Orbit. Lacrimal syst. Lids..pptx
- Количество слайдов: 176
 DISORDERS OF THE LACRIMAL SYSTEM
DISORDERS OF THE LACRIMAL SYSTEM
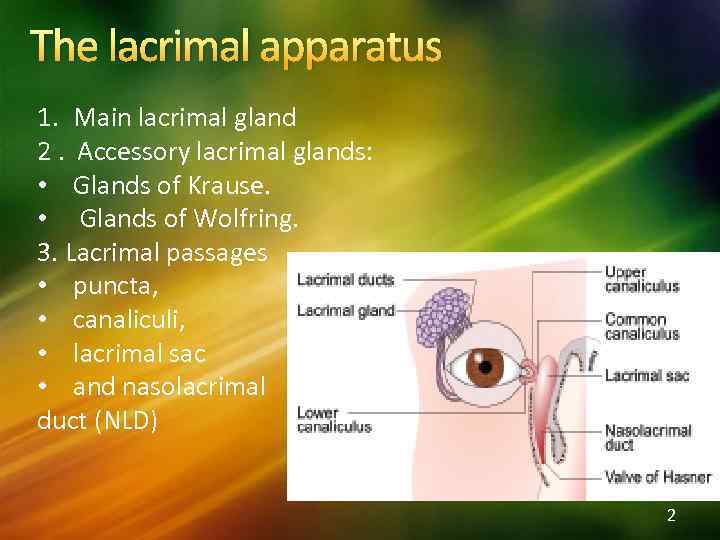 The lacrimal apparatus 1. Main lacrimal gland 2. Accessory lacrimal glands: • Glands of Krause. • Glands of Wolfring. 3. Lacrimal passages • puncta, • canaliculi, • lacrimal sac • and nasolacrimal duct (NLD) 2
The lacrimal apparatus 1. Main lacrimal gland 2. Accessory lacrimal glands: • Glands of Krause. • Glands of Wolfring. 3. Lacrimal passages • puncta, • canaliculi, • lacrimal sac • and nasolacrimal duct (NLD) 2
 Elimination of tears • going in lower fornix and then via lacus lacrimalis in the inner canthus. • lacrimal passages (punctum and canaliculi ) into the sac and nasolacrimal duct into the nasal cavity 3
Elimination of tears • going in lower fornix and then via lacus lacrimalis in the inner canthus. • lacrimal passages (punctum and canaliculi ) into the sac and nasolacrimal duct into the nasal cavity 3
 Lacrimal System Disorders Tear film disorders (all phases) The dry eye The wet eye Drainage obstruction Lacrimal gland inflammation Lacrimal gland tumours Lacrimal sac tumours 4
Lacrimal System Disorders Tear film disorders (all phases) The dry eye The wet eye Drainage obstruction Lacrimal gland inflammation Lacrimal gland tumours Lacrimal sac tumours 4
 The dry eye Aqueous phase deficiency Symptoms Redness Burning sensation Gritty sensation Epiphora 5
The dry eye Aqueous phase deficiency Symptoms Redness Burning sensation Gritty sensation Epiphora 5
 Tear film tests. Schirmer-test. Normal values of Schirmer- test are more than 15 mm (after 5 minutes). Values of 5 -10 mm are suggestive of moderate to mild keratoconjunctivitis sicca (KCS) and less than 5 mm of severe KCS. 6
Tear film tests. Schirmer-test. Normal values of Schirmer- test are more than 15 mm (after 5 minutes). Values of 5 -10 mm are suggestive of moderate to mild keratoconjunctivitis sicca (KCS) and less than 5 mm of severe KCS. 6
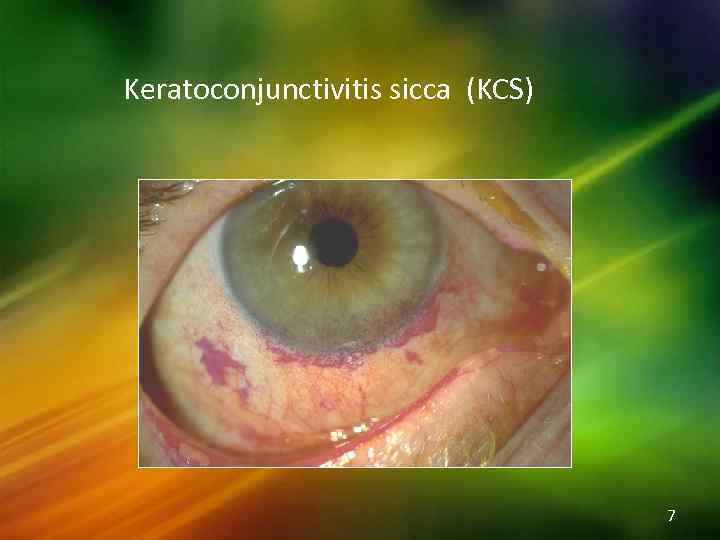 Keratoconjunctivitis sicca (KCS) 7
Keratoconjunctivitis sicca (KCS) 7
 Causes of aqueous deficiency Idiopathic/age related Sjögren’s syndrome Inflammatory or infiltrative lesions e. g. Lymphoma, TB, sarcoidosis Congenital/iatrogenic absence of lacrimal gland Antihistamines ; -blockers; phenothiazines; CN V defect (sensory arc), CN VII defect (motor arc) 8
Causes of aqueous deficiency Idiopathic/age related Sjögren’s syndrome Inflammatory or infiltrative lesions e. g. Lymphoma, TB, sarcoidosis Congenital/iatrogenic absence of lacrimal gland Antihistamines ; -blockers; phenothiazines; CN V defect (sensory arc), CN VII defect (motor arc) 8
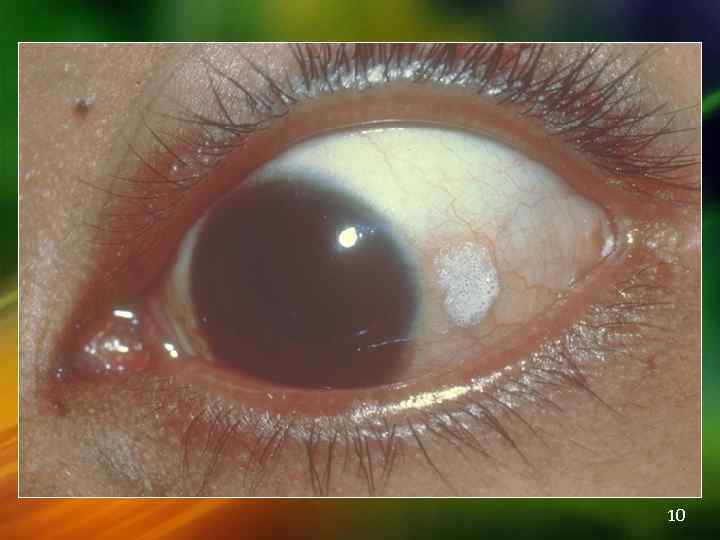
 Mucin Deficiency Signs The dry eye interpalpebral conjunctival foamy patches associated with severe vitamin A & xerophthalmia Causes Vitamin A deficiency Cicatrising disease: trachoma, cicatricial pemphigoid, chemical burns 9
Mucin Deficiency Signs The dry eye interpalpebral conjunctival foamy patches associated with severe vitamin A & xerophthalmia Causes Vitamin A deficiency Cicatrising disease: trachoma, cicatricial pemphigoid, chemical burns 9
 10
10
 Oily Layer Abnormalities Meibomianitis Blepharitis, often staphylococcal & compounding aqueous deficiency 11
Oily Layer Abnormalities Meibomianitis Blepharitis, often staphylococcal & compounding aqueous deficiency 11
 Management of Dry Eyes Artificial tears - if used very frequently Lid toilet and compresses with occasional use of topical antibiotics Vitamin A supplements in xerophthalmia (topically is experimental) Stop appointment medication Surgery to lid deformities/punctal occlusion 12
Management of Dry Eyes Artificial tears - if used very frequently Lid toilet and compresses with occasional use of topical antibiotics Vitamin A supplements in xerophthalmia (topically is experimental) Stop appointment medication Surgery to lid deformities/punctal occlusion 12
 THE WATERING EYE(Epiphora) Causes Exclude eye disease Allergic/infective/irritative conjunctivitis Trichiasis, distichiasis Corneal disease Lacrimal pump failure (e. g. CN VII palsy) Ectropion Lacrimal drainage system obstruction Hypersecretion 13
THE WATERING EYE(Epiphora) Causes Exclude eye disease Allergic/infective/irritative conjunctivitis Trichiasis, distichiasis Corneal disease Lacrimal pump failure (e. g. CN VII palsy) Ectropion Lacrimal drainage system obstruction Hypersecretion 13
 Epiphora Specific tests of patency Fluorescein disappearance test Jones’ test - staining of nasal swab after instillation of fluorescein into fornix Syringing & probing (diagnostic & therapeutic) CT & MRI scans, radionucleotide scans Lacrimal Drainage System Obstruction 14
Epiphora Specific tests of patency Fluorescein disappearance test Jones’ test - staining of nasal swab after instillation of fluorescein into fornix Syringing & probing (diagnostic & therapeutic) CT & MRI scans, radionucleotide scans Lacrimal Drainage System Obstruction 14
 Lacrimal Drainage System Obstruction Causes: Congenital Absence/atresia of the canaliculi &/or puncta Incomplete opening of the nasolacrimal duct Craniofacial anomalies Senile: punctal stenosis or associated with chronic infection, Ectropion or Conjunctival cicatrisation 15
Lacrimal Drainage System Obstruction Causes: Congenital Absence/atresia of the canaliculi &/or puncta Incomplete opening of the nasolacrimal duct Craniofacial anomalies Senile: punctal stenosis or associated with chronic infection, Ectropion or Conjunctival cicatrisation 15
 Causes Trauma (physical or radiation) Inflammation (sarcoid, Wegener’s) Drug induced (pilocarpine, adrenaline et al) Infection Acute or chronic dacryocystitis Canaliculitis Sinusitis Lacrimal sac tumours 16
Causes Trauma (physical or radiation) Inflammation (sarcoid, Wegener’s) Drug induced (pilocarpine, adrenaline et al) Infection Acute or chronic dacryocystitis Canaliculitis Sinusitis Lacrimal sac tumours 16
 Lacrimal Drainage System Obstruction Treatment depends on site of obstruction Puncta may be dilated (± snips) Lid malposition correction Recanalisation operations Treat infectious causes (e. g. canaliculitis, dacryocystitis) Recurrent dacryocystitis requires DCR Probing atretic nasolacrimal ducts DCR = mainstay of treatment of NLD obstruction 17
Lacrimal Drainage System Obstruction Treatment depends on site of obstruction Puncta may be dilated (± snips) Lid malposition correction Recanalisation operations Treat infectious causes (e. g. canaliculitis, dacryocystitis) Recurrent dacryocystitis requires DCR Probing atretic nasolacrimal ducts DCR = mainstay of treatment of NLD obstruction 17
 Lacrimal Gland Inflammation Viral dacroadenitis e. g mumps, glandular fever Acute bacterial dacryoadenitis Chronic bacterial e. g. TB, syphilis Inflammatory conditions e. g. Sjögren’s, sarcoidosis, Wegener’s Reactive lymphoid hyperplasia, lymphoma 18
Lacrimal Gland Inflammation Viral dacroadenitis e. g mumps, glandular fever Acute bacterial dacryoadenitis Chronic bacterial e. g. TB, syphilis Inflammatory conditions e. g. Sjögren’s, sarcoidosis, Wegener’s Reactive lymphoid hyperplasia, lymphoma 18
 INFECTIONS OF LACRIMAL PASSAGES 1. Congenital nasolacrimal duct obstruction 2. Congenital dacryocele 3. Chronic canaliculitis 4. Dacryocystitis Acute • Chronic •
INFECTIONS OF LACRIMAL PASSAGES 1. Congenital nasolacrimal duct obstruction 2. Congenital dacryocele 3. Chronic canaliculitis 4. Dacryocystitis Acute • Chronic •
 Congenital nasolacrimal duct obstruction • On pressure reflux of purulent material from punctum Epiphora and matting Infrequently acute dacryocystitis
Congenital nasolacrimal duct obstruction • On pressure reflux of purulent material from punctum Epiphora and matting Infrequently acute dacryocystitis
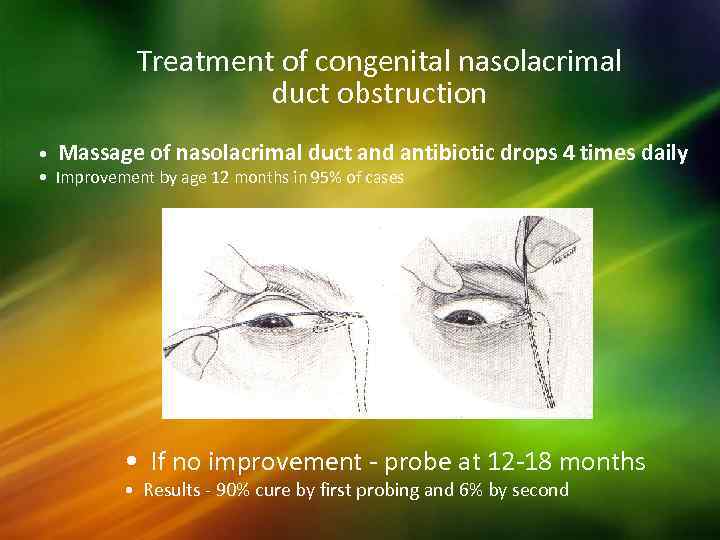 Treatment of congenital nasolacrimal duct obstruction • Massage of nasolacrimal duct and antibiotic drops 4 times daily • Improvement by age 12 months in 95% of cases • If no improvement - probe at 12 -18 months • Results - 90% cure by first probing and 6% by second
Treatment of congenital nasolacrimal duct obstruction • Massage of nasolacrimal duct and antibiotic drops 4 times daily • Improvement by age 12 months in 95% of cases • If no improvement - probe at 12 -18 months • Results - 90% cure by first probing and 6% by second
 Congenital dacryocele Distension of lacrimal sac by trapped amniotic fluid (amniontocele) • Bluish cystic swelling at or below medial canthus • May become secondarily infected Treatment • Initially massage • Probing
Congenital dacryocele Distension of lacrimal sac by trapped amniotic fluid (amniontocele) • Bluish cystic swelling at or below medial canthus • May become secondarily infected Treatment • Initially massage • Probing
 Chronic canaliculitis Frequently caused by Actinomyces (Streptothrix sp. ) • Unilateral epiphora and chronic mucopurulent discharge • Oedema of canaliculus and pouting punctum Expressed concretions consisting of sulphur granules Treatment - simple curettage or canaliculotomy
Chronic canaliculitis Frequently caused by Actinomyces (Streptothrix sp. ) • Unilateral epiphora and chronic mucopurulent discharge • Oedema of canaliculus and pouting punctum Expressed concretions consisting of sulphur granules Treatment - simple curettage or canaliculotomy
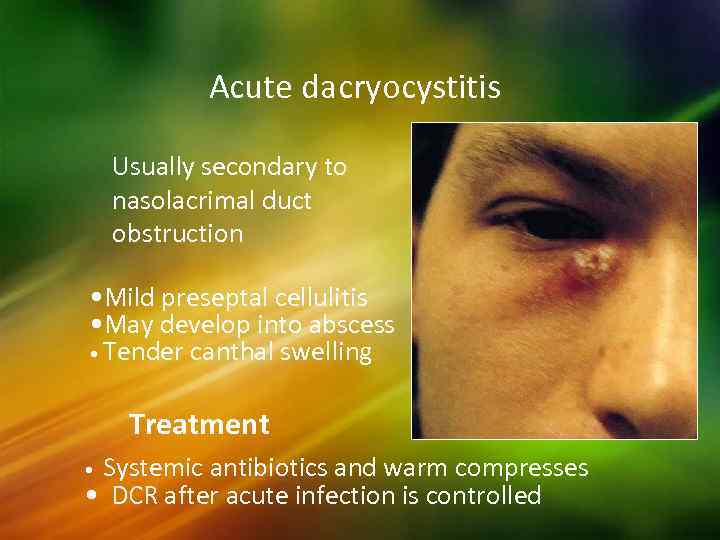 Acute dacryocystitis Usually secondary to nasolacrimal duct obstruction • Mild preseptal cellulitis • May develop into abscess • Tender canthal swelling Treatment Systemic antibiotics and warm compresses • DCR after acute infection is controlled •
Acute dacryocystitis Usually secondary to nasolacrimal duct obstruction • Mild preseptal cellulitis • May develop into abscess • Tender canthal swelling Treatment Systemic antibiotics and warm compresses • DCR after acute infection is controlled •
 25
25
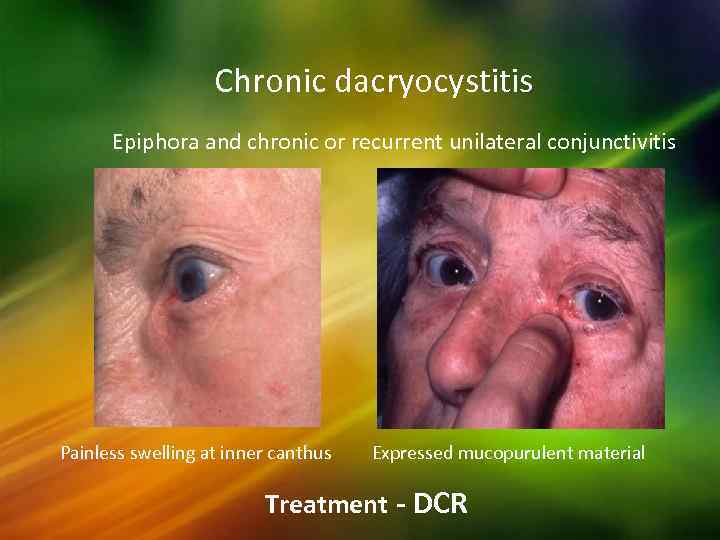 Chronic dacryocystitis Epiphora and chronic or recurrent unilateral conjunctivitis Painless swelling at inner canthus Expressed mucopurulent material Treatment - DCR
Chronic dacryocystitis Epiphora and chronic or recurrent unilateral conjunctivitis Painless swelling at inner canthus Expressed mucopurulent material Treatment - DCR
 Lacrimal Gland Tumours 50% are inflammations & lymphoid proliferations Pleomorphic adenoma (benign mixed cell tumour) Epithelial origin 20 -60 yrs Painless, usually with long history (>1 yr) Palpable hard nodular mass Non-axial proptosis; astigmatism Surgical removal en bloc rather than biopsy Good prognosis if completely removed 27
Lacrimal Gland Tumours 50% are inflammations & lymphoid proliferations Pleomorphic adenoma (benign mixed cell tumour) Epithelial origin 20 -60 yrs Painless, usually with long history (>1 yr) Palpable hard nodular mass Non-axial proptosis; astigmatism Surgical removal en bloc rather than biopsy Good prognosis if completely removed 27
 28
28
 Lacrimal Gland Tumours Carcinoma Epithelial origin Painful, usually short history Causes local bony erosion Usually biopsied after trial of antibiotics If biopsy +ve, requires radical local resection with RT Poor prognosis 29
Lacrimal Gland Tumours Carcinoma Epithelial origin Painful, usually short history Causes local bony erosion Usually biopsied after trial of antibiotics If biopsy +ve, requires radical local resection with RT Poor prognosis 29
 Lacrimal Sac Tumours Features Rare Painless swelling Punctal reflux of pus & blood Can be SCC, adenocarcinoma 30
Lacrimal Sac Tumours Features Rare Painless swelling Punctal reflux of pus & blood Can be SCC, adenocarcinoma 30
 The Orbit
The Orbit
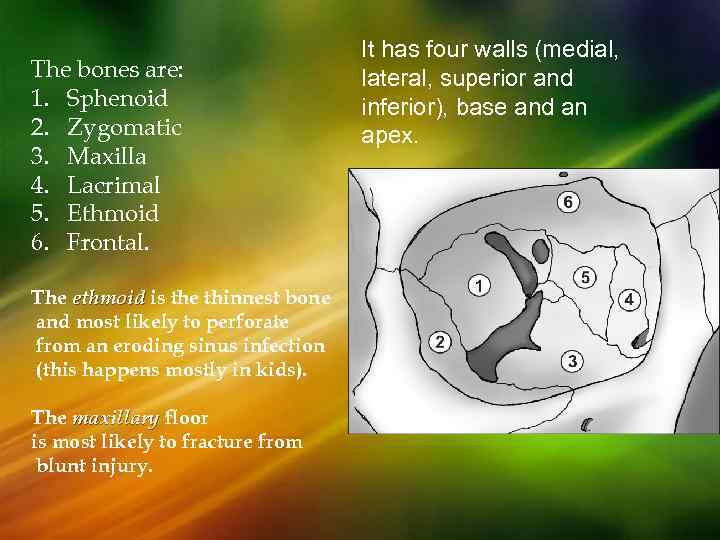 The bones are: 1. Sphenoid 2. Zygomatic 3. Maxilla 4. Lacrimal 5. Ethmoid 6. Frontal. The ethmoid is the thinnest bone and most likely to perforate from an eroding sinus infection (this happens mostly in kids). The maxillary floor is most likely to fracture from blunt injury. It has four walls (medial, lateral, superior and inferior), base and an apex.
The bones are: 1. Sphenoid 2. Zygomatic 3. Maxilla 4. Lacrimal 5. Ethmoid 6. Frontal. The ethmoid is the thinnest bone and most likely to perforate from an eroding sinus infection (this happens mostly in kids). The maxillary floor is most likely to fracture from blunt injury. It has four walls (medial, lateral, superior and inferior), base and an apex.
 The three basic structures that determine globe position of the eye are the bony orbits, the ligament and muscle system & the orbital fat. The orbit also protects the eye because the bones surrounding the eye “stick out” further than the eye Transmits nerves and blood vessels.
The three basic structures that determine globe position of the eye are the bony orbits, the ligament and muscle system & the orbital fat. The orbit also protects the eye because the bones surrounding the eye “stick out” further than the eye Transmits nerves and blood vessels.
