2282bed5b15849aa0bd4e460bd7273a1.ppt
- Количество слайдов: 36
Dr. Huda Anan Habib
Every year 529, 000 women die as a direct result of being pregnant-99% of them in the developing world. In turn, these deaths contribute to the deaths of at least 1. 5 million infants in the first week of life and 1. 4 million still babies. The tragedy is that almost all of these deaths could be prevented through the provision of some of the most basic health care measures.
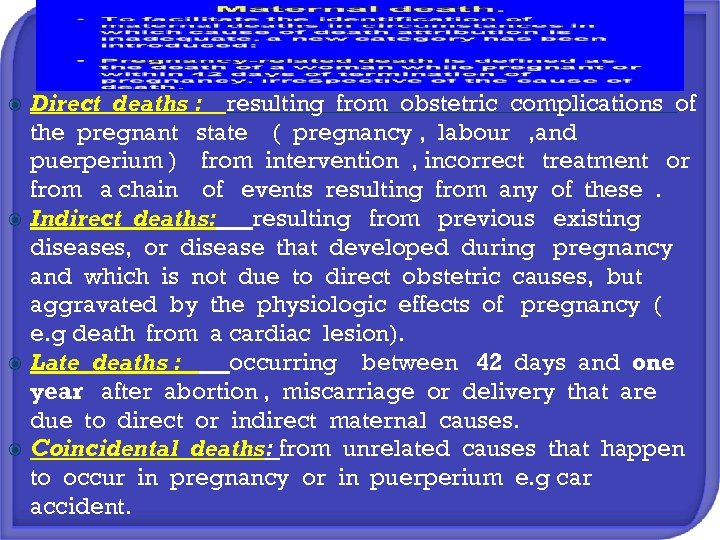
Direct deaths : resulting from obstetric complications of the pregnant state ( pregnancy , labour , and puerperium ) from intervention , incorrect treatment or from a chain of events resulting from any of these. Indirect deaths: resulting from previous existing diseases, or disease that developed during pregnancy and which is not due to direct obstetric causes, but aggravated by the physiologic effects of pregnancy ( e. g death from a cardiac lesion). Late deaths : occurring between 42 days and one year after abortion , miscarriage or delivery that are due to direct or indirect maternal causes. Coincidental deaths: from unrelated causes that happen to occur in pregnancy or in puerperium e. g car accident.

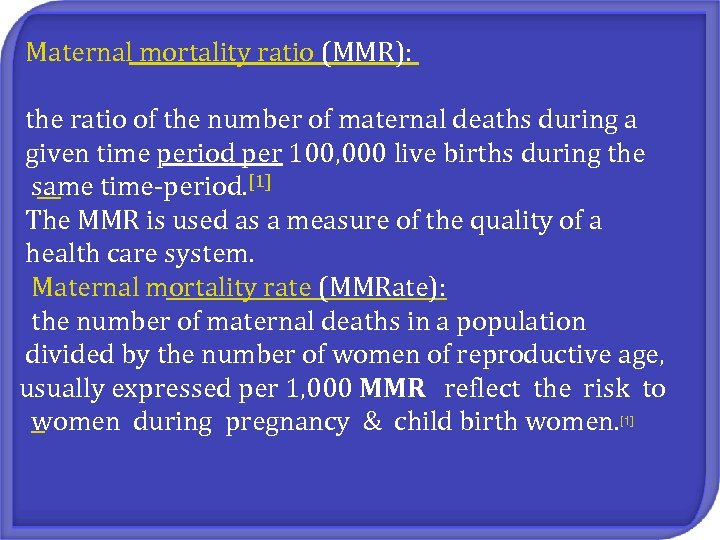
Maternal mortality ratio (MMR): the ratio of the number of maternal deaths during a given time period per 100, 000 live births during the same time-period. [1] The MMR is used as a measure of the quality of a health care system. Maternal mortality rate (MMRate): the number of maternal deaths in a population divided by the number of women of reproductive age, usually expressed per 1, 000 MMR reflect the risk to women during pregnancy & child birth women. [1]
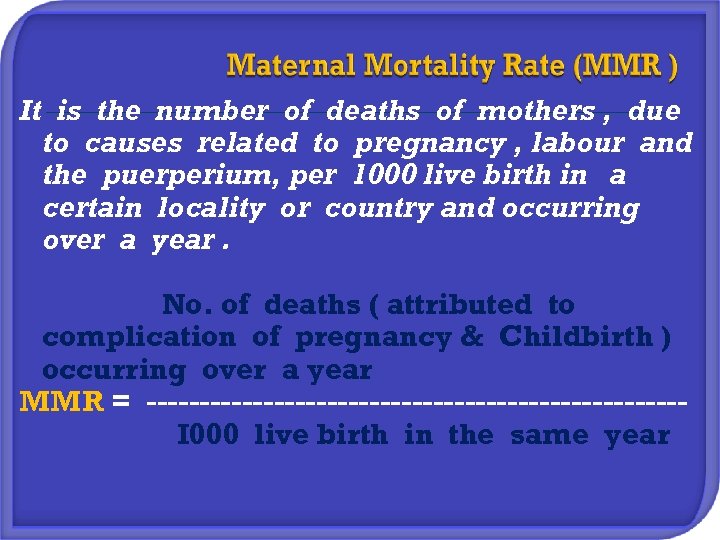
