Myelodysplastic Syndromes.pptx
- Количество слайдов: 44
 Dr. Fineman MYELODYSPLASTIC SYNDROMES
Dr. Fineman MYELODYSPLASTIC SYNDROMES
 MDS • Clonal stem cell disorders • Maturation defects • Ineffective hematopoiesis • Blood cytopenias • Risk of transformation to AML
MDS • Clonal stem cell disorders • Maturation defects • Ineffective hematopoiesis • Blood cytopenias • Risk of transformation to AML
 FEATURES USED TO DEFINE MDS • Blood cytopenias • Ineffective hematopoiesis • Dyserythropoiesis • Dysgranulopoiesis • Dysmegakaryopoiesis • Increased myeloblasts
FEATURES USED TO DEFINE MDS • Blood cytopenias • Ineffective hematopoiesis • Dyserythropoiesis • Dysgranulopoiesis • Dysmegakaryopoiesis • Increased myeloblasts
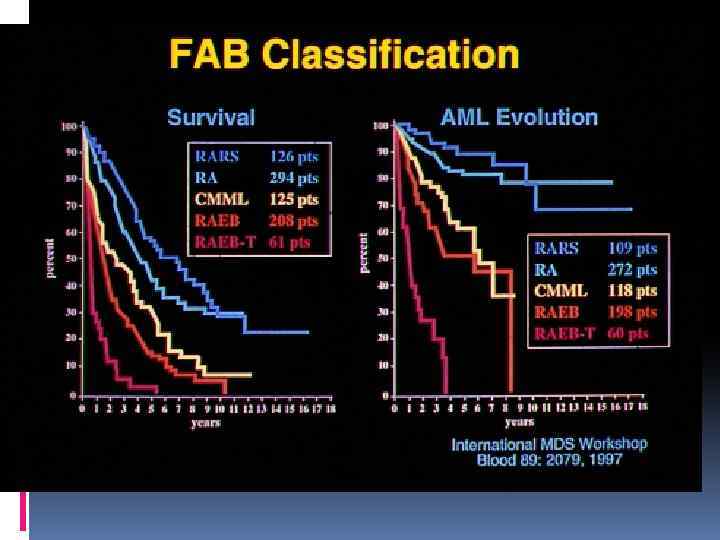
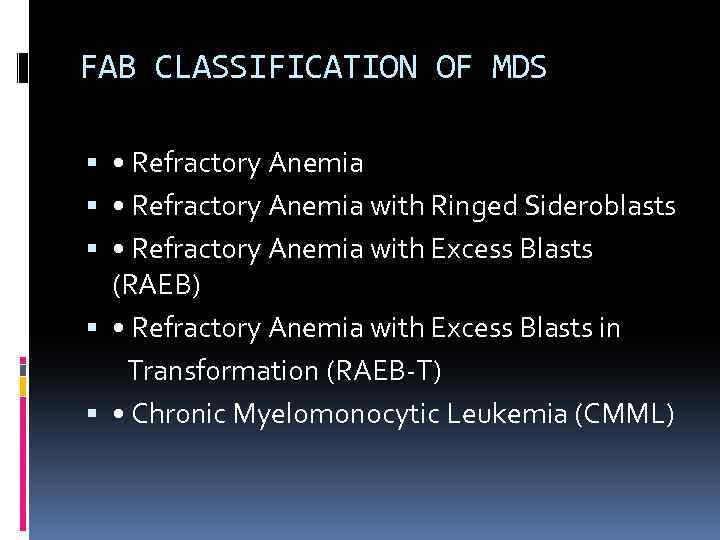 FAB CLASSIFICATION OF MDS • Refractory Anemia with Ringed Sideroblasts • Refractory Anemia with Excess Blasts (RAEB) • Refractory Anemia with Excess Blasts in Transformation (RAEB-T) • Chronic Myelomonocytic Leukemia (CMML)
FAB CLASSIFICATION OF MDS • Refractory Anemia with Ringed Sideroblasts • Refractory Anemia with Excess Blasts (RAEB) • Refractory Anemia with Excess Blasts in Transformation (RAEB-T) • Chronic Myelomonocytic Leukemia (CMML)
