c156e080a39f79b8dda46b317b56fa8a.ppt
- Количество слайдов: 61
DISEASE OUTBREAK DEPARTMENT OF EPIDEMIOLOGY AND BIOSTATISTICS 2011 1
§ OUTBREAK § EPIDEMIC § ENDEMIC § PANDEMIC § SEASONAL VARIATION § CHANCE 2
EPIDEMIC/OUTBREAK The occurrence of cases of an illness, specific health-related behavior, or other health-related events, in a community or region, clearly in excess of normal expectations. The community or region and the period in which the cases occur are specified precisely. 3
EPIDEMIC • The number of cases indicating the presence of an epidemic varies according to the agent, size and type of population exposed, previous experience or lack of exposure to the disease, and time and place of occurrence. 4
ENDEMIC The constant presence of a disease or infectious agent within a given geographic area or population group; may also refer to the usual prevalence of a given disease within such area or group 5
PANDEMIC • Worldwide epidemic SEASONAL VARIATION • Change in physiological status or in disease occurrence that conforms to a regular seasonal pattern 6
CHANCE • A set of cases that occur in a short period of time, BUT do not surpass the expected number of cases for the region 7
Infectious Disease (Communicable Disease) An illness due to specific infectious agent or its toxic product that arises through transmission that agent or its products from an infectious person, animal or reservoir to a susceptible host. 8
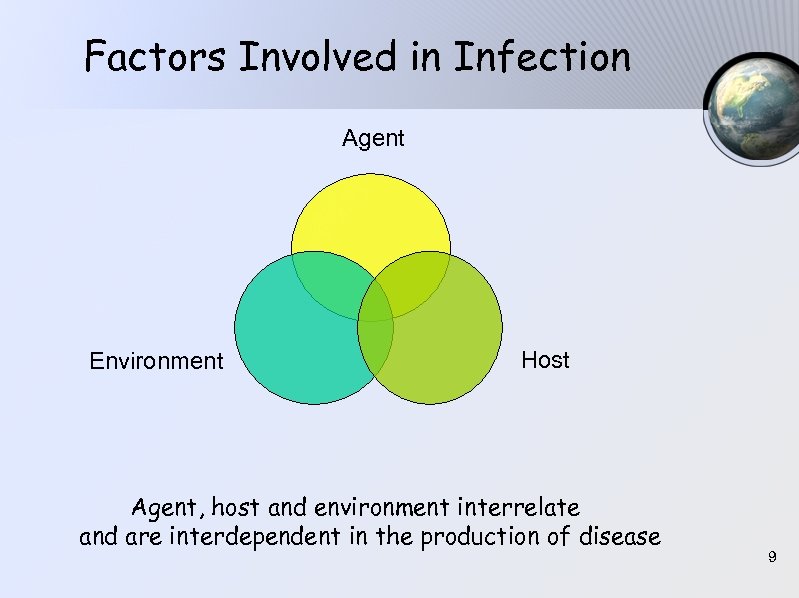
Factors Involved in Infection Agent Environment Host Agent, host and environment interrelate and are interdependent in the production of disease 9
Types of Transmission Direct transmission (person to person) § Direct projection of droplet spray (sneezes and coughs : measles) § Vertical transmission (transplacental, from mother to child : HIV) § Mucosa to mucosa (sexually transmitted disease) § Blood and transplants (hepatitis) § Skin to skin (staphylococcus) 10
Types of Transmission Indirect transmission § Vehicle-borne transmission (water, food, milk, biological products, contaminated materials or objects) § Vector-borne transmission (mechanical, biological) § Airborne transmission (microbial aerosols) 11
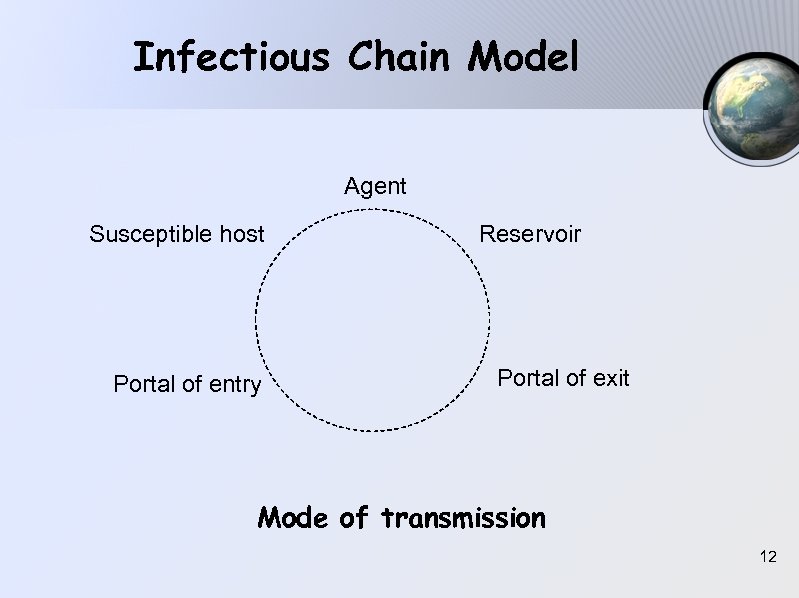
Infectious Chain Model Agent Susceptible host Portal of entry Reservoir Portal of exit Mode of transmission 12
