55a8b26e38d44bafa6f26928dad748be.ppt
- Количество слайдов: 54
 DRAFT Draft Phase 1 Report Northern Health & Social Care Trust Review of Emergency Care & Medical Specialities – Phase 1 A&E and MAU Patricia Kilpatrick 23 rd June 2010
DRAFT Draft Phase 1 Report Northern Health & Social Care Trust Review of Emergency Care & Medical Specialities – Phase 1 A&E and MAU Patricia Kilpatrick 23 rd June 2010
 Content 1 The Scope and Objectives for the Review 2 2 The Review Process 5 3 The Current Emergency Care System 8 4 Opportunities for Improvement using UK Best Practice 31 5 Appendices 41 1
Content 1 The Scope and Objectives for the Review 2 2 The Review Process 5 3 The Current Emergency Care System 8 4 Opportunities for Improvement using UK Best Practice 31 5 Appendices 41 1
 1 The Scope and Objectives for the Review 2
1 The Scope and Objectives for the Review 2
 Scope and Objectives for the Review Background and Scope All aspects of unscheduled care including the flow through A&E, MAU and specialities are included in the review The Northern Health and Social Care Trust engaged Tribal Consulting to undertake a major review of the provision of Unscheduled Care in order to: n Achieve increased performance n Improve the quality of the patient experience n Create a more efficient care process n Deliver optimum utilisation of healthcare resources. The review focussed on the specialities and services provided from the following hospitals: n Antrim Area n Causeway n Whiteabbey n Mid Ulster In addition the Dalriada, Moyle, Robinson and Braid Valley community hospitals were also reviewed. The review included all aspects of non elective patient flow and with a particular focus on: n Accident & Emergency (A&E) Acute medicine n Medical specialties n Intermediate and n A & E services in terms of achieving and sustaining the 4 hour access target n Medical Assessment Units (MAU) n Medical specialities n Care of the Elderly n General Medicine n Cardiology n Respiratory Medicine n Gastroenterology n Neurology n Stroke n Rehabilitation n Pharmacy and medicines Management team n Intermediate and step down care with a clearly defined diagnosis and robust assessment of the current problem The review process involved: n an appraisal of the current models of care n evaluation against UK best practice n recommendations on the future design and configuration of these services 3
Scope and Objectives for the Review Background and Scope All aspects of unscheduled care including the flow through A&E, MAU and specialities are included in the review The Northern Health and Social Care Trust engaged Tribal Consulting to undertake a major review of the provision of Unscheduled Care in order to: n Achieve increased performance n Improve the quality of the patient experience n Create a more efficient care process n Deliver optimum utilisation of healthcare resources. The review focussed on the specialities and services provided from the following hospitals: n Antrim Area n Causeway n Whiteabbey n Mid Ulster In addition the Dalriada, Moyle, Robinson and Braid Valley community hospitals were also reviewed. The review included all aspects of non elective patient flow and with a particular focus on: n Accident & Emergency (A&E) Acute medicine n Medical specialties n Intermediate and n A & E services in terms of achieving and sustaining the 4 hour access target n Medical Assessment Units (MAU) n Medical specialities n Care of the Elderly n General Medicine n Cardiology n Respiratory Medicine n Gastroenterology n Neurology n Stroke n Rehabilitation n Pharmacy and medicines Management team n Intermediate and step down care with a clearly defined diagnosis and robust assessment of the current problem The review process involved: n an appraisal of the current models of care n evaluation against UK best practice n recommendations on the future design and configuration of these services 3
 Scope and Objectives for the Review Objectives The main objective is to improve the triage and streaming of the patient flow in order to build a more efficient model of emergency care. The Review aimed to: n Reduce rate of presentations and to provide alternatives to A&E and reduce physical congestion n Segment flows and define appropriate resources to improve quality and reduce waiting and congestion n Match staffing with peaks in demand reduce breaches n Create alternatives to admission by increasing slots in imaging , scopes, outpatient services, direct referral to rapid access clinics and reduce numbers in A&E n Exploit ambulatory emergency care and bed reduction at both sites n Reduce the number and categories of patients who will have their detailed assessment and work up in A&E e. g. Ambulatory Care Service, GP referred medical patients, urgent / emergency Gynaecology, miscarriages, early pregnancy bleeds – eradicate congestion and breaches. n Reduce length of stay in MAU where appropriate n Benchmarking current performance with peer group and best practice n Review current intermediate care arrangements and performance n Prepare and plan for implementation of change to new models of care. n Plan for the recourses needed to implement and run the new model of care. The review process developed: n An unscheduled care model focussed on bringing together the key elements within the service to create an integrated emergency care department n An emergency ambulatory care reflecting UK best practice and supporting any existing “see and treat” functions within the Trust. n A bed model for the Trust based on achieving rapid access to streaming, assessment and specialty based care in line with Department of Health (DOH) guidance, UK best practice in the design of emergency care and the requirements of the Royal College of Physicians. n A resource plan to provide a sustainable solution that includes proposals to deliver the efficiencies required in the context of Comprehensive Spending Review (CSR) n A detailed implementation plan that focuses on the costs and timeframe by which the proposed models may be implemented 4
Scope and Objectives for the Review Objectives The main objective is to improve the triage and streaming of the patient flow in order to build a more efficient model of emergency care. The Review aimed to: n Reduce rate of presentations and to provide alternatives to A&E and reduce physical congestion n Segment flows and define appropriate resources to improve quality and reduce waiting and congestion n Match staffing with peaks in demand reduce breaches n Create alternatives to admission by increasing slots in imaging , scopes, outpatient services, direct referral to rapid access clinics and reduce numbers in A&E n Exploit ambulatory emergency care and bed reduction at both sites n Reduce the number and categories of patients who will have their detailed assessment and work up in A&E e. g. Ambulatory Care Service, GP referred medical patients, urgent / emergency Gynaecology, miscarriages, early pregnancy bleeds – eradicate congestion and breaches. n Reduce length of stay in MAU where appropriate n Benchmarking current performance with peer group and best practice n Review current intermediate care arrangements and performance n Prepare and plan for implementation of change to new models of care. n Plan for the recourses needed to implement and run the new model of care. The review process developed: n An unscheduled care model focussed on bringing together the key elements within the service to create an integrated emergency care department n An emergency ambulatory care reflecting UK best practice and supporting any existing “see and treat” functions within the Trust. n A bed model for the Trust based on achieving rapid access to streaming, assessment and specialty based care in line with Department of Health (DOH) guidance, UK best practice in the design of emergency care and the requirements of the Royal College of Physicians. n A resource plan to provide a sustainable solution that includes proposals to deliver the efficiencies required in the context of Comprehensive Spending Review (CSR) n A detailed implementation plan that focuses on the costs and timeframe by which the proposed models may be implemented 4
 2 The Review Process 5
2 The Review Process 5
 The Review Process Clinical Engagement Frequent meetings and workshops enabled involvement and participation from all clinical groups. A range of methods where used to meet and engage with clinicians on all sites including meetings with the following: n The clinical director for emergency care. n The emergency and specialty clinical teams. n The Multi Disciplinary Teams from the Community Hospital sites. Though these meetings we have ensured involvement and participation of consultants, clinical leads, senior nurses, senior managers, AHP leads, diagnostic teams in lab, imaging, pharmacy, CDs and Executive Directors. Each phase of the review process is followed by a workshop to further strengthen the clinical engagement: n Phase 1: A&E & MAU - 28 th June 2010 n Phase 2: Bed Models for Speciality Based care – 17 th June 2010 n Phase 3: Resource Planning and Implementation – 21 st July 2010 This report covers the first phase of the report – the review of A&E and MAU. 6
The Review Process Clinical Engagement Frequent meetings and workshops enabled involvement and participation from all clinical groups. A range of methods where used to meet and engage with clinicians on all sites including meetings with the following: n The clinical director for emergency care. n The emergency and specialty clinical teams. n The Multi Disciplinary Teams from the Community Hospital sites. Though these meetings we have ensured involvement and participation of consultants, clinical leads, senior nurses, senior managers, AHP leads, diagnostic teams in lab, imaging, pharmacy, CDs and Executive Directors. Each phase of the review process is followed by a workshop to further strengthen the clinical engagement: n Phase 1: A&E & MAU - 28 th June 2010 n Phase 2: Bed Models for Speciality Based care – 17 th June 2010 n Phase 3: Resource Planning and Implementation – 21 st July 2010 This report covers the first phase of the report – the review of A&E and MAU. 6
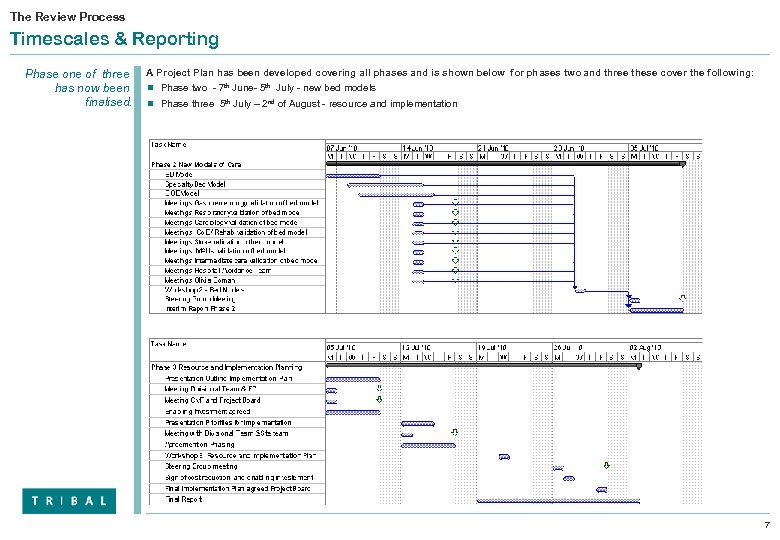 The Review Process Timescales & Reporting Phase one of three has now been finalised. A Project Plan has been developed covering all phases and is shown below for phases two and three these cover the following: n Phase two - 7 th June- 5 th July - new bed models n Phase three 5 th July – 2 nd of August - resource and implementation 7
The Review Process Timescales & Reporting Phase one of three has now been finalised. A Project Plan has been developed covering all phases and is shown below for phases two and three these cover the following: n Phase two - 7 th June- 5 th July - new bed models n Phase three 5 th July – 2 nd of August - resource and implementation 7
 3 The Current Emergency Care System 8
3 The Current Emergency Care System 8
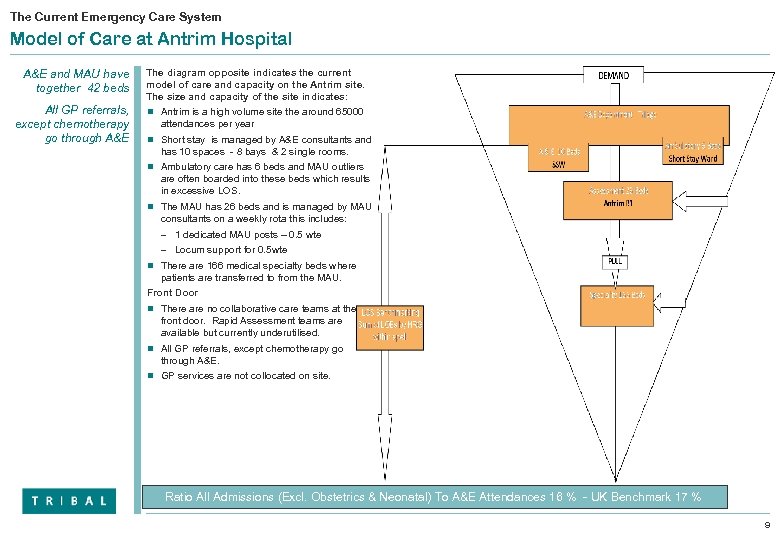 The Current Emergency Care System Model of Care at Antrim Hospital A&E and MAU have together 42 beds The diagram opposite indicates the current model of care and capacity on the Antrim site. The size and capacity of the site indicates: All GP referrals, except chemotherapy go through A&E n Antrim is a high volume site the around 65000 attendances per year n Short stay is managed by A&E consultants and has 10 spaces - 8 bays & 2 single rooms. n Ambulatory care has 6 beds and MAU outliers are often boarded into these beds which results in excessive LOS. n The MAU has 26 beds and is managed by MAU consultants on a weekly rota this includes: – 1 dedicated MAU posts – 0. 5 wte – Locum support for 0. 5 wte n There are 166 medical specialty beds where patients are transferred to from the MAU. Front Door n There are no collaborative care teams at the front door. Rapid Assessment teams are available but currently underutilised. n All GP referrals, except chemotherapy go through A&E. n GP services are not collocated on site. Ratio All Admissions (Excl. Obstetrics & Neonatal) To A&E Attendances 16 % - UK Benchmark 17 % 9
