85fb3b4e0cabbd5c0c1ca578d783b228.ppt
- Количество слайдов: 16
 Differentiating Lower Extremity Pain: Arteries, Veins, and Nerves! The Value of the ABI Amjad Al. Mahameed, MD, MPH Division of Cardiology Beth Israel Deaconess Medical Center Boston
Differentiating Lower Extremity Pain: Arteries, Veins, and Nerves! The Value of the ABI Amjad Al. Mahameed, MD, MPH Division of Cardiology Beth Israel Deaconess Medical Center Boston
 Objectives • Review the differential diagnosis of lower extremity dysfunction • Beyond intermittent claudication: Recognize the different clinical presentations of PAD • PAD as the cause of symptoms: Reflect on clinical evaluation
Objectives • Review the differential diagnosis of lower extremity dysfunction • Beyond intermittent claudication: Recognize the different clinical presentations of PAD • PAD as the cause of symptoms: Reflect on clinical evaluation
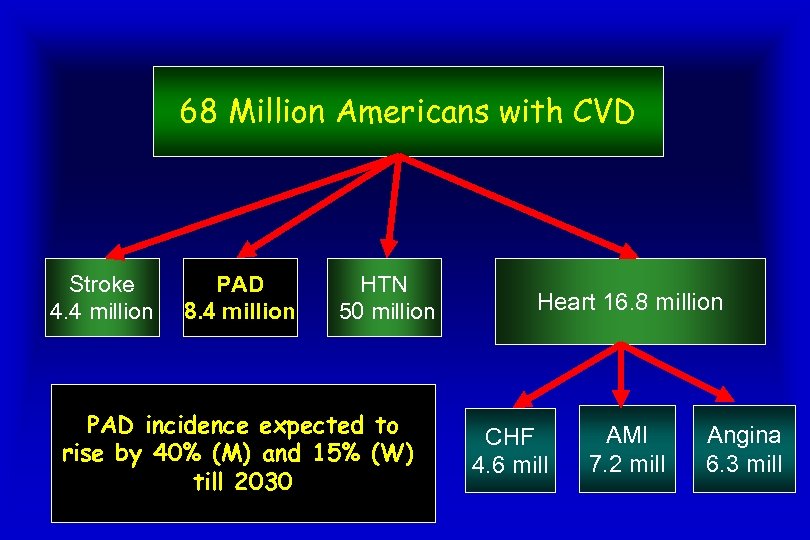 68 Million Americans with CVD Stroke 4. 4 million PAD 8. 4 million HTN 50 million PAD incidence expected to rise by 40% (M) and 15% (W) till 2030 Heart 16. 8 million CHF 4. 6 mill AMI 7. 2 mill Angina 6. 3 mill
68 Million Americans with CVD Stroke 4. 4 million PAD 8. 4 million HTN 50 million PAD incidence expected to rise by 40% (M) and 15% (W) till 2030 Heart 16. 8 million CHF 4. 6 mill AMI 7. 2 mill Angina 6. 3 mill