Other Definitions Vehicle Mode of transport of an infectious agent through the environment to a susceptible host. Vector A living carrier (usually an arthropod) that serves as a mode of transport for an infectious agent from an infected host to a susceptible host. Reservoir The primary habitat in which an infectious agent survives and reproduces. 13
Carrier A person or animal that harbors a specific infectious agent in the absence of discernable clinical disease and serves as a potential source of infection. § Asymptomatic carrier Subclinical infection throughout the infectious carrier state § Incubationary carrier Infectious carrier state occurs during the incubation period preceding clinically recognizable disease § Convalescent carrier Infectious carrier state continues during convalescence when clinically recognizable disease is no longer present 14
Periods Exposure period Time during which an individual or group is exposed to a source of infection Incubation period Time from initial infection (entry of infection) to onset of clinical illness. (Usually expressed as the median or sometimes the arithmetic or geometric mean, minimum and maximum incubation period) 15
Periods Infectious (or communicable) period Period during which an infected person is able to transmit the infectious agent. (Important to know this for various agents in order to impose appropriate control measures). 16
Periods Latent period Time from receiving infection to onset of infectiousness. Minimum interval between successive infections in a chain of transmission. 17
Periods Serial interval or generation time Interval between the same stage of illness in sucessive cases in a chain of transmission. (Only applicable when infection spreads from person to person e. g. the interval between onset of rash in the primary case to onset of rash in a secondary case) 18
Use of Periods Useful for several reasons : § § § Quarantine Contact tracing Identification of possible time of infection Outbreak investigation Disease modeling and forecasting 19
Types of Outbreak 1. Common source § § Transmission of an infectious agent involving a source that is common to all outbreak-associated cases Point source : brief common exposure. A single source of pathogen results in exposure of persons at one point in time Extended source : Common source exposure present over days or weeks - intermitten : at several points in time - continuous : over a continuous period Onset will still be abrupt but cases would be spread over a greater period of time than one incubation period 20 depending upon how long the exposure persists.
