094e727e5108e0032fd735bbcc67748d.ppt
- Количество слайдов: 56
Donation after Brain-Stem Death DBD Jerome Mc. Cann Arpan Guha 21 st May 2013 Organ Donation Past, Present and Future 1
Session Objectives • Present regional data for DBD • Understand that DBD gives better organs than DCD • Increase rate of neurological confirmation of death by increasing confidence in the Diagnosis of Death • Increase quality of DBD organs – adoption of extended care bundle and compliance with the six early interventions in donor optimisation – collaboration in Scout pilot Organ Donation Past, Present and Future 2
NORTH WEST Regional Data Jerome Mc. Cann Organ Donation Past, Present and Future 3
Donation after Brain Death (DBD) NORTH WEST Mechanically ventilated patient where death has been confirmed using neurological criteria. 74 donors -5. 1% increase Lungs Heart Small Intestine Organ Donation Past, Present and Future Kidneys Liver Pancreas
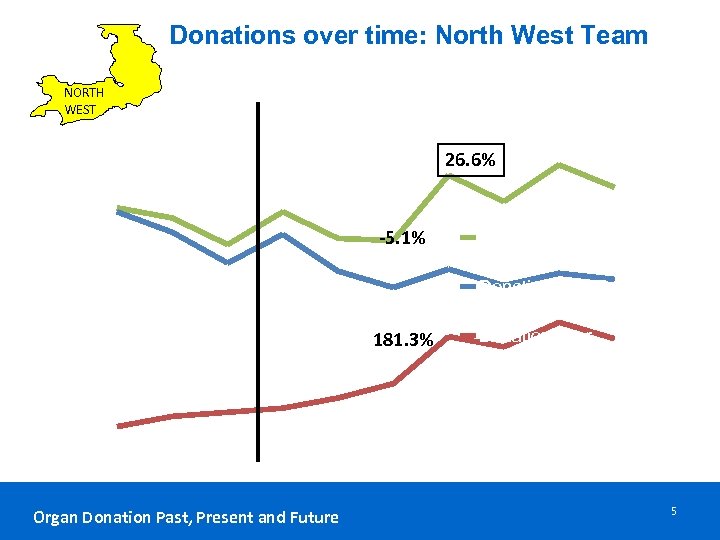
Donations over time: North West Team NORTH WEST 140 26. 6% 120 100 -5. 1% 80 Total Deceased Donation 60 Donation after Brain Death 181. 3% 40 Donation after Circulatory Death 20 0 2003 -04 2004 -05 2005 -06 2006 -07 2007 -08 2008 -09 2009 -10 2010 -11 2011 -12 2012 -13 Organ Donation Past, Present and Future 5
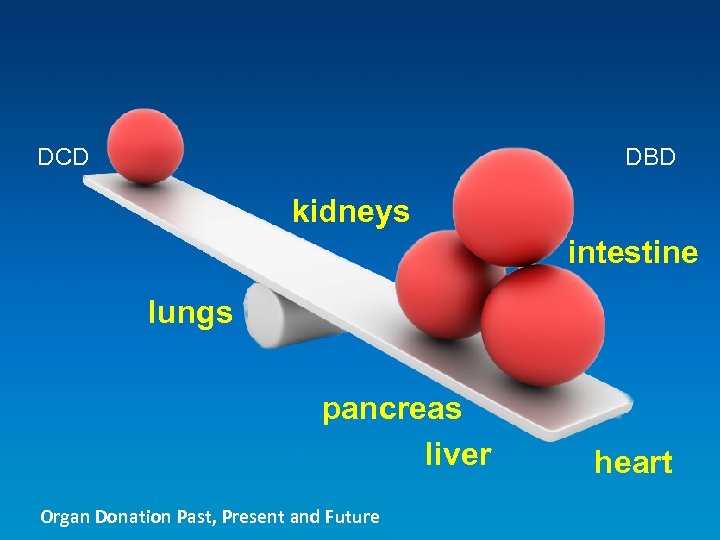
DCD DBD kidneys intestine lungs pancreas liver Organ Donation Past, Present and Future heart
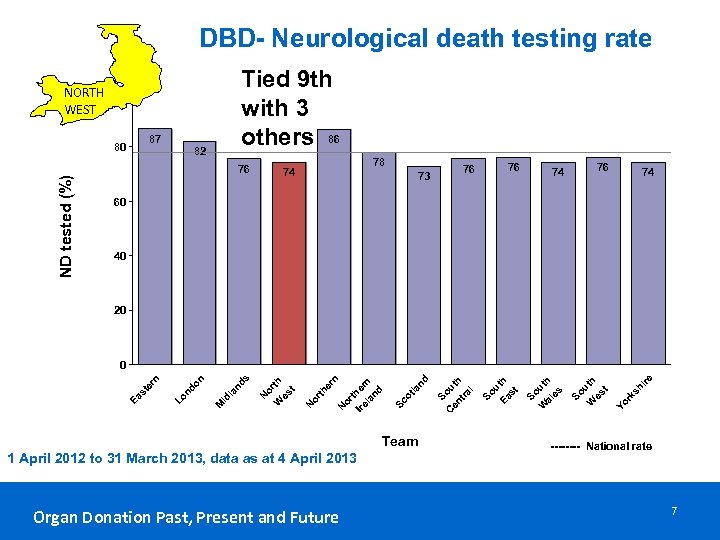
DBD- Neurological death testing rate Tied 9 th with 3 others 86 NORTH 100 WEST 87 ND tested (%) 80 82 76 78 74 76 76 73 76 74 74 60 40 20 Organ Donation Past, Present and Future sh ire rk Yo h t ut es So W So u Ea th st So W uth al es C Team 1 April 2012 to 31 March 2013, data as at 4 April 2013 So en uth tr al nd la ot Sc or t Ire her la n nd er n N or th N o W rth es t N s nd la M id on nd Lo Ea st er n 0 ---- National rate 7
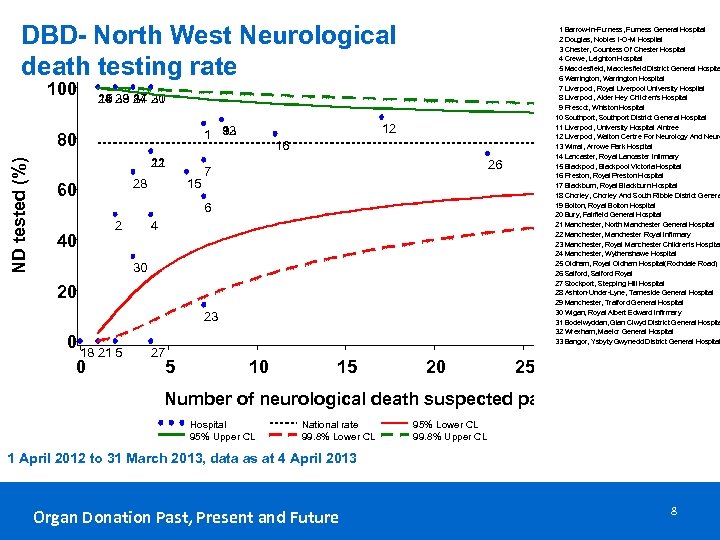
DBD- North West Neurological death testing rate 100 25 19 3 8 14 33 24 31 10 29 17 20 12 9 32 1 13 80 ND tested (%) 1 Barrow-In-Furness, Furness General Hospital 2 Douglas, Nobles I-O-M Hospital 3 Chester, Countess Of Chester Hospital 4 Crewe, Leighton Hospital 5 Macclesfield, Macclesfield District General Hospita 6 Warrington, Warrington Hospital 7 Liverpool, Royal Liverpool University Hospital 8 Liverpool, Alder Hey Children's Hospital 9 Prescot, Whiston Hospital 