Differential diagnosis of pharyngitis Main inflammatory throat diseases


14036-diphtheria_tonsillitis_im.ppt
- Количество слайдов: 63
 Differential diagnosis of pharyngitis
Differential diagnosis of pharyngitis
 Main inflammatory throat diseases Pharyngitis Tonsillitis, tonsillopharyngitis Adenoiditis Paratonsillar abscess Retropharyngeal abscess
Main inflammatory throat diseases Pharyngitis Tonsillitis, tonsillopharyngitis Adenoiditis Paratonsillar abscess Retropharyngeal abscess
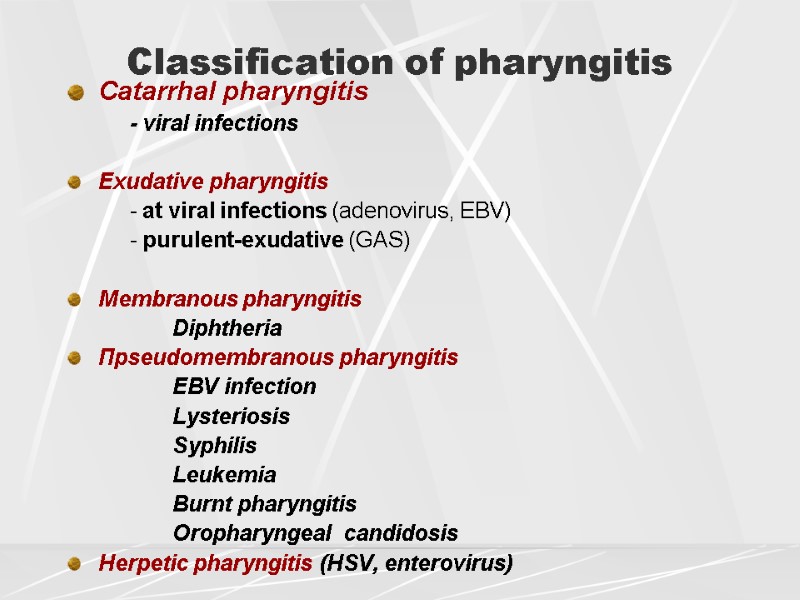
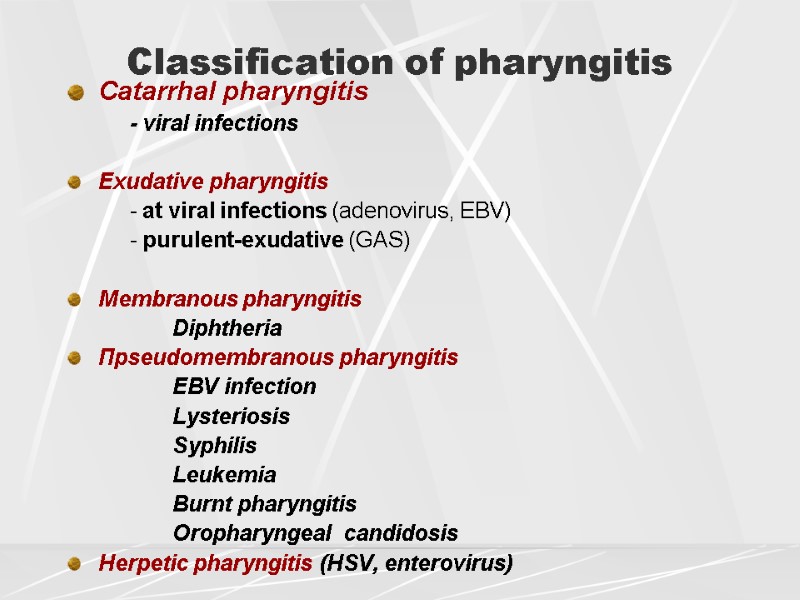 Classification of pharyngitis Catarrhal pharyngitis - viral infections Exudative pharyngitis - at viral infections (adenovirus, ЕВV) - purulent-exudative (GAS) Membranous pharyngitis Diphtheria Пpseudomembranous pharyngitis EBV infection Lysteriosis Syphilis Leukemia Burnt pharyngitis Oropharyngeal candidosis Herpetic pharyngitis (НSV, enterovirus)