The Current Emergency Care System Model of Care at Antrim Hospital A&E and MAU have together 42 beds The diagram opposite indicates the current model of care and capacity on the Antrim site. The size and capacity of the site indicates: All GP referrals, except chemotherapy go through A&E n Antrim is a high volume site the around 65000 attendances per year n Short stay is managed by A&E consultants and has 10 spaces - 8 bays & 2 single rooms. n Ambulatory care has 6 beds and MAU outliers are often boarded into these beds which results in excessive LOS. n The MAU has 26 beds and is managed by MAU consultants on a weekly rota this includes: – 1 dedicated MAU posts – 0. 5 wte – Locum support for 0. 5 wte n There are 166 medical specialty beds where patients are transferred to from the MAU. Front Door n There are no collaborative care teams at the front door. Rapid Assessment teams are available but currently underutilised. n All GP referrals, except chemotherapy go through A&E. n GP services are not collocated on site. Ratio All Admissions (Excl. Obstetrics & Neonatal) To A&E Attendances 16 % - UK Benchmark 17 % 9
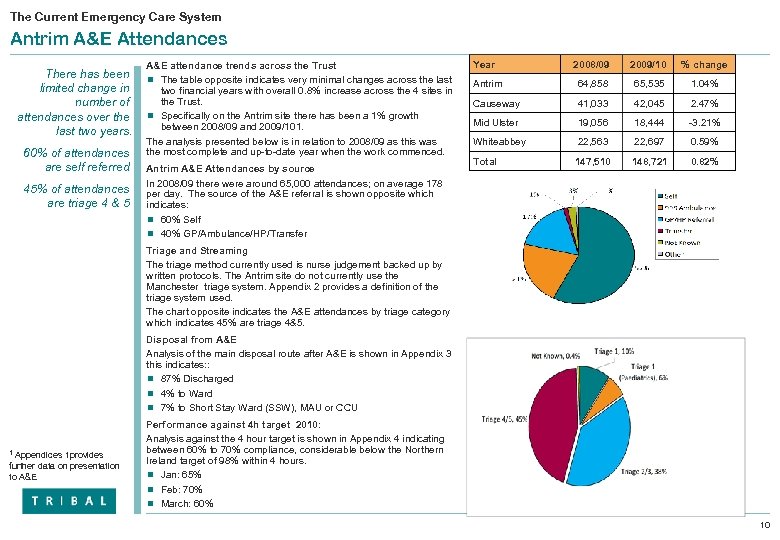 The Current Emergency Care System Antrim A&E Attendances There has been limited change in number of attendances over the last two years. 60% of attendances are self referred 45% of attendances are triage 4 & 5 A&E attendance trends across the Trust n The table opposite indicates very minimal changes across the last two financial years with overall 0. 8% increase across the 4 sites in the Trust. n Specifically on the Antrim site there has been a 1% growth between 2008/09 and 2009/101. The analysis presented below is in relation to 2008/09 as this was the most complete and up-to-date year when the work commenced. Antrim A&E Attendances by source In 2008/09 there were around 65, 000 attendances; on average 178 per day. The source of the A&E referral is shown opposite which indicates: n 60% Self n 40% GP/Ambulance/HP/Transfer Year 2008/09 2009/10 % change Antrim 64, 858 65, 535 1. 04% Causeway 41, 033 42, 045 2. 47% Mid Ulster 19, 056 18, 444 -3. 21% Whiteabbey 22, 563 22, 697 0. 59% Total 147, 510 148, 721 0. 82% Triage and Streaming The triage method currently used is nurse judgement backed up by written protocols. The Antrim site do not currently use the Manchester triage system. Appendix 2 provides a definition of the triage system used. The chart opposite indicates the A&E attendances by triage category which indicates 45% are triage 4&5. Disposal from A&E Analysis of the main disposal route after A&E is shown in Appendix 3 this indicates: : n 87% Discharged n 4% to Ward n 7% to Short Stay Ward (SSW), MAU or CCU 1 Appendices 1 provides further data on presentation to A&E Performance against 4 h target 2010: Analysis against the 4 hour target is shown in Appendix 4 indicating between 60% to 70% compliance, considerable below the Northern Ireland target of 98% within 4 hours. n Jan: 65% n Feb: 70% n March: 60% 10
The Current Emergency Care System Antrim A&E Attendances There has been limited change in number of attendances over the last two years. 60% of attendances are self referred 45% of attendances are triage 4 & 5 A&E attendance trends across the Trust n The table opposite indicates very minimal changes across the last two financial years with overall 0. 8% increase across the 4 sites in the Trust. n Specifically on the Antrim site there has been a 1% growth between 2008/09 and 2009/101. The analysis presented below is in relation to 2008/09 as this was the most complete and up-to-date year when the work commenced. Antrim A&E Attendances by source In 2008/09 there were around 65, 000 attendances; on average 178 per day. The source of the A&E referral is shown opposite which indicates: n 60% Self n 40% GP/Ambulance/HP/Transfer Year 2008/09 2009/10 % change Antrim 64, 858 65, 535 1. 04% Causeway 41, 033 42, 045 2. 47% Mid Ulster 19, 056 18, 444 -3. 21% Whiteabbey 22, 563 22, 697 0. 59% Total 147, 510 148, 721 0. 82% Triage and Streaming The triage method currently used is nurse judgement backed up by written protocols. The Antrim site do not currently use the Manchester triage system. Appendix 2 provides a definition of the triage system used. The chart opposite indicates the A&E attendances by triage category which indicates 45% are triage 4&5. Disposal from A&E Analysis of the main disposal route after A&E is shown in Appendix 3 this indicates: : n 87% Discharged n 4% to Ward n 7% to Short Stay Ward (SSW), MAU or CCU 1 Appendices 1 provides further data on presentation to A&E Performance against 4 h target 2010: Analysis against the 4 hour target is shown in Appendix 4 indicating between 60% to 70% compliance, considerable below the Northern Ireland target of 98% within 4 hours. n Jan: 65% n Feb: 70% n March: 60% 10
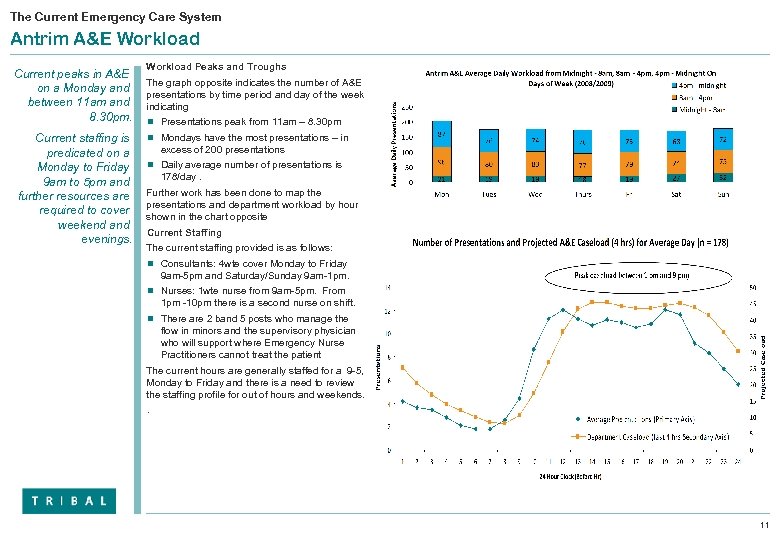 The Current Emergency Care System Antrim A&E Workload Current peaks in A&E on a Monday and between 11 am and 8. 30 pm. Current staffing is predicated on a Monday to Friday 9 am to 5 pm and further resources are required to cover weekend and evenings. Workload Peaks and Troughs The graph opposite indicates the number of A&E presentations by time period and day of the week indicating n Presentations peak from 11 am – 8. 30 pm n Mondays have the most presentations – in excess of 200 presentations n Daily average number of presentations is 178/day. Further work has been done to map the presentations and department workload by hour shown in the chart opposite Current Staffing The current staffing provided is as follows: n Consultants: 4 wte cover Monday to Friday 9 am-5 pm and Saturday/Sunday 9 am-1 pm. n Nurses: 1 wte nurse from 9 am-5 pm. From 1 pm -10 pm there is a second nurse on shift. n There are 2 band 5 posts who manage the flow in minors and the supervisory physician who will support where Emergency Nurse Practitioners cannot treat the patient The current hours are generally staffed for a 9 -5, Monday to Friday and there is a need to review the staffing profile for out of hours and weekends. . 11
The Current Emergency Care System Antrim A&E Workload Current peaks in A&E on a Monday and between 11 am and 8. 30 pm. Current staffing is predicated on a Monday to Friday 9 am to 5 pm and further resources are required to cover weekend and evenings. Workload Peaks and Troughs The graph opposite indicates the number of A&E presentations by time period and day of the week indicating n Presentations peak from 11 am – 8. 30 pm n Mondays have the most presentations – in excess of 200 presentations n Daily average number of presentations is 178/day. Further work has been done to map the presentations and department workload by hour shown in the chart opposite Current Staffing The current staffing provided is as follows: n Consultants: 4 wte cover Monday to Friday 9 am-5 pm and Saturday/Sunday 9 am-1 pm. n Nurses: 1 wte nurse from 9 am-5 pm. From 1 pm -10 pm there is a second nurse on shift. n There are 2 band 5 posts who manage the flow in minors and the supervisory physician who will support where Emergency Nurse Practitioners cannot treat the patient The current hours are generally staffed for a 9 -5, Monday to Friday and there is a need to review the staffing profile for out of hours and weekends. . 11
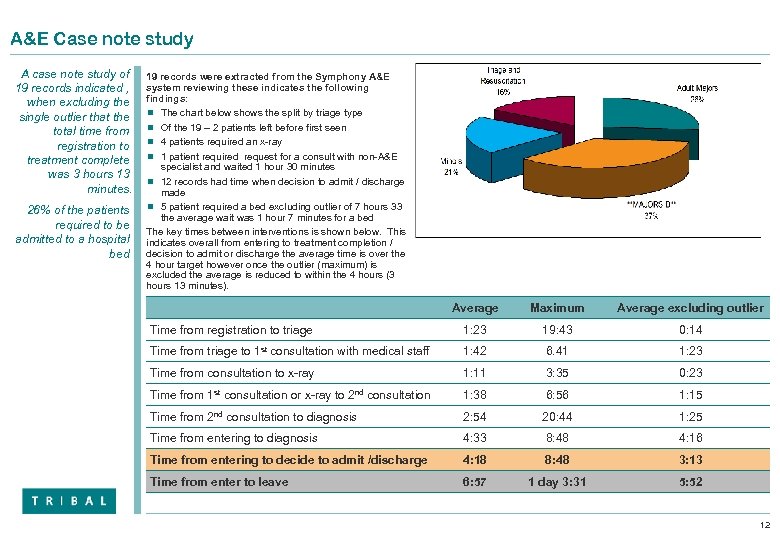 A&E Case note study A case note study of 19 records indicated , when excluding the single outlier that the total time from registration to treatment complete was 3 hours 13 minutes. 26% of the patients required to be admitted to a hospital bed 19 records were extracted from the Symphony A&E system reviewing these indicates the following findings: n The chart below shows the split by triage type n Of the 19 – 2 patients left before first seen n 4 patients required an x-ray n 1 patient required request for a consult with non-A&E specialist and waited 1 hour 30 minutes n 12 records had time when decision to admit / discharge made n 5 patient required a bed excluding outlier of 7 hours 33 the average wait was 1 hour 7 minutes for a bed The key times between interventions is shown below. This indicates overall from entering to treatment completion / decision to admit or discharge the average time is over the 4 hour target however once the outlier (maximum) is excluded the average is reduced to within the 4 hours (3 hours 13 minutes). Average Maximum Average excluding outlier Time from registration to triage 1: 23 19: 43 0: 14 Time from triage to 1 st consultation with medical staff 1: 42 6. 41 1: 23 Time from consultation to x-ray 1: 11 3: 35 0: 23 Time from 1 st consultation or x-ray to 2 nd consultation 1: 38 6: 56 1: 15 Time from 2 nd consultation to diagnosis 2: 54 20: 44 1: 25 Time from entering to diagnosis 4: 33 8: 48 4: 16 Time from entering to decide to admit /discharge 4: 18 8: 48 3: 13 Time from enter to leave 6: 57 1 day 3: 31 5: 52 12
A&E Case note study A case note study of 19 records indicated , when excluding the single outlier that the total time from registration to treatment complete was 3 hours 13 minutes. 26% of the patients required to be admitted to a hospital bed 19 records were extracted from the Symphony A&E system reviewing these indicates the following findings: n The chart below shows the split by triage type n Of the 19 – 2 patients left before first seen n 4 patients required an x-ray n 1 patient required request for a consult with non-A&E specialist and waited 1 hour 30 minutes n 12 records had time when decision to admit / discharge made n 5 patient required a bed excluding outlier of 7 hours 33 the average wait was 1 hour 7 minutes for a bed The key times between interventions is shown below. This indicates overall from entering to treatment completion / decision to admit or discharge the average time is over the 4 hour target however once the outlier (maximum) is excluded the average is reduced to within the 4 hours (3 hours 13 minutes). Average Maximum Average excluding outlier Time from registration to triage 1: 23 19: 43 0: 14 Time from triage to 1 st consultation with medical staff 1: 42 6. 41 1: 23 Time from consultation to x-ray 1: 11 3: 35 0: 23 Time from 1 st consultation or x-ray to 2 nd consultation 1: 38 6: 56 1: 15 Time from 2 nd consultation to diagnosis 2: 54 20: 44 1: 25 Time from entering to diagnosis 4: 33 8: 48 4: 16 Time from entering to decide to admit /discharge 4: 18 8: 48 3: 13 Time from enter to leave 6: 57 1 day 3: 31 5: 52 12
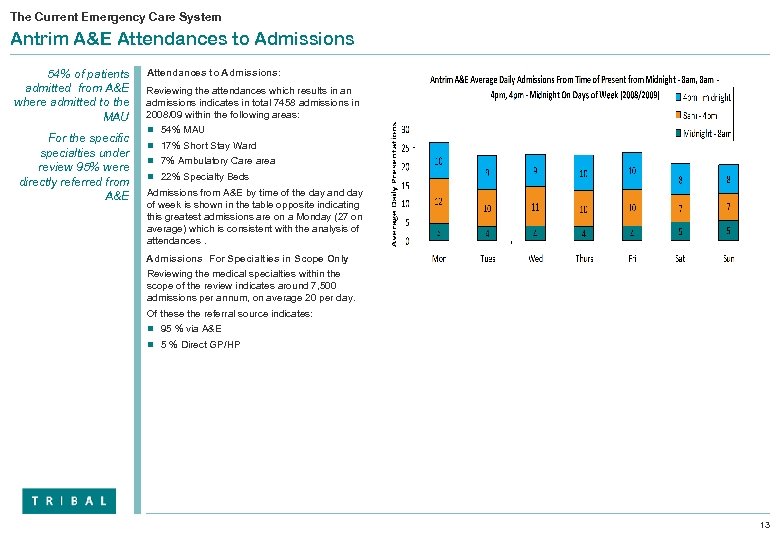 The Current Emergency Care System Antrim A&E Attendances to Admissions 54% of patients admitted from A&E where admitted to the MAU For the specific specialties under review 95% were directly referred from A&E Attendances to Admissions: Reviewing the attendances which results in an admissions indicates in total 7458 admissions in 2008/09 within the following areas: n 54% MAU n 17% Short Stay Ward n 7% Ambulatory Care area n 22% Specialty Beds Admissions from A&E by time of the day and day of week is shown in the table opposite indicating this greatest admissions are on a Monday (27 on average) which is consistent with the analysis of attendances. Admissions For Specialties in Scope Only Reviewing the medical specialties within the scope of the review indicates around 7, 500 admissions per annum, on average 20 per day. Of these the referral source indicates: n 95 % via A&E n 5 % Direct GP/HP 13
The Current Emergency Care System Antrim A&E Attendances to Admissions 54% of patients admitted from A&E where admitted to the MAU For the specific specialties under review 95% were directly referred from A&E Attendances to Admissions: Reviewing the attendances which results in an admissions indicates in total 7458 admissions in 2008/09 within the following areas: n 54% MAU n 17% Short Stay Ward n 7% Ambulatory Care area n 22% Specialty Beds Admissions from A&E by time of the day and day of week is shown in the table opposite indicating this greatest admissions are on a Monday (27 on average) which is consistent with the analysis of attendances. Admissions For Specialties in Scope Only Reviewing the medical specialties within the scope of the review indicates around 7, 500 admissions per annum, on average 20 per day. Of these the referral source indicates: n 95 % via A&E n 5 % Direct GP/HP 13
