delta) OP 2 (kappa) OP 3 (mu)
Opiods - Pathophysiology Can be taken, orally, nasally or by injection (venous, IM or SC) Avg. peak effects: 1 -2 h (oral) 90 min (SC) 30 min (IM) 10 min (IV) Large Volume of distribution Blood levels are pretty much useless Dialysis generally not helpful
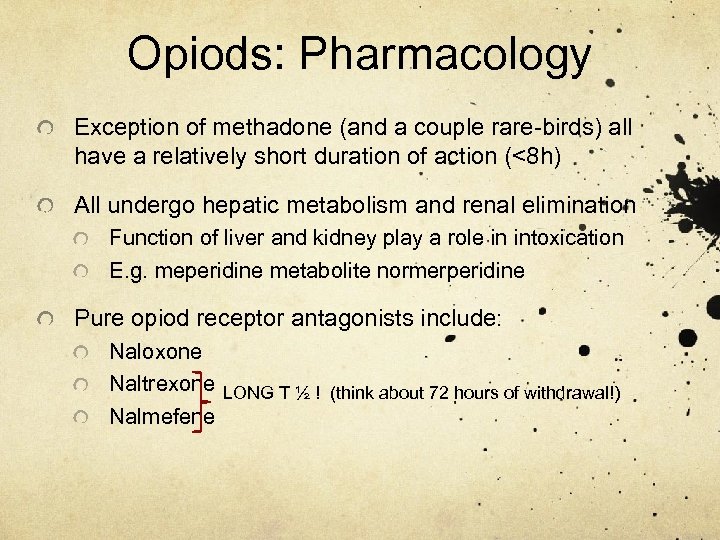
Opiods: Pharmacology Exception of methadone (and a couple rare-birds) all have a relatively short duration of action (<8 h) All undergo hepatic metabolism and renal elimination Function of liver and kidney play a role in intoxication E. g. meperidine metabolite normerperidine Pure opiod receptor antagonists include: Naloxone Naltrexone LONG T ½ ! (think about 72 hours of withdrawal!) Nalmefene
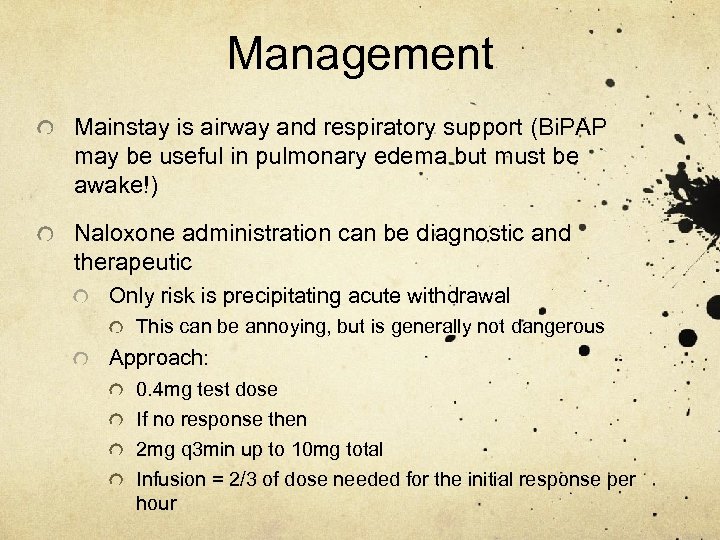
Management Mainstay is airway and respiratory support (Bi. PAP may be useful in pulmonary edema but must be awake!) Naloxone administration can be diagnostic and therapeutic Only risk is precipitating acute withdrawal This can be annoying, but is generally not dangerous Approach: 0. 4 mg test dose If no response then 2 mg q 3 min up to 10 mg total Infusion = 2/3 of dose needed for the initial response per hour
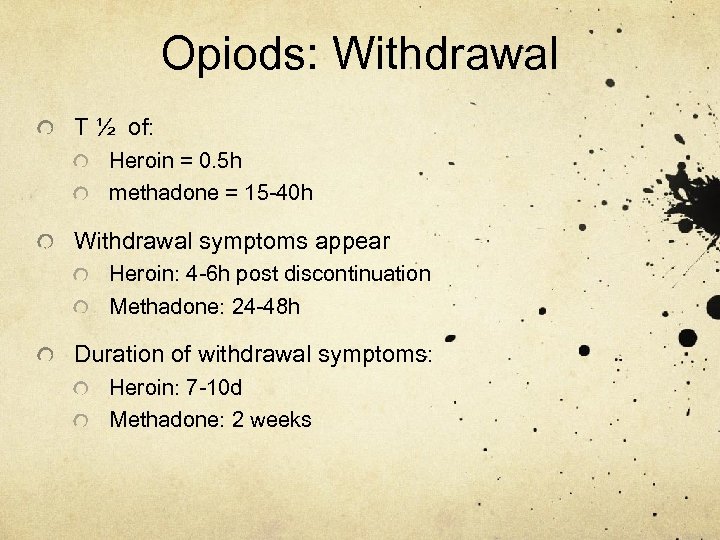
Opiods: Withdrawal T ½ of: Heroin = 0. 5 h methadone = 15 -40 h Withdrawal symptoms appear Heroin: 4 -6 h post discontinuation Methadone: 24 -48 h Duration of withdrawal symptoms: Heroin: 7 -10 d Methadone: 2 weeks
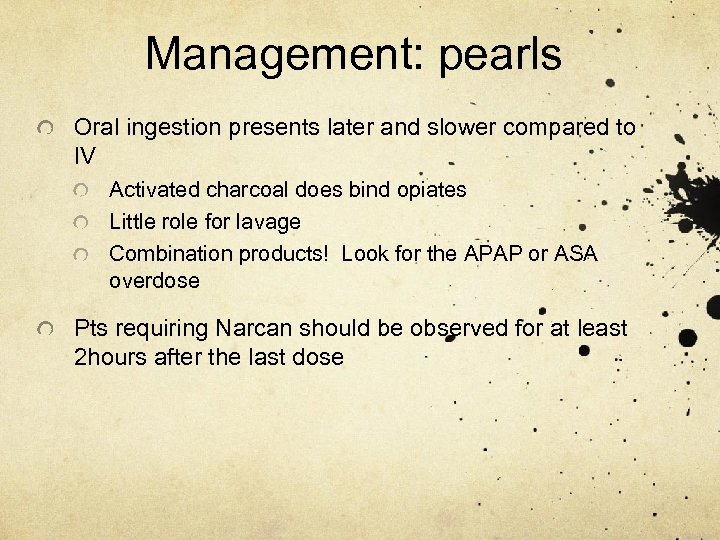
