206bd22ecbad6785ad870181885ac7ab.ppt
- Количество слайдов: 52
DISTRICT OF COLUMBIA DC HEALTH SYSTEMS PLAN: PUBLIC HEARING MAY 25, 2017 899 N. CAPITOL STREET NE CONFERENCE ROOM 6002
Goals of Session o Background & Purpose of Health Systems Plan o Overview Approach and Methods o Context of Health Systems Plan o Review of Core Findings and Recommendations o Discussion of Revisions to Certificate of Need 2
Background and Purpose of Health Systems Plan 3
Purpose of DC Health Systems Plan The purpose of the Health Systems Plan is to serve as a roadmap for the development of a comprehensive, accessible, and equitable health care system capable of providing the highest quality services in a cost effective manner to those who live and work in DC.
Purpose of DC Health Systems Plan • • Focus on DC health system & core elements of service Not a comprehensive community health needs assessment Not meant to replicate the broad range of health assessments and plans that have been released in past 2 -3 years • DOH CHNA, Healthy Communities CHNA, Comprehensive Plan, DC Health Matters, HP 2020, BRFSS, Age-Friendly DC, Cancer Control Plan Meant to add value to other assessments and serve as a guide for the SHCC with respect to the Certificate of Need Program.
Components of DC Health Systems Plan • Community Characteristics: Demographics, underlying social determinants of health, barriers to care, and health status • Health System Strengths, Service Distribution, and Utilization: Hospital services, primary care and specialty care, behavioral health, and post-acute care services • Health System Structures: Surveillance, health information technology, workforce development, collaboration, health literacy • Strategic Recommendations
Overview of Approach 7
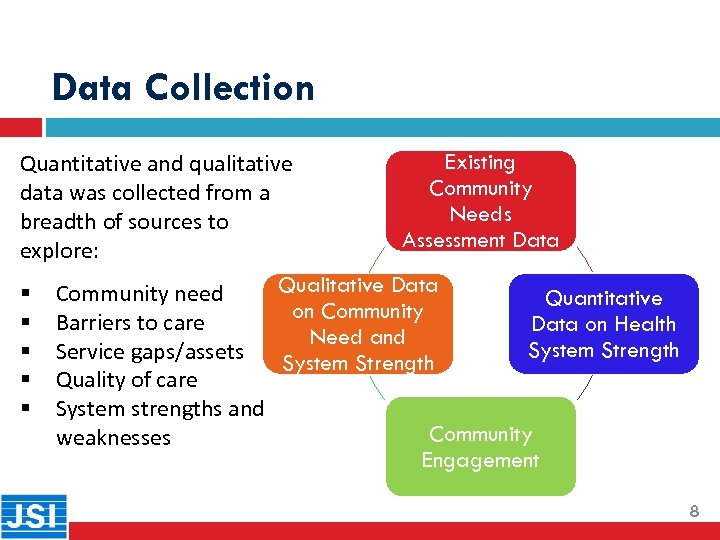
Data Collection Existing Quantitative and qualitative Community data was collected from a Needs breadth of sources to Assessment Data explore: Qualitative Data § Community need Quantitative on Community § Barriers to care Data on Health Need and System Strength § Service gaps/assets System Strength § Quality of care § System strengths and Community weaknesses Engagement 8
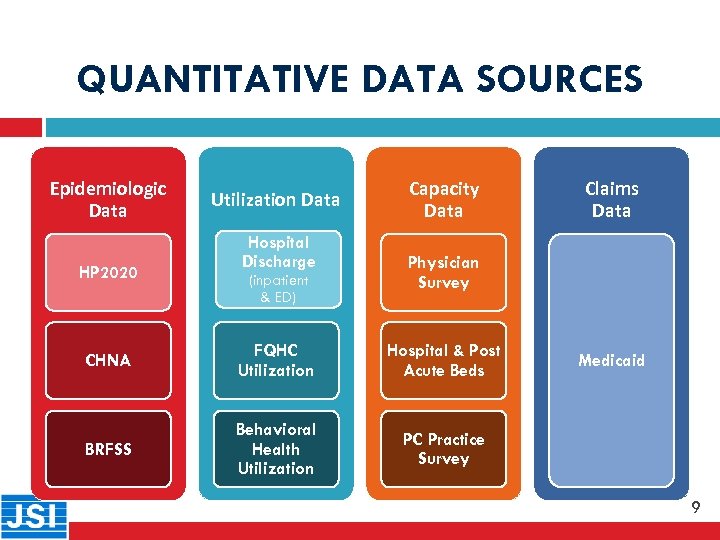
QUANTITATIVE DATA SOURCES 9 Epidemiologic Data HP 2020 Utilization Data Hospital Discharge (inpatient & ED) Capacity Data Claims Data Physician Survey CHNA FQHC Utilization Hospital & Post Acute Beds BRFSS Behavioral Health Utilization PC Practice Survey Medicaid 9

