Болезни почек англ 2013.ppt
- Количество слайдов: 82
 DISEASES OF KIDNEYS LECTURE
DISEASES OF KIDNEYS LECTURE
 Diseases of kidney Brite‘s Disease – 1827 - Proteinuria - Edema - Hypertension (myocardial hypertrophy)
Diseases of kidney Brite‘s Disease – 1827 - Proteinuria - Edema - Hypertension (myocardial hypertrophy)
 Classification of F. Folgard and K. Farr (1914) • Nephritis • Nephrosclerosis • Tumors • Congenital anomalies
Classification of F. Folgard and K. Farr (1914) • Nephritis • Nephrosclerosis • Tumors • Congenital anomalies
 Classification according to functional-anatomical characteristics - Glomerular diseases - Tubular diseases - Interstitial diseases - Congenital anomalies - Tumors
Classification according to functional-anatomical characteristics - Glomerular diseases - Tubular diseases - Interstitial diseases - Congenital anomalies - Tumors
 • The clinical manifestations of renal diseases can be grouped into reasonably well-defined syndromes.
• The clinical manifestations of renal diseases can be grouped into reasonably well-defined syndromes.
 The major renal syndromes: • 1. Acute nephritic syndrome is a glomerular syndrome dominated by the acute inset of usually grossly visible hematuria (red blood cells in urine), mild to moderate proteinuria, and hypertension; it is the classic presentation of acute poststreptococcal glomerulonephritis.
The major renal syndromes: • 1. Acute nephritic syndrome is a glomerular syndrome dominated by the acute inset of usually grossly visible hematuria (red blood cells in urine), mild to moderate proteinuria, and hypertension; it is the classic presentation of acute poststreptococcal glomerulonephritis.
 The major renal syndromes: • 2. The nephrotic syndrome is characterized by heavy proteinuria, hypoalbuminuria, severe edema, hyperlipidemia, and lipiduria. • 3. Asymptomatic hematuria or proteinuria, or a combination of these two, is usually manifestation of mild glomerular abnormalities.
The major renal syndromes: • 2. The nephrotic syndrome is characterized by heavy proteinuria, hypoalbuminuria, severe edema, hyperlipidemia, and lipiduria. • 3. Asymptomatic hematuria or proteinuria, or a combination of these two, is usually manifestation of mild glomerular abnormalities.
 The major renal syndromes: • 4. Acute renal failure is dominated by oliguria or anuria, with recent onset of azotemia. It can result from glomerular injury, interstitial injury, or acute tubular necrosis. • 5. Chronic renal failure, characterized by prolonged symptoms and signs of uremia, is the end result of all chronic renal • diseases.
The major renal syndromes: • 4. Acute renal failure is dominated by oliguria or anuria, with recent onset of azotemia. It can result from glomerular injury, interstitial injury, or acute tubular necrosis. • 5. Chronic renal failure, characterized by prolonged symptoms and signs of uremia, is the end result of all chronic renal • diseases.
 The major renal syndromes: • 6. Renal tubular defects are dominated by polyuria and electrolyte disorders. They are the result of either diseases directly affecting tubular structure or defects in specific tubular infection. The latter may be inherited or acquired.
The major renal syndromes: • 6. Renal tubular defects are dominated by polyuria and electrolyte disorders. They are the result of either diseases directly affecting tubular structure or defects in specific tubular infection. The latter may be inherited or acquired.
 The major renal syndromes: • 7. Urinary tract infection is characterized by bacteriuria and pyuria. The infection may be symptomatic or asymptomatic, and it may affect the kidney or the bladder only. • 8. Nephrolithiasis (renal stone) is manifested by renal colic, hematuria, and recurrent stone formation.
The major renal syndromes: • 7. Urinary tract infection is characterized by bacteriuria and pyuria. The infection may be symptomatic or asymptomatic, and it may affect the kidney or the bladder only. • 8. Nephrolithiasis (renal stone) is manifested by renal colic, hematuria, and recurrent stone formation.
 Glomerular diseases (glomerulopathy) primary and initial lesion of glomeruli
Glomerular diseases (glomerulopathy) primary and initial lesion of glomeruli
 Classification of glomerulopathy • Glomerulonephritis • Amyloid nephrosis • Nephrotic syndrome – Lipoid nephrosis (minimal change disease) – Focal segmental glomerular hyalinosis – Membranous glomerulopathy
Classification of glomerulopathy • Glomerulonephritis • Amyloid nephrosis • Nephrotic syndrome – Lipoid nephrosis (minimal change disease) – Focal segmental glomerular hyalinosis – Membranous glomerulopathy
 GLOMERULONEPHRITIS double-sided non purulent inflammation of glomerular system of the infectious-allergic or unstated nature.
GLOMERULONEPHRITIS double-sided non purulent inflammation of glomerular system of the infectious-allergic or unstated nature.
 Etiology of Glomerulonephritis • Bacterial – hemolytic streptococcus, staphylococcus, pneumococcus, viruses • Non-bacterial - alcohol, drugs, cool trauma
Etiology of Glomerulonephritis • Bacterial – hemolytic streptococcus, staphylococcus, pneumococcus, viruses • Non-bacterial - alcohol, drugs, cool trauma
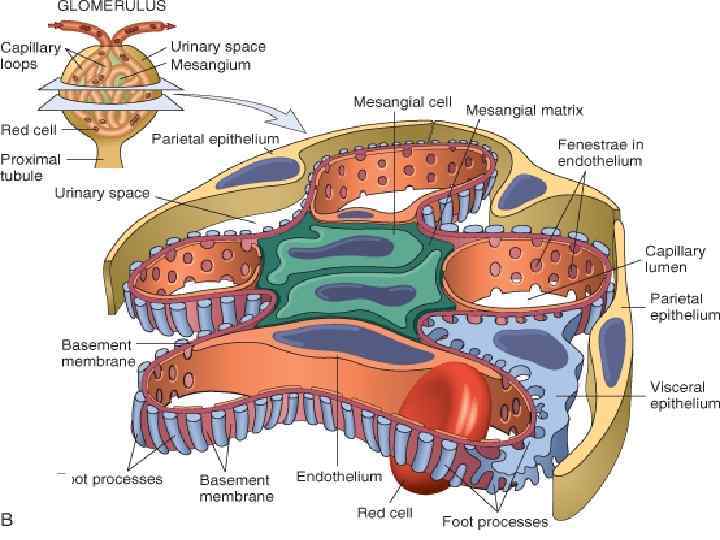
 Pathogenesis of Glomerulonephritis • Antibodies mechanism • Immune complex mechanism: 1) heterologic 2) autologic
Pathogenesis of Glomerulonephritis • Antibodies mechanism • Immune complex mechanism: 1) heterologic 2) autologic
 Pathogenesis Circulative immune complexes or antibodies are fixed on basal membrane→ Injure of basal membrane→ Proliferation of mesangial cells→ Mesangial cells produce IM→ They stimulate inflammation in glomerulus.
