0c6d21523457068e3dc1d10949f080ba.ppt
- Количество слайдов: 42
Displaced Abomasum Barb Knust Jenny Kohn
Outline: Displaced Abomasum n History and Signalment n Pathophysiology n Diagnosis n Clinical signs, clin path, R/O’s n Treatment n Non-surgical n Surgical (4 approaches) n Ancillary care (Fluids, Abx, …) n Risk Factors for LDA
Displaced Abomasums n DA’s, LDA’s, RTA’s n Adult lactating dairy n Production problem n Herd problem [related to nutrition] n Majority of DA’s have concurrent diseases
History and Signalment of DA n Age: older lactating dairy cattle n Timing: 80% occur during first month after parturition n Nutrition: n Dry cow rations: +DCAD / inadeq efv fiber n Fresh cow: excess NSC’s / inadeq efv fiber n. Concurrent disease: 40% of DA’s have retained placenta, mastitis, or metritis

Normal location of abomasum
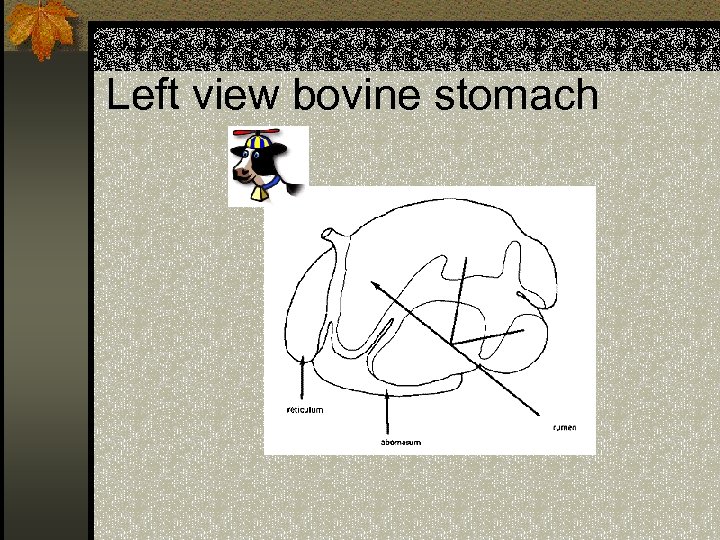
Left view bovine stomach
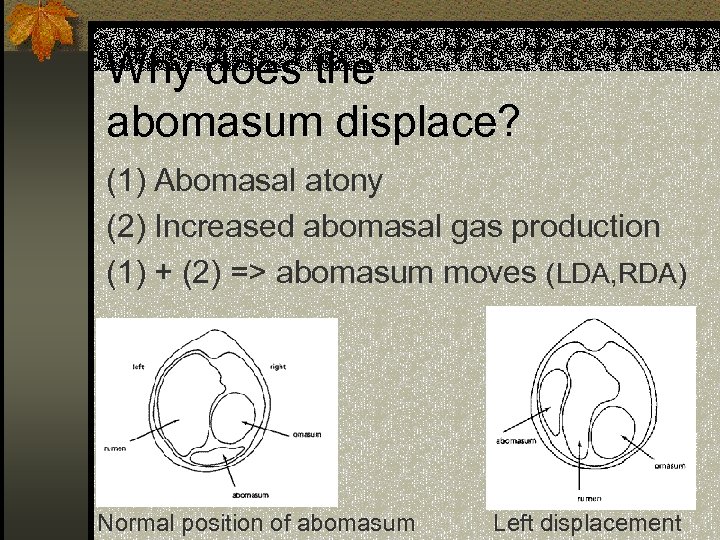