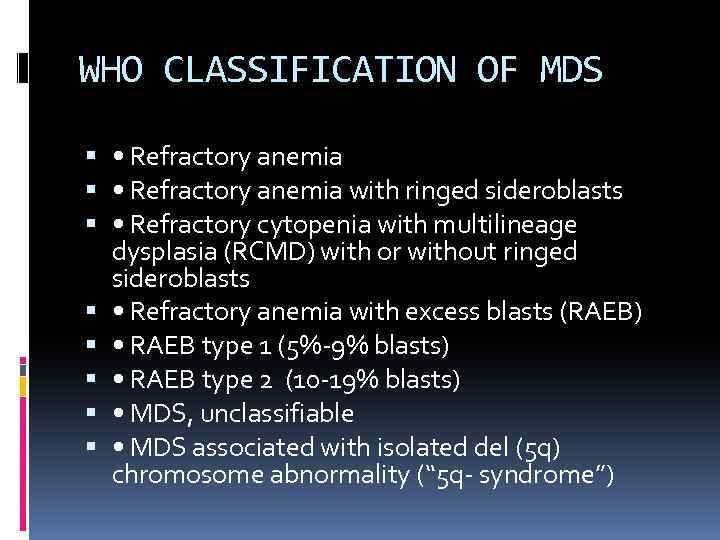 WHO CLASSIFICATION OF MDS • Refractory anemia with ringed sideroblasts • Refractory cytopenia with multilineage dysplasia (RCMD) with or without ringed sideroblasts • Refractory anemia with excess blasts (RAEB) • RAEB type 1 (5%-9% blasts) • RAEB type 2 (10 -19% blasts) • MDS, unclassifiable • MDS associated with isolated del (5 q) chromosome abnormality (“ 5 q- syndrome”)
WHO CLASSIFICATION OF MDS • Refractory anemia with ringed sideroblasts • Refractory cytopenia with multilineage dysplasia (RCMD) with or without ringed sideroblasts • Refractory anemia with excess blasts (RAEB) • RAEB type 1 (5%-9% blasts) • RAEB type 2 (10 -19% blasts) • MDS, unclassifiable • MDS associated with isolated del (5 q) chromosome abnormality (“ 5 q- syndrome”)
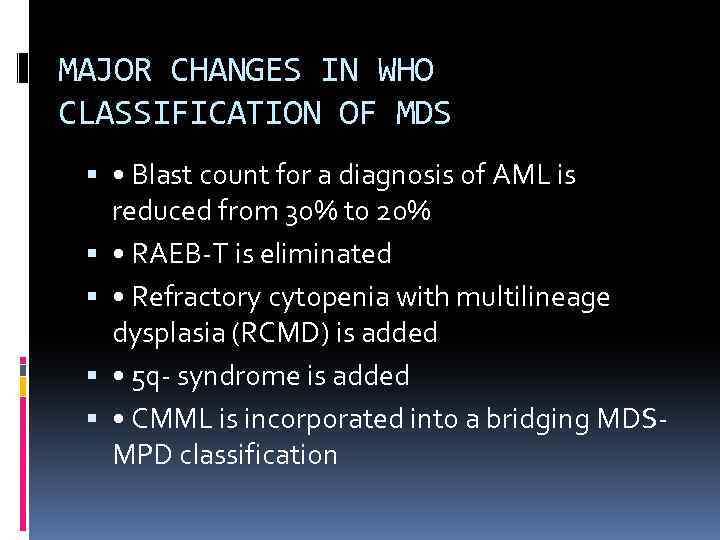 MAJOR CHANGES IN WHO CLASSIFICATION OF MDS • Blast count for a diagnosis of AML is reduced from 30% to 20% • RAEB-T is eliminated • Refractory cytopenia with multilineage dysplasia (RCMD) is added • 5 q- syndrome is added • CMML is incorporated into a bridging MDSMPD classification
MAJOR CHANGES IN WHO CLASSIFICATION OF MDS • Blast count for a diagnosis of AML is reduced from 30% to 20% • RAEB-T is eliminated • Refractory cytopenia with multilineage dysplasia (RCMD) is added • 5 q- syndrome is added • CMML is incorporated into a bridging MDSMPD classification
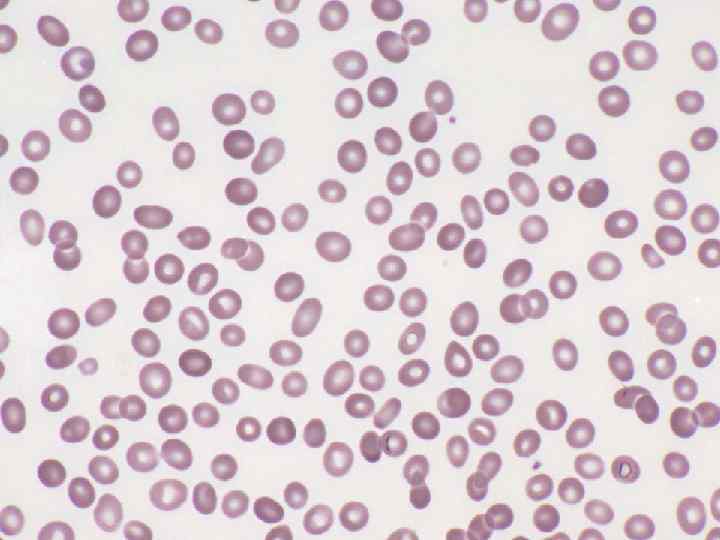