Pathogenesis Circulative immune complexes or antibodies are fixed on basal membrane→ Injure of basal membrane→ Proliferation of mesangial cells→ Mesangial cells produce IM→ They stimulate inflammation in glomerulus.
 Classification according to process localization • intracapillary • extracapillary
Classification according to process localization • intracapillary • extracapillary
 Intracapillary glomerulonephritis 1. Exudative: infiltration by leucocytes, edema, hyperemia. 2. Proliferative: membranous, mesangial, membranous-proliferative, fibroplastic.
Intracapillary glomerulonephritis 1. Exudative: infiltration by leucocytes, edema, hyperemia. 2. Proliferative: membranous, mesangial, membranous-proliferative, fibroplastic.
 Extracapillary glomerulonephritis 1. Exudative: serous, fibrinous, hemorrhagic 2. Proliferative: with formation of semilunes
Extracapillary glomerulonephritis 1. Exudative: serous, fibrinous, hemorrhagic 2. Proliferative: with formation of semilunes
 Classification according to the course: • acute – 1, 5 -12 months • subacute – 6 months - 1, 5 years (“large motley (gay) kidney”) • chronic – more than 10 years (“secondary-wrinkled kidney”)
Classification according to the course: • acute – 1, 5 -12 months • subacute – 6 months - 1, 5 years (“large motley (gay) kidney”) • chronic – more than 10 years (“secondary-wrinkled kidney”)
 Clinical manifestations of all glomerulonephrites: - Proteinuria - Edema - Arterial hypertension
Clinical manifestations of all glomerulonephrites: - Proteinuria - Edema - Arterial hypertension



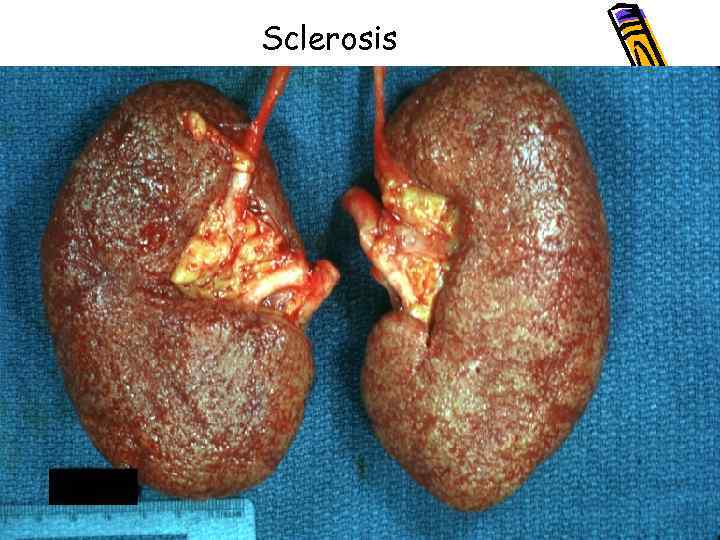 Sclerosis
Sclerosis
 Complications of glomerulonephritis: acute renal failure, uremia. ( Most patients are hypertensive, and sometimes the dominant clinical manifestation is cerebral or cardiovascular) cardiovascular failure, cerebral hemorrhage.
Complications of glomerulonephritis: acute renal failure, uremia. ( Most patients are hypertensive, and sometimes the dominant clinical manifestation is cerebral or cardiovascular) cardiovascular failure, cerebral hemorrhage.
 AMYLOID NEPHROSIS: More often it‘s secondary amyloidosis (due to tuberculosis, syphilis, rheumatism, chronic inflammation - osteomyelitis, chronic abscesses)
AMYLOID NEPHROSIS: More often it‘s secondary amyloidosis (due to tuberculosis, syphilis, rheumatism, chronic inflammation - osteomyelitis, chronic abscesses)
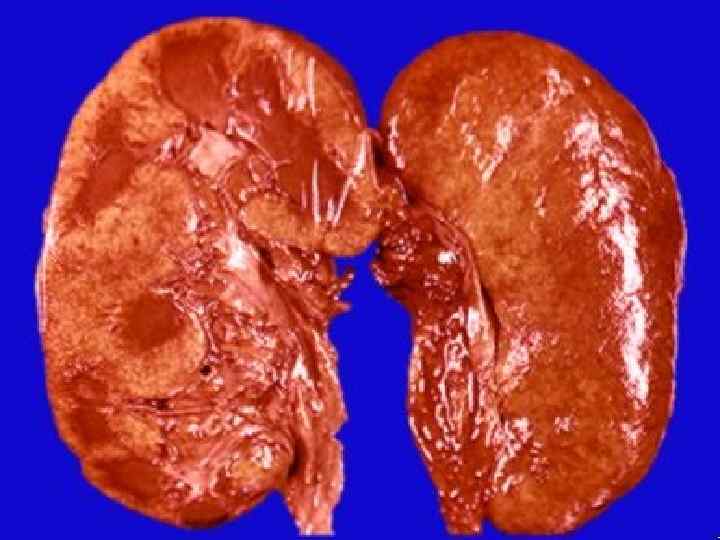
 Stages of renal amyloidosis • 1. Latent: amyloidosis and sclerosis in stroma of pyramids; • 2. Proteinuremic: amyloidosis of glomeruli, stroma, vessels; • 3. Nephrotic: amyloidosis of glomeruli, stroma, vessels, dystrophy of tubules (“big sebaceous kidney”); • 4. Azotemic: amyloid-wrinkled kidneys.
Stages of renal amyloidosis • 1. Latent: amyloidosis and sclerosis in stroma of pyramids; • 2. Proteinuremic: amyloidosis of glomeruli, stroma, vessels; • 3. Nephrotic: amyloidosis of glomeruli, stroma, vessels, dystrophy of tubules (“big sebaceous kidney”); • 4. Azotemic: amyloid-wrinkled kidneys.