Why does the abomasum displace? (1) Abomasal atony (2) Increased abomasal gas production (1) + (2) => abomasum moves (LDA, RDA) Normal position of abomasum Left displacement
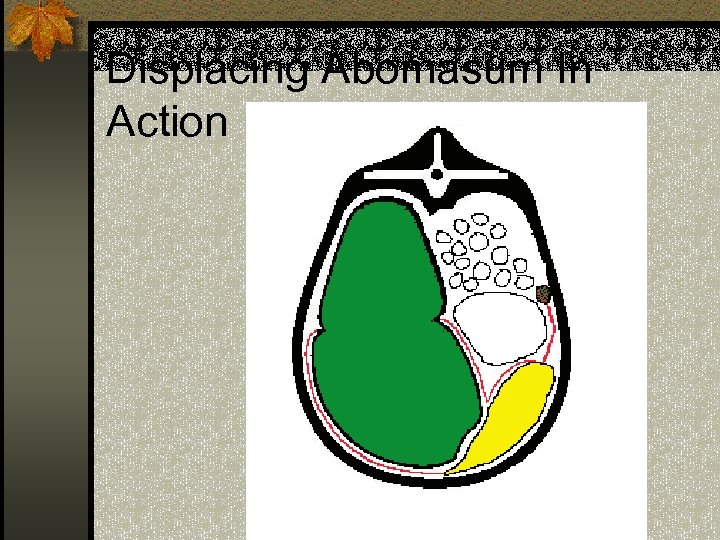
Displacing Abomasum In Action
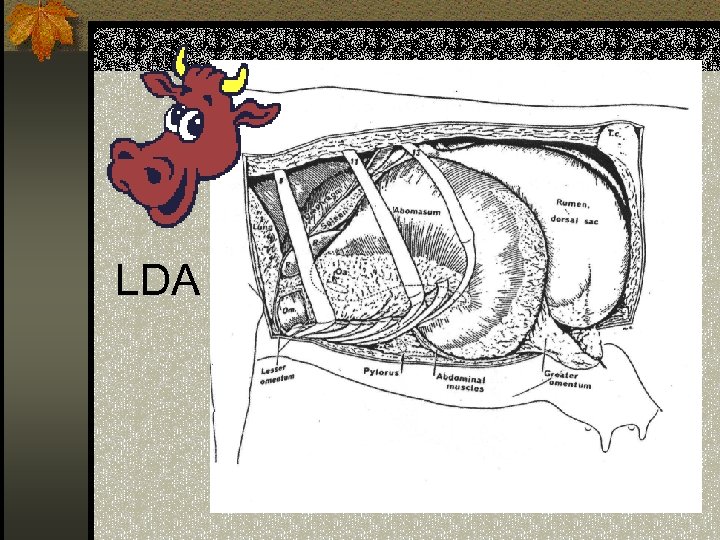
LDA
![Why does abomasal atony occur? n Hypocalcaemia due to n +DCAD, [Ca]blood, mastitis, - Why does abomasal atony occur? n Hypocalcaemia due to n +DCAD, [Ca]blood, mastitis, -](https://present5.com/presentation/0c6d21523457068e3dc1d10949f080ba/image-10.jpg)
Why does abomasal atony occur? n Hypocalcaemia due to n +DCAD, [Ca]blood, mastitis, - E balance n 7 times more likely to develop DA’s n Inadequate effective fiber n VFA’s reach abomasum => abomasal hypomotility => HCl refluxes back into rumen => systemic metabolic alkalosis n Endotoxemia n Released during Gm – sepsis (mastitis/metritis)
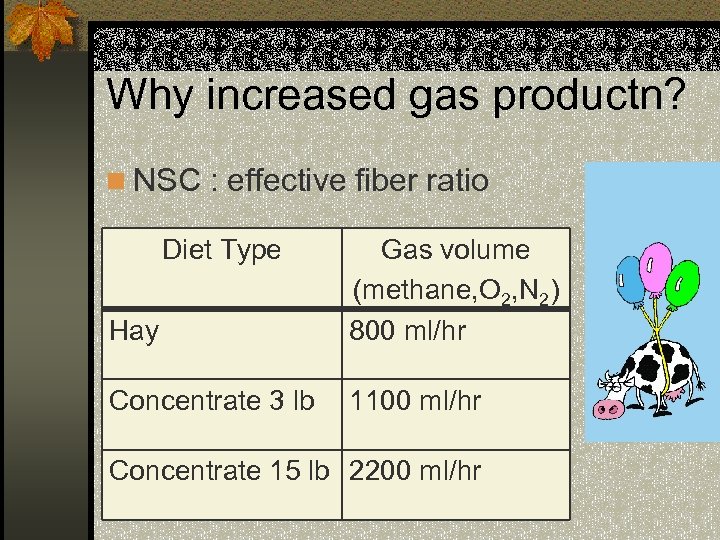
Why increased gas productn? n NSC : effective fiber ratio Diet Type Hay Gas volume (methane, O 2, N 2) 800 ml/hr Concentrate 3 lb 1100 ml/hr Concentrate 15 lb 2200 ml/hr