QUALITATIVE DATA SOURCES Key informant interviews with: • 10 • • • Hospitals and Hospital Affiliates: Med. Star Georgetown, Med. Star Washington, Med. Star Health, Med. Star Primary Care/Prompt Care, Children’s Hospital, Providence, Sibley, Howard, UMC, GWU, Medical Faculty Associates, etc. DC DOH: Office of Health Equity, Oral Health, HAHSTA, Health Care Finance, Licensing and Regulation, etc. DC Government: DBH, Office of Planning, Dept. of Insurance, Securities, and Banking, Fire and EMS, Metropolitan Police Department, etc. Health Associations and Boards: Hospital Association, Health Care Association, Board of Nursing, Primary Care Association, Home Health Association, Medical Society, etc. Community Advocacy Groups: DC Coalition for the Homeless, Coalition for Non Profit Housing and Economic Development, Capitol Area Food Bank, etc. Health Care Providers: Community of Hope, Unity, Mary’s Center, Bread for the City, SOME, Whitman-Walker, Core Health, Planned Parenthood, Psychiatric Institute, Stoddard Baptist Home, etc. Other: Amerihealth, Health EC, Georgetown University, etc. 10
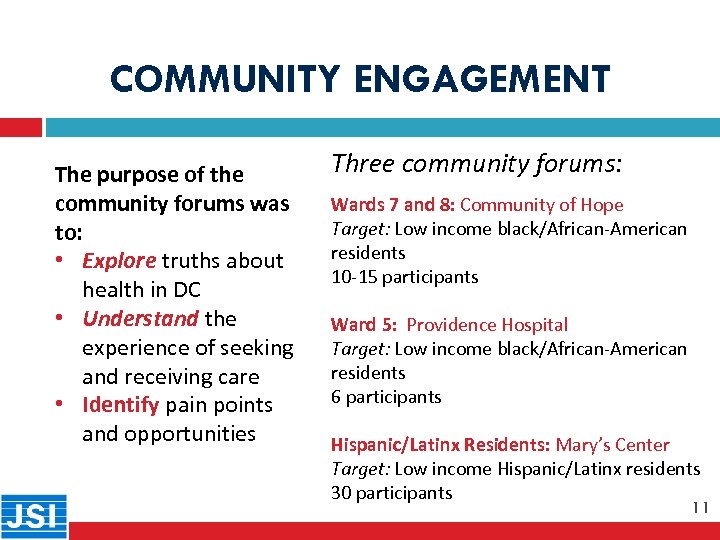
COMMUNITY ENGAGEMENT 11 The purpose of the community forums was to: • Explore truths about health in DC • Understand the experience of seeking and receiving care • Identify pain points and opportunities Three community forums: Wards 7 and 8: Community of Hope Target: Low income black/African-American residents 10 -15 participants Ward 5: Providence Hospital Target: Low income black/African-American residents 6 participants Hispanic/Latinx Residents: Mary’s Center Target: Low income Hispanic/Latinx residents 30 participants 11
Context of Health Systems Plan 12
Population Health Model Researchers have consistently determined that only 10 -20% of health is attributable to clinical services; the remainder is linked to genetics, behavior, and social and physical environments. http: //www. countyhealthrankings. org/ranking-methods
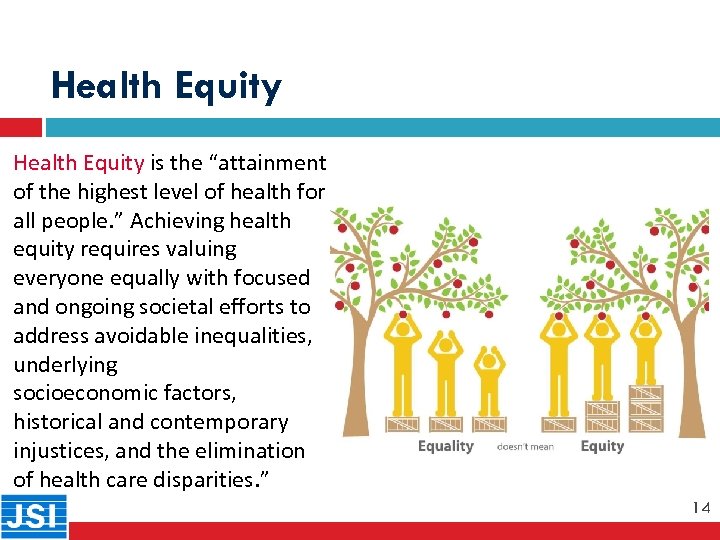
Health Equity is the “attainment of the highest level of health for all people. ” Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, underlying socioeconomic factors, historical and contemporary injustices, and the elimination of health care disparities. ” 14
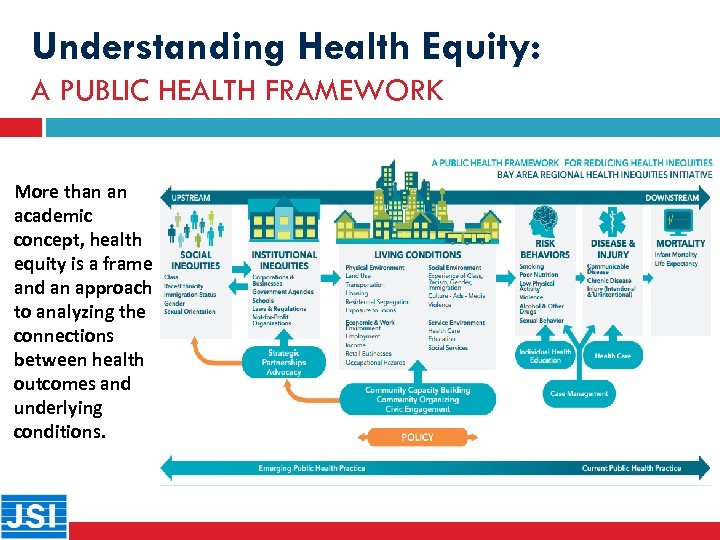
Understanding Health Equity: A PUBLIC HEALTH FRAMEWORK More than an academic concept, health equity is a frame and an approach to analyzing the connections between health outcomes and underlying conditions.
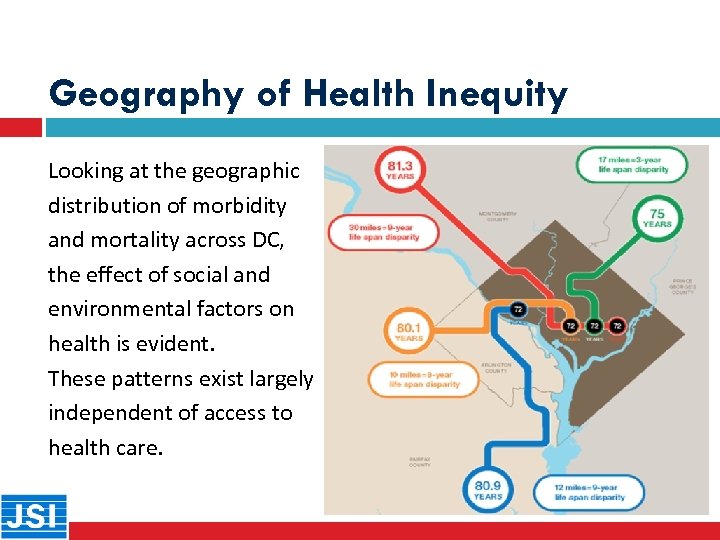
Geography of Health Inequity Looking at the geographic distribution of morbidity and mortality across DC, the effect of social and environmental factors on health is evident. These patterns exist largely independent of access to health care.