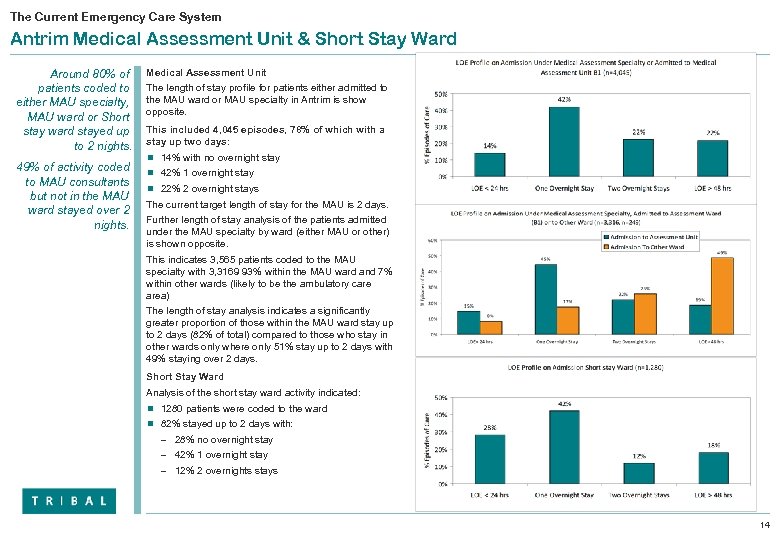 The Current Emergency Care System Antrim Medical Assessment Unit & Short Stay Ward Around 80% of patients coded to either MAU specialty, MAU ward or Short stay ward stayed up to 2 nights. 49% of activity coded to MAU consultants but not in the MAU ward stayed over 2 nights. Medical Assessment Unit The length of stay profile for patients either admitted to the MAU ward or MAU specialty in Antrim is show opposite. This included 4, 045 episodes, 78% of which with a stay up two days: n 14% with no overnight stay n 42% 1 overnight stay n 22% 2 overnight stays The current target length of stay for the MAU is 2 days. Further length of stay analysis of the patients admitted under the MAU specialty by ward (either MAU or other) is shown opposite. This indicates 3, 565 patients coded to the MAU specialty with 3, 3169 93% within the MAU ward and 7% within other wards (likely to be the ambulatory care area) The length of stay analysis indicates a significantly greater proportion of those within the MAU ward stay up to 2 days (82% of total) compared to those who stay in other wards only where only 51% stay up to 2 days with 49% staying over 2 days. Short Stay Ward Analysis of the short stay ward activity indicated: n 1280 patients were coded to the ward n 82% stayed up to 2 days with: – 28% no overnight stay – 42% 1 overnight stay – 12% 2 overnights stays 14
The Current Emergency Care System Antrim Medical Assessment Unit & Short Stay Ward Around 80% of patients coded to either MAU specialty, MAU ward or Short stay ward stayed up to 2 nights. 49% of activity coded to MAU consultants but not in the MAU ward stayed over 2 nights. Medical Assessment Unit The length of stay profile for patients either admitted to the MAU ward or MAU specialty in Antrim is show opposite. This included 4, 045 episodes, 78% of which with a stay up two days: n 14% with no overnight stay n 42% 1 overnight stay n 22% 2 overnight stays The current target length of stay for the MAU is 2 days. Further length of stay analysis of the patients admitted under the MAU specialty by ward (either MAU or other) is shown opposite. This indicates 3, 565 patients coded to the MAU specialty with 3, 3169 93% within the MAU ward and 7% within other wards (likely to be the ambulatory care area) The length of stay analysis indicates a significantly greater proportion of those within the MAU ward stay up to 2 days (82% of total) compared to those who stay in other wards only where only 51% stay up to 2 days with 49% staying over 2 days. Short Stay Ward Analysis of the short stay ward activity indicated: n 1280 patients were coded to the ward n 82% stayed up to 2 days with: – 28% no overnight stay – 42% 1 overnight stay – 12% 2 overnights stays 14
 The Current Emergency Care System The Current Model of Care at Antrim Hospital A & E The access to speciality beds is not fast enough The social worker response time is good. A&E attendances are streamed into three areas: n Majors – Patients arrive by self referral, GP or ambulance. – Protocols exists for triage, – There is a point of care testing in place and some delays due to pathology. n Minors – Self referred patients will on arrival choose against a list of conditions (minor/majors). – Minors move to a separate area with 7 cubicles available. – An Emergency Nurse Practitioner (ENP) manages minors with the supervision of a physician (any grade). n Paediatrics – There is a separate area for children. – A dedicated nurse from majors and a physician covers this area in conjunction with A&E. – They have not all received paediatric specific training. Access to clinics n Elective clinics should allow for acute management of patients within specialities. The rapid access clinics with a 2 week wait are not ‘rapid’ enough. n There is a direct access to Stroke and Cardiology, admission from A&E to MAU. n Gynaecology is a particular problem and the teams are working to identify a clear pathway to Gynaecology services to reduce response times Occupational Therapy/Physiotherapy/Social Care support in A&E and Short stay: n Physiotherapy and Occupational Therapy are available on weekdays and for a few hours in the morning on weekends. n Social worker is on call at weekends and dedicated in the department weekdays n The response time is good 15
The Current Emergency Care System The Current Model of Care at Antrim Hospital A & E The access to speciality beds is not fast enough The social worker response time is good. A&E attendances are streamed into three areas: n Majors – Patients arrive by self referral, GP or ambulance. – Protocols exists for triage, – There is a point of care testing in place and some delays due to pathology. n Minors – Self referred patients will on arrival choose against a list of conditions (minor/majors). – Minors move to a separate area with 7 cubicles available. – An Emergency Nurse Practitioner (ENP) manages minors with the supervision of a physician (any grade). n Paediatrics – There is a separate area for children. – A dedicated nurse from majors and a physician covers this area in conjunction with A&E. – They have not all received paediatric specific training. Access to clinics n Elective clinics should allow for acute management of patients within specialities. The rapid access clinics with a 2 week wait are not ‘rapid’ enough. n There is a direct access to Stroke and Cardiology, admission from A&E to MAU. n Gynaecology is a particular problem and the teams are working to identify a clear pathway to Gynaecology services to reduce response times Occupational Therapy/Physiotherapy/Social Care support in A&E and Short stay: n Physiotherapy and Occupational Therapy are available on weekdays and for a few hours in the morning on weekends. n Social worker is on call at weekends and dedicated in the department weekdays n The response time is good 15
 The Current Emergency Care System Current Model of Care Antrim Hospital A & E Access to mental health acute beds is an issue Mental Health n Crisis response from Mental Health is excellent. n Daily presence in the mornings and good response time n Access to Mental Health acute beds is an issue and can cause delays for up to a day where patients are admitted to the ward/short stay until a bed can be found within the region if none available at Holywell. The role of the flow coordinator should be expanded to better manage breaches Flow Management/Coordinator: n This post does exist but it is not working optimally. It is felt this role would significantly improve the management of patient flow and managing breaches within the department and allocating resource where required. . Delays downstream n MAU is unable to create capacity. n Wards are not discharging enough to allow pulling from MAU to release capacity. Information/Monitoring of the target: n An electronic system, Symphony, is in use and flags patients when they are coming up to breaching. Symphony shows: Name of Patient, Registration time, pre streamed (ED 1), ED 2, Decision to Admit, Depart. n Performance against 4 hours / 12 hours high level of breaches. - waiting for breach report from Seamus n There are full admitting rights to surgery therefore no delays in terms of response times n There is unlimited access to CT, ultrasound and X-ray in hours and unlimited access to X-ray out of hours. However access to ultrasound and CT out of hours is by patient demand on call. There is access to a morning endoscopy list 16
The Current Emergency Care System Current Model of Care Antrim Hospital A & E Access to mental health acute beds is an issue Mental Health n Crisis response from Mental Health is excellent. n Daily presence in the mornings and good response time n Access to Mental Health acute beds is an issue and can cause delays for up to a day where patients are admitted to the ward/short stay until a bed can be found within the region if none available at Holywell. The role of the flow coordinator should be expanded to better manage breaches Flow Management/Coordinator: n This post does exist but it is not working optimally. It is felt this role would significantly improve the management of patient flow and managing breaches within the department and allocating resource where required. . Delays downstream n MAU is unable to create capacity. n Wards are not discharging enough to allow pulling from MAU to release capacity. Information/Monitoring of the target: n An electronic system, Symphony, is in use and flags patients when they are coming up to breaching. Symphony shows: Name of Patient, Registration time, pre streamed (ED 1), ED 2, Decision to Admit, Depart. n Performance against 4 hours / 12 hours high level of breaches. - waiting for breach report from Seamus n There are full admitting rights to surgery therefore no delays in terms of response times n There is unlimited access to CT, ultrasound and X-ray in hours and unlimited access to X-ray out of hours. However access to ultrasound and CT out of hours is by patient demand on call. There is access to a morning endoscopy list 16
 The Current Emergency Care System Model of Care Antrim Hospital MAU All patients , except cardiology, go from A&E to MAU. The Model n All patients, except Cardiology, go to MAU and are coded to the single consultant regardless of whether it is their rotaed week on n There are 26 beds and one extra bed without call buttons or gas/air. n There is no high dependency unit in the MAU n Length of stay is longer than needed due to capacity issues in specialty beds n It is a push model rather than a pull from MAU to specialist or discharge. n There are no electronic boards to track A&E waits n The discharge services are poor at weekends. Staffing n 1 wte consultant post (work each 2 nd week in MAU) – 0. 5 Respiratory – 0. 5 Locum –The recruitment for this post is delayed. n Nurses work over 3 areas to increase flexibly (MAU, Clinical Decision Unit, Short Stay Ward) n The nursing skill mix in MAU is high (3 qualified to 1 non) n Receiving arrangements – Consultant rota between 8 am-5 pm – On call Physician of the day working a 1 in 11 rota. – There is no Rheumatology in rota – Cardiology, Renal & Haematology have separate rotas n There is in reach from Cardiology and Stroke but not Gastrointestinal (GI) n Typical 5 days service across MAU and hospital with limited consultant input at weekend – 50% reduction in discharges at weekend 17
The Current Emergency Care System Model of Care Antrim Hospital MAU All patients , except cardiology, go from A&E to MAU. The Model n All patients, except Cardiology, go to MAU and are coded to the single consultant regardless of whether it is their rotaed week on n There are 26 beds and one extra bed without call buttons or gas/air. n There is no high dependency unit in the MAU n Length of stay is longer than needed due to capacity issues in specialty beds n It is a push model rather than a pull from MAU to specialist or discharge. n There are no electronic boards to track A&E waits n The discharge services are poor at weekends. Staffing n 1 wte consultant post (work each 2 nd week in MAU) – 0. 5 Respiratory – 0. 5 Locum –The recruitment for this post is delayed. n Nurses work over 3 areas to increase flexibly (MAU, Clinical Decision Unit, Short Stay Ward) n The nursing skill mix in MAU is high (3 qualified to 1 non) n Receiving arrangements – Consultant rota between 8 am-5 pm – On call Physician of the day working a 1 in 11 rota. – There is no Rheumatology in rota – Cardiology, Renal & Haematology have separate rotas n There is in reach from Cardiology and Stroke but not Gastrointestinal (GI) n Typical 5 days service across MAU and hospital with limited consultant input at weekend – 50% reduction in discharges at weekend 17