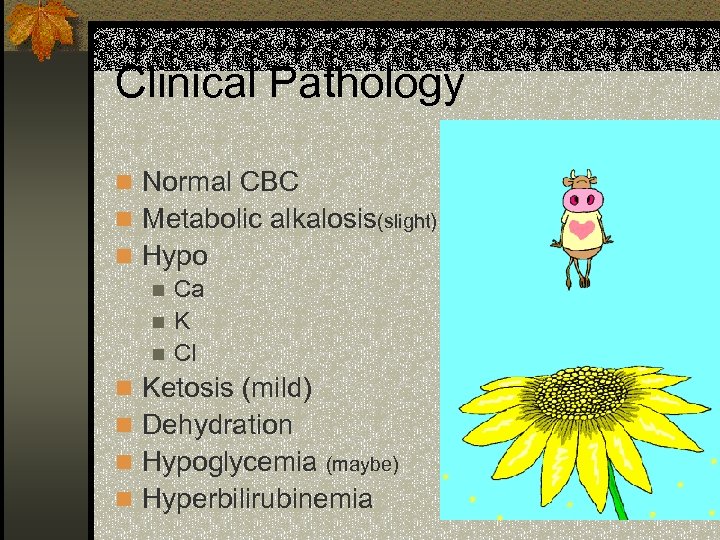
Clinical Pathology n Normal CBC n Metabolic alkalosis(slight) n Hypo n Ca n. K n Cl n Ketosis (mild) n Dehydration n Hypoglycemia (maybe) n Hyperbilirubinemia
Clinical Signs of DA’s n Normal TPR (most cases) n Partial anorexia (“off feed”) n Hypogalactia (“down in milk” ~ 5 -10 lb/day) n Depression (ADR) n Secondary ketosis n mild to moderate n Scant stool firm/loose n undigested particles n
Clinical Signs (continued) n Paralumbar fossa: n “slab-sided” abdomen n Visualize / Palpate PLF n Rectal palpation (can’t) n Mild colic n Mild hypocalcemia n Hypotonic rumen n Cold ears, widely dilated pupils
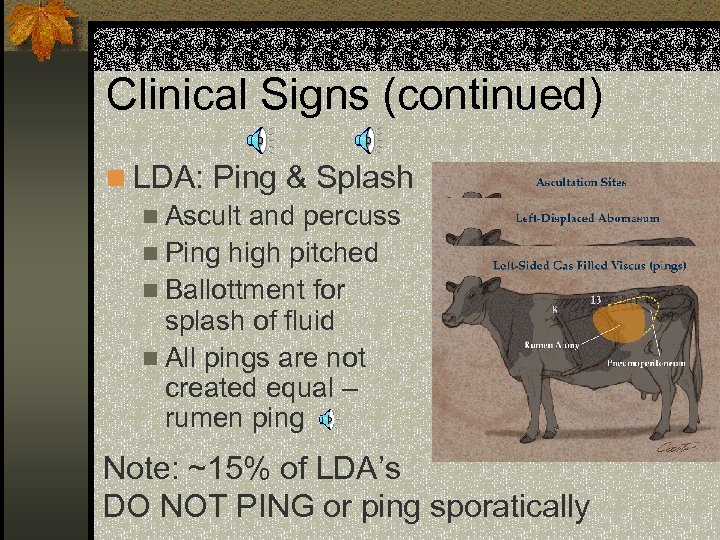
Clinical Signs (continued) n LDA: Ping & Splash n Ascult and percuss n Ping high pitched n Ballottment for splash of fluid n All pings are not created equal – rumen ping Note: ~15% of LDA’s DO NOT PING or ping sporatically