10 Southport, Southport District General Hospital 11 Liverpool, University Hospital Aintree 12 Liverpool, Walton Centre For Neurology And Neuro 13 Wirral, Arrowe Park Hospital 14 Lancaster, Royal Lancaster Infirmary 15 Blackpool, Blackpool Victoria Hospital 16 Preston, Royal Preston Hospital 17 Blackburn, Royal Blackburn Hospital 18 Chorley, Chorley And South Ribble District Genera 19 Bolton, Royal Bolton Hospital 20 Bury, Fairfield General Hospital 21 Manchester, North Manchester General Hospital 22 Manchester, Manchester Royal Infirmary 23 Manchester, Royal Manchester Children's Hospital 24 Manchester, Wythenshawe Hospital 25 Oldham, Royal Oldham Hospital(Rochdale Road) 26 Salford, Salford Royal 27 Stockport, Stepping Hill Hospital 28 Ashton-Under-Lyne, Tameside General Hospital 29 Manchester, Trafford General Hospital 30 Wigan, Royal Albert Edward Infirmary 31 Bodelwyddan, Glan Clwyd District General Hospita 32 Wrexham, Maelor General Hospital 33 Bangor, Ysbyty Gwynedd District General Hospital 22 11 28 60 15 16 26 7 6 40 2 4 30 20 23 0 18 21 5 0 27 5 10 15 20 25 30 Number of neurological death suspected patients Hospital 95% Upper CL National rate 99. 8% Lower CL 95% Lower CL 99. 8% Upper CL 1 April 2012 to 31 March 2013, data as at 4 April 2013 Organ Donation Past, Present and Future 8
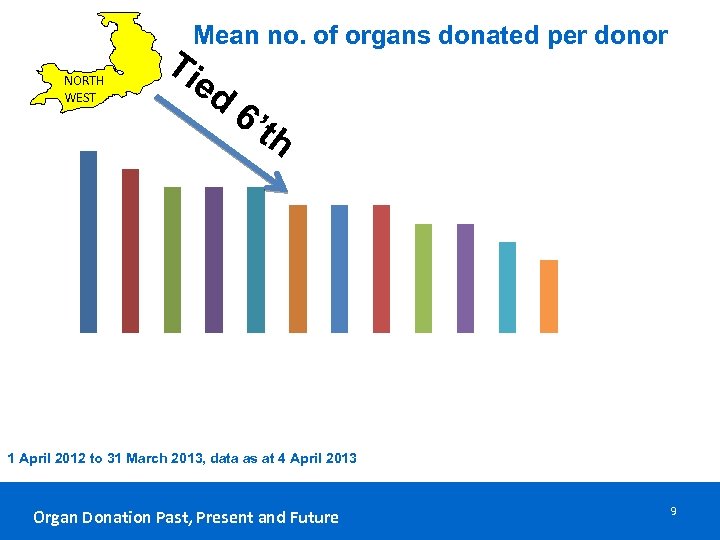
Ti Mean no. of organs donated per donor ed NORTH WEST 4. 4 4. 2 6’ th 4. 0 3. 8 3. 6 3. 4 an or ds th er Ire la nd So ut h Ea st N or th W es t Sc ot la nd Yo rk sh ire Lo nd on So ut h W So es ut t h C en So tra l ut h W al es id l N M st er n Ea N or th er n 3. 2 1 April 2012 to 31 March 2013, data as at 4 April 2013 Organ Donation Past, Present and Future 9
Diagnosis of brain-stem death 1976 2008 37 years on Organ Donation Past, Present and Future 10
Moses Maimonides: a decapitated person was immediately dead despite the presence of residual movement in the body History of Diagnosing Death Organ Donation Past, Present and Future 12 th Century 11
Harvey Cushing describes increased brain pressure provoking respiratory arrest with preserved heartbeat. History of Diagnosing Death Early Organ Donation Past, Present and Future 20 th Century 12
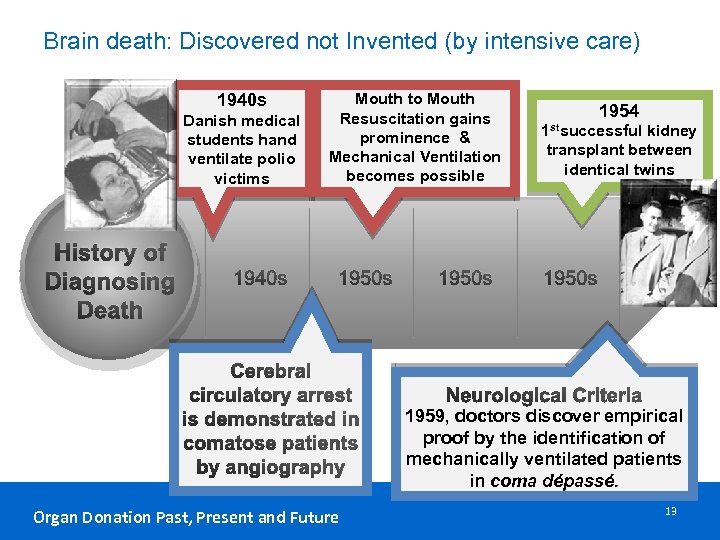
