b4248ecfa3e2e2e7bdbb04364bf8cef7.ppt
- Количество слайдов: 29
 Dr: Eman Elsheshtawy Ass. Prof. Psychiatry
Dr: Eman Elsheshtawy Ass. Prof. Psychiatry

 Transient Heightened emotional reactivity 50 -85% women experience baby blues Peaks 3 -5 days after delivery Lasts up to 10 -14 days
Transient Heightened emotional reactivity 50 -85% women experience baby blues Peaks 3 -5 days after delivery Lasts up to 10 -14 days
 Considered normal experience of childbirth Symptoms can be distressing Usually don’t affect mother’s ability to function and care for child
Considered normal experience of childbirth Symptoms can be distressing Usually don’t affect mother’s ability to function and care for child
 Characteristics: Mild mood swings Irritability Anxiety Decreased concentration Insomnia Tearfulness Crying spells
Characteristics: Mild mood swings Irritability Anxiety Decreased concentration Insomnia Tearfulness Crying spells
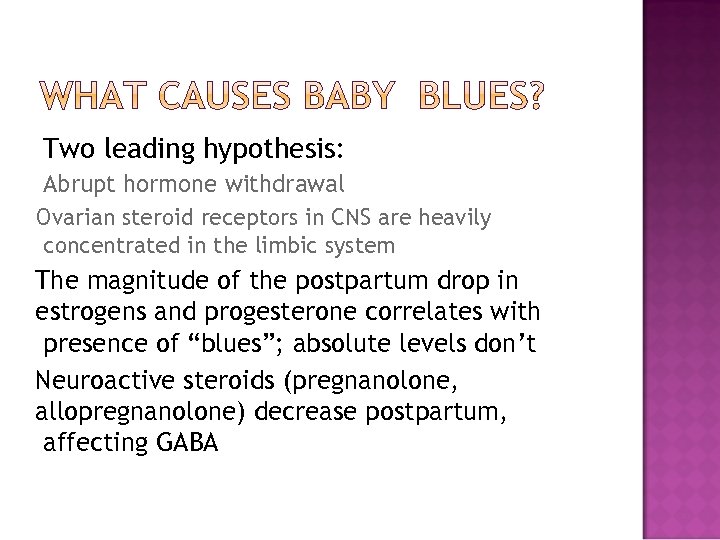 Two leading hypothesis: Abrupt hormone withdrawal Ovarian steroid receptors in CNS are heavily concentrated in the limbic system The magnitude of the postpartum drop in estrogens and progesterone correlates with presence of “blues”; absolute levels don’t Neuroactive steroids (pregnanolone, allopregnanolone) decrease postpartum, affecting GABA
Two leading hypothesis: Abrupt hormone withdrawal Ovarian steroid receptors in CNS are heavily concentrated in the limbic system The magnitude of the postpartum drop in estrogens and progesterone correlates with presence of “blues”; absolute levels don’t Neuroactive steroids (pregnanolone, allopregnanolone) decrease postpartum, affecting GABA
 Neurobiological systems foster attachment between mammalian mothers & infants Oxytocin activates limbic structures (e. g. the ACG) that mediate the interface between attention & emotion Postpartum With reactivity may stem from this stressors, depression may result
Neurobiological systems foster attachment between mammalian mothers & infants Oxytocin activates limbic structures (e. g. the ACG) that mediate the interface between attention & emotion Postpartum With reactivity may stem from this stressors, depression may result

 About 10% of women after delivery Average duration 7 months ¼ still affected at child’s first birthday Overlooked and under diagnosed
About 10% of women after delivery Average duration 7 months ¼ still affected at child’s first birthday Overlooked and under diagnosed
 Female is a 27 year old mother brought into my office as an urgent care appointment. She just had a baby 4 weeks ago after much anticipation. Her husband is an only child and her in-laws filled the nursery with toys and clothes for the baby and are very excited. She is unable to sleep and eat, extremely doubtful of her ability to do anything. She is preoccupied with the fear that she will harm the baby and intense guilt of her inability to meet the expectations of the family. She has been thinking that how easy it is kill herself than to be this worthless
Female is a 27 year old mother brought into my office as an urgent care appointment. She just had a baby 4 weeks ago after much anticipation. Her husband is an only child and her in-laws filled the nursery with toys and clothes for the baby and are very excited. She is unable to sleep and eat, extremely doubtful of her ability to do anything. She is preoccupied with the fear that she will harm the baby and intense guilt of her inability to meet the expectations of the family. She has been thinking that how easy it is kill herself than to be this worthless
 Depression negatively effects: Mother’s ability to mother Mother—infant Emotional relationship and cognitive development of the child