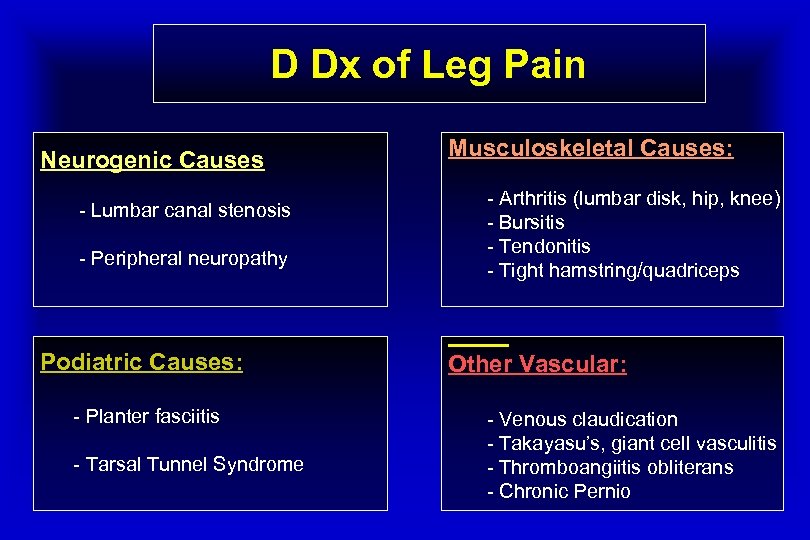 D Dx of Leg Pain Neurogenic Causes - Lumbar canal stenosis - Peripheral neuropathy Podiatric Causes: - Planter fasciitis - Tarsal Tunnel Syndrome Musculoskeletal Causes: - Arthritis (lumbar disk, hip, knee) - Bursitis - Tendonitis - Tight hamstring/quadriceps Other Vascular: - Venous claudication - Takayasu’s, giant cell vasculitis - Thromboangiitis obliterans - Chronic Pernio
D Dx of Leg Pain Neurogenic Causes - Lumbar canal stenosis - Peripheral neuropathy Podiatric Causes: - Planter fasciitis - Tarsal Tunnel Syndrome Musculoskeletal Causes: - Arthritis (lumbar disk, hip, knee) - Bursitis - Tendonitis - Tight hamstring/quadriceps Other Vascular: - Venous claudication - Takayasu’s, giant cell vasculitis - Thromboangiitis obliterans - Chronic Pernio
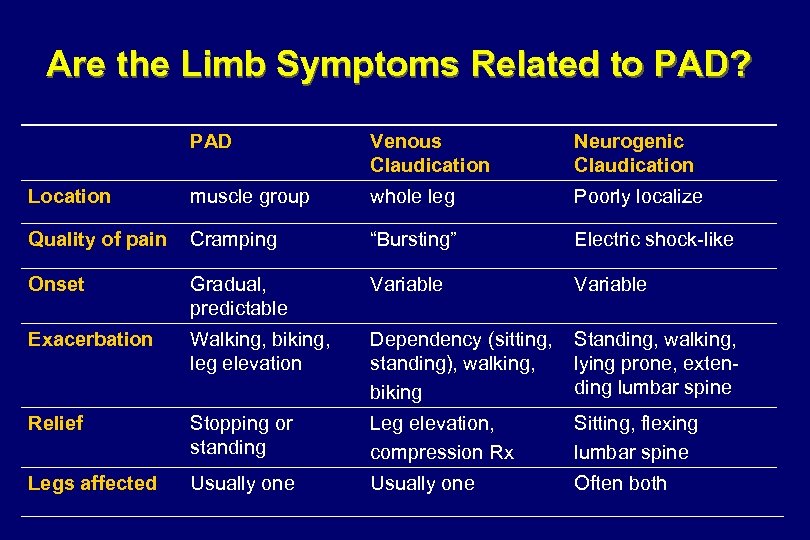 Are the Limb Symptoms Related to PAD? PAD Venous Claudication Neurogenic Claudication Location muscle group whole leg Poorly localize Quality of pain Cramping “Bursting” Electric shock-like Onset Gradual, predictable Variable Exacerbation Walking, biking, leg elevation Dependency (sitting, standing), walking, biking Standing, walking, lying prone, extending lumbar spine Relief Stopping or standing Leg elevation, compression Rx Sitting, flexing lumbar spine Legs affected Usually one Often both
Are the Limb Symptoms Related to PAD? PAD Venous Claudication Neurogenic Claudication Location muscle group whole leg Poorly localize Quality of pain Cramping “Bursting” Electric shock-like Onset Gradual, predictable Variable Exacerbation Walking, biking, leg elevation Dependency (sitting, standing), walking, biking Standing, walking, lying prone, extending lumbar spine Relief Stopping or standing Leg elevation, compression Rx Sitting, flexing lumbar spine Legs affected Usually one Often both