Brain death: Discovered not Invented (by intensive care) 1940 s Danish medical students hand ventilate polio victims History of Diagnosing Death 1940 s Mouth to Mouth Resuscitation gains prominence & Mechanical Ventilation becomes possible 1950 s Cerebral circulatory arrest is demonstrated in comatose patients by angiography Organ Donation Past, Present and Future 1950 s 1954 1 stsuccessful kidney transplant between identical twins 1950 s Neurological Criteria 1959, doctors discover empirical proof by the identification of mechanically ventilated patients in coma dépassé. 13
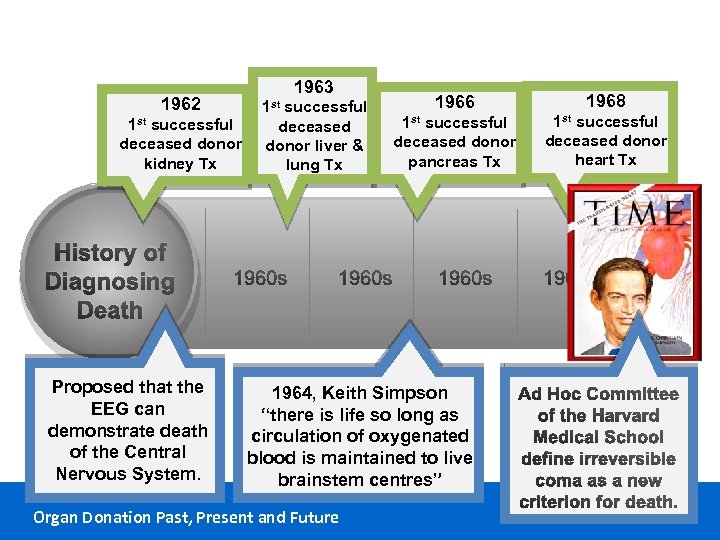
1963 1962 1 st successful deceased donor kidney Tx History of Diagnosing Death Proposed that the EEG can demonstrate death of the Central Nervous System. 1 st successful deceased donor liver & lung Tx 1960 s 1966 1968 1 st successful deceased donor pancreas Tx 1 st successful deceased donor heart Tx 1960 s 1964, Keith Simpson “there is life so long as circulation of oxygenated blood is maintained to live brainstem centres” Organ Donation Past, Present and Future 1960 s Ad Hoc Committee of the Harvard Medical School define irreversible coma as a new criterion for death. 14

Organ Donation from Brain Dead donors increases worldwide. Modern intensive care practice grows. History of Diagnosing Death Late 20 th Century 1976 (clarified 1979) UK Criteria for Diagnosing Death using Neurological Criteria Published. Organ Donation Past, Present and Future 15
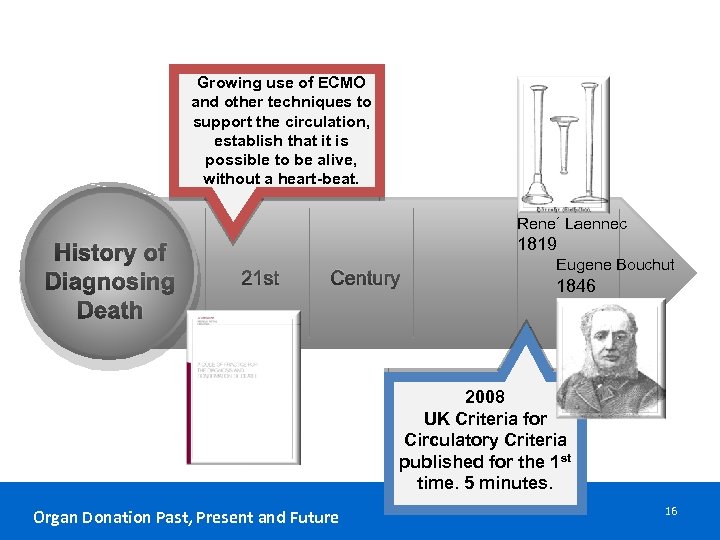
Growing use of ECMO and other techniques to support the circulation, establish that it is possible to be alive, without a heart-beat. Rene´ Laennec History of Diagnosing Death 1819 21 st Century Eugene Bouchut 1846 2008 UK Criteria for Circulatory Criteria published for the 1 st time. 5 minutes. Organ Donation Past, Present and Future 16
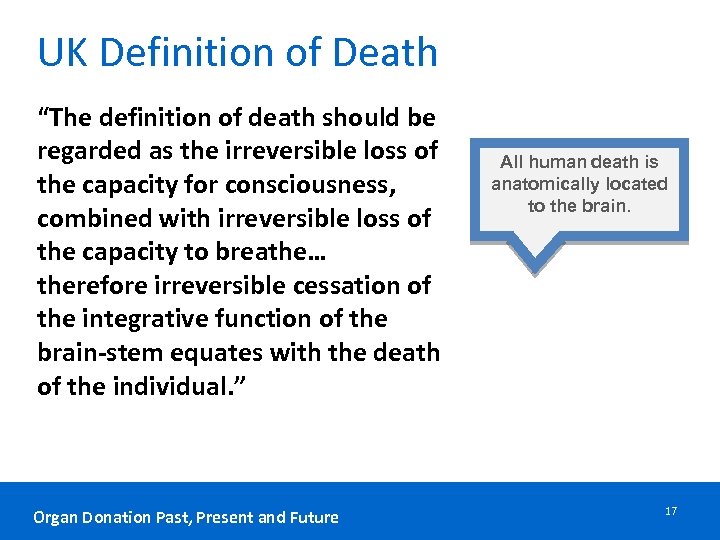
UK Definition of Death “The definition of death should be regarded as the irreversible loss of the capacity for consciousness, combined with irreversible loss of the capacity to breathe… therefore irreversible cessation of the integrative function of the brain-stem equates with the death of the individual. ” Organ Donation Past, Present and Future All human death is anatomically located to the brain. 17
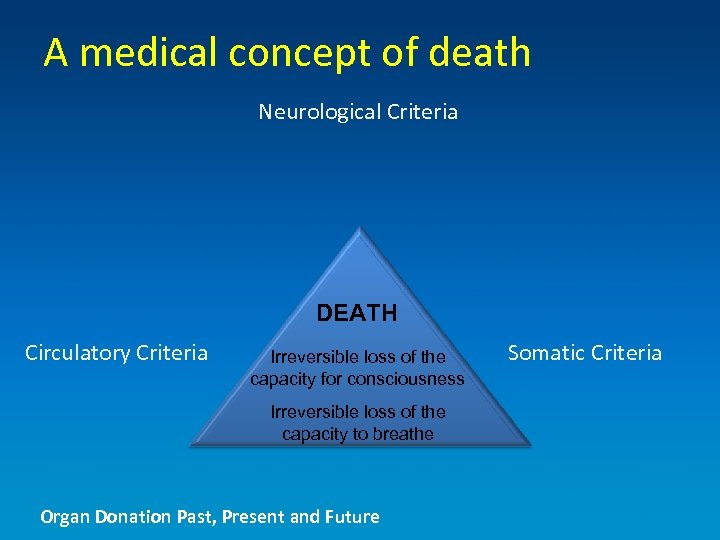
A medical concept of death Neurological Criteria DEATH Circulatory Criteria Irreversible loss of the capacity for consciousness Irreversible loss of the capacity to breathe Organ Donation Past, Present and Future Somatic Criteria