Classification of pharyngitis Catarrhal pharyngitis - viral infections Exudative pharyngitis - at viral infections (adenovirus, ЕВV) - purulent-exudative (GAS) Membranous pharyngitis Diphtheria Пpseudomembranous pharyngitis EBV infection Lysteriosis Syphilis Leukemia Burnt pharyngitis Oropharyngeal candidosis Herpetic pharyngitis (НSV, enterovirus)
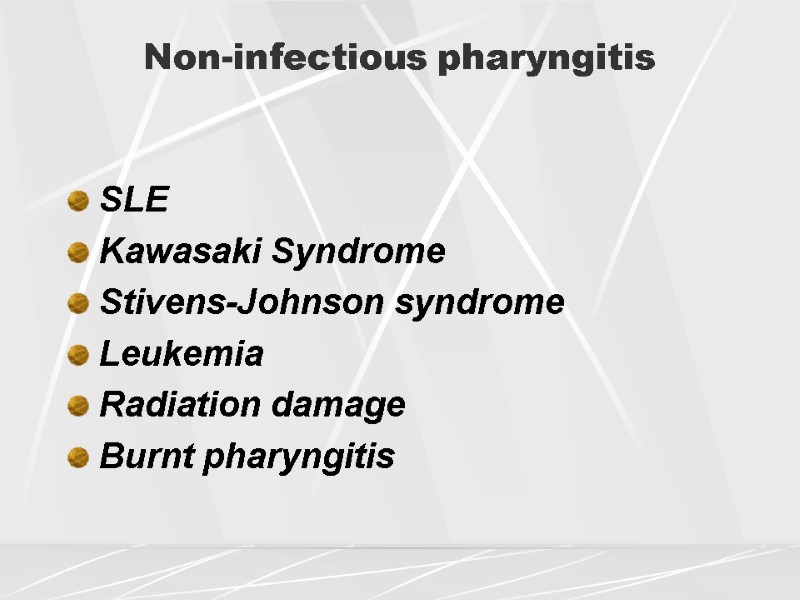 Non-infectious pharyngitis SLE Kawasaki Syndrome Stivens-Johnson syndrome Leukemia Radiation damage Burnt pharyngitis
Non-infectious pharyngitis SLE Kawasaki Syndrome Stivens-Johnson syndrome Leukemia Radiation damage Burnt pharyngitis
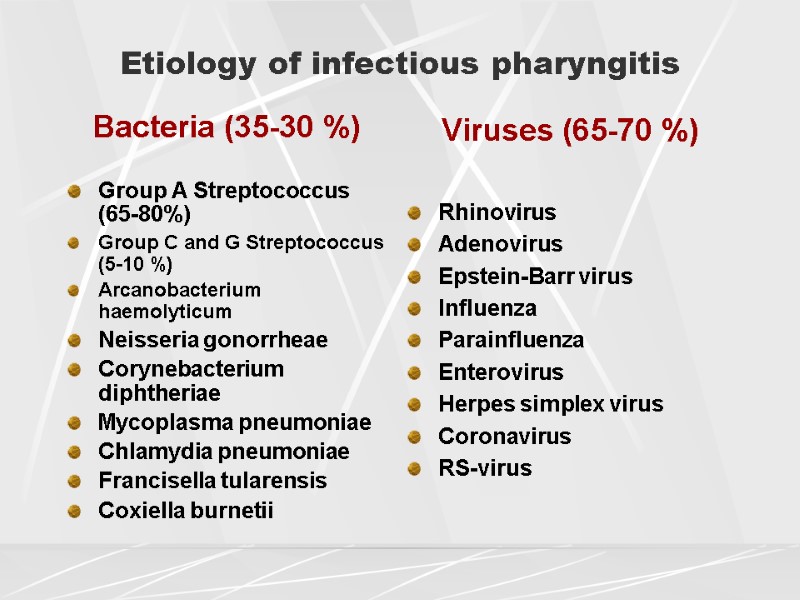
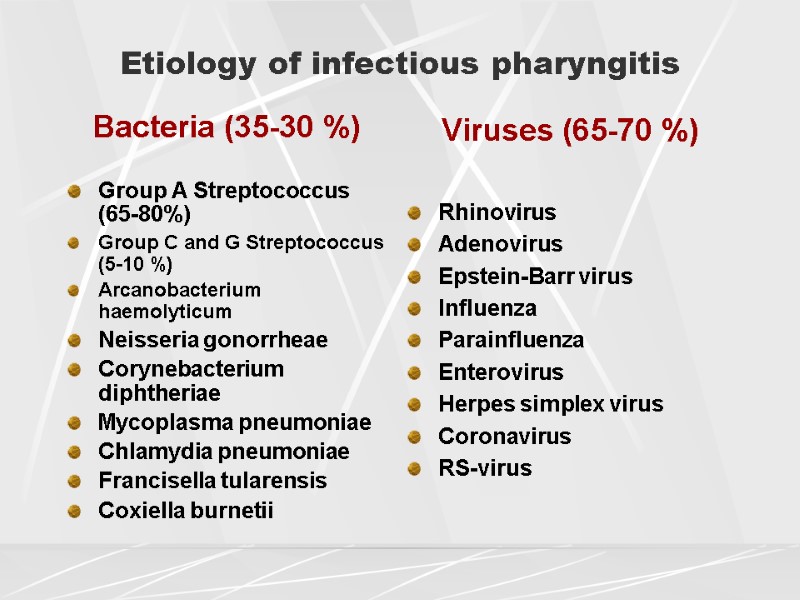 Etiology of infectious pharyngitis Bacteria (35-30 %) Group A Streptococcus (65-80%) Group C and G Streptococcus (5-10 %) Arcanobacterium haemolyticum Neisseria gonorrheae Corynebacterium diphtheriae Mycoplasma pneumoniae Chlamydia pneumoniae Francisella tularensis Coxiella burnetii Viruses (65-70 %) Rhinovirus Adenovirus Epstein-Barr virus Influenza Parainfluenza Enterovirus Herpes simplex virus Coronavirus RS-virus
