Differetial diagnosis and treatment of EH Essential Hypertension









differetial_diagnosis_and_treatment_of_eh.ppt
- Размер: 514.5 Кб
- Количество слайдов: 50
Описание презентации Differetial diagnosis and treatment of EH Essential Hypertension по слайдам
 Differetial diagnosis and treatment of EH Essential Hypertension is the disease in which high arterial pressure is not associated with any primary organic lesion of organs or systems. . The World Health Organization’s criterion for the definition of hypertension is arterial hypertension more than 140/90 mm Hg.
Differetial diagnosis and treatment of EH Essential Hypertension is the disease in which high arterial pressure is not associated with any primary organic lesion of organs or systems. . The World Health Organization’s criterion for the definition of hypertension is arterial hypertension more than 140/90 mm Hg.
 EH has a multifactorial aetiologi The factors promoting the onset of EH are following: hereditory and constitutional factors, nervous and phychic trauma (acute or chronic), emotional stress, age, sex, race, nutritive factors (salt-rich diet, magnesium deficit), obesity. ВВ P is associated with overrall body mass and with central obesity. insulin resistance. Recently a syndrome has been described of hyperinsulinemia, glucose intolerance, reduced levels of HDL cholesterol, hypertriglyceride-mia and central obesity
EH has a multifactorial aetiologi The factors promoting the onset of EH are following: hereditory and constitutional factors, nervous and phychic trauma (acute or chronic), emotional stress, age, sex, race, nutritive factors (salt-rich diet, magnesium deficit), obesity. ВВ P is associated with overrall body mass and with central obesity. insulin resistance. Recently a syndrome has been described of hyperinsulinemia, glucose intolerance, reduced levels of HDL cholesterol, hypertriglyceride-mia and central obesity
 Assessment of patients During the first stage of diagnostic examination it is necessary: to establish the fact of high arterial pressure, to suggest primary or secondary hypertension. The management of patients should be considered in some stages : assessment, non-pharmacological treatment, drug treatment.
Assessment of patients During the first stage of diagnostic examination it is necessary: to establish the fact of high arterial pressure, to suggest primary or secondary hypertension. The management of patients should be considered in some stages : assessment, non-pharmacological treatment, drug treatment.
 Assessment period During the assessment period, secondary causes of hypertension should be excluded, the target-organ effect of the blood pressure should be evaluated, and any concomitant conditions (dyslipidemia or diabetes) should be identified.
Assessment period During the assessment period, secondary causes of hypertension should be excluded, the target-organ effect of the blood pressure should be evaluated, and any concomitant conditions (dyslipidemia or diabetes) should be identified.
 Symptomatic arterial hypertension is secondary to diseases or lesions of the organs (or systems) involved in regulation of arterial pressure. The incidence of symptomatic hypertension is 10 -12 per cent of all patients hospitalized for elevated arterial pressure. .
Symptomatic arterial hypertension is secondary to diseases or lesions of the organs (or systems) involved in regulation of arterial pressure. The incidence of symptomatic hypertension is 10 -12 per cent of all patients hospitalized for elevated arterial pressure. .
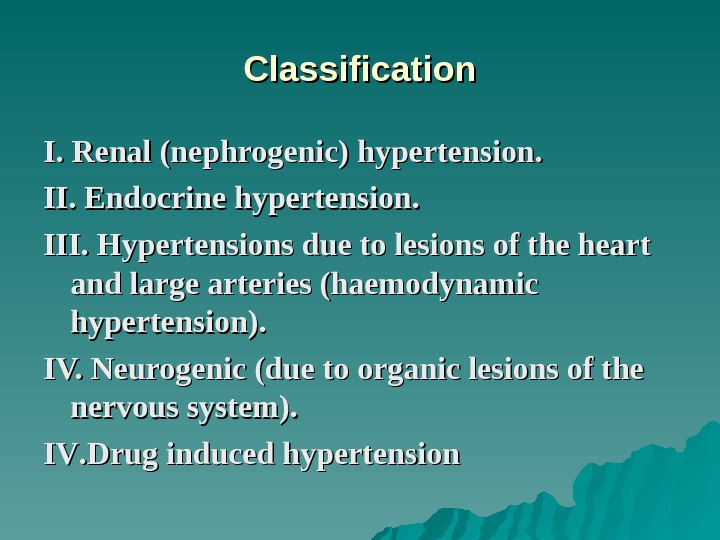
 Classification I. Renal (nephrogenic) hypertension. II. Endocrine hypertension. III. Hypertensions due to lesions of the heart and large arteries (haemodynamic hypertension). IV. Neurogenic (due to organic lesions of the nervous system). IVIV. . Drug induced hypertension
Classification I. Renal (nephrogenic) hypertension. II. Endocrine hypertension. III. Hypertensions due to lesions of the heart and large arteries (haemodynamic hypertension). IV. Neurogenic (due to organic lesions of the nervous system). IVIV. . Drug induced hypertension
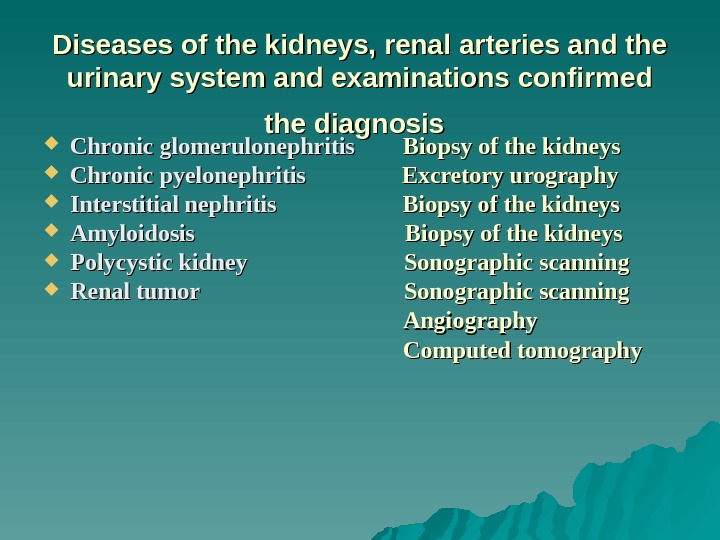
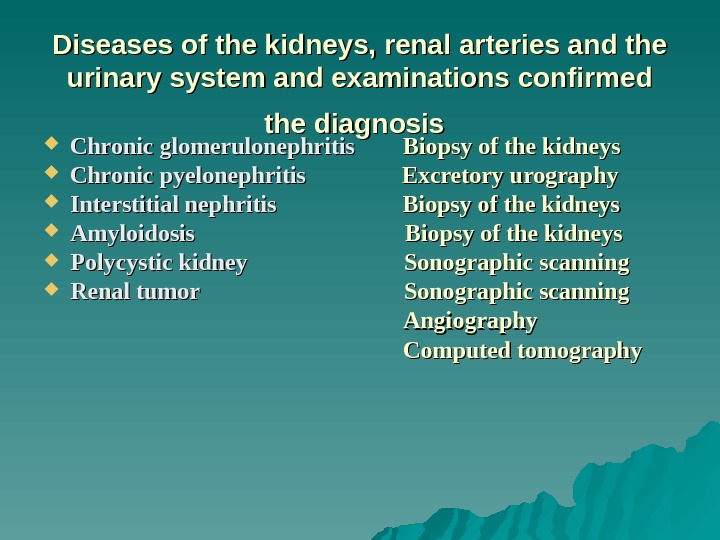 Diseases of the kidneys, renal arteries and the urinary system and examinations confirmed the diagnosis Chronic glomerulonephritis Biopsy of the kidneys Chronic pyelonephritis Excretory urography Interstitial nephritis Biopsy of the kidneys Amyloidosis Biopsy of the kidneys Polycystic kidney Sonographic scanning Renal tumor Sonographic scanning Angiography Computed tomography
Diseases of the kidneys, renal arteries and the urinary system and examinations confirmed the diagnosis Chronic glomerulonephritis Biopsy of the kidneys Chronic pyelonephritis Excretory urography Interstitial nephritis Biopsy of the kidneys Amyloidosis Biopsy of the kidneys Polycystic kidney Sonographic scanning Renal tumor Sonographic scanning Angiography Computed tomography
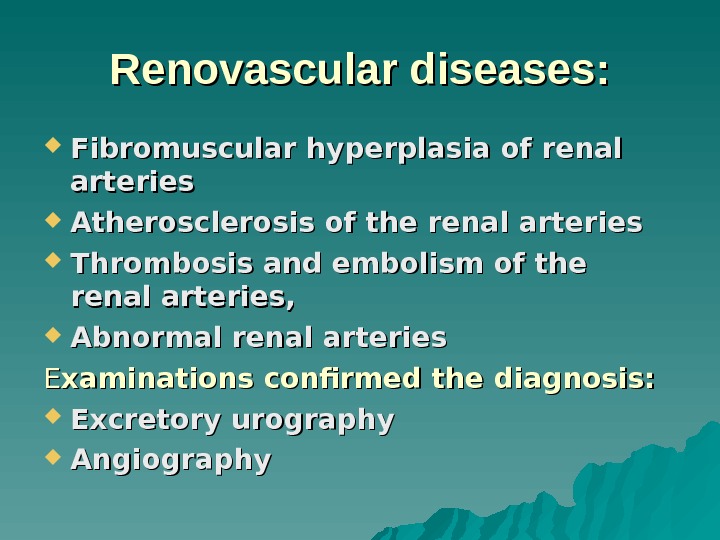 Renovascular diseases: Fibromuscular hyperplasia of renal arteries Atherosclerosis of the renal arteries Thrombosis and embolism of the renal arteries, Abnormal renal arteries EE xaminations confirmed the diagnosis: Excretory urography Angiography
Renovascular diseases: Fibromuscular hyperplasia of renal arteries Atherosclerosis of the renal arteries Thrombosis and embolism of the renal arteries, Abnormal renal arteries EE xaminations confirmed the diagnosis: Excretory urography Angiography