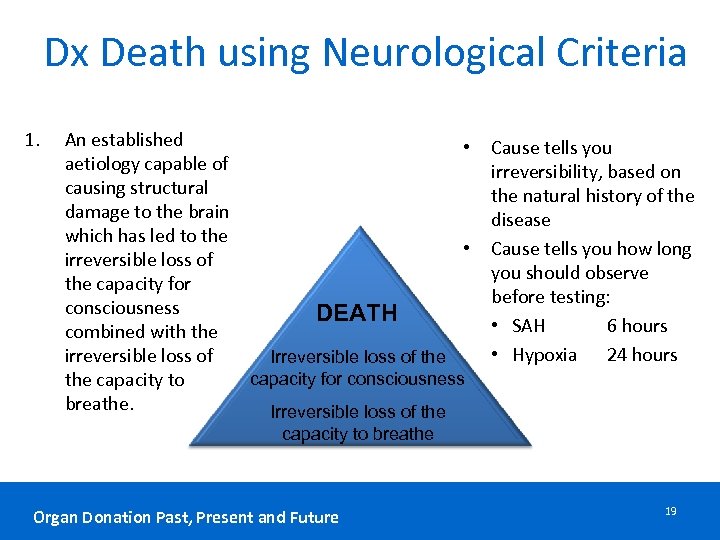
Dx Death using Neurological Criteria 1. An established • aetiology capable of causing structural damage to the brain which has led to the • irreversible loss of the capacity for consciousness DEATH combined with the irreversible loss of Irreversible loss of the capacity for consciousness the capacity to breathe. Irreversible loss of the Cause tells you irreversibility, based on the natural history of the disease Cause tells you how long you should observe before testing: • SAH 6 hours • Hypoxia 24 hours capacity to breathe Organ Donation Past, Present and Future 19
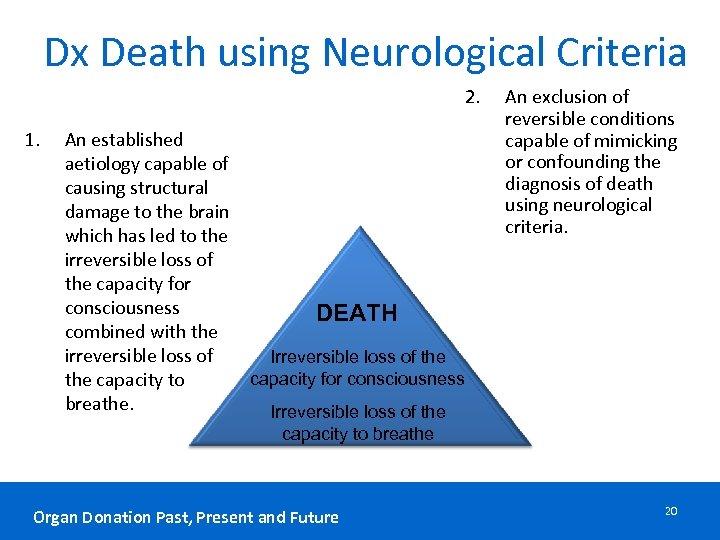
Dx Death using Neurological Criteria 2. 1. An established aetiology capable of causing structural damage to the brain which has led to the irreversible loss of the capacity for consciousness DEATH combined with the irreversible loss of Irreversible loss of the capacity for consciousness the capacity to breathe. Irreversible loss of the An exclusion of reversible conditions capable of mimicking or confounding the diagnosis of death using neurological criteria. capacity to breathe Organ Donation Past, Present and Future 20
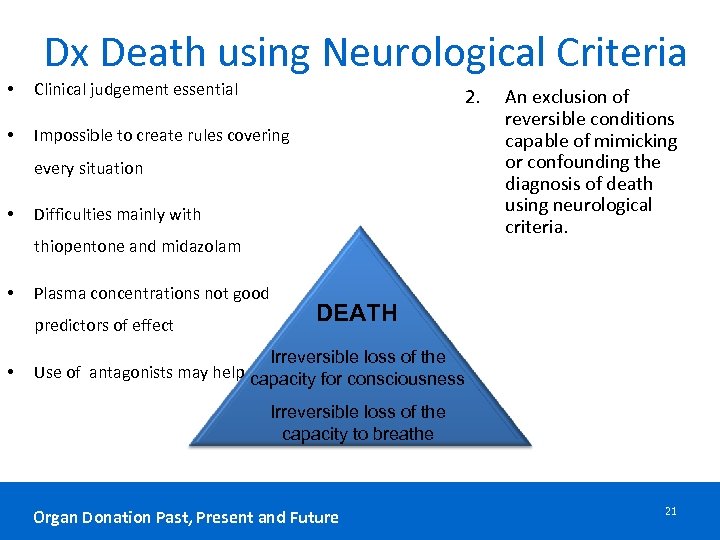
Dx Death using Neurological Criteria • Clinical judgement essential • Impossible to create rules covering 2. every situation • Difficulties mainly with thiopentone and midazolam • Plasma concentrations not good predictors of effect • An exclusion of reversible conditions capable of mimicking or confounding the diagnosis of death using neurological criteria. DEATH Irreversible loss of the Use of antagonists may help capacity for consciousness Irreversible loss of the capacity to breathe Organ Donation Past, Present and Future 21
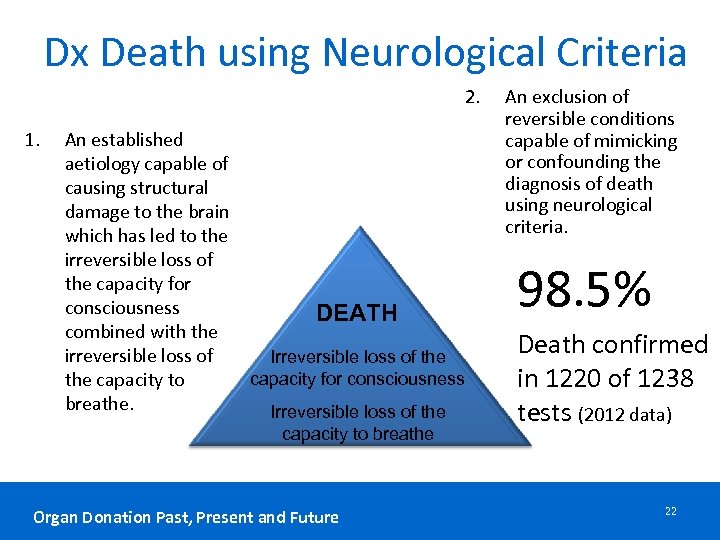
Dx Death using Neurological Criteria 2. 1. An established aetiology capable of causing structural damage to the brain which has led to the irreversible loss of the capacity for consciousness DEATH combined with the irreversible loss of Irreversible loss of the capacity for consciousness the capacity to breathe. Irreversible loss of the capacity to breathe Organ Donation Past, Present and Future An exclusion of reversible conditions capable of mimicking or confounding the diagnosis of death using neurological criteria. 98. 5% Death confirmed in 1220 of 1238 tests (2012 data) 22
