hypercal hypocalc 2016.pptx
- Количество слайдов: 60
Disorders of Calcium Metabolism Elena Segal Rambam Medical Center Haifa

Calcium • • An essential intracellular and extracellular cation • Intracellular calcium is needed for normal activity of many enzymes. • Regulation of endocrine and exocrine secretory activities: • • Activation of compliment system Extracellular calcium is required to maintain normal biological function of nervous system, the musculoskeletal system, regulation of neuromuscular contractility and blood coagulation insulin, aldosterone Bone metabolism: calcium salts provide structural integrity of the skeleton ( mineralization)
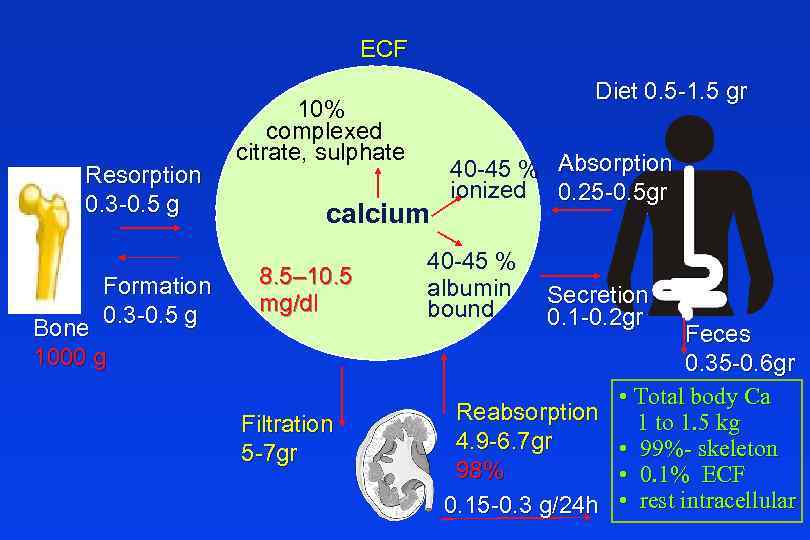
ECF Resorption 0. 3 -0. 5 g Formation 0. 3 -0. 5 g Bone 1000 g Diet 0. 5 -1. 5 gr 10% complexed citrate, sulphate calcium 8. 5– 10. 5 mg/dl Filtration 5 -7 gr 40 -45 % Absorption ionized 0. 25 -0. 5 gr 40 -45 % albumin bound Secretion 0. 1 -0. 2 gr Feces 0. 35 -0. 6 gr • Total body Ca Reabsorption 1 to 1. 5 kg 4. 9 -6. 7 gr • 99%- skeleton 98% • 0. 1% ECF 0. 15 -0. 3 g/24 h • rest intracellular
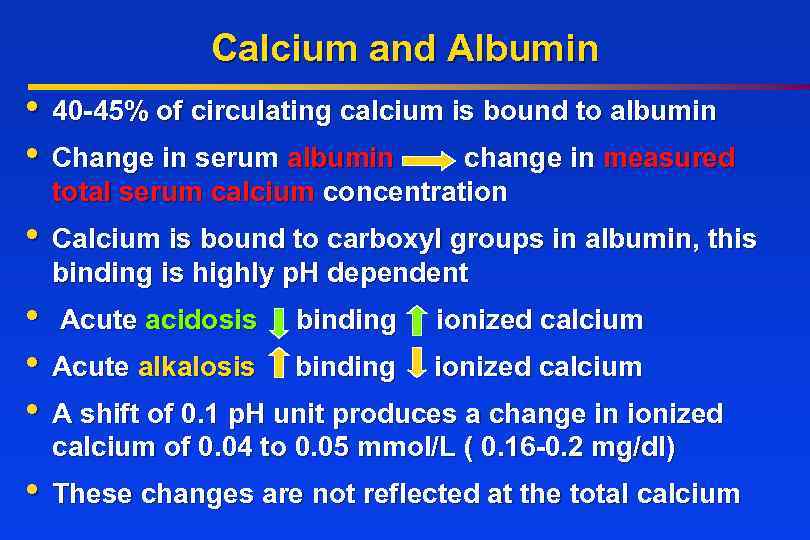
Calcium and Albumin • 40 -45% of circulating calcium is bound to albumin • Change in serum albumin change in measured total serum calcium concentration • Calcium is bound to carboxyl groups in albumin, this binding is highly p. H dependent • Acute acidosis binding ionized calcium • Acute alkalosis binding ionized calcium • A shift of 0. 1 p. H unit produces a change in ionized calcium of 0. 04 to 0. 05 mmol/L ( 0. 16 -0. 2 mg/dl) • These changes are not reflected at the total calcium
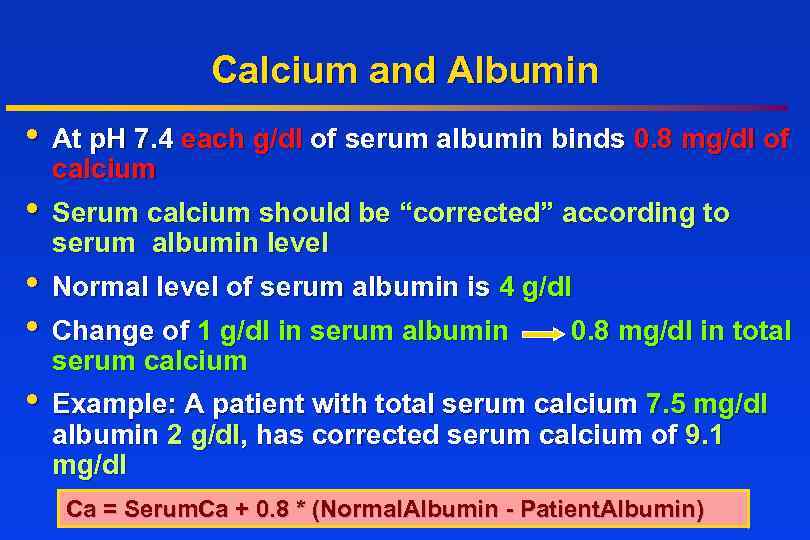
Calcium and Albumin • At p. H 7. 4 each g/dl of serum albumin binds 0. 8 mg/dl of calcium • Serum calcium should be “corrected” according to serum albumin level • Normal level of serum albumin is 4 g/dl • Change of 1 g/dl in serum albumin 0. 8 mg/dl in total serum calcium • Example: A patient with total serum calcium 7. 5 mg/dl albumin 2 g/dl, has corrected serum calcium of 9. 1 mg/dl Ca = Serum. Ca + 0. 8 * (Normal. Albumin - Patient. Albumin)
Disorders of Calcium Metabolism • Hypercalcemia • Hypocalcemia Serum Calcium >10. 4 mg/dl Serum Calcium < 8. 5 mg/dl
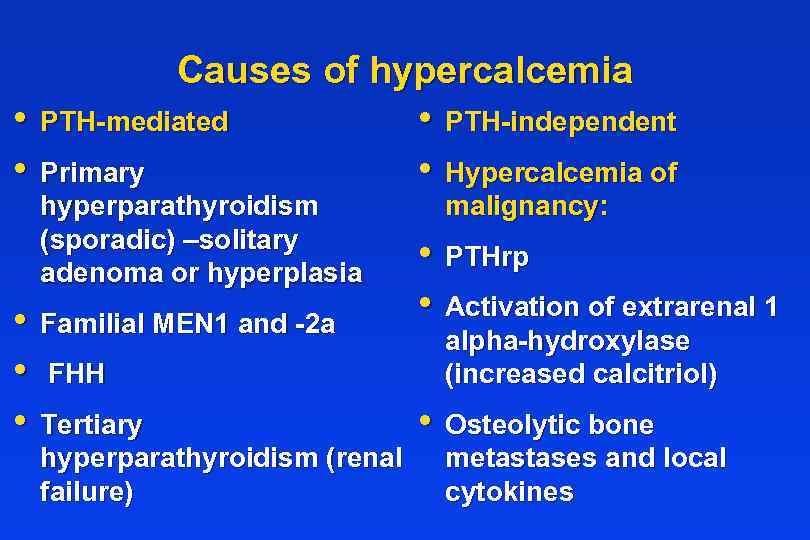