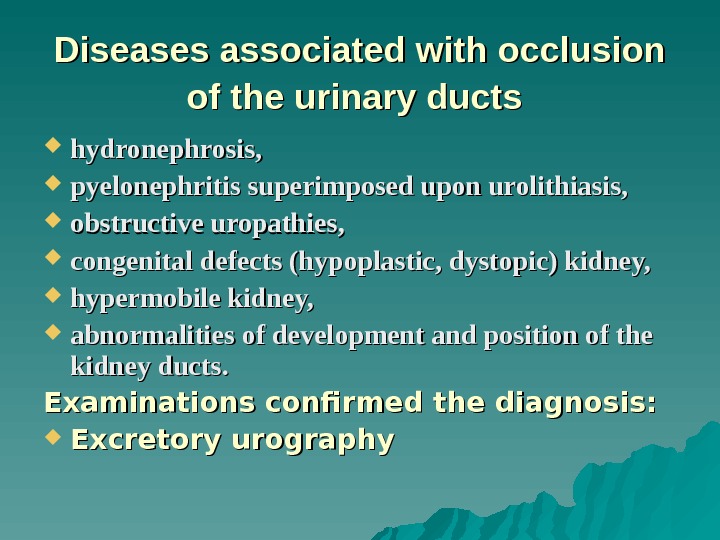 Diseases associated with occlusion of the urinary ducts hydronephrosis, pyelonephritis superimposed upon urolithiasis, obstructive uropathies, congenital defects (hypoplastic, dystopic) kidney, hypermobile kidney, abnormalities of development and position of the kidney ducts. Examinations confirmed the diagnosis: Excretory urography
Diseases associated with occlusion of the urinary ducts hydronephrosis, pyelonephritis superimposed upon urolithiasis, obstructive uropathies, congenital defects (hypoplastic, dystopic) kidney, hypermobile kidney, abnormalities of development and position of the kidney ducts. Examinations confirmed the diagnosis: Excretory urography
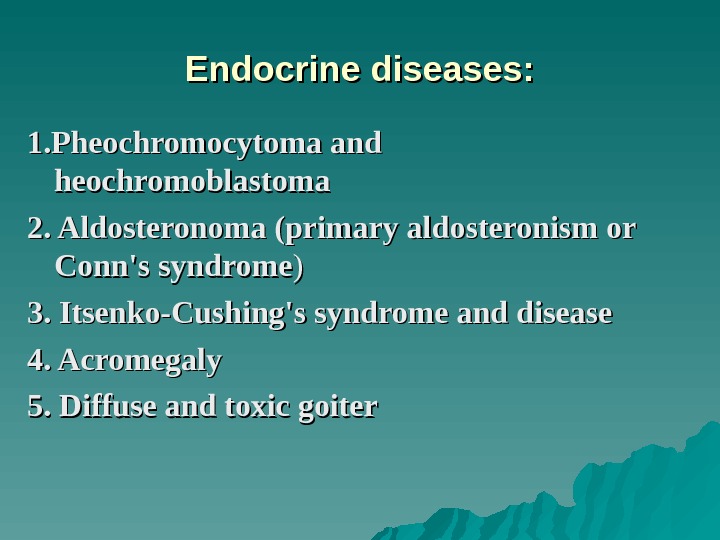 Endocrine diseases: 1. Pheochromocytoma and heochromoblastoma 2. Aldosteronoma (primary aldosteronism or Conn’s syndrome )) 3. Itsenko-Cushing’s syndrome and disease 4. Acromegaly 5. Diffuse and toxic goiter
Endocrine diseases: 1. Pheochromocytoma and heochromoblastoma 2. Aldosteronoma (primary aldosteronism or Conn’s syndrome )) 3. Itsenko-Cushing’s syndrome and disease 4. Acromegaly 5. Diffuse and toxic goiter
 Examinations confirmed the diagnosis: 1. Determining daily excretion of catecholamines with the urine during attac and in blood; Computed tomography (to reveal tumors) 2. 2. Determining aldosterone and renin in the blood. Computed tomography (to reveal tumors) 3. Determining 17 -hydroxycorticosteroids in daily urine and daily secretion into the blood. Computed tomography (to reveal pituitary adenoma) 4. 4. Computed tomography 5. 5. Determining of the hyperfunction of the gland
Examinations confirmed the diagnosis: 1. Determining daily excretion of catecholamines with the urine during attac and in blood; Computed tomography (to reveal tumors) 2. 2. Determining aldosterone and renin in the blood. Computed tomography (to reveal tumors) 3. Determining 17 -hydroxycorticosteroids in daily urine and daily secretion into the blood. Computed tomography (to reveal pituitary adenoma) 4. 4. Computed tomography 5. 5. Determining of the hyperfunction of the gland
 Diseases of the heart, aorta and large vessels Acquired heart diseases (aortic insufficiency), Congenital heart defects (patent arterial duct); Diseases of the heart attended by congestive failure Complete atrioventricular block; Congenital defects of the aorta (coarctation) Acquired diseases (arteritis of the aorta and its branches, atherosclerosis); Stenosed carotid and vertebral arteries. Examinations confirmed the diagnosis: Angiography, Sonographic scanning Computed tomography
Diseases of the heart, aorta and large vessels Acquired heart diseases (aortic insufficiency), Congenital heart defects (patent arterial duct); Diseases of the heart attended by congestive failure Complete atrioventricular block; Congenital defects of the aorta (coarctation) Acquired diseases (arteritis of the aorta and its branches, atherosclerosis); Stenosed carotid and vertebral arteries. Examinations confirmed the diagnosis: Angiography, Sonographic scanning Computed tomography
 Diseases of the central nervous system: Tumour of the brain Encephalitis Trauma Focal ischaemic lesions Examinations confirmed the diagnosis: Neurological examination Sonographic scanning Computed tomography
Diseases of the central nervous system: Tumour of the brain Encephalitis Trauma Focal ischaemic lesions Examinations confirmed the diagnosis: Neurological examination Sonographic scanning Computed tomography
 Clinical picture. The symptomatic character of AH is suggested by the following: development of AH in young patients and in persons aged over 50 -55; acute onset and rapid stabilization of BP at high values; asymptomatic course of AH; resistance to hypertensive therapy; malignant course of AH. The variability of the clinical picture is explained by the different symptoms and by the great number of diseases that are attended by AH.
Clinical picture. The symptomatic character of AH is suggested by the following: development of AH in young patients and in persons aged over 50 -55; acute onset and rapid stabilization of BP at high values; asymptomatic course of AH; resistance to hypertensive therapy; malignant course of AH. The variability of the clinical picture is explained by the different symptoms and by the great number of diseases that are attended by AH.
 Diagnostic examination The object of first stage of diagnostic examination is: (1) to collect information concerning uropathy or renal pathology in the previous history; (2) purposeful search for symptoms characteristic of pathology in which AH can be a symptom. In the second stage of diagnostic examination, it is necessary to reveal the symptoms that are due to elevated BP and the underlying disease. The third stage of diagnostic examination includes: (a) obligatory examination for all patients, (b) special examination for indications.
Diagnostic examination The object of first stage of diagnostic examination is: (1) to collect information concerning uropathy or renal pathology in the previous history; (2) purposeful search for symptoms characteristic of pathology in which AH can be a symptom. In the second stage of diagnostic examination, it is necessary to reveal the symptoms that are due to elevated BP and the underlying disease. The third stage of diagnostic examination includes: (a) obligatory examination for all patients, (b) special examination for indications.
