1c45e2483611d994df751d0936a5a82c.ppt
- Количество слайдов: 14
Disaster Planning Drills and Readiness Assessment Gary B. Green, MD, MPH, FACEP Associate Professor of Emergency Medicine & Pathology Johns Hopkins University School of Medicine and Johns Hopkins University Evidence-Based Practice Center President, Emergency International, Inc.
“Training of Clinicians for Public Health Events Relevant to Bioterrorism Preparedness” (AHRQ Evidence Report/Technology Assessment #51) n n n First evidence based report on this topic Work sponsored by AHRQ, done by JHU EPC Structured review & evaluation of literature Released January 2002 Available on Web at: www. ahrq. gov
Current Evidence About Hospital Disaster Preparedness Training n n n n Very few high quality/scientifically based publications Basic “building blocks” of response system established Variety of training, assessment techniques reported Drills shown to be effective training tools Drills are dual purpose, also provide opportunity for system evaluation Terminology not yet standardized “Best” practices not yet defined Rapid development and dissemination of training and evaluation techniques (growing “toolbox”)
Basic Steps Toward Hospital Disaster Preparedness n n n n Assemble key stakeholders into interdisciplinary team Review current resources, strengths, weaknesses Develop detailed, written response plan Disseminate and practice plan Evaluate adequacy of knowledge, skills and resources Review and re-engineer plan based on data Modify training as needed to target weaknesses Continuously repeat cycle
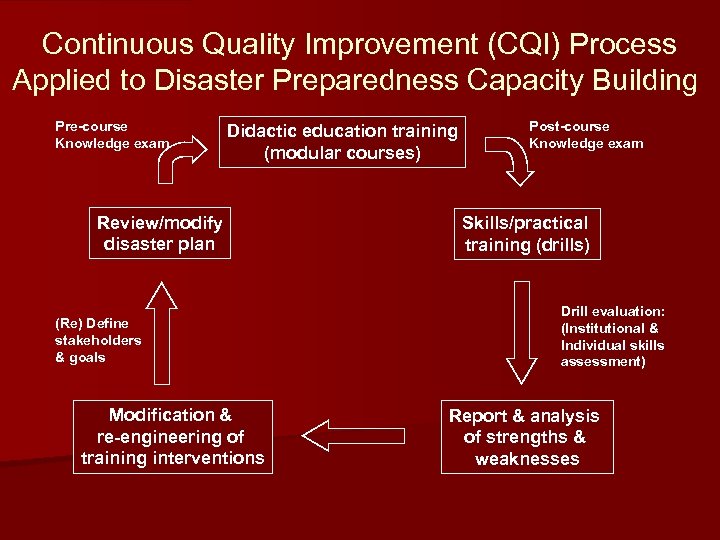
Continuous Quality Improvement (CQI) Process Applied to Disaster Preparedness Capacity Building Pre-course Knowledge exam Didactic education training (modular courses) Review/modify disaster plan (Re) Define stakeholders & goals Modification & re-engineering of training interventions Post-course Knowledge exam Skills/practical training (drills) Drill evaluation: (Institutional & Individual skills assessment) Report & analysis of strengths & weaknesses
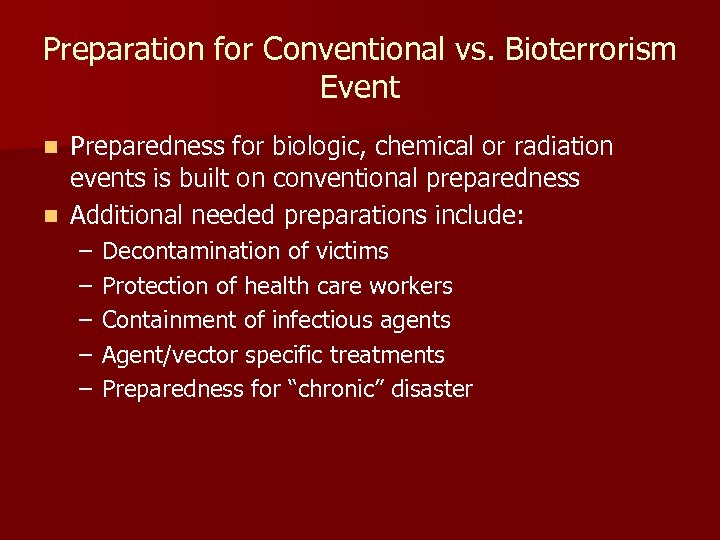
Preparation for Conventional vs. Bioterrorism Event Preparedness for biologic, chemical or radiation events is built on conventional preparedness n Additional needed preparations include: n – – – Decontamination of victims Protection of health care workers Containment of infectious agents Agent/vector specific treatments Preparedness for “chronic” disaster