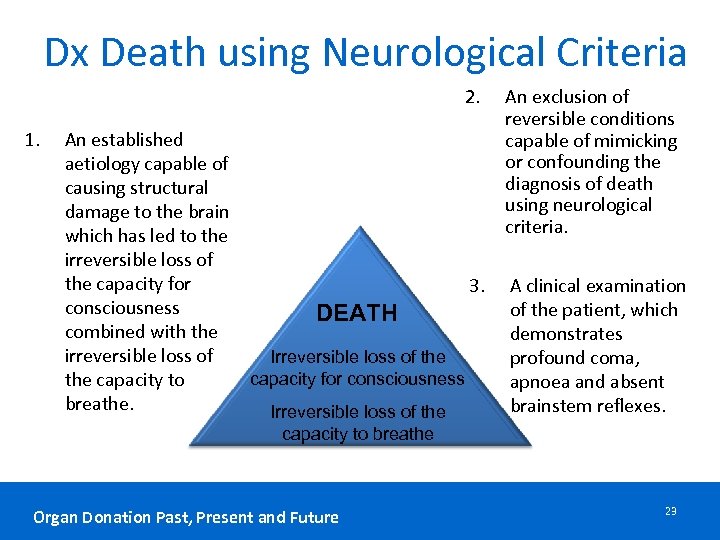
Dx Death using Neurological Criteria 2. 1. An established aetiology capable of causing structural damage to the brain which has led to the irreversible loss of the capacity for 3. consciousness DEATH combined with the irreversible loss of Irreversible loss of the capacity for consciousness the capacity to breathe. Irreversible loss of the An exclusion of reversible conditions capable of mimicking or confounding the diagnosis of death using neurological criteria. A clinical examination of the patient, which demonstrates profound coma, apnoea and absent brainstem reflexes. capacity to breathe Organ Donation Past, Present and Future 23
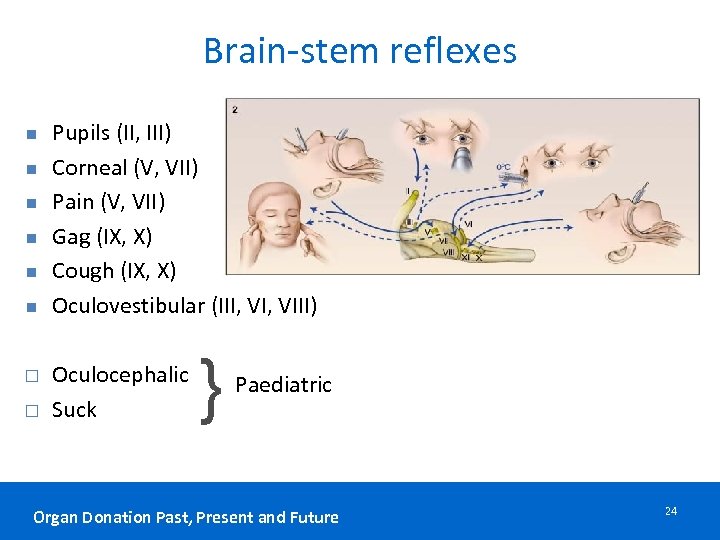
Brain-stem reflexes n n n Pupils (II, III) Corneal (V, VII) Pain (V, VII) Gag (IX, X) Cough (IX, X) Oculovestibular (III, VIII) Oculocephalic Suck } Paediatric Organ Donation Past, Present and Future 24
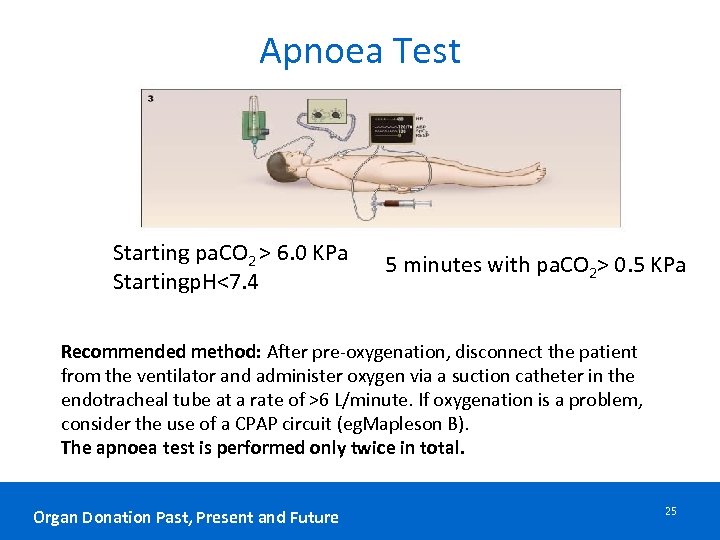
Apnoea Test Starting pa. CO 2 > 6. 0 KPa Startingp. H<7. 4 5 minutes with pa. CO 2> 0. 5 KPa Recommended method: After pre-oxygenation, disconnect the patient from the ventilator and administer oxygen via a suction catheter in the endotracheal tube at a rate of >6 L/minute. If oxygenation is a problem, consider the use of a CPAP circuit (eg. Mapleson B). The apnoea test is performed only twice in total. Organ Donation Past, Present and Future 25
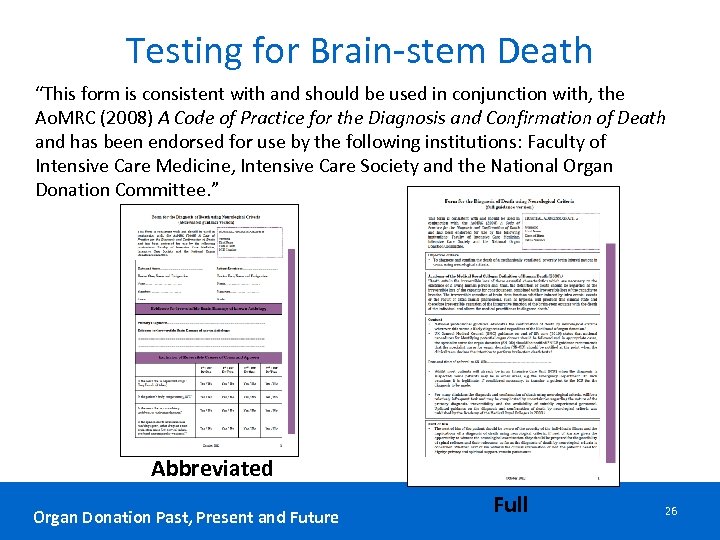
Testing for Brain-stem Death “This form is consistent with and should be used in conjunction with, the Ao. MRC (2008) A Code of Practice for the Diagnosis and Confirmation of Death and has been endorsed for use by the following institutions: Faculty of Intensive Care Medicine, Intensive Care Society and the National Organ Donation Committee. ” Abbreviated Organ Donation Past, Present and Future Full 26

Organ Donation Past, Present and Future 27

WHY TEST? Organ Donation Past, Present and Future
A guiding dignity consistent approach to declaring death • Dying, is a process, which effects different functions and cells of the body at different rates of decay. • Doctors must decide at what moment along this process there is permanence and death can be appropriately declared. Organ Donation Past, Present and Future
A doctors duty Diagnose the dead 1. Safe – no coming back to life after death declared 2. Timely – no unnecessary delay Organ Donation Past, Present and Future