 Obligatory examinations 1. Electrocardiography 2. Chest X-ray 3. Studies of the optic fundus 4. Excretory urography 5. Blood analysis: total blood counts, determining urea, creatinine, cholesterol, triglycerides, sugar, protein and its fractions 66. Studies of the urine: clinical analysis, determination of the formed blood elements (Nechiporenko`s test), test for daily variation of specific gravity of urine (Zimnitsky`s test), determination of daily proteinuria, bacteriuria, qualitative studies on leucocytes.
Obligatory examinations 1. Electrocardiography 2. Chest X-ray 3. Studies of the optic fundus 4. Excretory urography 5. Blood analysis: total blood counts, determining urea, creatinine, cholesterol, triglycerides, sugar, protein and its fractions 66. Studies of the urine: clinical analysis, determination of the formed blood elements (Nechiporenko`s test), test for daily variation of specific gravity of urine (Zimnitsky`s test), determination of daily proteinuria, bacteriuria, qualitative studies on leucocytes.
 Examinations for special indications 1. Quantitative estimation of bacteriuria, daily protein excreted with urine, 2. Total testing of the renal function, 3. Testing the function of each separate kidney (radionuclide renography and scanning, infusion and retrograde pyelography, chromocytoscopy), 4. Sonographic scanning of the kidneys, 5. Computed tomography of the kidneys, 6. Contrast angiography (aortography with estimation of the renal blood flow and cavography with phlebography of the renal veins), 7. Testing blood for the renin and angiotensin content.
Examinations for special indications 1. Quantitative estimation of bacteriuria, daily protein excreted with urine, 2. Total testing of the renal function, 3. Testing the function of each separate kidney (radionuclide renography and scanning, infusion and retrograde pyelography, chromocytoscopy), 4. Sonographic scanning of the kidneys, 5. Computed tomography of the kidneys, 6. Contrast angiography (aortography with estimation of the renal blood flow and cavography with phlebography of the renal veins), 7. Testing blood for the renin and angiotensin content.
 Treatment General measures Weight reduction Reduction of heavy alcohol intake and smoking. Salt restriction Regular exercise. .
Treatment General measures Weight reduction Reduction of heavy alcohol intake and smoking. Salt restriction Regular exercise. .
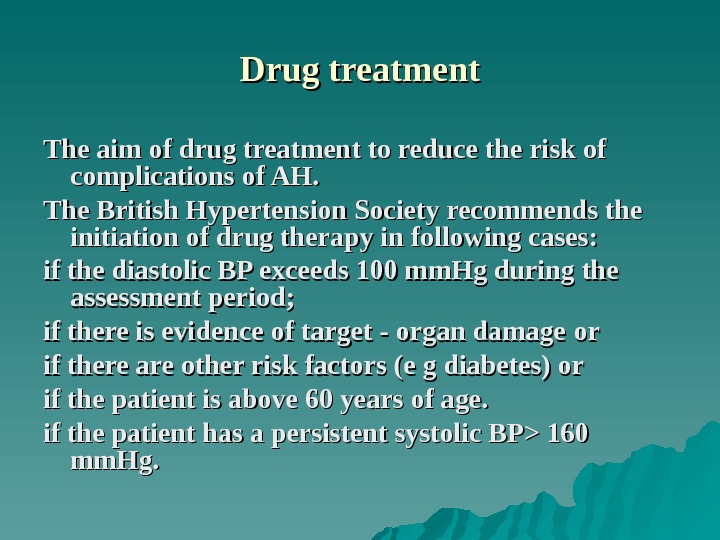
 Drug treatment The aim of drug treatment to reduce the risk of complications of AH. The British Hypertension Society recommends the initiation of drug therap уу in following cases: if the diastolic BP exceeds 100 mm. Hg during the assessment period; if there is evidence of target — organ damage оо rr if there are other risk factors (e g diabetes) or if the patient is above 60 years of age. if the patient has a persistent systolic BP> 160 mm. Hg.
Drug treatment The aim of drug treatment to reduce the risk of complications of AH. The British Hypertension Society recommends the initiation of drug therap уу in following cases: if the diastolic BP exceeds 100 mm. Hg during the assessment period; if there is evidence of target — organ damage оо rr if there are other risk factors (e g diabetes) or if the patient is above 60 years of age. if the patient has a persistent systolic BP> 160 mm. Hg.
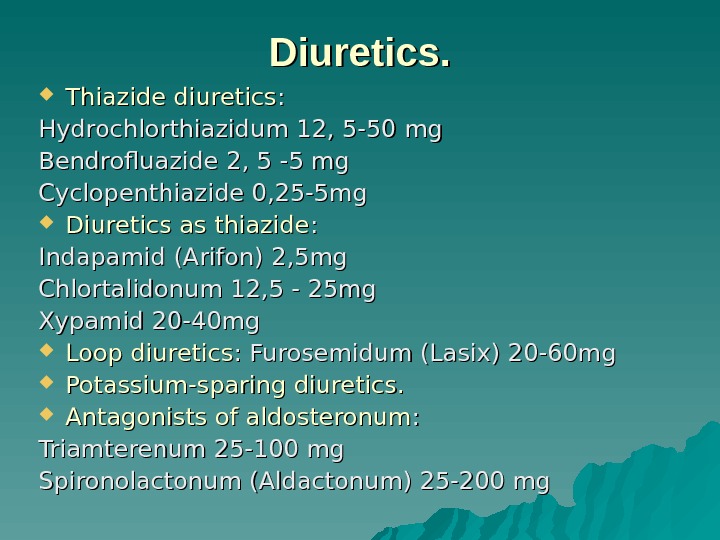
 Diuretics. Thiazide diuretics : : Hydrochlorthiazidum 12, 5 -50 mgmg Bendrofluazide 2, 5 -5 mg Cyclopenthiazide 0, 25 -5 mg Diuretics as thiazide : : Indapamid (Arifon) 2, 5 mg Chlortalidonum 12, 5 — 25 mg Xypamid 20 -40 mg Loop diuretics : Furosemidum (Lasix) 20 -60 mg Potassium-sparing diuretics. Antagonists of aldosteronum : : Triamterenum 25 -100 mg Spironolactonum (Aldactonum) 25 -200 mg