 The Current Emergency Care System Model of Care Antrim Hospital MAU Difficult to discharge within 72 hours due to lack of specialty beds. Systems and Processes n There are 2 ward rounds a day during Monday -Friday – am ward round followed by review – pm white board round with Multi Disciplinary Team (MDT). n There is one daily (am) ward round during Sat & Sun n MDT including occupational therapists, physiotherapist and social worker, are meeting daily at 10. 30 n The post take round is done by a MAU consultant – either from respiratory or locum (geriatric medicine) n The goal is to discharge within 72 hours where possible but this is currently difficult due to lack of specialty beds n The current general model is to hold patients in MAU awaiting correct specialty bed rather than put in other specialty n There are is treatment plan proforma in use except for stroke Integrated Care Pathway (ICP) n Estimated date of discharge is set in MAU together with date of admission, details of any investigations, referral and discharge. The status of each patient is kept up to date on a whiteboard. All patients in BAY 1, 2, 3, 4 and side room 1 and 2 are tracked. n Nurses are currently not able to order Radiology or Diagnostics. n MAU staff have access to A&E system to identify patients Improvements and issues n There has been recent improvements to CT that allows early am session and weekend session for strokes n Blockage in the process appears to be diagnostics in particular Endoscopy – A solution could be setting up early 8 am session Monday to Friday. 18
The Current Emergency Care System Model of Care Antrim Hospital MAU Difficult to discharge within 72 hours due to lack of specialty beds. Systems and Processes n There are 2 ward rounds a day during Monday -Friday – am ward round followed by review – pm white board round with Multi Disciplinary Team (MDT). n There is one daily (am) ward round during Sat & Sun n MDT including occupational therapists, physiotherapist and social worker, are meeting daily at 10. 30 n The post take round is done by a MAU consultant – either from respiratory or locum (geriatric medicine) n The goal is to discharge within 72 hours where possible but this is currently difficult due to lack of specialty beds n The current general model is to hold patients in MAU awaiting correct specialty bed rather than put in other specialty n There are is treatment plan proforma in use except for stroke Integrated Care Pathway (ICP) n Estimated date of discharge is set in MAU together with date of admission, details of any investigations, referral and discharge. The status of each patient is kept up to date on a whiteboard. All patients in BAY 1, 2, 3, 4 and side room 1 and 2 are tracked. n Nurses are currently not able to order Radiology or Diagnostics. n MAU staff have access to A&E system to identify patients Improvements and issues n There has been recent improvements to CT that allows early am session and weekend session for strokes n Blockage in the process appears to be diagnostics in particular Endoscopy – A solution could be setting up early 8 am session Monday to Friday. 18
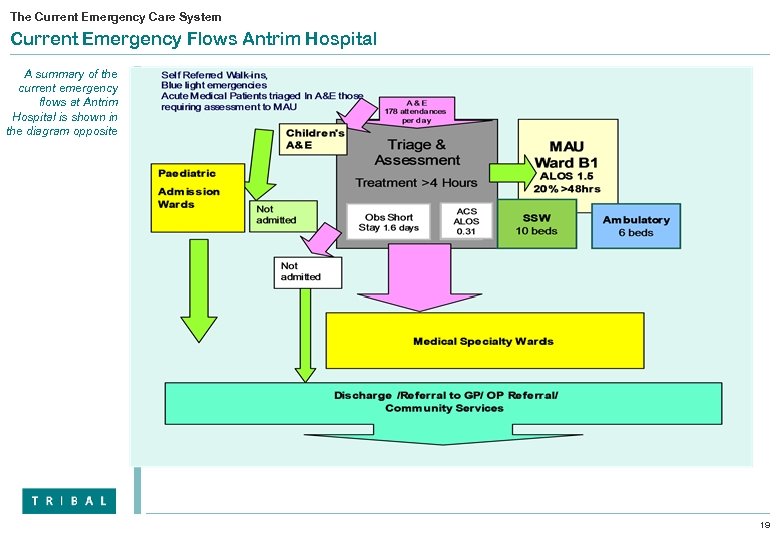 The Current Emergency Care System Current Emergency Flows Antrim Hospital A summary of the current emergency flows at Antrim Hospital is shown in the diagram opposite 19
The Current Emergency Care System Current Emergency Flows Antrim Hospital A summary of the current emergency flows at Antrim Hospital is shown in the diagram opposite 19
 The Current Emergency Care System Antrim Hospital: Issues emerging from the review A standardised triage method would reduce risk of clinical variation. . Front Door n High level of Urgent Care cases presenting at A&E in 08/09 – Triage 4/5 = 29, 043 represents 45% of total, a daily average of 80 patients per day n Lack of protocols for streaming patients to minors and majors (self referral only) – at present this is based on patient’s own allocation at reception according to a list of conditions. This could result in inappropriate use of resources should patient’s default to the wrong stream. n Triage is undertaken using protocols and nursing judgement. There needs to be a standardised mechanism for triage to reduce clinical variation practices. n The self referred & GP referred medical patients are being managed through A&E. this is not UK best practice. On average 80% of the breaches are related to medical assessment of self referred cases with lower admission rate. Admissions n There were 7, 458 non-elective admissions for all medical specialties admitted; excluding Stroke and MI there are 6910 n Of these 54% are subsequently admitted to MAU, 17% admitted to Short Stay Ward, 7 % to Ambulatory and 22% to specialty beds n Of the 4045 admitted to MAU, 15 % are discharged within 24 hours Staff n Significant problems recruiting to junior doctors and also managing to cover these posts with locums. With the merger across Whiteabbey and Mid Ulster there is funding available for 3. 5 middle grades. The suggestion is to use this funding for 2 additional consultant posts in order to plan medical workforce in line with demand peaks. Length Of Stay n Average length of stay in MAU is 1. 5 days; compared to the UK average of 0. 8 days n 532 admission in A&E related to ante natal not related to delivery or an event of which 63 were discharged same day Suggestions to improve flow: n Active streaming & minors can be managed in a separate area by emergency nurse practitioners n All GP referred cases should go direct to MAU n All strokes following assessment and confirmed stroke should go to Hyper Acute Stoke Unit. n All Myocardial Infarctions following confirmed diagnosis should go to Cardiology /Coronary Care Unit n A care of the elderly service at the front door to manage patients through Care of elderly assessment beds in the community and establishment of an older people rapid access clinics. 20
The Current Emergency Care System Antrim Hospital: Issues emerging from the review A standardised triage method would reduce risk of clinical variation. . Front Door n High level of Urgent Care cases presenting at A&E in 08/09 – Triage 4/5 = 29, 043 represents 45% of total, a daily average of 80 patients per day n Lack of protocols for streaming patients to minors and majors (self referral only) – at present this is based on patient’s own allocation at reception according to a list of conditions. This could result in inappropriate use of resources should patient’s default to the wrong stream. n Triage is undertaken using protocols and nursing judgement. There needs to be a standardised mechanism for triage to reduce clinical variation practices. n The self referred & GP referred medical patients are being managed through A&E. this is not UK best practice. On average 80% of the breaches are related to medical assessment of self referred cases with lower admission rate. Admissions n There were 7, 458 non-elective admissions for all medical specialties admitted; excluding Stroke and MI there are 6910 n Of these 54% are subsequently admitted to MAU, 17% admitted to Short Stay Ward, 7 % to Ambulatory and 22% to specialty beds n Of the 4045 admitted to MAU, 15 % are discharged within 24 hours Staff n Significant problems recruiting to junior doctors and also managing to cover these posts with locums. With the merger across Whiteabbey and Mid Ulster there is funding available for 3. 5 middle grades. The suggestion is to use this funding for 2 additional consultant posts in order to plan medical workforce in line with demand peaks. Length Of Stay n Average length of stay in MAU is 1. 5 days; compared to the UK average of 0. 8 days n 532 admission in A&E related to ante natal not related to delivery or an event of which 63 were discharged same day Suggestions to improve flow: n Active streaming & minors can be managed in a separate area by emergency nurse practitioners n All GP referred cases should go direct to MAU n All strokes following assessment and confirmed stroke should go to Hyper Acute Stoke Unit. n All Myocardial Infarctions following confirmed diagnosis should go to Cardiology /Coronary Care Unit n A care of the elderly service at the front door to manage patients through Care of elderly assessment beds in the community and establishment of an older people rapid access clinics. 20
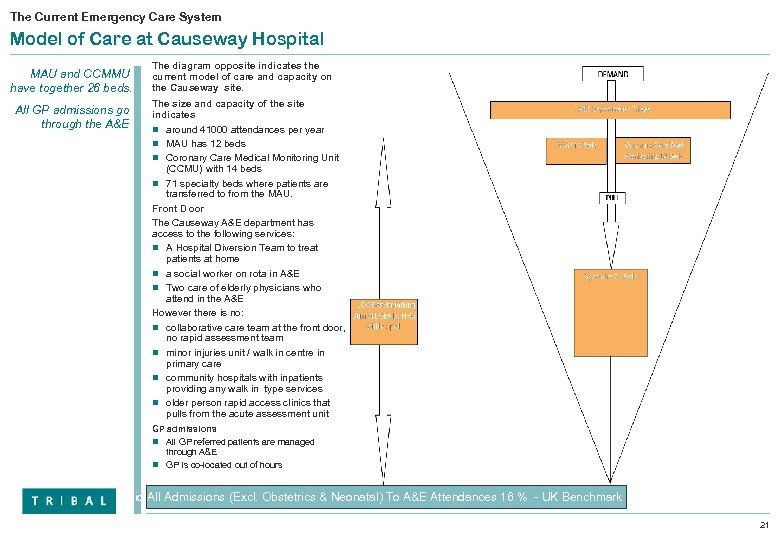 The Current Emergency Care System Model of Care at Causeway Hospital MAU and CCMMU have together 26 beds. All GP admissions go through the A&E The diagram opposite indicates the current model of care and capacity on the Causeway site. The size and capacity of the site indicates n around 41000 attendances per year n MAU has 12 beds n Coronary Care Medical Monitoring Unit (CCMU) with 14 beds n 71 specialty beds where patients are transferred to from the MAU. Front Door The Causeway A&E department has access to the following services: n A Hospital Diversion Team to treat patients at home n a social worker on rota in A&E n Two care of elderly physicians who attend in the A&E However there is no: n collaborative care team at the front door, no rapid assessment team n minor injuries unit / walk in centre in primary care n community hospitals with inpatients providing any walk in type services n older person rapid access clinics that pulls from the acute assessment unit GP admissions n All GP referred patients are managed through A&E n GP is co-located out of hours Ratio All Admissions (Excl. Obstetrics & Neonatal) To A&E Attendances 16 % - UK Benchmark 17 % 21
The Current Emergency Care System Model of Care at Causeway Hospital MAU and CCMMU have together 26 beds. All GP admissions go through the A&E The diagram opposite indicates the current model of care and capacity on the Causeway site. The size and capacity of the site indicates n around 41000 attendances per year n MAU has 12 beds n Coronary Care Medical Monitoring Unit (CCMU) with 14 beds n 71 specialty beds where patients are transferred to from the MAU. Front Door The Causeway A&E department has access to the following services: n A Hospital Diversion Team to treat patients at home n a social worker on rota in A&E n Two care of elderly physicians who attend in the A&E However there is no: n collaborative care team at the front door, no rapid assessment team n minor injuries unit / walk in centre in primary care n community hospitals with inpatients providing any walk in type services n older person rapid access clinics that pulls from the acute assessment unit GP admissions n All GP referred patients are managed through A&E n GP is co-located out of hours Ratio All Admissions (Excl. Obstetrics & Neonatal) To A&E Attendances 16 % - UK Benchmark 17 % 21
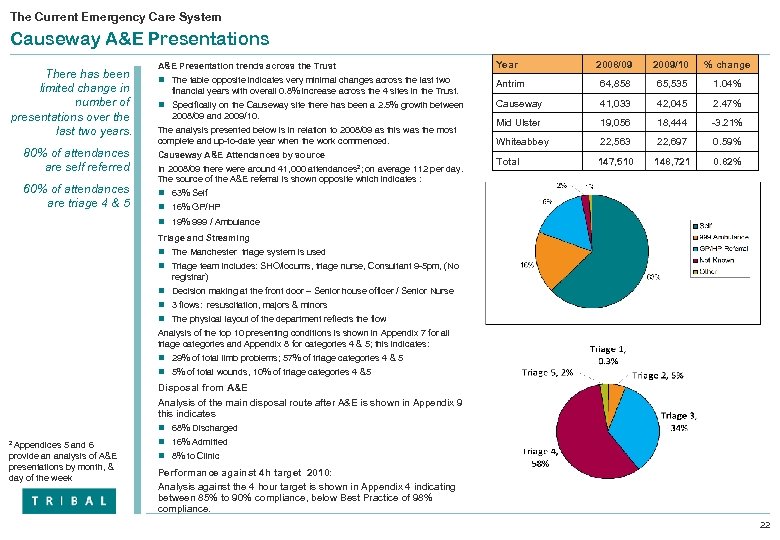 The Current Emergency Care System Causeway A&E Presentations There has been limited change in number of presentations over the last two years. 80% of attendances are self referred 60% of attendances are triage 4 & 5 A&E Presentation trends across the Trust Year 2008/09 2009/10 % change n The table opposite indicates very minimal changes across the last two Antrim 64, 858 65, 535 1. 04% Causeway 41, 033 42, 045 2. 47% Mid Ulster 19, 056 18, 444 -3. 21% Whiteabbey 22, 563 22, 697 0. 59% Total 147, 510 148, 721 0. 82% financial years with overall 0. 8% increase across the 4 sites in the Trust. n Specifically on the Causeway site there has been a 2. 5% growth between 2008/09 and 2009/10. The analysis presented below is in relation to 2008/09 as this was the most complete and up-to-date year when the work commenced. Causeway A&E Attendances by source In 2008/09 there were around 41, 000 attendances 2; on average 112 per day. The source of the A&E referral is shown opposite which indicates : n 63% Self n 16% GP/HP n 19% 999 / Ambulance Triage and Streaming n The Manchester triage system is used n Triage team includes: SHO/locums, triage nurse, Consultant 9 -5 pm, (No registrar) n Decision making at the front door – Senior house officer / Senior Nurse n 3 flows: resuscitation, majors & minors n The physical layout of the department reflects the flow Analysis of the top 10 presenting conditions is shown in Appendix 7 for all triage categories and Appendix 8 for categories 4 & 5; this indicates: n 29% of total limb problems; 57% of triage categories 4 & 5 n 5% of total wounds, 10% of triage categories 4 &5 Disposal from A&E Analysis of the main disposal route after A&E is shown in Appendix 9 this indicates n 68% Discharged 2 Appendices 5 and 6 provide an analysis of A&E presentations by month, & day of the week n 16% Admitted n 8% to Clinic Performance against 4 h target 2010: Analysis against the 4 hour target is shown in Appendix 4 indicating between 85% to 90% compliance, below Best Practice of 98% compliance. 22