Etiology of infectious pharyngitis Bacteria (35-30 %) Group A Streptococcus (65-80%) Group C and G Streptococcus (5-10 %) Arcanobacterium haemolyticum Neisseria gonorrheae Corynebacterium diphtheriae Mycoplasma pneumoniae Chlamydia pneumoniae Francisella tularensis Coxiella burnetii Viruses (65-70 %) Rhinovirus Adenovirus Epstein-Barr virus Influenza Parainfluenza Enterovirus Herpes simplex virus Coronavirus RS-virus
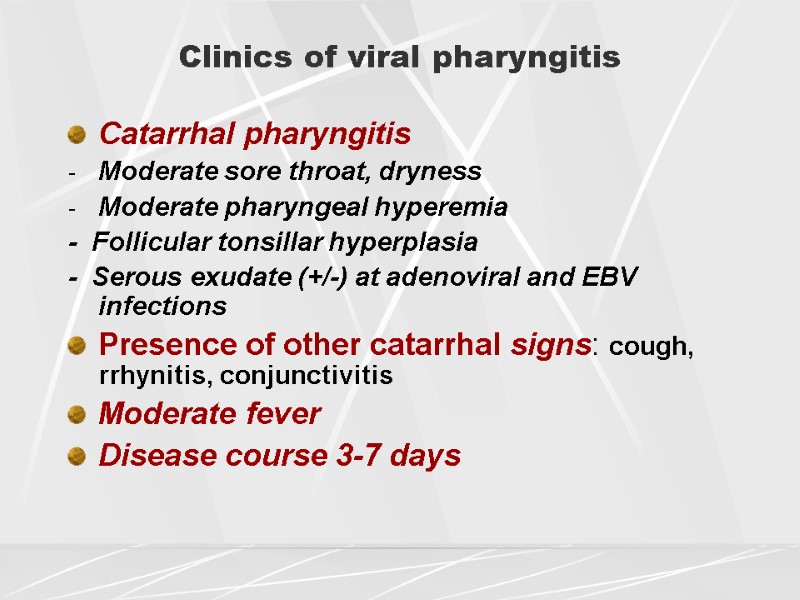
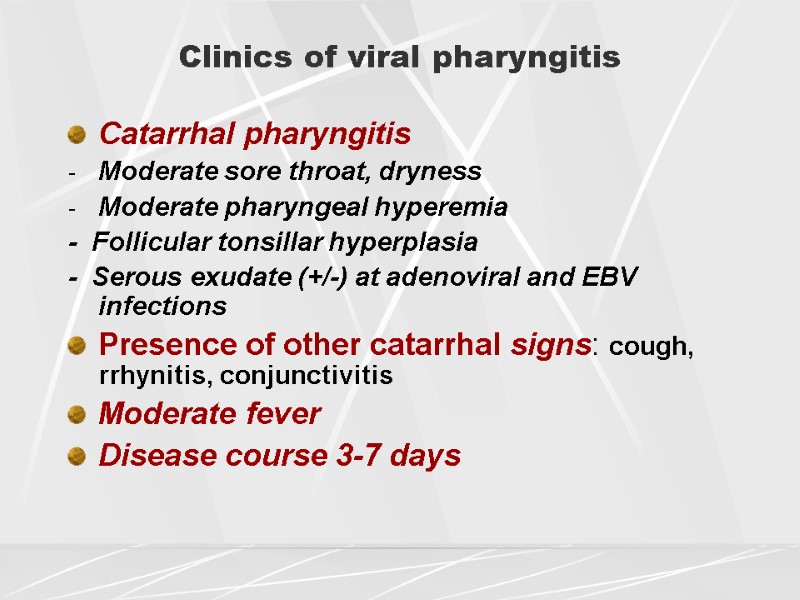 Clinics of viral pharyngitis Catarrhal pharyngitis Moderate sore throat, dryness Moderate pharyngeal hyperemia - Follicular tonsillar hyperplasia - Serous exudate (+/-) at adenoviral and EBV infections Presence of other catarrhal signs: cough, rrhynitis, conjunctivitis Moderate fever Disease course 3-7 days
Clinics of viral pharyngitis Catarrhal pharyngitis Moderate sore throat, dryness Moderate pharyngeal hyperemia - Follicular tonsillar hyperplasia - Serous