Depression negatively effects: Mother’s ability to mother Mother—infant Emotional relationship and cognitive development of the child
 Infants perceived to be more bothersome Make harsh judgments of their infants Feelings of guilt, resentment, and ambivalence toward child Loss of affection toward child
Infants perceived to be more bothersome Make harsh judgments of their infants Feelings of guilt, resentment, and ambivalence toward child Loss of affection toward child
 Gaze less at their infants Take longer to respond to infant’s utterances Show fewer positive facial expressions Lack awareness of their infants
Gaze less at their infants Take longer to respond to infant’s utterances Show fewer positive facial expressions Lack awareness of their infants
 Negative interactive patterns with infant Children exposed to maternal psychiatric illness have: Higher incidence of conduct disorders Inappropriate Cognitive aggression and attention deficits
Negative interactive patterns with infant Children exposed to maternal psychiatric illness have: Higher incidence of conduct disorders Inappropriate Cognitive aggression and attention deficits
 London study 2001 demonstrated lower IQ’s in 11 year olds whose mothers were depressed at 3 months age Increased behavior concerns and ADHD (sp. in boys) Shorter duration of breastfeeding in PPD Continued protective breastfeeding in PPD was
London study 2001 demonstrated lower IQ’s in 11 year olds whose mothers were depressed at 3 months age Increased behavior concerns and ADHD (sp. in boys) Shorter duration of breastfeeding in PPD Continued protective breastfeeding in PPD was
 Patient, society, and physicians dismiss or minimize patients experiences as “normal” Patient without a primary care physician don’t know who to turn to Women’s fear and shame about not being a “good mother” Patients don’t present with CC of depression
Patient, society, and physicians dismiss or minimize patients experiences as “normal” Patient without a primary care physician don’t know who to turn to Women’s fear and shame about not being a “good mother” Patients don’t present with CC of depression
 Noted in medical history since Hippo crates Recognized in DSM-IV in 1994 Major depression that occurs within 4 weeks of delivery Definition used by researchers usually allows up to 6 months 5 symptoms, every day, at least 2 weeks AND functional impairment
Noted in medical history since Hippo crates Recognized in DSM-IV in 1994 Major depression that occurs within 4 weeks of delivery Definition used by researchers usually allows up to 6 months 5 symptoms, every day, at least 2 weeks AND functional impairment
 Depressed mood Lack of pleasure or interest Appetite disturbance or weight loss* Sleep disturbance* Physical agitation or psychomotor slowing Fatigue, loss of energy* Feelings of worthlessness or excessive guilt Diminished concentration, or indecisiveness* Thoughts of death or suicidal ideation , Thoughts of harming infant
Depressed mood Lack of pleasure or interest Appetite disturbance or weight loss* Sleep disturbance* Physical agitation or psychomotor slowing Fatigue, loss of energy* Feelings of worthlessness or excessive guilt Diminished concentration, or indecisiveness* Thoughts of death or suicidal ideation , Thoughts of harming infant
 Severe Symptoms: Thoughts of dying Thoughts of suicide Wanting to flee or get away Being unable to feel love for the baby Thoughts of harming the baby Thoughts of not being able to protect the infant Hopelessnes
Severe Symptoms: Thoughts of dying Thoughts of suicide Wanting to flee or get away Being unable to feel love for the baby Thoughts of harming the baby Thoughts of not being able to protect the infant Hopelessnes
 Cause unclear Rapid decline in reproductive hormones Several factors increase risk