 Nephrotic syndrome 1. Lipoid nephrosis (minimal change disease) 2. Focal segmental glomerular hyalinosissclerosis 3. Membranous glomerulopathy
Nephrotic syndrome 1. Lipoid nephrosis (minimal change disease) 2. Focal segmental glomerular hyalinosissclerosis 3. Membranous glomerulopathy
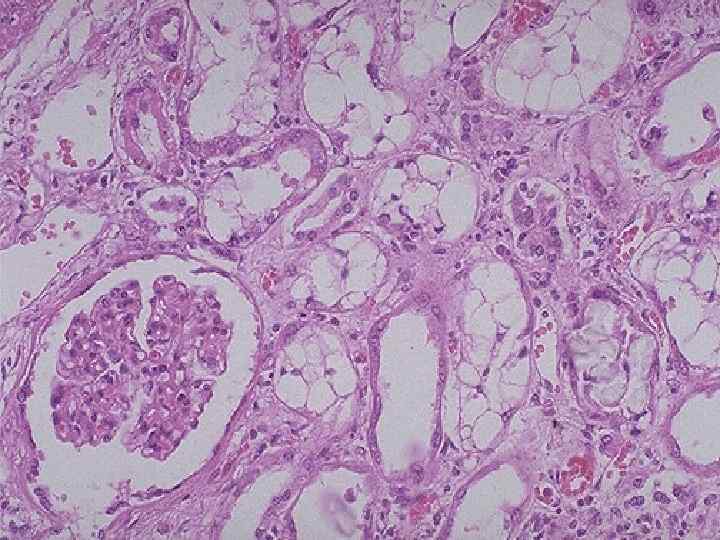
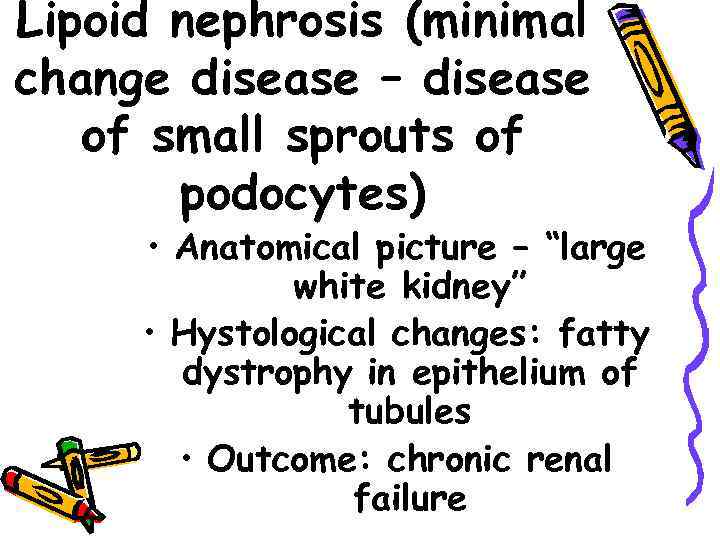 Lipoid nephrosis (minimal change disease – disease of small sprouts of podocytes) • Anatomical picture – “large white kidney” • Hystological changes: fatty dystrophy in epithelium of tubules • Outcome: chronic renal failure
Lipoid nephrosis (minimal change disease – disease of small sprouts of podocytes) • Anatomical picture – “large white kidney” • Hystological changes: fatty dystrophy in epithelium of tubules • Outcome: chronic renal failure
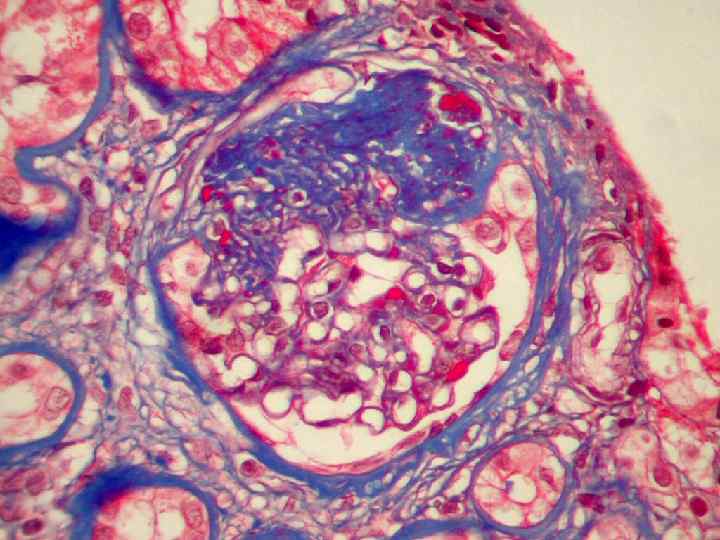
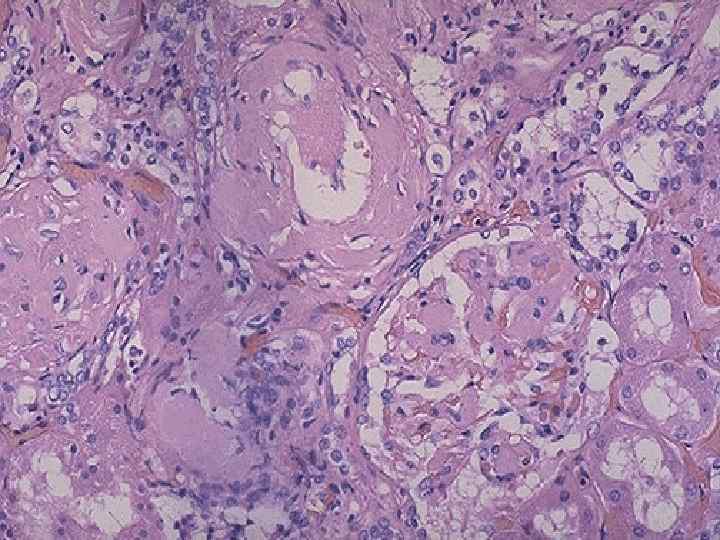
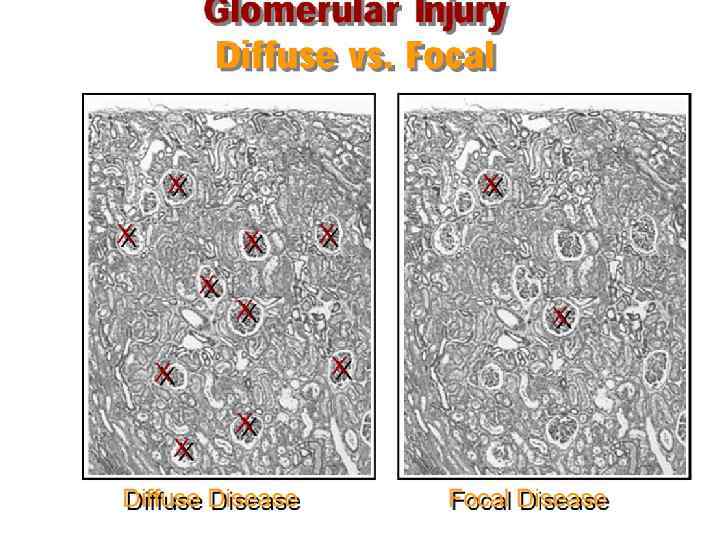
 Focal segmental glomerular hyalinosis (sclerosis) 1. Some glomeruli show partial (segmental) hyalinization 2. Unknown pathogenesis 3. Poor prognosis
Focal segmental glomerular hyalinosis (sclerosis) 1. Some glomeruli show partial (segmental) hyalinization 2. Unknown pathogenesis 3. Poor prognosis

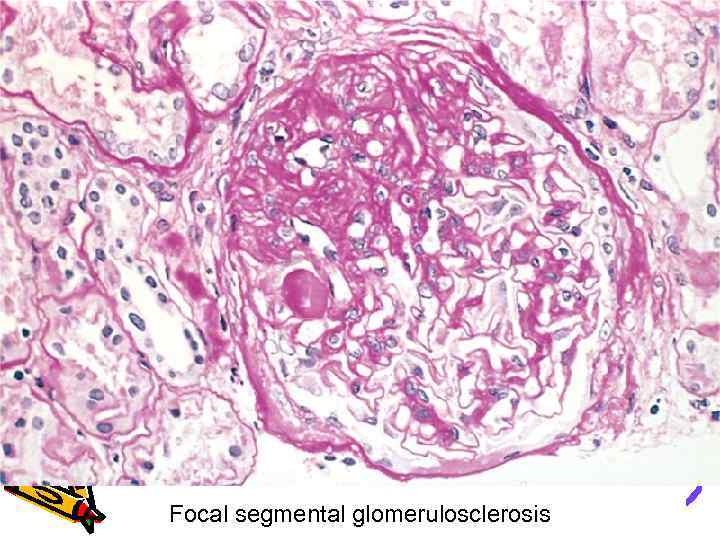 Focal segmental glomerulosclerosis
Focal segmental glomerulosclerosis
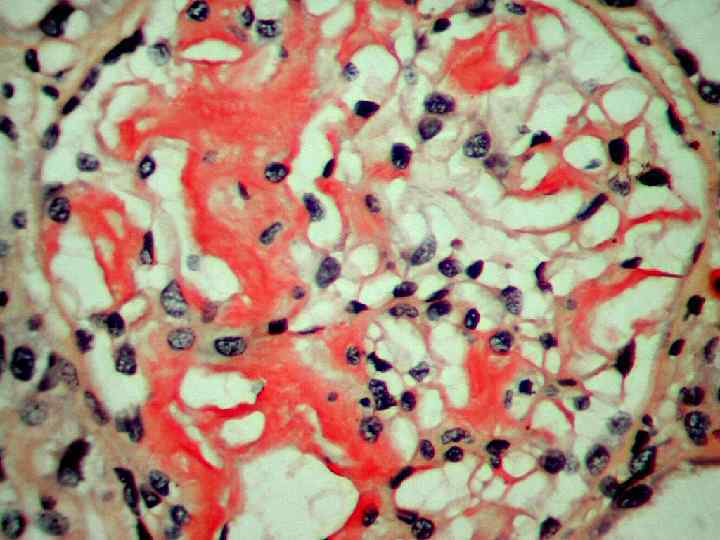