Diuretics. Thiazide diuretics : : Hydrochlorthiazidum 12, 5 -50 mgmg Bendrofluazide 2, 5 -5 mg Cyclopenthiazide 0, 25 -5 mg Diuretics as thiazide : : Indapamid (Arifon) 2, 5 mg Chlortalidonum 12, 5 — 25 mg Xypamid 20 -40 mg Loop diuretics : Furosemidum (Lasix) 20 -60 mg Potassium-sparing diuretics. Antagonists of aldosteronum : : Triamterenum 25 -100 mg Spironolactonum (Aldactonum) 25 -200 mg
 The mechanism of action of diuretics: Decrease of volume of a circulating and extracellular liquid Decrease of cardiac output during long application Direct dilatation
The mechanism of action of diuretics: Decrease of volume of a circulating and extracellular liquid Decrease of cardiac output during long application Direct dilatation
 Indications to using diuretics Heart failure AH in advanced age Systolic AH Possible indications to using diuretics: Diabetes Osteoporosis Contraindications: gout
Indications to using diuretics Heart failure AH in advanced age Systolic AH Possible indications to using diuretics: Diabetes Osteoporosis Contraindications: gout
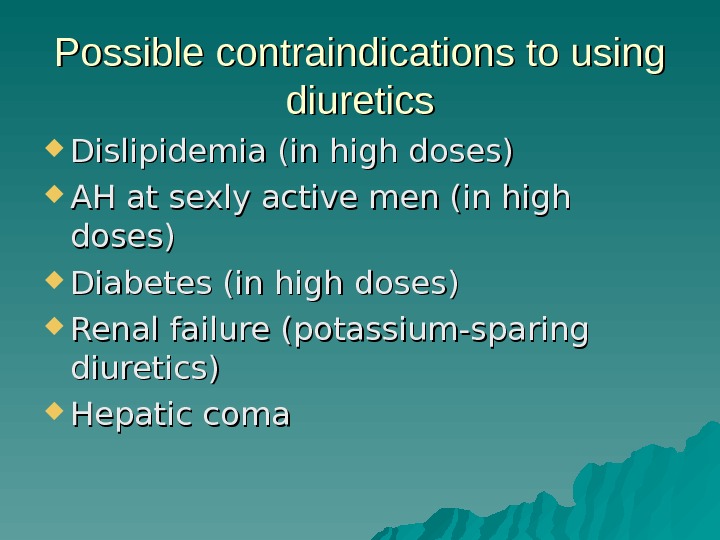
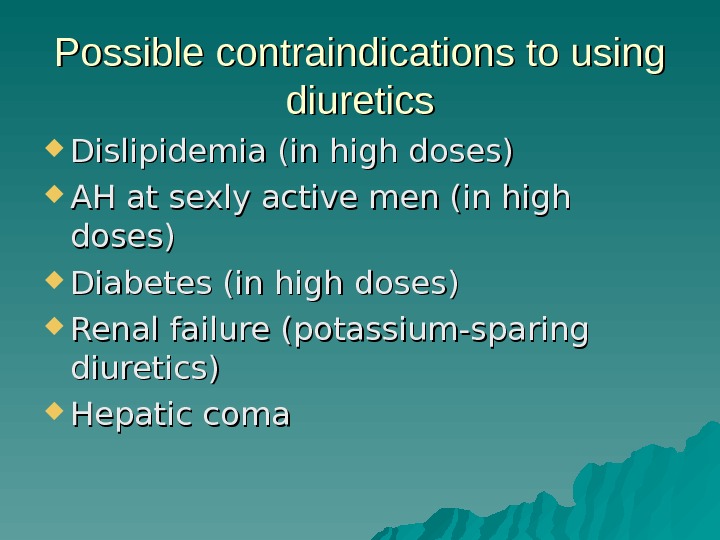 Possible contraindications to using diuretics Dislipidemia (in high doses) AH at sexly active men (in high doses) Diabetes (in high doses) Renal failure (potassium-sparing diuretics) Hepatic coma
Possible contraindications to using diuretics Dislipidemia (in high doses) AH at sexly active men (in high doses) Diabetes (in high doses) Renal failure (potassium-sparing diuretics) Hepatic coma
 Side effects of diuretics: Hypokalemia, Hypomagnesiemia, Hyponatremia, Hypocholiemia, Hyperuricemia, Hyperglycemia, Nitrogenemia, Hypercalcemia, Impotency, Orthostatic hypotension, Metabolic alkalosis, The secondary hyperreninemia and hyperaldosteronism, Dermatitis, pancreatitis, vasculitis
Side effects of diuretics: Hypokalemia, Hypomagnesiemia, Hyponatremia, Hypocholiemia, Hyperuricemia, Hyperglycemia, Nitrogenemia, Hypercalcemia, Impotency, Orthostatic hypotension, Metabolic alkalosis, The secondary hyperreninemia and hyperaldosteronism, Dermatitis, pancreatitis, vasculitis
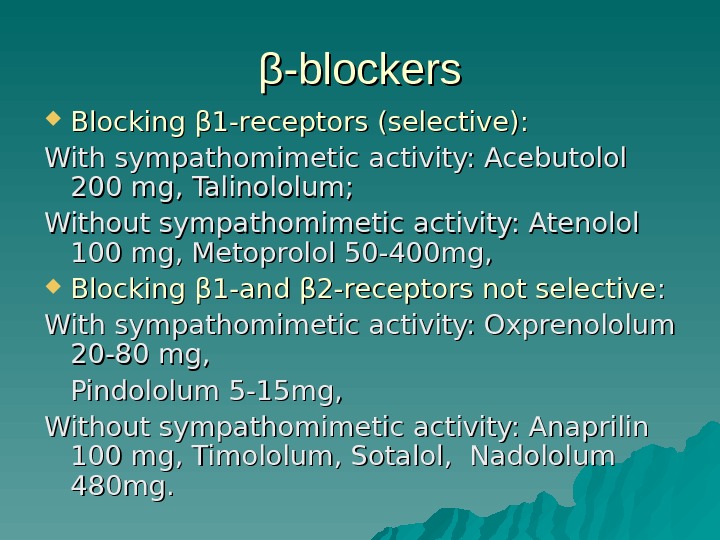
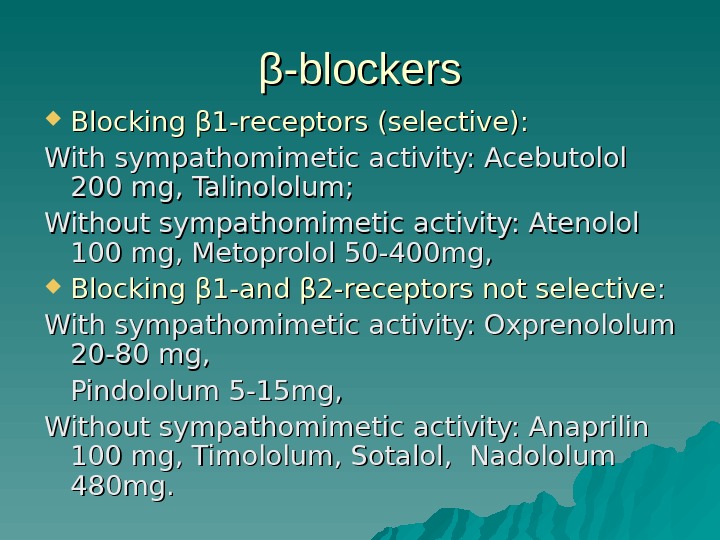 ββ -blockers Blocking β 1 -receptors (selective): With sympathomimetic activity: Acebutolol 200 mg, Talinololum; Without sympathomimetic activity: Atenolol 100 mg, Metoprolol 50 -400 mg, Blocking β 11 -and β 2 -receptors not selective : : With sympathomimetic activity: Oxprenololum 20 -80 mg, Pindololum 5 -15 mg, Without sympathomimetic activity: Anaprilin 100 mg, Timololum, Sotalol, Nadololum 480 mg.
ββ -blockers Blocking β 1 -receptors (selective): With sympathomimetic activity: Acebutolol 200 mg, Talinololum; Without sympathomimetic activity: Atenolol 100 mg, Metoprolol 50 -400 mg, Blocking β 11 -and β 2 -receptors not selective : : With sympathomimetic activity: Oxprenololum 20 -80 mg, Pindololum 5 -15 mg, Without sympathomimetic activity: Anaprilin 100 mg, Timololum, Sotalol, Nadololum 480 mg.
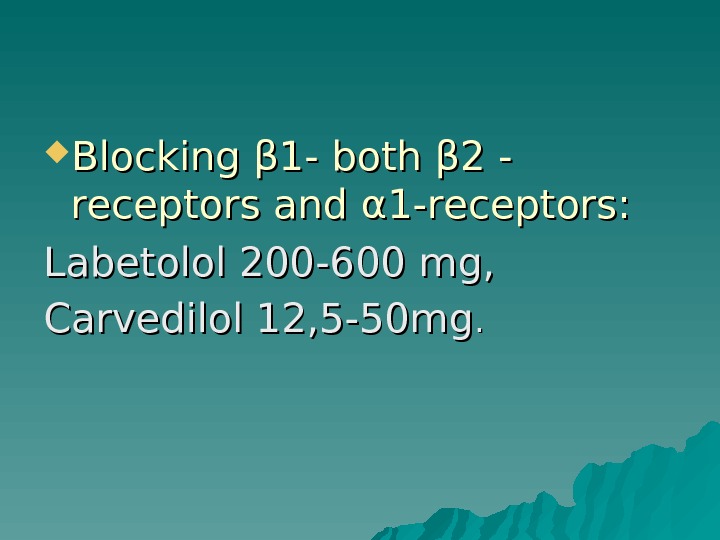 Blocking β 1 — both β 2 — receptors and α 1 -receptors: Labetolol 200 -600 mg, Carvedilol 12, 5 -50 mg. .
Blocking β 1 — both β 2 — receptors and α 1 -receptors: Labetolol 200 -600 mg, Carvedilol 12, 5 -50 mg. .
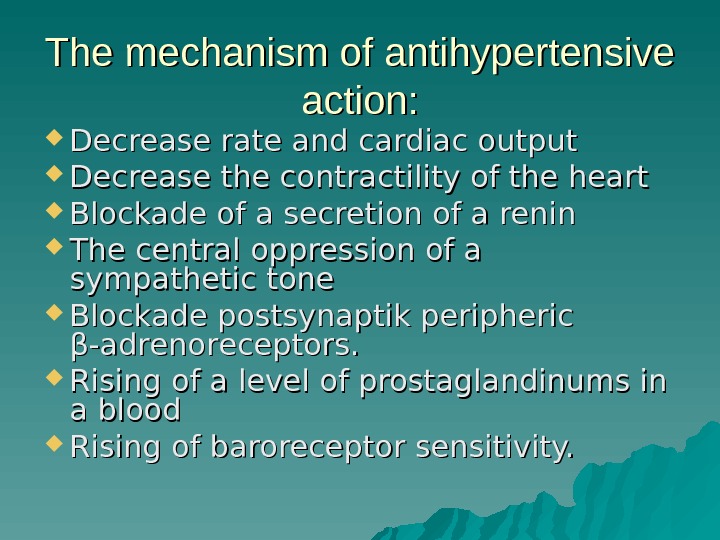 The mechanism of antihypertensive action: Decrease rate and cardiac output Decrease the contractility of the heart Blockade of a secretion of a renin The central oppression of a sympathetic tone Blockade postsynaptik peripheric β-adrenoreceptors. Rising of a level of prostaglandinums in a blood Rising of baroreceptor sensitivity.