It is the number of deaths of mothers , due to causes related to pregnancy , labour and the puerperium, per 1000 live birth in a certain locality or country and occurring over a year. No. of deaths ( attributed to complication of pregnancy & Childbirth ) occurring over a year MMR = -------------------------I 000 live birth in the same year
MMR reflect the risk to women during pregnancy & child birth. it is influenced by : General socioeconomic condition Nutrition Sanitation Maternal health care
Women die as a result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy. Other complications may exist before pregnancy but are worsened during pregnancy. The major complications that account for nearly 75% of all maternal deaths are: severe bleeding (mostly bleeding after childbirth) infections (usually after childbirth) high blood pressure during pregnancy (pre-eclampsia and eclampsia) complications from delivery unsafe abortion.

Millennium Development Goal 5 calls for an improvement in maternal health and reduction in maternal mortality by 75% by 2015 from 1990 levels.
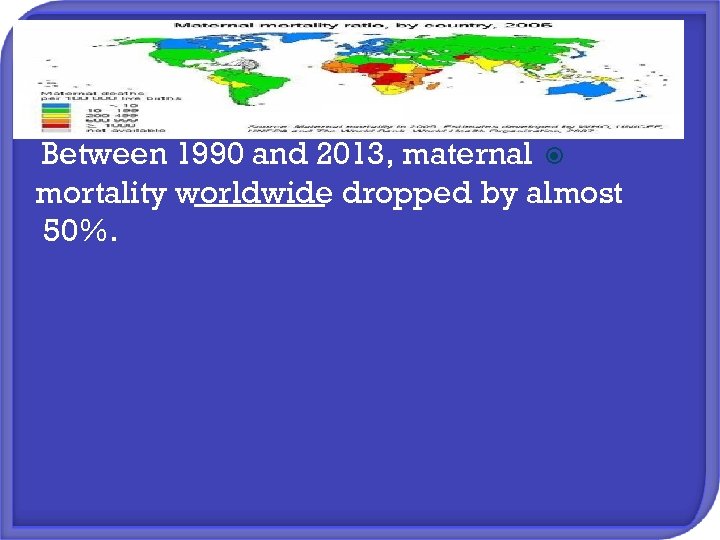
Between 1990 and 2013, maternal mortality worldwide dropped by almost 50%.

To improve maternal health, barriers that limit access to quality maternal health services must be identified and addressed at all levels of the health system.
Why do women not get the care they need? Poor women in remote areas are the least likely to receive adequate health care. This is especially true for regions with low numbers of skilled health workers, such as sub-Saharan Africa and South Asia. In high-income countries, virtually all women have at least 4 antenatal care visits, are attended by a skilled health worker during childbirth and receive postpartum care. In low-income countries, just over a third of all pregnant women have the recommended 4 antenatal care visits.
So factors that prevent women from receiving or seeking care during pregnancy and childbirth are: poverty distance lack of information inadequate services cultural practices.