Types of Outbreak 2. Propagated or progressive (person to person) - Caused by the spread of the pathogen from one susceptible person to another. - The curve tend to have a series of irregular peaks reflecting the number of generations of infection. 3. Mixed epidemic Involves both a common source epidemic and secondary propagated spread to other individuals. Many foodborne pathogens commonly exhibit this mode of spread (hepatitis A, Shigella, E. coli). 21
Elements of Control § Removal or elimination of the source of the pathogen § Blockage of the transmission process § Elimination of susceptibility (e. g. vaccination) 22
DISEASE OUTBREAK INVESTIGATION Data sources § § The public The media Reports of clinical cases from health care providers Surveillance data (laboratory reports, disease notifications) 23
When reports of an outbreak are received, the following information should be gathered : § The person(s) reporting the outbreak § Characteristics of the suspected outbreak (clinical information, suspected etiologies) § Persons directly affected by the outbreak (epidemiological information) 24
Steps in outbreak investigation § § § § Establishing the existence of an outbreak Verifying the diagnosis Defining and counting cases Determining the population at risk Describing the epidemiology Developing hypotheses Evaluating the hypotheses Undertaking additional epidemiological, environmental and laboratory studies, as necessary § Implementing control and prevention measures § Communicating findings 25
CONFIRMATION & VERIFICATION OF DIAGNOSIS § Check the report whether it is true or not (see the case by yourself in the field) § Verify the sign or symptoms and the diagnosis § To proof the case is based on the history of the disease and the sign or symptoms § Estimate the number of cases § If there is sufficient of time, a laboratory examination should be done to make an etiological diagnosis 26