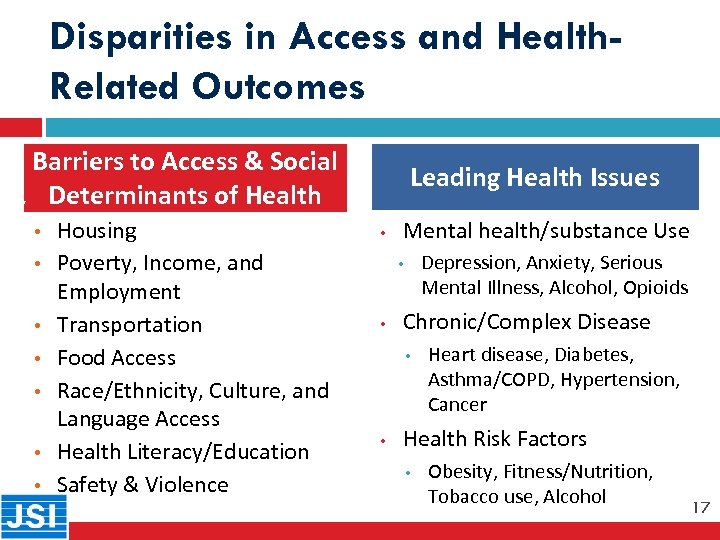
Disparities in Access and Health. Related Outcomes Barriers to Access & Social Determinants of Health 17 • • Housing Poverty, Income, and Employment Transportation Food Access Race/Ethnicity, Culture, and Language Access Health Literacy/Education Safety & Violence Leading Health Issues • Mental health/substance Use Depression, Anxiety, Serious Mental Illness, Alcohol, Opioids • • Chronic/Complex Disease • • Heart disease, Diabetes, Asthma/COPD, Hypertension, Cancer Health Risk Factors • Obesity, Fitness/Nutrition, Tobacco use, Alcohol 17
Segments of the Population Most At-Risk Populations Most At-Risk • • Low income individuals and families Racial/ethnic minorities Immigrants and refugees Older adults Children, youth, and adolescents LGBTQ Incarcerated Populations Developmentally/intellectually challenged or special needs adults and children
Health System Strengths: Review of Core Findings 19
Core Finding # 1: SERVICE GAPS/CAPACITY Distribution and capacity of services is not the leading concern across service sectors 20 o o o DC is rich in health-related resources Limited to no gaps in service o Reasonably well-distributed services o High quality of care This is not to say that all segments of the population are fully engaged in care or that there are not some who face barriers to access 20
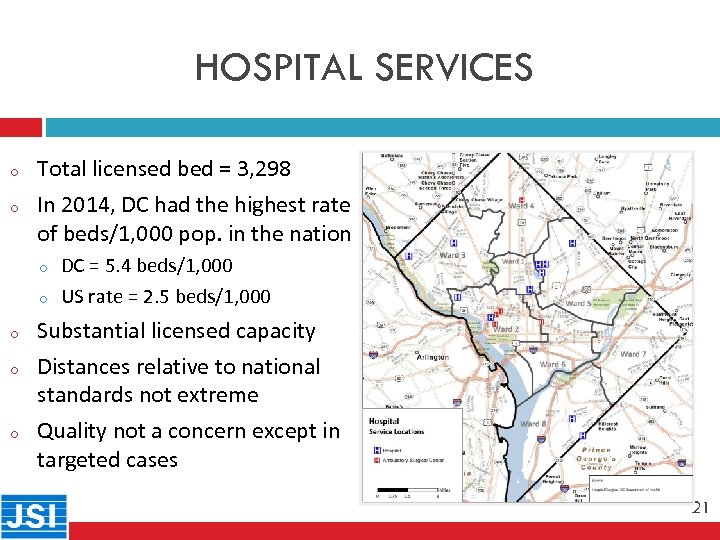
HOSPITAL SERVICES o 21 o Total licensed bed = 3, 298 In 2014, DC had the highest rate of beds/1, 000 pop. in the nation o o o DC = 5. 4 beds/1, 000 US rate = 2. 5 beds/1, 000 Substantial licensed capacity Distances relative to national standards not extreme Quality not a concern except in targeted cases 21
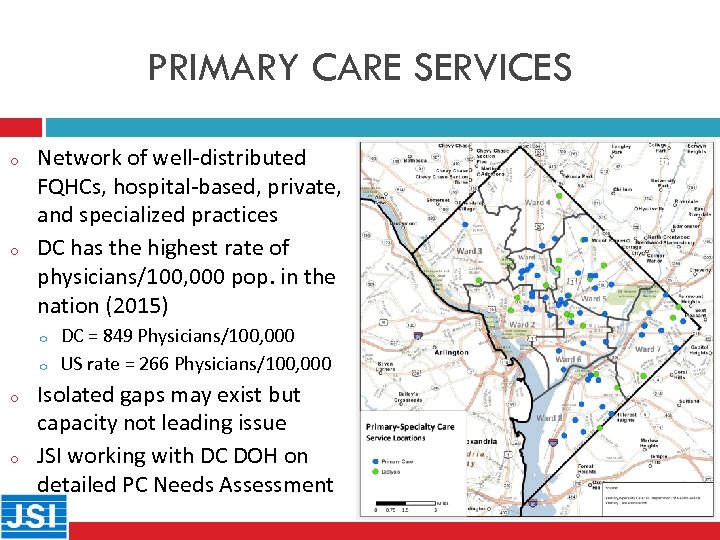
PRIMARY CARE SERVICES o 22 o Network of well-distributed FQHCs, hospital-based, private, and specialized practices DC has the highest rate of physicians/100, 000 pop. in the nation (2015) o o DC = 849 Physicians/100, 000 US rate = 266 Physicians/100, 000 Isolated gaps may exist but capacity not leading issue JSI working with DC DOH on detailed PC Needs Assessment 22
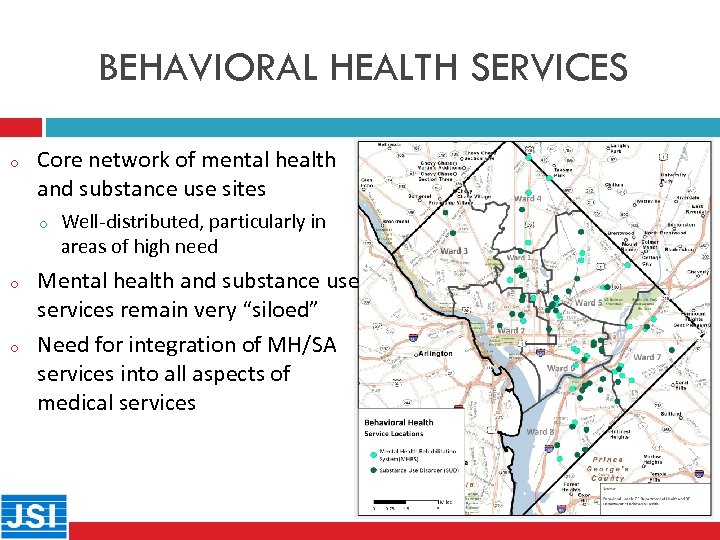
BEHAVIORAL HEALTH SERVICES o 23 Core network of mental health and substance use sites o o o Well-distributed, particularly in areas of high need Mental health and substance use services remain very “siloed” Need for integration of MH/SA services into all aspects of medical services 23
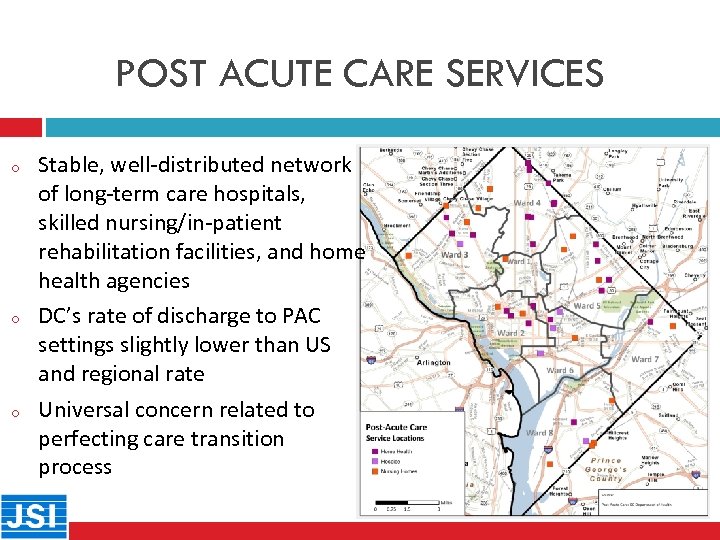
POST ACUTE CARE SERVICES o 24 o o Stable, well-distributed network of long-term care hospitals, skilled nursing/in-patient rehabilitation facilities, and home health agencies DC’s rate of discharge to PAC settings slightly lower than US and regional rate Universal concern related to perfecting care transition process 24