The mechanism of antihypertensive action: Decrease rate and cardiac output Decrease the contractility of the heart Blockade of a secretion of a renin The central oppression of a sympathetic tone Blockade postsynaptik peripheric β-adrenoreceptors. Rising of a level of prostaglandinums in a blood Rising of baroreceptor sensitivity.
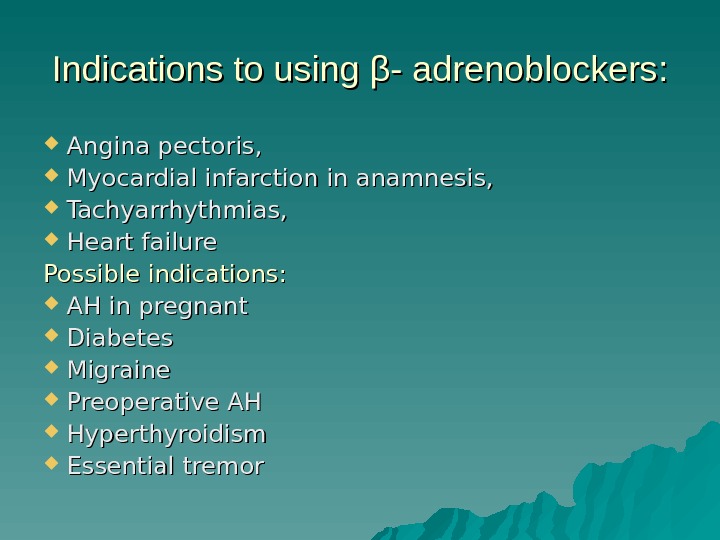 Indications to using β- adrenoblockers: Angina pectoris, Myocardial infarction in anamnesis, Tachyarrhythmias, Heart failure Possible indications: AH in pregnant Diabetes Migraine Preoperative AH Hyperthyroidism Essential tremor
Indications to using β- adrenoblockers: Angina pectoris, Myocardial infarction in anamnesis, Tachyarrhythmias, Heart failure Possible indications: AH in pregnant Diabetes Migraine Preoperative AH Hyperthyroidism Essential tremor
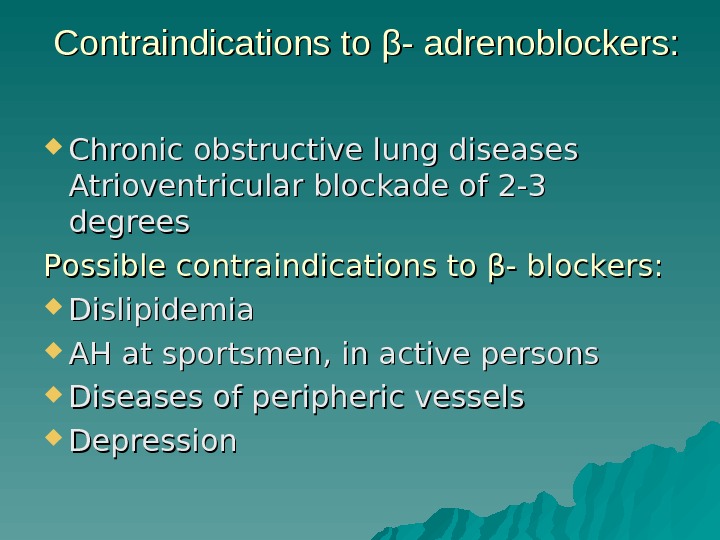 Contraindications to β- adrenoblockers: Chronic obstructive lung diseases Atrioventricular blockade of 2 -3 degrees Possible contraindications to β- blockers: Dislipidemia AH at sportsmen, in active persons Diseases of peripheric vessels Depression
Contraindications to β- adrenoblockers: Chronic obstructive lung diseases Atrioventricular blockade of 2 -3 degrees Possible contraindications to β- blockers: Dislipidemia AH at sportsmen, in active persons Diseases of peripheric vessels Depression
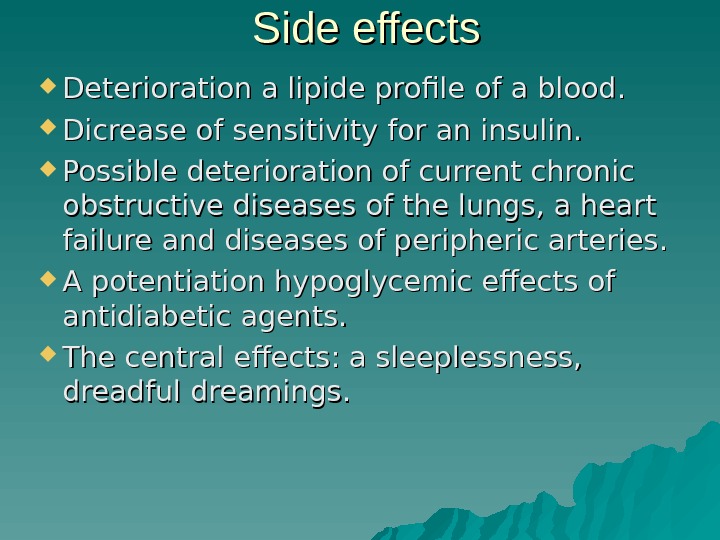
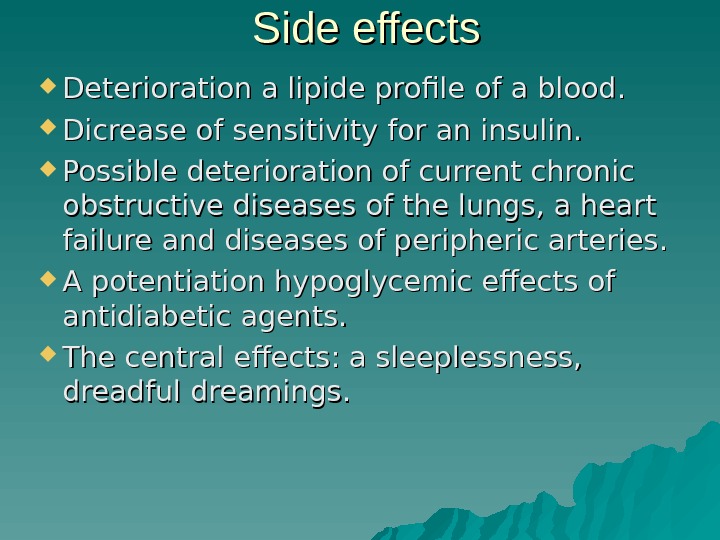 Side effects Deterioration a lipide profile of a blood. Dicrease of sensitivity for an insulin. Possible deterioration of current chronic obstructive diseases of the lungs, a heart failure and diseases of peripheric arteries. A potentiation hypoglycemic effects of antidiabetic agents. The central effects: a sleeplessness, dreadful dreamings.
Side effects Deterioration a lipide profile of a blood. Dicrease of sensitivity for an insulin. Possible deterioration of current chronic obstructive diseases of the lungs, a heart failure and diseases of peripheric arteries. A potentiation hypoglycemic effects of antidiabetic agents. The central effects: a sleeplessness, dreadful dreamings.