Causes of hypercalcemia • PTH-mediated • PTH-independent • Primary • Hypercalcemia of hyperparathyroidism (sporadic) –solitary adenoma or hyperplasia • Familial MEN 1 and -2 a • FHH • Tertiary hyperparathyroidism (renal failure) malignancy: • PTHrp • Activation of extrarenal 1 alpha-hydroxylase (increased calcitriol) • Osteolytic bone metastases and local cytokines
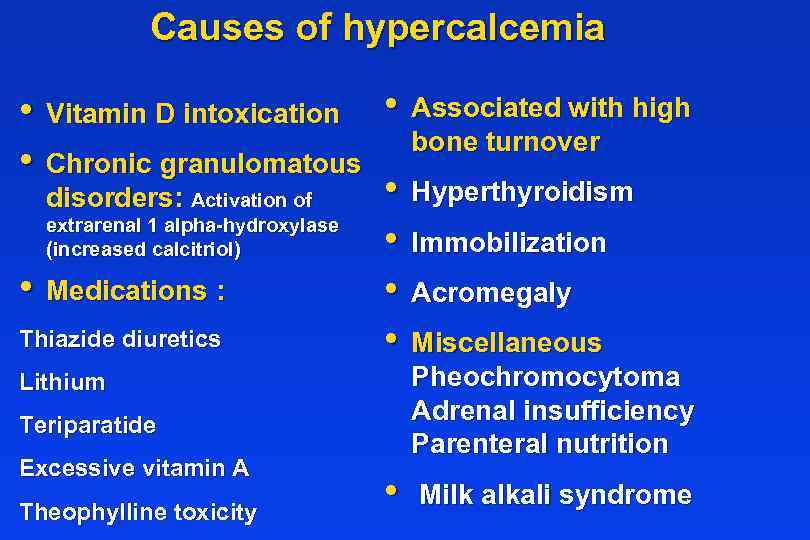
Causes of hypercalcemia • Vitamin D intoxication • Associated with high bone turnover • Chronic granulomatous • Hyperthyroidism disorders: Activation of extrarenal 1 alpha-hydroxylase • Immobilization (increased calcitriol) • Medications : • Acromegaly Thiazide diuretics • Miscellaneous Pheochromocytoma Adrenal insufficiency Parenteral nutrition Lithium Teriparatide Excessive vitamin A Theophylline toxicity • Milk alkali syndrome

Diagnosis of Hypercalcemia Serum Ca Measure serum albumin or ionized calcium Albumin corrected calcium normal Medical history and medication use history Measure PTH or N Check calciuria If high- Primary HPT; if low FHH Check 1, 25(OH)2 D 3 Lymphomas Malignancy
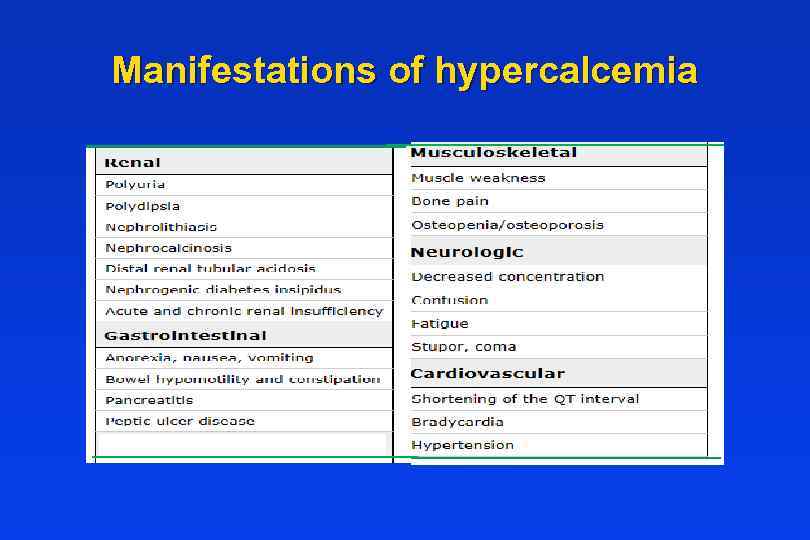
Manifestations of hypercalcemia
Renal manifestations • The most important renal manifestations are polyuria, resulting from decreased concentrating ability in the distal tubule, nephrolithiasis, and acute and chronic renal insufficiency. • Nephrogenic diabetes insipidus — Chronic hypercalcemia leads to a defect in concentrating ability that may induce polyuria and polydipsia in up to 20 percent of patients. The mechanism is incompletely understood, but the downregulation of aquaporin-2 water channels receptors, and calcium deposition in the medulla with secondary tubulointerstitial injury and impaired generation of the interstitial osmotic gradient may play important roles.
Renal manifestations • Nephrolithiasis — When hypercalcemia is due to primary hyperparathyroidism or sarcoidosis, it is often longstanding, and the resulting chronic hypercalciuria may cause nephrolithiasis. Increased calcitriol production may also play an important role in both diseases. • Renal tubular acidosis — Chronic hypercalcemia causes type 1 (distal) renal tubular acidosis. The ensuing hypercalciuria and hypocitraturia can contribute to the development of nephrolithiasis.