SERVICE CAPACITY CONCERNS o 25 o o There is a need to explore if there are isolated primary care gaps for specific geographic/demographic segments of pop. Lack of primary care providers in some communities that do not take insurance at all or only limited plans (“concierge” medicine) Medical specialty care and oral health services are not welldistributed and there are gaps for low income Medicaid insured, uninsured, and underinsured populations Need for greater integration of behavioral health services in primary care settings Enhance access and/or address barriers to hospital inpatient services in selected wards in DC 25
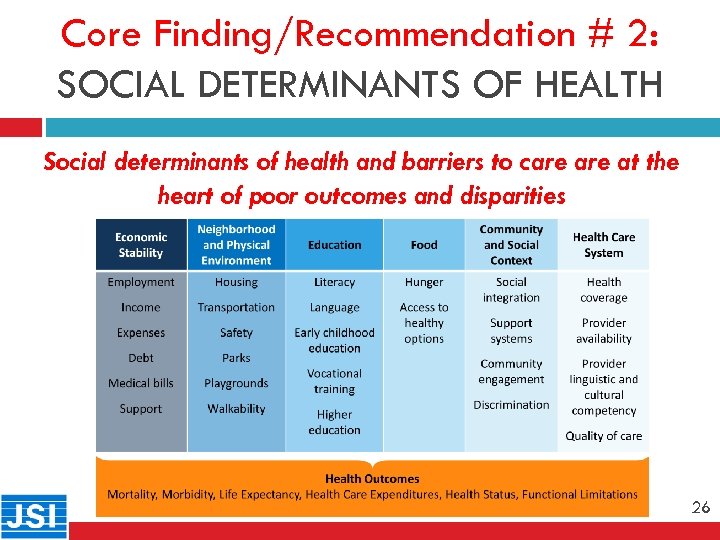
Core Finding/Recommendation # 2: SOCIAL DETERMINANTS OF HEALTH 26 Social determinants of health and barriers to care at the heart of poor outcomes and disparities 26

Core Finding/Recommendation # 2: SOCIAL DETERMINANTS OF HEALTH 27 Social determinants of health and barriers to care at the heart of poor outcomes and disparities 27
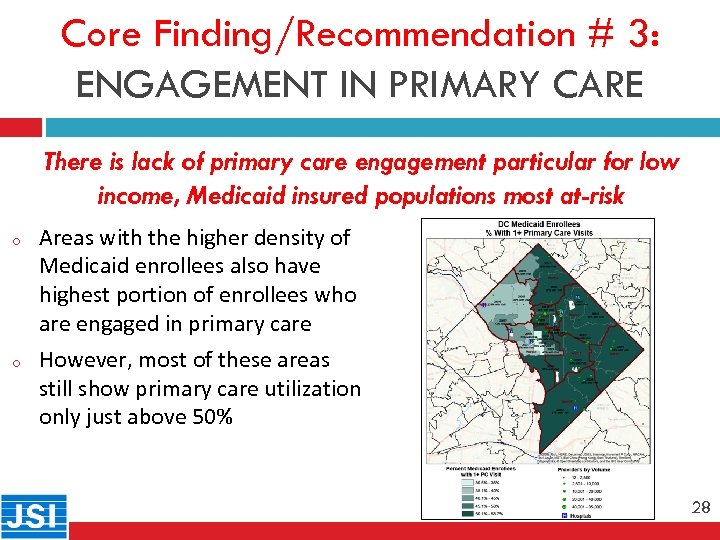
Core Finding/Recommendation # 3: ENGAGEMENT IN PRIMARY CARE 28 o o There is lack of primary care engagement particular for low income, Medicaid insured populations most at-risk Areas with the higher density of Medicaid enrollees also have highest portion of enrollees who are engaged in primary care However, most of these areas still show primary care utilization only just above 50% 28
Core Finding/Recommendation # 3: ENGAGEMENT IN PRIMARY CARE 29 There is lack of primary care engagement particular for low income, Medicaid insured populations most at-risk 29
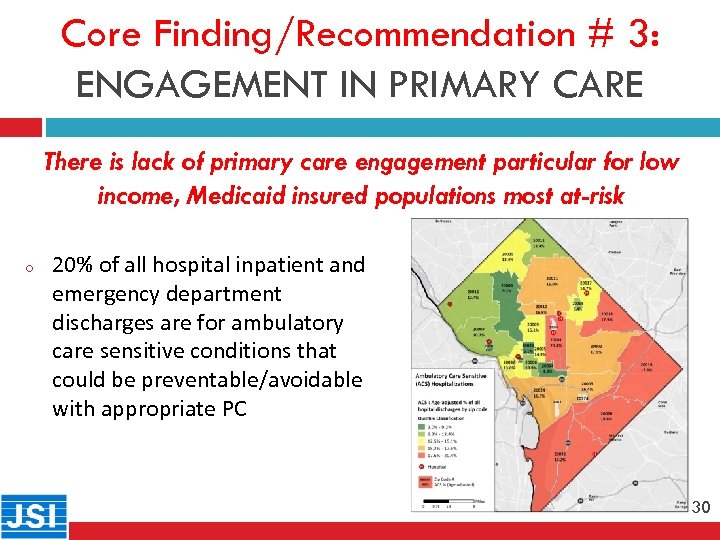
Core Finding/Recommendation # 3: ENGAGEMENT IN PRIMARY CARE 30 o There is lack of primary care engagement particular for low income, Medicaid insured populations most at-risk 20% of all hospital inpatient and emergency department discharges are for ambulatory care sensitive conditions that could be preventable/avoidable with appropriate PC 30
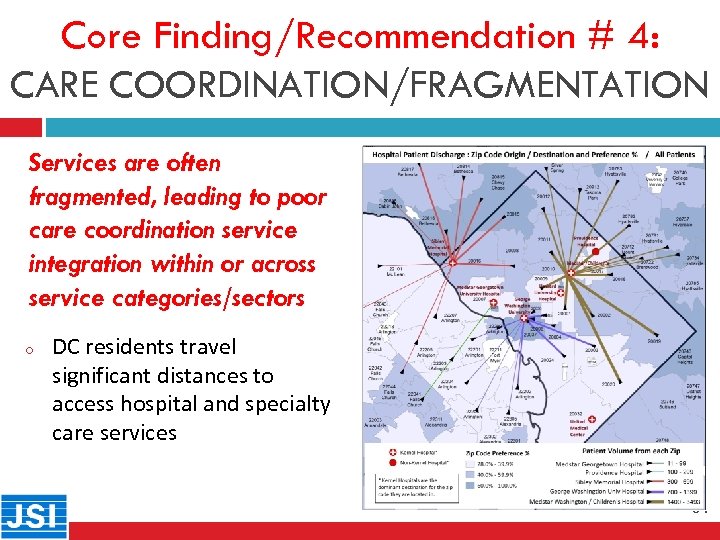
Core Finding/Recommendation # 4: CARE COORDINATION/FRAGMENTATION Services are often 31 fragmented, leading to poor care coordination service integration within or across service categories/sectors o DC residents travel significant distances to access hospital and specialty care services 31
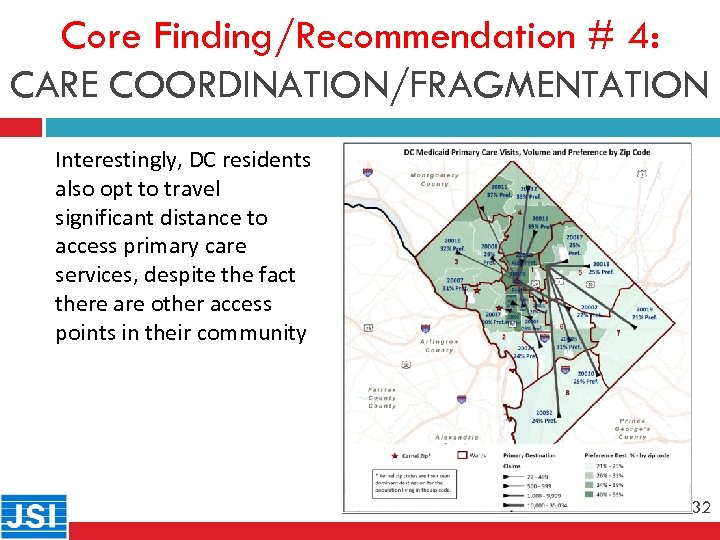
Core Finding/Recommendation # 4: CARE COORDINATION/FRAGMENTATION 32 Interestingly, DC residents also opt to travel significant distance to access primary care services, despite the fact there are other access points in their community 32