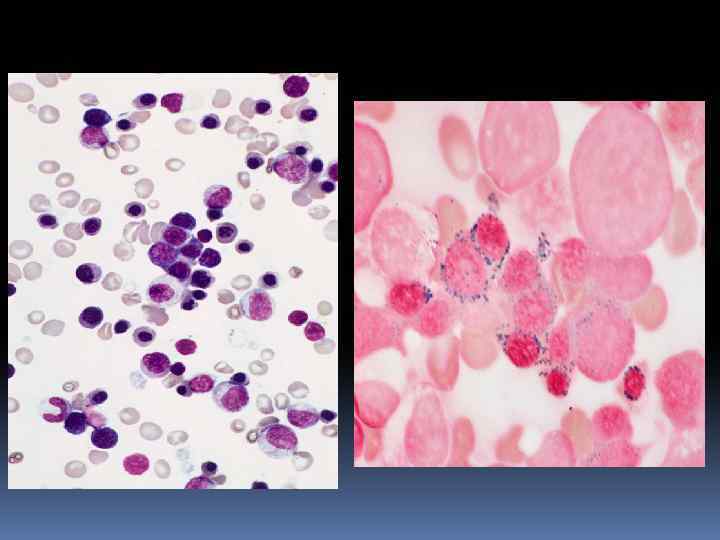
 REFRACTORY ANEMIA (RA) • Only erythroid lineage involved • Normocytic or macrocytic anemia • Reticulocytopenia • Usually normal or ↑RBC precursors • Variable dyserythropoiesis • <5% blasts in BM, none in blood
REFRACTORY ANEMIA (RA) • Only erythroid lineage involved • Normocytic or macrocytic anemia • Reticulocytopenia • Usually normal or ↑RBC precursors • Variable dyserythropoiesis • <5% blasts in BM, none in blood
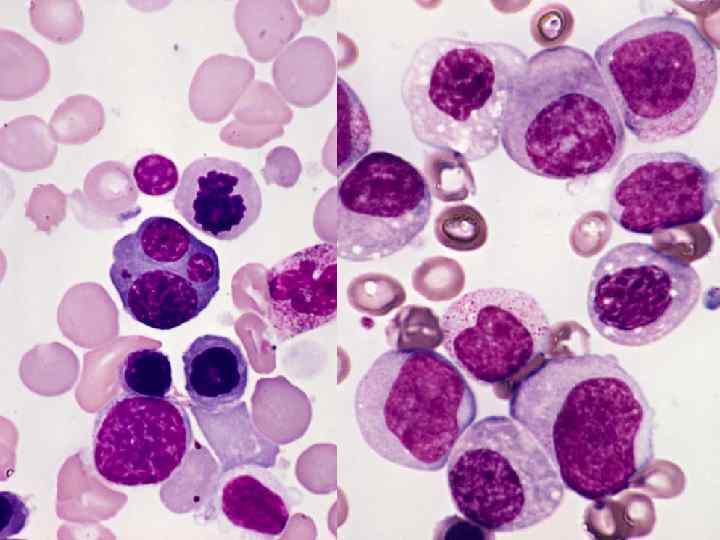
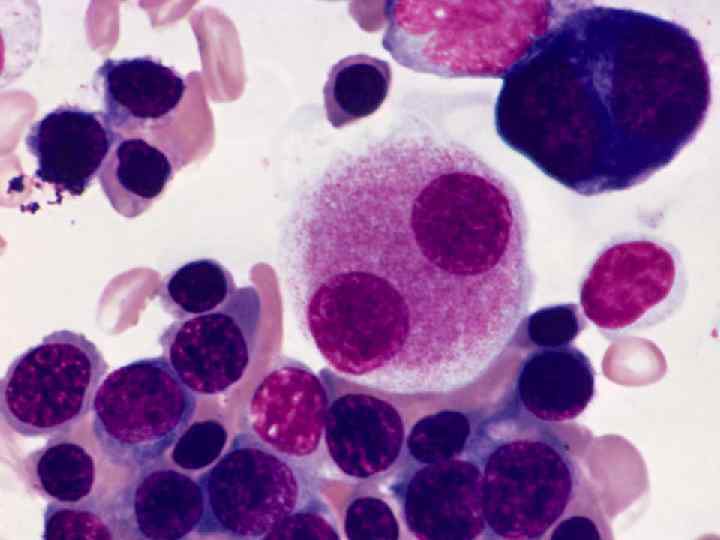
 REFRACTORY CYTOPENIA WITH MULTILINEAGE DYSPLASIA (RCMD) • Usually bicytopenia or pancytopenia • Multilineage dysplasia • <5% blasts in blood or BM • May have ringed sideroblasts • Worse prognosis than for RA and RARS and a higher incidence of cytogenetic abnormalities
REFRACTORY CYTOPENIA WITH MULTILINEAGE DYSPLASIA (RCMD) • Usually bicytopenia or pancytopenia • Multilineage dysplasia • <5% blasts in blood or BM • May have ringed sideroblasts • Worse prognosis than for RA and RARS and a higher incidence of cytogenetic abnormalities
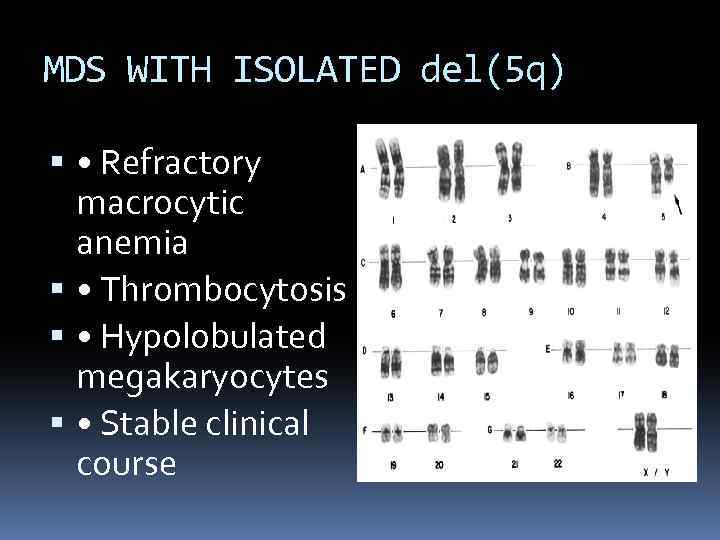 MDS WITH ISOLATED del(5 q) • Refractory macrocytic anemia • Thrombocytosis • Hypolobulated megakaryocytes • Stable clinical course