 Membranous glomerulopathy 1. Autoimmune reaction against unknown renal antigen 2. Immune complexes 3. Thickened GBM 4. Looks like membranous glomerulonephritis
Membranous glomerulopathy 1. Autoimmune reaction against unknown renal antigen 2. Immune complexes 3. Thickened GBM 4. Looks like membranous glomerulonephritis
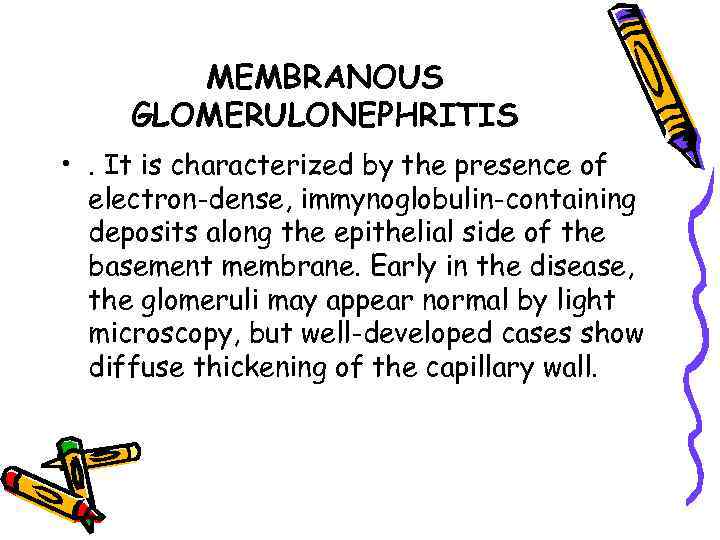 MEMBRANOUS GLOMERULONEPHRITIS • . It is characterized by the presence of electron-dense, immynoglobulin-containing deposits along the epithelial side of the basement membrane. Early in the disease, the glomeruli may appear normal by light microscopy, but well-developed cases show diffuse thickening of the capillary wall.
MEMBRANOUS GLOMERULONEPHRITIS • . It is characterized by the presence of electron-dense, immynoglobulin-containing deposits along the epithelial side of the basement membrane. Early in the disease, the glomeruli may appear normal by light microscopy, but well-developed cases show diffuse thickening of the capillary wall.
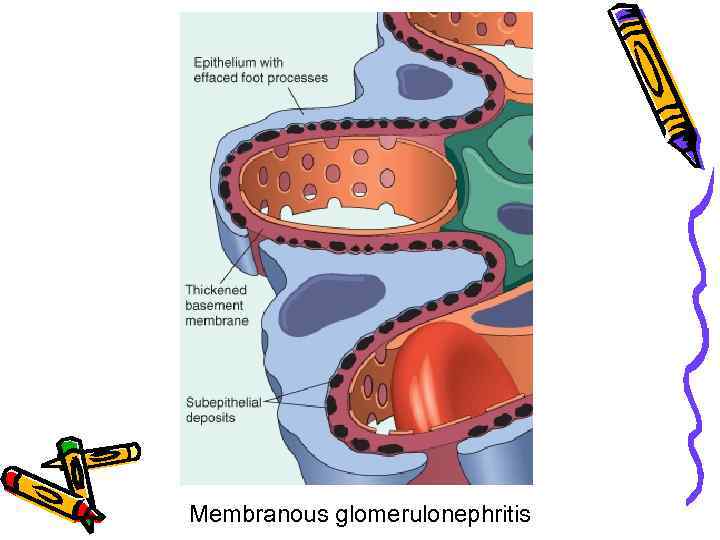 Membranous glomerulonephritis
Membranous glomerulonephritis
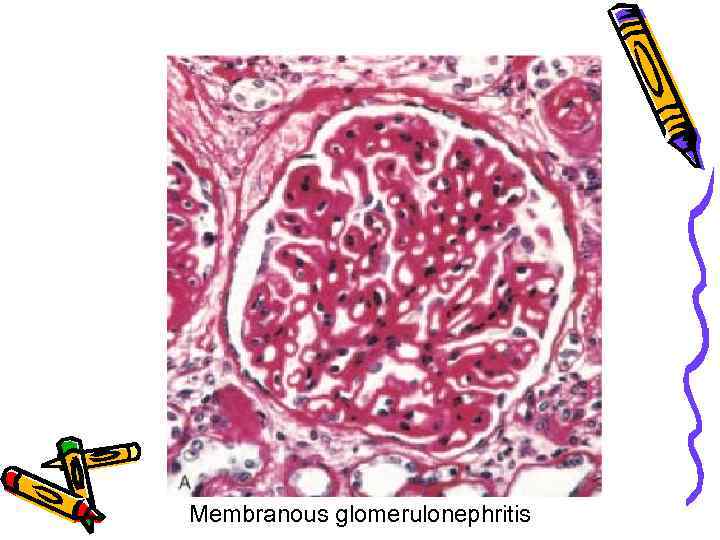 Membranous glomerulonephritis
Membranous glomerulonephritis
 TUBULOPATHY it‘s initial or leading lesion of tubules epithelium
TUBULOPATHY it‘s initial or leading lesion of tubules epithelium
 TUBULOPATHY • Acute course - acute renal failure or necrotic nephrosis • Chronic course – "myeloma kidney", "gouty kidney".