Differential Diagnosis n LDA R/O’s n 1° ketosis (non-pinging LDA) n Rumen ping n RDA R/O’s n 1° ketosis (non-pinging RDA) n Other Right-sided pings: n Uterus, cecum, peritoneum, colon, rectum n “off feed” ping
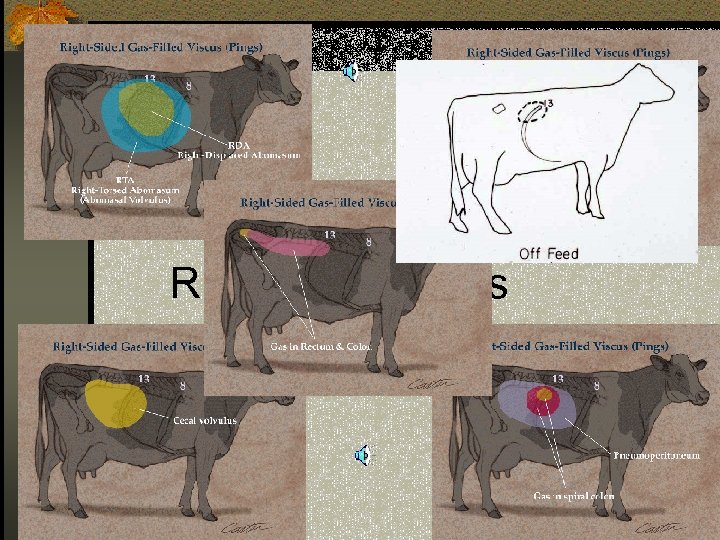
Right-sided pings
Treatment of Displaced Abomasum
Therapeutic Goals n Return Abomasum to proper position n Create a permanent attachment n Correct electrolyte, acid-base, & hydration deficits n Treat other concurrent diseases
Therapeutic Choices n Upper 25% of herd: “cut ‘em” n Middle 50%: “tack ‘em” n Lower 25%: “cull ‘em”
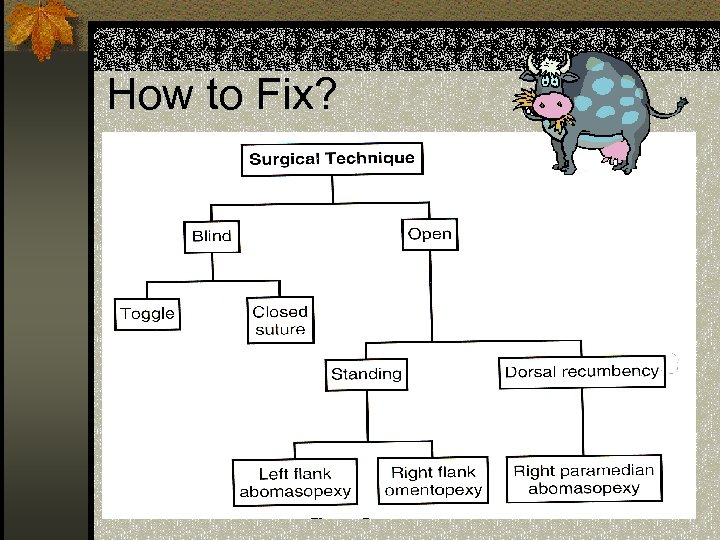
How to Fix?
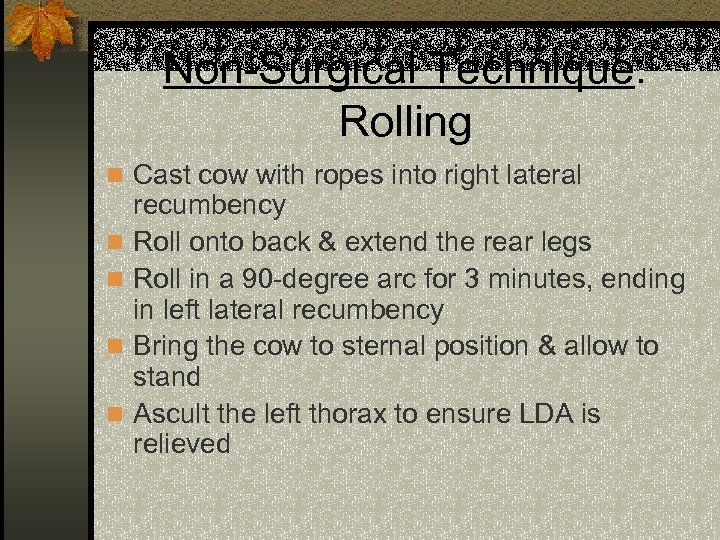
Non-Surgical Technique: Rolling n Cast cow with ropes into right lateral n n recumbency Roll onto back & extend the rear legs Roll in a 90 -degree arc for 3 minutes, ending in left lateral recumbency Bring the cow to sternal position & allow to stand Ascult the left thorax to ensure LDA is relieved