MDS WITH ISOLATED del(5 q) • Refractory macrocytic anemia • Thrombocytosis • Hypolobulated megakaryocytes • Stable clinical course
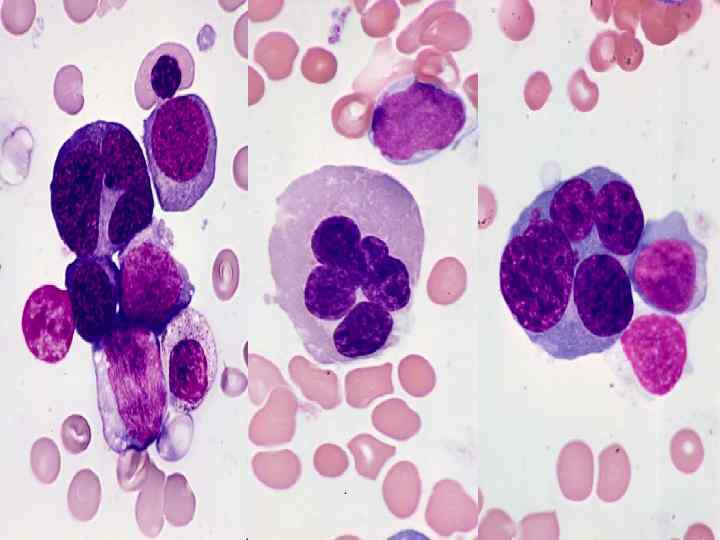
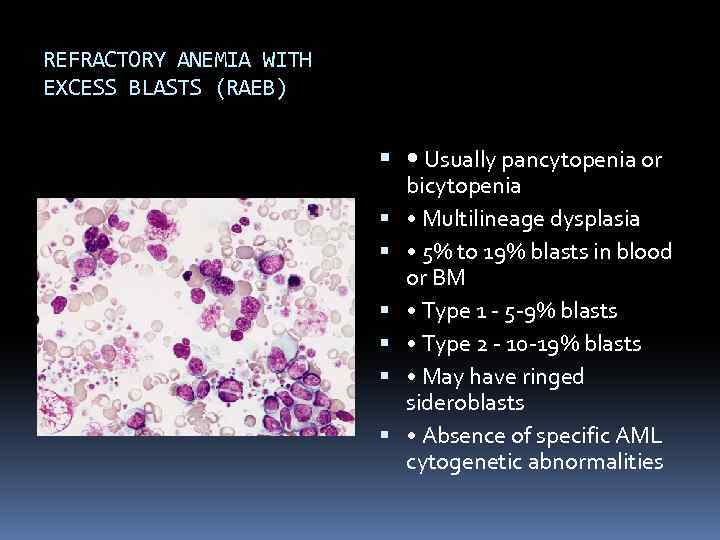 REFRACTORY ANEMIA WITH EXCESS BLASTS (RAEB) • Usually pancytopenia or bicytopenia • Multilineage dysplasia • 5% to 19% blasts in blood or BM • Type 1 - 5 -9% blasts • Type 2 - 10 -19% blasts • May have ringed sideroblasts • Absence of specific AML cytogenetic abnormalities
REFRACTORY ANEMIA WITH EXCESS BLASTS (RAEB) • Usually pancytopenia or bicytopenia • Multilineage dysplasia • 5% to 19% blasts in blood or BM • Type 1 - 5 -9% blasts • Type 2 - 10 -19% blasts • May have ringed sideroblasts • Absence of specific AML cytogenetic abnormalities
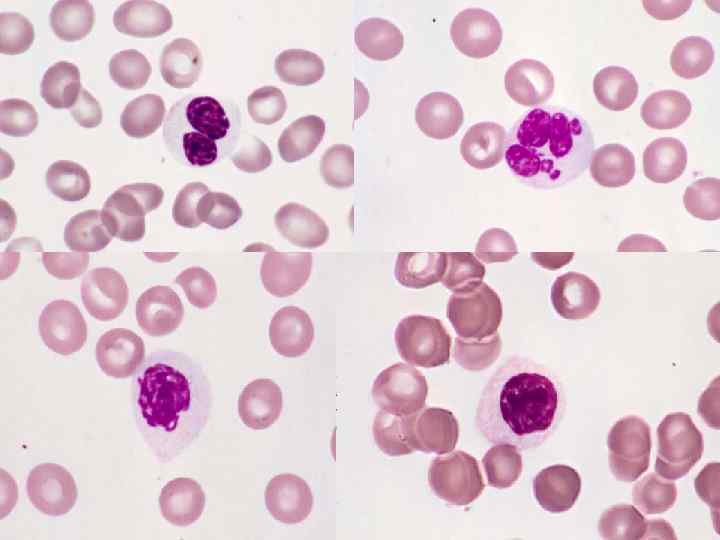
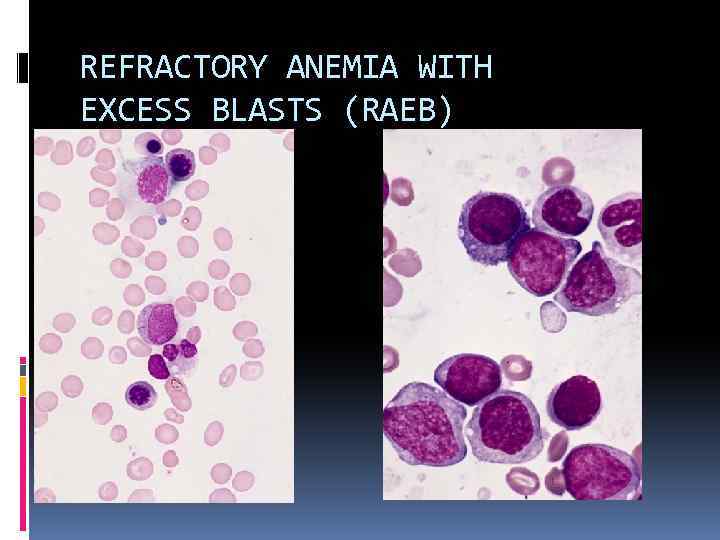 REFRACTORY ANEMIA WITH EXCESS BLASTS (RAEB)
REFRACTORY ANEMIA WITH EXCESS BLASTS (RAEB)
 MYELODYSPLASTIC SYNDROME UNCLASSIFIABLE (MDS-U) • Cytopenias • No or rare blasts in blood • Unilineage dysplasia • <5% marrow blasts • No Auer rods
MYELODYSPLASTIC SYNDROME UNCLASSIFIABLE (MDS-U) • Cytopenias • No or rare blasts in blood • Unilineage dysplasia • <5% marrow blasts • No Auer rods
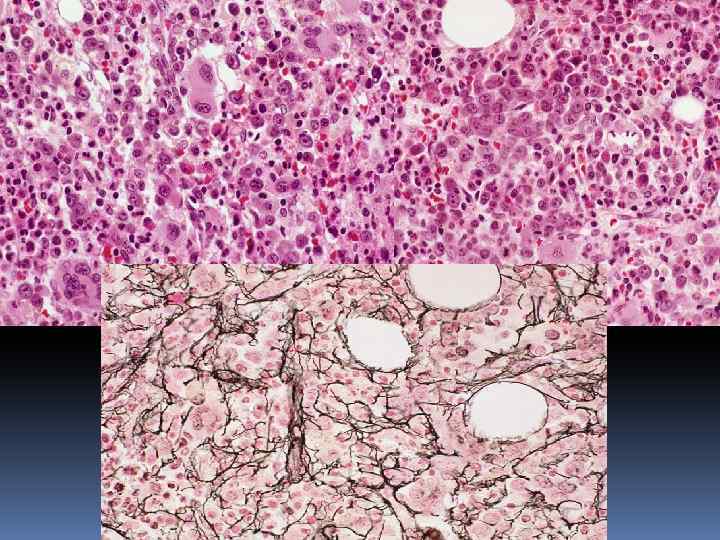
 MYELODYSPLASTIC SYNDROME WITH INCREASED MARROW FIBROSIS • Pancytopenia • Trilineage dysplasia • Bone marrow fibrosis • ↑and dysplastic megakaryocytes • No splenomegaly • ? poor survival