TUBULOPATHY • Acute course - acute renal failure or necrotic nephrosis • Chronic course – "myeloma kidney", "gouty kidney".
 Acute renal failure (necrotic nephrosis) It‘s syndrome, which morphologically looks like acute tubular necrosis
Acute renal failure (necrotic nephrosis) It‘s syndrome, which morphologically looks like acute tubular necrosis
 Acute tubular necrosis • Acute tubular necrosis is a clinicopathologic entity characterized morphologically by destruction of tubular epithelial cells and clinically by acute suppression of renal function. It is the most common cause of acute renal failure.
Acute tubular necrosis • Acute tubular necrosis is a clinicopathologic entity characterized morphologically by destruction of tubular epithelial cells and clinically by acute suppression of renal function. It is the most common cause of acute renal failure.
 Pathogenesis of acute renal failure • Direct – nephrotoxical substances influence to epithelium • Indirect
Pathogenesis of acute renal failure • Direct – nephrotoxical substances influence to epithelium • Indirect
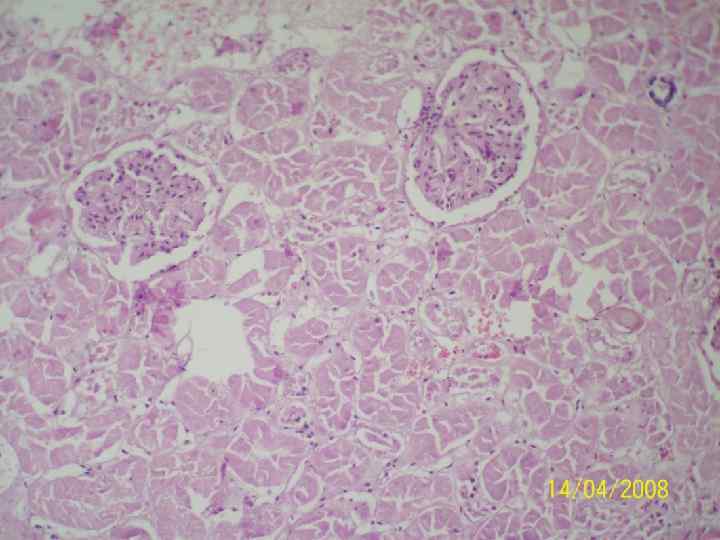
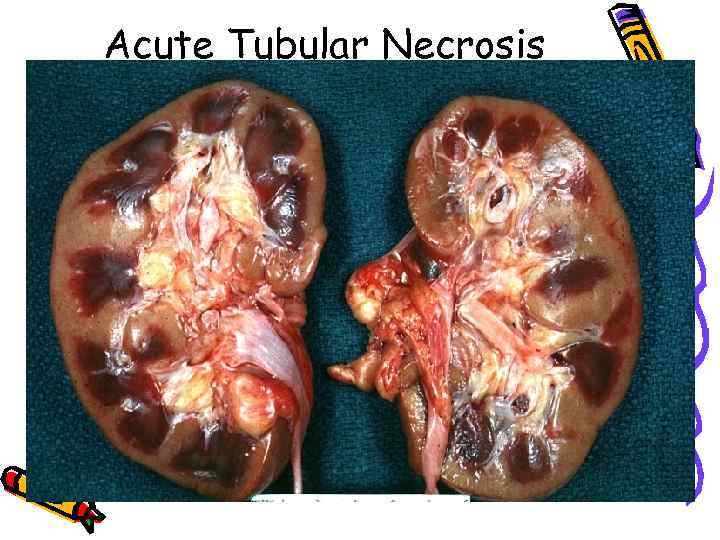 Acute Tubular Necrosis
Acute Tubular Necrosis
 Stages of development of acute renal failure • shock stage - collapse of capillaries of glomeruli, dystrophy of tubules epithelium; • oligoanuric stage - necrosis of tubules epithelium, edema, infiltration of stroma • Regenerative (recover) stage hyperemia of glomeruli, regeneration of tubules epithelium, focal nephrosclerosis
Stages of development of acute renal failure • shock stage - collapse of capillaries of glomeruli, dystrophy of tubules epithelium; • oligoanuric stage - necrosis of tubules epithelium, edema, infiltration of stroma • Regenerative (recover) stage hyperemia of glomeruli, regeneration of tubules epithelium, focal nephrosclerosis
 Outcomes of acute renal failure • recovery • uremia
Outcomes of acute renal failure • recovery • uremia
 uremia • azotemia is a biochemical abnormality that refers to an elevation of the blood urea nitrogen and creatinite levels and is related largely to a decreased glomerular filtration rate. When azotemia becomes associated with a constellation of clinical signs and symptoms and biochemical abnormalities, it is termed uremia.
uremia • azotemia is a biochemical abnormality that refers to an elevation of the blood urea nitrogen and creatinite levels and is related largely to a decreased glomerular filtration rate. When azotemia becomes associated with a constellation of clinical signs and symptoms and biochemical abnormalities, it is termed uremia.