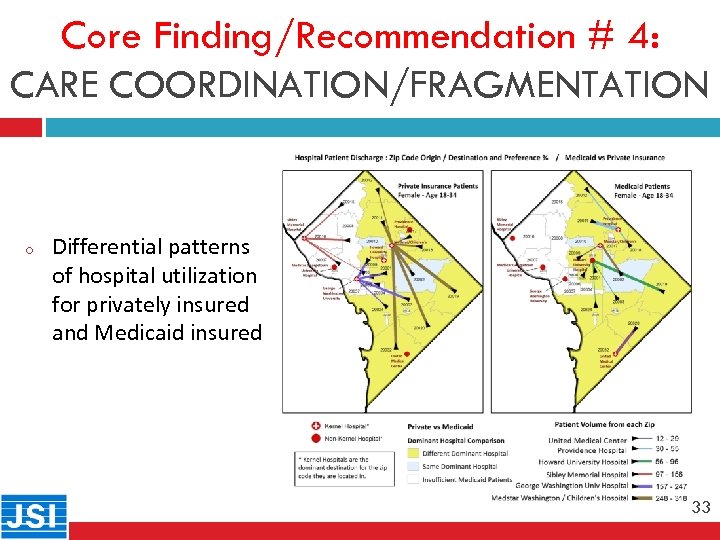
Core Finding/Recommendation # 4: CARE COORDINATION/FRAGMENTATION 33 o Differential patterns of hospital utilization for privately insured and Medicaid insured 33
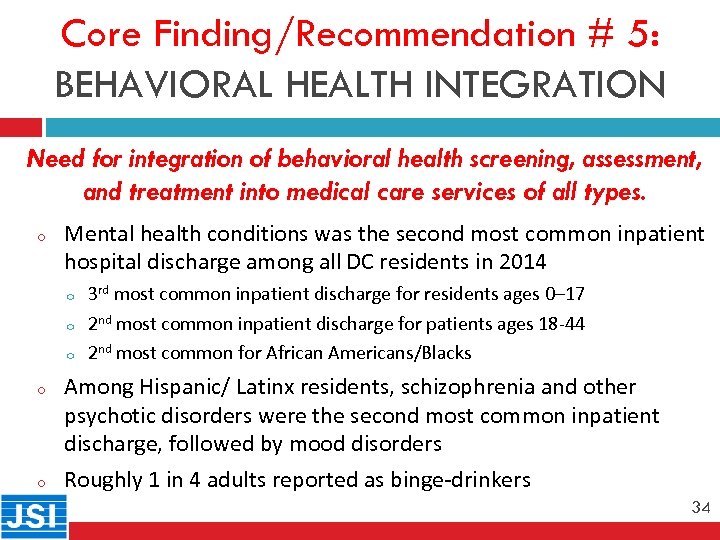
Core Finding/Recommendation # 5: BEHAVIORAL HEALTH INTEGRATION Need for integration of behavioral health screening, assessment, and treatment into medical care services of all types. 34 o Mental health conditions was the second most common inpatient hospital discharge among all DC residents in 2014 o o o 3 rd most common inpatient discharge for residents ages 0– 17 2 nd most common inpatient discharge for patients ages 18 -44 2 nd most common for African Americans/Blacks Among Hispanic/ Latinx residents, schizophrenia and other psychotic disorders were the second most common inpatient discharge, followed by mood disorders Roughly 1 in 4 adults reported as binge-drinkers 34
Core Finding/Recommendation # 5: BEHAVIORAL HEALTH INTEGRATION Need for integration of behavioral health screening, assessment, 35 and treatment into medical care services of all types. o o Mental health and substance abuse services continue to be siloed, leading to barriers to care and poor care coordination Suicide 2 nd most common cause of morbidity for adolescents Need for broad awareness and education campaign regarding impacts, risk factors, signs, and symptoms of leading behavioral health issues (i. e. , depression, anxiety, alcohol, and opioid use) Need for evidence-informed, multi-sector strategies for those with behavioral health issues that promote recovery and independence 35
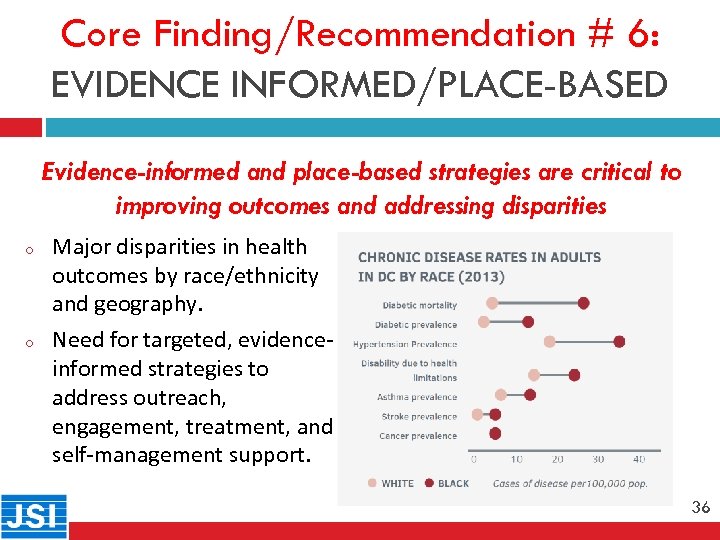
Core Finding/Recommendation # 6: EVIDENCE INFORMED/PLACE-BASED 36 o o Evidence-informed and place-based strategies are critical to improving outcomes and addressing disparities Major disparities in health outcomes by race/ethnicity and geography. Need for targeted, evidenceinformed strategies to address outreach, engagement, treatment, and self-management support. 36
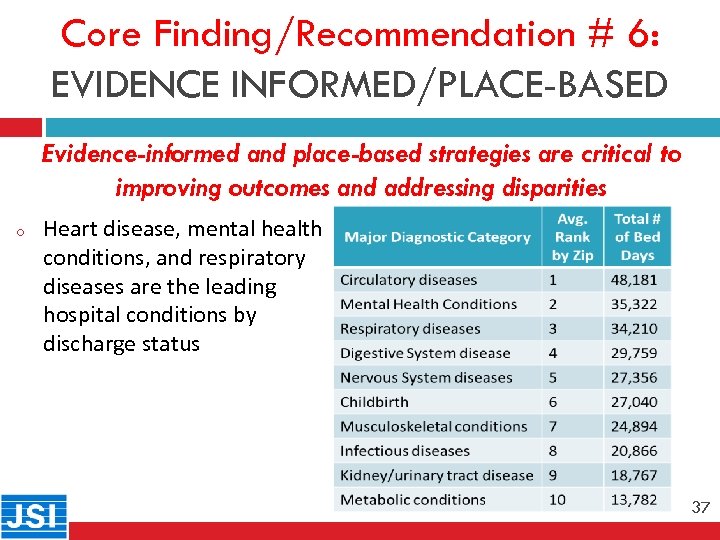
Core Finding/Recommendation # 6: EVIDENCE INFORMED/PLACE-BASED 37 o Evidence-informed and place-based strategies are critical to improving outcomes and addressing disparities Heart disease, mental health conditions, and respiratory diseases are the leading hospital conditions by discharge status 37