WHY TEST? Where Brain Stem Death (BSD) is suspected, it is highly desirable to confirm this by Brain Stem Testing: • To eliminate all possible doubt regarding survivability • To confirm diagnosis for families • In cases subject to medico-legal scrutiny • To provide choice regarding organ donation Organ Donation Past, Present and Future

diagnosis decision Organ Donation Past, Present and Future
TWO TESTS or ONE? • National professional guidance mandates two tests to be performed regardless of organ donation (Bolam&Bolithio). • Same two doctors carry out the second set of tests immediately after the first set (update family and stabilise patient). • Death is retrospectively confirmed at the conclusion of the second test. Until then, as a matter of law and ethics, it is necessary to treat the patient as alive. Organ Donation Past, Present and Future
1976 2008 Lesson 1 Organ Donation Past, Present and Future
Lesson 2 To Dx Use Organ Donation Past, Present and Future
Lesson 3 Take your time • Atypical presentation • Hypoxic brain injury >24 hours Organ Donation Past, Present and Future
Lesson 4 Induced hypothermia has unpredictable consequences See Lesson 3 Organ Donation Past, Present and Future

Lesson 5 NO EEG Organ Donation Past, Present and Future
Lesson 6 Start with Lesson 2 = use your brain and examine your patient 1. Clinical brain death + NO flow 2. Clinical brain death + flow = Death = Wait See Lesson 3 = take your time and ask ‘Is reversibility possible? ’ Organ Donation Past, Present and Future

Optimising the brainstem dead donor Organ Donation Past, Present and Future 40
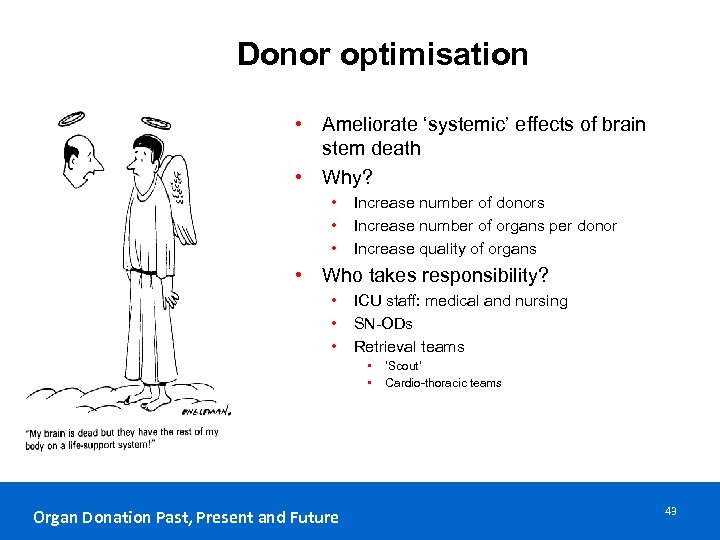
Donor optimisation • Ameliorate ‘systemic’ effects of brain stem death • Why? • • • Increase number of donors Increase number of organs per donor Increase quality of organs • Who takes responsibility? • • • ICU staff: medical and nursing SN-ODs Retrieval teams • • Organ Donation Past, Present and Future ‘Scout’ Cardio-thoracic teams 43
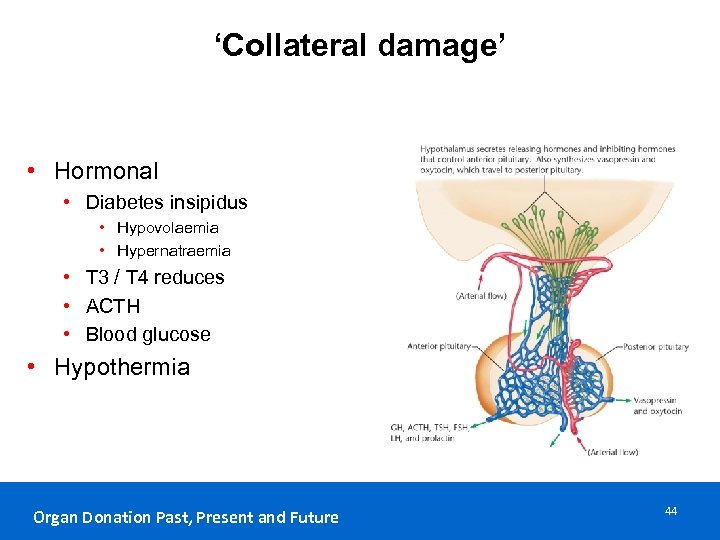
‘Collateral damage’ • Hormonal • Diabetes insipidus • Hypovolaemia • Hypernatraemia • T 3 / T 4 reduces • ACTH • Blood glucose • Hypothermia Organ Donation Past, Present and Future 44
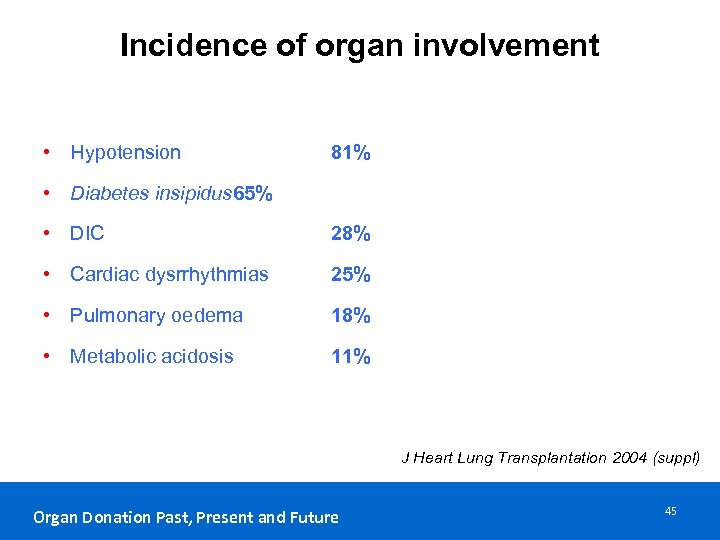
Incidence of organ involvement • Hypotension 81% • Diabetes insipidus 65% • DIC 28% • Cardiac dysrrhythmias 25% • Pulmonary oedema 18% • Metabolic acidosis 11% J Heart Lung Transplantation 2004 (suppl) Organ Donation Past, Present and Future 45