Rolling Technique n Advantages n Quick & easy technique n No invasive surgery n DISADVANTAGES n >50% redisplace n If RDA or RTA are present, can exacerbate problems
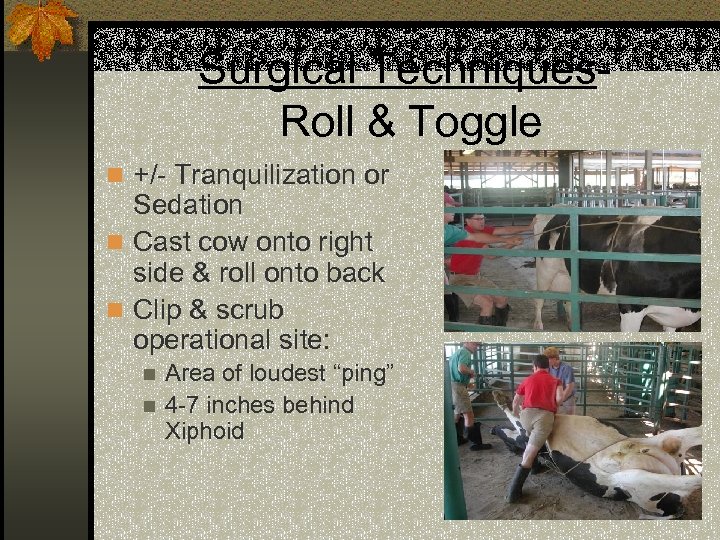
Surgical Techniques. Roll & Toggle n +/- Tranquilization or Sedation n Cast cow onto right side & roll onto back n Clip & scrub operational site: Area of loudest “ping” n 4 -7 inches behind Xiphoid n
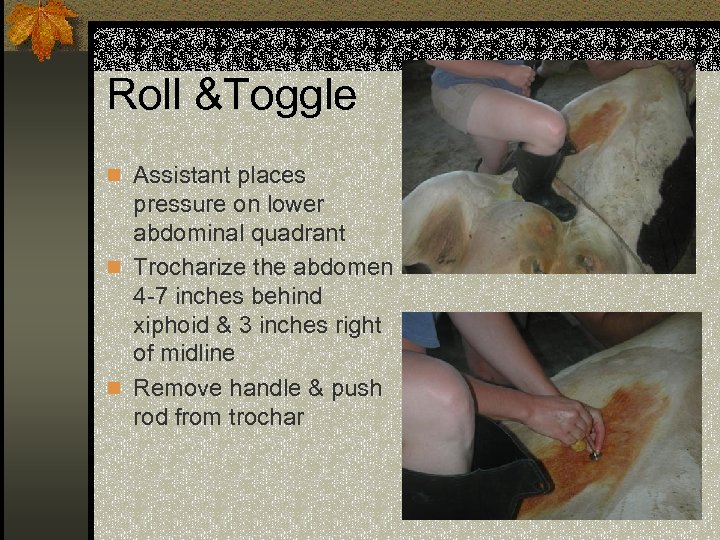
Roll &Toggle n Assistant places pressure on lower abdominal quadrant n Trocharize the abdomen 4 -7 inches behind xiphoid & 3 inches right of midline n Remove handle & push rod from trochar
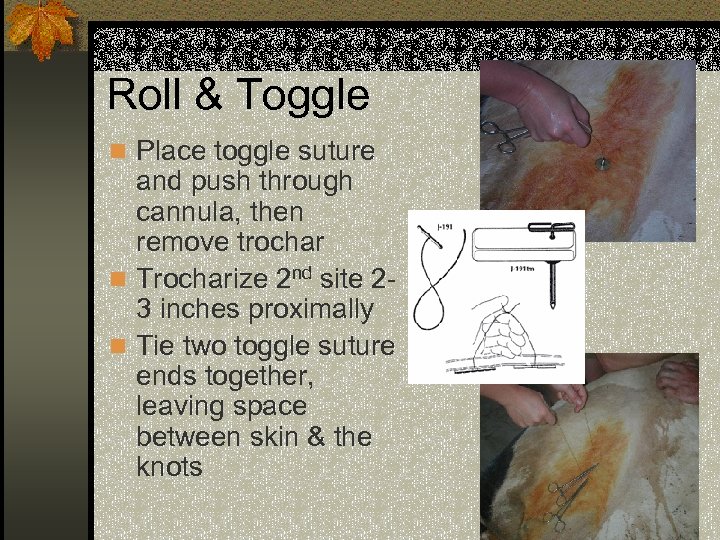
Roll & Toggle n Place toggle suture and push through cannula, then remove trochar n Trocharize 2 nd site 2 inches proximally 3 n Tie two toggle suture ends together, leaving space between skin & the knots
Roll & Toggle n Advantages: n Simple, quick, inexpensive n Minimally invasive n High success rate (60 -80%) n Disadvantages: n Blind technique- cannot see abomasum n Dorsal recumbent position