MYELODYSPLASTIC SYNDROME WITH INCREASED MARROW FIBROSIS • Pancytopenia • Trilineage dysplasia • Bone marrow fibrosis • ↑and dysplastic megakaryocytes • No splenomegaly • ? poor survival
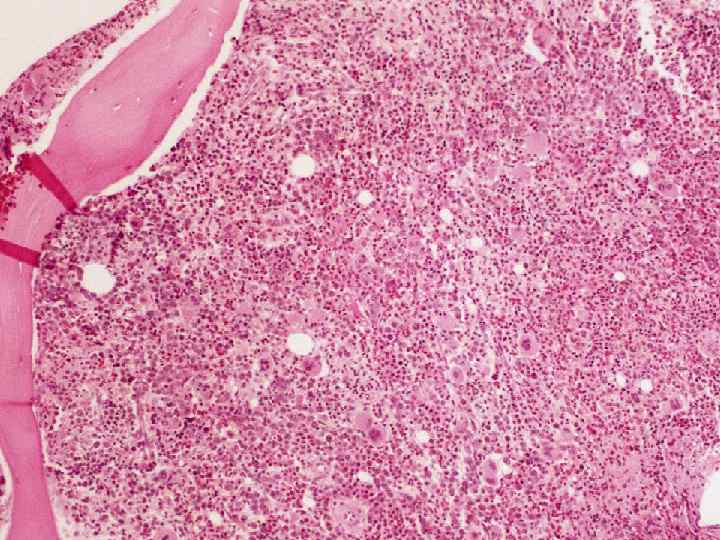
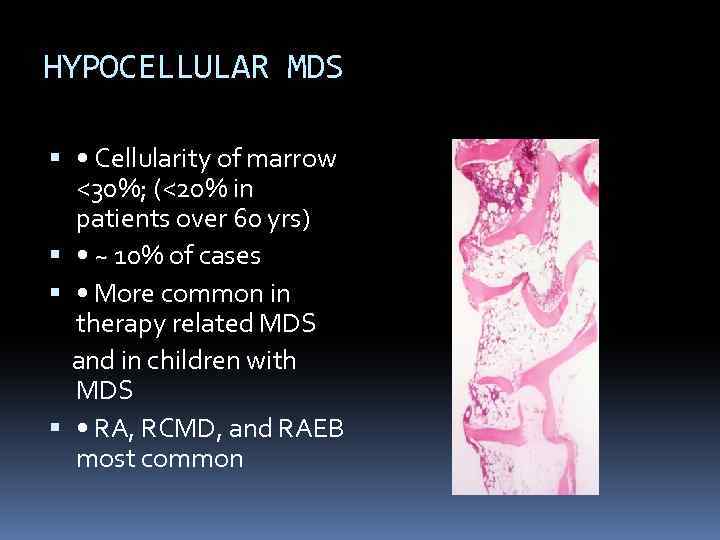 HYPOCELLULAR MDS • Cellularity of marrow <30%; (<20% in patients over 60 yrs) • ~ 10% of cases • More common in therapy related MDS and in children with MDS • RA, RCMD, and RAEB most common
HYPOCELLULAR MDS • Cellularity of marrow <30%; (<20% in patients over 60 yrs) • ~ 10% of cases • More common in therapy related MDS and in children with MDS • RA, RCMD, and RAEB most common
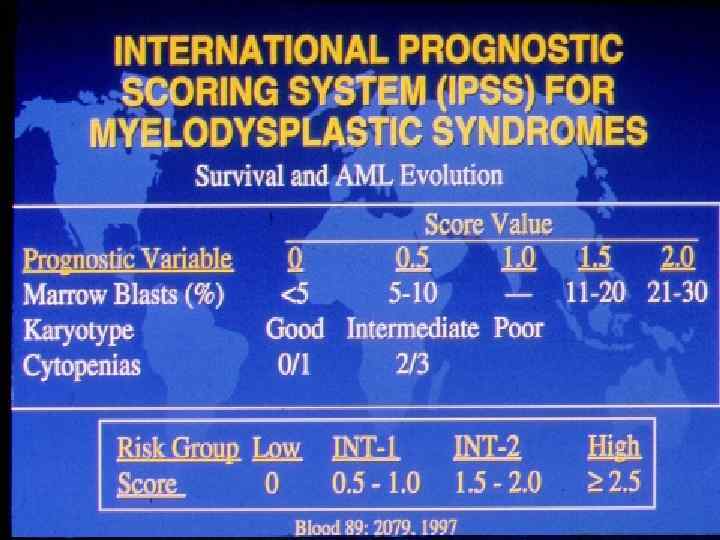
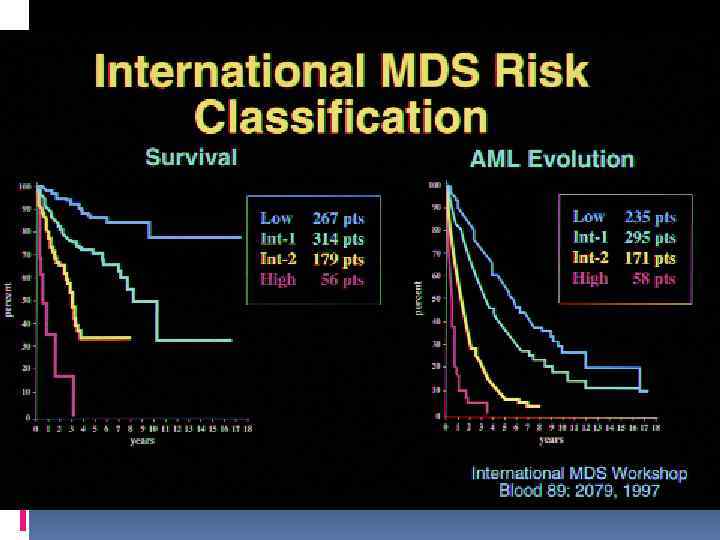
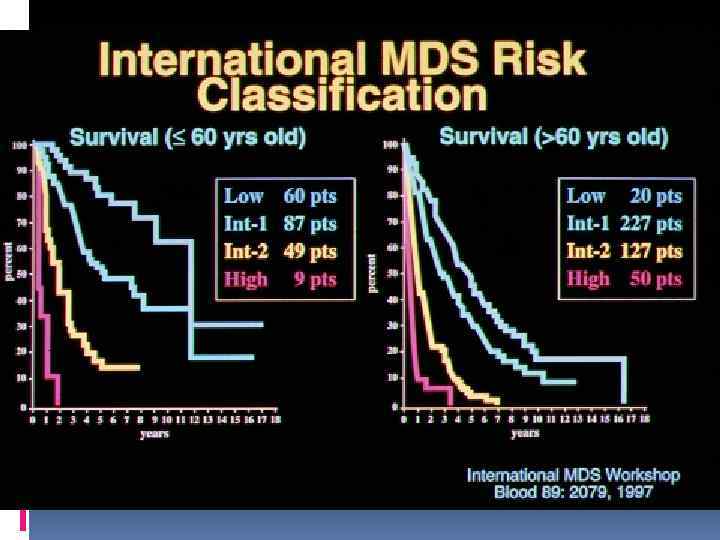
 PROGNOSTIC INDICATORS IN MDS • Age • Gender • Bone marrow blast % • # of cytopenias • Cytogenetics
PROGNOSTIC INDICATORS IN MDS • Age • Gender • Bone marrow blast % • # of cytopenias • Cytogenetics
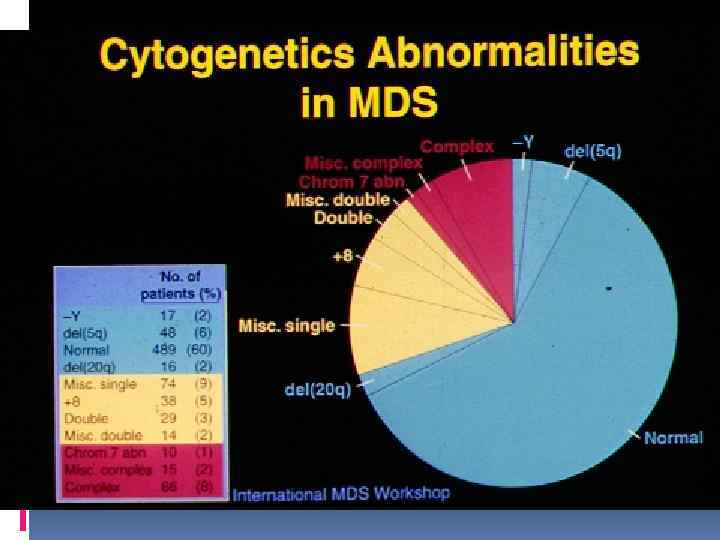
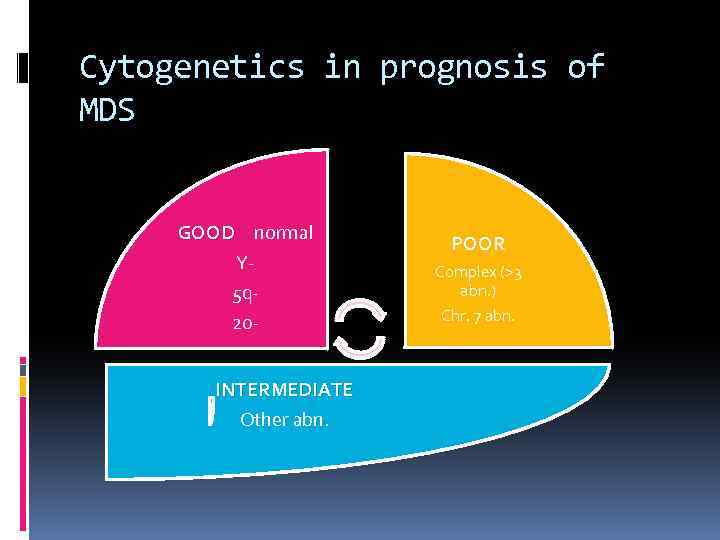 Cytogenetics in prognosis of MDS GOOD normal Y 5 q 20 INTERMEDIATE Other abn. POOR Complex (>3 abn. ) Chr. 7 abn.
Cytogenetics in prognosis of MDS GOOD normal Y 5 q 20 INTERMEDIATE Other abn. POOR Complex (>3 abn. ) Chr. 7 abn.