DETERMINE THE EVENT : IS IT AN EPIDEMIC OR NOT? § How much the usual morbidity rate are? § Based on time, place, person § How are the usual pattern of the disease in the community? § Is the disease usually presence or never? § Is there an increase of the number of cases? § Is it conspicuous or not? § Make a graph of epidemic curve based on time of onset of the sign in each case! 27
DESCRIBE THE EPIDEMIC : IN TIME, PLACE AND PERSON TIME • When was the first case founded? The last? • How long the epidemic/outbreak happened? • Find the probable of the first exposed time! • Assume the type of the epidemic! (common source ? person to person? ) 28
PLACE • What place is the most prominent number of cases? • What are the attack rate based on places? PERSON • Identify the age specific and sex specific attack rate! • What group has the highest and the lowest attack rate? • Determine that the characteristic of the cases are differ significantly compared with the whole population 29
COLLECTING DATA § To get the real data. § Can be simultaneously with the activity of diagnosis verification : - What are the exact number of cases ? - Who are the population at risk ? - Who are the contact person ? - Think about loss of observation ! - Who are the carrier ? § Those data could be obtained by house to house visits ! 30
IDENTIFICATION OF AGENT OR THE SOURCE OF INFECTION AND TRANSMISSION First we have to set hypothesis of : • The etiological agent • The source of infection • The exposure time • The incubation period • The transmission of infection • The population at risk 31
EPIDEMIC CONTROL (MANAGEMENT) 1. THE PATIENT Adequate and prompt treatment 2. CONTROLLING against : • the primary source of infection • the reservoir (carrier, vector, environment) • Transmission vehicle (food, fluid, air etc. ) • Susceptible contact person 3. EPIDEMIOLOGICAL SURVEILLANCE 32
INVESTIGATION REPORT The main objection of the report is to describe the experience and all findings in the occurrence of epidemic, to organize and operate a surveillance activity and to improve the previous prevention and controlling activity. 33