The Current Emergency Care System Causeway A&E Presentations There has been limited change in number of presentations over the last two years. 80% of attendances are self referred 60% of attendances are triage 4 & 5 A&E Presentation trends across the Trust Year 2008/09 2009/10 % change n The table opposite indicates very minimal changes across the last two Antrim 64, 858 65, 535 1. 04% Causeway 41, 033 42, 045 2. 47% Mid Ulster 19, 056 18, 444 -3. 21% Whiteabbey 22, 563 22, 697 0. 59% Total 147, 510 148, 721 0. 82% financial years with overall 0. 8% increase across the 4 sites in the Trust. n Specifically on the Causeway site there has been a 2. 5% growth between 2008/09 and 2009/10. The analysis presented below is in relation to 2008/09 as this was the most complete and up-to-date year when the work commenced. Causeway A&E Attendances by source In 2008/09 there were around 41, 000 attendances 2; on average 112 per day. The source of the A&E referral is shown opposite which indicates : n 63% Self n 16% GP/HP n 19% 999 / Ambulance Triage and Streaming n The Manchester triage system is used n Triage team includes: SHO/locums, triage nurse, Consultant 9 -5 pm, (No registrar) n Decision making at the front door – Senior house officer / Senior Nurse n 3 flows: resuscitation, majors & minors n The physical layout of the department reflects the flow Analysis of the top 10 presenting conditions is shown in Appendix 7 for all triage categories and Appendix 8 for categories 4 & 5; this indicates: n 29% of total limb problems; 57% of triage categories 4 & 5 n 5% of total wounds, 10% of triage categories 4 &5 Disposal from A&E Analysis of the main disposal route after A&E is shown in Appendix 9 this indicates n 68% Discharged 2 Appendices 5 and 6 provide an analysis of A&E presentations by month, & day of the week n 16% Admitted n 8% to Clinic Performance against 4 h target 2010: Analysis against the 4 hour target is shown in Appendix 4 indicating between 85% to 90% compliance, below Best Practice of 98% compliance. 22
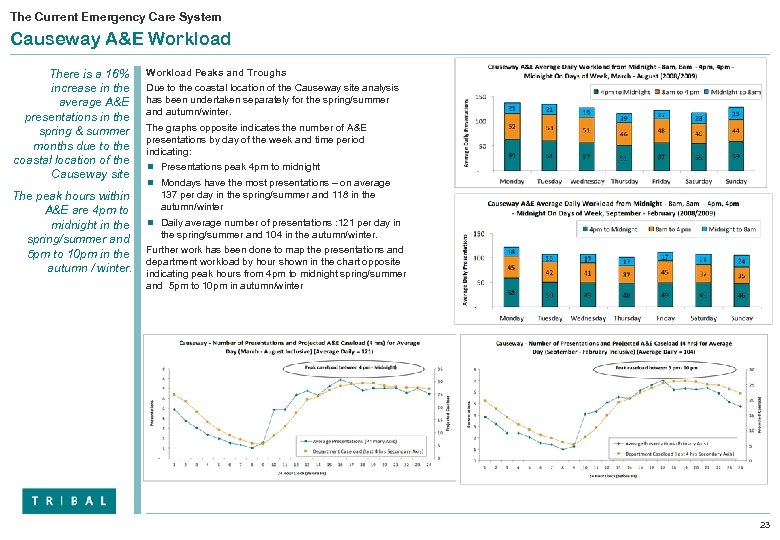 The Current Emergency Care System Causeway A&E Workload There is a 16% increase in the average A&E presentations in the spring & summer months due to the coastal location of the Causeway site The peak hours within A&E are 4 pm to midnight in the spring/summer and 5 pm to 10 pm in the autumn / winter. Workload Peaks and Troughs Due to the coastal location of the Causeway site analysis has been undertaken separately for the spring/summer and autumn/winter. The graphs opposite indicates the number of A&E presentations by day of the week and time period indicating: n Presentations peak 4 pm to midnight n Mondays have the most presentations – on average 137 per day in the spring/summer and 118 in the autumn/winter n Daily average number of presentations : 121 per day in the spring/summer and 104 in the autumn/winter. Further work has been done to map the presentations and department workload by hour shown in the chart opposite indicating peak hours from 4 pm to midnight spring/summer and 5 pm to 10 pm in autumn/winter 23
The Current Emergency Care System Causeway A&E Workload There is a 16% increase in the average A&E presentations in the spring & summer months due to the coastal location of the Causeway site The peak hours within A&E are 4 pm to midnight in the spring/summer and 5 pm to 10 pm in the autumn / winter. Workload Peaks and Troughs Due to the coastal location of the Causeway site analysis has been undertaken separately for the spring/summer and autumn/winter. The graphs opposite indicates the number of A&E presentations by day of the week and time period indicating: n Presentations peak 4 pm to midnight n Mondays have the most presentations – on average 137 per day in the spring/summer and 118 in the autumn/winter n Daily average number of presentations : 121 per day in the spring/summer and 104 in the autumn/winter. Further work has been done to map the presentations and department workload by hour shown in the chart opposite indicating peak hours from 4 pm to midnight spring/summer and 5 pm to 10 pm in autumn/winter 23
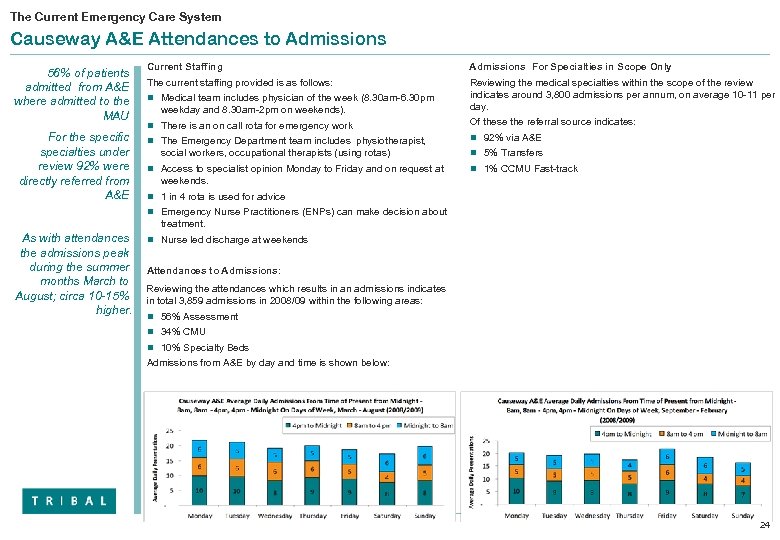 The Current Emergency Care System Causeway A&E Attendances to Admissions 56% of patients admitted from A&E where admitted to the MAU For the specific specialties under review 92% were directly referred from A&E Current Staffing Admissions For Specialties in Scope Only The current staffing provided is as follows: Reviewing the medical specialties within the scope of the review indicates around 3, 800 admissions per annum, on average 10 -11 per day. n Medical team includes physician of the week (8. 30 am-6. 30 pm weekday and 8. 30 am-2 pm on weekends). n There is an on call rota for emergency work Of these the referral source indicates: n The Emergency Department team includes physiotherapist, n 92% via A&E social workers, occupational therapists (using rotas) n Access to specialist opinion Monday to Friday and on request at n 5% Transfers n 1% CCMU Fast-track weekends. n 1 in 4 rota is used for advice n Emergency Nurse Practitioners (ENPs) can make decision about treatment. As with attendances the admissions peak during the summer months March to August; circa 10 -15% higher. n Nurse led discharge at weekends Attendances to Admissions: Reviewing the attendances which results in an admissions indicates in total 3, 859 admissions in 2008/09 within the following areas: n 56% Assessment n 34% CMU n 10% Specialty Beds Admissions from A&E by day and time is shown below: 24
The Current Emergency Care System Causeway A&E Attendances to Admissions 56% of patients admitted from A&E where admitted to the MAU For the specific specialties under review 92% were directly referred from A&E Current Staffing Admissions For Specialties in Scope Only The current staffing provided is as follows: Reviewing the medical specialties within the scope of the review indicates around 3, 800 admissions per annum, on average 10 -11 per day. n Medical team includes physician of the week (8. 30 am-6. 30 pm weekday and 8. 30 am-2 pm on weekends). n There is an on call rota for emergency work Of these the referral source indicates: n The Emergency Department team includes physiotherapist, n 92% via A&E social workers, occupational therapists (using rotas) n Access to specialist opinion Monday to Friday and on request at n 5% Transfers n 1% CCMU Fast-track weekends. n 1 in 4 rota is used for advice n Emergency Nurse Practitioners (ENPs) can make decision about treatment. As with attendances the admissions peak during the summer months March to August; circa 10 -15% higher. n Nurse led discharge at weekends Attendances to Admissions: Reviewing the attendances which results in an admissions indicates in total 3, 859 admissions in 2008/09 within the following areas: n 56% Assessment n 34% CMU n 10% Specialty Beds Admissions from A&E by day and time is shown below: 24
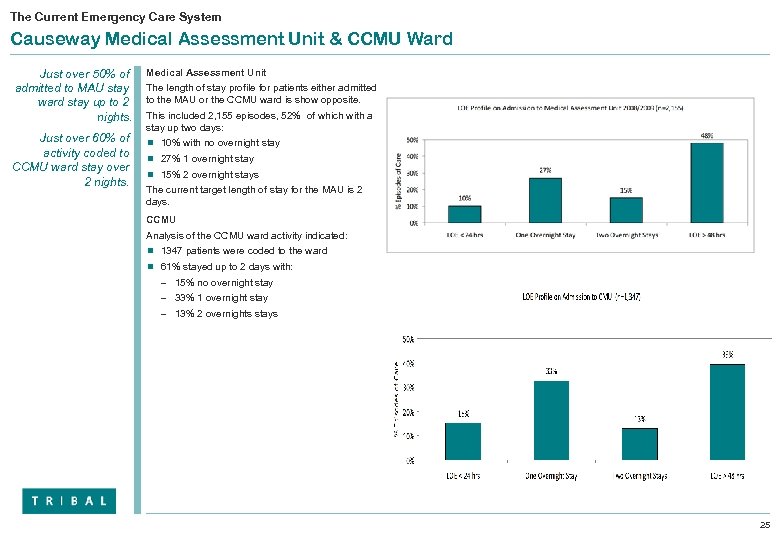 The Current Emergency Care System Causeway Medical Assessment Unit & CCMU Ward Just over 50% of admitted to MAU stay ward stay up to 2 nights. Just over 60% of activity coded to CCMU ward stay over 2 nights. Medical Assessment Unit The length of stay profile for patients either admitted to the MAU or the CCMU ward is show opposite. This included 2, 155 episodes, 52% of which with a stay up two days: n 10% with no overnight stay n 27% 1 overnight stay n 15% 2 overnight stays The current target length of stay for the MAU is 2 days. CCMU Analysis of the CCMU ward activity indicated: n 1347 patients were coded to the ward n 61% stayed up to 2 days with: – 15% no overnight stay – 33% 1 overnight stay – 13% 2 overnights stays 25
The Current Emergency Care System Causeway Medical Assessment Unit & CCMU Ward Just over 50% of admitted to MAU stay ward stay up to 2 nights. Just over 60% of activity coded to CCMU ward stay over 2 nights. Medical Assessment Unit The length of stay profile for patients either admitted to the MAU or the CCMU ward is show opposite. This included 2, 155 episodes, 52% of which with a stay up two days: n 10% with no overnight stay n 27% 1 overnight stay n 15% 2 overnight stays The current target length of stay for the MAU is 2 days. CCMU Analysis of the CCMU ward activity indicated: n 1347 patients were coded to the ward n 61% stayed up to 2 days with: – 15% no overnight stay – 33% 1 overnight stay – 13% 2 overnights stays 25
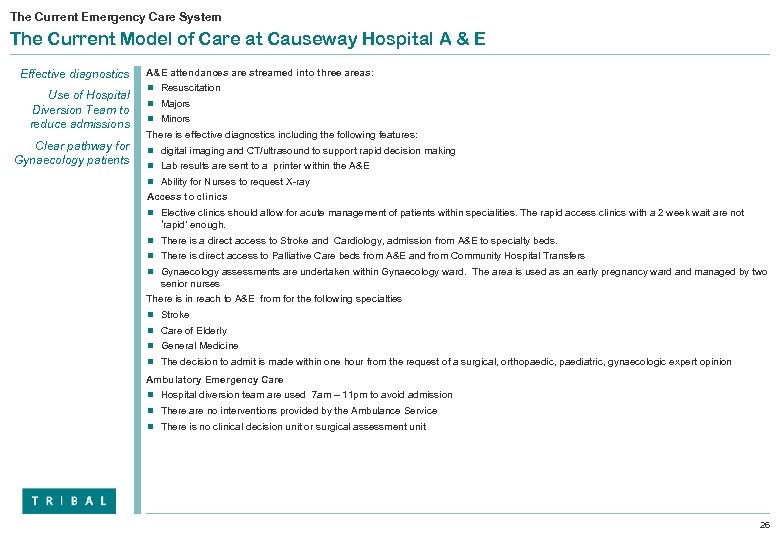 The Current Emergency Care System The Current Model of Care at Causeway Hospital A & E Effective diagnostics Use of Hospital Diversion Team to reduce admissions Clear pathway for Gynaecology patients A&E attendances are streamed into three areas: n Resuscitation n Majors n Minors There is effective diagnostics including the following features: n digital imaging and CT/ultrasound to support rapid decision making n Lab results are sent to a printer within the A&E n Ability for Nurses to request X-ray Access to clinics n Elective clinics should allow for acute management of patients within specialities. The rapid access clinics with a 2 week wait are not ‘rapid’ enough. n There is a direct access to Stroke and Cardiology, admission from A&E to specialty beds. n There is direct access to Palliative Care beds from A&E and from Community Hospital Transfers n Gynaecology assessments are undertaken within Gynaecology ward. The area is used as an early pregnancy ward and managed by two senior nurses There is in reach to A&E from for the following specialties n Stroke n Care of Elderly n General Medicine n The decision to admit is made within one hour from the request of a surgical, orthopaedic, paediatric, gynaecologic expert opinion Ambulatory Emergency Care n Hospital diversion team are used 7 am – 11 pm to avoid admission n There are no interventions provided by the Ambulance Service n There is no clinical decision unit or surgical assessment unit 26
The Current Emergency Care System The Current Model of Care at Causeway Hospital A & E Effective diagnostics Use of Hospital Diversion Team to reduce admissions Clear pathway for Gynaecology patients A&E attendances are streamed into three areas: n Resuscitation n Majors n Minors There is effective diagnostics including the following features: n digital imaging and CT/ultrasound to support rapid decision making n Lab results are sent to a printer within the A&E n Ability for Nurses to request X-ray Access to clinics n Elective clinics should allow for acute management of patients within specialities. The rapid access clinics with a 2 week wait are not ‘rapid’ enough. n There is a direct access to Stroke and Cardiology, admission from A&E to specialty beds. n There is direct access to Palliative Care beds from A&E and from Community Hospital Transfers n Gynaecology assessments are undertaken within Gynaecology ward. The area is used as an early pregnancy ward and managed by two senior nurses There is in reach to A&E from for the following specialties n Stroke n Care of Elderly n General Medicine n The decision to admit is made within one hour from the request of a surgical, orthopaedic, paediatric, gynaecologic expert opinion Ambulatory Emergency Care n Hospital diversion team are used 7 am – 11 pm to avoid admission n There are no interventions provided by the Ambulance Service n There is no clinical decision unit or surgical assessment unit 26