 Clinical features of orbit diseases: 1. 2. 3. 4. 5. 6. Exophthalmos (proptosis) Enophthalmos Pain Diplopia Visual acuity disturbances Eyelid and conjunctival changes
Clinical features of orbit diseases: 1. 2. 3. 4. 5. 6. Exophthalmos (proptosis) Enophthalmos Pain Diplopia Visual acuity disturbances Eyelid and conjunctival changes
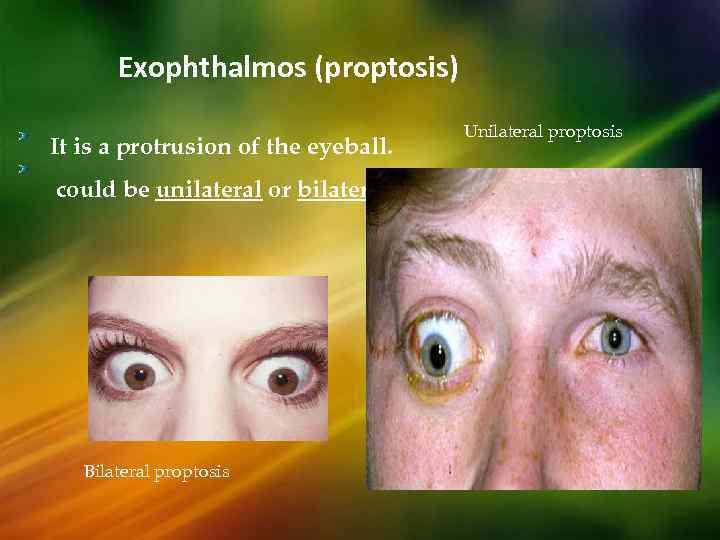 Exophthalmos (proptosis) It is a protrusion of the eyeball. could be unilateral or bilateral. Bilateral proptosis Unilateral proptosis
Exophthalmos (proptosis) It is a protrusion of the eyeball. could be unilateral or bilateral. Bilateral proptosis Unilateral proptosis
 CLASSIFICATION Proptosis can be divided into following clinical groups: • Unilateral proptosis • Bilateral proptosis • Acute proptosis • Intermittent proptosis • Pulsating proptosis 36
CLASSIFICATION Proptosis can be divided into following clinical groups: • Unilateral proptosis • Bilateral proptosis • Acute proptosis • Intermittent proptosis • Pulsating proptosis 36
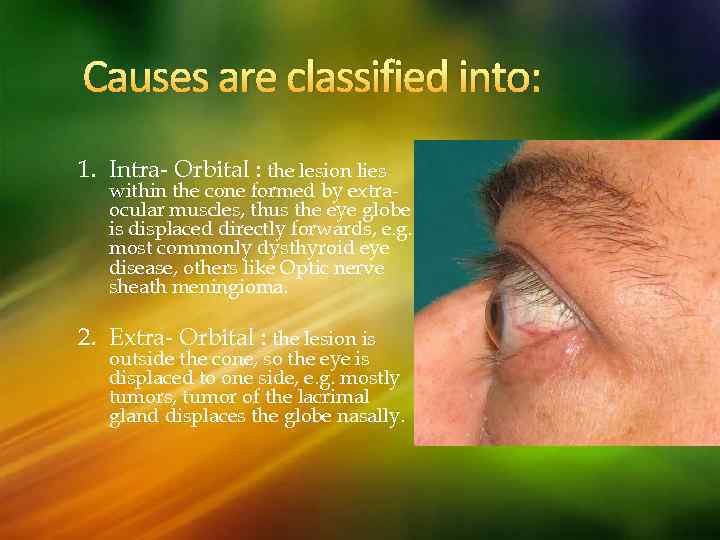 Causes are classified into: 1. Intra- Orbital : the lesion lies within the cone formed by extraocular muscles, thus the eye globe is displaced directly forwards, e. g. most commonly dysthyroid eye disease, others like Optic nerve sheath meningioma. 2. Extra- Orbital : the lesion is outside the cone, so the eye is displaced to one side, e. g. mostly tumors, tumor of the lacrimal gland displaces the globe nasally.
Causes are classified into: 1. Intra- Orbital : the lesion lies within the cone formed by extraocular muscles, thus the eye globe is displaced directly forwards, e. g. most commonly dysthyroid eye disease, others like Optic nerve sheath meningioma. 2. Extra- Orbital : the lesion is outside the cone, so the eye is displaced to one side, e. g. mostly tumors, tumor of the lacrimal gland displaces the globe nasally.
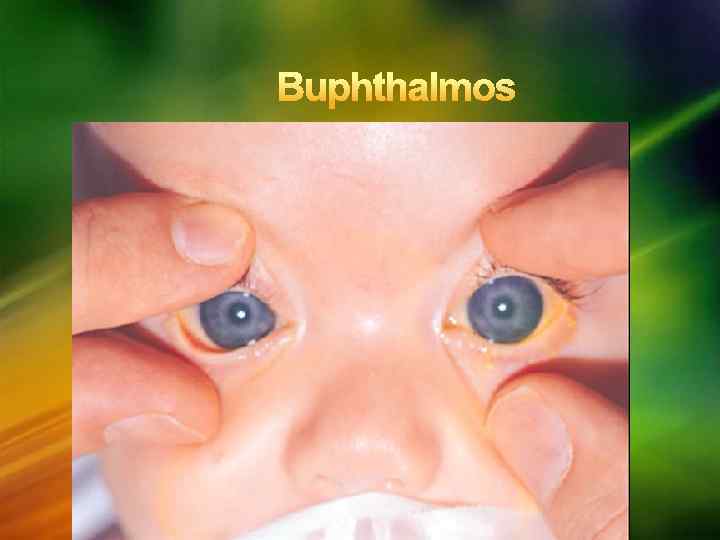
 Ø Ø Ø Graves disease Infectious (Orbital cellulitis) Orbital Inflammatory disease Vasculitis (wegener’s granulomatosis) Neoplastic (unilateral): Lacrimal, Lymphoma, Metastatic. Ø Orbital vascular disease Ø Trauma Ø Pseudoproptosis (pseudoexophthalmos) Ø Buphthalmos ( congenital open angle glaucoma) Ø Contralateral enophthalmos
Ø Ø Ø Graves disease Infectious (Orbital cellulitis) Orbital Inflammatory disease Vasculitis (wegener’s granulomatosis) Neoplastic (unilateral): Lacrimal, Lymphoma, Metastatic. Ø Orbital vascular disease Ø Trauma Ø Pseudoproptosis (pseudoexophthalmos) Ø Buphthalmos ( congenital open angle glaucoma) Ø Contralateral enophthalmos
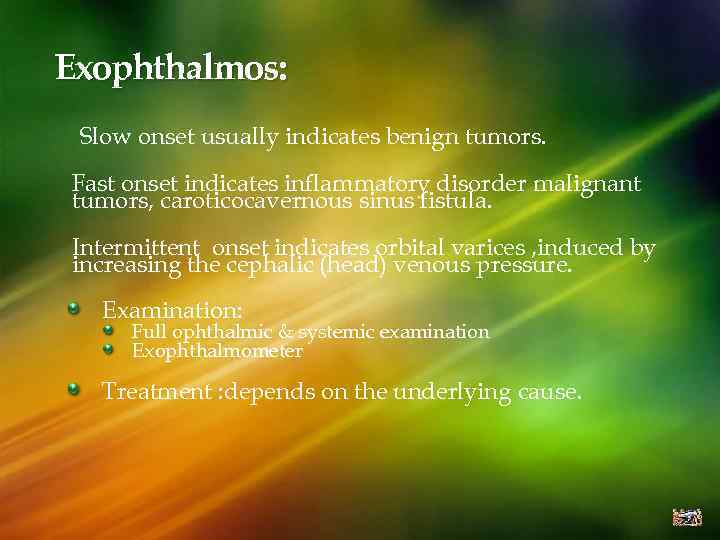 Exophthalmos: Slow onset usually indicates benign tumors. Fast onset indicates inflammatory disorder malignant tumors, caroticocavernous sinus fistula. Intermittent onset indicates orbital varices , induced by increasing the cephalic (head) venous pressure. Examination: Full ophthalmic & systemic examination Exophthalmometer Treatment : depends on the underlying cause.
Exophthalmos: Slow onset usually indicates benign tumors. Fast onset indicates inflammatory disorder malignant tumors, caroticocavernous sinus fistula. Intermittent onset indicates orbital varices , induced by increasing the cephalic (head) venous pressure. Examination: Full ophthalmic & systemic examination Exophthalmometer Treatment : depends on the underlying cause.
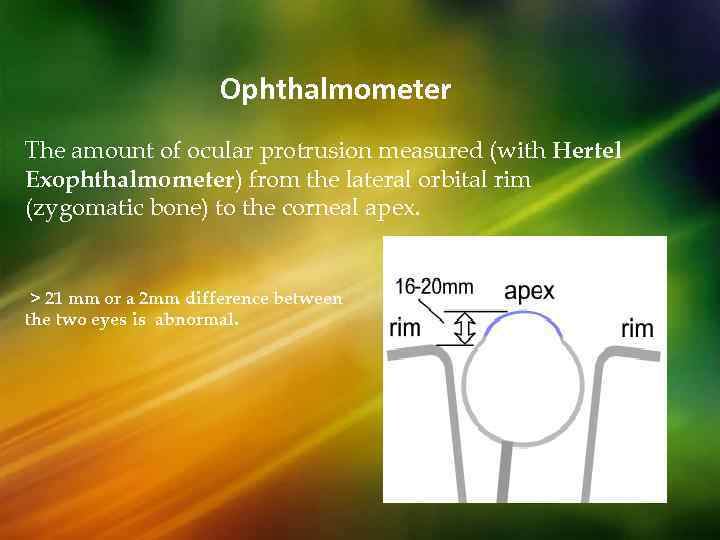 Ophthalmometer The amount of ocular protrusion measured (with Hertel Exophthalmometer) from the lateral orbital rim (zygomatic bone) to the corneal apex. > 21 mm or a 2 mm difference between the two eyes is abnormal.
Ophthalmometer The amount of ocular protrusion measured (with Hertel Exophthalmometer) from the lateral orbital rim (zygomatic bone) to the corneal apex. > 21 mm or a 2 mm difference between the two eyes is abnormal.
 42
42
 Complications Failure of the eyelid to close leading to corneal damage , ulceration , & Possibly perforation. Compression on the optic nerve or ophthalmic artery leading to blindness Restriction of eye movements & squint …
Complications Failure of the eyelid to close leading to corneal damage , ulceration , & Possibly perforation. Compression on the optic nerve or ophthalmic artery leading to blindness Restriction of eye movements & squint …
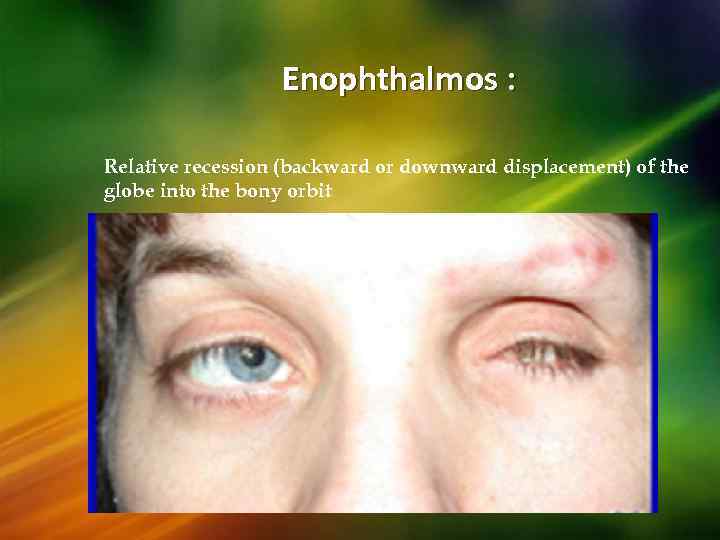 Enophthalmos : Relative recession (backward or downward displacement) of the globe into the bony orbit
Enophthalmos : Relative recession (backward or downward displacement) of the globe into the bony orbit
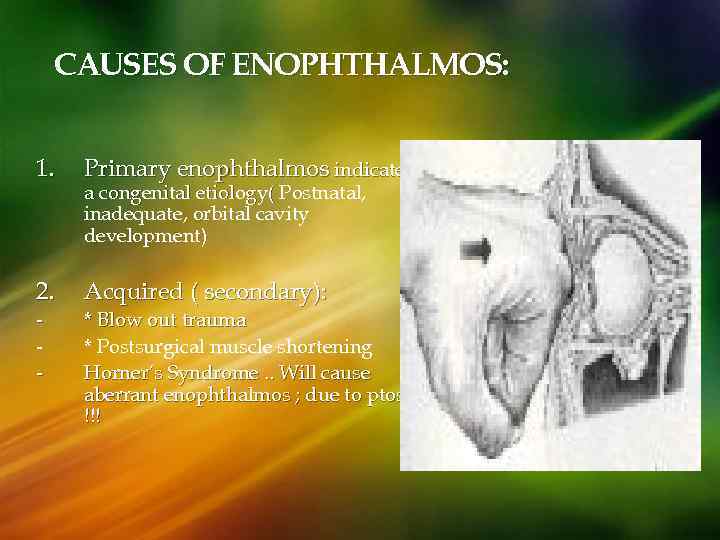 CAUSES OF ENOPHTHALMOS: 1. Primary enophthalmos indicates 2. Acquired ( secondary): - a congenital etiology( Postnatal, inadequate, orbital cavity development) * Blow out trauma * Postsurgical muscle shortening Horner’s Syndrome. . Will cause aberrant enophthalmos ; due to ptosis !!!
CAUSES OF ENOPHTHALMOS: 1. Primary enophthalmos indicates 2. Acquired ( secondary): - a congenital etiology( Postnatal, inadequate, orbital cavity development) * Blow out trauma * Postsurgical muscle shortening Horner’s Syndrome. . Will cause aberrant enophthalmos ; due to ptosis !!!
 Treatment : involves reconstruction of the bony orbit with restoration of bony orbital volume and repositioning of the globe. Complications : Long-standing enophthalmos, especially associated with very extensive orbital trauma, may be associated with severe orbital scarring, and correction can be very difficult or impossible.
Treatment : involves reconstruction of the bony orbit with restoration of bony orbital volume and repositioning of the globe. Complications : Long-standing enophthalmos, especially associated with very extensive orbital trauma, may be associated with severe orbital scarring, and correction can be very difficult or impossible.
 Investigation of orbital disease 1. 2. 3. CT MRI Systemic tests
Investigation of orbital disease 1. 2. 3. CT MRI Systemic tests
 Differential diagnosis of orbital diseases Trauma Disorders of extra-ocular muscles (Dysthyroid eye disease and ocular myositis, rhabdomyosacroma) Infective disorders (orbital cellulitis and preseptal cellulitis) Inflammatory diseases (Sarcoidosis, orbital pseudotumors) Vascular abnormalities (Carotico-Cavernous sinus fistula, orbital varix, capillary hemangioma) Orbital tumors (lacrimal gland tumors, meningioma of the optic nerve, optic nerve glioma, rhabdomyosarcoma) Dermoid cysts
Differential diagnosis of orbital diseases Trauma Disorders of extra-ocular muscles (Dysthyroid eye disease and ocular myositis, rhabdomyosacroma) Infective disorders (orbital cellulitis and preseptal cellulitis) Inflammatory diseases (Sarcoidosis, orbital pseudotumors) Vascular abnormalities (Carotico-Cavernous sinus fistula, orbital varix, capillary hemangioma) Orbital tumors (lacrimal gland tumors, meningioma of the optic nerve, optic nerve glioma, rhabdomyosarcoma) Dermoid cysts
 Dysthyroid eye disorders Disorder of the thyroid gland that is associated with eye and orbital manifestation. Infiltration of the extra-ocular muscles with lymphocytes and the deposition of glycosaminoglycan. Usually occurs more in Females between 30 – 50 years old. It has a poor prognosis in Males. 90% occurs in smokers!
Dysthyroid eye disorders Disorder of the thyroid gland that is associated with eye and orbital manifestation. Infiltration of the extra-ocular muscles with lymphocytes and the deposition of glycosaminoglycan. Usually occurs more in Females between 30 – 50 years old. It has a poor prognosis in Males. 90% occurs in smokers!
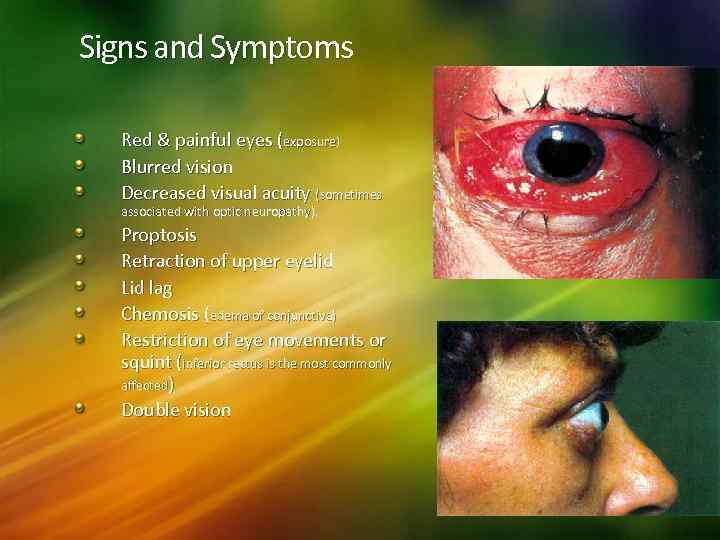 Signs and Symptoms Red & painful eyes (exposure) Blurred vision Decreased visual acuity (sometimes associated with optic neuropathy). Proptosis Retraction of upper eyelid Lid lag Chemosis (edema of conjunctiva) Restriction of eye movements or squint (inferior rectus is the most commonly affected) Double vision
Signs and Symptoms Red & painful eyes (exposure) Blurred vision Decreased visual acuity (sometimes associated with optic neuropathy). Proptosis Retraction of upper eyelid Lid lag Chemosis (edema of conjunctiva) Restriction of eye movements or squint (inferior rectus is the most commonly affected) Double vision
 Lab & Investigations: o o Biochemical tests for hyperthyroidism (TFT & antibodies) CT & MRI Management: o Emergency (corneal problem & pressure of optic nerve) is managed by systemic steroids, surgical orbital decompression & radiotherapy. o The long term management aims to restore E. O. M function & cosmetic. 1. The first step is the regulation of thyroid hormones levels 2. Artificial tears (prevent corneal drying and ulceration) 3. Glasses to correct any double vision (diplopia) 4. Guanethidine 5% drops may reduce lid retraction 5. Eyelid surgery to overcome lid retraction 6. Stop smoking.
Lab & Investigations: o o Biochemical tests for hyperthyroidism (TFT & antibodies) CT & MRI Management: o Emergency (corneal problem & pressure of optic nerve) is managed by systemic steroids, surgical orbital decompression & radiotherapy. o The long term management aims to restore E. O. M function & cosmetic. 1. The first step is the regulation of thyroid hormones levels 2. Artificial tears (prevent corneal drying and ulceration) 3. Glasses to correct any double vision (diplopia) 4. Guanethidine 5% drops may reduce lid retraction 5. Eyelid surgery to overcome lid retraction 6. Stop smoking.
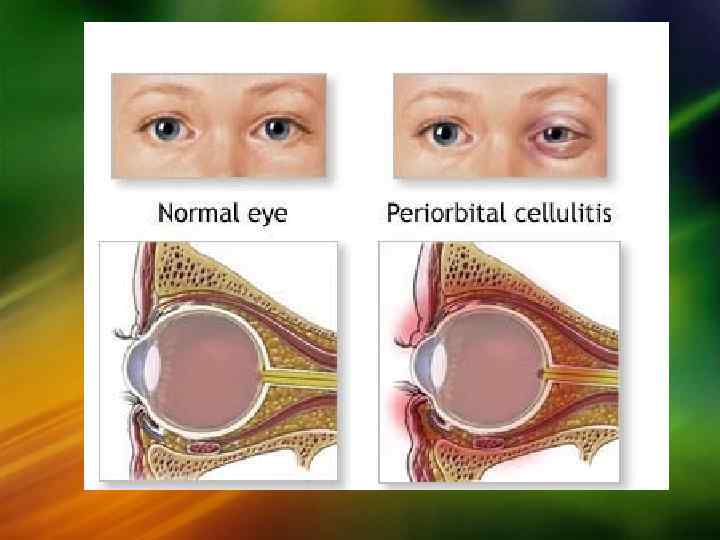
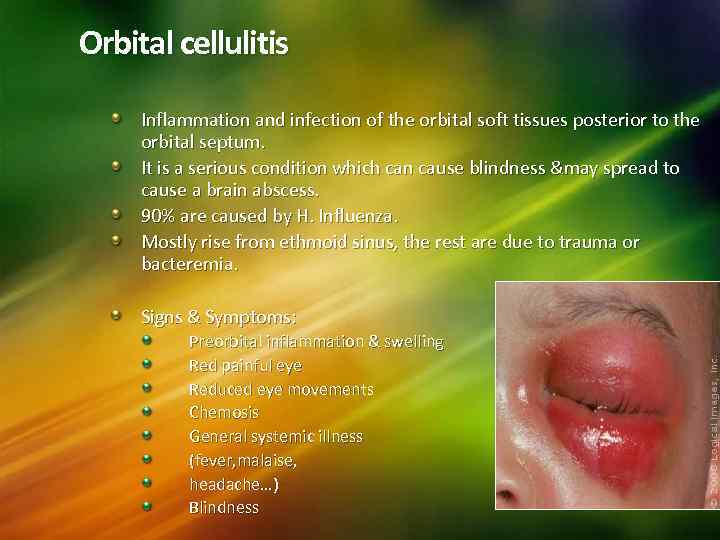 Orbital cellulitis Inflammation and infection of the orbital soft tissues posterior to the orbital septum. It is a serious condition which can cause blindness &may spread to cause a brain abscess. 90% are caused by H. Influenza. Mostly rise from ethmoid sinus, the rest are due to trauma or bacteremia. Signs & Symptoms: Preorbital inflammation & swelling Red painful eye Reduced eye movements Chemosis General systemic illness (fever, malaise, headache…) Blindness
Orbital cellulitis Inflammation and infection of the orbital soft tissues posterior to the orbital septum. It is a serious condition which can cause blindness &may spread to cause a brain abscess. 90% are caused by H. Influenza. Mostly rise from ethmoid sinus, the rest are due to trauma or bacteremia. Signs & Symptoms: Preorbital inflammation & swelling Red painful eye Reduced eye movements Chemosis General systemic illness (fever, malaise, headache…) Blindness
 Diagnosis: Mainly by clinical evaluation. MRI. CT Scan (ascertain precipitating sinus involvement, identify orbital abscess). Treatment: Broad spectrum IV antibiotics. Surgical intervention (draining the abscess) is Indicated when there is: Poor response to antibiotics. Decreased vision because of optic nerve compromise. Afferent papillary defect. Patients older than 16 years old.
Diagnosis: Mainly by clinical evaluation. MRI. CT Scan (ascertain precipitating sinus involvement, identify orbital abscess). Treatment: Broad spectrum IV antibiotics. Surgical intervention (draining the abscess) is Indicated when there is: Poor response to antibiotics. Decreased vision because of optic nerve compromise. Afferent papillary defect. Patients older than 16 years old.