INVESTIGATION REPORT The form of the report are : 1. INTRODUCTION It content description of the condition that stimulate to carry out an investigation. 2. BACKGROUND A brief description about factors that cause the problem (e. g. geographic, politic, economic, demographic and historic) 34
3. DESCRIPTION OF INVESTIGATION ARRANGEMENT Include : - the reason - the method - source of information - how to explore the cases - verification of diagnoses - use of sample cases and control in analyzing data, etc. 35
4. THE FINDINGS • Only the fact finding should be reported; without any comment, discussion or suggestion. The recent data could be related to the previous data as it happened as an epidemic. • The findings will be presented in tables or graph such as : - characteristic table of age, sex, race, occupation etc. and their attack rate - the onset of illness with the graph - the result of laboratory test - other evidence which might direct the possibility of the source of infection or suspected source. 36
ANALYZING DATA AND CONCLUSION Data should be interpreted to construct hypothesis of : - agent of infection - source of infection - reservoir - disease transmission, including the vehicle or vector - the high risk group population It is exactly useful if the characteristic of the recent epidemic compared with the similar epidemic before. 37
DESCRIBE THE CONTROL ACTION Clarify the objective of the action specifically. Discuss each of this action based on : How, When, Where and by Whom. Describe the results and the expenses of the actions. Explain that there might be possibility of explosion of new cases after passing one incubation period after the control action. 38