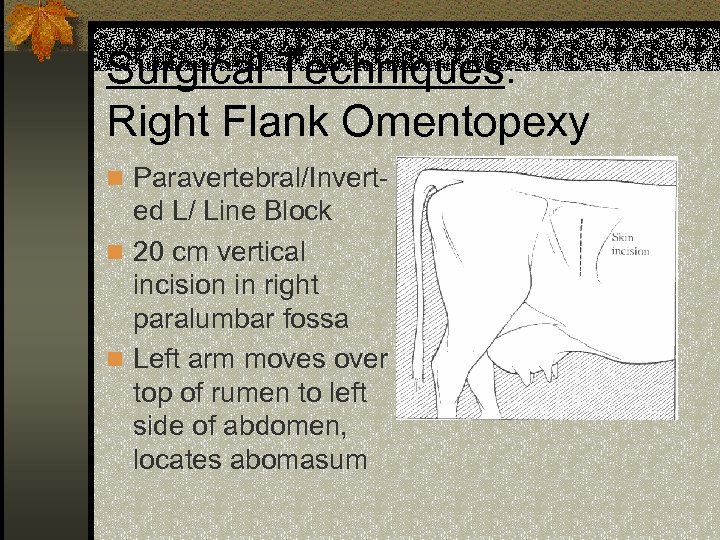
Surgical Techniques: Right Flank Omentopexy n Paravertebral/Invert- ed L/ Line Block n 20 cm vertical incision in right paralumbar fossa n Left arm moves over top of rumen to left side of abdomen, locates abomasum
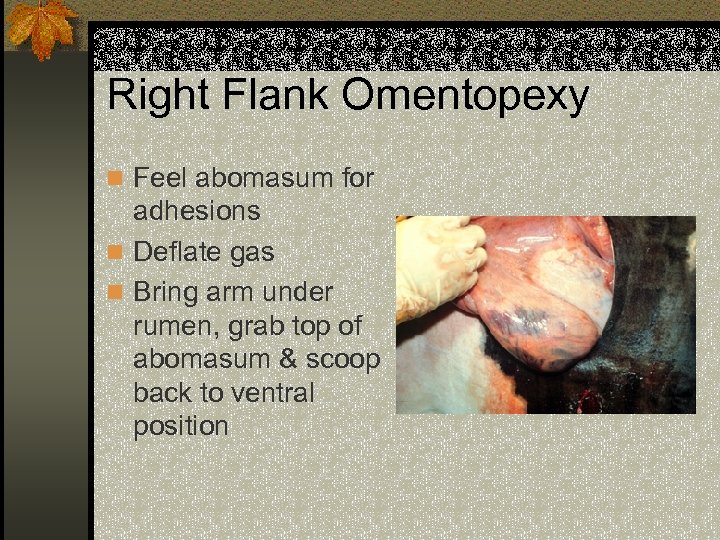
Right Flank Omentopexy n Feel abomasum for adhesions n Deflate gas n Bring arm under rumen, grab top of abomasum & scoop back to ventral position
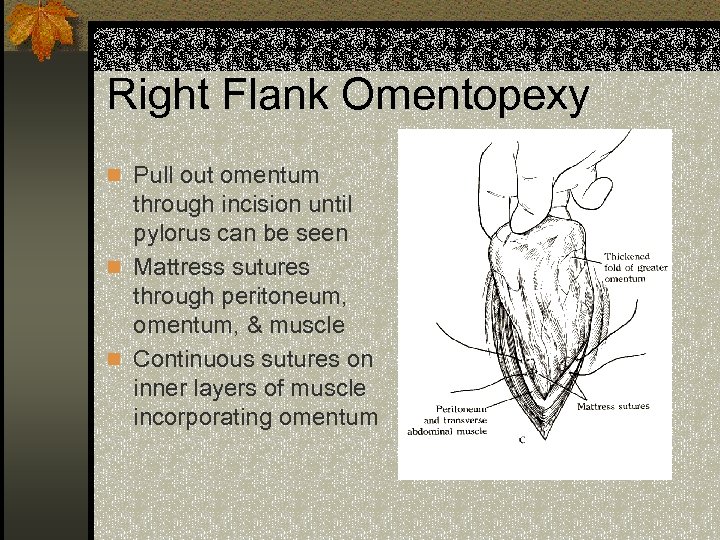
Right Flank Omentopexy n Pull out omentum through incision until pylorus can be seen n Mattress sutures through peritoneum, omentum, & muscle n Continuous sutures on inner layers of muscle incorporating omentum
Right Flank Omentopexy n Advantages: n High success rate in experienced surgeons n Standing procedure n Can perform exploratory n Disadvantages: n Omentum can tear & redisplacement n Cannot see abomasum to evaluate n Need long arms to reach across abdomen!