Cause unclear Rapid decline in reproductive hormones Several factors increase risk
 Prior episodes depression, anxiety, OCD, bipolar d/o, eating d/o Prior depression = 25% risk PPD Prior PPD = 50% risk recurrent PPD Stressful FHx Hx life events mood disorders of PMDD Inadequate social support
Prior episodes depression, anxiety, OCD, bipolar d/o, eating d/o Prior depression = 25% risk PPD Prior PPD = 50% risk recurrent PPD Stressful FHx Hx life events mood disorders of PMDD Inadequate social support
 Education Sex level of infant Breastfeeding Mode of delivery Planned or unplanned pregnancy
Education Sex level of infant Breastfeeding Mode of delivery Planned or unplanned pregnancy
 During Pregnancy A young and single mother H/O Mental illness or substance abuse Financial or relationship difficulties Previous Pregnancy or postpartum depression After Birth Labor/Birth Complications Low confidence as a parent Problems with Baby’s Health Lack of supports Major Life change at the same time as birth of the baby
During Pregnancy A young and single mother H/O Mental illness or substance abuse Financial or relationship difficulties Previous Pregnancy or postpartum depression After Birth Labor/Birth Complications Low confidence as a parent Problems with Baby’s Health Lack of supports Major Life change at the same time as birth of the baby

 2: 1, 000 births Psychiatric emergency Usually within 3 weeks Usually manifestation of bipolar d/o 70% women experience recurrence in PPP
2: 1, 000 births Psychiatric emergency Usually within 3 weeks Usually manifestation of bipolar d/o 70% women experience recurrence in PPP
 Severe disturbances Rapidly evolving manic episodes Dramatic presentation Initial signs are restlessness, irritability, insomnia Infanticide: Suicide: 4% of untreated PPP 5% of untreated PPP
Severe disturbances Rapidly evolving manic episodes Dramatic presentation Initial signs are restlessness, irritability, insomnia Infanticide: Suicide: 4% of untreated PPP 5% of untreated PPP
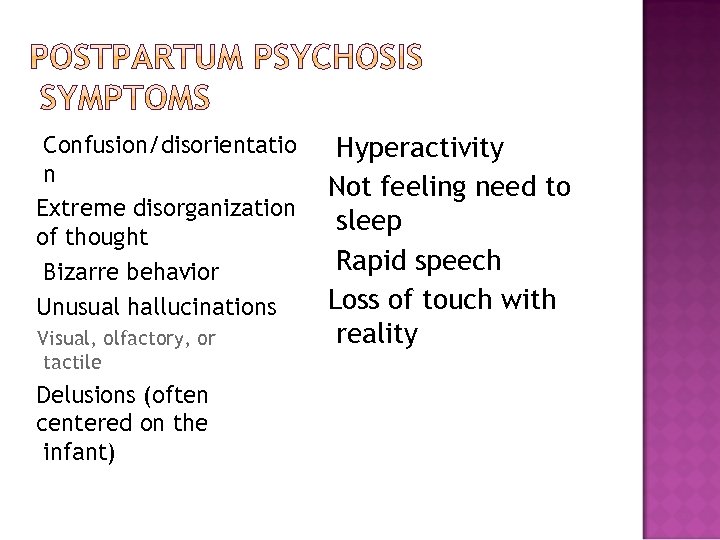 Confusion/disorientatio n Extreme disorganization of thought Bizarre behavior Unusual hallucinations Visual, olfactory, or tactile Delusions (often centered on the infant) Hyperactivity Not feeling need to sleep Rapid speech Loss of touch with reality
Confusion/disorientatio n Extreme disorganization of thought Bizarre behavior Unusual hallucinations Visual, olfactory, or tactile Delusions (often centered on the infant) Hyperactivity Not feeling need to sleep Rapid speech Loss of touch with reality
 Inform the public Depression screening in public health settings Provide appropriate referrals Partnership with mental health, social service agencies Follow up care (home visits, support services
Inform the public Depression screening in public health settings Provide appropriate referrals Partnership with mental health, social service agencies Follow up care (home visits, support services
 “Behind the Smile: My Journey Out of Postpartum Depression”, Marie Osmond “Down Came the Rain”, Brooke Shields Anne Lamott, “Operating Instructions: A Journal of My Son’s First Year” Depression After Delivery 1 -800 -944 -4 PPD (http: //www. depressionafterdelivery. com ) National Women’s Health Information Center (www. 4 woman. gov) Postpartum Support International 1 -805 -967 -7636
“Behind the Smile: My Journey Out of Postpartum Depression”, Marie Osmond “Down Came the Rain”, Brooke Shields Anne Lamott, “Operating Instructions: A Journal of My Son’s First Year” Depression After Delivery 1 -800 -944 -4 PPD (http: //www. depressionafterdelivery. com ) National Women’s Health Information Center (www. 4 woman. gov) Postpartum Support International 1 -805 -967 -7636