Core Finding/Recommendation # 7: HEALTH LITERACY AND EDUCATION Need for comprehensive health literacy, health education, and awareness campaign(s) 38 o o Extremely high rates or chronic disease, behavioral health issues, and many health risk factors combined with tremendous disparities among certain segments of population Many segments of the population struggle with health literacy and lack basic levels of health literacy o o o Hispanics – 41% , American Indians/Alaskan Natives – 25%, African Americans/Blacks – 24%, Asian/Pacific Islanders – 13%, Whites – 9% Older Adults - 29% In DC, more than 20% of individuals in Wards 1, 2, 3, and 4 speak a second language at home. 38
Core Finding/Recommendation # 8: MULTI-SECTOR COLLABORATION 39 Need to develop systems and structures that enhance collaboration and partnership across and within sectors o o o Expand existing relatively robust collaboratives currently in place and promote Increasing understanding that sustainable solutions arise from multiple interacting factors Organizations must actively coordinate actions, share lessons learned, and implement mutually reinforcing activities 39
Core Finding/Recommendation # 9: ALIGNMENT OF STRATEGY/PRIORITIES Alignment of priorities, core strategies, and messaging is critical to promoting cross sector collaboration 40 o o o Sectors, agencies, organizations, service providers, community coalitions across spectrum must align priorities, goals, strategies, and measures Establish multi-sector, District-wide priorities and develop detailed action plans. Drive accountability by tracking and monitoring impact. 40
Health System Structures: Strategic Recommendations 41
Health System Structures: Recommendations o 42 o o o Promote multi-sector collaboration and strategic alignment within and across service systems and sectors. Enhance population health surveillance. Promote health literacy “universal precautions” to improve health outcomes. Enhance health information exchange and technology systems in the District and surrounding region. Support workforce training and capacity building efforts. Explore sustainable financing structures to address SDOH, barriers to access and engagement, care coordination, and service integration. 42

Community Health Improvement: Strategic Recommendations 43

Community Health Improvement: Recommendations and Objectives/Strategies o 44 o o Promote health equity by implementing policies and practices across all sectors that aim to address social determinants of health, improve health outcomes, and reduce disparities. Support initiatives to expand affordable and safe housing. Promote economic prosperity for low-income individuals and families. Expand access to affordable and nutritious foods to promote healthy eating and reduce food insecurity. Promote healthy aging. 44
Questions / Comments 45
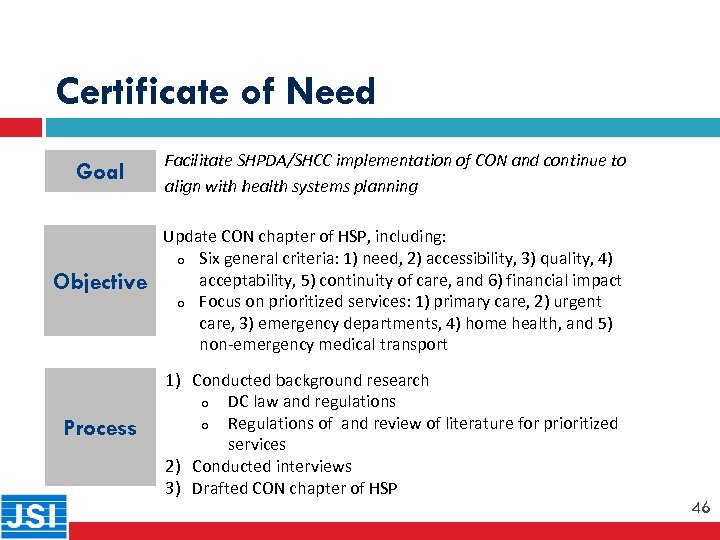