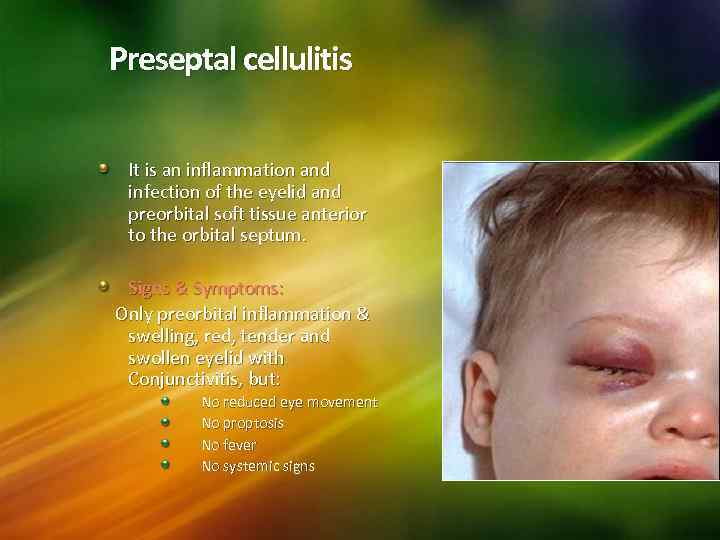 Preseptal cellulitis It is an inflammation and infection of the eyelid and preorbital soft tissue anterior to the orbital septum. Signs & Symptoms: Only preorbital inflammation & swelling, red, tender and swollen eyelid with Conjunctivitis, but: No reduced eye movement No proptosis No fever No systemic signs
Preseptal cellulitis It is an inflammation and infection of the eyelid and preorbital soft tissue anterior to the orbital septum. Signs & Symptoms: Only preorbital inflammation & swelling, red, tender and swollen eyelid with Conjunctivitis, but: No reduced eye movement No proptosis No fever No systemic signs
 1. 2. 3. 4. 5. 6. 7. Causes: Trauma (local infection) Infections (especially sinusitis) Recent surgeries near eyelids or oral procedures Bug bites Chalazion: a cyst in the eyelid that is caused by inflammation of a blocked meibomian gland Dacrocystitis: infection of the nasolacrimal sac Systemic diseases (asthma, neutropenia, nasal polyp) Complications: 1. Orbital abscess 2. Orbital mucocele
1. 2. 3. 4. 5. 6. 7. Causes: Trauma (local infection) Infections (especially sinusitis) Recent surgeries near eyelids or oral procedures Bug bites Chalazion: a cyst in the eyelid that is caused by inflammation of a blocked meibomian gland Dacrocystitis: infection of the nasolacrimal sac Systemic diseases (asthma, neutropenia, nasal polyp) Complications: 1. Orbital abscess 2. Orbital mucocele
 Treatment: If mild, treat with oral antibiotics (Augmantin or 1 st generation cephalosporins), warm compressors. If severe the patient should be admitted and given IV antibiotics (2 nd or 3 rd generation cephalosporins with or without Clindamycin) Improvement should be noted after 2 – 3 days. Surgery is indicated for eyelid abscess drainage.
Treatment: If mild, treat with oral antibiotics (Augmantin or 1 st generation cephalosporins), warm compressors. If severe the patient should be admitted and given IV antibiotics (2 nd or 3 rd generation cephalosporins with or without Clindamycin) Improvement should be noted after 2 – 3 days. Surgery is indicated for eyelid abscess drainage.
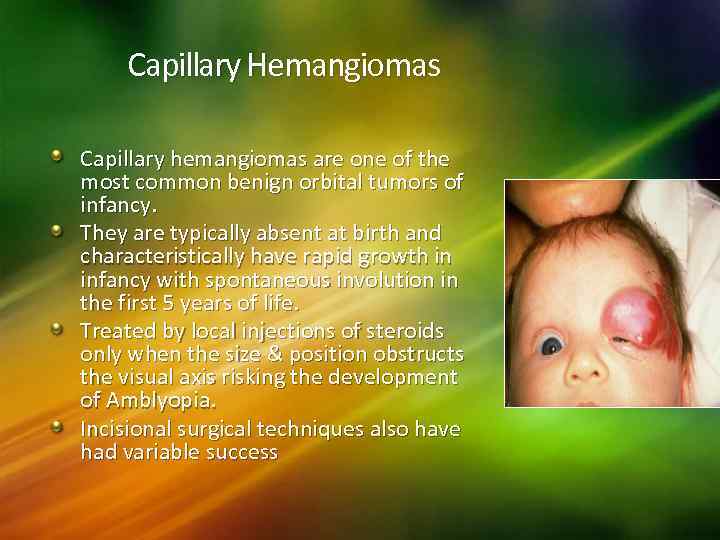 Capillary Hemangiomas Capillary hemangiomas are one of the most common benign orbital tumors of infancy. They are typically absent at birth and characteristically have rapid growth in infancy with spontaneous involution in the first 5 years of life. Treated by local injections of steroids only when the size & position obstructs the visual axis risking the development of Amblyopia. Incisional surgical techniques also have had variable success
Capillary Hemangiomas Capillary hemangiomas are one of the most common benign orbital tumors of infancy. They are typically absent at birth and characteristically have rapid growth in infancy with spontaneous involution in the first 5 years of life. Treated by local injections of steroids only when the size & position obstructs the visual axis risking the development of Amblyopia. Incisional surgical techniques also have had variable success
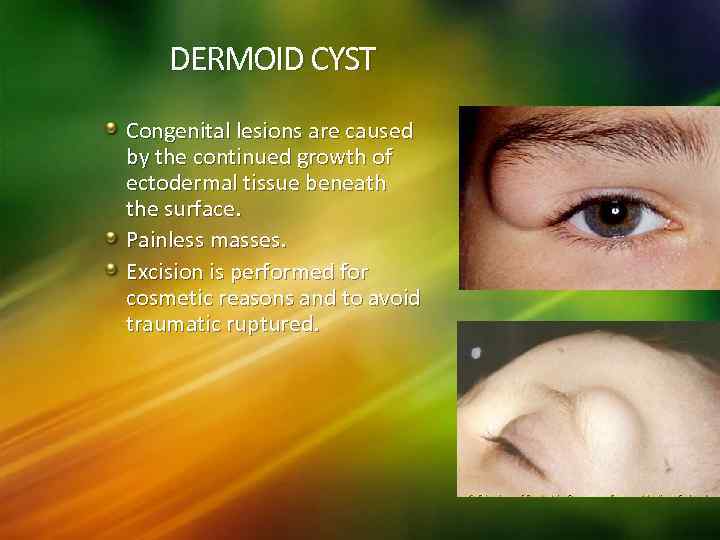 DERMOID CYST Congenital lesions are caused by the continued growth of ectodermal tissue beneath the surface. Painless masses. Excision is performed for cosmetic reasons and to avoid traumatic ruptured.
DERMOID CYST Congenital lesions are caused by the continued growth of ectodermal tissue beneath the surface. Painless masses. Excision is performed for cosmetic reasons and to avoid traumatic ruptured.
 ORBITAL TUMORS Primary: Rhabdomyosarcoma( malignant) Optic nerve glioma Lacrimal gland tumors Meningiomas Lymphoma Secondary (Metastasis)
ORBITAL TUMORS Primary: Rhabdomyosarcoma( malignant) Optic nerve glioma Lacrimal gland tumors Meningiomas Lymphoma Secondary (Metastasis)
 RHABDOMYOSARCOMA Commonest primary malignancy of the orbit in children Rapidly growing arises from striated muscles. appears everywhere there is skeletal muscles. 40% usually found in the superonasal orbit 90% occurs before the age of 16. Signs & Symptoms: Painless visible mass, proptosis, ptosis. Diagnosis: CT Scan; MRI
RHABDOMYOSARCOMA Commonest primary malignancy of the orbit in children Rapidly growing arises from striated muscles. appears everywhere there is skeletal muscles. 40% usually found in the superonasal orbit 90% occurs before the age of 16. Signs & Symptoms: Painless visible mass, proptosis, ptosis. Diagnosis: CT Scan; MRI
 Complications: Metastasis to the lungs or brain. Treatment: Radiotherapy & chemotherapy, if there is no recurrence after 3 years then it is controlled. Surgery might be used but it is difficult because the tumor is embedded deep in the tissue Prognosis depends on the size, type & stage.
Complications: Metastasis to the lungs or brain. Treatment: Radiotherapy & chemotherapy, if there is no recurrence after 3 years then it is controlled. Surgery might be used but it is difficult because the tumor is embedded deep in the tissue Prognosis depends on the size, type & stage.
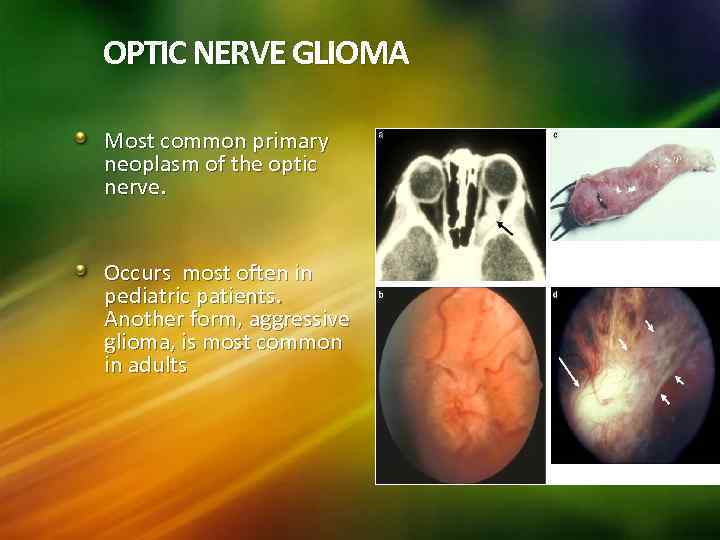 OPTIC NERVE GLIOMA Most common primary neoplasm of the optic nerve. Occurs most often in pediatric patients. Another form, aggressive glioma, is most common in adults
OPTIC NERVE GLIOMA Most common primary neoplasm of the optic nerve. Occurs most often in pediatric patients. Another form, aggressive glioma, is most common in adults
 1. 2. 3. 4. Signs & Symptoms: Proptosis (mainly) Strabismus Reduced visual acuity Ptosis Diagnosis: CT Scan, MRI Treatment: Only observation. They are slowly growing & the treatment is very difficult. Surgery, radiation, chemotherapy.
1. 2. 3. 4. Signs & Symptoms: Proptosis (mainly) Strabismus Reduced visual acuity Ptosis Diagnosis: CT Scan, MRI Treatment: Only observation. They are slowly growing & the treatment is very difficult. Surgery, radiation, chemotherapy.
 SECONDARY TUMORS Metastasis to the Orbit from: Breast cancer (40%) Lung cancer Prostate cancer Liver cancer
SECONDARY TUMORS Metastasis to the Orbit from: Breast cancer (40%) Lung cancer Prostate cancer Liver cancer
 66
66
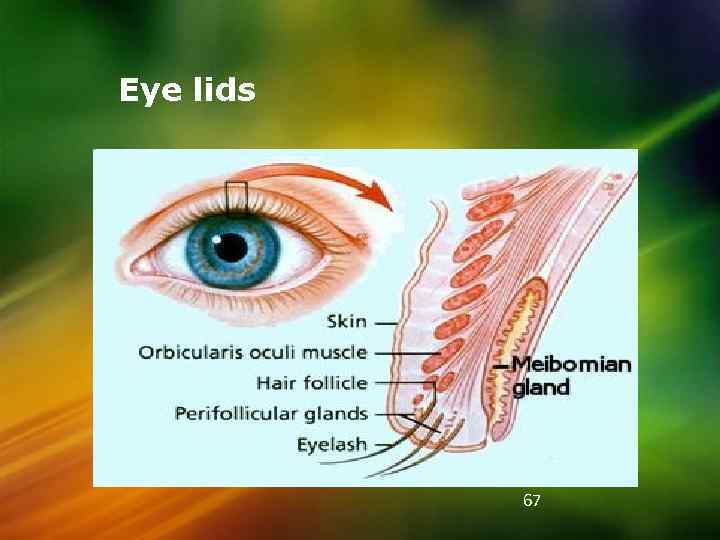 Eye lids 67
Eye lids 67
 The eye lid is made up of 4 layers. 1) Skin 2) Muscle layer. a) b) c) Orbicular is oculi muscle Levator palpebrae superiors. Muller's muscle 3) Tarsus and meibomian (tarsal) glands. 4) Mucous layer : formed by the palpebra conjunctiva.
The eye lid is made up of 4 layers. 1) Skin 2) Muscle layer. a) b) c) Orbicular is oculi muscle Levator palpebrae superiors. Muller's muscle 3) Tarsus and meibomian (tarsal) glands. 4) Mucous layer : formed by the palpebra conjunctiva.
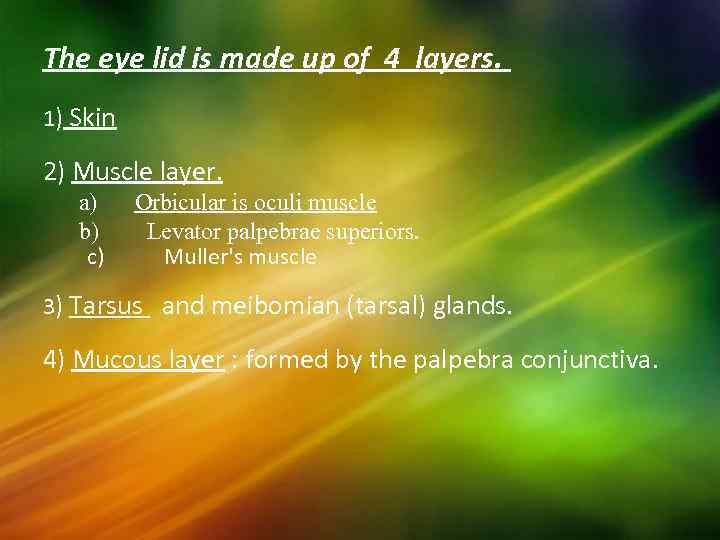
 Muscle layer Orbicularis oculi muscle Levator palpebrae superioris
Muscle layer Orbicularis oculi muscle Levator palpebrae superioris
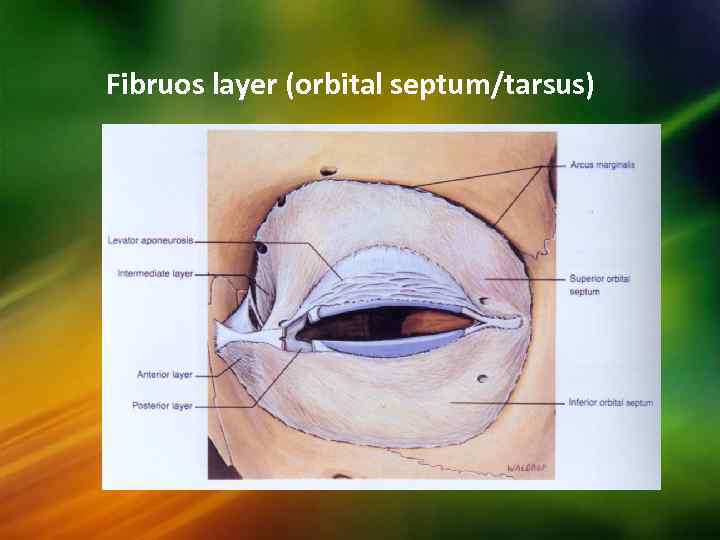 Fibruos layer (orbital septum/tarsus)
Fibruos layer (orbital septum/tarsus)
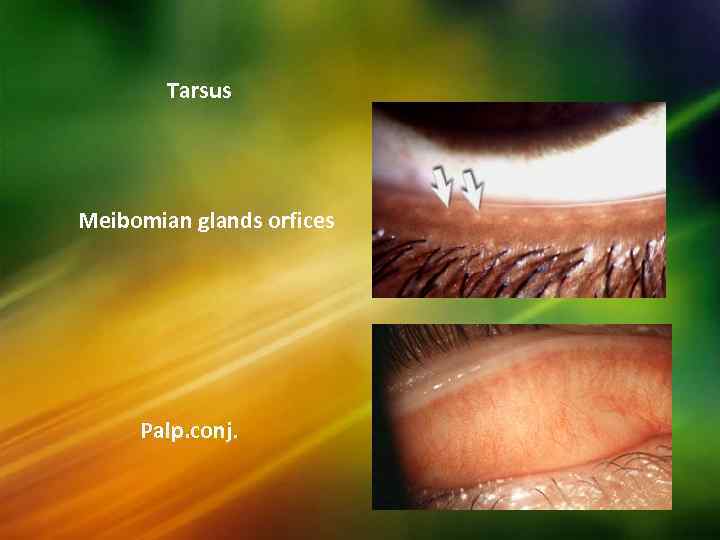 Tarsus Meibomian glands orfices Palp. conj.
Tarsus Meibomian glands orfices Palp. conj.
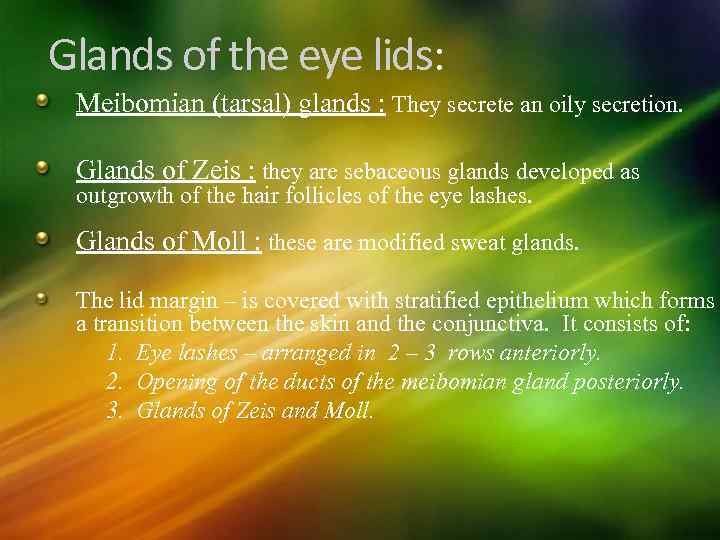 Glands of the eye lids: Meibomian (tarsal) glands : They secrete an oily secretion. Glands of Zeis : they are sebaceous glands developed as outgrowth of the hair follicles of the eye lashes. Glands of Moll : these are modified sweat glands. The lid margin – is covered with stratified epithelium which forms a transition between the skin and the conjunctiva. It consists of: 1. Eye lashes – arranged in 2 – 3 rows anteriorly. 2. Opening of the ducts of the meibomian gland posteriorly. 3. Glands of Zeis and Moll.
Glands of the eye lids: Meibomian (tarsal) glands : They secrete an oily secretion. Glands of Zeis : they are sebaceous glands developed as outgrowth of the hair follicles of the eye lashes. Glands of Moll : these are modified sweat glands. The lid margin – is covered with stratified epithelium which forms a transition between the skin and the conjunctiva. It consists of: 1. Eye lashes – arranged in 2 – 3 rows anteriorly. 2. Opening of the ducts of the meibomian gland posteriorly. 3. Glands of Zeis and Moll.
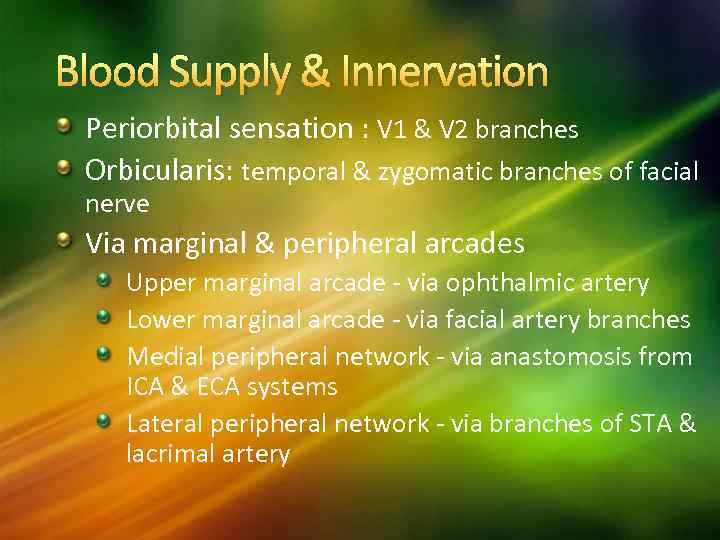 Blood Supply & Innervation Periorbital sensation : V 1 & V 2 branches Orbicularis: temporal & zygomatic branches of facial nerve Via marginal & peripheral arcades Upper marginal arcade - via ophthalmic artery Lower marginal arcade - via facial artery branches Medial peripheral network - via anastomosis from ICA & ECA systems Lateral peripheral network - via branches of STA & lacrimal artery
Blood Supply & Innervation Periorbital sensation : V 1 & V 2 branches Orbicularis: temporal & zygomatic branches of facial nerve Via marginal & peripheral arcades Upper marginal arcade - via ophthalmic artery Lower marginal arcade - via facial artery branches Medial peripheral network - via anastomosis from ICA & ECA systems Lateral peripheral network - via branches of STA & lacrimal artery
 EYELID DISEASE
EYELID DISEASE
 Diseases of the eyelids. Infections & inflammation of the eyelid : e. g. Blepharitis =infection of the eyelid & eyelid margin Positional abnormalities e. g. ptosis=drooping of the eyelid. Shape abnormalities e. g. entropion=inward deviation of the eyelid, entropion=outward deviation of the eyelid Trichiasis & Distichiasis : - is an inversion of a varying number of eye lashes Inflammation of the glands of the lids: external hordeolum (stye) & chalazion Tumors of the eyelid , squamous cell & basal cell carcinoma. Miscellaneous e. g. eyelid wart & nevus. Trauma & eyelid laceration 75
Diseases of the eyelids. Infections & inflammation of the eyelid : e. g. Blepharitis =infection of the eyelid & eyelid margin Positional abnormalities e. g. ptosis=drooping of the eyelid. Shape abnormalities e. g. entropion=inward deviation of the eyelid, entropion=outward deviation of the eyelid Trichiasis & Distichiasis : - is an inversion of a varying number of eye lashes Inflammation of the glands of the lids: external hordeolum (stye) & chalazion Tumors of the eyelid , squamous cell & basal cell carcinoma. Miscellaneous e. g. eyelid wart & nevus. Trauma & eyelid laceration 75
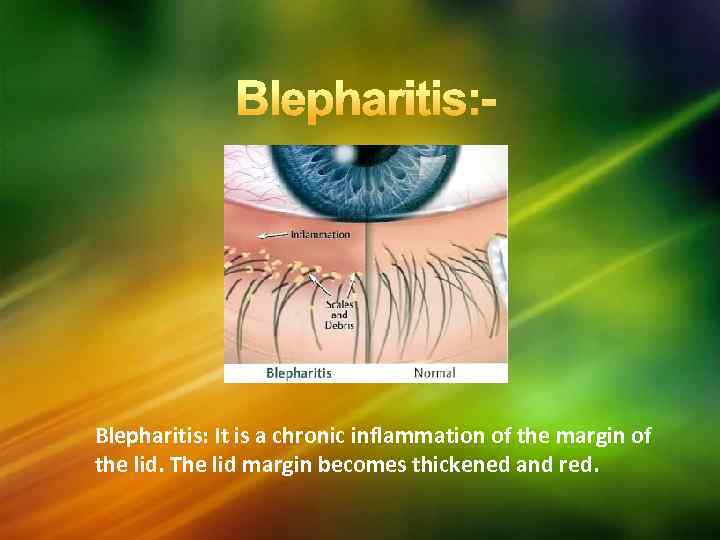 Blepharitis: It is a chronic inflammation of the margin of the lid. The lid margin becomes thickened and red.