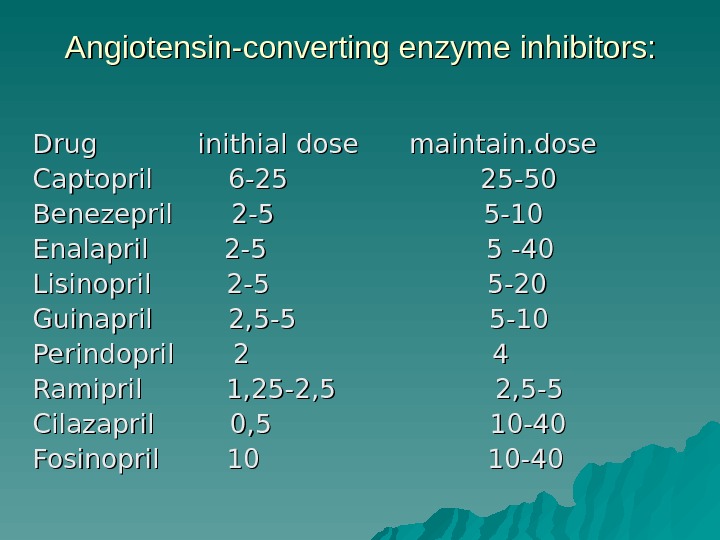
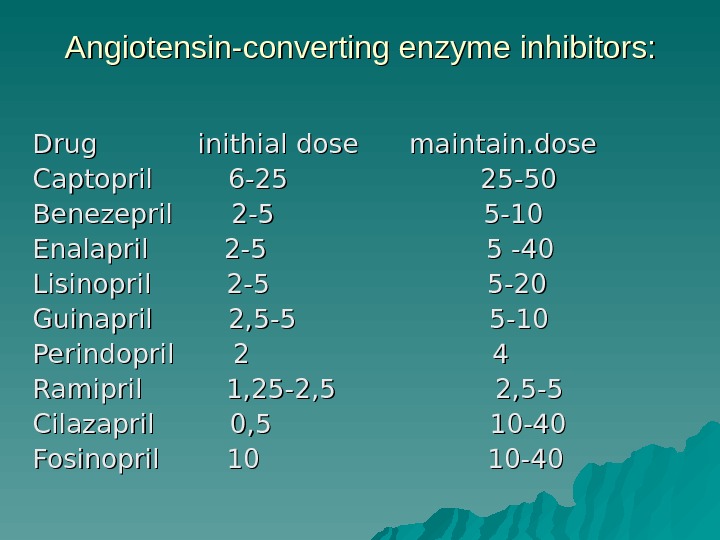 Angiotensin-converting enzyme inhibitors: Drug inithial dose maintain. dose Captopril 6 -25 25 -50 Benezepril 2 -5 5 -10 Enalapril 2 -5 55 -40 -40 Lisinopril 2 -5 5 -20 Guinapril 2, 5 -5 5 -10 Perindopril 2 4 Ramipril 1, 25 -2, 5 2, 5 -5 Cilazapril 0, 5 10 -40 Fosinopril 10 10 —
Angiotensin-converting enzyme inhibitors: Drug inithial dose maintain. dose Captopril 6 -25 25 -50 Benezepril 2 -5 5 -10 Enalapril 2 -5 55 -40 -40 Lisinopril 2 -5 5 -20 Guinapril 2, 5 -5 5 -10 Perindopril 2 4 Ramipril 1, 25 -2, 5 2, 5 -5 Cilazapril 0, 5 10 -40 Fosinopril 10 10 —
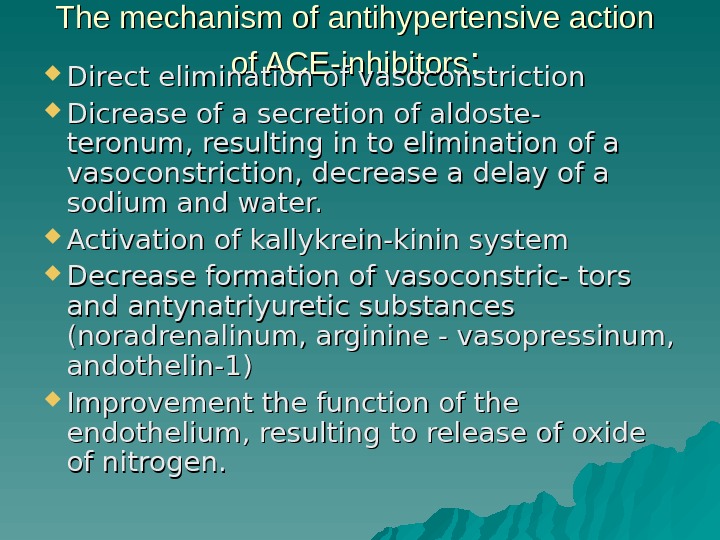
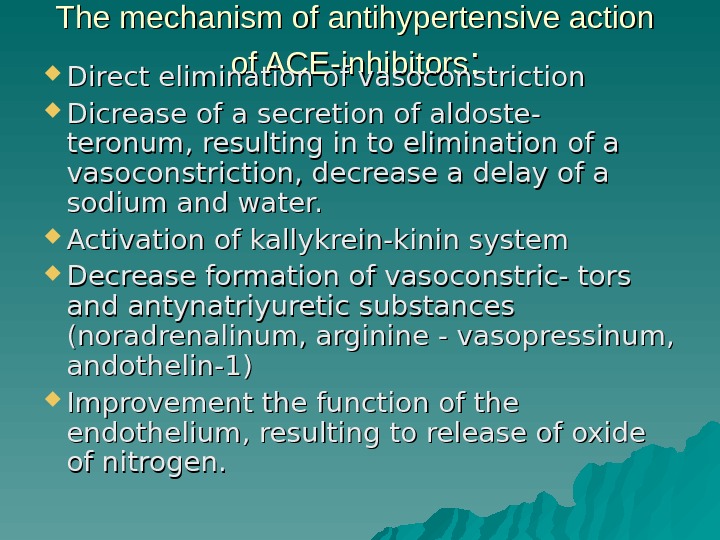 The mechanism of antihypertensive action of ACE-inhibitors : : Direct elimination of vasoconstriction Dicrease of a secretion of aldoste- teronum, resulting in to elimination of a vasoconstriction, decrease a delay of a sodium and water. Activation of kallykrein-kinin system Decrease formation of vasoconstric- tors and antynatriyuretic substances (noradrenalinum, arginine — vasopressinum, andothelin-1) Improvement the function of the endothelium, resulting to release of oxide of nitrogen.
The mechanism of antihypertensive action of ACE-inhibitors : : Direct elimination of vasoconstriction Dicrease of a secretion of aldoste- teronum, resulting in to elimination of a vasoconstriction, decrease a delay of a sodium and water. Activation of kallykrein-kinin system Decrease formation of vasoconstric- tors and antynatriyuretic substances (noradrenalinum, arginine — vasopressinum, andothelin-1) Improvement the function of the endothelium, resulting to release of oxide of nitrogen.
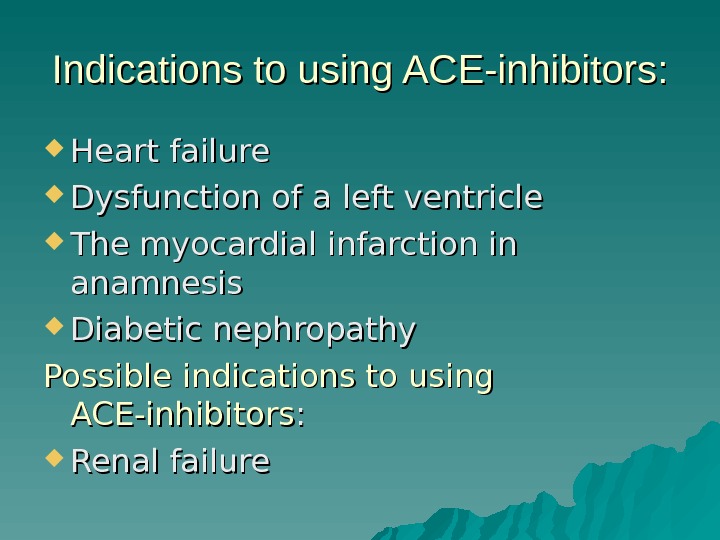
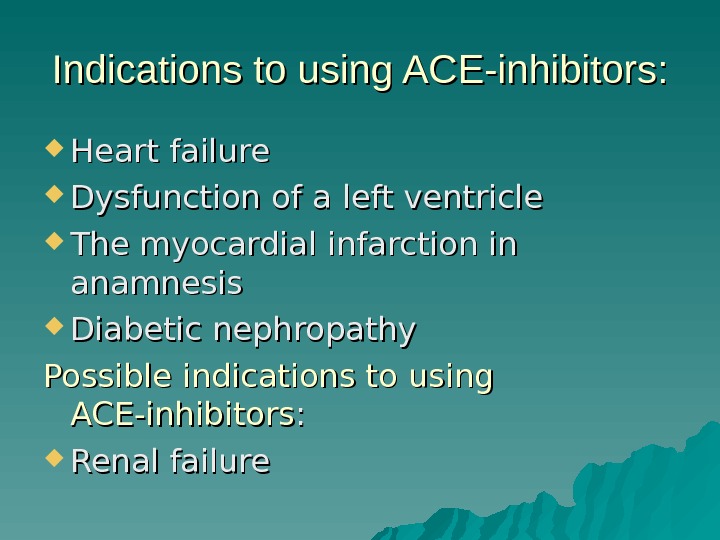 Indications to using ACE-inhibitors: Heart failure Dysfunction of a left ventricle The myocardial infarction in anamnesis Diabetic nephropathy Possible indications to using ACE-inhibitors : : Renal failure
Indications to using ACE-inhibitors: Heart failure Dysfunction of a left ventricle The myocardial infarction in anamnesis Diabetic nephropathy Possible indications to using ACE-inhibitors : : Renal failure