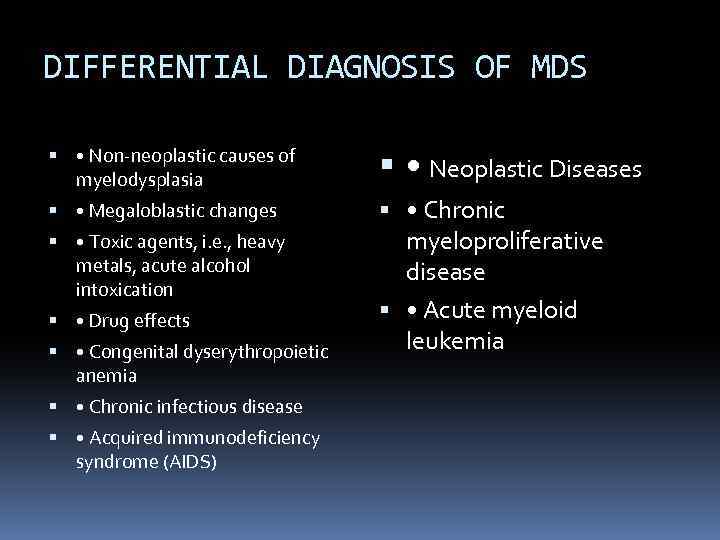 DIFFERENTIAL DIAGNOSIS OF MDS • Non-neoplastic causes of myelodysplasia • Neoplastic Diseases • Megaloblastic changes • Chronic myeloproliferative disease • Toxic agents, i. e. , heavy metals, acute alcohol intoxication • Drug effects • Congenital dyserythropoietic anemia • Chronic infectious disease • Acquired immunodeficiency syndrome (AIDS) • Acute myeloid leukemia
DIFFERENTIAL DIAGNOSIS OF MDS • Non-neoplastic causes of myelodysplasia • Neoplastic Diseases • Megaloblastic changes • Chronic myeloproliferative disease • Toxic agents, i. e. , heavy metals, acute alcohol intoxication • Drug effects • Congenital dyserythropoietic anemia • Chronic infectious disease • Acquired immunodeficiency syndrome (AIDS) • Acute myeloid leukemia
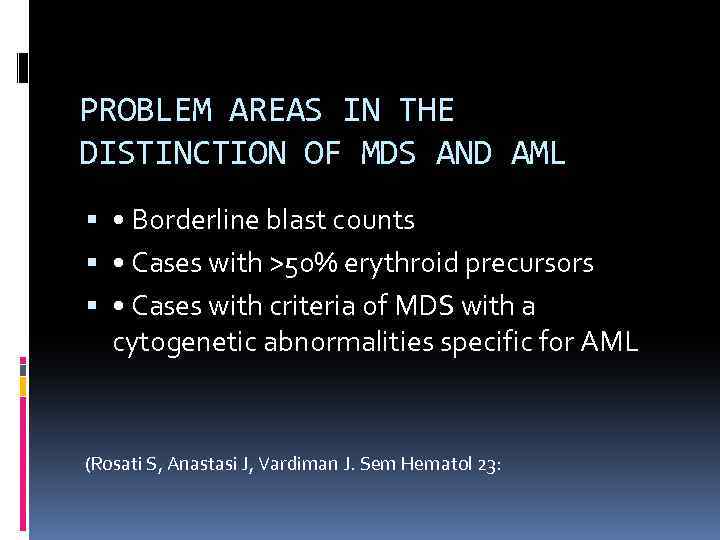 PROBLEM AREAS IN THE DISTINCTION OF MDS AND AML • Borderline blast counts • Cases with >50% erythroid precursors • Cases with criteria of MDS with a cytogenetic abnormalities specific for AML (Rosati S, Anastasi J, Vardiman J. Sem Hematol 23:
PROBLEM AREAS IN THE DISTINCTION OF MDS AND AML • Borderline blast counts • Cases with >50% erythroid precursors • Cases with criteria of MDS with a cytogenetic abnormalities specific for AML (Rosati S, Anastasi J, Vardiman J. Sem Hematol 23:
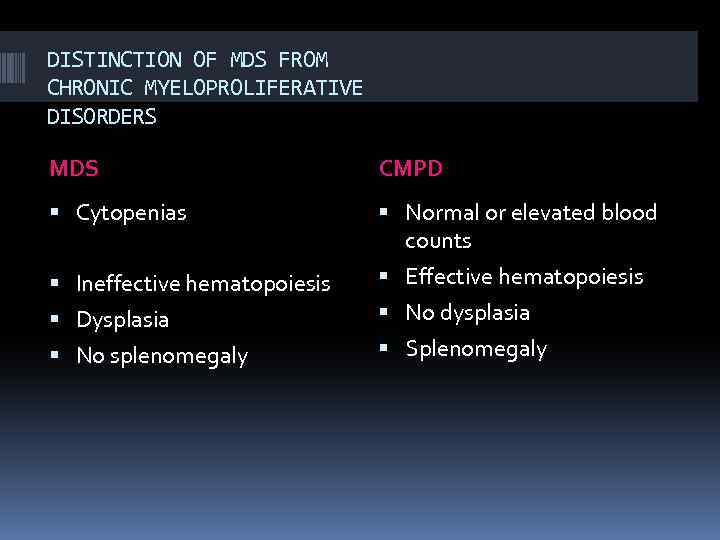 DISTINCTION OF MDS FROM CHRONIC MYELOPROLIFERATIVE DISORDERS MDS CMPD Cytopenias Normal or elevated blood counts Ineffective hematopoiesis Effective hematopoiesis Dysplasia No splenomegaly No dysplasia Splenomegaly
DISTINCTION OF MDS FROM CHRONIC MYELOPROLIFERATIVE DISORDERS MDS CMPD Cytopenias Normal or elevated blood counts Ineffective hematopoiesis Effective hematopoiesis Dysplasia No splenomegaly No dysplasia Splenomegaly
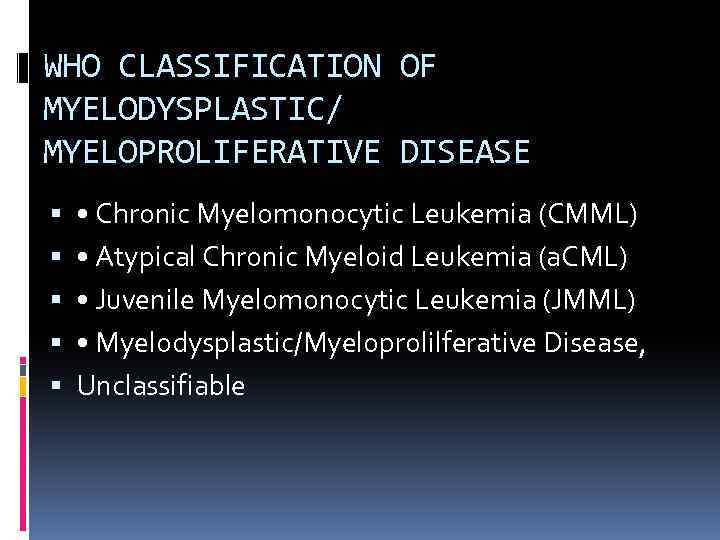 WHO CLASSIFICATION OF MYELODYSPLASTIC/ MYELOPROLIFERATIVE DISEASE • Chronic Myelomonocytic Leukemia (CMML) • Atypical Chronic Myeloid Leukemia (a. CML) • Juvenile Myelomonocytic Leukemia (JMML) • Myelodysplastic/Myeloprolilferative Disease, Unclassifiable
WHO CLASSIFICATION OF MYELODYSPLASTIC/ MYELOPROLIFERATIVE DISEASE • Chronic Myelomonocytic Leukemia (CMML) • Atypical Chronic Myeloid Leukemia (a. CML) • Juvenile Myelomonocytic Leukemia (JMML) • Myelodysplastic/Myeloprolilferative Disease, Unclassifiable