Blepharitis: It is a chronic inflammation of the margin of the lid. The lid margin becomes thickened and red.
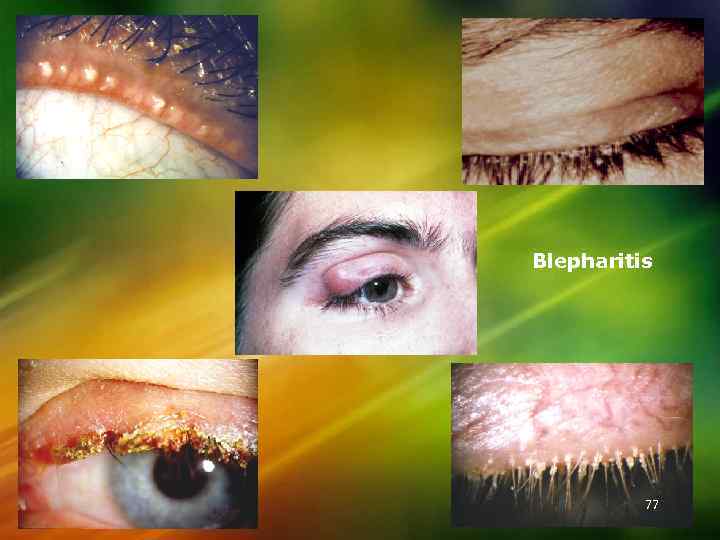 Blepharitis 77
Blepharitis 77
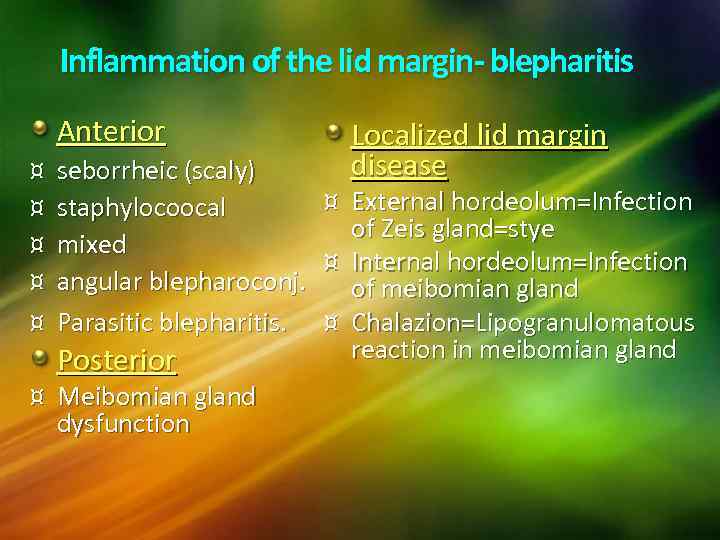 Inflammation of the lid margin- blepharitis Anterior ¤ ¤ ¤ seborrheic (scaly) staphylocoocal mixed angular blepharoconj. Parasitic blepharitis. Posterior ¤ Meibomian gland dysfunction Localized lid margin disease ¤ External hordeolum=Infection of Zeis gland=stye ¤ Internal hordeolum=Infection of meibomian gland ¤ Chalazion=Lipogranulomatous reaction in meibomian gland
Inflammation of the lid margin- blepharitis Anterior ¤ ¤ ¤ seborrheic (scaly) staphylocoocal mixed angular blepharoconj. Parasitic blepharitis. Posterior ¤ Meibomian gland dysfunction Localized lid margin disease ¤ External hordeolum=Infection of Zeis gland=stye ¤ Internal hordeolum=Infection of meibomian gland ¤ Chalazion=Lipogranulomatous reaction in meibomian gland
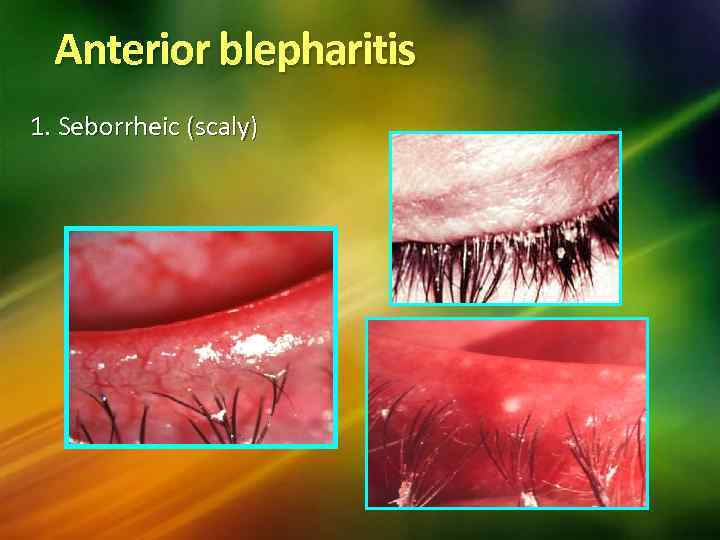 Anterior blepharitis 1. Seborrheic (scaly)
Anterior blepharitis 1. Seborrheic (scaly)
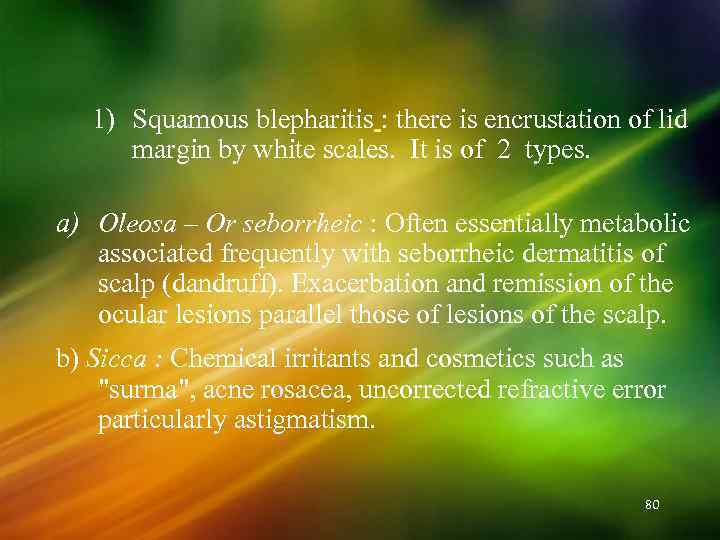 1) Squamous blepharitis : there is encrustation of lid margin by white scales. It is of 2 types. a) Oleosa – Or seborrheic : Often essentially metabolic associated frequently with seborrheic dermatitis of scalp (dandruff). Exacerbation and remission of the ocular lesions parallel those of lesions of the scalp. b) Sicca : Chemical irritants and cosmetics such as "surma", acne rosacea, uncorrected refractive error particularly astigmatism. 80
1) Squamous blepharitis : there is encrustation of lid margin by white scales. It is of 2 types. a) Oleosa – Or seborrheic : Often essentially metabolic associated frequently with seborrheic dermatitis of scalp (dandruff). Exacerbation and remission of the ocular lesions parallel those of lesions of the scalp. b) Sicca : Chemical irritants and cosmetics such as "surma", acne rosacea, uncorrected refractive error particularly astigmatism. 80
 Squamous Blepharitis 81
Squamous Blepharitis 81
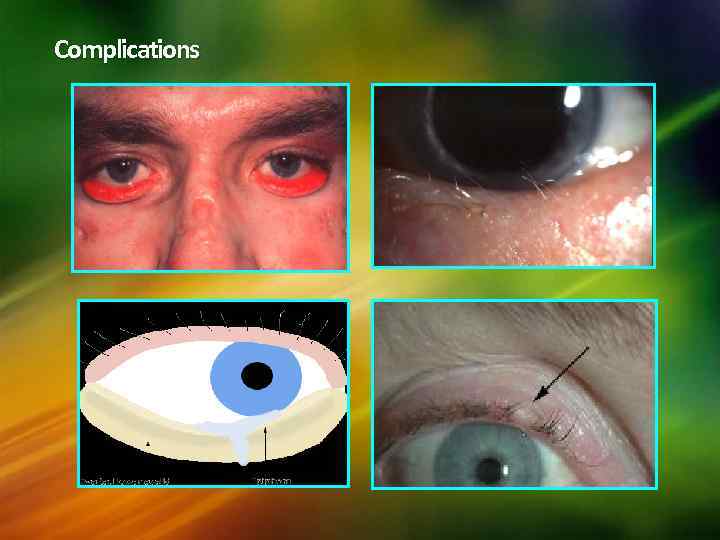 Complications
Complications
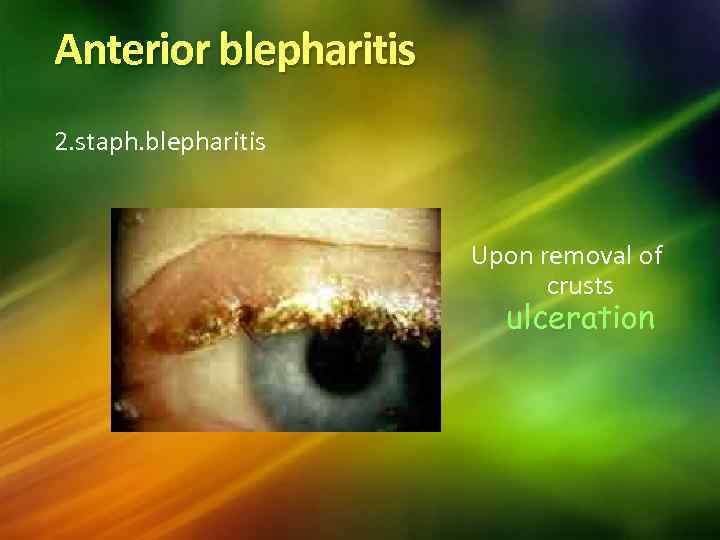 Anterior blepharitis 2. staph. blepharitis Upon removal of crusts ulceration
Anterior blepharitis 2. staph. blepharitis Upon removal of crusts ulceration
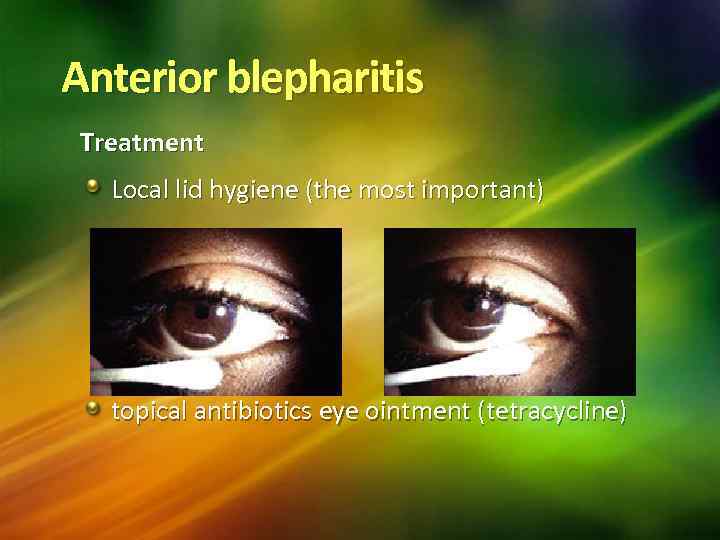 Anterior blepharitis Treatment Local lid hygiene (the most important) topical antibiotics eye ointment (tetracycline)
Anterior blepharitis Treatment Local lid hygiene (the most important) topical antibiotics eye ointment (tetracycline)
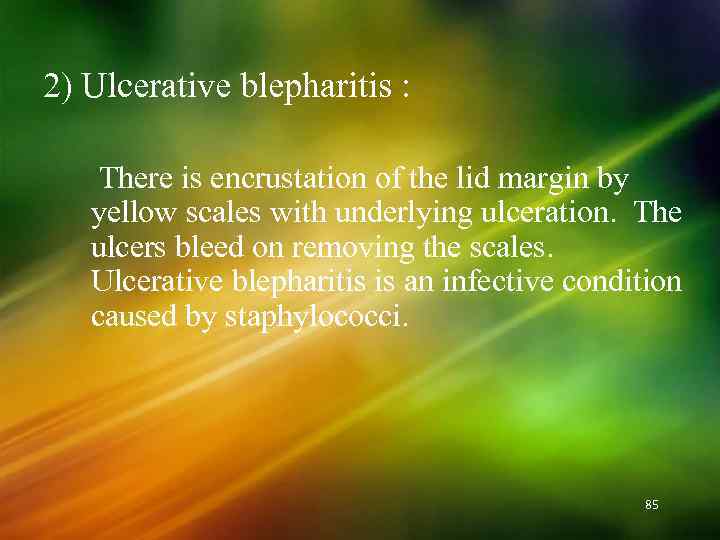 2) Ulcerative blepharitis : There is encrustation of the lid margin by yellow scales with underlying ulceration. The ulcers bleed on removing the scales. Ulcerative blepharitis is an infective condition caused by staphylococci. 85
2) Ulcerative blepharitis : There is encrustation of the lid margin by yellow scales with underlying ulceration. The ulcers bleed on removing the scales. Ulcerative blepharitis is an infective condition caused by staphylococci. 85
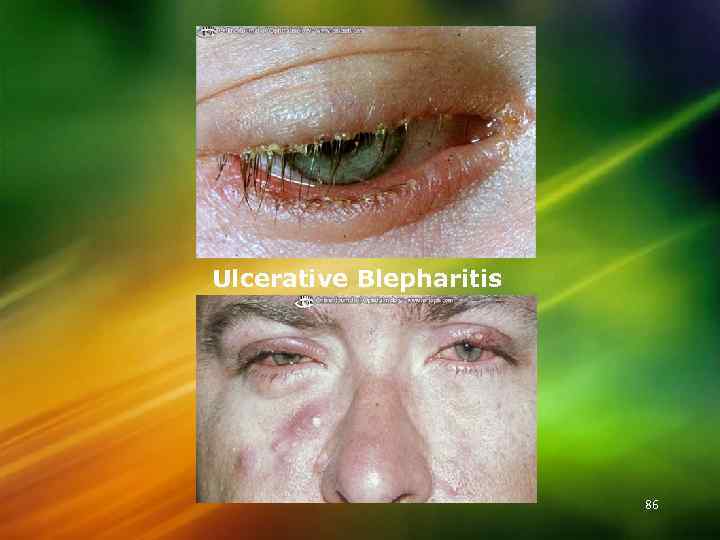 Ulcerative Blepharitis 86
Ulcerative Blepharitis 86
 3) Mixed blepharitis: Staphylococci infection super imposed on Squamous blepharitis 4) Margin is associated: with angular conjunctivitis – foamy discharge and excoriation of the skin of the lateral and medial canthi.
3) Mixed blepharitis: Staphylococci infection super imposed on Squamous blepharitis 4) Margin is associated: with angular conjunctivitis – foamy discharge and excoriation of the skin of the lateral and medial canthi.
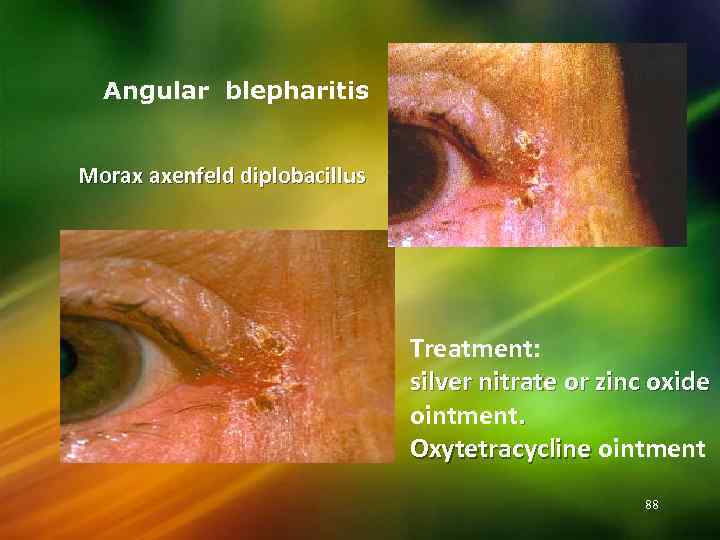 Angular blepharitis Morax axenfeld diplobacillus Treatment: silver nitrate or zinc oxide ointment. Oxytetracycline ointment 88
Angular blepharitis Morax axenfeld diplobacillus Treatment: silver nitrate or zinc oxide ointment. Oxytetracycline ointment 88
 The patients are usually children debilitated from : 1) Living under poor hygienic conditions – exposure to dust, smoke. 2) DISEASES – exanthematous disease, upper respiratory infections, tuberculosis, diabetes. 3) Dietary deficiency – malnutrition. Symptoms : Itching, soreness, lacrimation, photophobia. 89
The patients are usually children debilitated from : 1) Living under poor hygienic conditions – exposure to dust, smoke. 2) DISEASES – exanthematous disease, upper respiratory infections, tuberculosis, diabetes. 3) Dietary deficiency – malnutrition. Symptoms : Itching, soreness, lacrimation, photophobia. 89
 Complications: 1. Chronic conjunctivitis. 2. 3. 4. 5. 6. 7. 8. Marginal corneal ulcer. Styes. Permanent loss of lashes (madarosis ) Tylosis – usuall affects upper lid. Trichiasis. Entropion Ectropion 90
Complications: 1. Chronic conjunctivitis. 2. 3. 4. 5. 6. 7. 8. Marginal corneal ulcer. Styes. Permanent loss of lashes (madarosis ) Tylosis – usuall affects upper lid. Trichiasis. Entropion Ectropion 90
 5. Parasitic blepharitis Typically affects children with poor hygienic conditions. Pubic louse& its ova(nits). Itching. Treatment - removal, destruction and delousing
5. Parasitic blepharitis Typically affects children with poor hygienic conditions. Pubic louse& its ova(nits). Itching. Treatment - removal, destruction and delousing
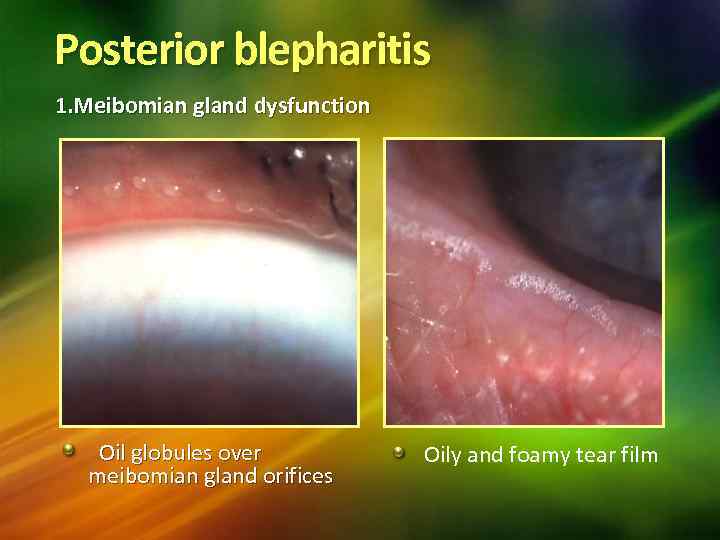 Posterior blepharitis 1. Meibomian gland dysfunction Oil globules over meibomian gland orifices Oily and foamy tear film
Posterior blepharitis 1. Meibomian gland dysfunction Oil globules over meibomian gland orifices Oily and foamy tear film
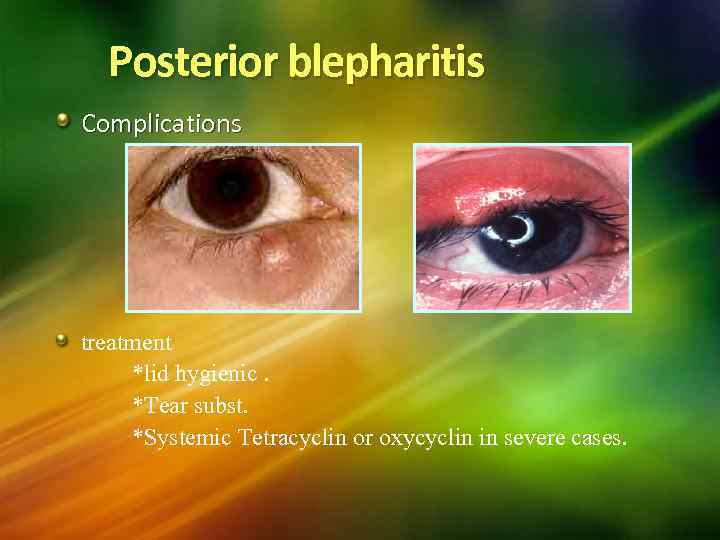 Posterior blepharitis Complications treatment *lid hygienic. *Tear subst. *Systemic Tetracyclin or oxycyclin in severe cases.
Posterior blepharitis Complications treatment *lid hygienic. *Tear subst. *Systemic Tetracyclin or oxycyclin in severe cases.