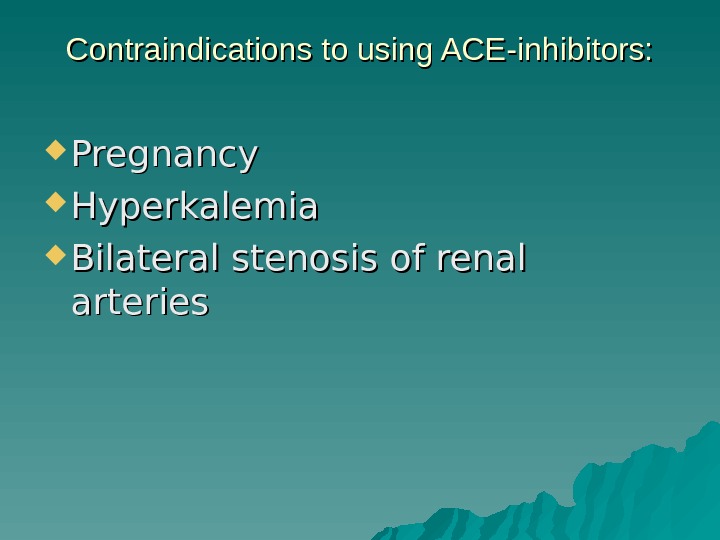 Contraindications to using ACE-inhibitors: Pregnancy Hyperkalemia Bilateral stenosis of renal arteries
Contraindications to using ACE-inhibitors: Pregnancy Hyperkalemia Bilateral stenosis of renal arteries
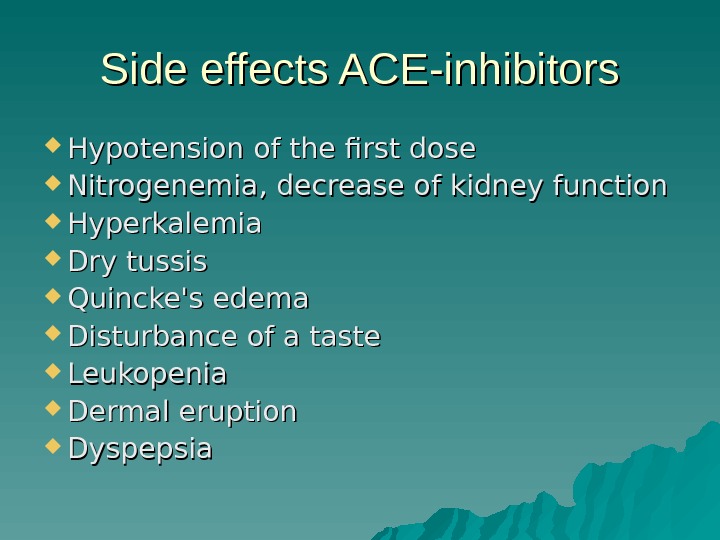 Side effects ACE-inhibitors Hypotension of the first dose Nitrogenemia, decrease of kidney function Hyperkalemia Dry tussis Quincke’s edema Disturbance of a taste Leukopenia Dermal eruption Dyspepsia
Side effects ACE-inhibitors Hypotension of the first dose Nitrogenemia, decrease of kidney function Hyperkalemia Dry tussis Quincke’s edema Disturbance of a taste Leukopenia Dermal eruption Dyspepsia
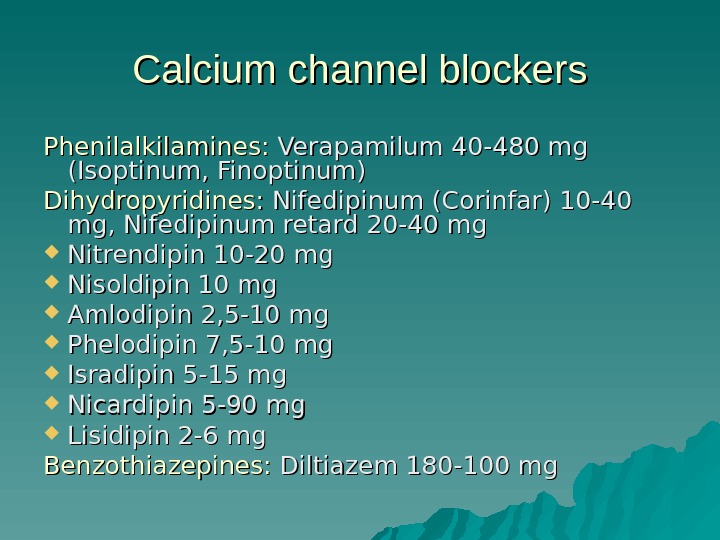 Calcium channel blockers Phenilalkilamines: Verapamilum 40 -480 mg (Isoptinum, Finoptinum) Dihydropyridines: Nifedipinum (Corinfar) 10 -40 mg, Nifedipinum retard 20 -40 mg Nitrendipin 10 -20 mg Nisoldipin 10 mg Amlodipin 2, 5 -10 mg Phelodipin 7, 5 -10 mg Isradipin 5 -15 mg Nicardipin 5 -90 mg Lisidipin 2 -6 mg Benzothiazepines: Diltiazem 180 -100 mg
Calcium channel blockers Phenilalkilamines: Verapamilum 40 -480 mg (Isoptinum, Finoptinum) Dihydropyridines: Nifedipinum (Corinfar) 10 -40 mg, Nifedipinum retard 20 -40 mg Nitrendipin 10 -20 mg Nisoldipin 10 mg Amlodipin 2, 5 -10 mg Phelodipin 7, 5 -10 mg Isradipin 5 -15 mg Nicardipin 5 -90 mg Lisidipin 2 -6 mg Benzothiazepines: Diltiazem 180 -100 mg
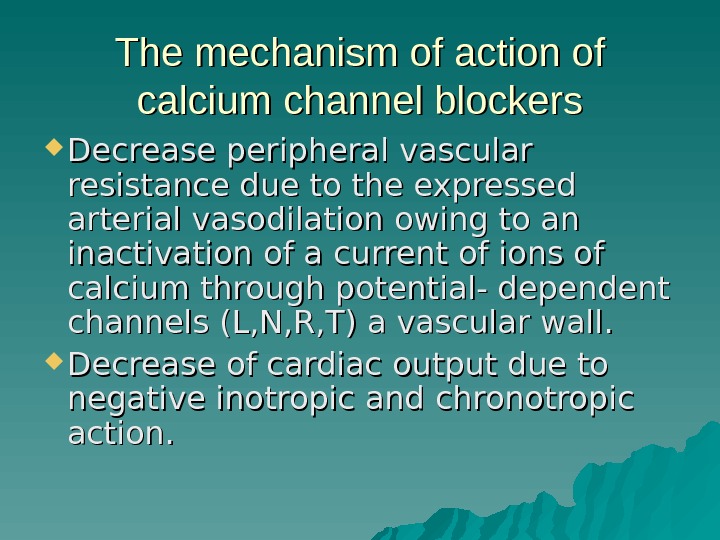 The mechanism of action of calcium channel blockers Decrease peripheral vascular resistance due to the expressed arterial vasodilation owing to an inactivation of a current of ions of calcium through potential- dependent channels (L, N, R, T) a vascular wall. Decrease of cardiac output due to negative inotropic and chronotropic action.
The mechanism of action of calcium channel blockers Decrease peripheral vascular resistance due to the expressed arterial vasodilation owing to an inactivation of a current of ions of calcium through potential- dependent channels (L, N, R, T) a vascular wall. Decrease of cardiac output due to negative inotropic and chronotropic action.