Certificate of Need Goal Facilitate SHPDA/SHCC implementation of CON and continue to align with health systems planning 46 Objective Process Update CON chapter of HSP, including: o Six general criteria: 1) need, 2) accessibility, 3) quality, 4) acceptability, 5) continuity of care, and 6) financial impact o Focus on prioritized services: 1) primary care, 2) urgent care, 3) emergency departments, 4) home health, and 5) non-emergency medical transport 1) Conducted background research o DC law and regulations o Regulations of and review of literature for prioritized services 2) Conducted interviews 3) Drafted CON chapter of HSP 46
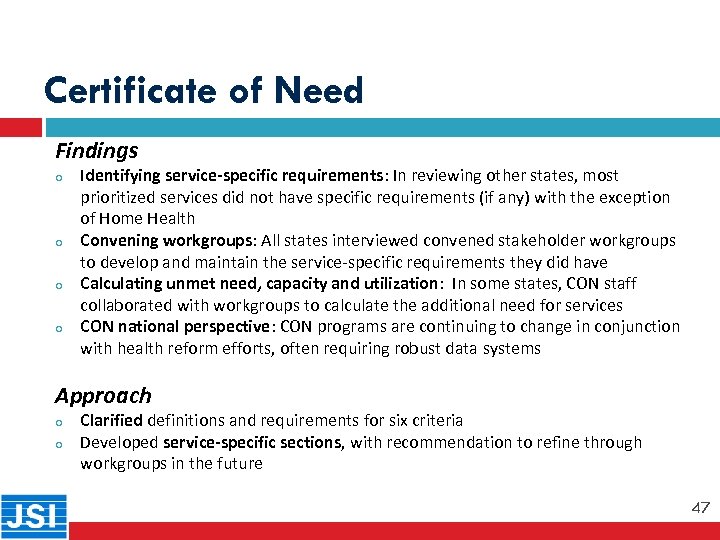
Certificate of Need Findings o 47 o o o Identifying service-specific requirements: In reviewing other states, most prioritized services did not have specific requirements (if any) with the exception of Home Health Convening workgroups: All states interviewed convened stakeholder workgroups to develop and maintain the service-specific requirements they did have Calculating unmet need, capacity and utilization: In some states, CON staff collaborated with workgroups to calculate the additional need for services CON national perspective: CON programs are continuing to change in conjunction with health reform efforts, often requiring robust data systems Approach o o Clarified definitions and requirements for six criteria Developed service-specific sections, with recommendation to refine through workgroups in the future 47
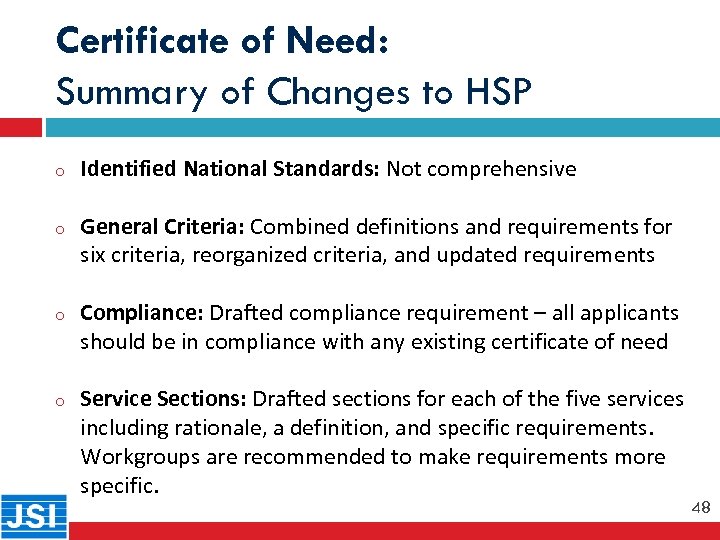
Certificate of Need: Summary of Changes to HSP o Identified National Standards: Not comprehensive o General Criteria: Combined definitions and requirements for six criteria, reorganized criteria, and updated requirements o Compliance: Drafted compliance requirement – all applicants should be in compliance with any existing certificate of need o Service Sections: Drafted sections for each of the five services including rationale, a definition, and specific requirements. Workgroups are recommended to make requirements more specific. 48 48
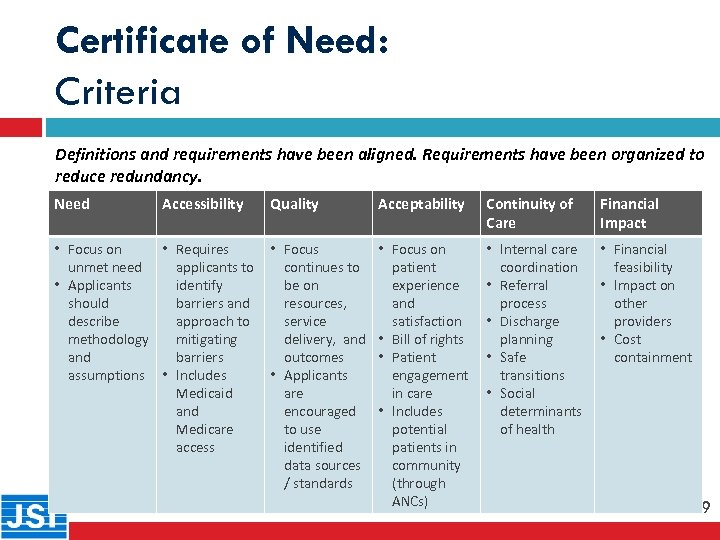
Certificate of Need: Criteria Definitions and requirements have been aligned. Requirements have been organized to reduce redundancy. 49 Need Accessibility • Focus on • Requires unmet need applicants to • Applicants identify should barriers and describe approach to methodology mitigating and barriers assumptions • Includes Medicaid and Medicare access Quality Acceptability Continuity of Care Financial Impact • Focus continues to be on resources, service delivery, and outcomes • Applicants are encouraged to use identified data sources / standards • Focus on patient experience and satisfaction • Bill of rights • Patient engagement in care • Includes potential patients in community (through ANCs) • Internal care coordination • Referral process • Discharge planning • Safe transitions • Social determinants of health • Financial feasibility • Impact on other providers • Cost containment 49