DESCRIBE THE OUTCOMES a. The consequences of the epidemic to health condition and economic status b. The consequences of the control action to : Population → immunity status, way of life, etc. Reservoir → number and distribution Vector → number, density, distribution c. The invention of new infectious agent, reservoir, transmission of agent etc. 39
RECOMMENDATION The objection is to improve the surveillance activity and control. These report can be useful as reference in surveillance activity, what data should be collected, what is the source of data, how to consolidate after an epidemic, dissemination of the report, who will be responsible in an epidemic, what kind of cooperation should be organized. 40
EPIDEMIC CURVE A graph of cases of disease plotted against time (date or hour) of onset of illness. Mainly used in outbreak investigation. 41
EPIDEMIC CURVE STEPS OF MAKING DIAGRAM 1. Draw the X and Y line : X for time of onset of cases Y for the number of cases 2. Select interval of time depend on the incubation period of the disease, e. g. hourly, daily, weekly or monthly To estimate the first contact or exposed to source of the disease : 1. Take a line from the first case(s) backward at length of 14 days (the minimum I. P. ) and from the last case(s) at length of 21 days (maximum I. P. ). The results are fallen at the 7 th and 8 th days; it means that the first contact to the source of disease was at the 7 th and 8 th days. 2. It can also can be done by subtraction the last and the first time of onset by the maximum and the minimum incubation period 42
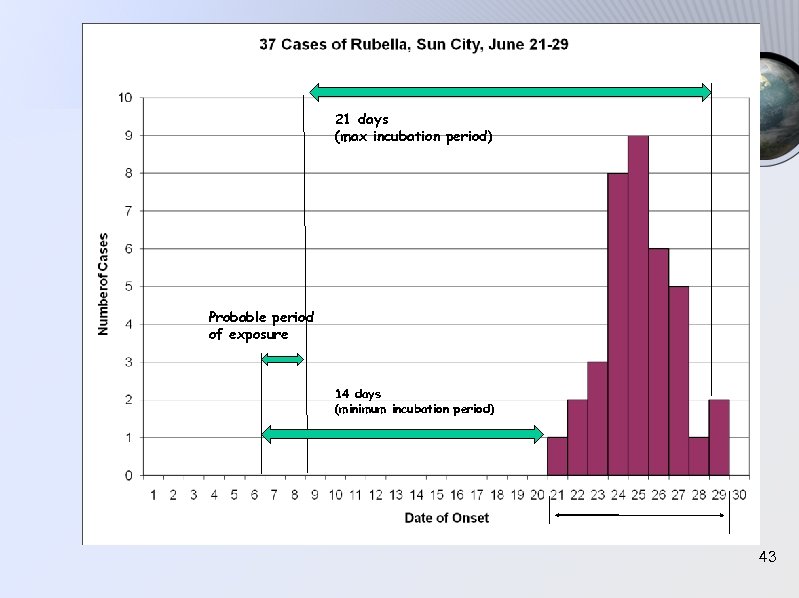
21 days (max incubation period) Probable period of exposure 14 days (minimum incubation period) 43
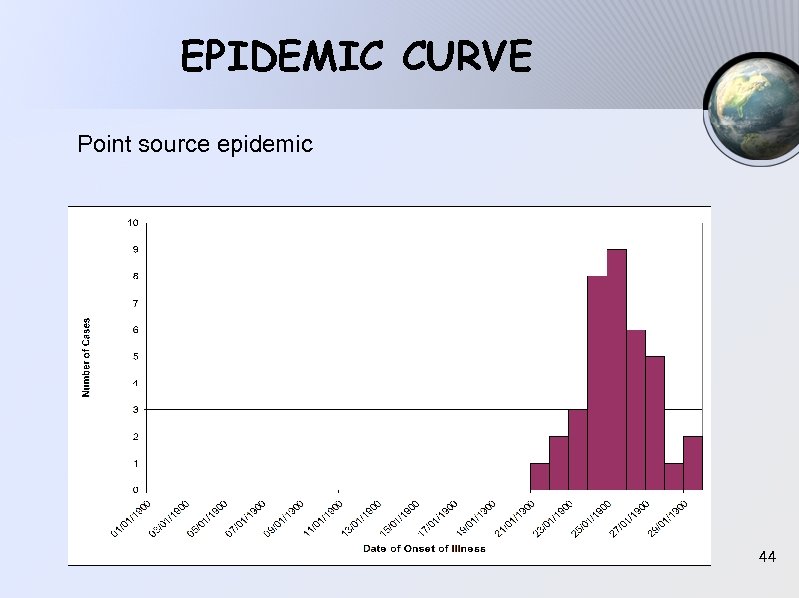
EPIDEMIC CURVE Point source epidemic 44
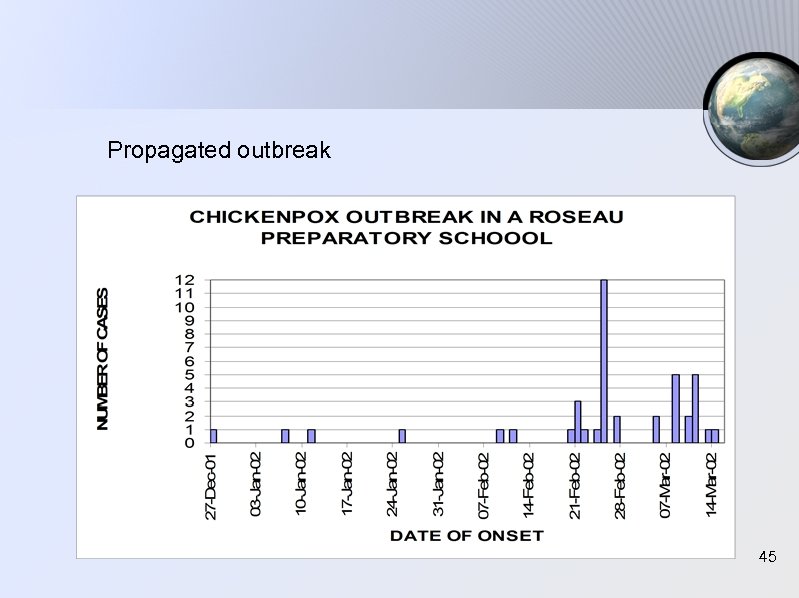
Propagated outbreak 45
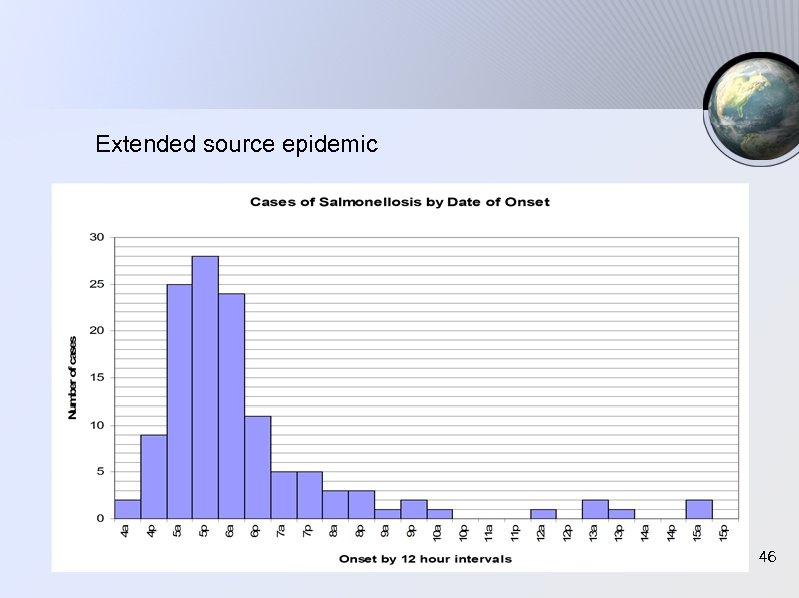
Extended source epidemic 46
ATTACK RATE Similar as incidence rate : new events / cases Incidence Rate = x k Population at risk It is used in a short period of an event - an outbreak -, the population being affected is limited closely, the duration of epidemic is short period. 47