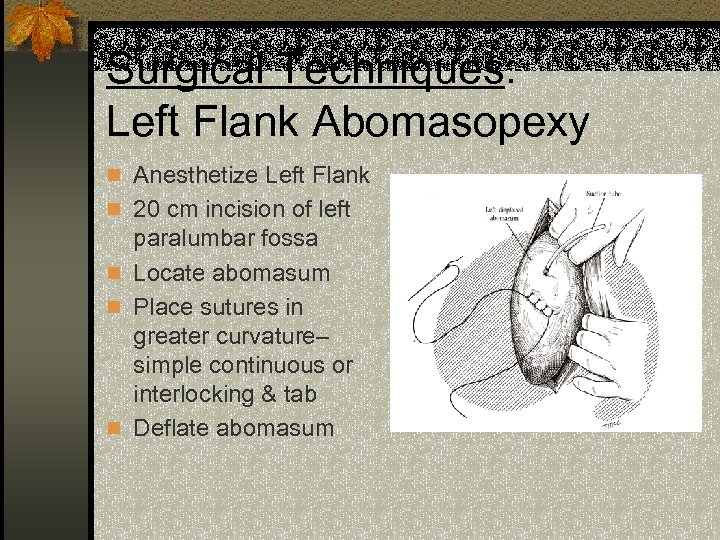
Surgical Techniques: Left Flank Abomasopexy n Anesthetize Left Flank n 20 cm incision of left paralumbar fossa n Locate abomasum n Place sutures in greater curvature– simple continuous or interlocking & tab n Deflate abomasum
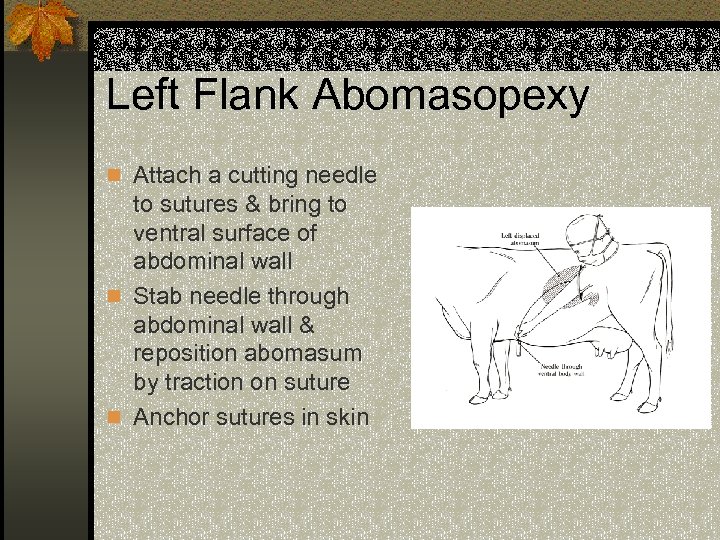
Left Flank Abomasopexy n Attach a cutting needle to sutures & bring to ventral surface of abdominal wall n Stab needle through abdominal wall & reposition abomasum by traction on suture n Anchor sutures in skin
Left Flank Abomasopexy n Advantages n Direct fixation of abomasum to body wall n Standing surgery n Can see abomasum n Disadvantages n Not as secure of anchorage as ventral paramedian approach
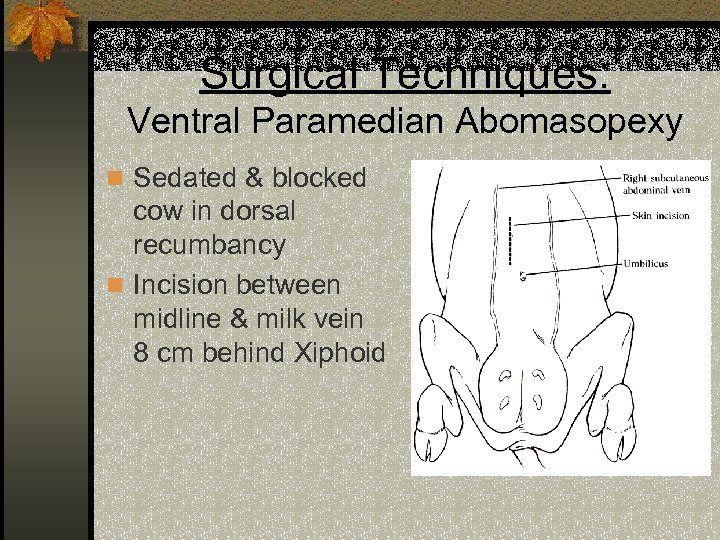
Surgical Techniques: Ventral Paramedian Abomasopexy n Sedated & blocked cow in dorsal recumbancy n Incision between midline & milk vein 8 cm behind Xiphoid
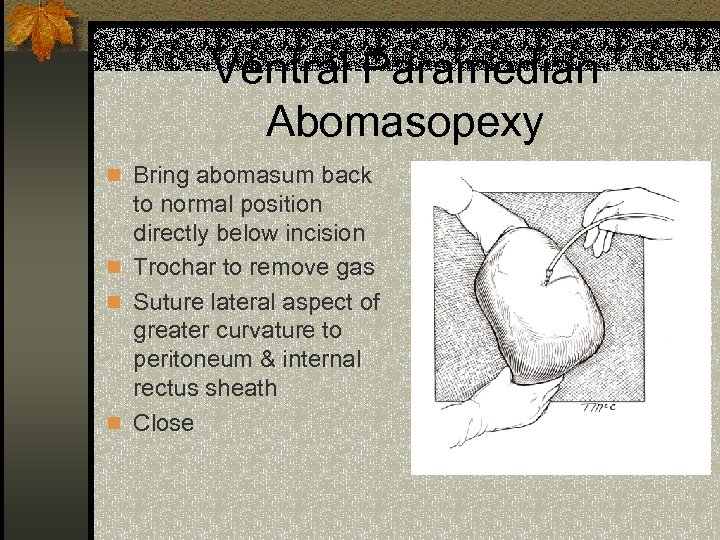
Ventral Paramedian Abomasopexy n Bring abomasum back to normal position directly below incision n Trochar to remove gas n Suture lateral aspect of greater curvature to peritoneum & internal rectus sheath n Close
Ventral Paramedian Abomasopexy n Advantages n Very secure fixation with good adhesion n Can visualize abomasum n Casting usually repositions abomasum n Disadvantages n Stressful to cast the cow, danger of regurgitation in dorsal recumbency n Rest of abdomen cannot be explored