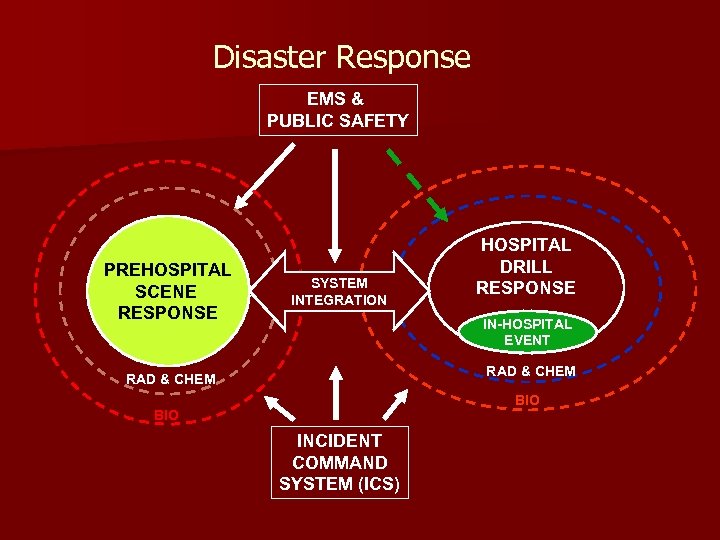
Disaster Response EMS & PUBLIC SAFETY PREHOSPITAL SCENE RESPONSE SYSTEM INTEGRATION HOSPITAL DRILL RESPONSE IN-HOSPITAL EVENT RAD & CHEM BIO INCIDENT COMMAND SYSTEM (ICS)
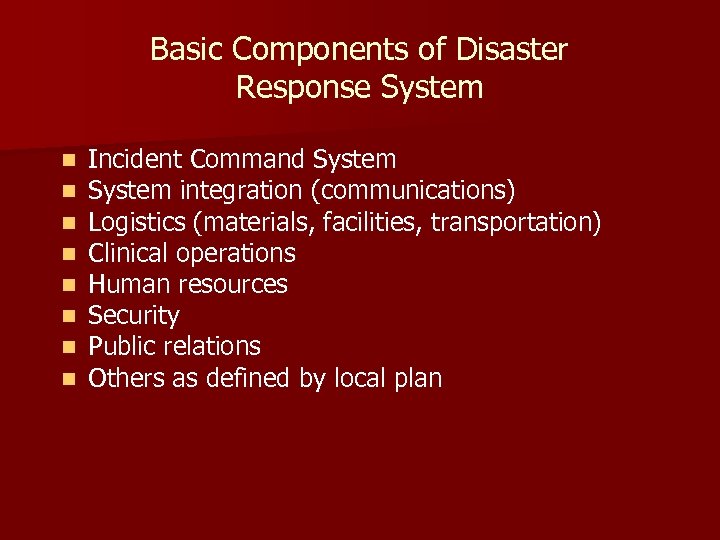
Basic Components of Disaster Response System n n n n Incident Command System integration (communications) Logistics (materials, facilities, transportation) Clinical operations Human resources Security Public relations Others as defined by local plan
Training Techniques Results of AHRQ-sponsored EPC report n “Traditional” educational techniques – Lectures, discussions, AV aids, written material n Standardized (smart) patients – – n Accepted by physicians Effective for one-on-one training Usefulness for training of large numbers? Cost prohibitive? Teleconferencing or satellite broadcasting – Simultaneously reaches large numbers – Seems as effective as traditional techniques
Training Techniques n “Tabletop” exercises – “Theoretical” drill with limited/no physical operations – Usually focuses on ICS, system integration – Successfully applied to physician training for bioterrorism preparedness – Best as part of comprehensive training plan? n Computer simulations – May replace expensive drills, allow identification of weaknesses in disaster plan and implementation – Very limited data available
Training Techniques n Disaster Drills – – – “Cornerstone” of disaster preparedness efforts Significant collective experience High variability in methods used Limited data concerning objective evaluation Shown to improve knowledge of disaster plan Successful in identifying problems in plan execution
Drill Evaluation: Define Goals & Boundaries n Define specific goals for the drill – Don’t be ambitious beyond resources!! § Clinical response training? § ICS effectiveness evaluation? § Chem, Bio, Rads included? n Define borders of drill activities n Resources available – – Interface with outside agencies? ED only, entire hospital, selected departments? Moulaged patients, “smart” victims, no victims? Security, pharmacy, radiology also involved? – – – Adequate time before drill? Buy-in by key stakeholders? Separate evaluation team?