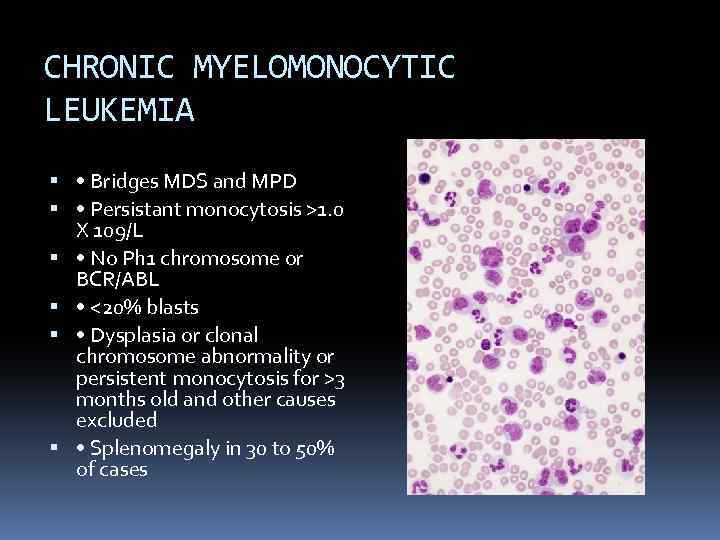 CHRONIC MYELOMONOCYTIC LEUKEMIA • Bridges MDS and MPD • Persistant monocytosis >1. 0 X 109/L • No Ph 1 chromosome or BCR/ABL • <20% blasts • Dysplasia or clonal chromosome abnormality or persistent monocytosis for >3 months old and other causes excluded • Splenomegaly in 30 to 50% of cases
CHRONIC MYELOMONOCYTIC LEUKEMIA • Bridges MDS and MPD • Persistant monocytosis >1. 0 X 109/L • No Ph 1 chromosome or BCR/ABL • <20% blasts • Dysplasia or clonal chromosome abnormality or persistent monocytosis for >3 months old and other causes excluded • Splenomegaly in 30 to 50% of cases
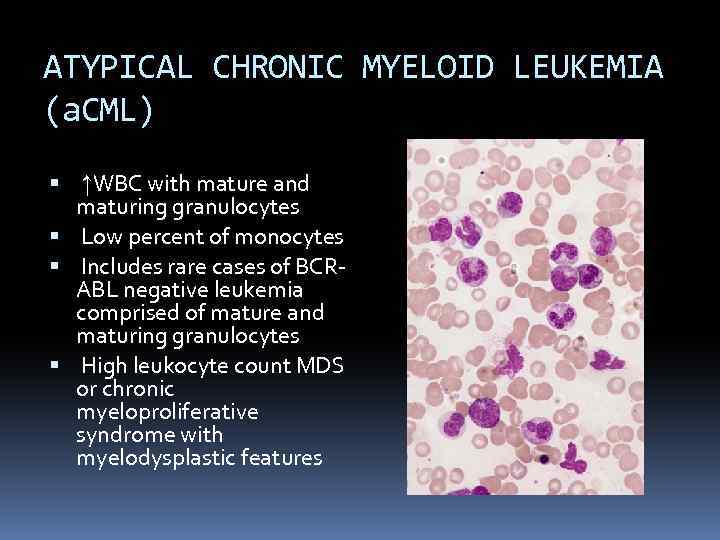 ATYPICAL CHRONIC MYELOID LEUKEMIA (a. CML) ↑WBC with mature and maturing granulocytes Low percent of monocytes Includes rare cases of BCRABL negative leukemia comprised of mature and maturing granulocytes High leukocyte count MDS or chronic myeloproliferative syndrome with myelodysplastic features
ATYPICAL CHRONIC MYELOID LEUKEMIA (a. CML) ↑WBC with mature and maturing granulocytes Low percent of monocytes Includes rare cases of BCRABL negative leukemia comprised of mature and maturing granulocytes High leukocyte count MDS or chronic myeloproliferative syndrome with myelodysplastic features
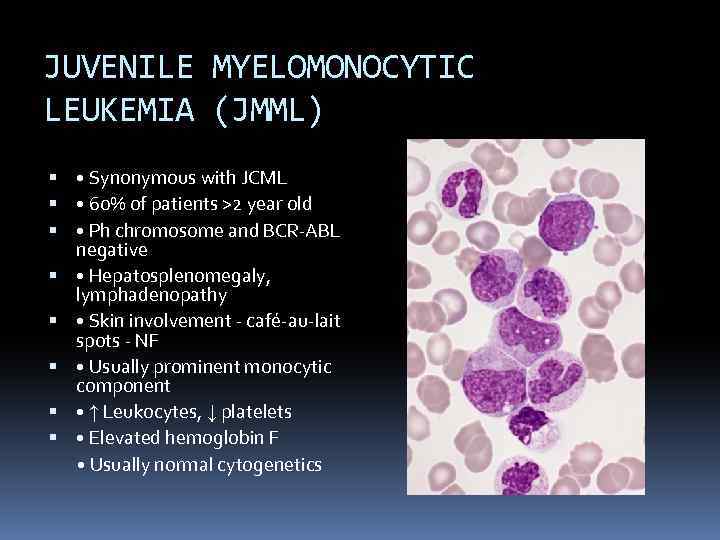 JUVENILE MYELOMONOCYTIC LEUKEMIA (JMML) • Synonymous with JCML • 60% of patients >2 year old • Ph chromosome and BCR-ABL negative • Hepatosplenomegaly, lymphadenopathy • Skin involvement - café-au-lait spots - NF • Usually prominent monocytic component • ↑ Leukocytes, ↓ platelets • Elevated hemoglobin F • Usually normal cytogenetics
JUVENILE MYELOMONOCYTIC LEUKEMIA (JMML) • Synonymous with JCML • 60% of patients >2 year old • Ph chromosome and BCR-ABL negative • Hepatosplenomegaly, lymphadenopathy • Skin involvement - café-au-lait spots - NF • Usually prominent monocytic component • ↑ Leukocytes, ↓ platelets • Elevated hemoglobin F • Usually normal cytogenetics
 MONOSOMY 7 SYNDROME • Anemia and leukocytosis • Thrombocytopenia in 50% • Monocytosis • Defective neutrophil function with recurrent infections • Hypercellular BM with ↑ reticulin • Dysplasia • Hepatosplenomegaly • Neurofibromatosis