 The Current Emergency Care System Current Model of Care Causeway Hospital A & E The diagnostic routine is functioning well with few delays Access to mental health acute provision an issue The role of the flow coordinator should be expanded to better manage breaches. Mental Health n The mental health provision can be improved as there is limited service provision out of hours is limited and the patients are kept in A&E beds with no mental health medics on site n The service is lead by Community psychiatric nurses who are available 9 -5 pm in A&E. Flow Management/Coordinator: n This post does exist but it is not working optimally. It is felt this role would significantly improve the management of patient flow and managing breaches within the department and allocating resource where required. Outlying to Surgical beds n Recently Surgery stopped taking outliers in last 2 months after removed surgery from Mid Ulster and only permits if an Estimated Discharge Date (EDD) and a discharge letter are provided n The A&E could benefit from creation of surgical assessment room for transfers Information/Monitoring of targets n A manual system is used for bed management information n There are delays in accessing both assessment beds and specialty beds n Twice daily emails regarding bed availability are sent across the Trust n There are online printed manual for all conditions but no tick box pathway protocols n A discharge date is set on admission (where possible). n Performance against 4 hours are close to 90% n The trust has set a 1 hour limit for the surgical specialties to respond within n No reported delays in waiting for a surgical opinion (orthopaedics, paediatrician, gynaecology) obstructs the flow n Operational policies are perceived as success n There are however inappropriate nursing home admissions including end of life care. 27
The Current Emergency Care System Current Model of Care Causeway Hospital A & E The diagnostic routine is functioning well with few delays Access to mental health acute provision an issue The role of the flow coordinator should be expanded to better manage breaches. Mental Health n The mental health provision can be improved as there is limited service provision out of hours is limited and the patients are kept in A&E beds with no mental health medics on site n The service is lead by Community psychiatric nurses who are available 9 -5 pm in A&E. Flow Management/Coordinator: n This post does exist but it is not working optimally. It is felt this role would significantly improve the management of patient flow and managing breaches within the department and allocating resource where required. Outlying to Surgical beds n Recently Surgery stopped taking outliers in last 2 months after removed surgery from Mid Ulster and only permits if an Estimated Discharge Date (EDD) and a discharge letter are provided n The A&E could benefit from creation of surgical assessment room for transfers Information/Monitoring of targets n A manual system is used for bed management information n There are delays in accessing both assessment beds and specialty beds n Twice daily emails regarding bed availability are sent across the Trust n There are online printed manual for all conditions but no tick box pathway protocols n A discharge date is set on admission (where possible). n Performance against 4 hours are close to 90% n The trust has set a 1 hour limit for the surgical specialties to respond within n No reported delays in waiting for a surgical opinion (orthopaedics, paediatrician, gynaecology) obstructs the flow n Operational policies are perceived as success n There are however inappropriate nursing home admissions including end of life care. 27
 The Current Emergency Care System The Current Model of Care Causeway Hospital MAU All patients go from A&E to MAU on average 6 per day. The Model n There are 6 admissions to the MAU per day. This is 56 % of all medical admissions (34% go to CCMU and 10 % to Specialty Beds) n All patients come through A&E n There is no High dependency unit, Short stay ward or Clinical decision unit n The Length of stay should be up to 48 hours. Staffing n 1 wte Physician cover MAU according to a physician of the week model n There are 4 band 7 nurses n The physicians rota arrangement is 1 in 6 week but there is no acute physician. n Specialists present at ward rounds: – Geriatrics present weekends only – All other specialities are present daily. (Stroke, Diabetes nurses, cardiac, respiratory, early discharge team. ) n The discharge pattern is even though the week with but low during weekends. n Social worker is available but no dedicated Physiotherapist n The community and step down beds doesn’t receive patients during weekends. Systems & Processes n Two daily rounds: morning and afternoon, coronary care unit is included in the round. n Physicians for all areas except geriatrics participates on the ward rounds (Physician, Physiotherapist, Pharmacist, Social worker ) n There is a daily ward meeting with the board team. n SOLVER System is used to get input from as many specialists as possible. This process is still in progress. n If the patient is likely to be discharged within 72 hours they will be retained and managed on the MAU. n There is a treatment plan pro forma in use in the MAU n The estimated date of discharge is set in MAU, multi disciplinary team meetings are held morning and evening. n There are no ICPs in use for treatment guidelines. n The lack of isolation wards effects the patient flow n There is a need for more speciality physicians in the intensive care unit so that all patients are seen by professional staff 28
The Current Emergency Care System The Current Model of Care Causeway Hospital MAU All patients go from A&E to MAU on average 6 per day. The Model n There are 6 admissions to the MAU per day. This is 56 % of all medical admissions (34% go to CCMU and 10 % to Specialty Beds) n All patients come through A&E n There is no High dependency unit, Short stay ward or Clinical decision unit n The Length of stay should be up to 48 hours. Staffing n 1 wte Physician cover MAU according to a physician of the week model n There are 4 band 7 nurses n The physicians rota arrangement is 1 in 6 week but there is no acute physician. n Specialists present at ward rounds: – Geriatrics present weekends only – All other specialities are present daily. (Stroke, Diabetes nurses, cardiac, respiratory, early discharge team. ) n The discharge pattern is even though the week with but low during weekends. n Social worker is available but no dedicated Physiotherapist n The community and step down beds doesn’t receive patients during weekends. Systems & Processes n Two daily rounds: morning and afternoon, coronary care unit is included in the round. n Physicians for all areas except geriatrics participates on the ward rounds (Physician, Physiotherapist, Pharmacist, Social worker ) n There is a daily ward meeting with the board team. n SOLVER System is used to get input from as many specialists as possible. This process is still in progress. n If the patient is likely to be discharged within 72 hours they will be retained and managed on the MAU. n There is a treatment plan pro forma in use in the MAU n The estimated date of discharge is set in MAU, multi disciplinary team meetings are held morning and evening. n There are no ICPs in use for treatment guidelines. n The lack of isolation wards effects the patient flow n There is a need for more speciality physicians in the intensive care unit so that all patients are seen by professional staff 28
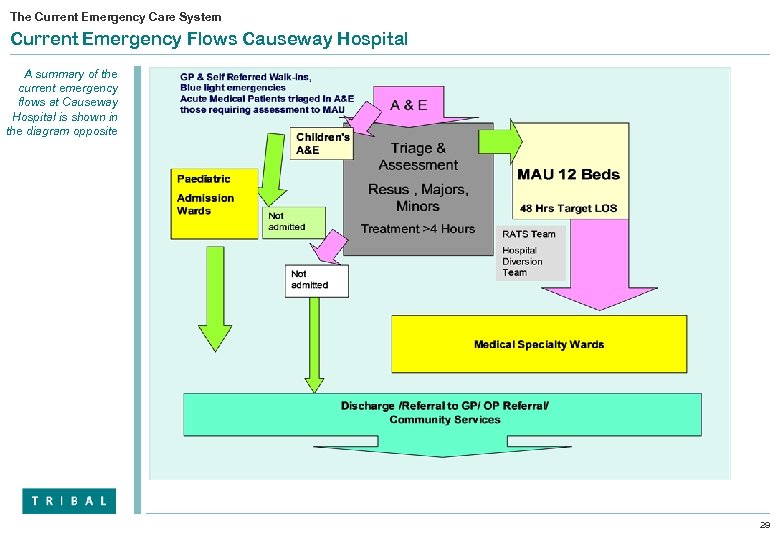 The Current Emergency Care System Current Emergency Flows Causeway Hospital A summary of the current emergency flows at Causeway Hospital is shown in the diagram opposite 29
The Current Emergency Care System Current Emergency Flows Causeway Hospital A summary of the current emergency flows at Causeway Hospital is shown in the diagram opposite 29
 The Current Emergency Care System Causeway Hospital – Issues Emerging from the Review The key object of the review is to assess the efficiency of triage and streaming of patients in the A&E. . Front Door n High level of Urgent Care cases presenting at A&E in 08/09 Triage 4/5 = 24, 000 represents 60% of total a daily average of 65 -70 patients per day n Use of the Manchester triage system ensures standardised mechanism for triage to reduce clinical variation practices. n The self referred & GP referred medical patients are being managed through A&E which is not UK best practice. n Self referred patients being managed through A&E Admissions n There are 3859 non-elective admissions for all medical specialties, excluding Stroke and Myocardial Infarction (MI) there are 3571; of these 56% go to MAU n 10 % of the MAU admissions are discharged within 24 hours n 473 admissions in A&E were ante natal not related to delivery or an event of which 53 were discharged same day (11%). Length of Stay n Average Length of stay (ALOS) in MAU is 2. 0 days compared to the UK average of 0. 8 days Suggestions to improve flow: n Active streaming and management of minors by emergency nurse practitioners in a separate area n All GP referred cases should go direct to MAU n All strokes following assessment and confirmed stroke should go to Hyper Acute Stoke Unit. n All Myocardial Infarctions following confirmed diagnosis should go to CCMU n A care of the elderly service at the front door to manage patients through Care of Elderly assessment beds in the community and establishment of an older people rapid access clinics. 30
The Current Emergency Care System Causeway Hospital – Issues Emerging from the Review The key object of the review is to assess the efficiency of triage and streaming of patients in the A&E. . Front Door n High level of Urgent Care cases presenting at A&E in 08/09 Triage 4/5 = 24, 000 represents 60% of total a daily average of 65 -70 patients per day n Use of the Manchester triage system ensures standardised mechanism for triage to reduce clinical variation practices. n The self referred & GP referred medical patients are being managed through A&E which is not UK best practice. n Self referred patients being managed through A&E Admissions n There are 3859 non-elective admissions for all medical specialties, excluding Stroke and Myocardial Infarction (MI) there are 3571; of these 56% go to MAU n 10 % of the MAU admissions are discharged within 24 hours n 473 admissions in A&E were ante natal not related to delivery or an event of which 53 were discharged same day (11%). Length of Stay n Average Length of stay (ALOS) in MAU is 2. 0 days compared to the UK average of 0. 8 days Suggestions to improve flow: n Active streaming and management of minors by emergency nurse practitioners in a separate area n All GP referred cases should go direct to MAU n All strokes following assessment and confirmed stroke should go to Hyper Acute Stoke Unit. n All Myocardial Infarctions following confirmed diagnosis should go to CCMU n A care of the elderly service at the front door to manage patients through Care of Elderly assessment beds in the community and establishment of an older people rapid access clinics. 30
 4 Opportunities for Improvement using UK Best Practice 31
4 Opportunities for Improvement using UK Best Practice 31
 Opportunities for Improvement Proposed Model of Care CAU is a Combined Assessment Unit for both medical and surgical assessments All GP referrals direct to CAU • Self Referred Walk-ins, & Blue light emergencies direct to A&E • Acute Medical Self Referred Patients triaged In A&E those requiring assessment to CAU A & E Triage See & Treat, Minors Further Assessment Observation Beds Children's A&E MIU Treatment Direct Ambulatory Treatment Triaged SR Medical Patients Rapid Transfer to CAU • All GP referred medical & surgical patients direct to MAU • Patient s admitted to A&E where treatment is >4 hours transfer to CAU Triaged Self referred Cases to MAU for assessment prior to admission/ discharge Not admitted Treated within CAU 24 hours Short Stay Unit Admitted to Specialty Ward with a treatment plan/ EDD Discharged from specialty beds Collaborative Care Teams Discharge /Referral to GP/ OP Referral/ Community Services 32