Replacement Fluids n Isotonic Saline, Lactated Ringer’s IV to replace deficit n K, Ca salts as needed to correct electrolyte imbalances n Free-choice oral fluids with Na. Cl, KCl
Antibiotics? ? ? n The Three T’s: n Time- how long was the procedure? Time n Trash- how clean was the surgical site? Trash n Trauma- are tissues damaged? Trauma n Also evaluate for other concurrent problems, cost, withdrawal times, route, and ability of agent to reach the tissue
Risk Factors for LDA n High-production Dairy Cows High concentrate, low roughage diet n Large body size n Limited exercise n n Post-partum n Abomasal Atony
Questions? ? ?
References n Dr. Kent Ames n Web references: http: //www. ldatogglesuture. com/ n http: //www. vet. ohiostate. edu/docs/Clin. Sci/bovine/prevmed/abomasum. htm n http: //www. ianr. unl. edu/pubs/dairy/g 1201. htm n n http: //muextension. missouri. edu/xplor/agguides/pests/g 0770 1. htm n Books: Noordsy, John, L. Food Animal Surgery, 3 rd ed. n Oehme, Frederick W. Textbook of Large Animal Surgery, 2 nd ed. n Smith, Bradford P. Large Animal Internal Medicine. n Turner, Mc. Ilwraith. Techniques in Large Animal Surgery, 2 nd ed. n
0c6d21523457068e3dc1d10949f080ba.ppt