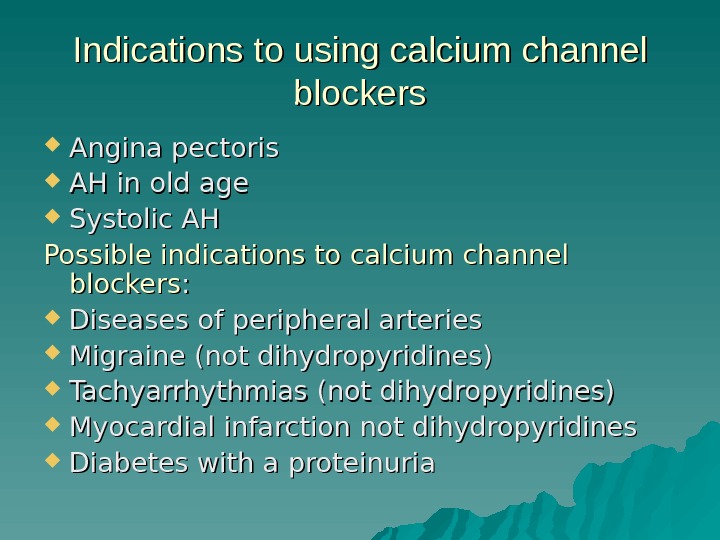 Indications to using calcium channel blockers Angina pectoris AH in old age Systolic AH Possible indications to calcium channel blockers : : Diseases of peripheral arteries Migraine (not dihydropyridines) Tachyarrhythmias (not dihydropyridines) Myocardial infarction not dihydropyridines Diabetes with a proteinuria
Indications to using calcium channel blockers Angina pectoris AH in old age Systolic AH Possible indications to calcium channel blockers : : Diseases of peripheral arteries Migraine (not dihydropyridines) Tachyarrhythmias (not dihydropyridines) Myocardial infarction not dihydropyridines Diabetes with a proteinuria
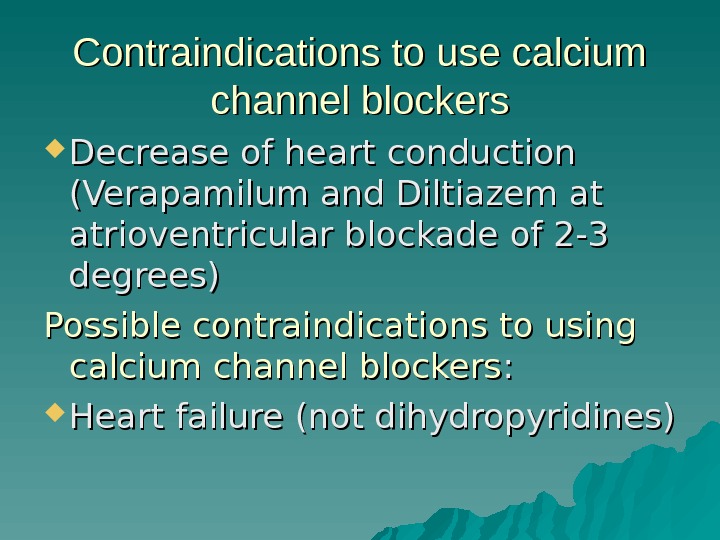 Contraindications to use calcium channel blockers Decrease of heart conduction (Verapamilum and Diltiazem at atrioventricular blockade of 2 -3 degrees) Possible contraindications to using calcium channel blockers : : Heart failure (not dihydropyridines)
Contraindications to use calcium channel blockers Decrease of heart conduction (Verapamilum and Diltiazem at atrioventricular blockade of 2 -3 degrees) Possible contraindications to using calcium channel blockers : : Heart failure (not dihydropyridines)
 Side effects of antagonists of calcium: The effects due to vasodilation (mainly dihydropyridines): peripheral eodema, a headache, giddiness, a hypotension. flushing of the face, palpitation, The effects due to negative chronotropic, inotropic-, and dromotropic effect (mainly Verapamil and Diltiazem): intensifying of a heart failure, dicrease of atrioventricular conduction. Action on alimentary tract: constipations, a diarrhea, a vomiting (Verapamil at old patients is more often)
Side effects of antagonists of calcium: The effects due to vasodilation (mainly dihydropyridines): peripheral eodema, a headache, giddiness, a hypotension. flushing of the face, palpitation, The effects due to negative chronotropic, inotropic-, and dromotropic effect (mainly Verapamil and Diltiazem): intensifying of a heart failure, dicrease of atrioventricular conduction. Action on alimentary tract: constipations, a diarrhea, a vomiting (Verapamil at old patients is more often)
 α — adrenoblockers 1. 1. Non selective α — adrenoblockers: Tropodiphenum (Tropaphenum) (has M — cholinolytic action), Phenoxybenzamine, Phentolaminum 5 -15 mg. 2. Selective α 1 -adrenoblockers: Doxazin 1 -16 mg Prazozinum 5 -20 mg, Terazozin 5 – 10 mg,
α — adrenoblockers 1. 1. Non selective α — adrenoblockers: Tropodiphenum (Tropaphenum) (has M — cholinolytic action), Phenoxybenzamine, Phentolaminum 5 -15 mg. 2. Selective α 1 -adrenoblockers: Doxazin 1 -16 mg Prazozinum 5 -20 mg, Terazozin 5 – 10 mg,
 Other drugs with α 1 -аdrenoblocker action: Dihydroergotoxin (an agonist DA — receptors), Droperidolum (neuroleptic), Carvedilol (α-, β-adrenoblocker), Cetanserin (a blocker of peripheral S 2 -serotonin receptors), Labetolol (α-, β — adrenoblocker ))
Other drugs with α 1 -аdrenoblocker action: Dihydroergotoxin (an agonist DA — receptors), Droperidolum (neuroleptic), Carvedilol (α-, β-adrenoblocker), Cetanserin (a blocker of peripheral S 2 -serotonin receptors), Labetolol (α-, β — adrenoblocker ))
 The mechanism of action selective α — adrenoblockers block action of Noradrenalinum on receptors of arterioles Indications to use α — adrenoblockers: Hypertrophy of prostatic gland. Possible indicat. to α-adrenoblockers Hypertryglicerinemia, Dislipidemia
The mechanism of action selective α — adrenoblockers block action of Noradrenalinum on receptors of arterioles Indications to use α — adrenoblockers: Hypertrophy of prostatic gland. Possible indicat. to α-adrenoblockers Hypertryglicerinemia, Dislipidemia
 Possible contraindications to use α — аdrenoblockers : : Possible contraindications to use α — аdrenoblockers: Orthostatic hypotension Heart failure. Side effects: Necessity to select a dose in connection with hypotension caused by the first dose. Subjective dose limiting effects.
Possible contraindications to use α — аdrenoblockers : : Possible contraindications to use α — аdrenoblockers: Orthostatic hypotension Heart failure. Side effects: Necessity to select a dose in connection with hypotension caused by the first dose. Subjective dose limiting effects.
 Blockers of АТ 1 -receptors 1. 1. Inactive drugs: Lozartan 50 — 100 mg, Candesartan 4 — 16 mg, Tazocartan. 2. Active medicinal substances: Valsartan 80 — 320 mg, Irbesartan 150 — 300, Telmisartan 40 — 80 mg, Eprosartan 400 — 800 mg.
Blockers of АТ 1 -receptors 1. 1. Inactive drugs: Lozartan 50 — 100 mg, Candesartan 4 — 16 mg, Tazocartan. 2. Active medicinal substances: Valsartan 80 — 320 mg, Irbesartan 150 — 300, Telmisartan 40 — 80 mg, Eprosartan 400 — 800 mg.
 The mechanism of antihypertensive action of blockers of АТ 1 -receptors selective elimination of effects of angiotensin II, prodused through АТ 1 -receptors Indications to use blockers of АТ 1 -receptors: Intolerance for ACE-inhybitors (tussis) Possible indications: Heart failure.
The mechanism of antihypertensive action of blockers of АТ 1 -receptors selective elimination of effects of angiotensin II, prodused through АТ 1 -receptors Indications to use blockers of АТ 1 -receptors: Intolerance for ACE-inhybitors (tussis) Possible indications: Heart failure.
 Contraindications to use of blockers АТ 1 -receptors: Pregnancy, Hyperkalemia, Bilateral stenosis of renal arterias. Side effects — are the same ACE-inhibitors, but frequency is less often.
Contraindications to use of blockers АТ 1 -receptors: Pregnancy, Hyperkalemia, Bilateral stenosis of renal arterias. Side effects — are the same ACE-inhibitors, but frequency is less often.
 Drugs of the central action 1. 1. Drugs of a first generation agonists of the central α 2 -adrenoreceptors (Methyldopa, Clonidinum). 2. Drugs of a second generation — agonists I 1 -imidasol receptors: Moxonidin, Rilmenidin.
Drugs of the central action 1. 1. Drugs of a first generation agonists of the central α 2 -adrenoreceptors (Methyldopa, Clonidinum). 2. Drugs of a second generation — agonists I 1 -imidasol receptors: Moxonidin, Rilmenidin.
 Pharmacological effects of agonists I 1 -imidazol — receptors: Activity of sympathetic nervous system is decreased. A tone of a vagus nerve is rised. Decrease reabsorbation of sodium and water in proximal channels of kidneys. Decrease peripheral resistence and cardiac output. Decrease of releasing of catecholamins. Intensifying of a lipolysis. Often side effects (a sleepiness, dryness in a mouth).
Pharmacological effects of agonists I 1 -imidazol — receptors: Activity of sympathetic nervous system is decreased. A tone of a vagus nerve is rised. Decrease reabsorbation of sodium and water in proximal channels of kidneys. Decrease peripheral resistence and cardiac output. Decrease of releasing of catecholamins. Intensifying of a lipolysis. Often side effects (a sleepiness, dryness in a mouth).