Gastrointestinal manifestations • • Nausea. • Peptic ulcer disease has been described in patients with hypercalcemia due to primary hyperparathyroidism and may be caused by calciuminduced increases in gastrin and acid secretion. • Pancreatitis due to deposition of calcium in the pancreatic duct and calcium activation of trypsinogen within the pancreatic parenchyma Constipation may be related to decreased smooth muscle tone and/or abnormal autonomic function.
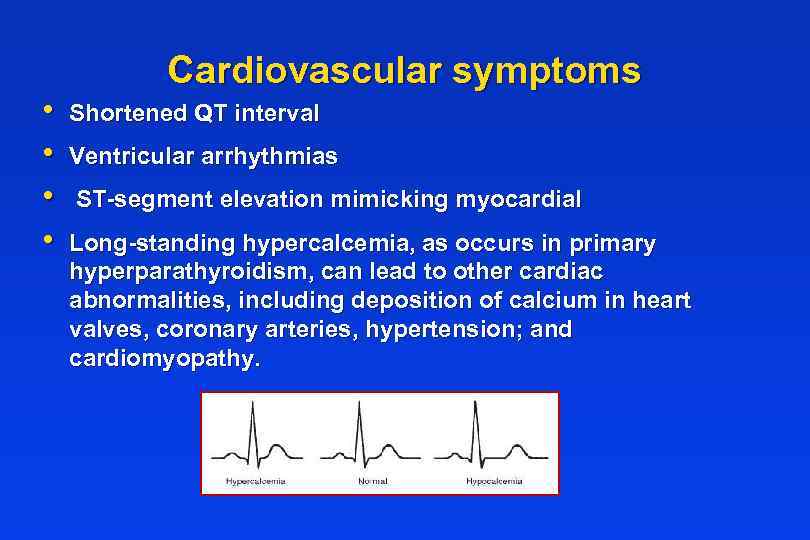
• • Cardiovascular symptoms Shortened QT interval Ventricular arrhythmias ST-segment elevation mimicking myocardial Long-standing hypercalcemia, as occurs in primary hyperparathyroidism, can lead to other cardiac abnormalities, including deposition of calcium in heart valves, coronary arteries, hypertension; and cardiomyopathy.
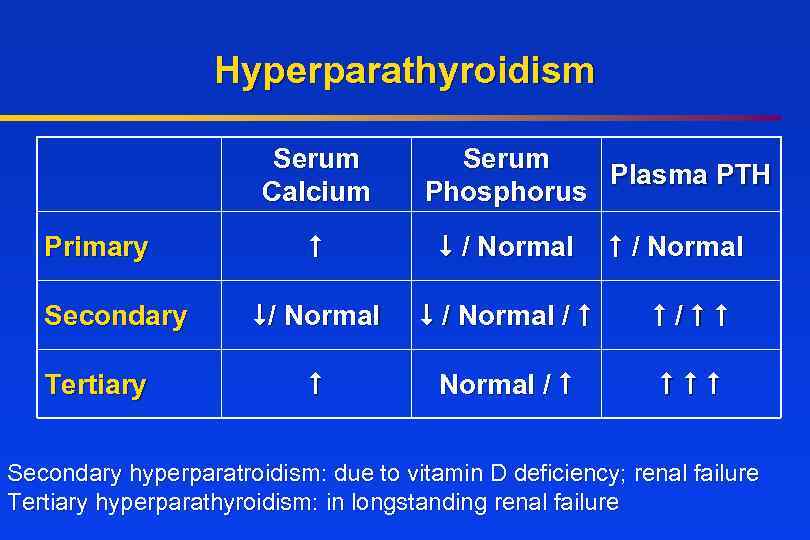
Hyperparathyroidism Serum Calcium Primary Secondary Tertiary Serum Plasma PTH Phosphorus / Normal / / Normal / Secondary hyperparatroidism: due to vitamin D deficiency; renal failure Tertiary hyperparathyroidism: in longstanding renal failure
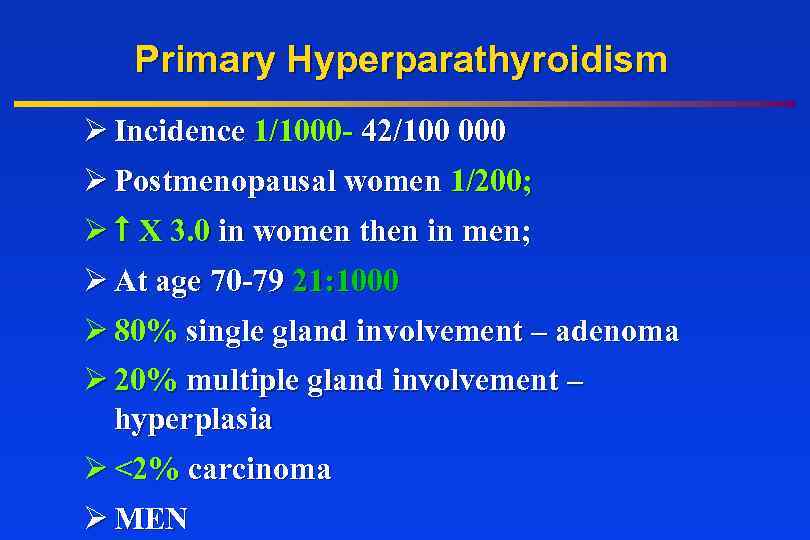
Primary Hyperparathyroidism Ø Incidence 1/1000 - 42/100 000 Ø Postmenopausal women 1/200; Ø X 3. 0 in women then in men; Ø At age 70 -79 21: 1000 Ø 80% single gland involvement – adenoma Ø 20% multiple gland involvement – hyperplasia Ø <2% carcinoma Ø MEN
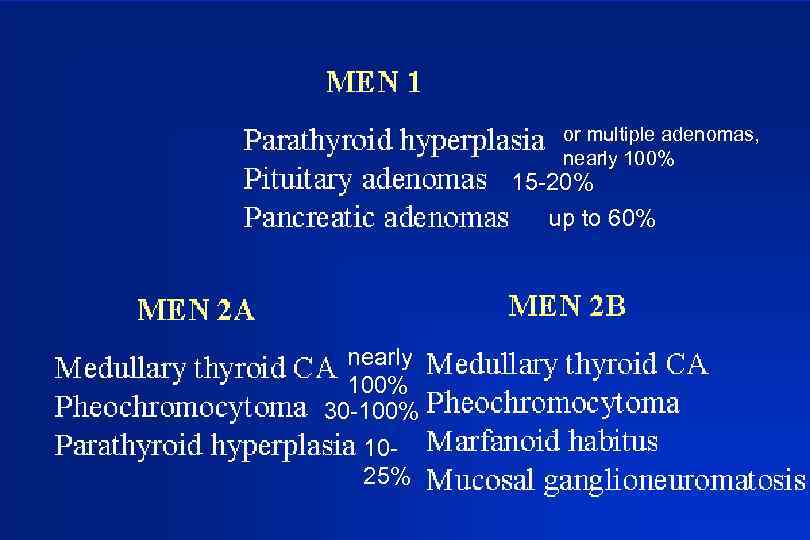
or multiple adenomas, nearly 100% 15 -20% up to 60% nearly 100% 30 -100% 1025%
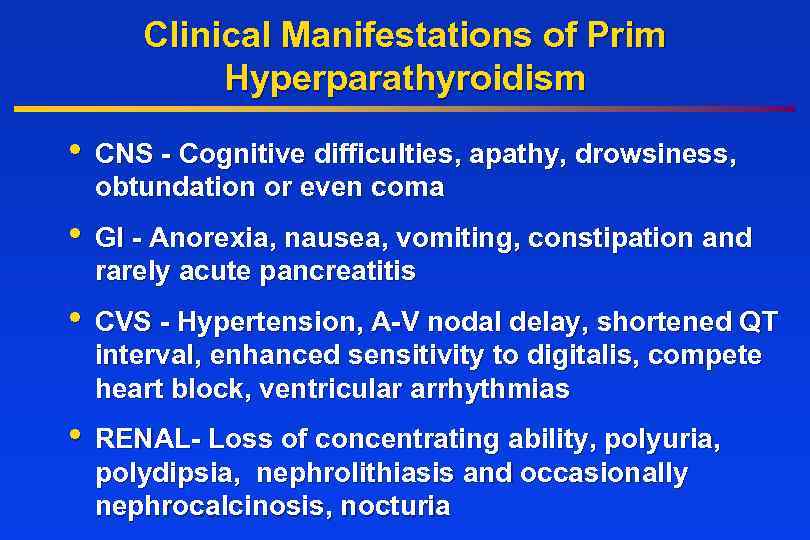
Clinical Manifestations of Prim Hyperparathyroidism • CNS - Cognitive difficulties, apathy, drowsiness, obtundation or even coma • GI - Anorexia, nausea, vomiting, constipation and rarely acute pancreatitis • CVS - Hypertension, A-V nodal delay, shortened QT interval, enhanced sensitivity to digitalis, compete heart block, ventricular arrhythmias • RENAL- Loss of concentrating ability, polyuria, polydipsia, nephrolithiasis and occasionally nephrocalcinosis, nocturia
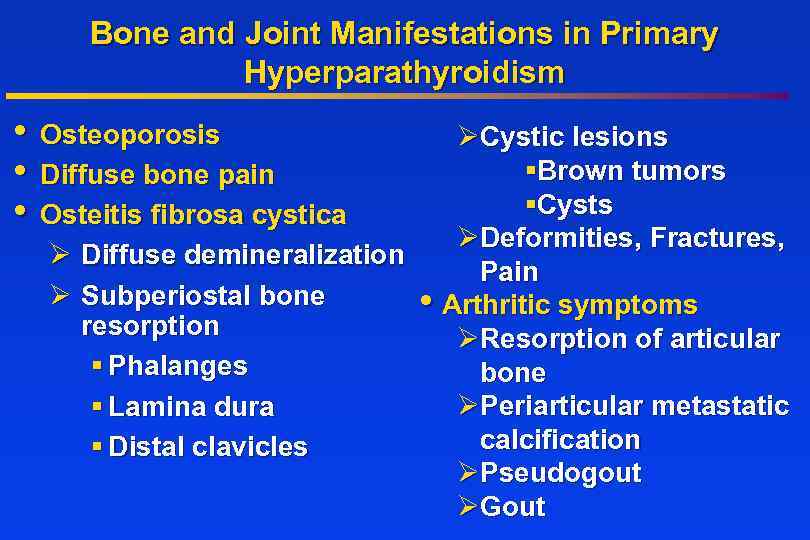
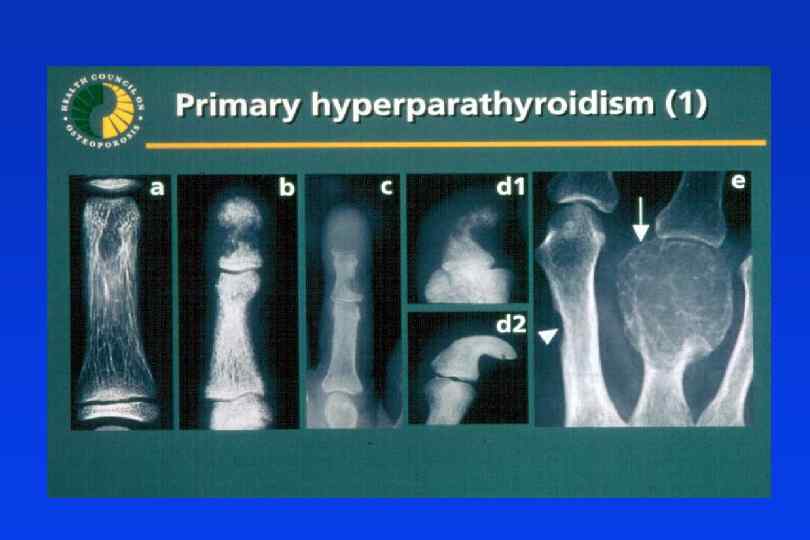
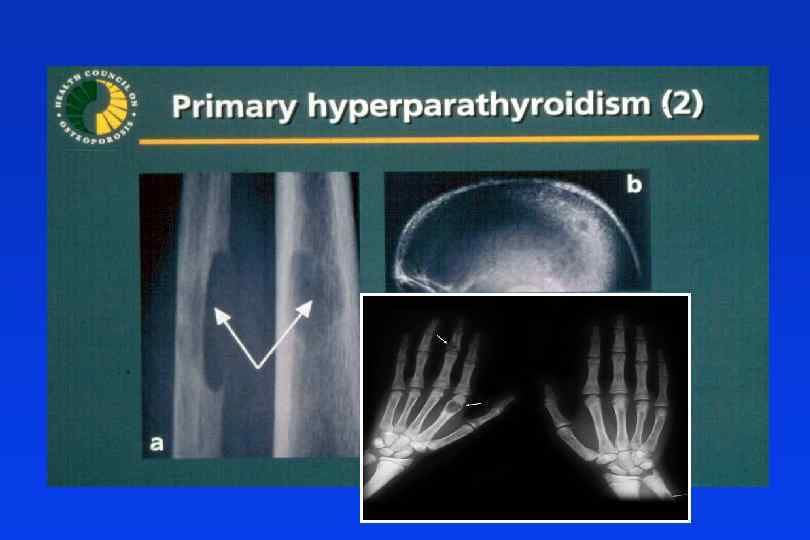
Bone and Joint Manifestations in Primary Hyperparathyroidism • Osteoporosis • Diffuse bone pain • Osteitis fibrosa cystica ØCystic lesions §Brown tumors §Cysts ØDeformities, Fractures, Ø Diffuse demineralization Pain Ø Subperiostal bone • Arthritic symptoms resorption ØResorption of articular § Phalanges bone ØPeriarticular metastatic § Lamina dura calcification § Distal clavicles ØPseudogout ØGout
Treatment When is surgery indicated in PHPT patients ?