exudate (+/-) at adenoviral and EBV infections Presence of other catarrhal signs: cough, rrhynitis, conjunctivitis Moderate fever Disease course 3-7 days
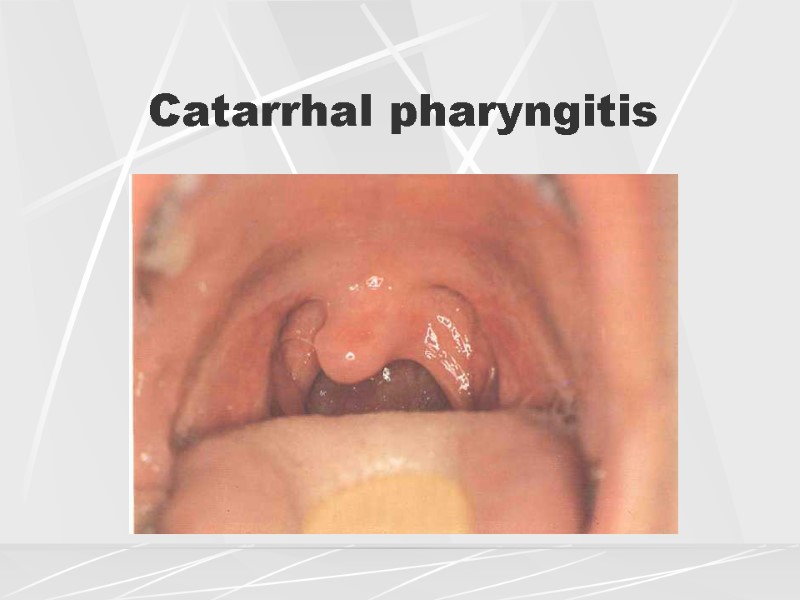
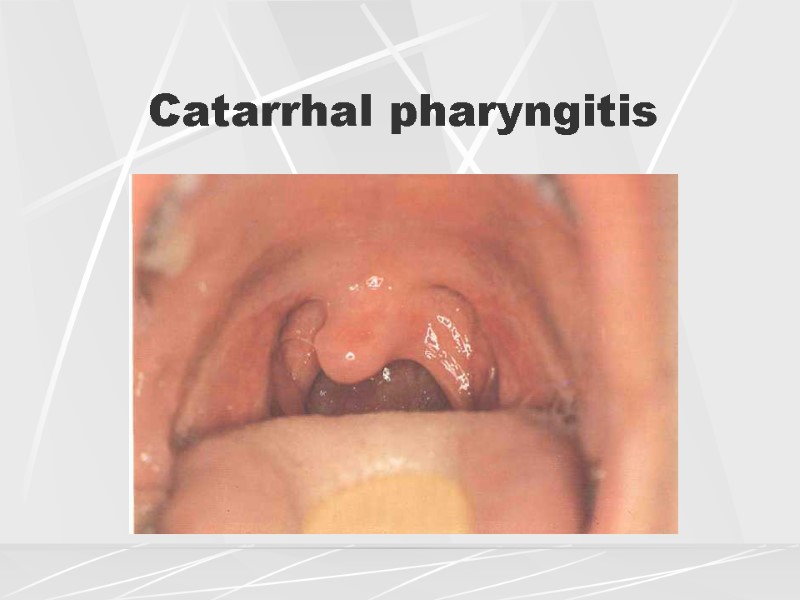 Catarrhal pharyngitis
Catarrhal pharyngitis
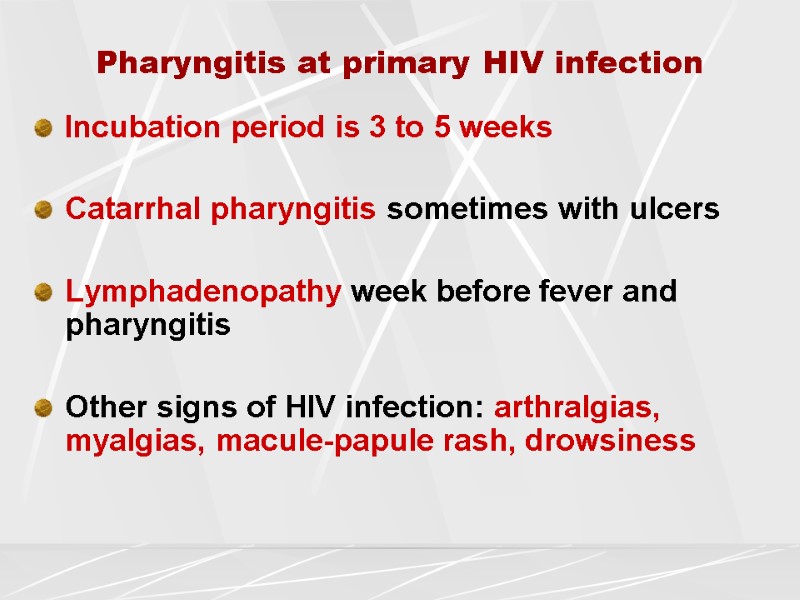
 Pharyngitis at primary HIV infection Incubation period is 3 to 5 weeks Catarrhal pharyngitis sometimes with ulcers Lymphadenopathy week before fever and pharyngitis Other signs of HIV infection: arthralgias, myalgias, macule-papule rash, drowsiness
Pharyngitis at primary HIV infection Incubation period is 3 to 5 weeks Catarrhal pharyngitis sometimes with ulcers Lymphadenopathy week before fever and pharyngitis Other signs of HIV infection: arthralgias, myalgias, macule-papule rash, drowsiness
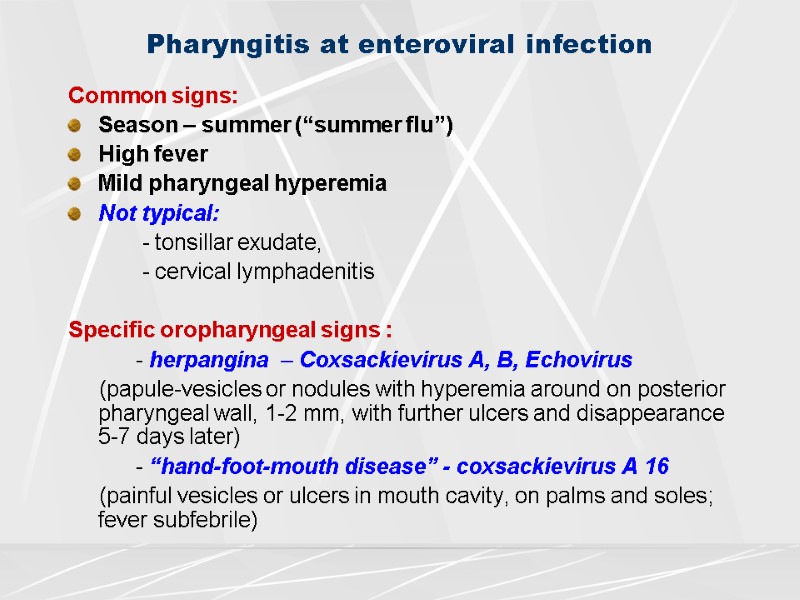
