1c96ffbc21d8068cde4467b219c476c5.ppt
- Количество слайдов: 30

Dollars and Sense of Rehab Part 2: Physician Payment Systems Sue Palsbo, Ph. D, MS NRH Center for Health & Disability Research

Goals for Understanding • • History of Medicare physician payment Alternatives to FFS payment Spreading financial risk Understand parts of a managed care contract

What is Medicare? • Federal program • Part A -- Inpatient (facility and house staff) -- acute hospitals, rehab hospitals, SNFs • Part B -- Outpatient, physician, durable medical equipment, home care

Who is Medicare? • Aged -- most people age 65+ – Entitled separately to Part A and Part B – Sometimes, your patient will be entitled to Part A, but NOT Part B • Disabled -- mostly people with psychiatric disabilities, or people who were employed and then became disabled • Sometimes, Medicare beneficiaries are also eligible for Medicaid

What is Medicaid? • State programs – Combined with Federal money • Pays for medical care • Often more generous than Medicare when covering durable medical equipment and assistive devices • Pays for Rx • Pays for transportation to doctor’s appointments

Who is Medicaid? • Eligibility varies state to state – Poor – Blind – TANF (temporary assistance to needy families) – SCHIP (state children’s health insurance programs) • Disabled -- mostly people with developmental disabilities

Dual Eligibles • People who have both Medicare and Medicaid coverage

History of Physician Payments FFS • UCR – Usual (simple average of what you charge) – Customary (what most people in your area charge) – Reasonable (some percentile of what everyone charges) – Insurers pay you the least of these 3 • You can BUY this information (so can other payers)

Example • CPT 99205. Evaluation and management of a new patient, which requires these 3 components: – a comprehensive history – a comprehensive examination – medical decision making of high complexity • Counseling and coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. • Usually, the presenting problems are of moderate to high severity. Physicians typically spend 60 minutes face-to-face with the patient and/or family • e. g. : Initial office evaluation and management of patient with systemic vasculitis and compromised circulation to the limbs. • Others?

How Much Do You Charge?

Consequences (Gaming the System)

History of Physician Payments RB-RVS

Overall PPS Methodology Nation-wide base dollar amount Nation-wide condition multiplier Local geographic wage multiplier Payment
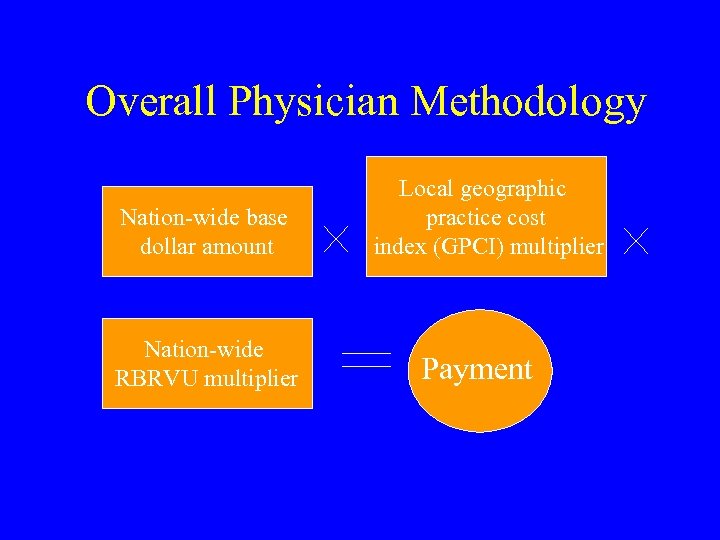
Overall Physician Methodology Nation-wide base dollar amount Nation-wide RBRVU multiplier Local geographic practice cost index (GPCI) multiplier Payment



Impact of RBRVS • • • Physicians increased volume CMS clamped down on fees to compensate Physicians upcoded complexity CMS rebalanced RVU scale to compensate Physicians declined to “participate” Congress passed limit on non-participating fees (115%? ) • Cottage industry to develop RVUs for “gap codes”

Private Sector Insurance

OWAs • Per Diem • Global Fees • Balance Billing

Difference Between HMOs and PPOs • Deductibles • Co-insurance • Co-payment

You Will Probably Not Be Alone

HMO Enrollment



Capitation Contracts by Specialty

Why Capitate? • Shifts financial risk from insurer to you! – Your patient may be on Medicaid; Medicaid capitates the HMO • • Large numbers of people/encounters Define by CPT Rate books (utilization and pmpm) Risk adjustment (age/sex/condition) – http: //www. nrhchdr. org/RAField. Guide. prn. pdf • My advice: Retain an actuary!

Contact capitation

Stop-loss reinsurance • Accumulators – Per patient – In aggregate • Thresholds

Coordination of Benefits • Primary • Secondary • Auto, etc.
1c96ffbc21d8068cde4467b219c476c5.ppt