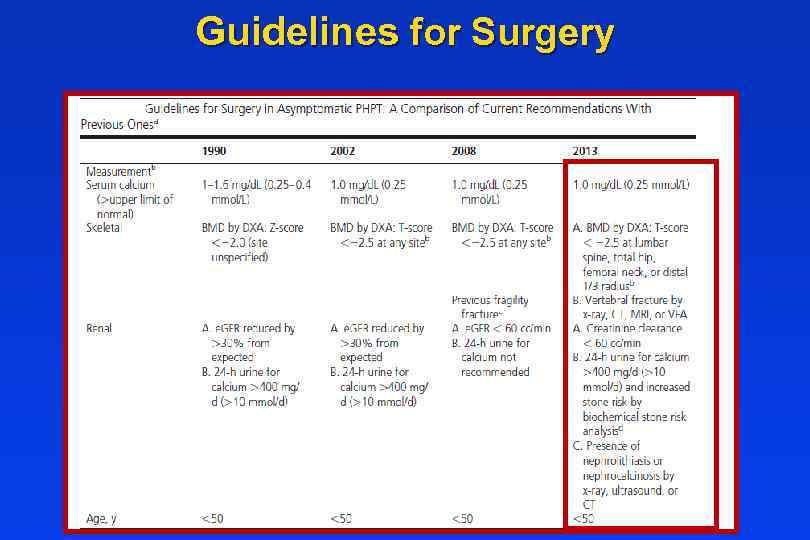
Guidelines for Surgery
Other Considerations • Neuropsychological disturbances • Weakness and easy fatigability • Depression • Intellectual weariness • Increased sleep requirements Improved by surgery • Onset of Menopause • Increased bone loss
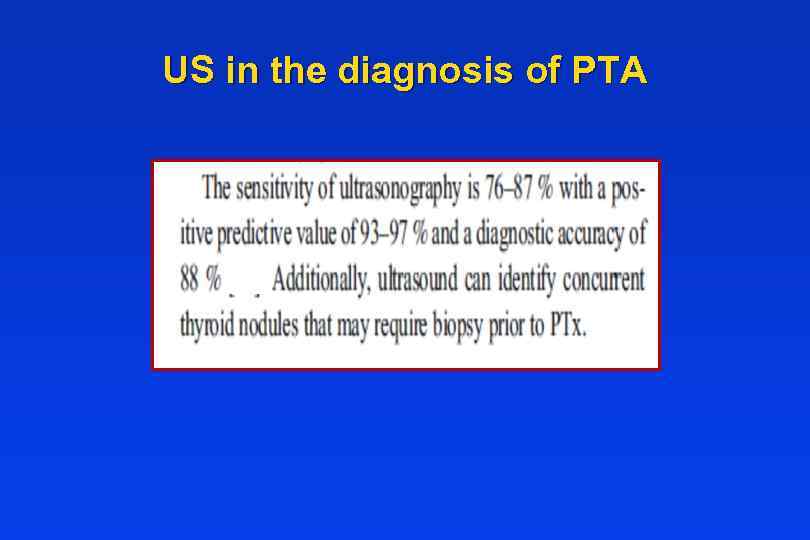
US in the diagnosis of PTA
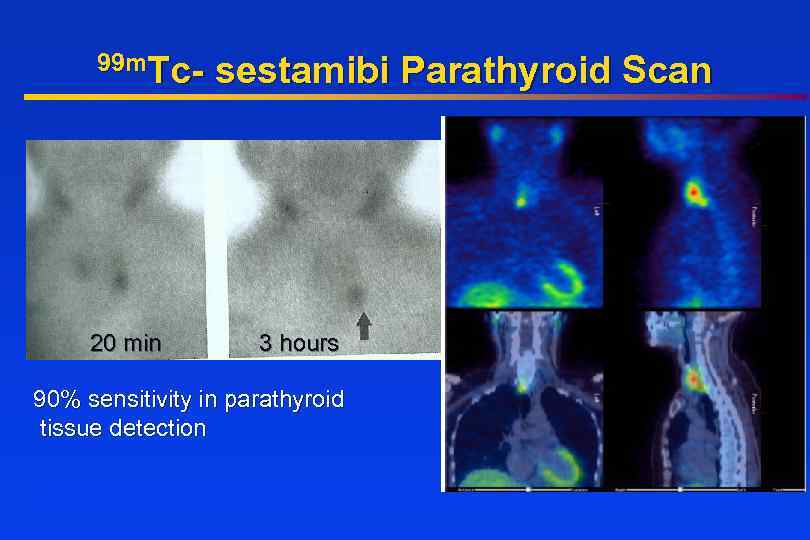
99 m. Tc- 20 min sestamibi Parathyroid Scan 3 hours 90% sensitivity in parathyroid tissue detection
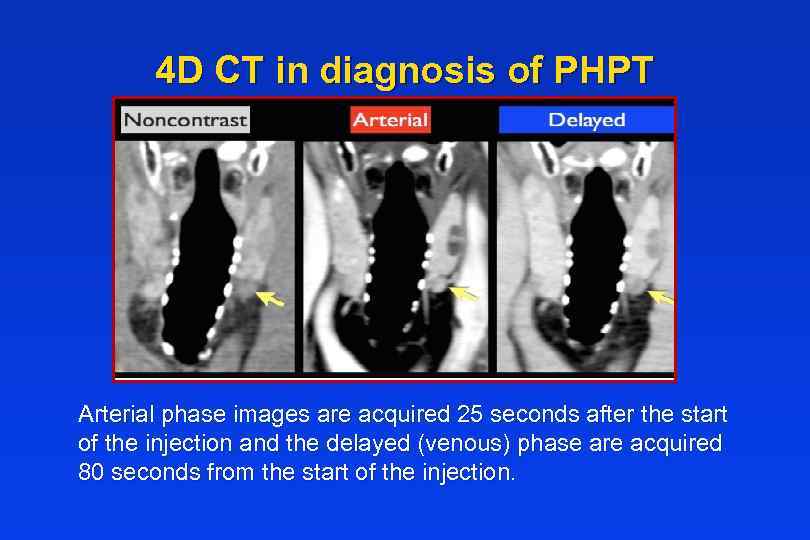
4 D CT in diagnosis of PHPT Arterial phase images are acquired 25 seconds after the start of the injection and the delayed (venous) phase are acquired 80 seconds from the start of the injection.
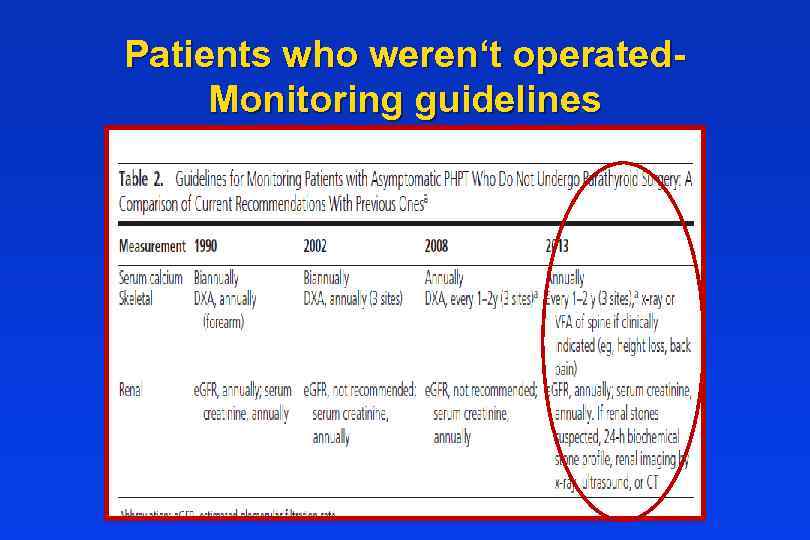
Patients who weren‘t operated. Monitoring guidelines
General Measures • Hydration • Adequate Mobility • Diet neither restrictive nor excessive in calcium • Adequate vitamin D status • Prompt medical attention for the possibility of worsening of hypercalcemia (intercurrent illness accompanied by risk of dehydration)
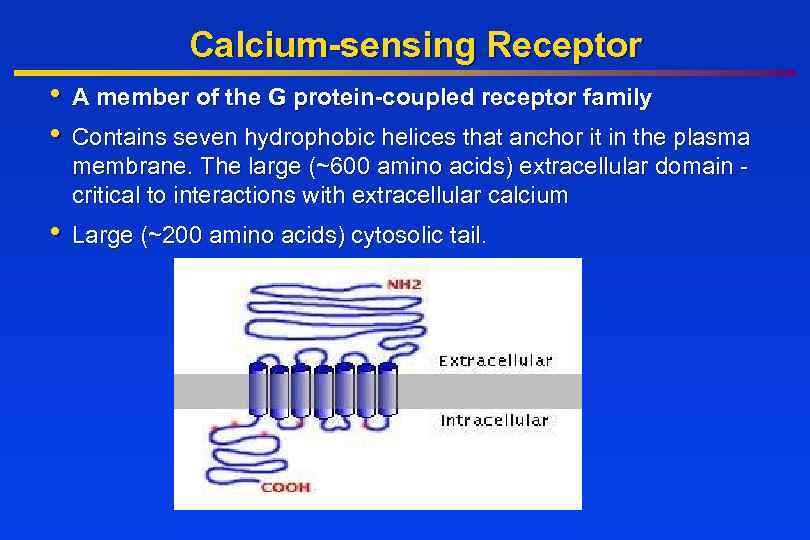
Calcium-sensing Receptor • A member of the G protein-coupled receptor family • Contains seven hydrophobic helices that anchor it in the plasma membrane. The large (~600 amino acids) extracellular domain critical to interactions with extracellular calcium • Large (~200 amino acids) cytosolic tail.