MONOSOMY 7 SYNDROME • Anemia and leukocytosis • Thrombocytopenia in 50% • Monocytosis • Defective neutrophil function with recurrent infections • Hypercellular BM with ↑ reticulin • Dysplasia • Hepatosplenomegaly • Neurofibromatosis
 OTHER MORPHOLOGIC FINDINGS IN MDS • Changes in marrow cellularity usually hypercellular • Increased iron stores • Myelofibrosis
OTHER MORPHOLOGIC FINDINGS IN MDS • Changes in marrow cellularity usually hypercellular • Increased iron stores • Myelofibrosis
 MDS/MPD, UNCLASSIFIABLE • Features of MDS but with thrombocytosis (>600 X 109/L) or leukocytosis (>13. 0 X 109/L) • (and) No prior history of MDS or MPD • (and) No cytogenetic abnormality associated with specific myeloid disorder • (or) Mixed MDS and MPD features and cannot be assigned to any other category
MDS/MPD, UNCLASSIFIABLE • Features of MDS but with thrombocytosis (>600 X 109/L) or leukocytosis (>13. 0 X 109/L) • (and) No prior history of MDS or MPD • (and) No cytogenetic abnormality associated with specific myeloid disorder • (or) Mixed MDS and MPD features and cannot be assigned to any other category
 Treatment Supportive care – blood products, infections etc. Growth factors – G-CSF, erythropoetin Hypomethylating agents – azacitidin, dacogen Revlimid – 5 q Allogeneic stem cell transplantation
Treatment Supportive care – blood products, infections etc. Growth factors – G-CSF, erythropoetin Hypomethylating agents – azacitidin, dacogen Revlimid – 5 q Allogeneic stem cell transplantation
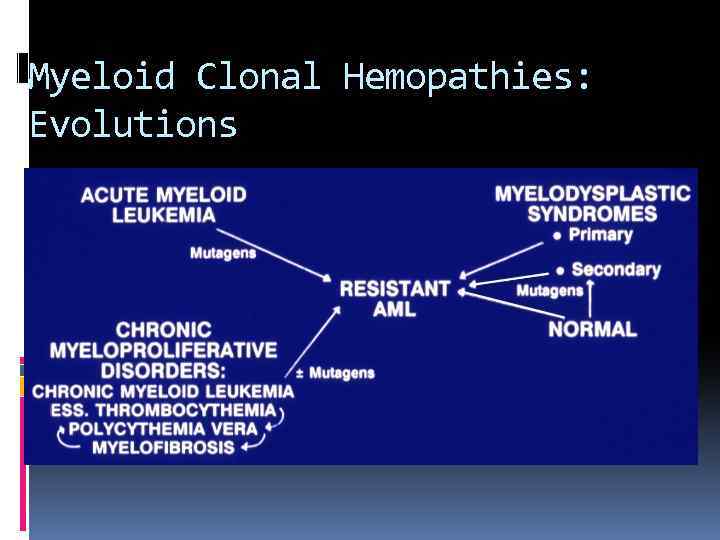 Myeloid Clonal Hemopathies: Evolutions
Myeloid Clonal Hemopathies: Evolutions
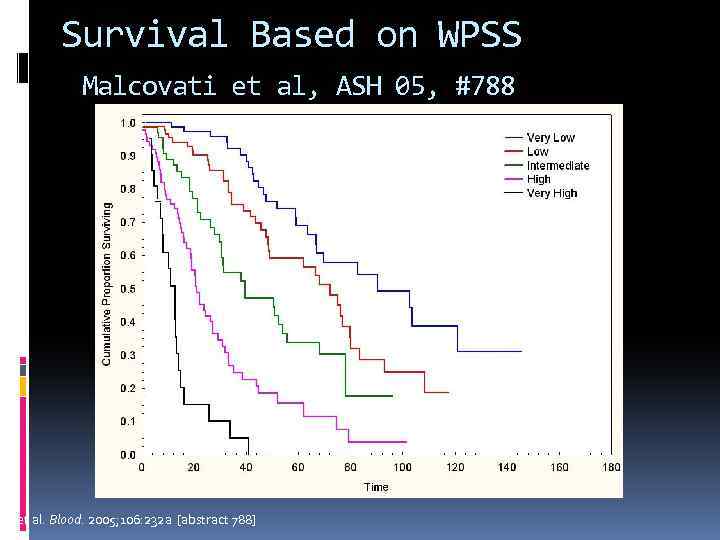 Survival Based on WPSS Malcovati et al, ASH 05, #788 L et al. Blood. 2005; 106: 232 a [abstract 788]
Survival Based on WPSS Malcovati et al, ASH 05, #788 L et al. Blood. 2005; 106: 232 a [abstract 788]
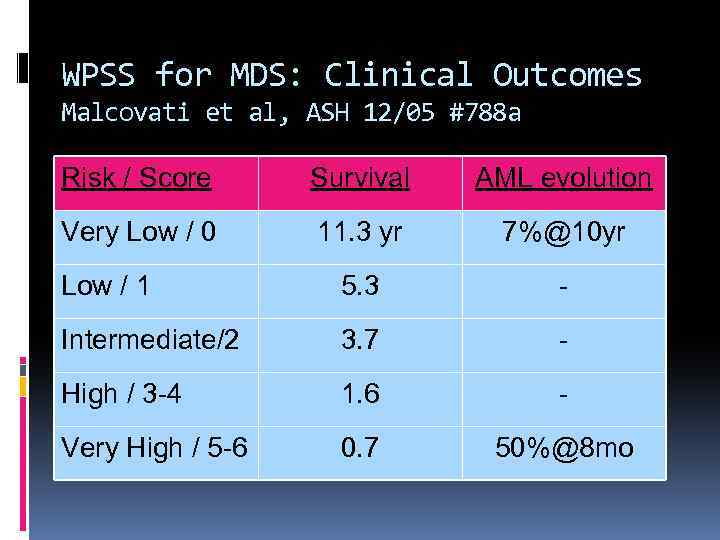 WPSS for MDS: Clinical Outcomes Malcovati et al, ASH 12/05 #788 a Risk / Score Survival AML evolution Very Low / 0 11. 3 yr 7%@10 yr Low / 1 5. 3 - Intermediate/2 3. 7 - High / 3 -4 1. 6 - Very High / 5 -6 0. 7 50%@8 mo
WPSS for MDS: Clinical Outcomes Malcovati et al, ASH 12/05 #788 a Risk / Score Survival AML evolution Very Low / 0 11. 3 yr 7%@10 yr Low / 1 5. 3 - Intermediate/2 3. 7 - High / 3 -4 1. 6 - Very High / 5 -6 0. 7 50%@8 mo
 THANK YOU
THANK YOU