 Treatment : 1. Improvement of general health and living condition. 2. Treatment of seborrheic dermatitis on scalp with shampoo. 3. Removal of scales and crust with warm 3% soda bicarb solution. 4. In cases of squamous blepharitis - In more obstinate lesions, ointment of selenium oxide is used. 5. allergy to chemical and cosmetic, 1% hydrocortisone ointment is applied to the lid margin thrice a day. 6. In cases of ulcerative blepharitis antibiotics such as chloromycetin, erythoromycin or tetracycline are applied to the lid margin. 7. In more severe cases the antibiotic which has proved to be effective is given systemically, in addition to local treatment. 8. In cases of angular blepharitis oxteracycline ointment is applied. 94
Treatment : 1. Improvement of general health and living condition. 2. Treatment of seborrheic dermatitis on scalp with shampoo. 3. Removal of scales and crust with warm 3% soda bicarb solution. 4. In cases of squamous blepharitis - In more obstinate lesions, ointment of selenium oxide is used. 5. allergy to chemical and cosmetic, 1% hydrocortisone ointment is applied to the lid margin thrice a day. 6. In cases of ulcerative blepharitis antibiotics such as chloromycetin, erythoromycin or tetracycline are applied to the lid margin. 7. In more severe cases the antibiotic which has proved to be effective is given systemically, in addition to local treatment. 8. In cases of angular blepharitis oxteracycline ointment is applied. 94
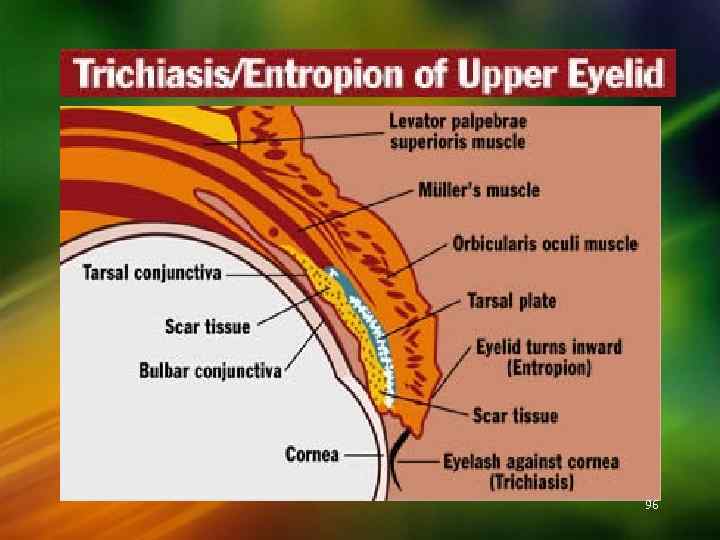
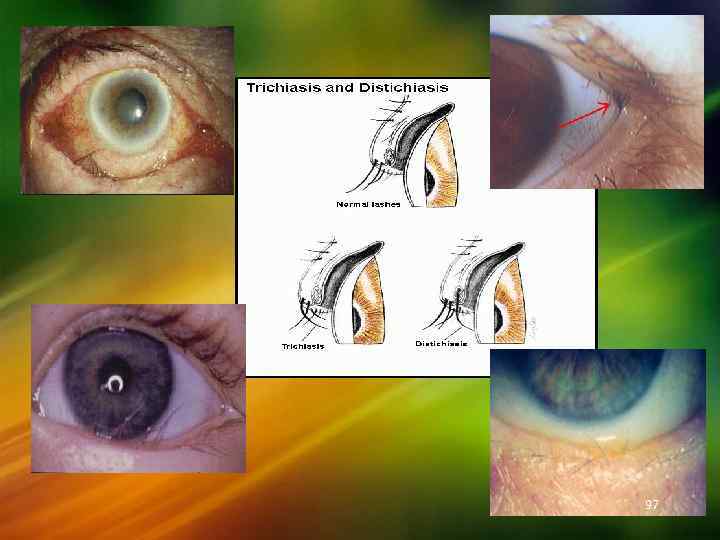
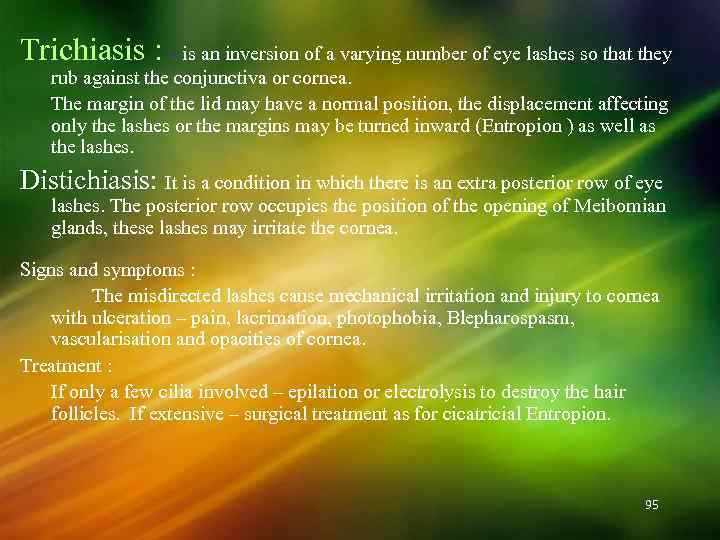 Trichiasis : - is an inversion of a varying number of eye lashes so that they rub against the conjunctiva or cornea. The margin of the lid may have a normal position, the displacement affecting only the lashes or the margins may be turned inward (Entropion ) as well as the lashes. Distichiasis: It is a condition in which there is an extra posterior row of eye lashes. The posterior row occupies the position of the opening of Meibomian glands, these lashes may irritate the cornea. Signs and symptoms : The misdirected lashes cause mechanical irritation and injury to cornea with ulceration – pain, lacrimation, photophobia, Blepharospasm, vascularisation and opacities of cornea. Treatment : If only a few cilia involved – epilation or electrolysis to destroy the hair follicles. If extensive – surgical treatment as for cicatricial Entropion. 95
Trichiasis : - is an inversion of a varying number of eye lashes so that they rub against the conjunctiva or cornea. The margin of the lid may have a normal position, the displacement affecting only the lashes or the margins may be turned inward (Entropion ) as well as the lashes. Distichiasis: It is a condition in which there is an extra posterior row of eye lashes. The posterior row occupies the position of the opening of Meibomian glands, these lashes may irritate the cornea. Signs and symptoms : The misdirected lashes cause mechanical irritation and injury to cornea with ulceration – pain, lacrimation, photophobia, Blepharospasm, vascularisation and opacities of cornea. Treatment : If only a few cilia involved – epilation or electrolysis to destroy the hair follicles. If extensive – surgical treatment as for cicatricial Entropion. 95
 96
96
 97
97
 Entropion : is a rolling of the margin of the lid and with it the lashes. I) Cicatricial entopion – due to cicatricial changes in the conjunctiva and distortion of the tarsal plate, most commonly affects the upper lid. a) Old case of trachoma. b) Blepharitis c) Burns and other injures to the lids d) Operation upon the lids e) Diphtheritic conjunctivitis, leprosy. Both upper and lower lids may be affected. 98
Entropion : is a rolling of the margin of the lid and with it the lashes. I) Cicatricial entopion – due to cicatricial changes in the conjunctiva and distortion of the tarsal plate, most commonly affects the upper lid. a) Old case of trachoma. b) Blepharitis c) Burns and other injures to the lids d) Operation upon the lids e) Diphtheritic conjunctivitis, leprosy. Both upper and lower lids may be affected. 98
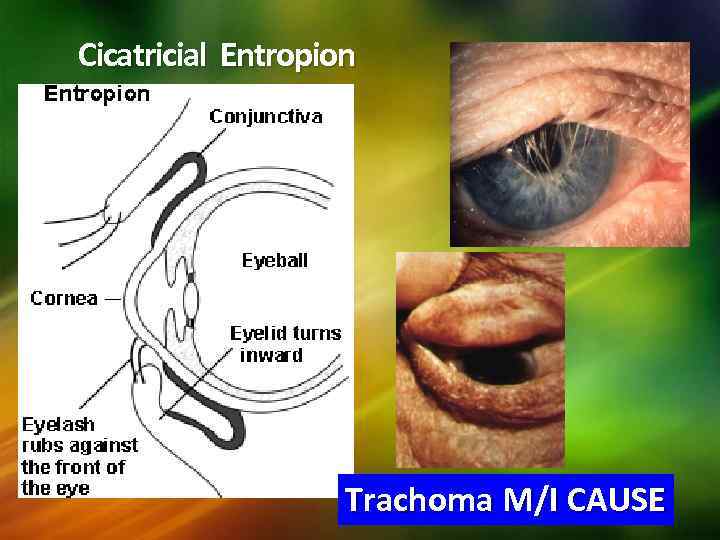 Cicatricial Entropion Trachoma M/I CAUSE
Cicatricial Entropion Trachoma M/I CAUSE
 II) Spastic entropion: Due to spasm of the palpebral portion of the orbicularis muscle, most commonly affecting lower lid, If the support is insufficient intropion is produced: 1) Atrophy or absence of eye ball 2) Old persons ( senile entropion) owing to absence of orbital fat. 3) Tight bandaging after surgical operation of the eye. 4) Blepharospasm Symptoms and signs – same as for trichiasis 100
II) Spastic entropion: Due to spasm of the palpebral portion of the orbicularis muscle, most commonly affecting lower lid, If the support is insufficient intropion is produced: 1) Atrophy or absence of eye ball 2) Old persons ( senile entropion) owing to absence of orbital fat. 3) Tight bandaging after surgical operation of the eye. 4) Blepharospasm Symptoms and signs – same as for trichiasis 100
 Involutional (senile) entropion • Redundancy of skin • weakness of lid retractors • resorption of orbital fat
Involutional (senile) entropion • Redundancy of skin • weakness of lid retractors • resorption of orbital fat
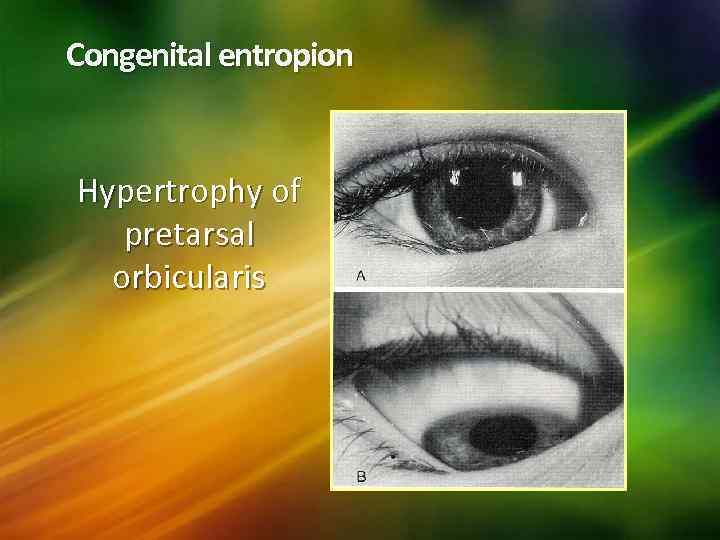 Congenital entropion Hypertrophy of pretarsal orbicularis
Congenital entropion Hypertrophy of pretarsal orbicularis
 Senile ectropion – the lower lid is affected in old age due to laxity of the tissue of the lid and due to loss of tone of the orbicularis muscle. 103
Senile ectropion – the lower lid is affected in old age due to laxity of the tissue of the lid and due to loss of tone of the orbicularis muscle. 103
 III. Paralytic ectropion – it occurs as a result of weakness of the orbicularis muscle due to facial nerve paralysis. The lower lid is affected. Symptoms – Epiphora due to eversion of lacrimal pucnta. Complications 1) Xerosis of conjunctiva 2) Chronic conjunctivitis and exposure keratitis particularly in Ectropion of upper lid. 104
III. Paralytic ectropion – it occurs as a result of weakness of the orbicularis muscle due to facial nerve paralysis. The lower lid is affected. Symptoms – Epiphora due to eversion of lacrimal pucnta. Complications 1) Xerosis of conjunctiva 2) Chronic conjunctivitis and exposure keratitis particularly in Ectropion of upper lid. 104
 Treatment: I) Cicatricial entrpion : 1) Altering the direction of eyelashes a) Snellen, s operation b) Jaesch Arlt operation 2) Straightening of the distorted tarsus. II) Spastic entropion 1) Pull the lower lid down and out and apply leucoplast which should extend below the mandible. 2) Injection of alcohol is made close to the lateral 3 rd of the lid margin. 3) Plastic surgery of lower lid - modified wheeler's operation 105
Treatment: I) Cicatricial entrpion : 1) Altering the direction of eyelashes a) Snellen, s operation b) Jaesch Arlt operation 2) Straightening of the distorted tarsus. II) Spastic entropion 1) Pull the lower lid down and out and apply leucoplast which should extend below the mandible. 2) Injection of alcohol is made close to the lateral 3 rd of the lid margin. 3) Plastic surgery of lower lid - modified wheeler's operation 105
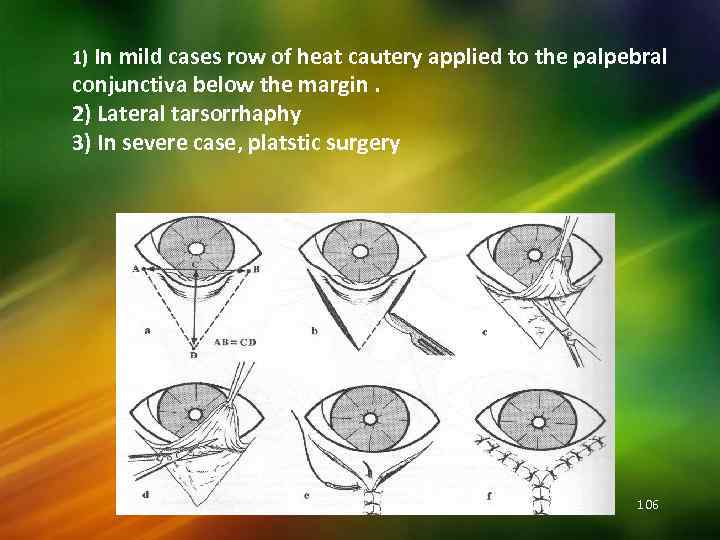 1) In mild cases row of heat cautery applied to the palpebral conjunctiva below the margin. 2) Lateral tarsorrhaphy 3) In severe case, platstic surgery 106
1) In mild cases row of heat cautery applied to the palpebral conjunctiva below the margin. 2) Lateral tarsorrhaphy 3) In severe case, platstic surgery 106
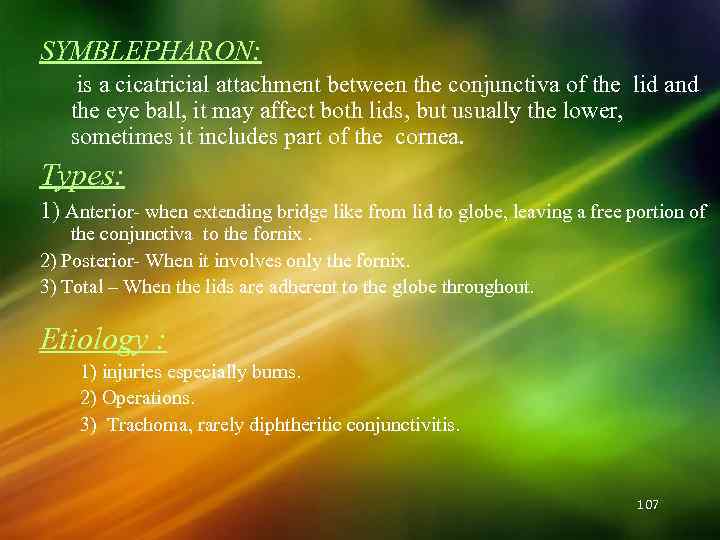 SYMBLEPHARON: is a cicatricial attachment between the conjunctiva of the lid and the eye ball, it may affect both lids, but usually the lower, sometimes it includes part of the cornea. Types: 1) Anterior- when extending bridge like from lid to globe, leaving a free portion of the conjunctiva to the fornix. 2) Posterior- When it involves only the fornix. 3) Total – When the lids are adherent to the globe throughout. Etiology : 1) injuries especially burns. 2) Operations. 3) Trachoma, rarely diphtheritic conjunctivitis. 107
SYMBLEPHARON: is a cicatricial attachment between the conjunctiva of the lid and the eye ball, it may affect both lids, but usually the lower, sometimes it includes part of the cornea. Types: 1) Anterior- when extending bridge like from lid to globe, leaving a free portion of the conjunctiva to the fornix. 2) Posterior- When it involves only the fornix. 3) Total – When the lids are adherent to the globe throughout. Etiology : 1) injuries especially burns. 2) Operations. 3) Trachoma, rarely diphtheritic conjunctivitis. 107
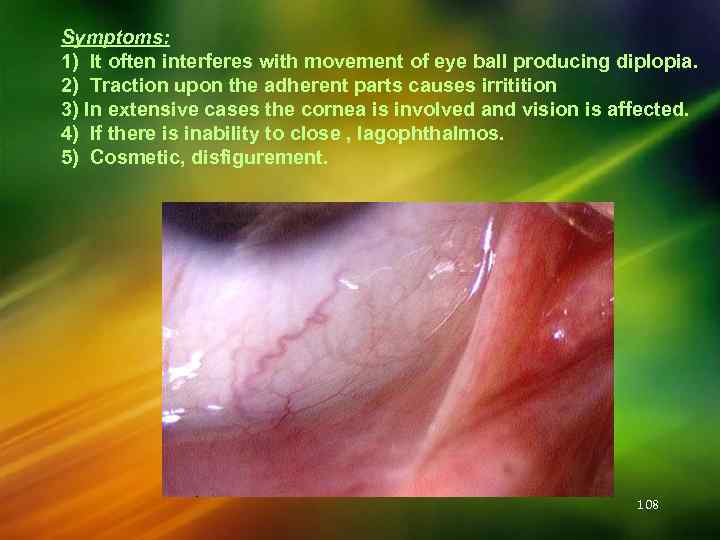 Symptoms: 1) It often interferes with movement of eye ball producing diplopia. 2) Traction upon the adherent parts causes irritition 3) In extensive cases the cornea is involved and vision is affected. 4) If there is inability to close , lagophthalmos. 5) Cosmetic, disfigurement. 108
Symptoms: 1) It often interferes with movement of eye ball producing diplopia. 2) Traction upon the adherent parts causes irritition 3) In extensive cases the cornea is involved and vision is affected. 4) If there is inability to close , lagophthalmos. 5) Cosmetic, disfigurement. 108
 Treatment: 1) Prophylactic - use of contact shell in fresh cases of alkal burns, after operations on lids. 2) Curative. a) If anterior and not extensive, the band is divided and the 2 raw surfaces kept from uniting by separating them daily with a glass rod smeared with antibiotic ointment. b) In more sever cases of anterior symblepharon, in posterior and total symblepharon the separated raw surfaces must be covered with conjunctiva or with grafts of mucous membrane from the lip to keep them from uniting. 109
Treatment: 1) Prophylactic - use of contact shell in fresh cases of alkal burns, after operations on lids. 2) Curative. a) If anterior and not extensive, the band is divided and the 2 raw surfaces kept from uniting by separating them daily with a glass rod smeared with antibiotic ointment. b) In more sever cases of anterior symblepharon, in posterior and total symblepharon the separated raw surfaces must be covered with conjunctiva or with grafts of mucous membrane from the lip to keep them from uniting. 109
 DIFFUSE EYELID DISEASE 1. Allergic • • Acute oedema Contact dermatitis Atopic dermatitis Blepharochalasis • • • Preseptal cellulitis Herpes simplex Herpes zoster ophthalmicus Impetigo Erysipelas Necrotizing fasciitis 2. Infections 3. Miscellaneous • Fat herniation • Systemic causes
DIFFUSE EYELID DISEASE 1. Allergic • • Acute oedema Contact dermatitis Atopic dermatitis Blepharochalasis • • • Preseptal cellulitis Herpes simplex Herpes zoster ophthalmicus Impetigo Erysipelas Necrotizing fasciitis 2. Infections 3. Miscellaneous • Fat herniation • Systemic causes
 Oedema of lids – this is common and owing to looseness of the tissue may be so great as to the eye. Causes: A. Inflammatory oedema. 1. 2. 3. 4. 5. 6. Inflammation of the lids – allergic dermatitis due to atropine ointment and cosmetics, stye, insect bite. Acute conjunctivitis. Acute dacryocystitis. Acute iridocyclitis. Panophthalmitis. Orbital cellulitis. B. Passive oederma due to circulatory obstruction. 1. 2. 3. clos Nephritic syndrome. Cardiac failure. Cavernous sinus thrombosis. 111
Oedema of lids – this is common and owing to looseness of the tissue may be so great as to the eye. Causes: A. Inflammatory oedema. 1. 2. 3. 4. 5. 6. Inflammation of the lids – allergic dermatitis due to atropine ointment and cosmetics, stye, insect bite. Acute conjunctivitis. Acute dacryocystitis. Acute iridocyclitis. Panophthalmitis. Orbital cellulitis. B. Passive oederma due to circulatory obstruction. 1. 2. 3. clos Nephritic syndrome. Cardiac failure. Cavernous sinus thrombosis. 111
 112
112
 Acute allergic oedema • Causes - insect bites, urticaria and angioedema • • Unilateral or bilateral Painless, red, pitting oedema Chemosis may be present Self-limiting
Acute allergic oedema • Causes - insect bites, urticaria and angioedema • • Unilateral or bilateral Painless, red, pitting oedema Chemosis may be present Self-limiting
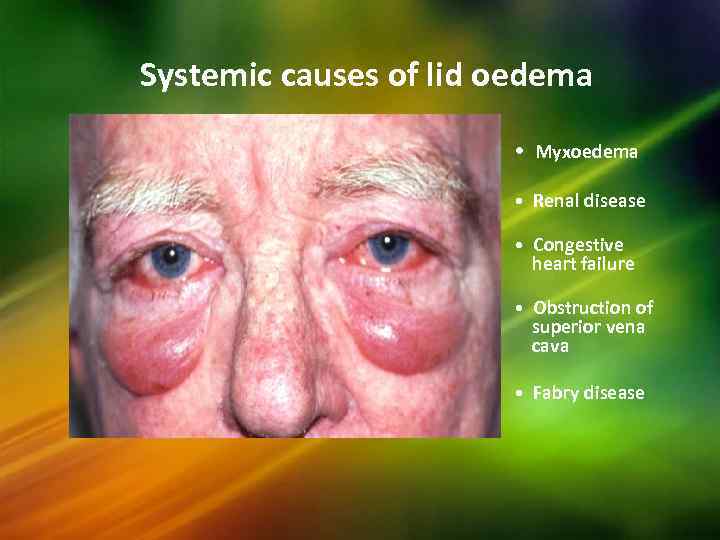 Systemic causes of lid oedema • Myxoedema • Renal disease • Congestive heart failure • Obstruction of superior vena cava • Fabry disease
Systemic causes of lid oedema • Myxoedema • Renal disease • Congestive heart failure • Obstruction of superior vena cava • Fabry disease
 Contact dermatitis • Sensitivity to topical medication • • Unilateral or bilateral Painless oedema and erythema Vesiculation and crusting Thickening if chronic
Contact dermatitis • Sensitivity to topical medication • • Unilateral or bilateral Painless oedema and erythema Vesiculation and crusting Thickening if chronic
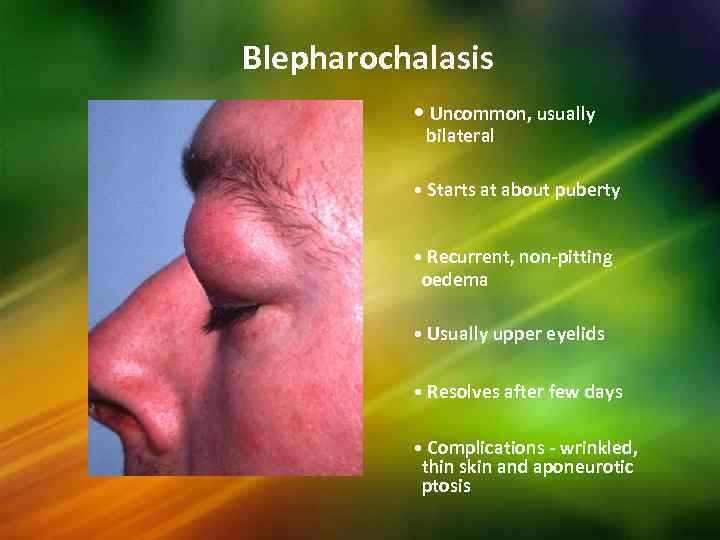 Blepharochalasis • Uncommon, usually bilateral • Starts at about puberty • Recurrent, non-pitting oedema • Usually upper eyelids • Resolves after few days • Complications - wrinkled, thin skin and aponeurotic ptosis
Blepharochalasis • Uncommon, usually bilateral • Starts at about puberty • Recurrent, non-pitting oedema • Usually upper eyelids • Resolves after few days • Complications - wrinkled, thin skin and aponeurotic ptosis
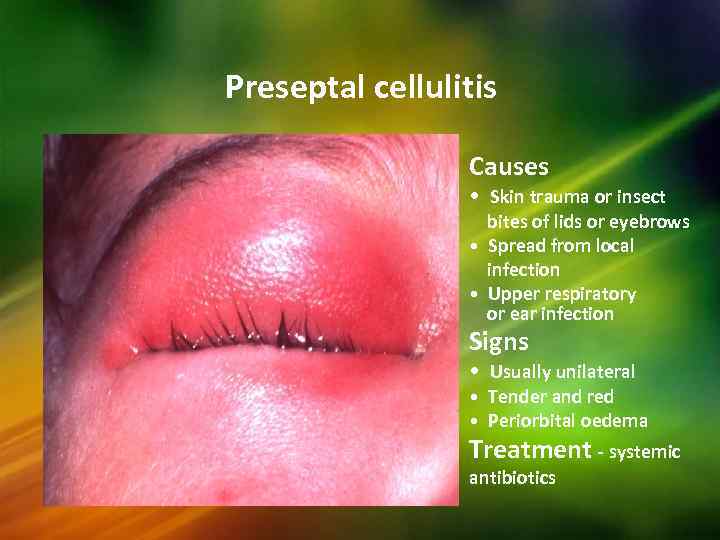 Preseptal cellulitis Causes • Skin trauma or insect bites of lids or eyebrows • Spread from local infection • Upper respiratory or ear infection Signs • Usually unilateral • Tender and red • Periorbital oedema Treatment - systemic antibiotics
Preseptal cellulitis Causes • Skin trauma or insect bites of lids or eyebrows • Spread from local infection • Upper respiratory or ear infection Signs • Usually unilateral • Tender and red • Periorbital oedema Treatment - systemic antibiotics
 Herpes simplex Signs • Crops of small vesicles • Rupture and crust • Heal without scarring after 7 days Complications • Follicular conjunctivitis • Keratitis Treatment - topical antivirals
Herpes simplex Signs • Crops of small vesicles • Rupture and crust • Heal without scarring after 7 days Complications • Follicular conjunctivitis • Keratitis Treatment - topical antivirals
 Herpes zoster ophthalmicus • Painful vesicles and pustules • Periorbital oedema - may be bilateral • Crusting ulceration Treatment - oral antivirals
Herpes zoster ophthalmicus • Painful vesicles and pustules • Periorbital oedema - may be bilateral • Crusting ulceration Treatment - oral antivirals
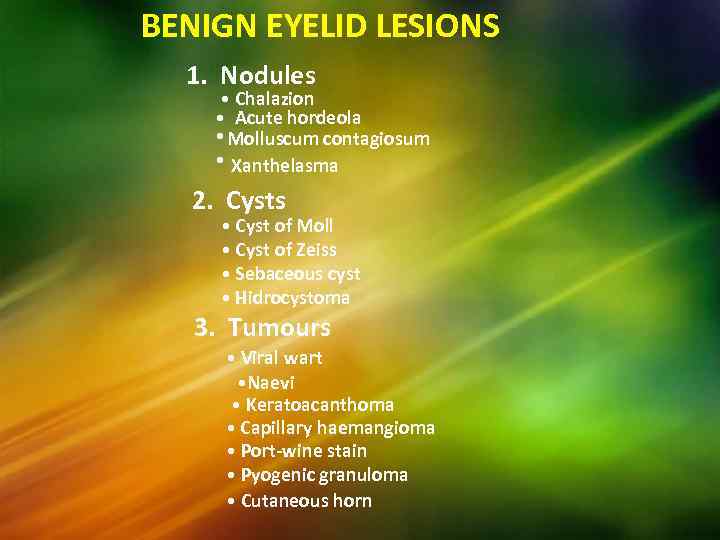 BENIGN EYELID LESIONS 1. Nodules • Chalazion • Acute hordeola • Molluscum contagiosum • Xanthelasma 2. Cysts • Cyst of Moll • Cyst of Zeiss • Sebaceous cyst • Hidrocystoma 3. Tumours • Viral wart • Naevi • Keratoacanthoma • Capillary haemangioma • Port-wine stain • Pyogenic granuloma • Cutaneous horn
BENIGN EYELID LESIONS 1. Nodules • Chalazion • Acute hordeola • Molluscum contagiosum • Xanthelasma 2. Cysts • Cyst of Moll • Cyst of Zeiss • Sebaceous cyst • Hidrocystoma 3. Tumours • Viral wart • Naevi • Keratoacanthoma • Capillary haemangioma • Port-wine stain • Pyogenic granuloma • Cutaneous horn
 INFLAMMATION OF THE GLANDS OF THE LIDS : 1) Eternal hordeolum or stye : is a circumscribed, acute inflammation at the edge of the lid, caused by staphylococcal infection of the glands of Zeis usually ending in suppuration. Etiology : Most common in children and young adults. Frequently associated with blepharitis or lowered state of health – diabetes mellitus, and uncorrected refractive error. 121
INFLAMMATION OF THE GLANDS OF THE LIDS : 1) Eternal hordeolum or stye : is a circumscribed, acute inflammation at the edge of the lid, caused by staphylococcal infection of the glands of Zeis usually ending in suppuration. Etiology : Most common in children and young adults. Frequently associated with blepharitis or lowered state of health – diabetes mellitus, and uncorrected refractive error. 121
 Stye: - pointing & related to lash follicle: Symptoms and Signs: Red swelling appears in the lash line of the margin of the lid, accompanied by pain, tenderness and often by considerable oedema of the lids. Very soon a yellowish summit will be seen order lid indicating suppuration.