 Renal Cell Carcinoma 1. Derived from tubular epithelium 2. Smoking - predisposing factor! 3. Early wide metastatic spreading. 4. 1 - 3% of malignant tumours
Renal Cell Carcinoma 1. Derived from tubular epithelium 2. Smoking - predisposing factor! 3. Early wide metastatic spreading. 4. 1 - 3% of malignant tumours
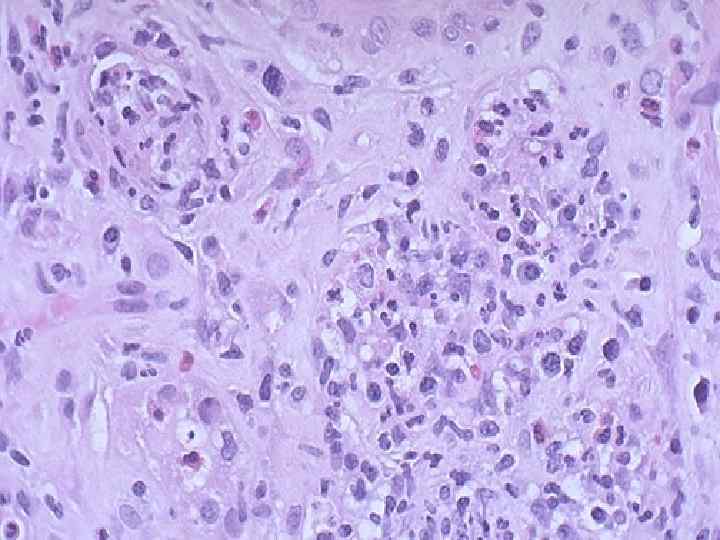
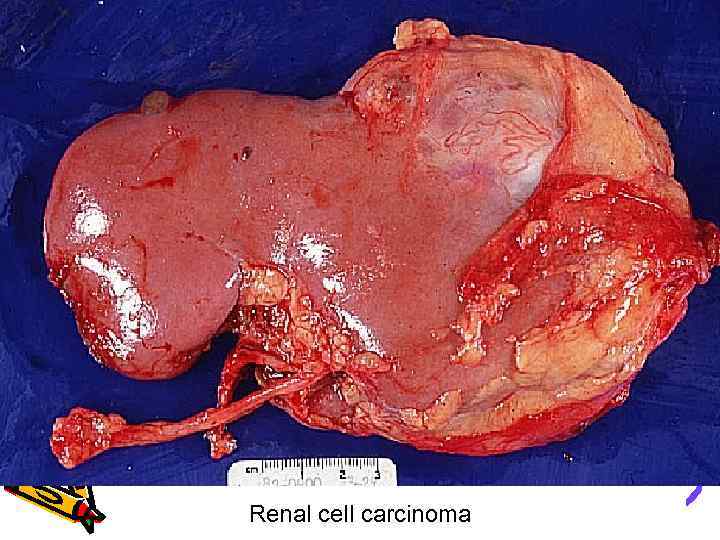 Renal cell carcinoma
Renal cell carcinoma
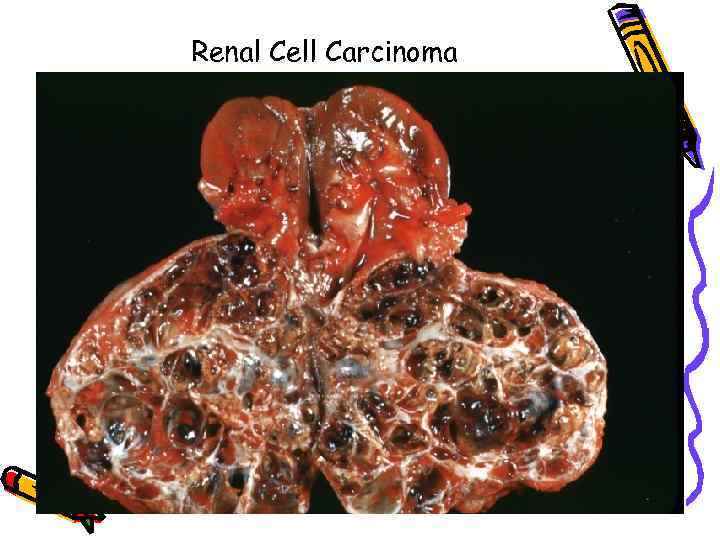 Renal Cell Carcinoma
Renal Cell Carcinoma
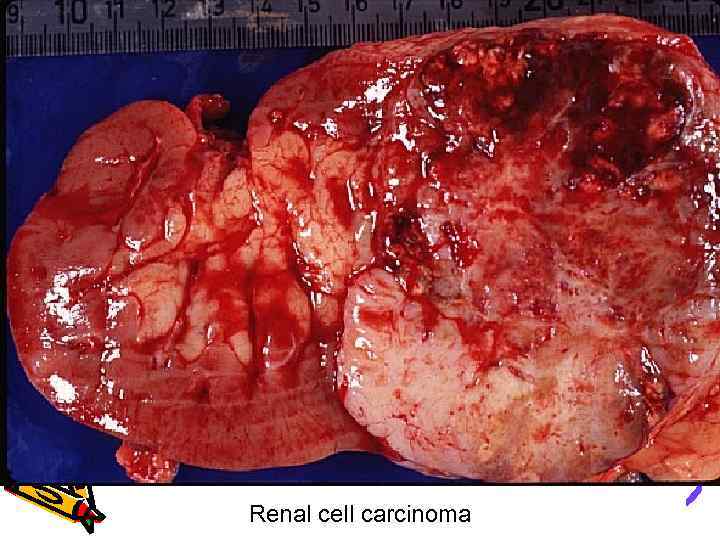 Renal cell carcinoma
Renal cell carcinoma
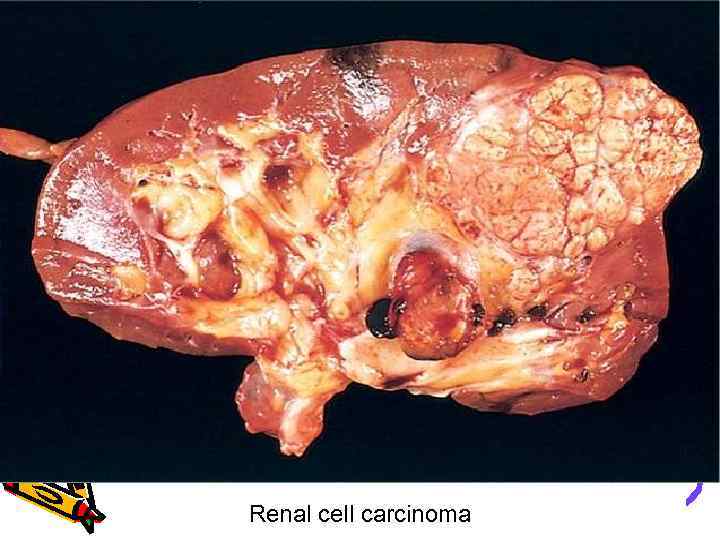 Renal cell carcinoma
Renal cell carcinoma
 Pyelonephritis • Pyelonephritis is a renal disorder affecting tubules, intrestitium, and renal pelvis and is one of the most common diseases of the kidney. It occurs in two forms. Acute pyelonephritis and chronic pyelonephritis.