Opportunities for Improvement Proposed Model of Care CAU is a Combined Assessment Unit for both medical and surgical assessments All GP referrals direct to CAU • Self Referred Walk-ins, & Blue light emergencies direct to A&E • Acute Medical Self Referred Patients triaged In A&E those requiring assessment to CAU A & E Triage See & Treat, Minors Further Assessment Observation Beds Children's A&E MIU Treatment Direct Ambulatory Treatment Triaged SR Medical Patients Rapid Transfer to CAU • All GP referred medical & surgical patients direct to MAU • Patient s admitted to A&E where treatment is >4 hours transfer to CAU Triaged Self referred Cases to MAU for assessment prior to admission/ discharge Not admitted Treated within CAU 24 hours Short Stay Unit Admitted to Specialty Ward with a treatment plan/ EDD Discharged from specialty beds Collaborative Care Teams Discharge /Referral to GP/ OP Referral/ Community Services 32
 Opportunities for Improvement Moving Forward The new model of care should reduce attendances through effective use of alternatives, match resources when most needed and ultimately improve patient experience and outcomes. Using What We Know About Best Practice in the Design and Management of A&E The Vision for the Emergency Department n Appropriate practitioner, right skills and expertise n Rapid access to diagnosis, assessment and treatment n Paediatrics and Adults n 98% compliance on the 4 hour target n Patient experience is good n Clinical outcomes are optimum n Readmission rate is low The Model n Reduce the number of attendances in the medium/ long term n Utilise and create alternatives to admission n Increase ambulatory emergency care The Flows n Segmentation and management of defined flows n Staffing of the flows n Process and systems Protocols and guidelines Resources n Understanding peaks and troughs n Matching staffing resources with demand n Appropriate skills and expertise n Admission rights – responsive specialty input n Availability of beds 33
Opportunities for Improvement Moving Forward The new model of care should reduce attendances through effective use of alternatives, match resources when most needed and ultimately improve patient experience and outcomes. Using What We Know About Best Practice in the Design and Management of A&E The Vision for the Emergency Department n Appropriate practitioner, right skills and expertise n Rapid access to diagnosis, assessment and treatment n Paediatrics and Adults n 98% compliance on the 4 hour target n Patient experience is good n Clinical outcomes are optimum n Readmission rate is low The Model n Reduce the number of attendances in the medium/ long term n Utilise and create alternatives to admission n Increase ambulatory emergency care The Flows n Segmentation and management of defined flows n Staffing of the flows n Process and systems Protocols and guidelines Resources n Understanding peaks and troughs n Matching staffing resources with demand n Appropriate skills and expertise n Admission rights – responsive specialty input n Availability of beds 33
 Opportunities for Improvement Key Issues to consider The key features and issues of the proposed model of care include Segmented flows GP referrals directed to MAU Maximum stay in MAU of 0. 8 day Best Practice Issues to be considered The following strategy is suggested to optimise the flow: Key Issues to be Address in the Proposed Model of Care n GP Referred acute medical patients are directed to the MAU for assessment – the role of emergency medicine n Self referred cases continue to be directed though A&E for n Direct the GP referred admissions to MAU this would potential take around 19 admission from Antrim and 13 from Causeway per day from A&E to MAU initial assessment and work up within four hour period n Segment the flows in A&E n DH Guidance supports 24 maximum LOS for effective assessment function Use of pathways Creating alternatives to admission Key Issues n UK ALOS for MAU is 0. 8 days n The Royal College of Physicians of England’s clear objective is rapid access to speciality based care n The stroke pathway – guidance from A&E to a Hyper Acute Stoke Unit. n Management of MI – Guidance supports from A&E to Coronary care unit primary PCI n Definitive list of ACS pathways which will be provided to model the trolleys/couches etc this will reduce bed days and inpatient beds. n Care of the Elderly consultant input at the front door with options to transfer to assessment beds, intermediate care beds, step down care n Consider how best to manage the Minor Flow – which constitutes 48% (Antrim) and around 60% (Causeway) of the overall attendances at A&E – looking at the best practice management of minor injury and minor illness n Development of ambulatory emergency care – potential for significant reduction in inpatient beds n Development of Gynaecology Direct Referral system and Early Pregnancy Assessment Unit n Creating alternatives to admission. 34
Opportunities for Improvement Key Issues to consider The key features and issues of the proposed model of care include Segmented flows GP referrals directed to MAU Maximum stay in MAU of 0. 8 day Best Practice Issues to be considered The following strategy is suggested to optimise the flow: Key Issues to be Address in the Proposed Model of Care n GP Referred acute medical patients are directed to the MAU for assessment – the role of emergency medicine n Self referred cases continue to be directed though A&E for n Direct the GP referred admissions to MAU this would potential take around 19 admission from Antrim and 13 from Causeway per day from A&E to MAU initial assessment and work up within four hour period n Segment the flows in A&E n DH Guidance supports 24 maximum LOS for effective assessment function Use of pathways Creating alternatives to admission Key Issues n UK ALOS for MAU is 0. 8 days n The Royal College of Physicians of England’s clear objective is rapid access to speciality based care n The stroke pathway – guidance from A&E to a Hyper Acute Stoke Unit. n Management of MI – Guidance supports from A&E to Coronary care unit primary PCI n Definitive list of ACS pathways which will be provided to model the trolleys/couches etc this will reduce bed days and inpatient beds. n Care of the Elderly consultant input at the front door with options to transfer to assessment beds, intermediate care beds, step down care n Consider how best to manage the Minor Flow – which constitutes 48% (Antrim) and around 60% (Causeway) of the overall attendances at A&E – looking at the best practice management of minor injury and minor illness n Development of ambulatory emergency care – potential for significant reduction in inpatient beds n Development of Gynaecology Direct Referral system and Early Pregnancy Assessment Unit n Creating alternatives to admission. 34
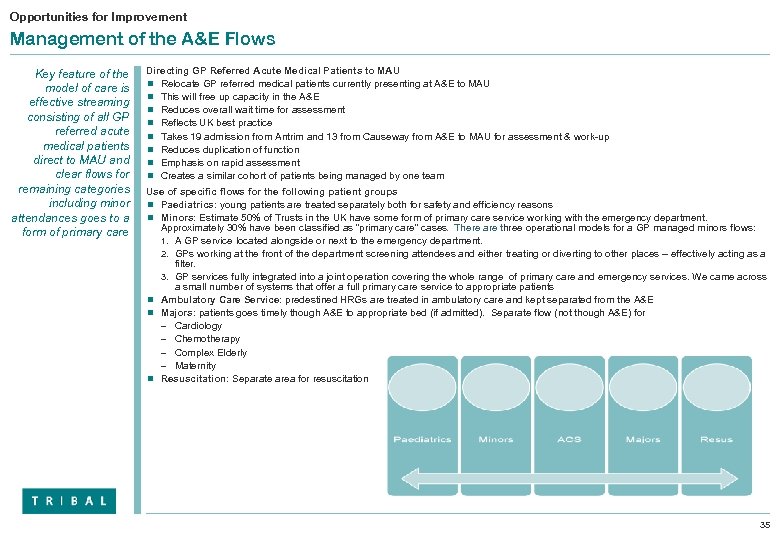 Opportunities for Improvement Management of the A&E Flows Key feature of the model of care is effective streaming consisting of all GP referred acute medical patients direct to MAU and clear flows for remaining categories including minor attendances goes to a form of primary care Directing GP Referred Acute Medical Patients to MAU n Relocate GP referred medical patients currently presenting at A&E to MAU n This will free up capacity in the A&E n Reduces overall wait time for assessment n Reflects UK best practice n Takes 19 admission from Antrim and 13 from Causeway from A&E to MAU for assessment & work-up n Reduces duplication of function n Emphasis on rapid assessment n Creates a similar cohort of patients being managed by one team Use of specific flows for the following patient groups n Paediatrics: young patients are treated separately both for safety and efficiency reasons n Minors: Estimate 50% of Trusts in the UK have some form of primary care service working with the emergency department. Approximately 30% have been classified as “primary care” cases. There are three operational models for a GP managed minors flows: 1. A GP service located alongside or next to the emergency department. 2. GPs working at the front of the department screening attendees and either treating or diverting to other places – effectively acting as a filter. 3. GP services fully integrated into a joint operation covering the whole range of primary care and emergency services. We came across a small number of systems that offer a full primary care service to appropriate patients n Ambulatory Care Service: predestined HRGs are treated in ambulatory care and kept separated from the A&E n Majors: patients goes timely though A&E to appropriate bed (if admitted). Separate flow (not though A&E) for – Cardiology – Chemotherapy – Complex Elderly – Maternity n Resuscitation: Separate area for resuscitation 35
Opportunities for Improvement Management of the A&E Flows Key feature of the model of care is effective streaming consisting of all GP referred acute medical patients direct to MAU and clear flows for remaining categories including minor attendances goes to a form of primary care Directing GP Referred Acute Medical Patients to MAU n Relocate GP referred medical patients currently presenting at A&E to MAU n This will free up capacity in the A&E n Reduces overall wait time for assessment n Reflects UK best practice n Takes 19 admission from Antrim and 13 from Causeway from A&E to MAU for assessment & work-up n Reduces duplication of function n Emphasis on rapid assessment n Creates a similar cohort of patients being managed by one team Use of specific flows for the following patient groups n Paediatrics: young patients are treated separately both for safety and efficiency reasons n Minors: Estimate 50% of Trusts in the UK have some form of primary care service working with the emergency department. Approximately 30% have been classified as “primary care” cases. There are three operational models for a GP managed minors flows: 1. A GP service located alongside or next to the emergency department. 2. GPs working at the front of the department screening attendees and either treating or diverting to other places – effectively acting as a filter. 3. GP services fully integrated into a joint operation covering the whole range of primary care and emergency services. We came across a small number of systems that offer a full primary care service to appropriate patients n Ambulatory Care Service: predestined HRGs are treated in ambulatory care and kept separated from the A&E n Majors: patients goes timely though A&E to appropriate bed (if admitted). Separate flow (not though A&E) for – Cardiology – Chemotherapy – Complex Elderly – Maternity n Resuscitation: Separate area for resuscitation 35
 Opportunities for Improvement Options for the Management of the Care of Elderly Care of the Elderly improvements to the model of care fundamental given the aging profile and significant pressure this specialty has on the unscheduled care Care of the Elderly n Options for the management of elderly patients n Use of care of elderly – geriatrician led rapid access clinics n Refer to care of the elderly assessment beds n Use of intermediate care coordinators in- reaching to A&E / MAU n Refer to intermediate care beds n Refer to palliative care , end of life care n Refer for social work assessment n Collaborative care team / home care package 36
Opportunities for Improvement Options for the Management of the Care of Elderly Care of the Elderly improvements to the model of care fundamental given the aging profile and significant pressure this specialty has on the unscheduled care Care of the Elderly n Options for the management of elderly patients n Use of care of elderly – geriatrician led rapid access clinics n Refer to care of the elderly assessment beds n Use of intermediate care coordinators in- reaching to A&E / MAU n Refer to intermediate care beds n Refer to palliative care , end of life care n Refer for social work assessment n Collaborative care team / home care package 36