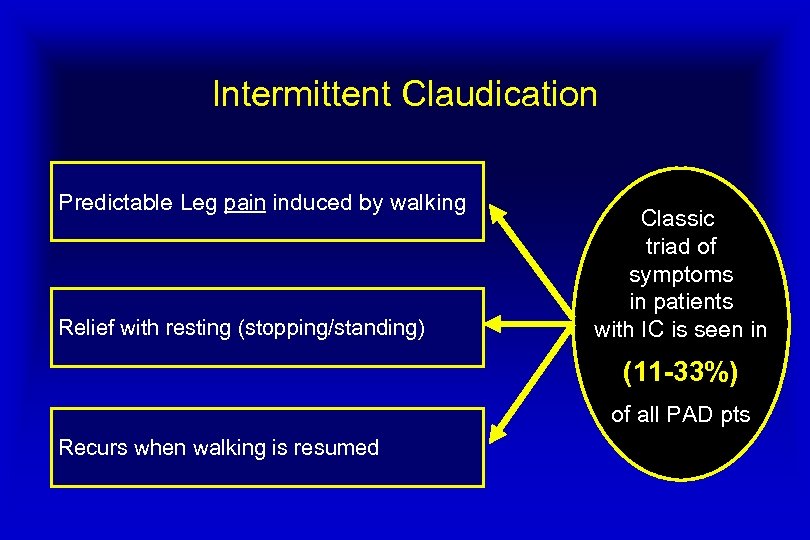 Intermittent Claudication Predictable Leg pain induced by walking Relief with resting (stopping/standing) Classic triad of symptoms in patients with IC is seen in (11 -33%) of all PAD pts Recurs when walking is resumed
Intermittent Claudication Predictable Leg pain induced by walking Relief with resting (stopping/standing) Classic triad of symptoms in patients with IC is seen in (11 -33%) of all PAD pts Recurs when walking is resumed
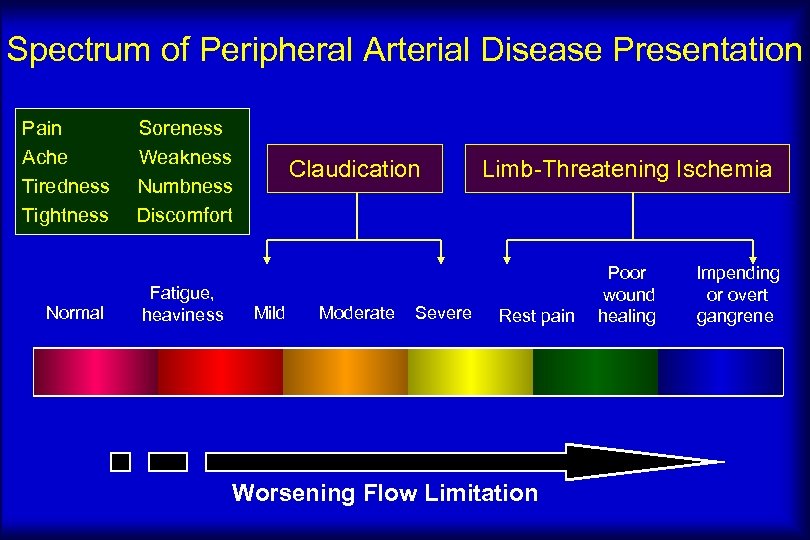 Spectrum of Peripheral Arterial Disease Presentation Pain Ache Tiredness Tightness Normal Soreness Weakness Numbness Discomfort Fatigue, heaviness Claudication Mild Limb-Threatening Ischemia Moderate Poor wound healing Severe Rest pain Worsening Flow Limitation Impending or overt gangrene
Spectrum of Peripheral Arterial Disease Presentation Pain Ache Tiredness Tightness Normal Soreness Weakness Numbness Discomfort Fatigue, heaviness Claudication Mild Limb-Threatening Ischemia Moderate Poor wound healing Severe Rest pain Worsening Flow Limitation Impending or overt gangrene
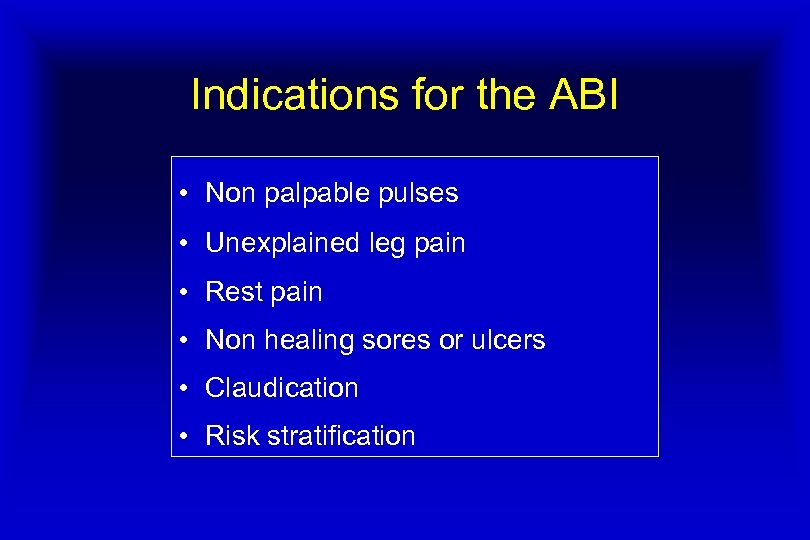 Indications for the ABI • Non palpable pulses • Unexplained leg pain • Rest pain • Non healing sores or ulcers • Claudication • Risk stratification
Indications for the ABI • Non palpable pulses • Unexplained leg pain • Rest pain • Non healing sores or ulcers • Claudication • Risk stratification