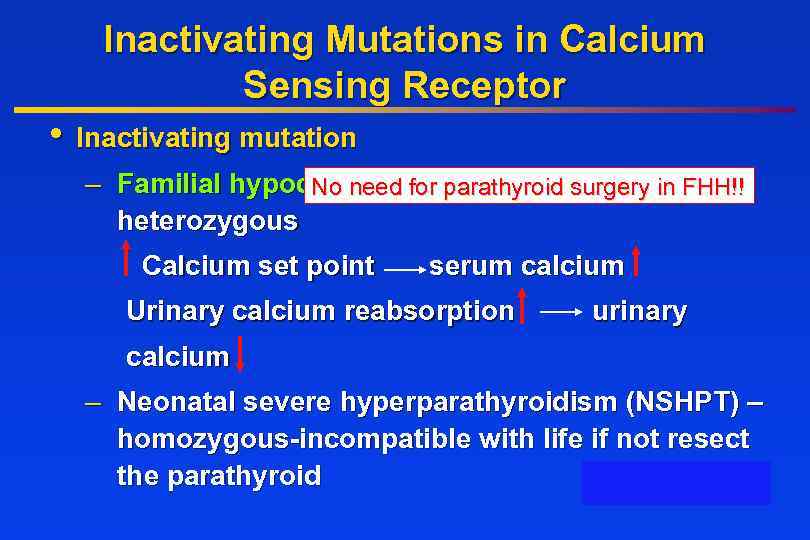
Inactivating Mutations in Calcium Sensing Receptor • Inactivating mutation – Familial hypocalciuricfor parathyroid surgery in FHH!! No need hypercalcemia (FHH) heterozygous Calcium set point serum calcium Urinary calcium reabsorption urinary calcium – Neonatal severe hyperparathyroidism (NSHPT) – homozygous-incompatible with life if not resect homozygous the parathyroid
Hypercalcemia of Malignancy • Lung, breast, and prostate cancer frequently invade skeleton and destroy bone tissue • Damage to skeleton usually late in course of disease • Bone damage associated with considerable worsening in patient’s quality of life • Multiple myeloma has skeletal complications in virtually 100% of cases • Breast and lung cancer also cause hypercalcemia of malignancy, without invading skeleton
Pthr. P Induced Hypercalcemia Squamous cell carcinoma Islet cell tumor (pancreas) Adult T cell leukemia Renal cell carcinoma Breast carcinoma
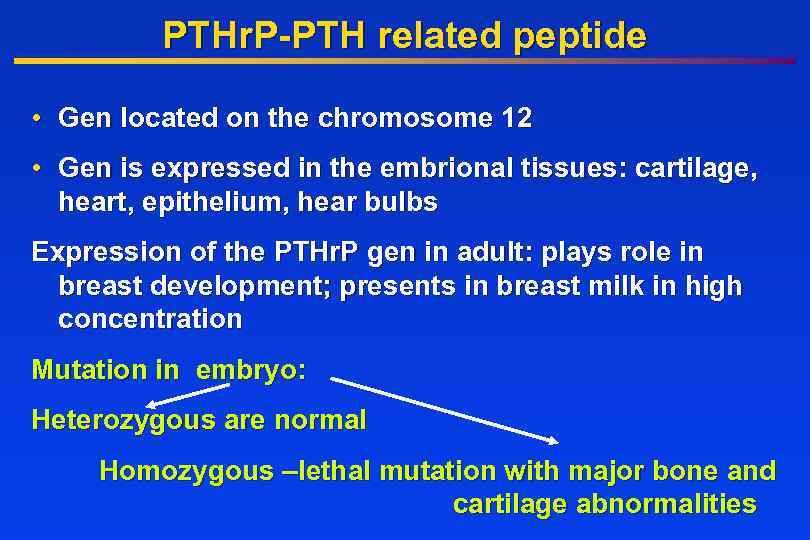
PTHr. P-PTH related peptide • Gen located on the chromosome 12 • Gen is expressed in the embrional tissues: cartilage, heart, epithelium, hear bulbs Expression of the PTHr. P gen in adult: plays role in breast development; presents in breast milk in high concentration Mutation in embryo: Heterozygous are normal Homozygous –lethal mutation with major bone and cartilage abnormalities
Treatment Ø Hydration Ø Bisphonates IV, Denosumab Ø Calcitonin Ø Glucocorticoids Ø Dialysis
Hydration • First step in the management of severe hypercalcemia - Isotonic saline • Usually serum calcium by 1. 6 -2. 4 mg/dl • Hydration alone rarely leads to normalization in severe hypercalcemia • Rate of IV saline based on severity of hypercalcemia and tolerance of CVS for volume expansion, if possible achieve urine output of 300 ml/hr, that is then adjusted to maintain the urine output at 100 to 150 m. L/hour.
Loop Diuretics • In the past intensive administration of furosemide was used (80 to 100 mg every one to two hours). • It needs aggressive fluid hydration (10 liters daily), saline therapy beyond that necessary to restore euvolemia. • Now use of calcitonin and bisphonates is more effective.
Calcitonin • The efficacy of calcitonin (4 IU/kg every 6 -12 hours) is limited to the first 48 hours, due to development of tachyphylaxis, perhaps due to receptor downregulation. • Calcitonin and hydration provide a rapid reduction in serum calcium concentration, while a bisphonate provides a more sustained effect.
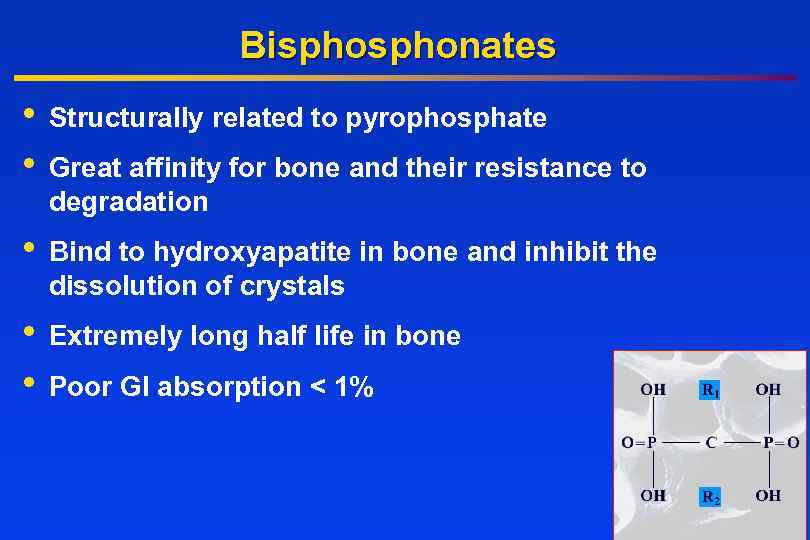
Bisphonates • • Structurally related to pyrophosphate • Bind to hydroxyapatite in bone and inhibit the dissolution of crystals • • Extremely long half life in bone Great affinity for bone and their resistance to degradation Poor GI absorption < 1%
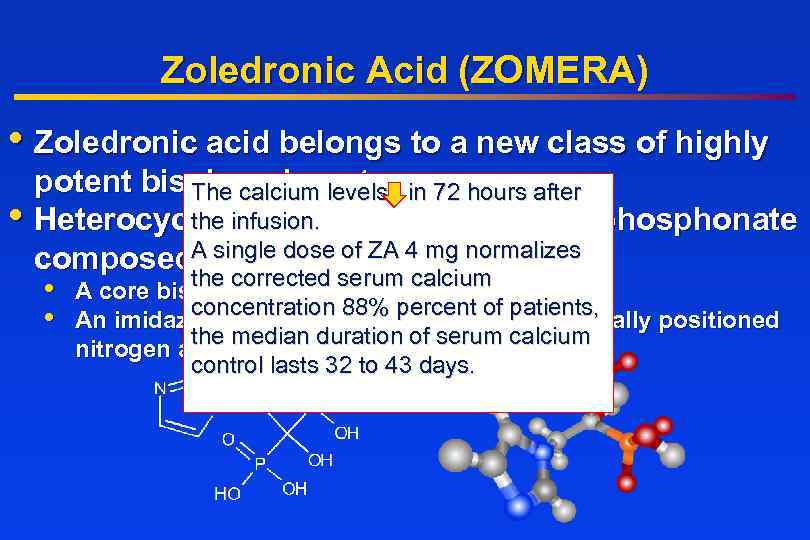
Zoledronic Acid (ZOMERA) • Zoledronic acid belongs to a new class of highly potent bisphonates in 72 hours after The calcium levels the nitrogen-containing bisphonate • Heterocyclic, infusion. single composed. Aof: dose of ZA 4 mg normalizes the corrected • A core bisphonateserum calcium moiety concentration 88% • An imidazole-ring side chainpercent of patients, containing 2 critically positioned the median duration of serum calcium nitrogen atoms control lasts 32 to 43 days.
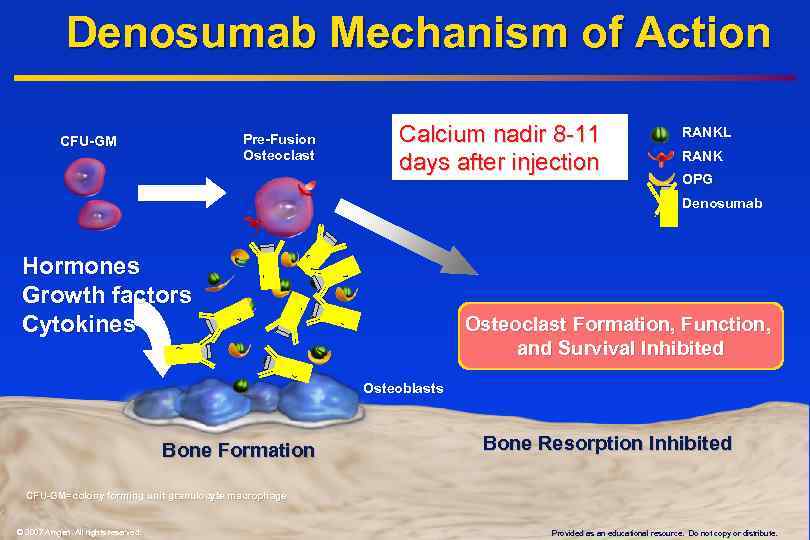
Denosumab Mechanism of Action Pre-Fusion Osteoclast CFU-GM Calcium nadir 8 -11 days after injection RANKL RANK OPG Denosumab Hormones Growth factors Cytokines Osteoclast Formation, Function, and Survival Inhibited Osteoblasts Bone Formation Bone Resorption Inhibited CFU-GM=colony forming unit granulocyte macrophage © 2007 Amgen. All rights reserved. Provided as an educational resource. Do not copy or distribute.