 Pharyngitis at enteroviral infection Common signs: Season – summer (“summer flu”) High fever Mild pharyngeal hyperemia Not typical: - tonsillar exudate, - cervical lymphadenitis Specific oropharyngeal signs : - herpangina – Сoxsackievirus A, B, Echovirus (papule-vesicles or nodules with hyperemia around on posterior pharyngeal wall, 1-2 mm, with further ulcers and disappearance 5-7 days later) - “hand-foot-mouth disease” - coxsackievirus A 16 (painful vesicles or ulcers in mouth cavity, on palms and soles; fever subfebrile)
Pharyngitis at enteroviral infection Common signs: Season – summer (“summer flu”) High fever Mild pharyngeal hyperemia Not typical: - tonsillar exudate, - cervical lymphadenitis Specific oropharyngeal signs : - herpangina – Сoxsackievirus A, B, Echovirus (papule-vesicles or nodules with hyperemia around on posterior pharyngeal wall, 1-2 mm, with further ulcers and disappearance 5-7 days later) - “hand-foot-mouth disease” - coxsackievirus A 16 (painful vesicles or ulcers in mouth cavity, on palms and soles; fever subfebrile)
 Herpangina at enteroviral infection
Herpangina at enteroviral infection
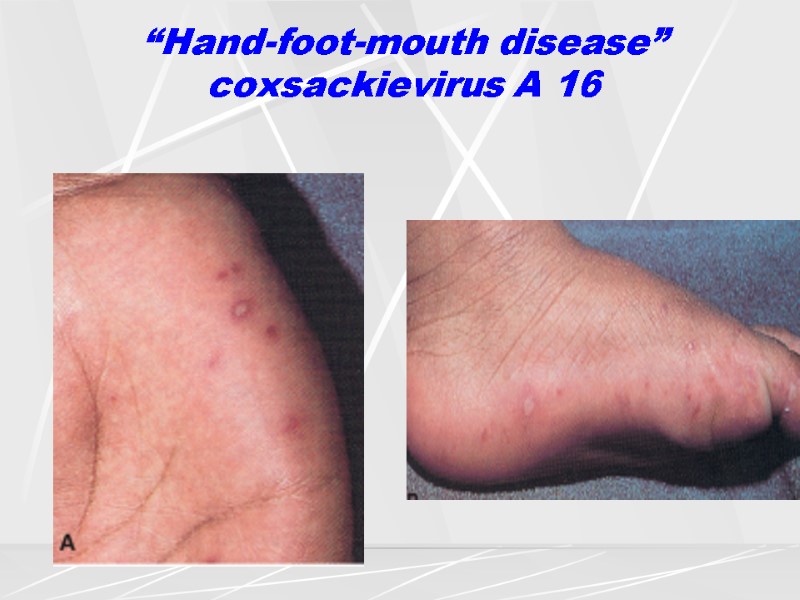
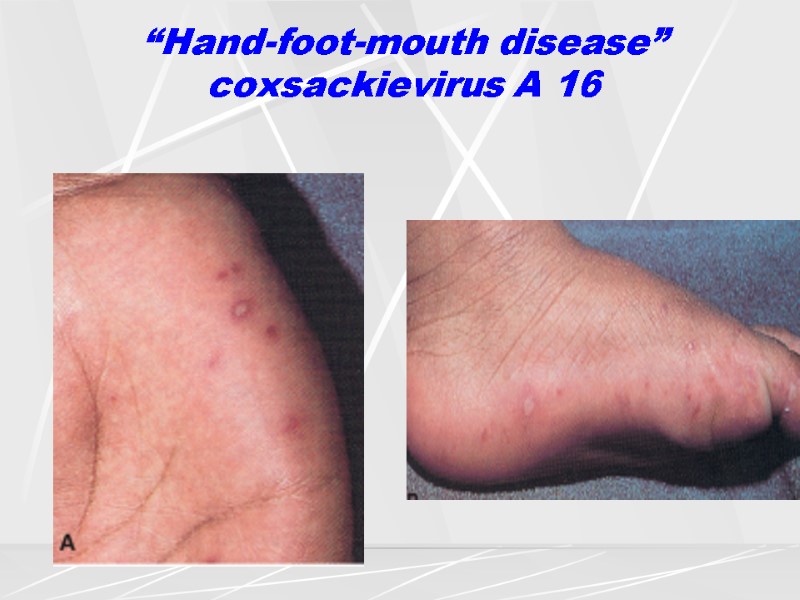 “Hand-foot-mouth disease” coxsackievirus A 16
“Hand-foot-mouth disease” coxsackievirus A 16
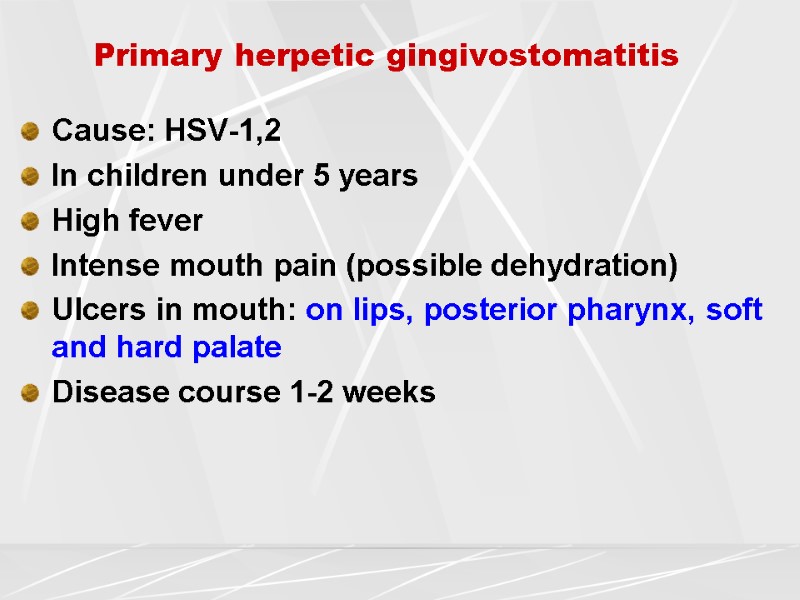
 Primary herpetic gingivostomatitis Cause: HSV-1,2 In children under 5 years High fever Intense mouth pain (possible dehydration) Ulcers in mouth: on lips, posterior pharynx, soft and hard palate Disease course 1-2 weeks
Primary herpetic gingivostomatitis Cause: HSV-1,2 In children under 5 years High fever Intense mouth pain (possible dehydration) Ulcers in mouth: on lips, posterior pharynx, soft and hard palate Disease course 1-2 weeks
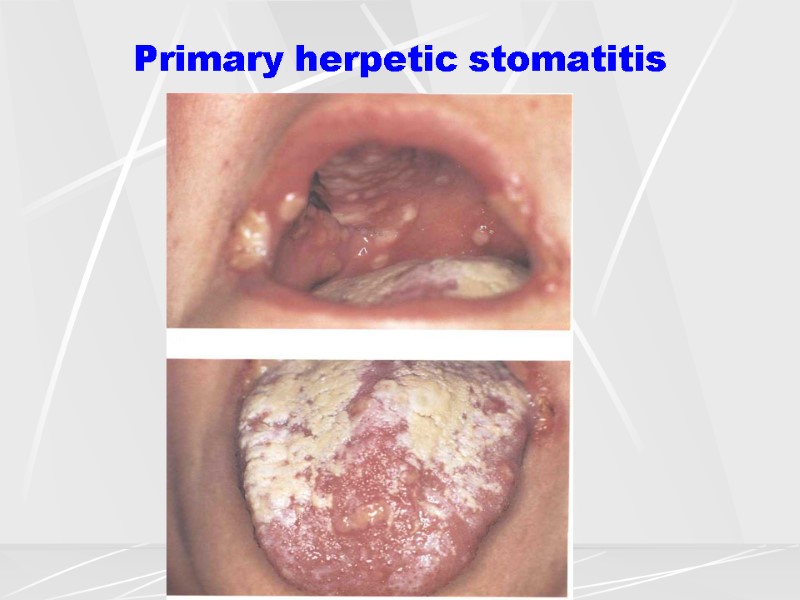
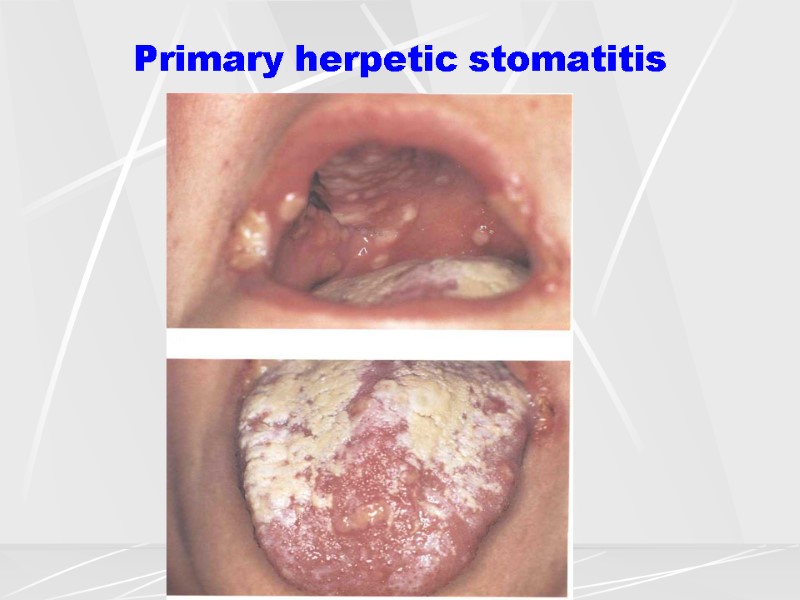 Primary herpetic stomatitis
Primary herpetic stomatitis
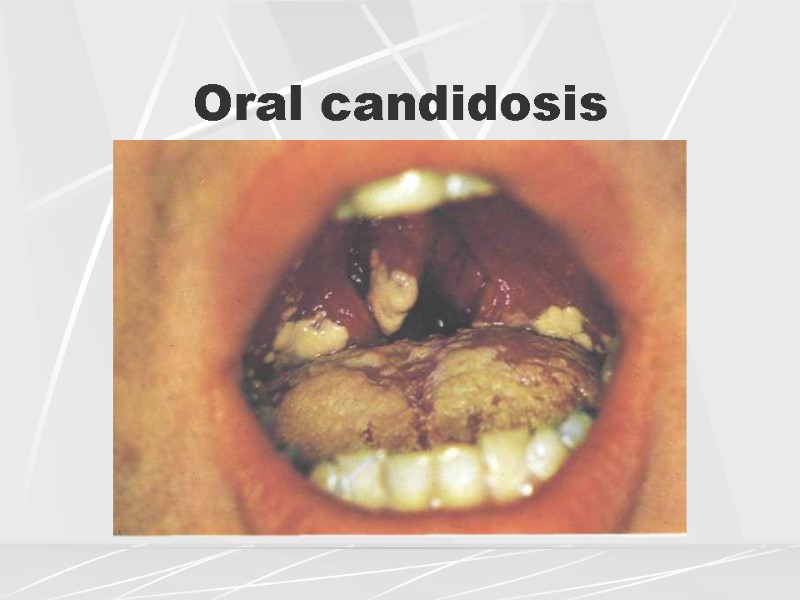
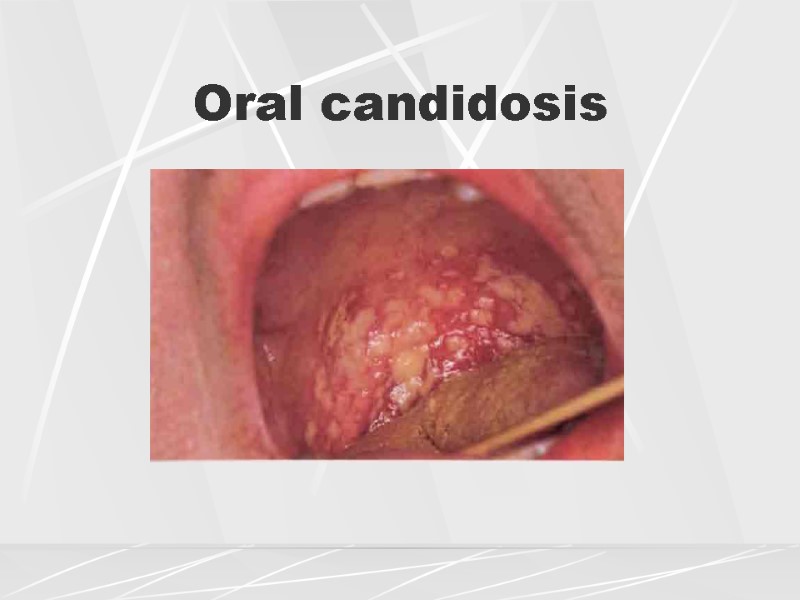
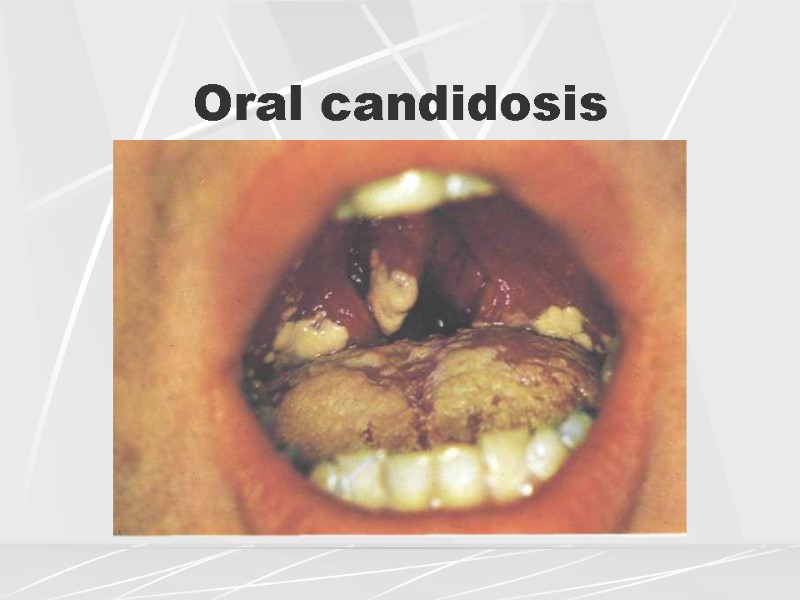 Oral candidosis
Oral candidosis
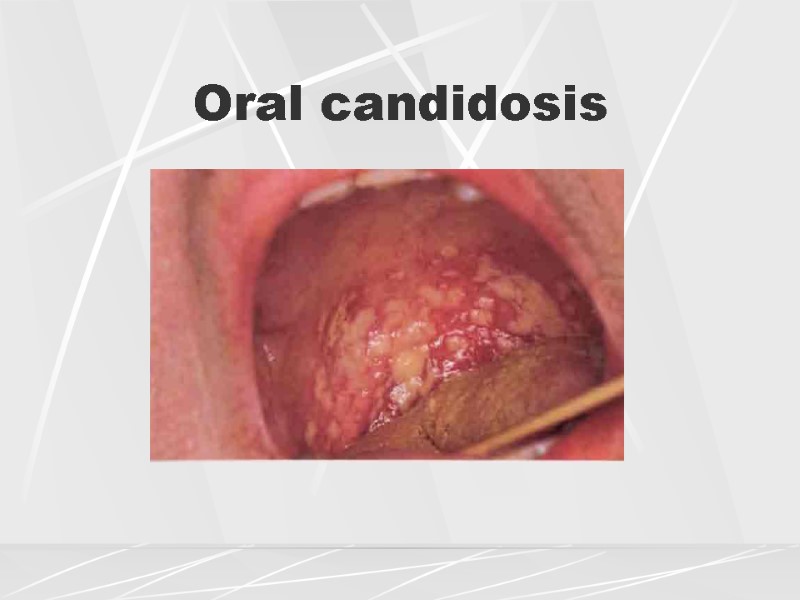 Oral candidosis
Oral candidosis