Organ Donation Past, Present and Future 46
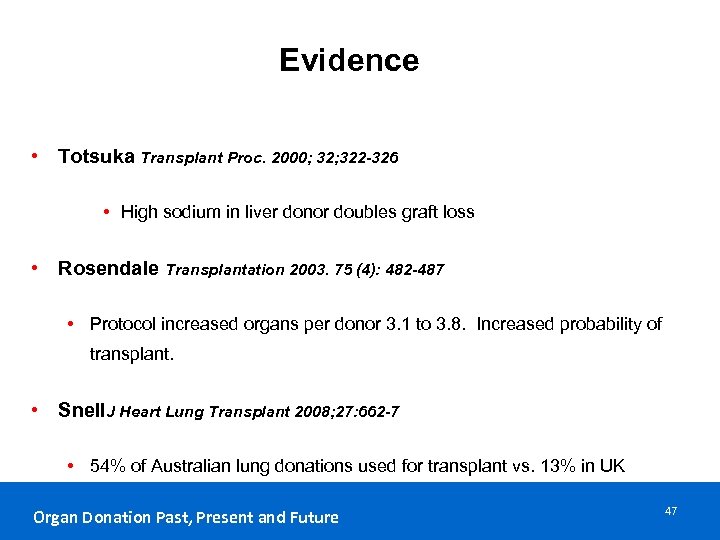
Evidence • Totsuka Transplant Proc. 2000; 322 -326 • High sodium in liver donor doubles graft loss • Rosendale Transplantation 2003. 75 (4): 482 -487 • Protocol increased organs per donor 3. 1 to 3. 8. Increased probability of transplant. • Snell. J Heart Lung Transplant 2008; 27: 662 -7 • 54% of Australian lung donations used for transplant vs. 13% in UK Organ Donation Past, Present and Future 47
Principles • Ameliorate ‘systemic’ effects of brain stem death • Why? • Increase number of donors • Increase number of organs per donor • Increase quality of organs • Who takes responsibility? • ICU staff: medical and nursing • SN-ODs • Retrieval teams • ‘Scout’: who are they attached to? • Cardio-thoracic teams • Abdominal teams • Free standing Organ Donation Past, Present and Future 48
What do we aim for ? • General stability • Examples of target values • MAP: 60 – 80 mm Hg • Heart rate: 60 – 100 / min SR • CI: > 2. 1 l/min/m 2 • Guidelines • • • Australian Canadian Map of Medicine ICS NHSBT Organ Donation Past, Present and Future 49
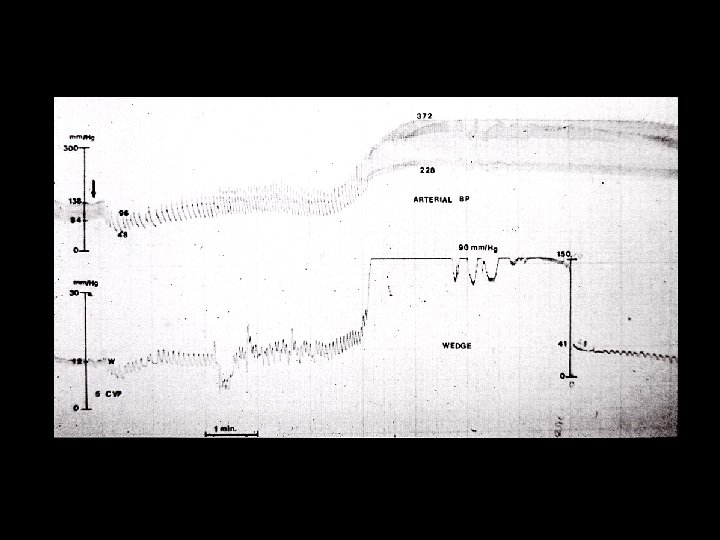
Cardiovascular management • Summary of cardio vascular target values • • • MAP: 60 – 80 mm Hg CVP: 4 – 10 mm Hg Heart rate: 60 – 100/min SR CI: > 2. 1 l/min/m 2 (can be higher, be aware of myocardial stunning) Filling targets: no good evidence for any specific targets, depends on device • Sv. O 2> 60% • SVRI target • Secondary target • Dehydration temptation to maintain MAP with vasopressors rather than filling Organ Donation Past, Present and Future 50
Respiratory management • Recruitment manoeuvre • Post BSD testing: apnoea test resulting in atelectasis • After suctioning / disconnection • When Sp. O 2 drops / Fi. O 2 increases • • Lung protective ventilation: 4 – 8 ml/kg ideal body weight Permissive hypercapnia with p. H > 7. 25 Optimum PEEP (5 – 10 cm H 2 O) and Fi. O 2 (aim for < 0. 4 as able) Head–up positioning (30 - 45°) Suctioning, physiotherapy as required Antibiotics for purulent secretions: local microbiology surveillance Avoid over-hydration Organ Donation Past, Present and Future 51