Glucocorticoids • Inhibit the growth of neoplastic lymphoid tissue • Counteract the effects of vitamin D
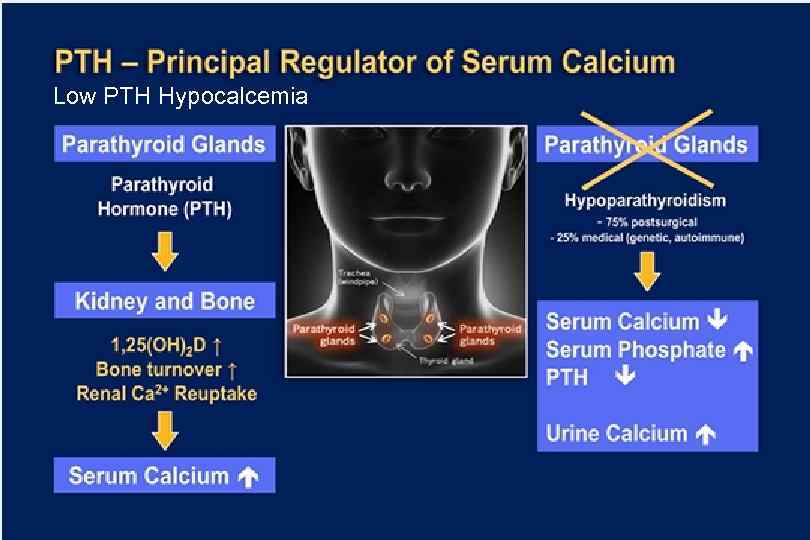
Low PTH Hypocalcemia
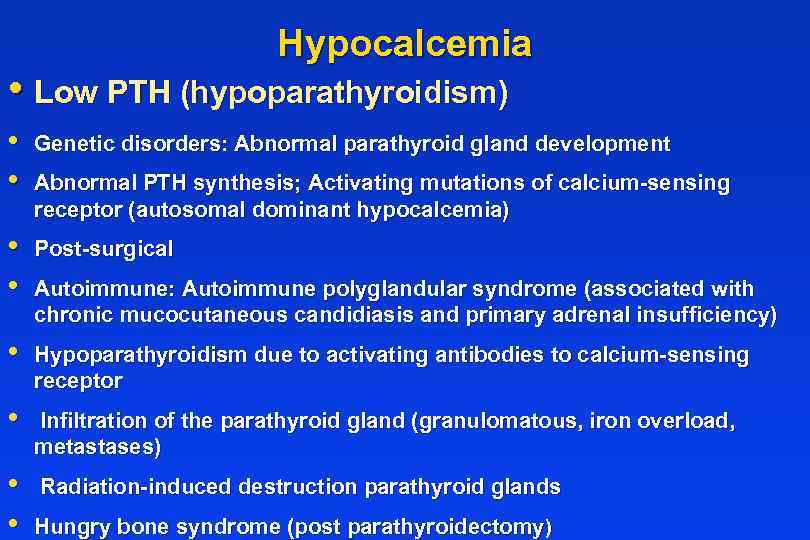
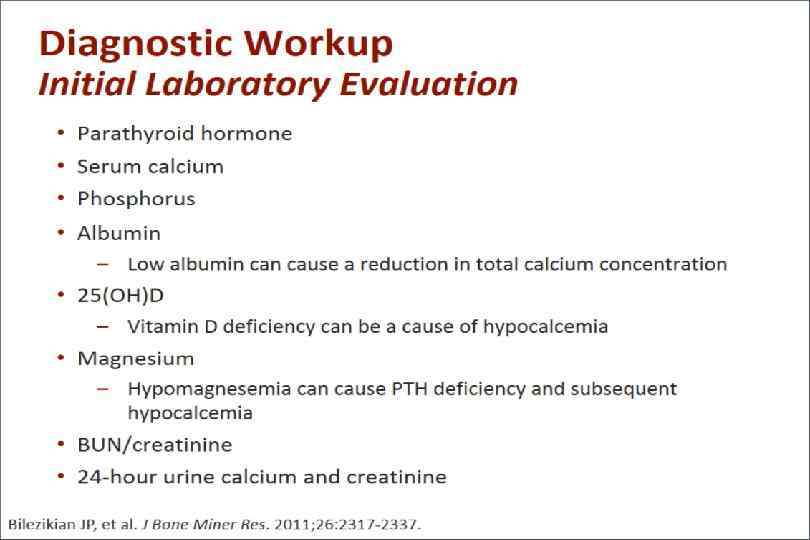
Hypocalcemia • Low PTH (hypoparathyroidism) • • Genetic disorders: Abnormal parathyroid gland development • • Post-surgical • Hypoparathyroidism due to activating antibodies to calcium-sensing receptor • Infiltration of the parathyroid gland (granulomatous, iron overload, metastases) • • Radiation-induced destruction parathyroid glands Abnormal PTH synthesis; Activating mutations of calcium-sensing receptor (autosomal dominant hypocalcemia) Autoimmune: Autoimmune polyglandular syndrome (associated with chronic mucocutaneous candidiasis and primary adrenal insufficiency) Hungry bone syndrome (post parathyroidectomy)
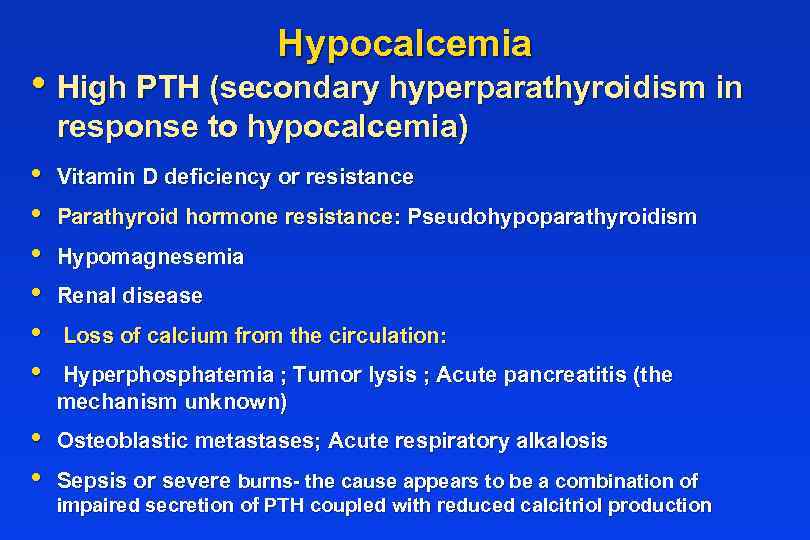
Hypocalcemia • High PTH (secondary hyperparathyroidism in response to hypocalcemia) • • • Vitamin D deficiency or resistance • • Osteoblastic metastases; Acute respiratory alkalosis Parathyroid hormone resistance: Pseudohypoparathyroidism Hypomagnesemia Renal disease Loss of calcium from the circulation: Hyperphosphatemia ; Tumor lysis ; Acute pancreatitis (the mechanism unknown) Sepsis or severe burns- the cause appears to be a combination of impaired secretion of PTH coupled with reduced calcitriol production
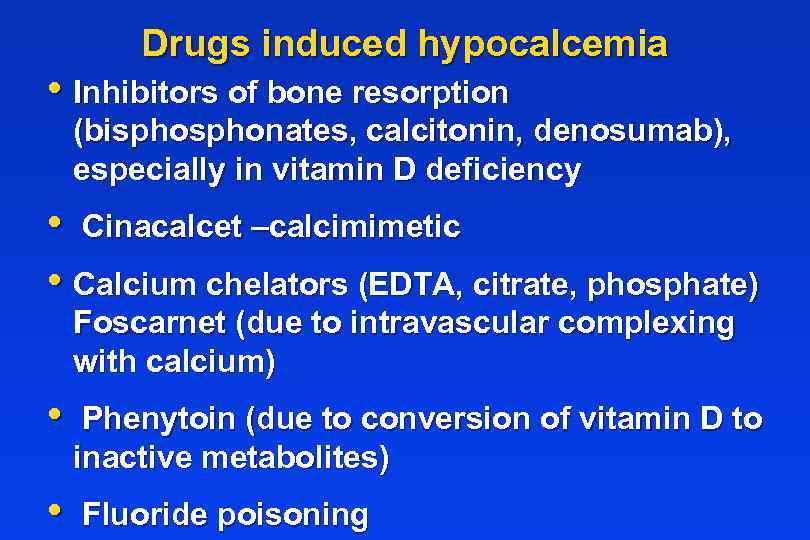
Drugs induced hypocalcemia • Inhibitors of bone resorption (bisphonates, calcitonin, denosumab), especially in vitamin D deficiency • Cinacalcet –calcimimetic • Calcium chelators (EDTA, citrate, phosphate) Foscarnet (due to intravascular complexing with calcium) • Phenytoin (due to conversion of vitamin D to inactive metabolites) • Fluoride poisoning