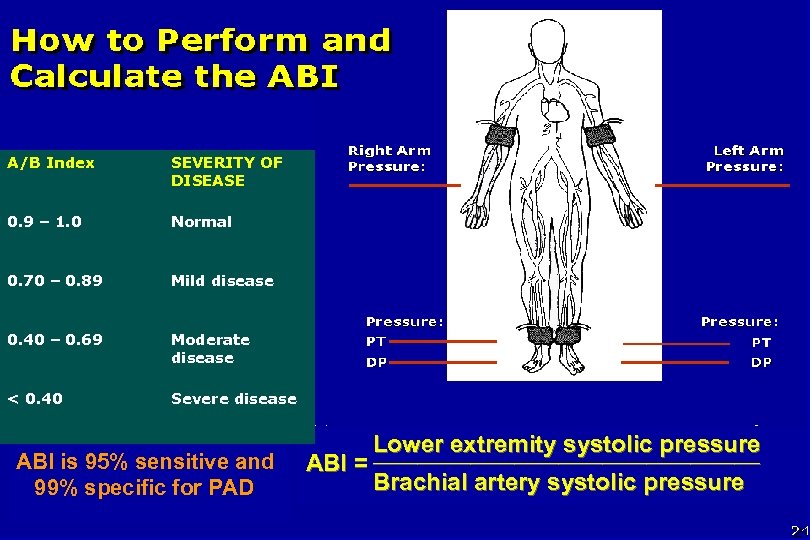 A/B Index SEVERITY OF DISEASE 0. 9 – 1. 0 Normal 0. 70 – 0. 89 Mild disease 0. 40 – 0. 69 Moderate disease < 0. 40 Severe disease ABI is 95% sensitive and 99% specific for PAD ABI = Lower extremity systolic pressure ______________________ Brachial artery systolic pressure
A/B Index SEVERITY OF DISEASE 0. 9 – 1. 0 Normal 0. 70 – 0. 89 Mild disease 0. 40 – 0. 69 Moderate disease < 0. 40 Severe disease ABI is 95% sensitive and 99% specific for PAD ABI = Lower extremity systolic pressure ______________________ Brachial artery systolic pressure
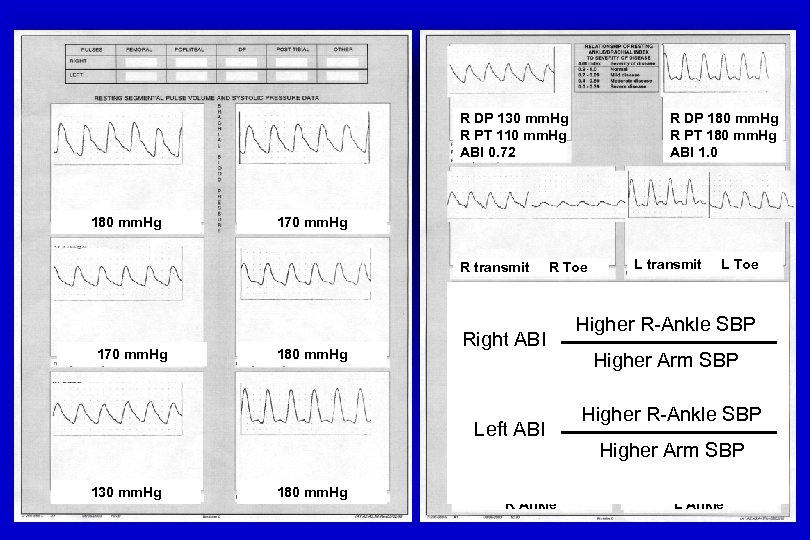 R DP 130 mm. Hg R PT 110 mm. Hg ABI 0. 72 180 mm. Hg 170 mm. Hg R transmit 170 mm. Hg 180 mm. Hg R Toe Right ABI Left ABI 130 mm. Hg R DP 180 mm. Hg R PT 180 mm. Hg ABI 1. 0 180 mm. Hg R Ankle L transmit L Toe Higher R-Ankle SBP Post Exercise Higher Arm SBP Higher R-Ankle SBP Higher Arm SBP L Ankle
R DP 130 mm. Hg R PT 110 mm. Hg ABI 0. 72 180 mm. Hg 170 mm. Hg R transmit 170 mm. Hg 180 mm. Hg R Toe Right ABI Left ABI 130 mm. Hg R DP 180 mm. Hg R PT 180 mm. Hg ABI 1. 0 180 mm. Hg R Ankle L transmit L Toe Higher R-Ankle SBP Post Exercise Higher Arm SBP Higher R-Ankle SBP Higher Arm SBP L Ankle
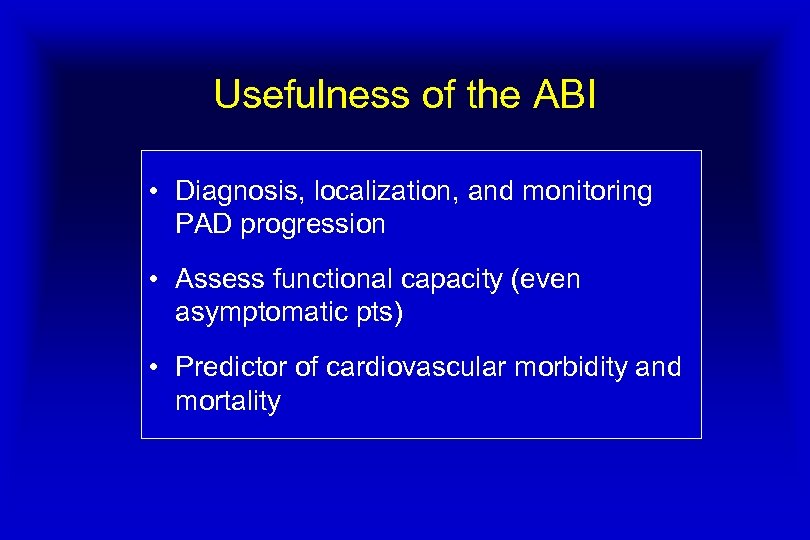 Usefulness of the ABI • Diagnosis, localization, and monitoring PAD progression • Assess functional capacity (even asymptomatic pts) • Predictor of cardiovascular morbidity and mortality