Outbreak Control Team (OCT) The criteria for convening a multidisciplinary OCT will vary according to the seriousness of the illness, its geographical spread, local circumstances and the available resources. 48
An OCT may be considered when : § The outbreak poses an immediate health hazard to the local population § There are many cases § The disease is important in terms of its severity or its propensity to spread § Cases have occured over a widespread area without obvious point source § Cases have occured in high-risk establishments (schools, day-care centres, hospitals, food premises, etc. ) 49
The role of the OCT : to coordinate all the activities involved in the investigation and control of an outbreak. This may involve : 1. Deciding whethere is really an outbreak 2. Deciding on the type of investigations to be conducted 3. Case-finding and interviews 4. Planning the appropriate clinical and environmental sampling 50
5. Ensuring that all collaborators use a complementary methodology 6. Conducting an environmental investigation of suspected source 7. Agreeing and implementing control measures to prevent the further spread 8. Working in concert with local medical providers to make recommendations on treatment and/or prophylaxis 51
9. Organizing ongoing communications among OCT members about the outbreak 10. Making arrangements for liaison with the media 11. Producing reports, including lessons learned, for health authorities and other interested parties 12. Requesting external assistance (e. g. secondment of a national investigation team) 52
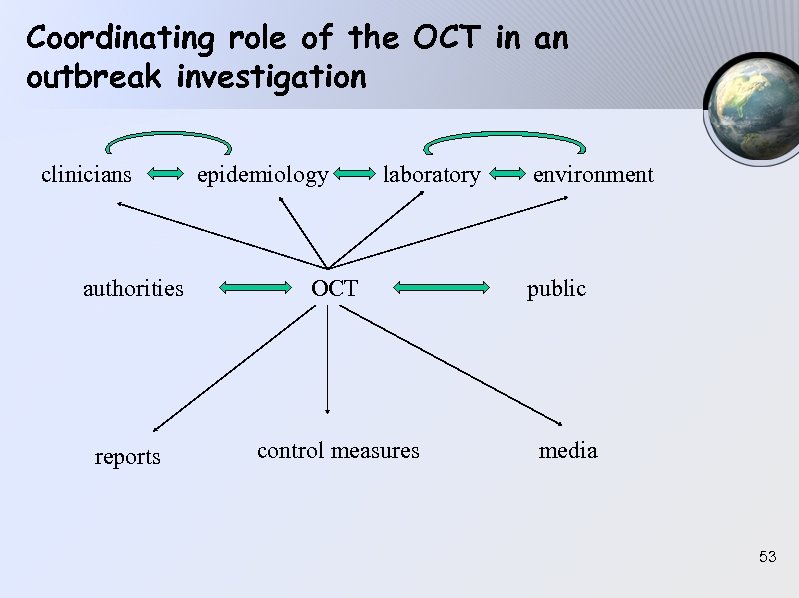
Coordinating role of the OCT in an outbreak investigation clinicians epidemiology laboratory authorities OCT reports control measures environment public media 53