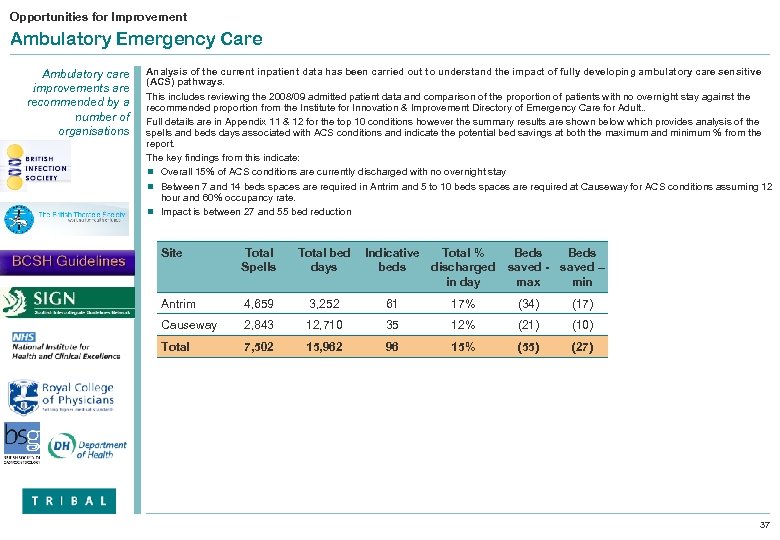 Opportunities for Improvement Ambulatory Emergency Care Ambulatory care improvements are recommended by a number of organisations Analysis of the current inpatient data has been carried out to understand the impact of fully developing ambulatory care sensitive (ACS) pathways. This includes reviewing the 2008/09 admitted patient data and comparison of the proportion of patients with no overnight stay against the recommended proportion from the Institute for Innovation & Improvement Directory of Emergency Care for Adult. . Full details are in Appendix 11 & 12 for the top 10 conditions however the summary results are shown below which provides analysis of the spells and beds days associated with ACS conditions and indicate the potential bed savings at both the maximum and minimum % from the report. The key findings from this indicate: n Overall 15% of ACS conditions are currently discharged with no overnight stay n Between 7 and 14 beds spaces are required in Antrim and 5 to 10 beds spaces are required at Causeway for ACS conditions assuming 12 hour and 60% occupancy rate. n Impact is between 27 and 55 bed reduction Site Total Spells Total bed days Indicative Total % beds discharged in day Beds saved - saved – max min Antrim 4, 659 3, 252 61 17% (34) (17) Causeway 2, 843 12, 710 35 12% (21) (10) Total 7, 502 15, 962 96 15% (55) (27) 37
Opportunities for Improvement Ambulatory Emergency Care Ambulatory care improvements are recommended by a number of organisations Analysis of the current inpatient data has been carried out to understand the impact of fully developing ambulatory care sensitive (ACS) pathways. This includes reviewing the 2008/09 admitted patient data and comparison of the proportion of patients with no overnight stay against the recommended proportion from the Institute for Innovation & Improvement Directory of Emergency Care for Adult. . Full details are in Appendix 11 & 12 for the top 10 conditions however the summary results are shown below which provides analysis of the spells and beds days associated with ACS conditions and indicate the potential bed savings at both the maximum and minimum % from the report. The key findings from this indicate: n Overall 15% of ACS conditions are currently discharged with no overnight stay n Between 7 and 14 beds spaces are required in Antrim and 5 to 10 beds spaces are required at Causeway for ACS conditions assuming 12 hour and 60% occupancy rate. n Impact is between 27 and 55 bed reduction Site Total Spells Total bed days Indicative Total % beds discharged in day Beds saved - saved – max min Antrim 4, 659 3, 252 61 17% (34) (17) Causeway 2, 843 12, 710 35 12% (21) (10) Total 7, 502 15, 962 96 15% (55) (27) 37
 The Scope for Improvement – Development of Early Pregnancy Assessment Unit & Gynaecology Direct Referral system Establishing an Early Pregnancy Assessment Unit in Antrim to treat direct Gynaecology referrals n At Antrim, currently all early pregnancy patients and gynaecology emergencies are directed through the A&E. At Causeway there is an Early Pregnancy Assessment Unit (EPAU) n In 2008/09 there were 532 spells of antenatal admissions in Antrim not related to a delivery presenting through A&E utilising 1283 occupied bed days only 12% were discharged within 24 hours of admission. n This HRG is clearly an ambulatory case sensitive (ACS) condition and the estimates based on the clinical evidence are that 30% to 60% of those patients could be managed through an EPAU, reducing the Occupied bed Days (OBDs) by almost 2 inpatient beds, improving the patient experience and reducing the burden on the A&E service by on average 2 cases per day. Emergency gynaecology / Early Pregnancy Assessment Unit service n A 24 hour consultant-led service for early pregnancy and emergency gynaecology that incorporates a 09. 00 – 17. 00 appointment service for direct referral from GPs. n Services provide assessment and management of early pregnancy problems, including early pregnancy bleeding up to 12 weeks’ gestation. n Units are part of the gynaecology department 38
The Scope for Improvement – Development of Early Pregnancy Assessment Unit & Gynaecology Direct Referral system Establishing an Early Pregnancy Assessment Unit in Antrim to treat direct Gynaecology referrals n At Antrim, currently all early pregnancy patients and gynaecology emergencies are directed through the A&E. At Causeway there is an Early Pregnancy Assessment Unit (EPAU) n In 2008/09 there were 532 spells of antenatal admissions in Antrim not related to a delivery presenting through A&E utilising 1283 occupied bed days only 12% were discharged within 24 hours of admission. n This HRG is clearly an ambulatory case sensitive (ACS) condition and the estimates based on the clinical evidence are that 30% to 60% of those patients could be managed through an EPAU, reducing the Occupied bed Days (OBDs) by almost 2 inpatient beds, improving the patient experience and reducing the burden on the A&E service by on average 2 cases per day. Emergency gynaecology / Early Pregnancy Assessment Unit service n A 24 hour consultant-led service for early pregnancy and emergency gynaecology that incorporates a 09. 00 – 17. 00 appointment service for direct referral from GPs. n Services provide assessment and management of early pregnancy problems, including early pregnancy bleeding up to 12 weeks’ gestation. n Units are part of the gynaecology department 38
 Opportunities for Improvement Diagnostic Support Improvements to diagnostics n Dedicated slots in imaging including Ultra Sound (US) and computerised tomography (CT) where delays are likely to contribute to breaches n Point -of -care -test (POCT) in A&E and MAU n Dedicated slots for endoscopy emergencies and “urgents” n Use of rapid access clinics n Dedicated slots in OP clinics n Care of the elderly consultant sessions in the A&E to “pull “ out from the A&E those patients who require assessment by a geriatrician rather than admission to an acute medical bed. n Use of the community hospital beds for , care of the elderly assessment step down and rehabilitation n Longer term the development of collaborative care teams (CCT) and better utilisation of the existing Rapid Access Teams to pick patients up at the front door & take home with support, home care packages. 39
Opportunities for Improvement Diagnostic Support Improvements to diagnostics n Dedicated slots in imaging including Ultra Sound (US) and computerised tomography (CT) where delays are likely to contribute to breaches n Point -of -care -test (POCT) in A&E and MAU n Dedicated slots for endoscopy emergencies and “urgents” n Use of rapid access clinics n Dedicated slots in OP clinics n Care of the elderly consultant sessions in the A&E to “pull “ out from the A&E those patients who require assessment by a geriatrician rather than admission to an acute medical bed. n Use of the community hospital beds for , care of the elderly assessment step down and rehabilitation n Longer term the development of collaborative care teams (CCT) and better utilisation of the existing Rapid Access Teams to pick patients up at the front door & take home with support, home care packages. 39
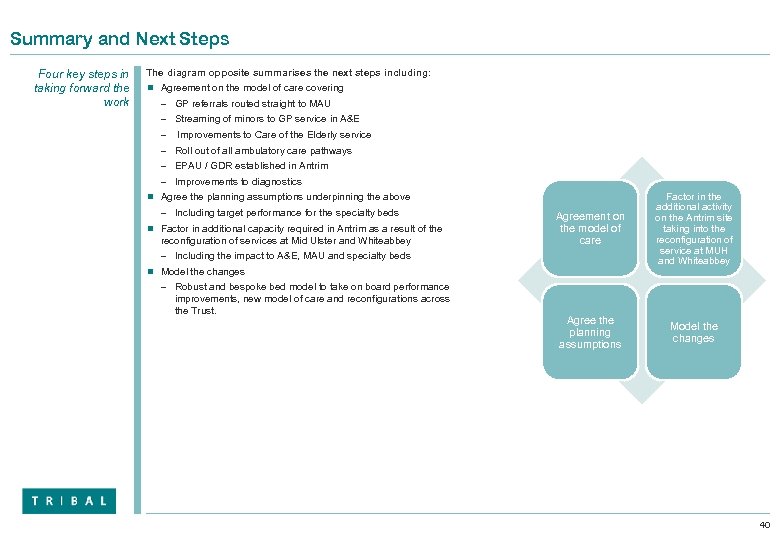 Summary and Next Steps Four key steps in taking forward the work The diagram opposite summarises the next steps including: n Agreement on the model of care covering – GP referrals routed straight to MAU – Streaming of minors to GP service in A&E – Improvements to Care of the Elderly service – Roll out of all ambulatory care pathways – EPAU / GDR established in Antrim – Improvements to diagnostics Agreement on the model of care Factor in the additional activity on the Antrim site taking into the reconfiguration of service at MUH and Whiteabbey Agree the planning assumptions Model the changes n Agree the planning assumptions underpinning the above – Including target performance for the specialty beds n Factor in additional capacity required in Antrim as a result of the reconfiguration of services at Mid Ulster and Whiteabbey – Including the impact to A&E, MAU and specialty beds n Model the changes – Robust and bespoke bed model to take on board performance improvements, new model of care and reconfigurations across the Trust. 40
Summary and Next Steps Four key steps in taking forward the work The diagram opposite summarises the next steps including: n Agreement on the model of care covering – GP referrals routed straight to MAU – Streaming of minors to GP service in A&E – Improvements to Care of the Elderly service – Roll out of all ambulatory care pathways – EPAU / GDR established in Antrim – Improvements to diagnostics Agreement on the model of care Factor in the additional activity on the Antrim site taking into the reconfiguration of service at MUH and Whiteabbey Agree the planning assumptions Model the changes n Agree the planning assumptions underpinning the above – Including target performance for the specialty beds n Factor in additional capacity required in Antrim as a result of the reconfiguration of services at Mid Ulster and Whiteabbey – Including the impact to A&E, MAU and specialty beds n Model the changes – Robust and bespoke bed model to take on board performance improvements, new model of care and reconfigurations across the Trust. 40
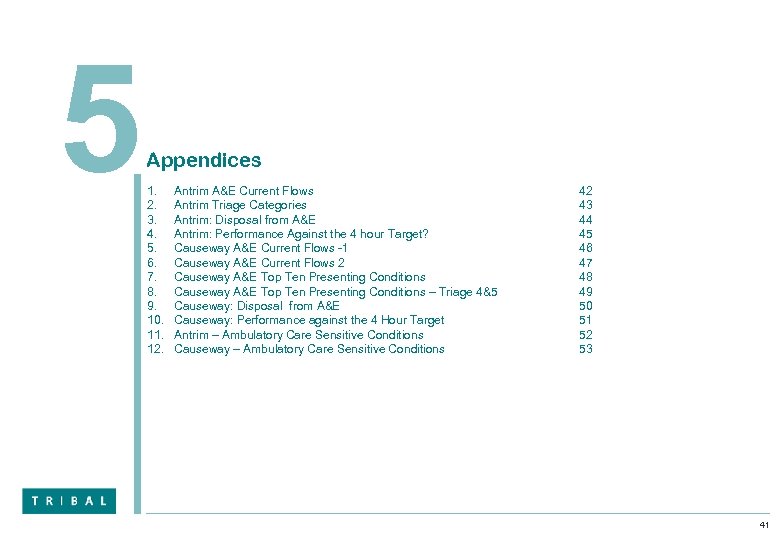 5 Appendices 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Antrim A&E Current Flows Antrim Triage Categories Antrim: Disposal from A&E Antrim: Performance Against the 4 hour Target? Causeway A&E Current Flows -1 Causeway A&E Current Flows 2 Causeway A&E Top Ten Presenting Conditions – Triage 4&5 Causeway: Disposal from A&E Causeway: Performance against the 4 Hour Target Antrim – Ambulatory Care Sensitive Conditions Causeway – Ambulatory Care Sensitive Conditions 42 43 44 45 46 47 48 49 50 51 52 53 41
5 Appendices 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Antrim A&E Current Flows Antrim Triage Categories Antrim: Disposal from A&E Antrim: Performance Against the 4 hour Target? Causeway A&E Current Flows -1 Causeway A&E Current Flows 2 Causeway A&E Top Ten Presenting Conditions – Triage 4&5 Causeway: Disposal from A&E Causeway: Performance against the 4 Hour Target Antrim – Ambulatory Care Sensitive Conditions Causeway – Ambulatory Care Sensitive Conditions 42 43 44 45 46 47 48 49 50 51 52 53 41
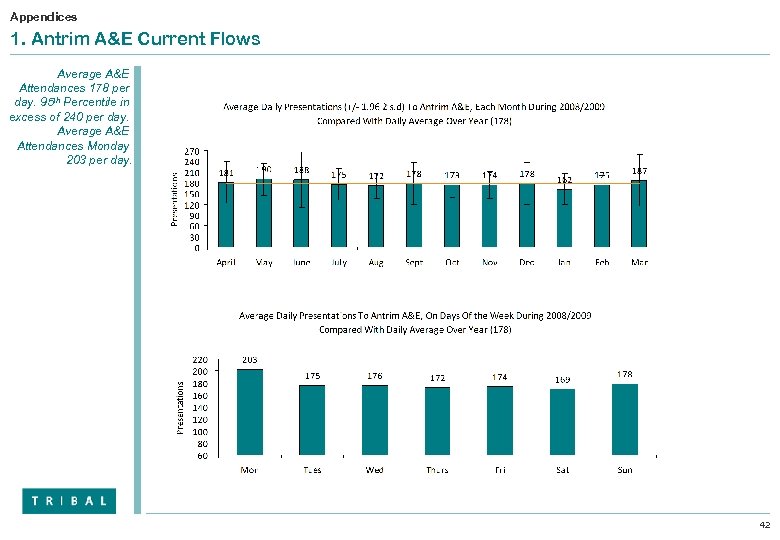 Appendices 1. Antrim A&E Current Flows Average A&E Attendances 178 per day. 95 th Percentile in excess of 240 per day. Average A&E Attendances Monday 203 per day. 42
Appendices 1. Antrim A&E Current Flows Average A&E Attendances 178 per day. 95 th Percentile in excess of 240 per day. Average A&E Attendances Monday 203 per day. 42
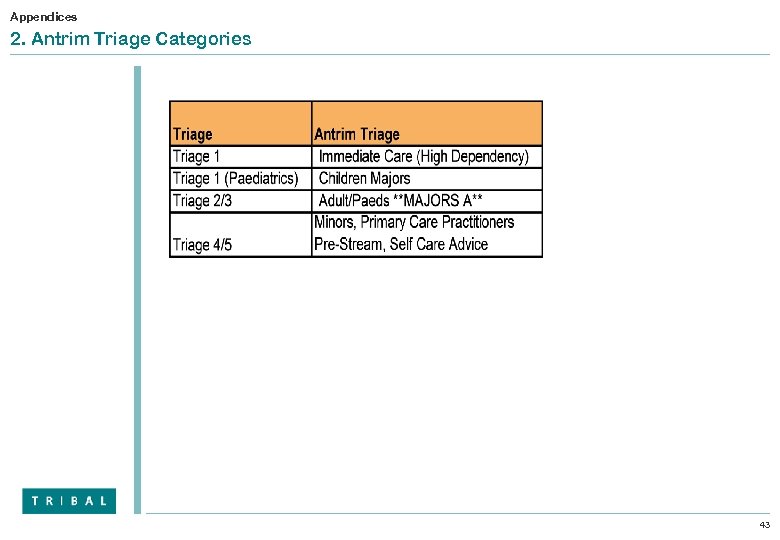 Appendices 2. Antrim Triage Categories 43
Appendices 2. Antrim Triage Categories 43
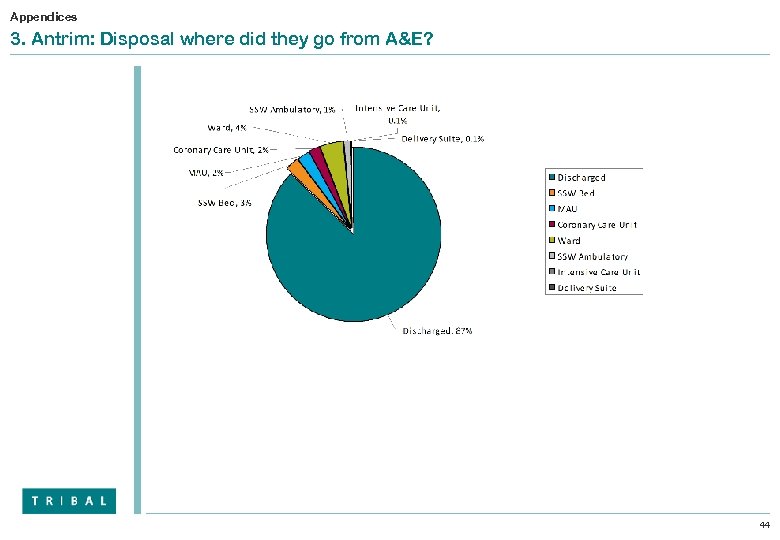 Appendices 3. Antrim: Disposal where did they go from A&E? 44
Appendices 3. Antrim: Disposal where did they go from A&E? 44
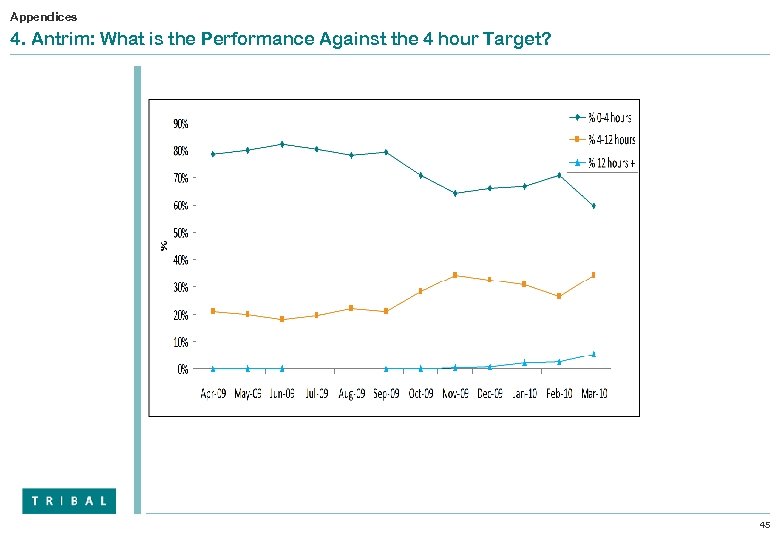 Appendices 4. Antrim: What is the Performance Against the 4 hour Target? 45
Appendices 4. Antrim: What is the Performance Against the 4 hour Target? 45
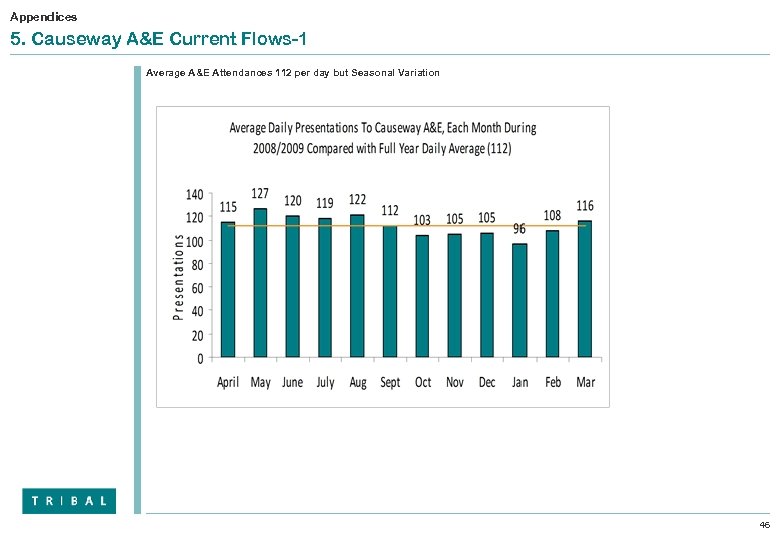 Appendices 5. Causeway A&E Current Flows-1 Average A&E Attendances 112 per day but Seasonal Variation 46
Appendices 5. Causeway A&E Current Flows-1 Average A&E Attendances 112 per day but Seasonal Variation 46
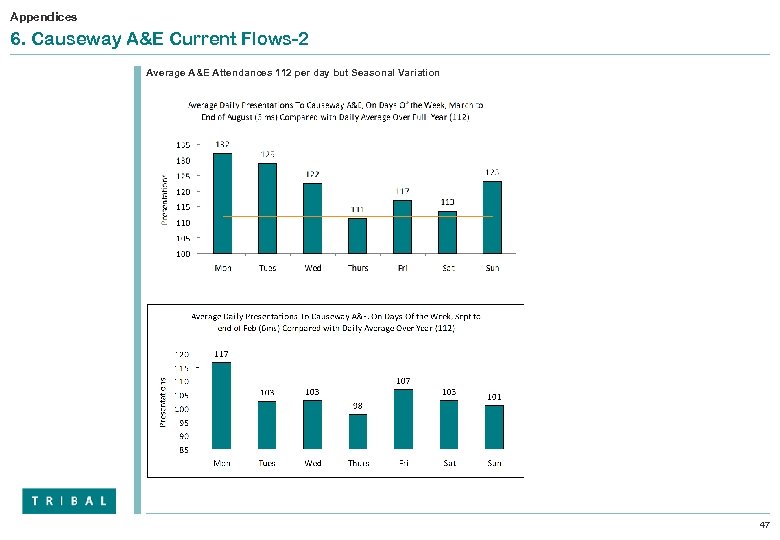 Appendices 6. Causeway A&E Current Flows-2 Average A&E Attendances 112 per day but Seasonal Variation 47
Appendices 6. Causeway A&E Current Flows-2 Average A&E Attendances 112 per day but Seasonal Variation 47
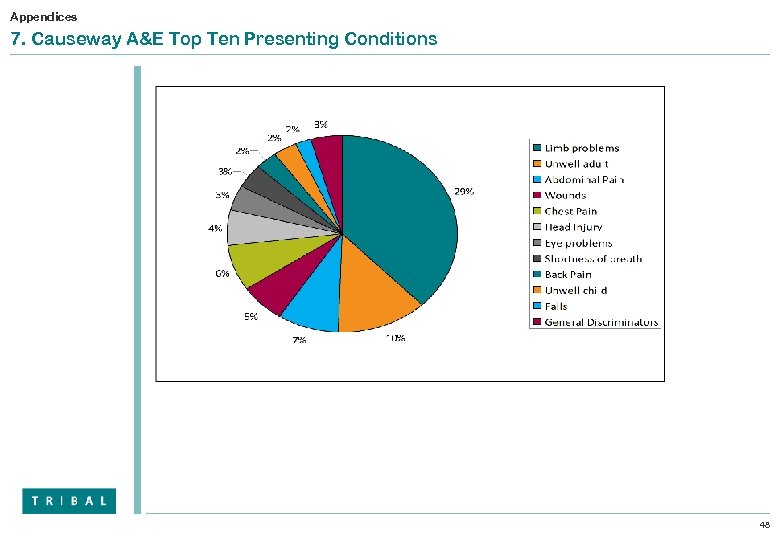 Appendices 7. Causeway A&E Top Ten Presenting Conditions 48
Appendices 7. Causeway A&E Top Ten Presenting Conditions 48
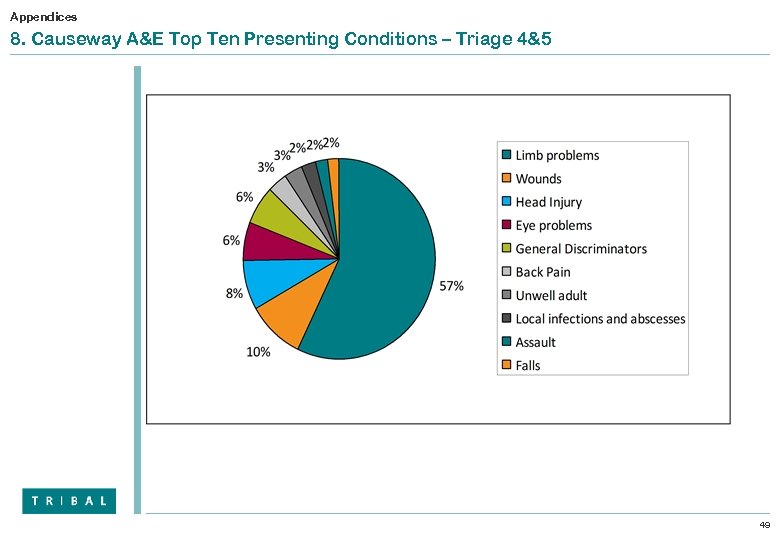 Appendices 8. Causeway A&E Top Ten Presenting Conditions – Triage 4&5 49
Appendices 8. Causeway A&E Top Ten Presenting Conditions – Triage 4&5 49
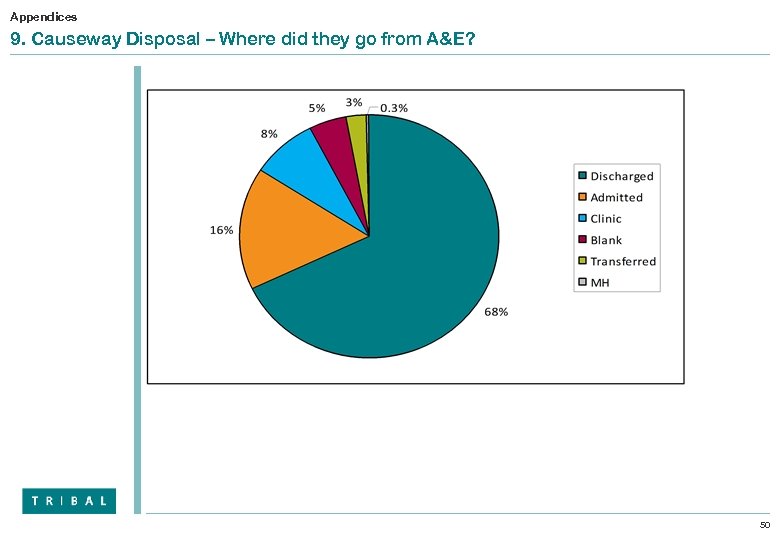 Appendices 9. Causeway Disposal – Where did they go from A&E? 50
Appendices 9. Causeway Disposal – Where did they go from A&E? 50
 Appendices 10. Causeway: What is the Performance against the 4 Hour Target? 51
Appendices 10. Causeway: What is the Performance against the 4 Hour Target? 51
 Appendices 11. Antrim – Ambulatory Care Sensitive Conditions 52
Appendices 11. Antrim – Ambulatory Care Sensitive Conditions 52
 Appendices 12. Causeway - Ambulatory Care Sensitive Conditions 53
Appendices 12. Causeway - Ambulatory Care Sensitive Conditions 53