Usefulness of the ABI • Diagnosis, localization, and monitoring PAD progression • Assess functional capacity (even asymptomatic pts) • Predictor of cardiovascular morbidity and mortality
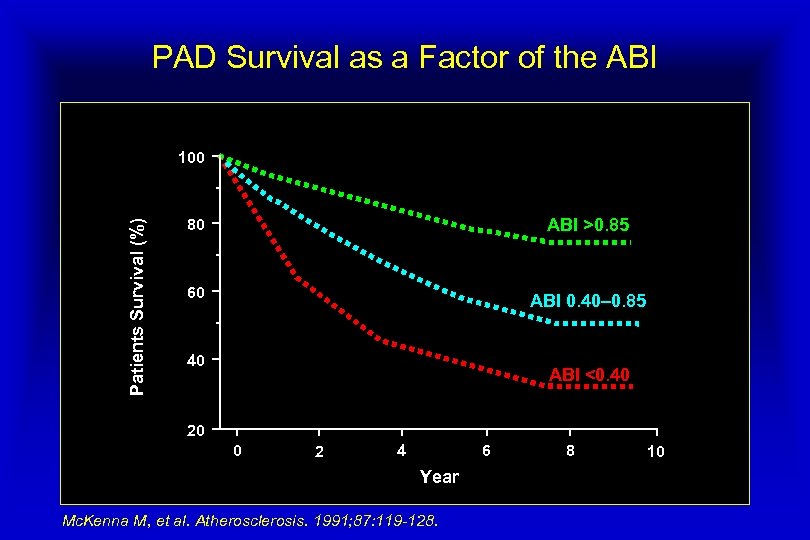 PAD Survival as a Factor of the ABI Patients Survival (%) 100 80 ABI >0. 85 60 ABI 0. 40– 0. 85 40 ABI <0. 40 20 0 2 6 4 Year Mc. Kenna M, et al. Atherosclerosis. 1991; 87: 119 -128. 8 10
PAD Survival as a Factor of the ABI Patients Survival (%) 100 80 ABI >0. 85 60 ABI 0. 40– 0. 85 40 ABI <0. 40 20 0 2 6 4 Year Mc. Kenna M, et al. Atherosclerosis. 1991; 87: 119 -128. 8 10
 PAD and Functional Impairment • Peripheral arterial disease (PAD) is associated with – – – Poorer walking endurance Slower walking speed Poorer balance • Compared to individuals without PAD Olin JW. AM J Med 10 -17, 1998. Scherer SA. Arch phys Med Rehab 79: 529 -531, 1998 Regensteiner JG. J Vasc Med Biol 2: 142 -152, 1990 Limited leisure and Work activities
PAD and Functional Impairment • Peripheral arterial disease (PAD) is associated with – – – Poorer walking endurance Slower walking speed Poorer balance • Compared to individuals without PAD Olin JW. AM J Med 10 -17, 1998. Scherer SA. Arch phys Med Rehab 79: 529 -531, 1998 Regensteiner JG. J Vasc Med Biol 2: 142 -152, 1990 Limited leisure and Work activities
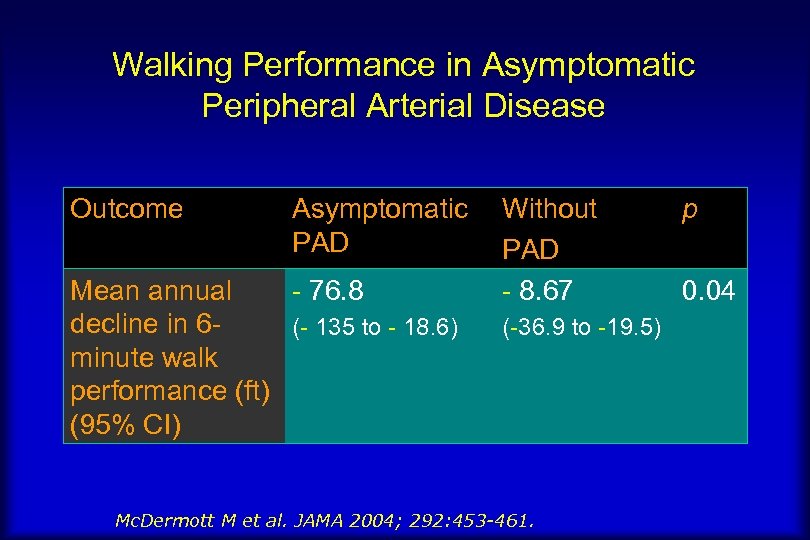 Walking Performance in Asymptomatic Peripheral Arterial Disease Outcome Asymptomatic PAD Mean annual - 76. 8 decline in 6(- 135 to - 18. 6) minute walk performance (ft) (95% CI) Without PAD - 8. 67 (-36. 9 to -19. 5) Mc. Dermott M et al. JAMA 2004; 292: 453 -461. p 0. 04