Stye: - pointing & related to lash follicle: Symptoms and Signs: Red swelling appears in the lash line of the margin of the lid, accompanied by pain, tenderness and often by considerable oedema of the lids. Very soon a yellowish summit will be seen order lid indicating suppuration.
 Hordeolum internum : this is an acute suppurative inflammation of a meibomian gland due to staphylococcus. Sometimes it may be due to secondary infection of a chalazion. Symptoms are more violent than those of stye. Very soon pus points on the palpebral conjunctiva. 123
Hordeolum internum : this is an acute suppurative inflammation of a meibomian gland due to staphylococcus. Sometimes it may be due to secondary infection of a chalazion. Symptoms are more violent than those of stye. Very soon pus points on the palpebral conjunctiva. 123
 Treatment : 1. Hot fomentation to hasten suppuration : as soon as a yellow spot is seen, the pus should be evacuated. 2. Antibiotics – choromycetin ointment. 3. Analgesics. 4. Prophylaxis. 5. Antibiotic ointment. 6. Treatment of diabetes, blepharitis, correction of refractive errors. 7. Avoidance of excess of sweets, oil in the diet. 124
Treatment : 1. Hot fomentation to hasten suppuration : as soon as a yellow spot is seen, the pus should be evacuated. 2. Antibiotics – choromycetin ointment. 3. Analgesics. 4. Prophylaxis. 5. Antibiotic ointment. 6. Treatment of diabetes, blepharitis, correction of refractive errors. 7. Avoidance of excess of sweets, oil in the diet. 124
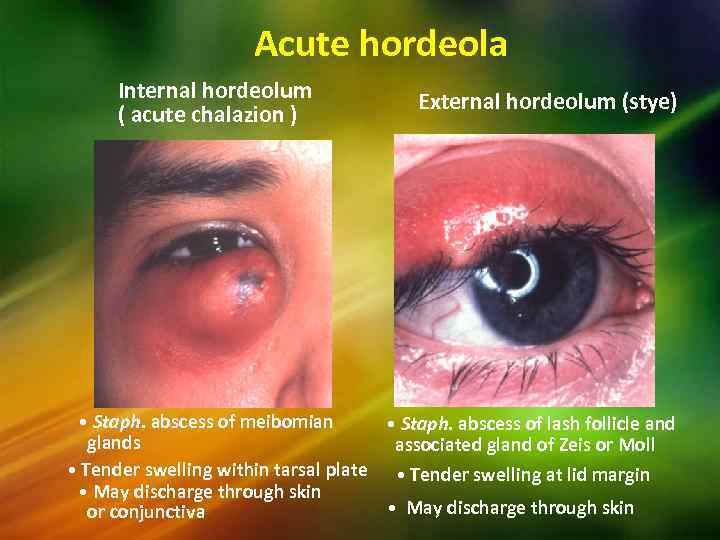 Acute hordeola Internal hordeolum ( acute chalazion ) External hordeolum (stye) • Staph. abscess of meibomian • Staph. abscess of lash follicle and glands associated gland of Zeis or Moll • Tender swelling within tarsal plate • Tender swelling at lid margin • May discharge through skin or conjunctiva
Acute hordeola Internal hordeolum ( acute chalazion ) External hordeolum (stye) • Staph. abscess of meibomian • Staph. abscess of lash follicle and glands associated gland of Zeis or Moll • Tender swelling within tarsal plate • Tender swelling at lid margin • May discharge through skin or conjunctiva
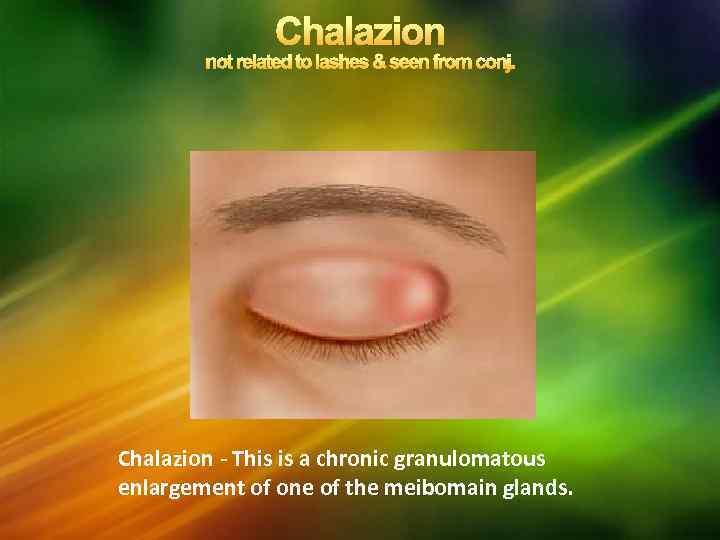 Chalazion - This is a chronic granulomatous enlargement of one of the meibomain glands.
Chalazion - This is a chronic granulomatous enlargement of one of the meibomain glands.
 Etiology & Pathology : It occurs most frequently in adults. The meibomian duct becomes obstructed through proliferation of its epithelium and consequently the gland enlarges. The fatty secretion escapes into the surrounding tissue and excites a foreign body reaction (lipogranuloma) which consists of lymphocytes, epitheloid cells and giant cells. The blood supply is cut off by the surrounding fibrous tissue leading to degeneration of contents – jelly like mass. 127
Etiology & Pathology : It occurs most frequently in adults. The meibomian duct becomes obstructed through proliferation of its epithelium and consequently the gland enlarges. The fatty secretion escapes into the surrounding tissue and excites a foreign body reaction (lipogranuloma) which consists of lymphocytes, epitheloid cells and giant cells. The blood supply is cut off by the surrounding fibrous tissue leading to degeneration of contents – jelly like mass. 127
 Chalazion 128
Chalazion 128
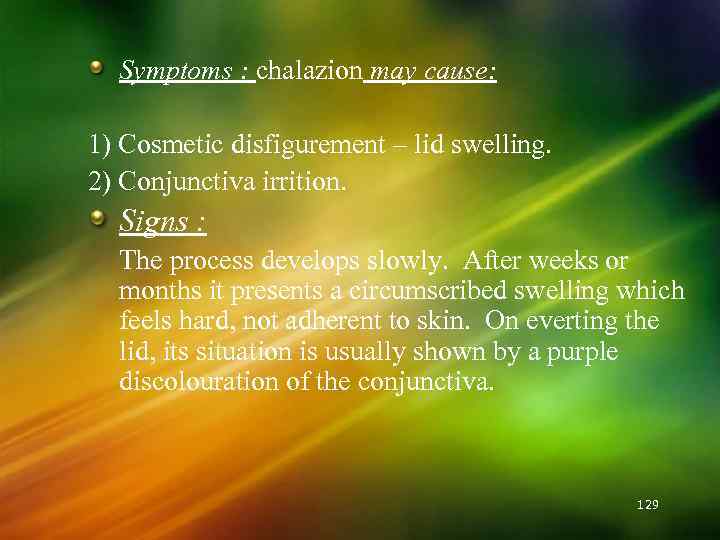 Symptoms : chalazion may cause: 1) Cosmetic disfigurement – lid swelling. 2) Conjunctiva irrition. Signs : The process develops slowly. After weeks or months it presents a circumscribed swelling which feels hard, not adherent to skin. On everting the lid, its situation is usually shown by a purple discolouration of the conjunctiva. 129
Symptoms : chalazion may cause: 1) Cosmetic disfigurement – lid swelling. 2) Conjunctiva irrition. Signs : The process develops slowly. After weeks or months it presents a circumscribed swelling which feels hard, not adherent to skin. On everting the lid, its situation is usually shown by a purple discolouration of the conjunctiva. 129
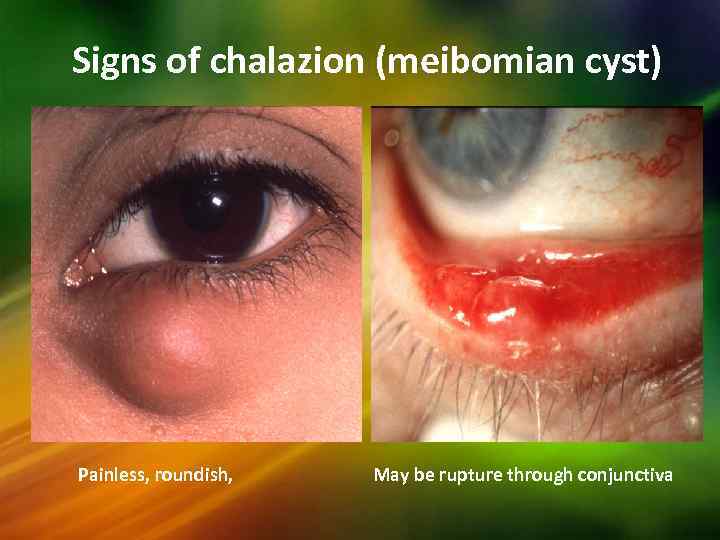 Signs of chalazion (meibomian cyst) Painless, roundish, May be rupture through conjunctiva
Signs of chalazion (meibomian cyst) Painless, roundish, May be rupture through conjunctiva
 Complications: 1. It may be secondarily infected forming an internal hordeolum. 2. In old people, recurrent chalazion may lead to the development of Meibomian gland carcinoma. 3. Mechanical ptosis in cases of large chalazion. 4. The chalazion may press on the cornea causing astigmatism. 5. The chalazion may burst either on the skin surface or on the conjunctival surface, with granulation tissue protruding. 6. The granuloma may protrude through a duct of the meibomian gland on the lid margin – marginal chalazion. 131
Complications: 1. It may be secondarily infected forming an internal hordeolum. 2. In old people, recurrent chalazion may lead to the development of Meibomian gland carcinoma. 3. Mechanical ptosis in cases of large chalazion. 4. The chalazion may press on the cornea causing astigmatism. 5. The chalazion may burst either on the skin surface or on the conjunctival surface, with granulation tissue protruding. 6. The granuloma may protrude through a duct of the meibomian gland on the lid margin – marginal chalazion. 131
 Treatment : 1. It may be removed by operation – incision and curettage through the conjunctiva. 2. Injection of cortisone into the chalazion can be used as an alternate from of treatment. 132
Treatment : 1. It may be removed by operation – incision and curettage through the conjunctiva. 2. Injection of cortisone into the chalazion can be used as an alternate from of treatment. 132
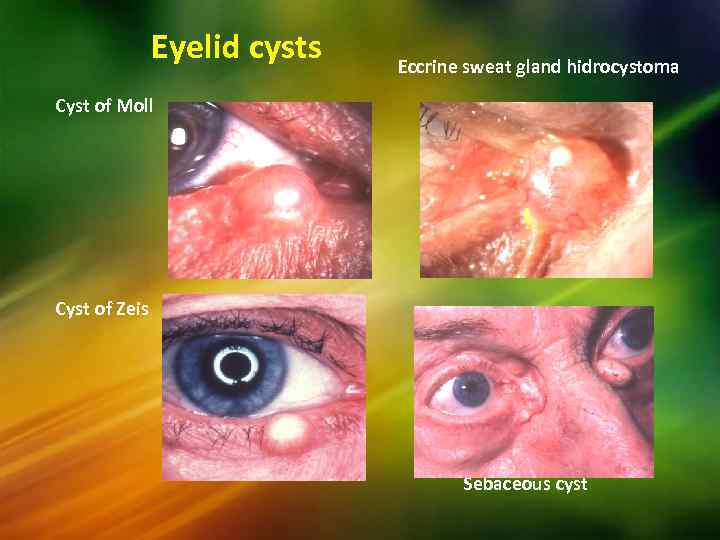 Eyelid cysts Eccrine sweat gland hidrocystoma Cyst of Moll Cyst of Zeis Sebaceous cyst
Eyelid cysts Eccrine sweat gland hidrocystoma Cyst of Moll Cyst of Zeis Sebaceous cyst
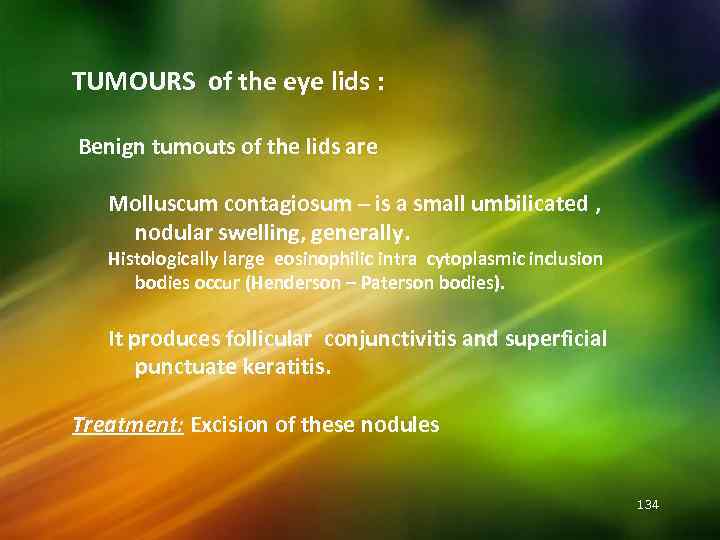 TUMOURS of the eye lids : Benign tumouts of the lids are Molluscum contagiosum – is a small umbilicated , nodular swelling, generally. Histologically large eosinophilic intra cytoplasmic inclusion bodies occur (Henderson – Paterson bodies). It produces follicular conjunctivitis and superficial punctuate keratitis. Treatment: Excision of these nodules 134
TUMOURS of the eye lids : Benign tumouts of the lids are Molluscum contagiosum – is a small umbilicated , nodular swelling, generally. Histologically large eosinophilic intra cytoplasmic inclusion bodies occur (Henderson – Paterson bodies). It produces follicular conjunctivitis and superficial punctuate keratitis. Treatment: Excision of these nodules 134
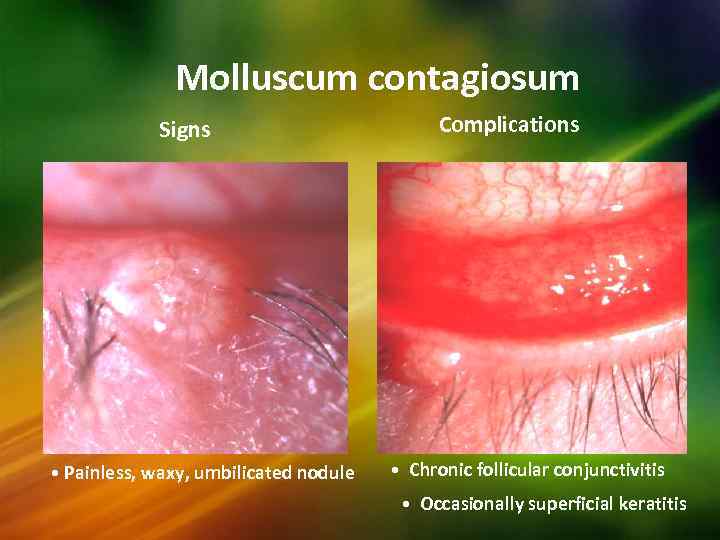 Molluscum contagiosum Signs • Painless, waxy, umbilicated nodule Complications • Chronic follicular conjunctivitis • Occasionally superficial keratitis
Molluscum contagiosum Signs • Painless, waxy, umbilicated nodule Complications • Chronic follicular conjunctivitis • Occasionally superficial keratitis
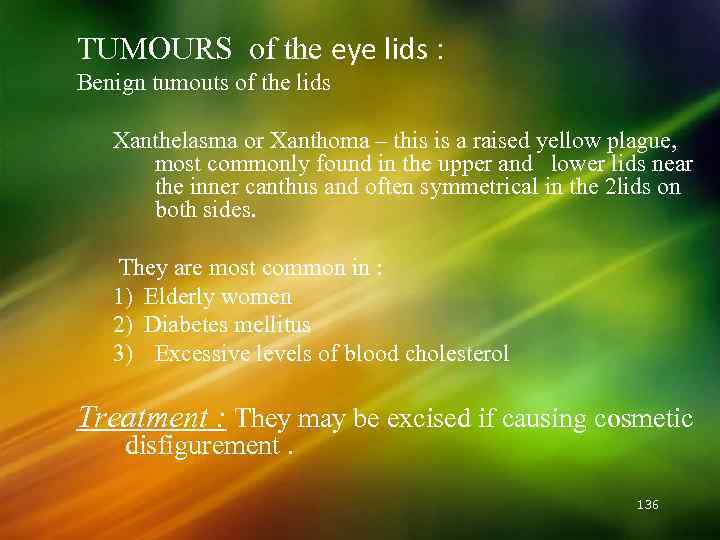 TUMOURS of the eye lids : Benign tumouts of the lids Xanthelasma or Xanthoma – this is a raised yellow plague, most commonly found in the upper and lower lids near the inner canthus and often symmetrical in the 2 lids on both sides. They are most common in : 1) Elderly women 2) Diabetes mellitus 3) Excessive levels of blood cholesterol Treatment : They may be excised if causing cosmetic disfigurement. 136
TUMOURS of the eye lids : Benign tumouts of the lids Xanthelasma or Xanthoma – this is a raised yellow plague, most commonly found in the upper and lower lids near the inner canthus and often symmetrical in the 2 lids on both sides. They are most common in : 1) Elderly women 2) Diabetes mellitus 3) Excessive levels of blood cholesterol Treatment : They may be excised if causing cosmetic disfigurement. 136
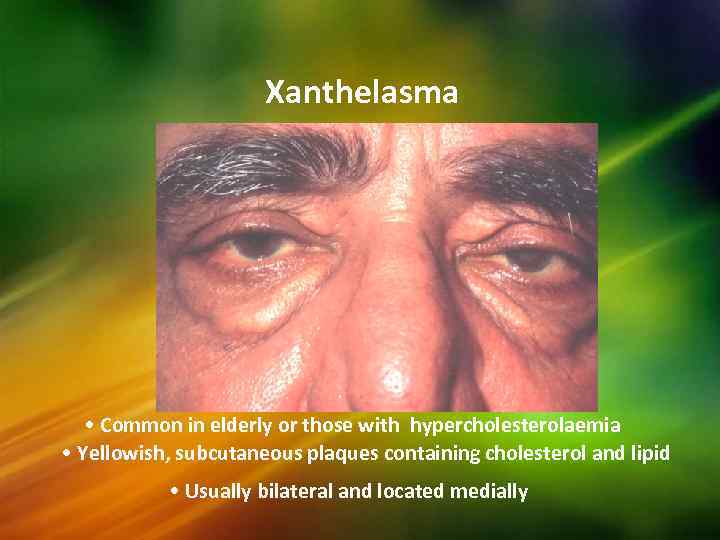 Xanthelasma • Common in elderly or those with hypercholesterolaemia • Yellowish, subcutaneous plaques containing cholesterol and lipid • Usually bilateral and located medially
Xanthelasma • Common in elderly or those with hypercholesterolaemia • Yellowish, subcutaneous plaques containing cholesterol and lipid • Usually bilateral and located medially
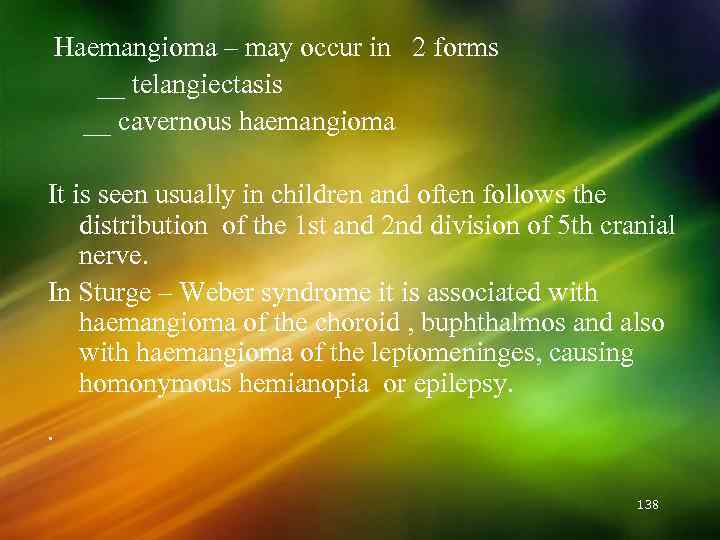 Haemangioma – may occur in 2 forms __ telangiectasis __ cavernous haemangioma It is seen usually in children and often follows the distribution of the 1 st and 2 nd division of 5 th cranial nerve. In Sturge – Weber syndrome it is associated with haemangioma of the choroid , buphthalmos and also with haemangioma of the leptomeninges, causing homonymous hemianopia or epilepsy. . 138