Certificate of Need: Specific Services Current draft chapter requires applications that include the following services to address service-specific requirements: 50 Primary Care Urgent Care Emergency Departments Home Health Medical Transport • Ability to identify and address SDOH needs • Extended hours to improve access • Meeting national standards (e. g. PCMH) • Support access to right care • Integration into the care continuum • Patient satisfaction and convenience • Appropriate staffing and hours • Support health reform efforts (e. g. reduce avoidable ED visits) • Appropriately sized for true need • Systems to address potentially avoidable ED visits (e. g. care manager, evaluation) • Emergency preparedness • Demonstrated track record including CMS HHC Star Rating • Ability to bill across diverse payer base • Quality care transitions continuity of care • Appropriate level of equipment and staffing • Improving care coordination • Emergency preparedness 50
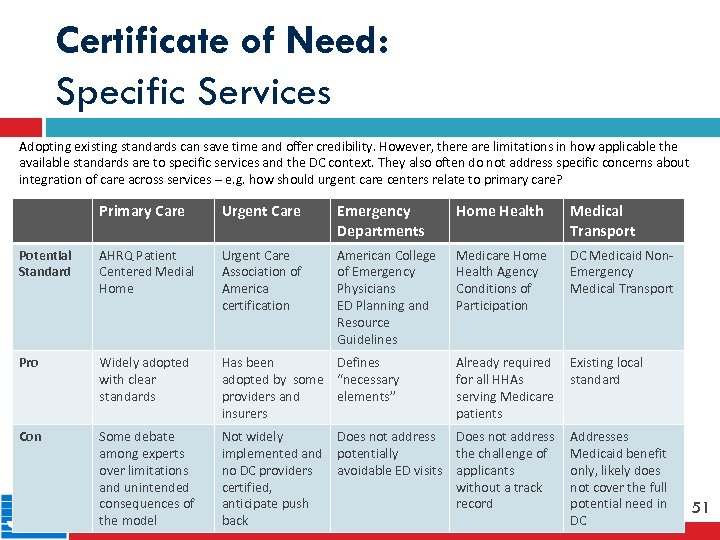
Certificate of Need: Specific Services Adopting existing standards can save time and offer credibility. However, there are limitations in how applicable the available standards are to specific services and the DC context. They also often do not address specific concerns about integration of care across services – e. g. how should urgent care centers relate to primary care? 51 Primary Care Urgent Care Emergency Departments Home Health Medical Transport Potential Standard AHRQ Patient Centered Medial Home Urgent Care Association of America certification American College of Emergency Physicians ED Planning and Resource Guidelines Medicare Home Health Agency Conditions of Participation DC Medicaid Non. Emergency Medical Transport Pro Widely adopted with clear standards Has been Defines adopted by some “necessary providers and elements” insurers Already required for all HHAs serving Medicare patients Existing local standard Con Some debate among experts over limitations and unintended consequences of the model Not widely implemented and no DC providers certified, anticipate push back Does not address potentially the challenge of avoidable ED visits applicants without a track record Addresses Medicaid benefit only, likely does not cover the full potential need in DC 51
Questions / Comments 52
206bd22ecbad6785ad870181885ac7ab.ppt