Pyelonephritis • Pyelonephritis is a renal disorder affecting tubules, intrestitium, and renal pelvis and is one of the most common diseases of the kidney. It occurs in two forms. Acute pyelonephritis and chronic pyelonephritis.
 Pyelonephritis • . Acute pyelonephritis is caused by bacterial infection and is the renal lesion associated with injury tract infection. Chronic pyelonephritis is a more complex disorder: bacterial infection plays a dominant role, but other factors (vesicoureteral reflux, obstruction) are involved in its pathogenesis.
Pyelonephritis • . Acute pyelonephritis is caused by bacterial infection and is the renal lesion associated with injury tract infection. Chronic pyelonephritis is a more complex disorder: bacterial infection plays a dominant role, but other factors (vesicoureteral reflux, obstruction) are involved in its pathogenesis.
 urinary tract infection • The term "urinary tract infection" implies involvement of either the bladder (cystitis) or the kidney and their collecting system (pyelonephritis), or both. Urinary tract infections are extremely common disorders.
urinary tract infection • The term "urinary tract infection" implies involvement of either the bladder (cystitis) or the kidney and their collecting system (pyelonephritis), or both. Urinary tract infections are extremely common disorders.
 etiology The dominant etiologic agents are the gramnegative bacilli that are normal inhabitants of the intestinal tract: E. coli (Proteus, Klebsiella and Enterobacter), Streptococcus faecalis, etc. In most patients with urinary tract infection, the infecting organisms are derived from the patient's own fecal flora. This is thus a form of endogenous infection.
etiology The dominant etiologic agents are the gramnegative bacilli that are normal inhabitants of the intestinal tract: E. coli (Proteus, Klebsiella and Enterobacter), Streptococcus faecalis, etc. In most patients with urinary tract infection, the infecting organisms are derived from the patient's own fecal flora. This is thus a form of endogenous infection.
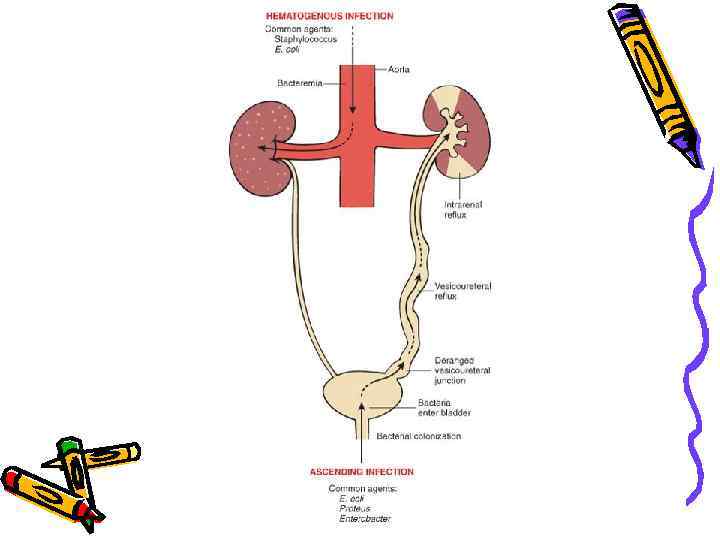
 Ways of infection • There are two routs by which bacteria can reach the kidneys: 1) through the bloodstream (hematogenous), and 2) from the lower urinary tract (ascending infection). Although obstruction is an important predisposing factor in the pathogenesis of ascending infection, it is incompetence of the vesicoureteral orifice that allows bacteria to ascend the ureter into the pelvis.