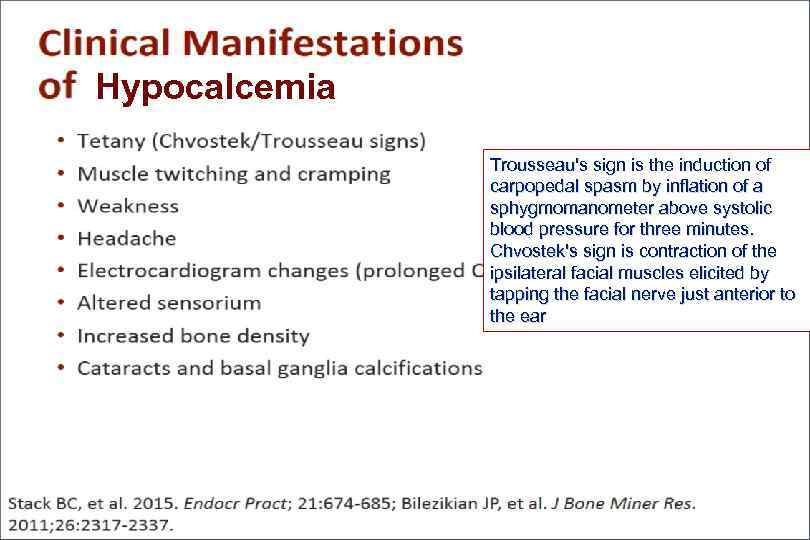
Hypocalcemia Trousseau's sign is the induction of carpopedal spasm by inflation of a sphygmomanometer above systolic blood pressure for three minutes. Chvostek's sign is contraction of the ipsilateral facial muscles elicited by tapping the facial nerve just anterior to the ear
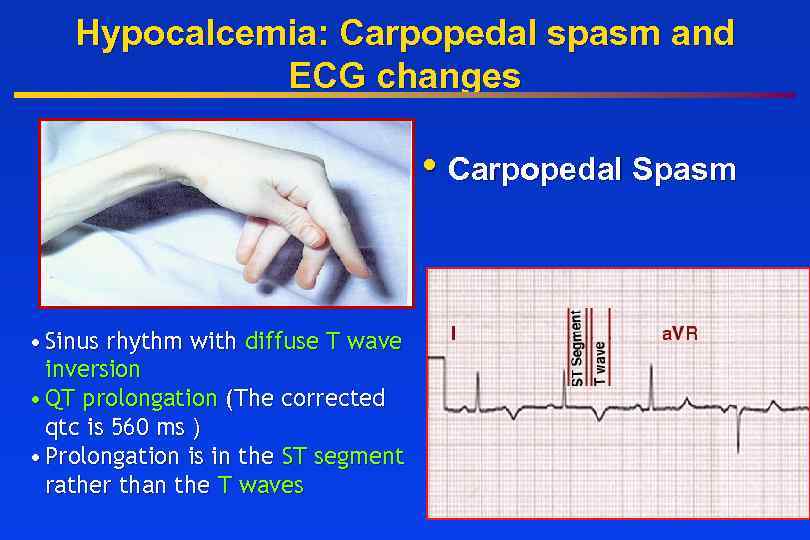
Hypocalcemia: Carpopedal spasm and ECG changes • Carpopedal Spasm • Sinus rhythm with diffuse T wave inversion • QT prolongation (The corrected qtc is 560 ms ) • Prolongation is in the ST segment rather than the T waves
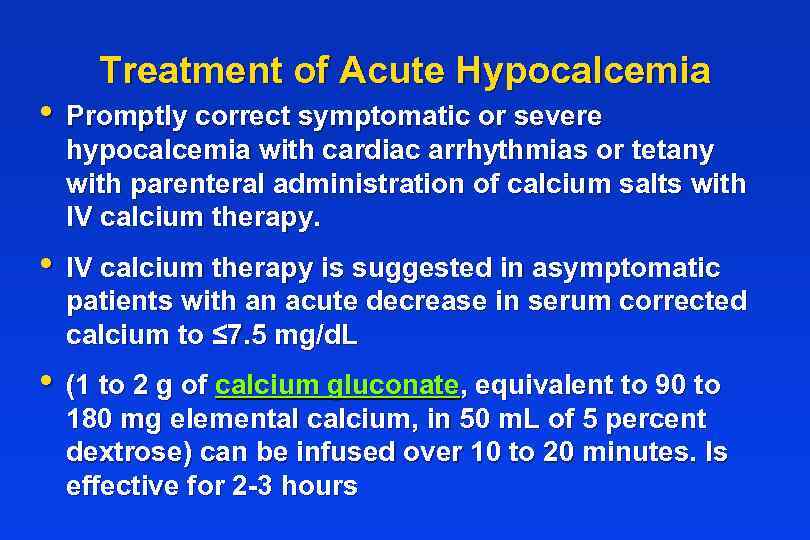
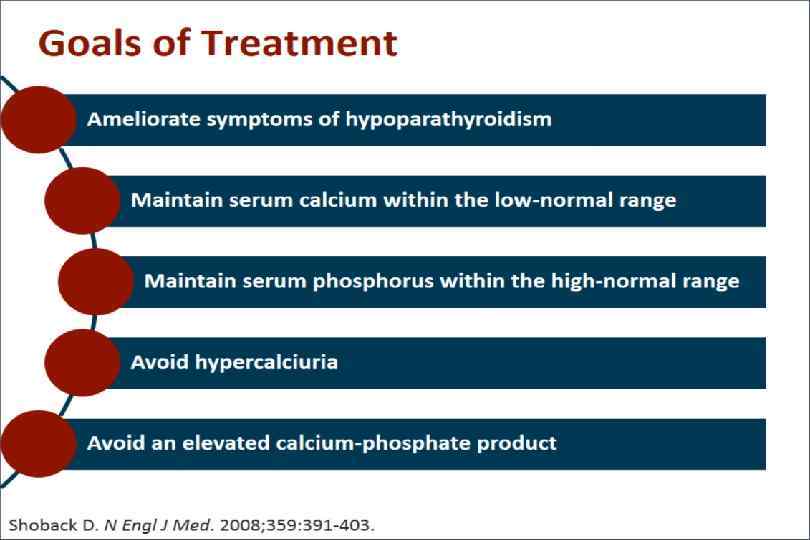
Treatment of Acute Hypocalcemia • Promptly correct symptomatic or severe hypocalcemia with cardiac arrhythmias or tetany with parenteral administration of calcium salts with IV calcium therapy. • IV calcium therapy is suggested in asymptomatic patients with an acute decrease in serum corrected calcium to ≤ 7. 5 mg/d. L • (1 to 2 g of calcium gluconate, equivalent to 90 to 180 mg elemental calcium, in 50 m. L of 5 percent dextrose) can be infused over 10 to 20 minutes. Is effective for 2 -3 hours
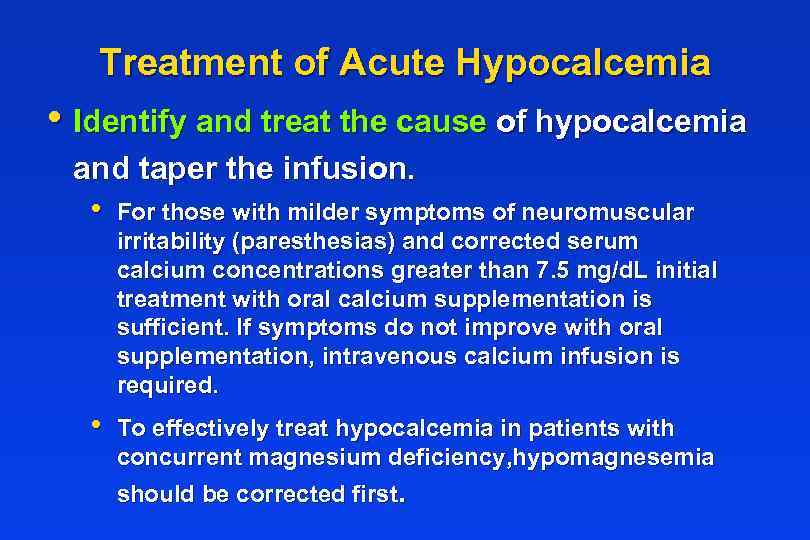
Treatment of Acute Hypocalcemia • Identify and treat the cause of hypocalcemia and taper the infusion. • For those with milder symptoms of neuromuscular irritability (paresthesias) and corrected serum calcium concentrations greater than 7. 5 mg/d. L initial treatment with oral calcium supplementation is sufficient. If symptoms do not improve with oral supplementation, intravenous calcium infusion is required. • To effectively treat hypocalcemia in patients with concurrent magnesium deficiency, hypomagnesemia should be corrected first.