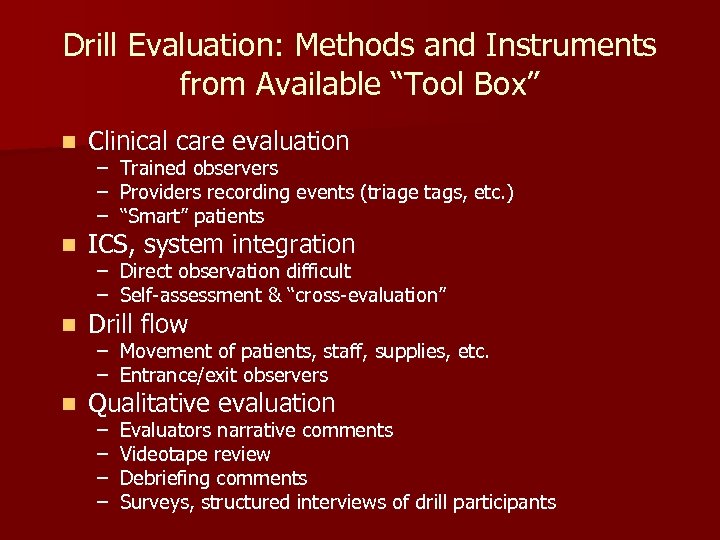
Drill Evaluation: Methods and Instruments from Available “Tool Box” n Clinical care evaluation n ICS, system integration n Drill flow n Qualitative evaluation – – – Trained observers Providers recording events (triage tags, etc. ) “Smart” patients – Direct observation difficult – Self-assessment & “cross-evaluation” – Movement of patients, staff, supplies, etc. – Entrance/exit observers – – Evaluators narrative comments Videotape review Debriefing comments Surveys, structured interviews of drill participants
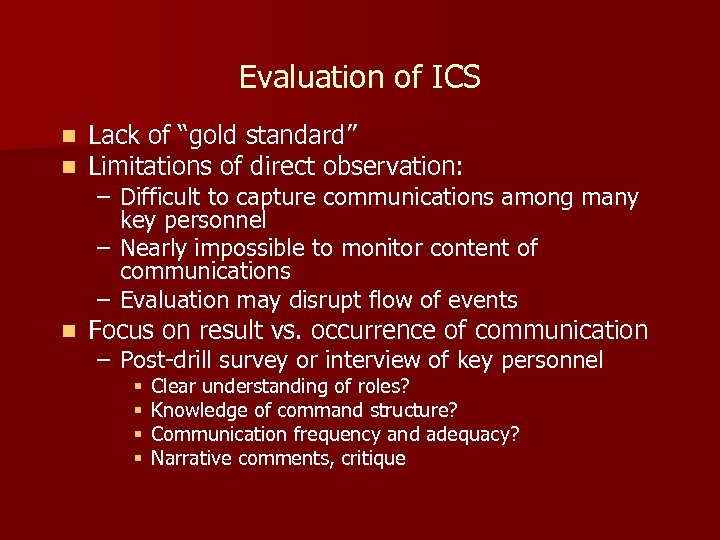
Evaluation of ICS n n Lack of “gold standard” Limitations of direct observation: n Focus on result vs. occurrence of communication – Difficult to capture communications among many key personnel – Nearly impossible to monitor content of communications – Evaluation may disrupt flow of events – Post-drill survey or interview of key personnel § § Clear understanding of roles? Knowledge of command structure? Communication frequency and adequacy? Narrative comments, critique
1c45e2483611d994df751d0936a5a82c.ppt