Ways of infection • There are two routs by which bacteria can reach the kidneys: 1) through the bloodstream (hematogenous), and 2) from the lower urinary tract (ascending infection). Although obstruction is an important predisposing factor in the pathogenesis of ascending infection, it is incompetence of the vesicoureteral orifice that allows bacteria to ascend the ureter into the pelvis.
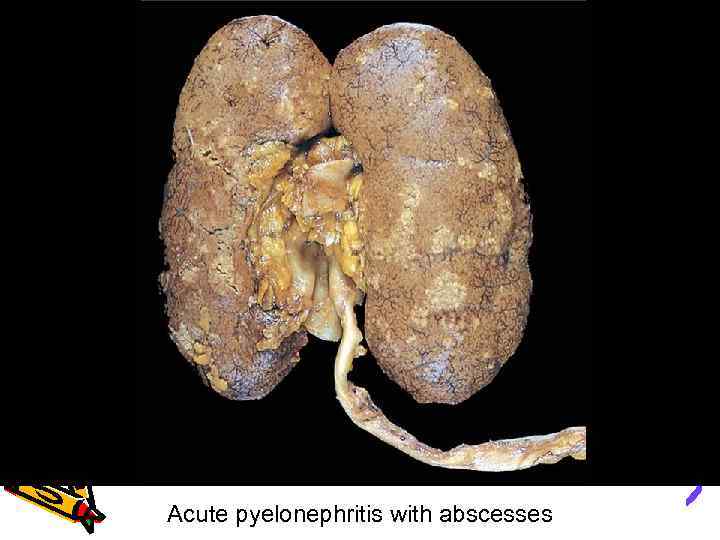 Acute pyelonephritis with abscesses
Acute pyelonephritis with abscesses
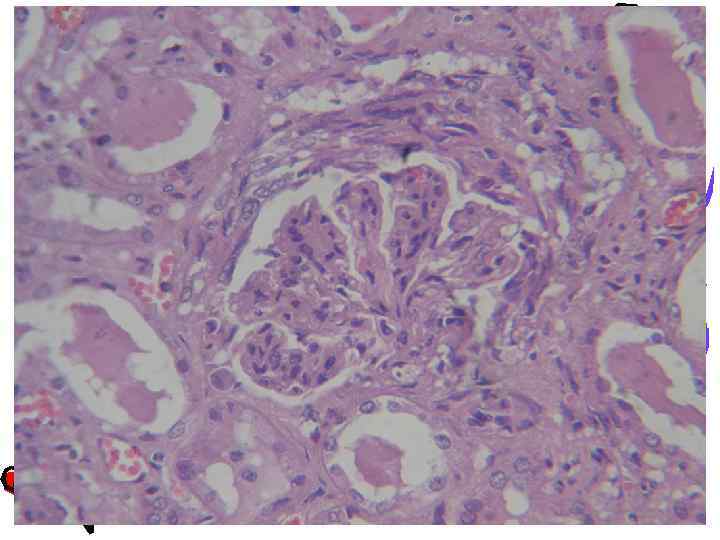
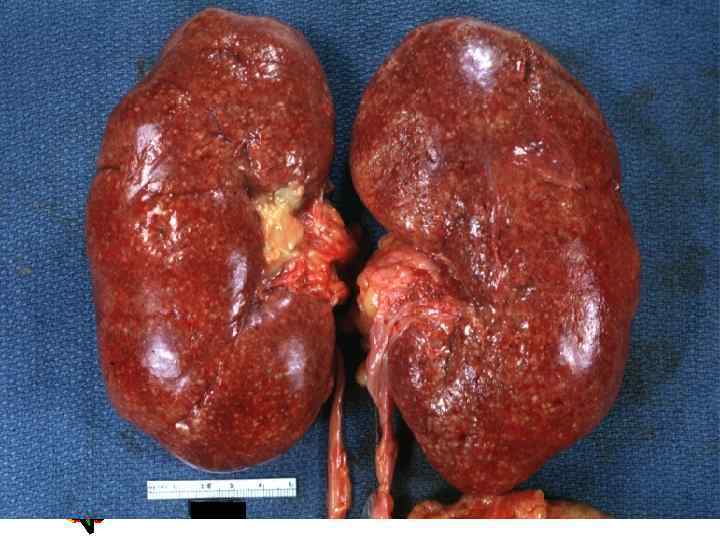 Acute Pyelonephritis
Acute Pyelonephritis
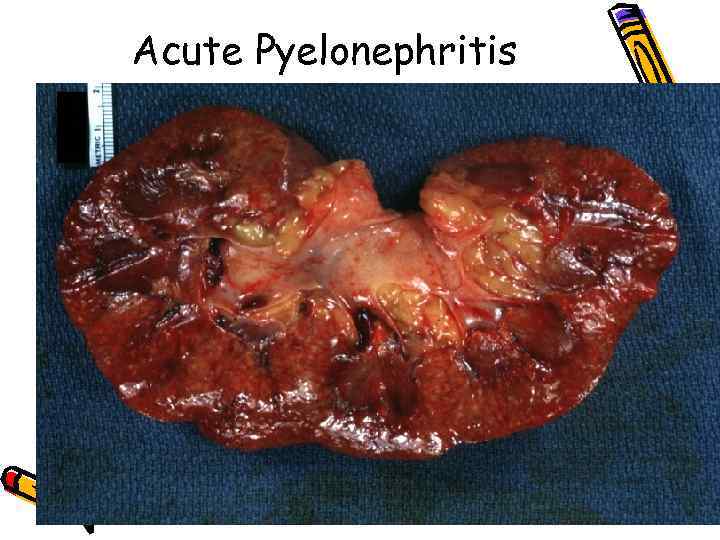 Acute Pyelonephritis
Acute Pyelonephritis
 Pyelonephritis
Pyelonephritis
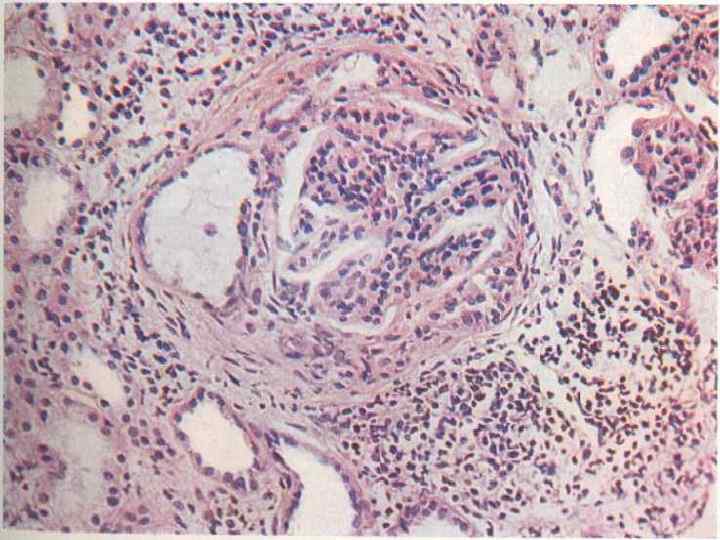
 Chronic pyelonephritis • Chronic pyelonephritis is a chronic tubulointerstitial renal disorder in which chronic tubulointerstitial inflammation and renal scarring are associated with pathologic involvement of the calices and pelvis.
Chronic pyelonephritis • Chronic pyelonephritis is a chronic tubulointerstitial renal disorder in which chronic tubulointerstitial inflammation and renal scarring are associated with pathologic involvement of the calices and pelvis.
 Chronic pyelonephritis • . The kidneys usually are irregularly scarred; if bilateral, the involvement is asymmetric. This contrasts with chronic glomerulonephritis, in which the kidneys are diffusely and symmetrically scarred. The scars can vary from one to several in number and may affect one or both kidneys. Most are in upper and lower poles, consistent with the frequency of reflux in these sites.
Chronic pyelonephritis • . The kidneys usually are irregularly scarred; if bilateral, the involvement is asymmetric. This contrasts with chronic glomerulonephritis, in which the kidneys are diffusely and symmetrically scarred. The scars can vary from one to several in number and may affect one or both kidneys. Most are in upper and lower poles, consistent with the frequency of reflux in these sites.
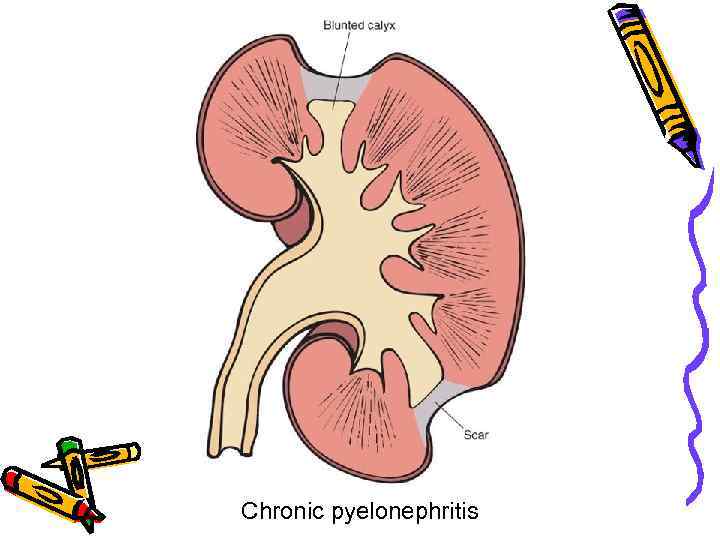 Chronic pyelonephritis
Chronic pyelonephritis
 Chronic pyelonephritis • The appearance of proteinuria and focal segmental glomerulosclerosis is a poor prognostic sign, and many such patients proceed to chronic endstage renal failure.
Chronic pyelonephritis • The appearance of proteinuria and focal segmental glomerulosclerosis is a poor prognostic sign, and many such patients proceed to chronic endstage renal failure.
 THE END
THE END