Definitions in an outbreak investigation CLINICAL DESCRIPTION Sign and symptoms found in the outbreak CASE DEFINITION • Standard set of criteria for deciding whether an individual should be classified as having the health condition of interest. • A case definition includes clinical criteria and particularly in the setting of an outbreak investigation restrictions by time, place, and person. 54
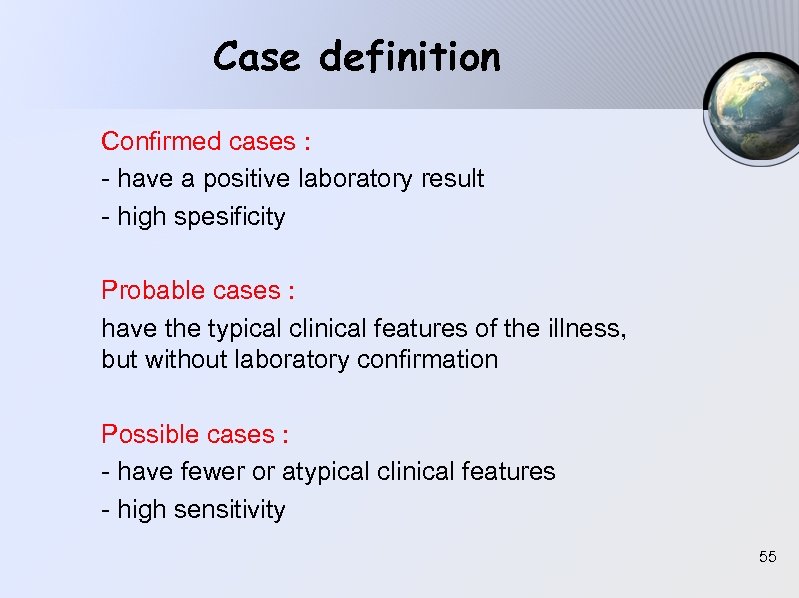
Case definition Confirmed cases : - have a positive laboratory result - high spesificity Probable cases : have the typical clinical features of the illness, but without laboratory confirmation Possible cases : - have fewer or atypical clinical features - high sensitivity 55
DIFFERENTIAL DIAGNOSIS List of possible diagnosis, ordered from the most possible one DESCRIPTIVE EPIDEMIOLOGY Characterize the outbreak by time, place and person 56
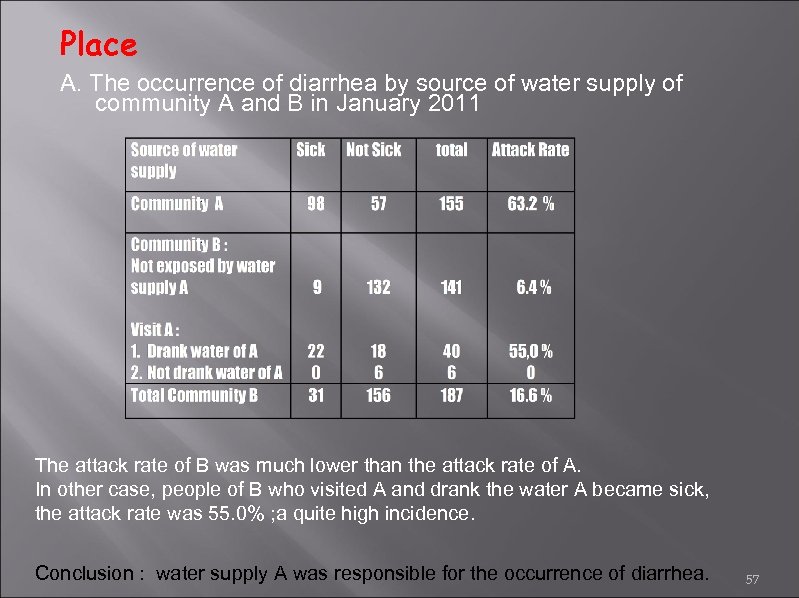
Place A. The occurrence of diarrhea by source of water supply of community A and B in January 2011 The attack rate of B was much lower than the attack rate of A. In other case, people of B who visited A and drank the water A became sick, the attack rate was 55. 0% ; a quite high incidence. Conclusion : water supply A was responsible for the occurrence of diarrhea. 57
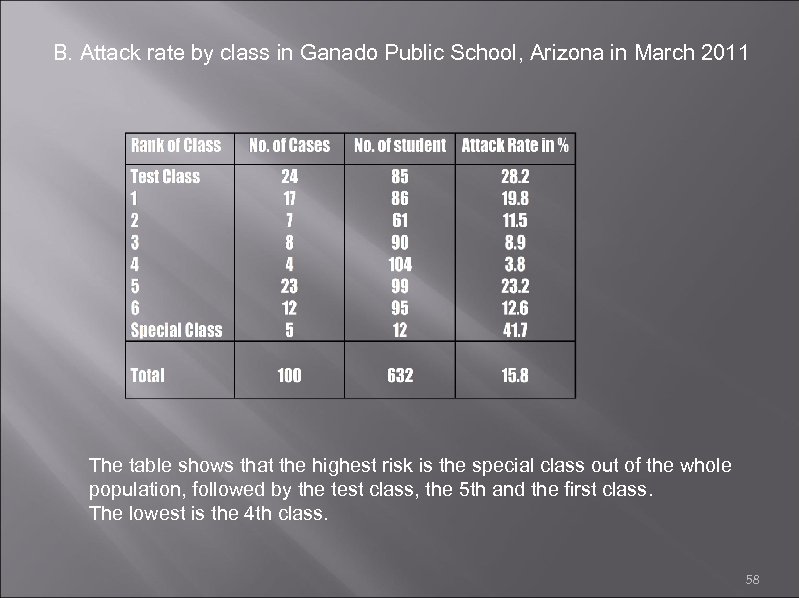
B. Attack rate by class in Ganado Public School, Arizona in March 2011 The table shows that the highest risk is the special class out of the whole population, followed by the test class, the 5 th and the first class. The lowest is the 4 th class. 58
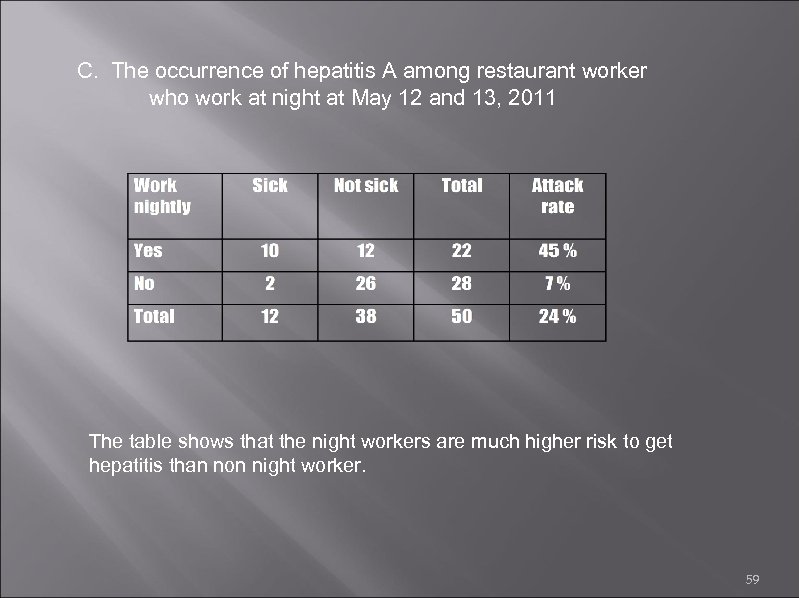
C. The occurrence of hepatitis A among restaurant worker who work at night at May 12 and 13, 2011 The table shows that the night workers are much higher risk to get hepatitis than non night worker. 59
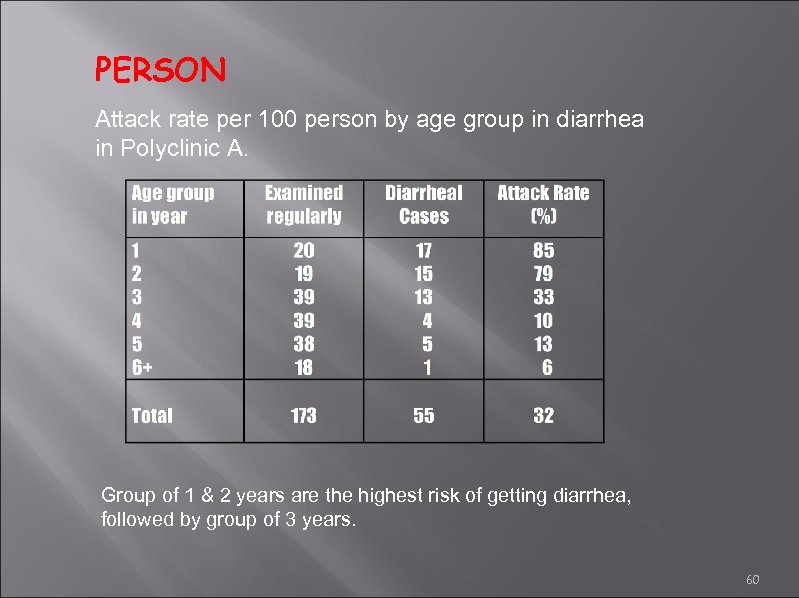
PERSON Attack rate per 100 person by age group in diarrhea in Polyclinic A. Group of 1 & 2 years are the highest risk of getting diarrhea, followed by group of 3 years. 60
Thank you. . . ! See you in lab activity. . 61
c156e080a39f79b8dda46b317b56fa8a.ppt