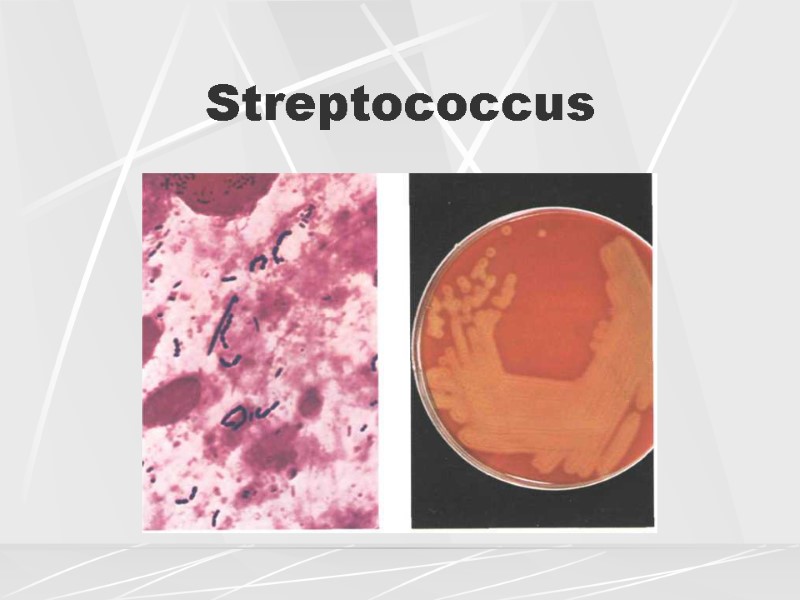
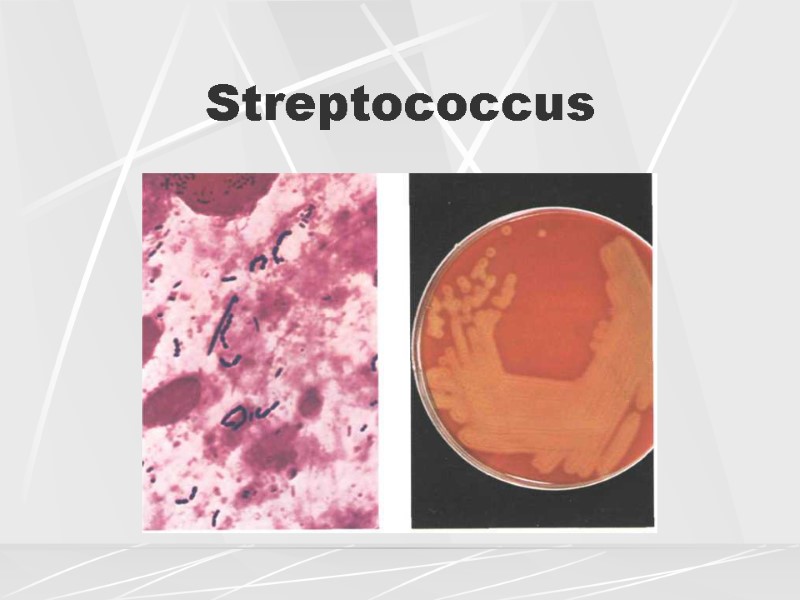 Streptococcus
Streptococcus
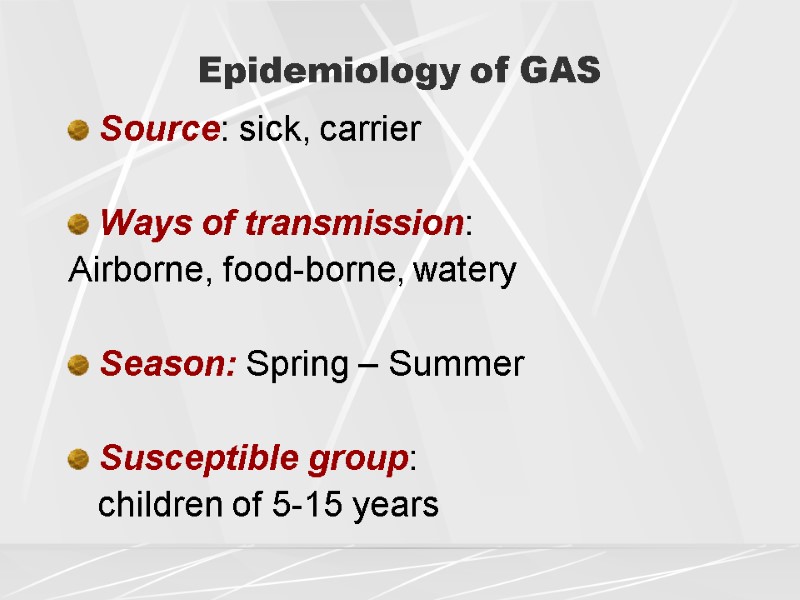
 Epidemiology of GAS Source: sick, carrier Ways of transmission: Airborne, food-borne, watery Season: Spring – Summer Susceptible group: children of 5-15 years
Epidemiology of GAS Source: sick, carrier Ways of transmission: Airborne, food-borne, watery Season: Spring – Summer Susceptible group: children of 5-15 years
 Streptococcal (GAS) infection Classification of GAS – associated diseases 1. Purulent diseases: - respiratory infections; - skin and soft tissue infections; - systemic purulent infections. 2. Toxin – mediated infections (scarlet fever, TSS, erysipelas). Infectious – allergic complications (rheumatic fever, carditis, glomerulonephritis, PANDAS)
Streptococcal (GAS) infection Classification of GAS – associated diseases 1. Purulent diseases: - respiratory infections; - skin and soft tissue infections; - systemic purulent infections. 