Most of maternal deaths could be prevented if women have: § Access to basic medical care during pregnancy , childbirth & postpartum period. § Skilled attendance of birth. most maternal deaths occur either during or shortly after delivery § High quality of postpartum care : health care immediately after a critical period of labor & delivery is a single most important intervention for preventing maternal mortality & newborn morbidity & mortality
Safe motherhood project aims to reduce MMR & perinatal death through providing: q Care by skilled health personnel before, during and after childbirth. Emergency care for life – threatening obstetric complication. Service to prevent and manage the complications of unsafe abortion. Family planning to enable women to plane their pregnancies and prevent unwanted pregnancies. Health education and services for adolescents. Community education for women , their families and decision makers. q q q
full term infant : infant born between 37 -42 week of gestation calculated from the LMP preterm birth ( premature birth ) : an infant born before the end of the 37 th week of pregnancy, calculated from the first day of the LMP. Low birth weight (LBW) : is a live borne baby weight less than 2500 grams ( 5 pounds & 8 ounces ). Very low birth weight : is a live borne baby weight less than 1500 grams ( 3 pounds & 5 ounces ).
Small for date babies : an infant borne with birth weight under the 10 th percentile line or 2 SD below the mean body weight for gestational age ( it is a sign of IUGR). Large for date babies : an infant borne above the 90 th percentile line or 2 SD above the mean body weight for certain gestational age.
Live birth : any baby that shows signs of life irrespective of gestation age. Still birth : a baby born with no sign of life ( dead ) at ≥ 24 weeks gestational age. Abortion ( miscarriage) : loss of products of conception occurring any time between implantation & 24 weeks gestational age.
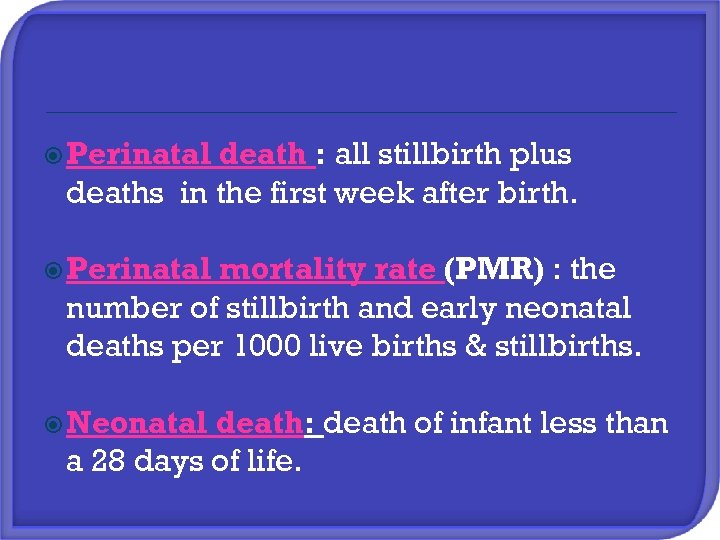
Perinatal death : all stillbirth plus deaths in the first week after birth. Perinatal mortality rate (PMR) : the number of stillbirth and early neonatal deaths per 1000 live births & stillbirths. Neonatal death: death of infant less than a 28 days of life.
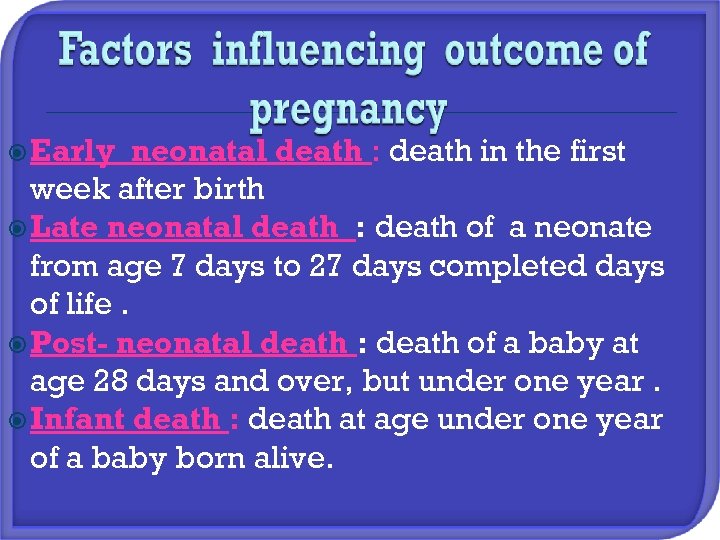
Early neonatal death : death in the first week after birth Late neonatal death : death of a neonate from age 7 days to 27 days completed days of life. Post- neonatal death : death of a baby at age 28 days and over, but under one year. Infant death : death at age under one year of a baby born alive.