Haemangioma – may occur in 2 forms __ telangiectasis __ cavernous haemangioma It is seen usually in children and often follows the distribution of the 1 st and 2 nd division of 5 th cranial nerve. In Sturge – Weber syndrome it is associated with haemangioma of the choroid , buphthalmos and also with haemangioma of the leptomeninges, causing homonymous hemianopia or epilepsy. . 138
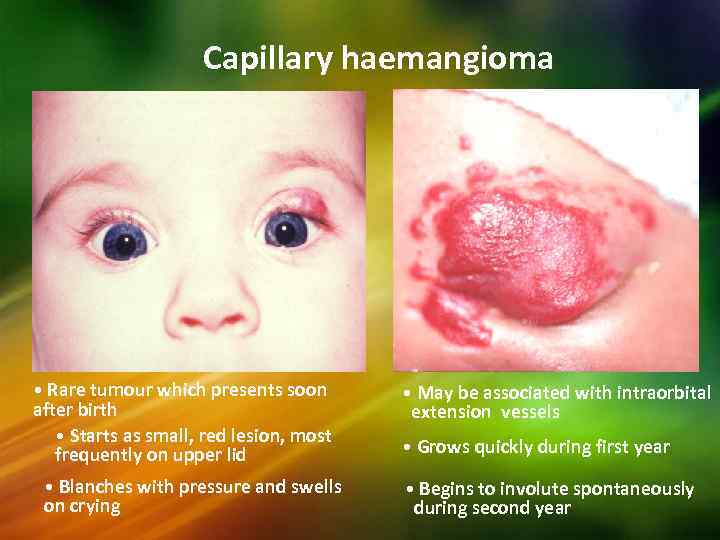 Capillary haemangioma • Rare tumour which presents soon after birth • Starts as small, red lesion, most frequently on upper lid • Blanches with pressure and swells on crying • May be associated with intraorbital extension vessels • Grows quickly during first year • Begins to involute spontaneously during second year
Capillary haemangioma • Rare tumour which presents soon after birth • Starts as small, red lesion, most frequently on upper lid • Blanches with pressure and swells on crying • May be associated with intraorbital extension vessels • Grows quickly during first year • Begins to involute spontaneously during second year
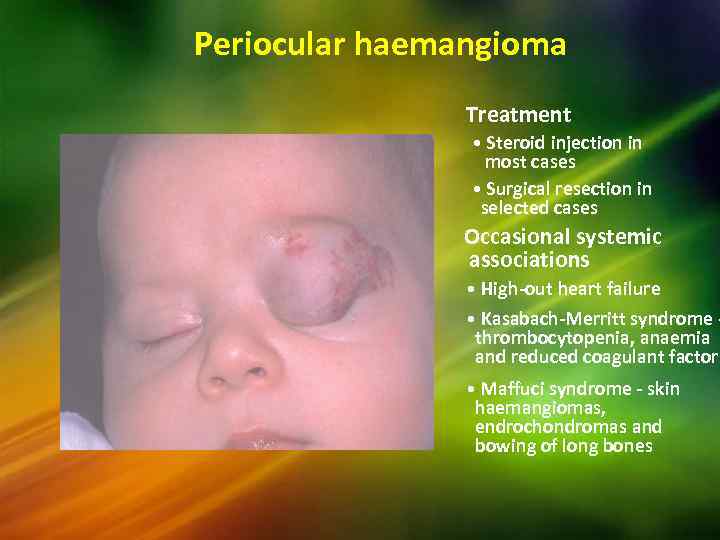 Periocular haemangioma Treatment • Steroid injection in most cases • Surgical resection in selected cases Occasional systemic associations • High-out heart failure • Kasabach-Merritt syndrome thrombocytopenia, anaemia and reduced coagulant factors • Maffuci syndrome - skin haemangiomas, endrochondromas and bowing of long bones
Periocular haemangioma Treatment • Steroid injection in most cases • Surgical resection in selected cases Occasional systemic associations • High-out heart failure • Kasabach-Merritt syndrome thrombocytopenia, anaemia and reduced coagulant factors • Maffuci syndrome - skin haemangiomas, endrochondromas and bowing of long bones
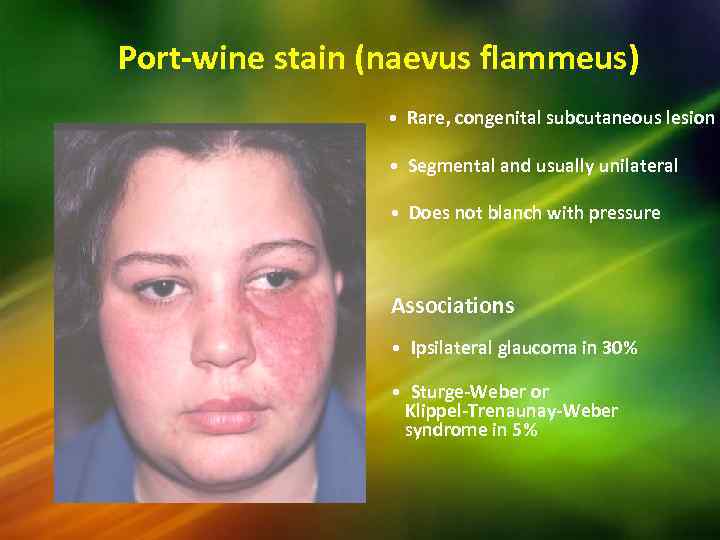 Port-wine stain (naevus flammeus) • Rare, congenital subcutaneous lesion • Segmental and usually unilateral • Does not blanch with pressure Associations • Ipsilateral glaucoma in 30% • Sturge-Weber or Klippel-Trenaunay-Weber syndrome in 5%
Port-wine stain (naevus flammeus) • Rare, congenital subcutaneous lesion • Segmental and usually unilateral • Does not blanch with pressure Associations • Ipsilateral glaucoma in 30% • Sturge-Weber or Klippel-Trenaunay-Weber syndrome in 5%
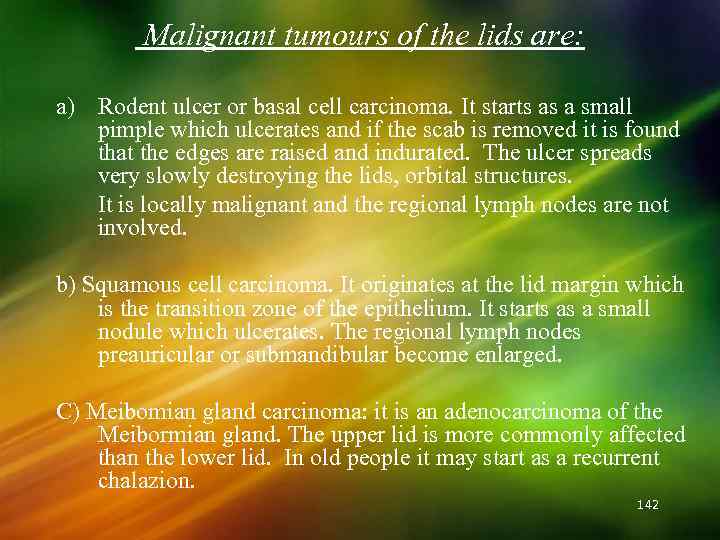 Malignant tumours of the lids are: a) Rodent ulcer or basal cell carcinoma. It starts as a small pimple which ulcerates and if the scab is removed it is found that the edges are raised and indurated. The ulcer spreads very slowly destroying the lids, orbital structures. It is locally malignant and the regional lymph nodes are not involved. b) Squamous cell carcinoma. It originates at the lid margin which is the transition zone of the epithelium. It starts as a small nodule which ulcerates. The regional lymph nodes preauricular or submandibular become enlarged. C) Meibomian gland carcinoma: it is an adenocarcinoma of the Meibormian gland. The upper lid is more commonly affected than the lower lid. In old people it may start as a recurrent chalazion. 142
Malignant tumours of the lids are: a) Rodent ulcer or basal cell carcinoma. It starts as a small pimple which ulcerates and if the scab is removed it is found that the edges are raised and indurated. The ulcer spreads very slowly destroying the lids, orbital structures. It is locally malignant and the regional lymph nodes are not involved. b) Squamous cell carcinoma. It originates at the lid margin which is the transition zone of the epithelium. It starts as a small nodule which ulcerates. The regional lymph nodes preauricular or submandibular become enlarged. C) Meibomian gland carcinoma: it is an adenocarcinoma of the Meibormian gland. The upper lid is more commonly affected than the lower lid. In old people it may start as a recurrent chalazion. 142
 Keratoacanthoma • Uncommon, fast growing nodule • Acquires rolled edges and keratin-filled crater • Involutes spontaneously within 1 year • Lesion above surface epithelium
Keratoacanthoma • Uncommon, fast growing nodule • Acquires rolled edges and keratin-filled crater • Involutes spontaneously within 1 year • Lesion above surface epithelium
 Naevi • Tend to become more pigmented at puberty Intradermal • Elevated Junctional • Flat, well-circumscribed • May be non-pigmented • Pigmented • No malignant potential • Low malignant potential Compound • Has both intradermal and junctional components
Naevi • Tend to become more pigmented at puberty Intradermal • Elevated Junctional • Flat, well-circumscribed • May be non-pigmented • Pigmented • No malignant potential • Low malignant potential Compound • Has both intradermal and junctional components
 Abnormal lid positions • Coloboma • Epicanthus • Blepharophimosis syndrome • PTOSIS
Abnormal lid positions • Coloboma • Epicanthus • Blepharophimosis syndrome • PTOSIS
 Coloboma of the lid: It is a triangular gap in the lid magin, generally affecting the upper lid. It may form part of Golden Har's syndrome- accessory auricles, dermolipoma at the limbus, hypoplasia of the maxilla and anomalies of the vertebral column. Ptosis or blepharoptosis : is a drooping of the upper lid usually due to defective development or paralysis of the levator palpebrae superioris (L. P. S. ). All degrees o ptosis occur- partial or complete. When severe it interferes with vision by covering the pupil. 146
Coloboma of the lid: It is a triangular gap in the lid magin, generally affecting the upper lid. It may form part of Golden Har's syndrome- accessory auricles, dermolipoma at the limbus, hypoplasia of the maxilla and anomalies of the vertebral column. Ptosis or blepharoptosis : is a drooping of the upper lid usually due to defective development or paralysis of the levator palpebrae superioris (L. P. S. ). All degrees o ptosis occur- partial or complete. When severe it interferes with vision by covering the pupil. 146

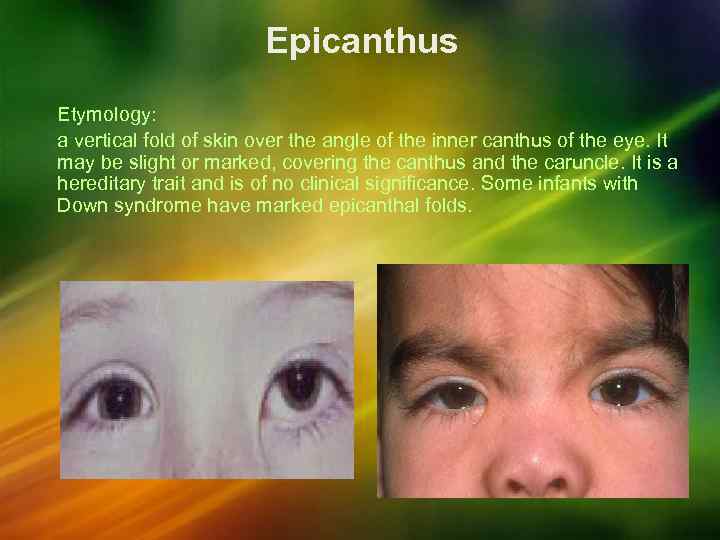 Epicanthus Etymology: a vertical fold of skin over the angle of the inner canthus of the eye. It may be slight or marked, covering the canthus and the caruncle. It is a hereditary trait and is of no clinical significance. Some infants with Down syndrome have marked epicanthal folds.
Epicanthus Etymology: a vertical fold of skin over the angle of the inner canthus of the eye. It may be slight or marked, covering the canthus and the caruncle. It is a hereditary trait and is of no clinical significance. Some infants with Down syndrome have marked epicanthal folds.
 Blepharophimosis syndrome 149
Blepharophimosis syndrome 149
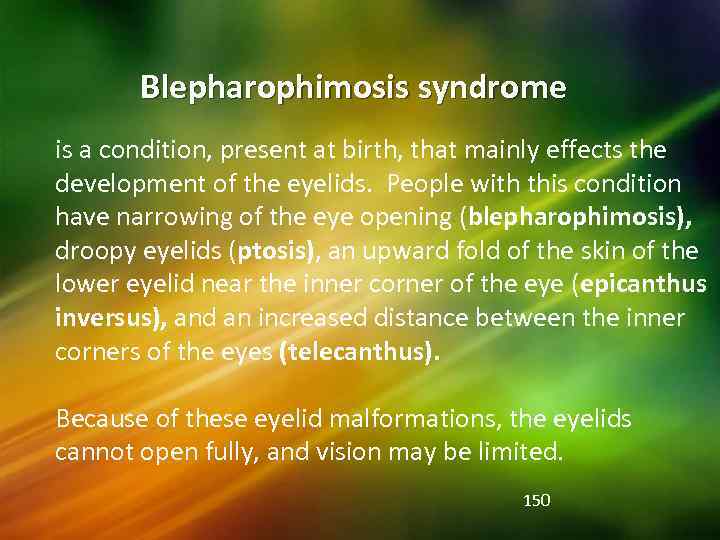 Blepharophimosis syndrome is a condition, present at birth, that mainly effects the development of the eyelids. People with this condition have narrowing of the eye opening (blepharophimosis), droopy eyelids (ptosis), an upward fold of the skin of the lower eyelid near the inner corner of the eye (epicanthus inversus), and an increased distance between the inner corners of the eyes (telecanthus). Because of these eyelid malformations, the eyelids cannot open fully, and vision may be limited. 150
Blepharophimosis syndrome is a condition, present at birth, that mainly effects the development of the eyelids. People with this condition have narrowing of the eye opening (blepharophimosis), droopy eyelids (ptosis), an upward fold of the skin of the lower eyelid near the inner corner of the eye (epicanthus inversus), and an increased distance between the inner corners of the eyes (telecanthus). Because of these eyelid malformations, the eyelids cannot open fully, and vision may be limited. 150
 CLASSIFICATION OF PTOSIS 1. Neurogenic • Third nerve palsy • Third nerve misdirection • Horner syndrome • Marcus Gunn jaw-winking syndrome 2. Myogenic • Myasthenia gravis • Myotonic dystrophy • Ocular myopathies • Simple congenital • Blepharophimosis syndrome 3. Aponeurotic 4. Mechanical 151
CLASSIFICATION OF PTOSIS 1. Neurogenic • Third nerve palsy • Third nerve misdirection • Horner syndrome • Marcus Gunn jaw-winking syndrome 2. Myogenic • Myasthenia gravis • Myotonic dystrophy • Ocular myopathies • Simple congenital • Blepharophimosis syndrome 3. Aponeurotic 4. Mechanical 151
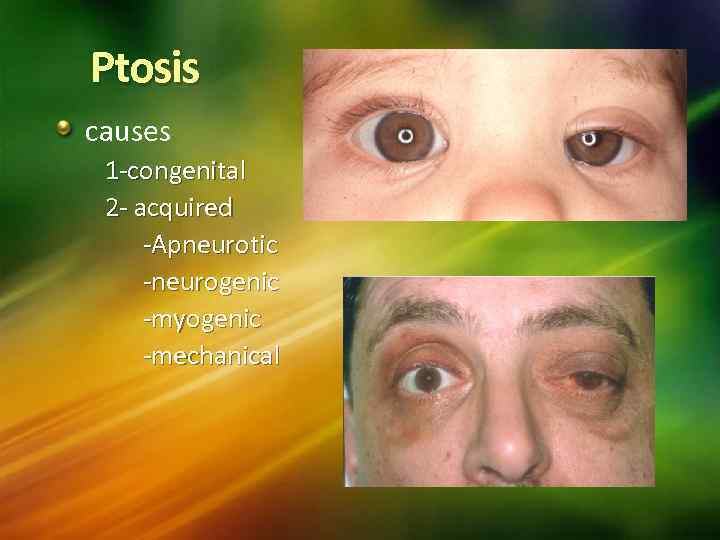 Ptosis causes 1 -congenital 2 - acquired -Apneurotic -neurogenic -myogenic -mechanical
Ptosis causes 1 -congenital 2 - acquired -Apneurotic -neurogenic -myogenic -mechanical
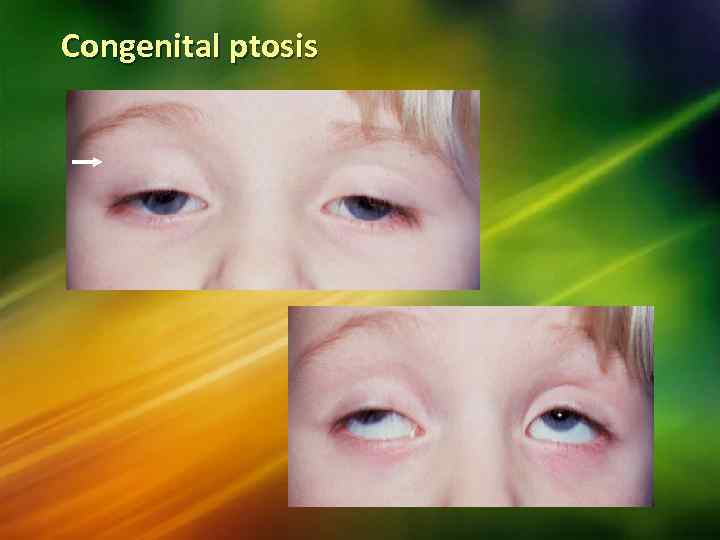 Congenital ptosis
Congenital ptosis
 Etiology & Classification: 1) Congenital ptosis: a) With normal superior rectus function. b) With superior rectus weakness- developmentally superior rectus is closely related to L. P. S. c) Marcus Gunn or jaw-winking ptosis.
Etiology & Classification: 1) Congenital ptosis: a) With normal superior rectus function. b) With superior rectus weakness- developmentally superior rectus is closely related to L. P. S. c) Marcus Gunn or jaw-winking ptosis.