Walking Performance in Asymptomatic Peripheral Arterial Disease Outcome Asymptomatic PAD Mean annual - 76. 8 decline in 6(- 135 to - 18. 6) minute walk performance (ft) (95% CI) Without PAD - 8. 67 (-36. 9 to -19. 5) Mc. Dermott M et al. JAMA 2004; 292: 453 -461. p 0. 04
 Clinical Tips • The DP pulse is congenitally absent in up to 32% of normal individual but the absence of PT pulse is always abnormal • Lack of hair on the shins is not always a sign of PAD • Patients with rest pain may present with pitting edema • Persistence of pallor > 40 second after 1 minute elevation is indicative of severe disease
Clinical Tips • The DP pulse is congenitally absent in up to 32% of normal individual but the absence of PT pulse is always abnormal • Lack of hair on the shins is not always a sign of PAD • Patients with rest pain may present with pitting edema • Persistence of pallor > 40 second after 1 minute elevation is indicative of severe disease
 PAD is NOT the Cause of Leg Symptoms if: • History and physical exam not suggestive • Normal rest ABI and treadmill exercise testing • Presence of alternative diagnosis • In this process, you may also obtain spine MRI, X-rays of the hips and knees, and even EMG/NCS
PAD is NOT the Cause of Leg Symptoms if: • History and physical exam not suggestive • Normal rest ABI and treadmill exercise testing • Presence of alternative diagnosis • In this process, you may also obtain spine MRI, X-rays of the hips and knees, and even EMG/NCS