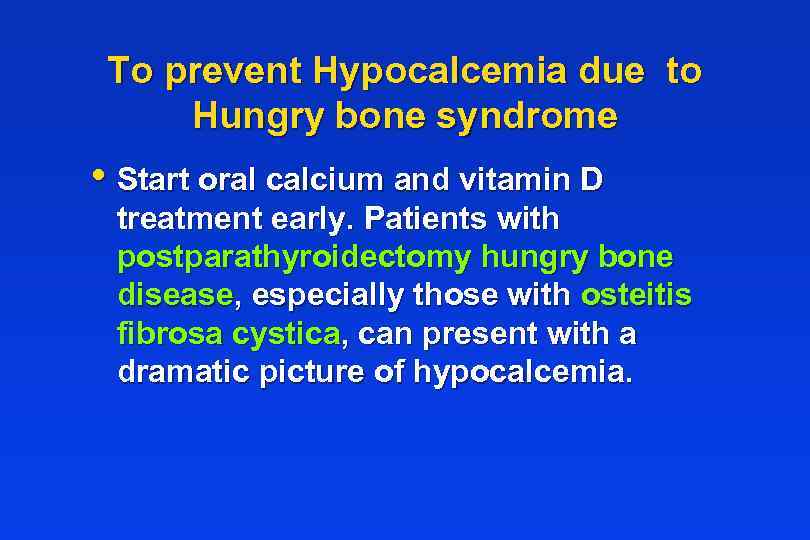
To prevent Hypocalcemia due to Hungry bone syndrome • Start oral calcium and vitamin D treatment early. Patients with postparathyroidectomy hungry bone disease, especially those with osteitis fibrosa cystica, can present with a dramatic picture of hypocalcemia.
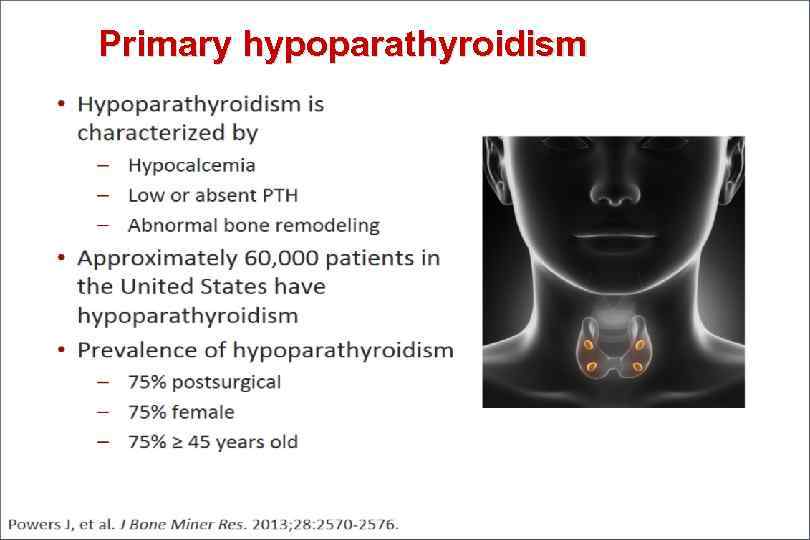
Primary hypoparathyroidism
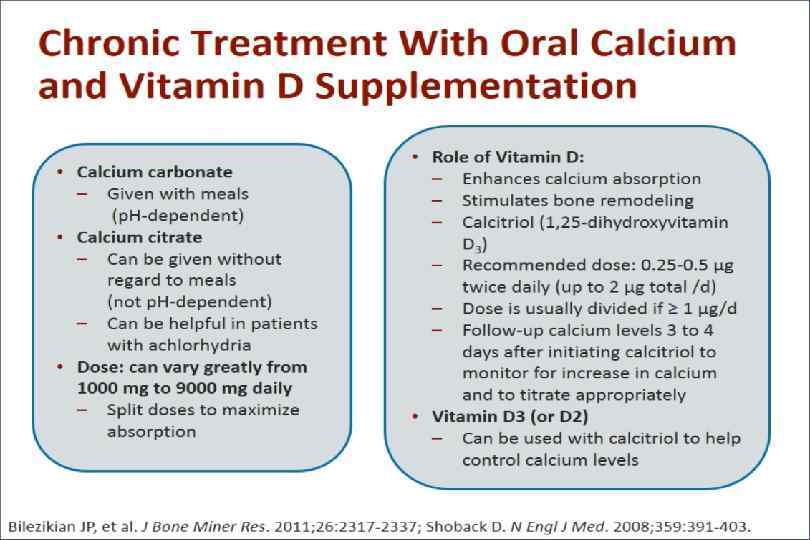
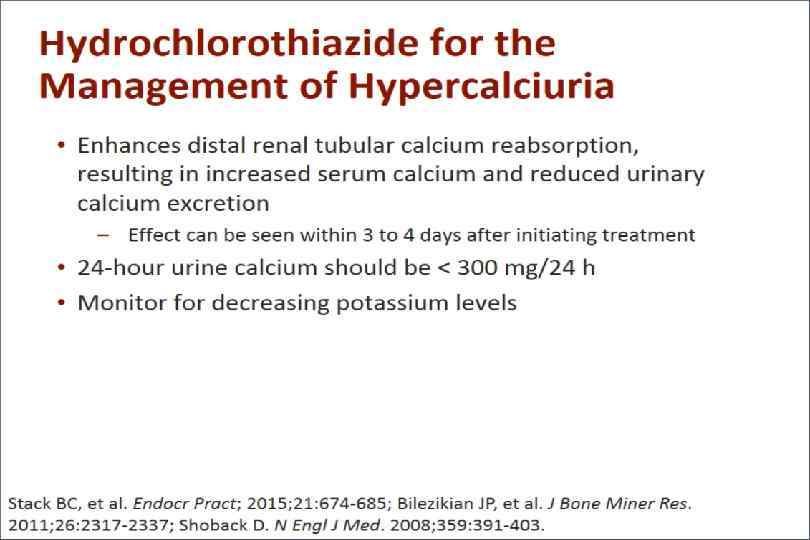
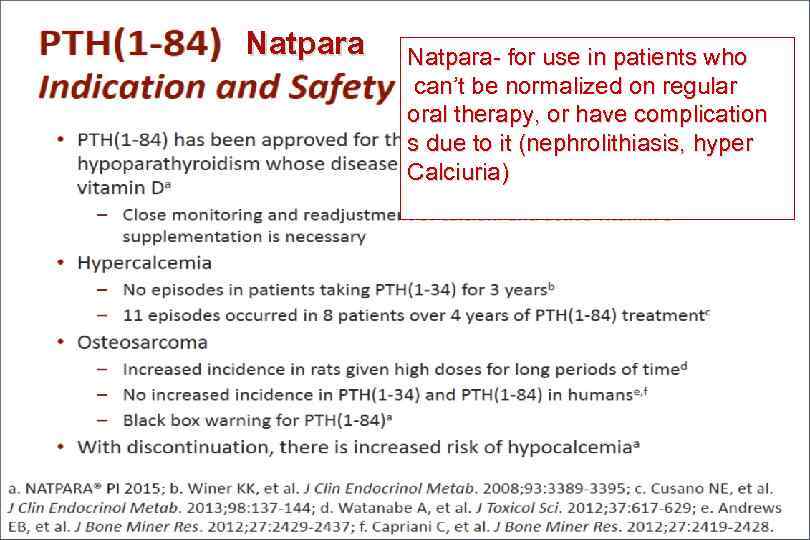
Natpara- for use in patients who can’t be normalized on regular oral therapy, or have complication s due to it (nephrolithiasis, hyper Calciuria)
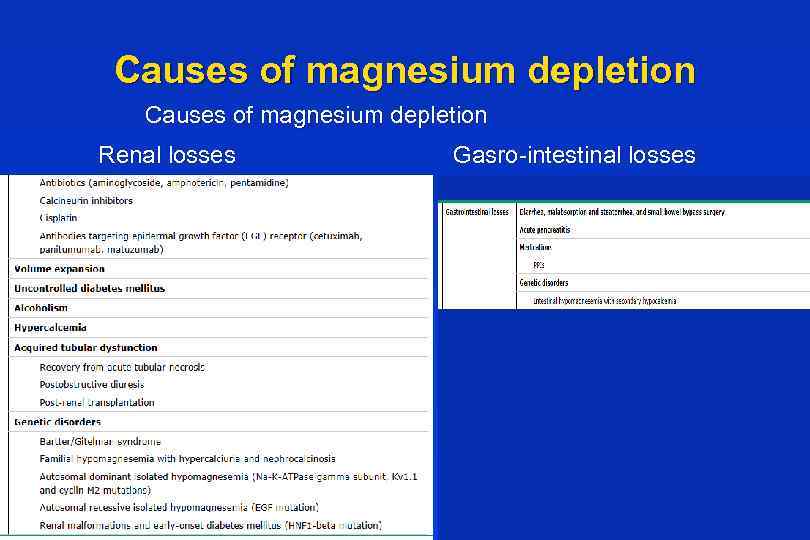
Causes of magnesium depletion Renal losses Gasro-intestinal losses
Treatment of Hypomagnesemia • • Oral repletion- if available and tolerable. • If a sustained-release preparation is not available, magnesium oxide 800 to 1600 mg (20 to 40 mmol [40 to 80 meq]) daily in divided doses may be used for moderate to severe hypomagnesemia. • Diarrhea frequently occurs with magnesium oxide therapy. A typical daily dose in a patient with normal renal function is 240 to 1000 mg (20 to 80 meq [10 to 40 mmol]) of elemental magnesium in divided doses.
Thank you and Good luck!
hypercal hypocalc 2016.pptx