Management: pearls Oral ingestion presents later and slower compared to IV Activated charcoal does bind opiates Little role for lavage Combination products! Look for the APAP or ASA overdose Pts requiring Narcan should be observed for at least 2 hours after the last dose
Case 3 You administer Narcan 0. 2 mg IV and there is no response, after a total of 4 mg, the pt seems to rouse a little, resp rate improves and pupils now appear to be 3 mm. Effect is short lived and she soon returns to her previous condition Somebody finally finds the chart for you. She’s admitted to the antenatal methadone program and had just received her dose ~30 min before the code. 40 mg, same as she had received the previous 2 days. You call the unit, and their narcotic count is off by 360 mg.
Case 3 You place the patient on a Narcan drip and 72 h later she is back to her baseline. You spend the next two days trying to figure out: A) if it was a nursing error or pharmacy error B) what the potential side effects would be on the fetus
Big 4 1. Rapid sedation with IV/IM benzodiazepine is the key treatment for most symptoms of toxicity from cocaine and other stimulants 2. Hyperthermia is a high risk sign and body temperature must be reduced rapidly 3. β-blockade may cause paradoxical hypertension and increase coronary vasoconstriction and is generally contraindicated in sympathomimetic toxicity 4. Wide-complex rhythms secondary to cocaine ingestion may respond to IV Na. HCO 3 therapy
0447f0a1ff5a9b1d1dd90c1528da8e65.ppt