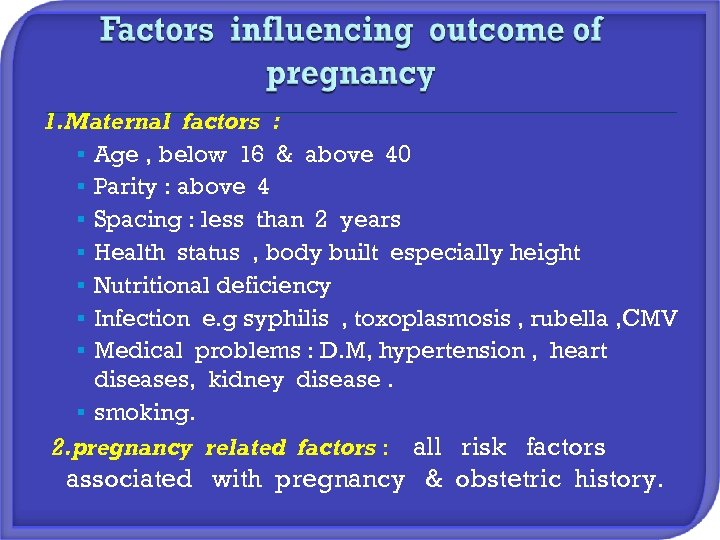
1. Maternal factors : § Age , below 16 & above 40 § Parity : above 4 § Spacing : less than 2 years § Health status , body built especially height § Nutritional deficiency § Infection e. g syphilis , toxoplasmosis , rubella , CMV § Medical problems : D. M, hypertension , heart diseases, kidney disease. § smoking. 2. pregnancy related factors : all risk factors associated with pregnancy & obstetric history.
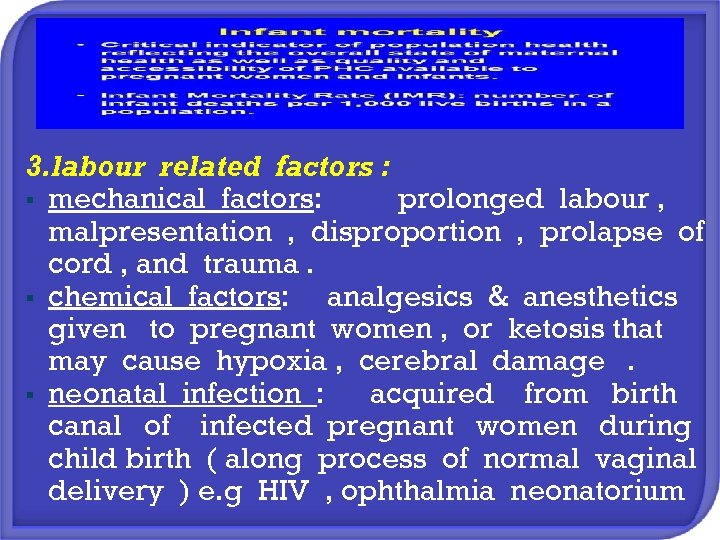
3. labour related factors : § mechanical factors: prolonged labour , malpresentation , disproportion , prolapse of cord , and trauma. § chemical factors: analgesics & anesthetics given to pregnant women , or ketosis that may cause hypoxia , cerebral damage. § neonatal infection : acquired from birth canal of infected pregnant women during child birth ( along process of normal vaginal delivery ) e. g HIV , ophthalmia neonatorium
4. fetal factors : that result from genetic ( inheritance problems) 5. Socioeconomic circumstances : may indirectly have adverse effect on outcome § low income & poor living condition § illiteracy or low education. § faulty tradition. § lack of medical care.


Improving maternal health is 1 of the 8 Millennium Development Goals (MDGs) adopted by the international community in 2000. Under MDG 5, countries committed to reducing maternal mortality by three quarters between 1990 and 2015. Since 1990, maternal deaths worldwide have dropped by 45%.
In sub-Saharan Africa, a number of countries have halved their levels of maternal mortality since 1990. In other regions, including Asia and North Africa, even greater headway has been made. However, between 1990 and 2013, the global maternal mortality ratio (i. e. the number of maternal deaths per 100 000 live births) declined by only 2. 6% per year. This is far from the annual decline of 5. 5% required to achieve MDG 5.
2282bed5b15849aa0bd4e460bd7273a1.ppt