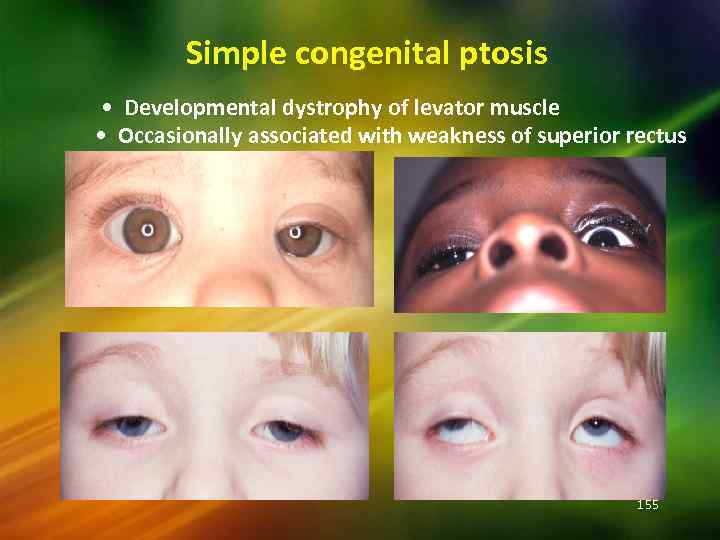 Simple congenital ptosis • Developmental dystrophy of levator muscle • Occasionally associated with weakness of superior rectus 155
Simple congenital ptosis • Developmental dystrophy of levator muscle • Occasionally associated with weakness of superior rectus 155
 2) Acquired ptosis: a) Aponeurotic ptosis (senile or age-related ptosis) b) Neurogenic – due to lesion of 3 rd never nucleus, 3 rd nerve trunk in its intracranial or orbital course as in cases of brain tumour, meningitis, aneurysm etc. Horner's syndrome due to affection of sympathetic nerves. c) Myogenic – Myasthenia gravis. d) Mechanical ptosis - due to increased weight of lid as in trachomatous ptosis, tylosis , tumours of upper lid or lack of support of upper lid as phthisis bulbi etc. e) Traumatic ptosis. 156
2) Acquired ptosis: a) Aponeurotic ptosis (senile or age-related ptosis) b) Neurogenic – due to lesion of 3 rd never nucleus, 3 rd nerve trunk in its intracranial or orbital course as in cases of brain tumour, meningitis, aneurysm etc. Horner's syndrome due to affection of sympathetic nerves. c) Myogenic – Myasthenia gravis. d) Mechanical ptosis - due to increased weight of lid as in trachomatous ptosis, tylosis , tumours of upper lid or lack of support of upper lid as phthisis bulbi etc. e) Traumatic ptosis. 156
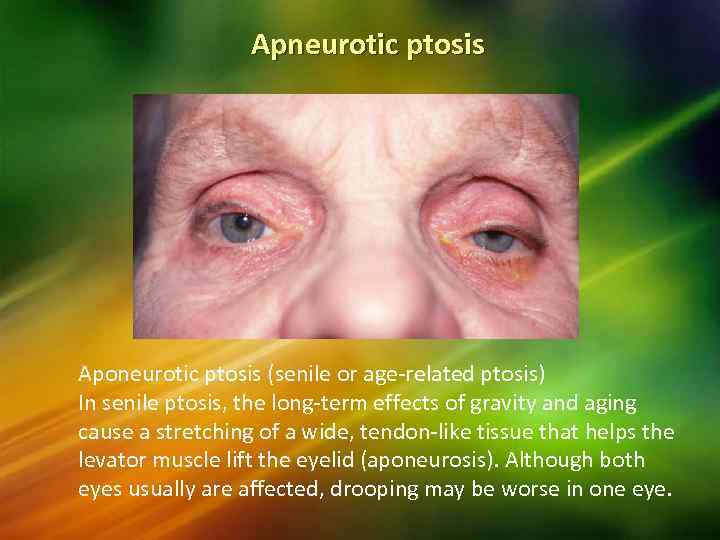 Apneurotic ptosis Aponeurotic ptosis (senile or age-related ptosis) In senile ptosis, the long-term effects of gravity and aging cause a stretching of a wide, tendon-like tissue that helps the levator muscle lift the eyelid (aponeurosis). Although both eyes usually are affected, drooping may be worse in one eye.
Apneurotic ptosis Aponeurotic ptosis (senile or age-related ptosis) In senile ptosis, the long-term effects of gravity and aging cause a stretching of a wide, tendon-like tissue that helps the levator muscle lift the eyelid (aponeurosis). Although both eyes usually are affected, drooping may be worse in one eye.
 Dermatochalasisexcessive eyelid skin
Dermatochalasisexcessive eyelid skin
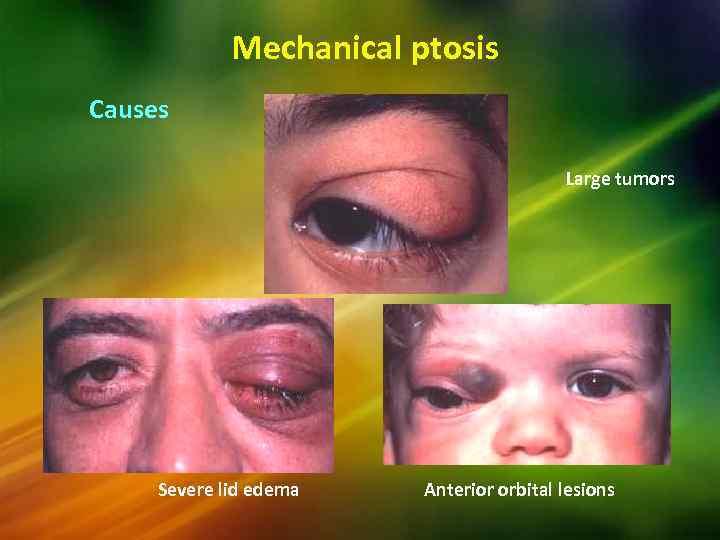 Mechanical ptosis Causes Large tumors Severe lid edema Anterior orbital lesions
Mechanical ptosis Causes Large tumors Severe lid edema Anterior orbital lesions
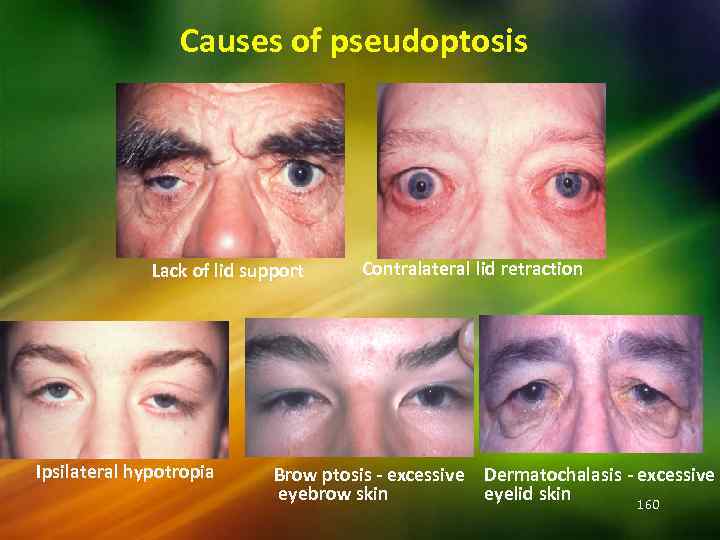 Causes of pseudoptosis Lack of lid support Ipsilateral hypotropia Contralateral lid retraction Brow ptosis - excessive Dermatochalasis - excessive eyebrow skin eyelid skin 160
Causes of pseudoptosis Lack of lid support Ipsilateral hypotropia Contralateral lid retraction Brow ptosis - excessive Dermatochalasis - excessive eyebrow skin eyelid skin 160
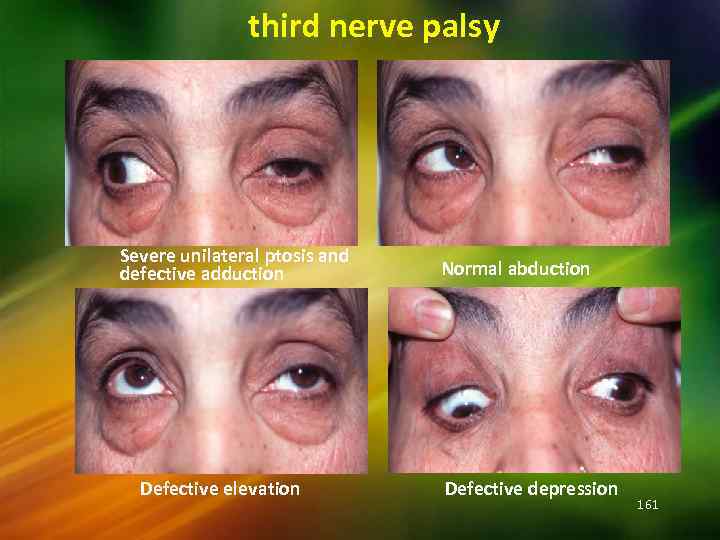 third nerve palsy Severe unilateral ptosis and defective adduction Defective elevation Normal abduction Defective depression 161
third nerve palsy Severe unilateral ptosis and defective adduction Defective elevation Normal abduction Defective depression 161
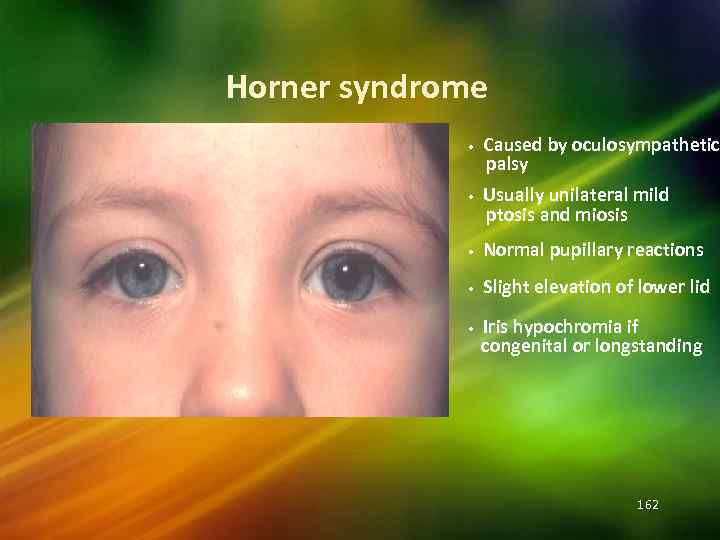 Horner syndrome • • Caused by oculosympathetic palsy Usually unilateral mild ptosis and miosis • Normal pupillary reactions • Slight elevation of lower lid • Iris hypochromia if congenital or longstanding 162
Horner syndrome • • Caused by oculosympathetic palsy Usually unilateral mild ptosis and miosis • Normal pupillary reactions • Slight elevation of lower lid • Iris hypochromia if congenital or longstanding 162
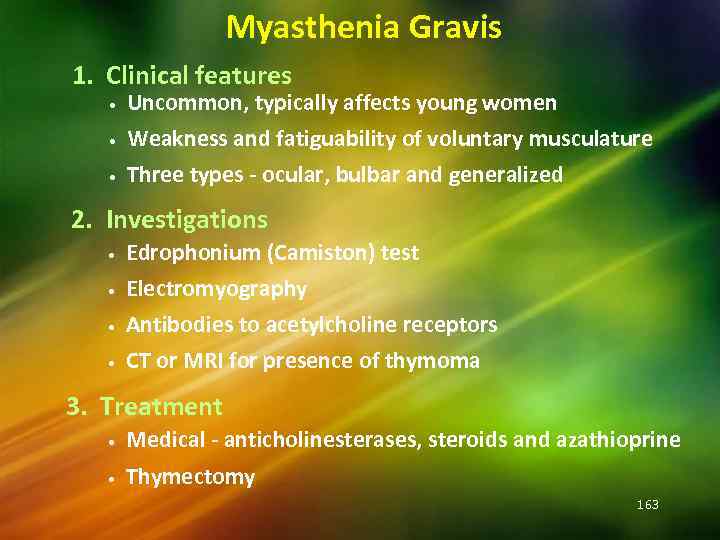 Myasthenia Gravis 1. Clinical features • Uncommon, typically affects young women Weakness and fatiguability of voluntary musculature • Three types - ocular, bulbar and generalized • 2. Investigations • • Edrophonium (Camiston) test Electromyography Antibodies to acetylcholine receptors CT or MRI for presence of thymoma 3. Treatment • Medical - anticholinesterases, steroids and azathioprine • Thymectomy 163
Myasthenia Gravis 1. Clinical features • Uncommon, typically affects young women Weakness and fatiguability of voluntary musculature • Three types - ocular, bulbar and generalized • 2. Investigations • • Edrophonium (Camiston) test Electromyography Antibodies to acetylcholine receptors CT or MRI for presence of thymoma 3. Treatment • Medical - anticholinesterases, steroids and azathioprine • Thymectomy 163
 Treatment: 1) Medical : in the acquired form cause is determined and treated – Syphilis – Inj. Penicillin I. M. – Myashthenia gravis _ Physostigmine 2) Surgical – usually necessary for Congenital ptosis. 164
Treatment: 1) Medical : in the acquired form cause is determined and treated – Syphilis – Inj. Penicillin I. M. – Myashthenia gravis _ Physostigmine 2) Surgical – usually necessary for Congenital ptosis. 164
 Examination Ocular motility pupil degree of ptosis degree of levator function
Examination Ocular motility pupil degree of ptosis degree of levator function
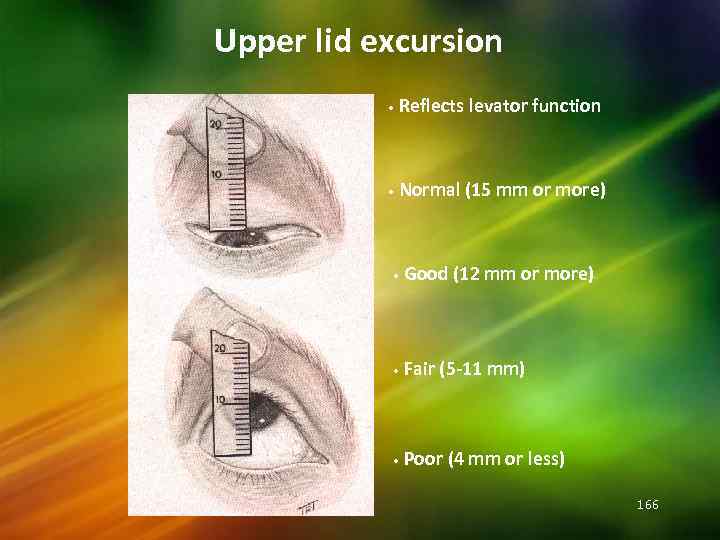 Upper lid excursion • Reflects levator function • Normal (15 mm or more) • Good (12 mm or more) • Fair (5 -11 mm) • Poor (4 mm or less) 166
Upper lid excursion • Reflects levator function • Normal (15 mm or more) • Good (12 mm or more) • Fair (5 -11 mm) • Poor (4 mm or less) 166
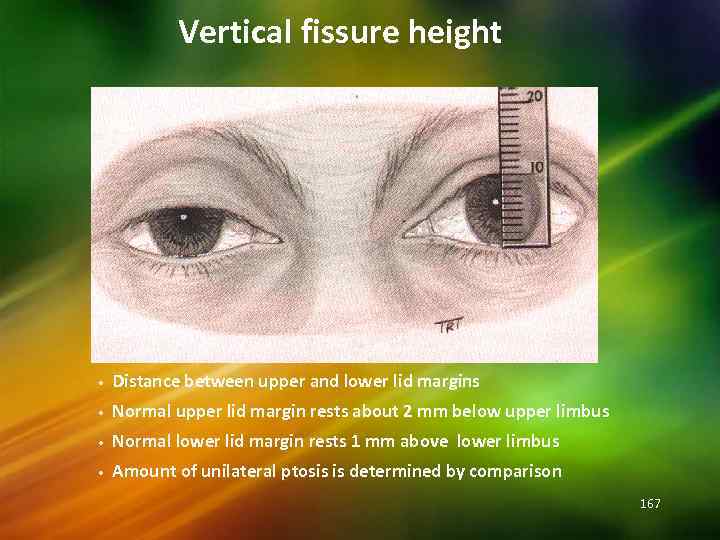 Vertical fissure height • Distance between upper and lower lid margins • Normal upper lid margin rests about 2 mm below upper limbus • Normal lower lid margin rests 1 mm above lower limbus • Amount of unilateral ptosis is determined by comparison 167
Vertical fissure height • Distance between upper and lower lid margins • Normal upper lid margin rests about 2 mm below upper limbus • Normal lower lid margin rests 1 mm above lower limbus • Amount of unilateral ptosis is determined by comparison 167
 Marginal reflex distance • Distance between upper lid margin and light reflex (MRD) • Mild ptosis (2 mm of droop) • Moderate ptosis (3 mm) • Severe ptosis (4 mm or more) 168
Marginal reflex distance • Distance between upper lid margin and light reflex (MRD) • Mild ptosis (2 mm of droop) • Moderate ptosis (3 mm) • Severe ptosis (4 mm or more) 168
 Lagophthalmos Definition: inability to close the palpebral fissure 169
Lagophthalmos Definition: inability to close the palpebral fissure 169
 Lagophthalmos: This is the condition of incomplete closure of the palpebral aperture when an attempt is made to shut the eyes. Causes: 1) Exophthalomos as in Graves' disease, proptosis due to orbital tumour. 2) Facial never paralysis. 3) Cicatricial ectropion of upper lid. 4) Symblepharon. 5) Laxity of the tissue and absence of reflex blinking in people who are extremely ill – coma, keratomalacia etc. 170
Lagophthalmos: This is the condition of incomplete closure of the palpebral aperture when an attempt is made to shut the eyes. Causes: 1) Exophthalomos as in Graves' disease, proptosis due to orbital tumour. 2) Facial never paralysis. 3) Cicatricial ectropion of upper lid. 4) Symblepharon. 5) Laxity of the tissue and absence of reflex blinking in people who are extremely ill – coma, keratomalacia etc. 170
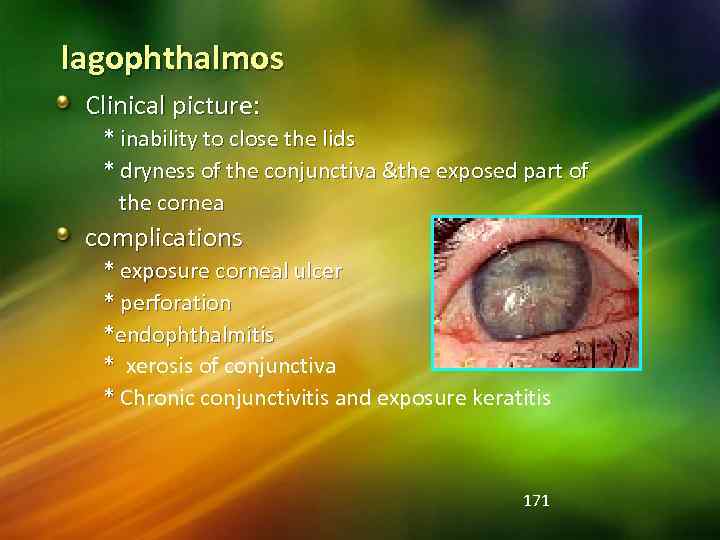 lagophthalmos Clinical picture: * inability to close the lids * dryness of the conjunctiva &the exposed part of the cornea complications * exposure corneal ulcer * perforation *endophthalmitis * xerosis of conjunctiva * Chronic conjunctivitis and exposure keratitis 171
lagophthalmos Clinical picture: * inability to close the lids * dryness of the conjunctiva &the exposed part of the cornea complications * exposure corneal ulcer * perforation *endophthalmitis * xerosis of conjunctiva * Chronic conjunctivitis and exposure keratitis 171
 Treatment: 1) Of the cause whenever possible. 2) Application of a bland or antibiotic ointment to protect cornea (eye drops & ointement). 3) Lateral or median tarsorrhaphy to protect the cornea. 172
Treatment: 1) Of the cause whenever possible. 2) Application of a bland or antibiotic ointment to protect cornea (eye drops & ointement). 3) Lateral or median tarsorrhaphy to protect the cornea. 172
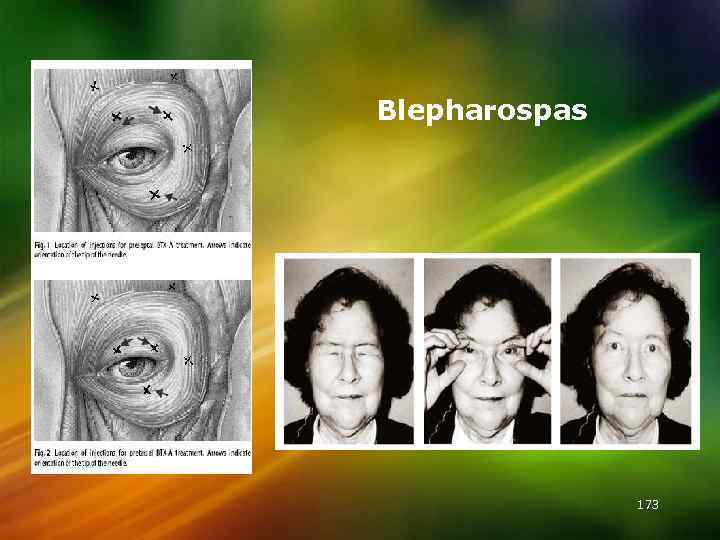 Blepharospas 173
Blepharospas 173
 Blepharospasm : It is a condition in which there are involuntary and forcible eyelid closure (difference from photophobia). 1) Reflex sensory stimulation through branches of 5 th cranial nerve – commonest. a) Phlyctenular keratoconjunctivitis. b) Foreign body on cornea. c) Membranous and pseudo membranous – conjunctivitis. d) Acute iridocyclitis. 2) Excessive stimulation of retina. a) Bright light on sensitive eye. b) Dilated pupil. c) Albinism. 3) Blepharospasm without any cause. 4) Hysteria. 174
Blepharospasm : It is a condition in which there are involuntary and forcible eyelid closure (difference from photophobia). 1) Reflex sensory stimulation through branches of 5 th cranial nerve – commonest. a) Phlyctenular keratoconjunctivitis. b) Foreign body on cornea. c) Membranous and pseudo membranous – conjunctivitis. d) Acute iridocyclitis. 2) Excessive stimulation of retina. a) Bright light on sensitive eye. b) Dilated pupil. c) Albinism. 3) Blepharospasm without any cause. 4) Hysteria. 174
 Surgical conditions of the eye lids Malposition of eye lashes: Distichiasis. Trichiasis. Malposition of the lid margin: Entropion Ectropion Abnormal position of the lids: Ptosis. Lid retraction. Anatomical deficiency: (coloboma)
Surgical conditions of the eye lids Malposition of eye lashes: Distichiasis. Trichiasis. Malposition of the lid margin: Entropion Ectropion Abnormal position of the lids: Ptosis. Lid retraction. Anatomical deficiency: (coloboma)
 176
176