Managing Diabetes insipidus • Very common occurrence • Pathophysiology • Posterior pituitary failure • Polyuria: output > 4 ml/kg/h • Dehydration with Na+ • Usually at least partially addressed with stabilisation for BSD testing • Treatment: • Fluids • Vasopressin • DDAVP • Aim for u-output 0. 5 – 2. 0 ml / kg / h Organ Donation Past, Present and Future 52
Hormonal treatment • Vasopressin • Reduction in other vaso-active drugs • Dose: 1 – 4 units/h (can start with boluses of 1 unit at a time) • Liothyronine (T 3) • No clear evidence yet for either use or not • May add haemodynamic stability in very unstable donor • Dose: 3 units/h, sometimes bolus of 4 units asked for by retrieval team • Methylprednisolone in all cases • Dose: 15 mg/kg up to 1 g • Insulin • At least 1 unit/h (Occasionally may need to add glucose infusion) • ‘Tight’ glycaemic control (4 - 10 mmol/l) Organ Donation Past, Present and Future 53
Haematological management • DIC seen occasionally as direct consequence of BSD • May require correcting prior to BSD testing if bleeding • Hb> 8 g/dl (~ 10 g/dl traditionally advocated) (even > 7 g/dl ? ) • No evidence on harm with lower Hb, but some evidence of harm with blood transfusions and organ function post transplant • Where Hb borderline, ensure blood available for retrieval procedure: local protocols and antibodies will determine whether G&S only, or units to be cross matched • Use of clotting factors • • Only where bleeding is an issue Monitor clotting status Use local hospital protocol Retrieval procedure may require additional products Organ Donation Past, Present and Future 54
General measures • Maintain normothermia (active warming may be required) • Thrombo-embolism prophylaxis • Stockings • Sequential compression devices • LMWH • Positioning • Head-up • Side to side • Attention to cuff pressures and leaks to prevent aspiration • Continue NG feeding (may be reduced/ stopped for bowel transplant) • Antibiotics according to sensitivities or empirical according to Trust guidelines Organ Donation Past, Present and Future 55
Monitoring optimisation • Implementation: use of care bundle • Adherence easy to monitor • Audit first 5 priorities • Results of optimisation evaluated • Number of organs retrieved • Increase in cardiothoracic organs retrieved • Quality of organs: organ function in recipients • Delayed graft function • Quality: biomarkers • Duration of graft function: long term project Organ Donation Past, Present and Future 56
094e727e5108e0032fd735bbcc67748d.ppt