2. Toxin – mediated infections (scarlet fever, TSS, erysipelas). Infectious – allergic complications (rheumatic fever, carditis, glomerulonephritis, PANDAS)
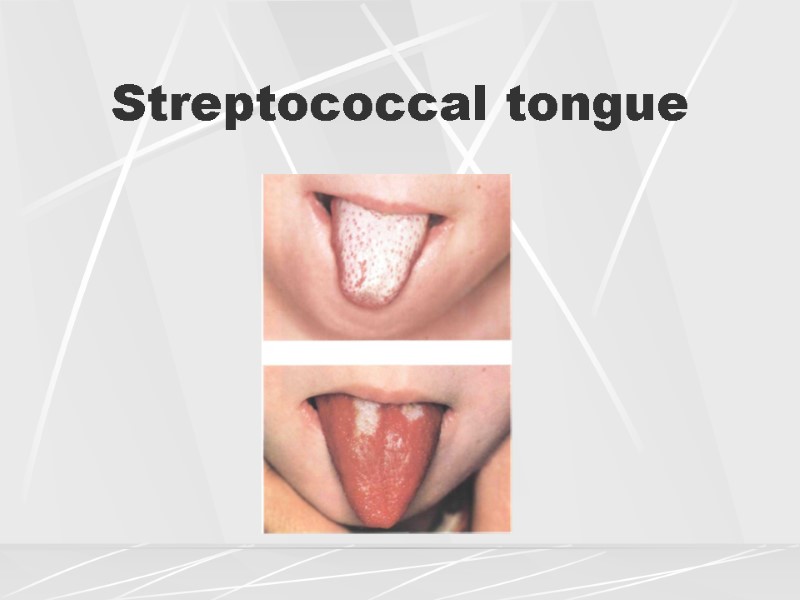
 Streptococcal pharyngitis Associated with hemolytic Streptococcus of groups А, С, G Fever 39.5 С and higher, chills Prominent throat pain and difficulty of swallowing PE: “burning throat”, uvualr edema, Yellowish purulent covers in lacunas or tonsillar follicules “Strawberry tongue” (papules + color) Tense and painful tonsillar lymph nodes
Streptococcal pharyngitis Associated with hemolytic Streptococcus of groups А, С, G Fever 39.5 С and higher, chills Prominent throat pain and difficulty of swallowing PE: “burning throat”, uvualr edema, Yellowish purulent covers in lacunas or tonsillar follicules “Strawberry tongue” (papules + color) Tense and painful tonsillar lymph nodes
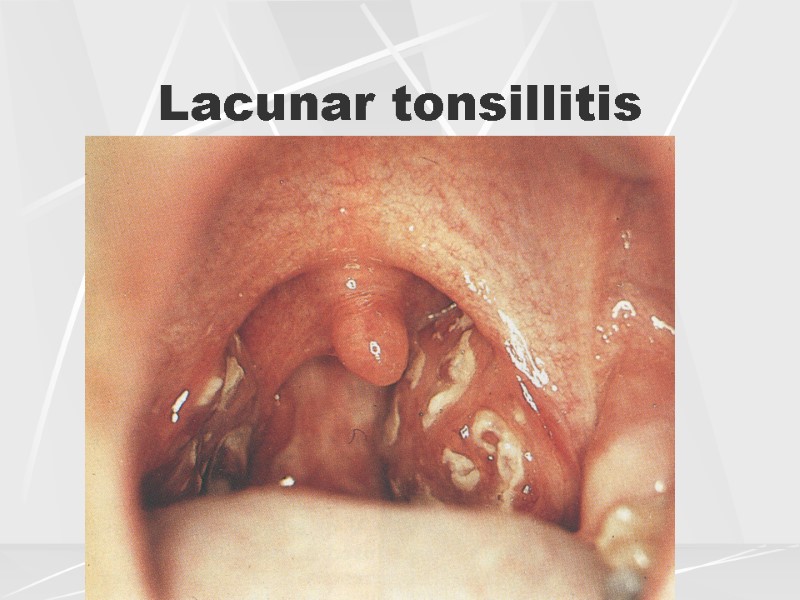
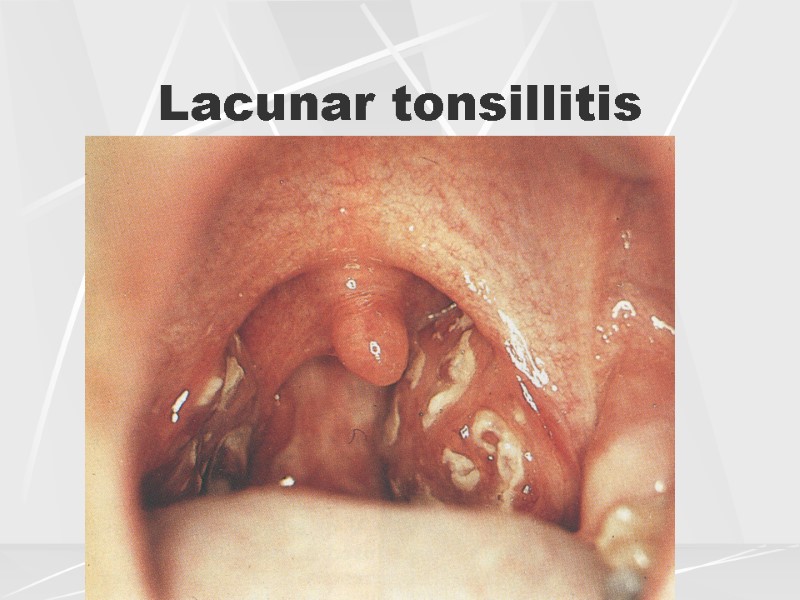 Lacunar tonsillitis
Lacunar tonsillitis
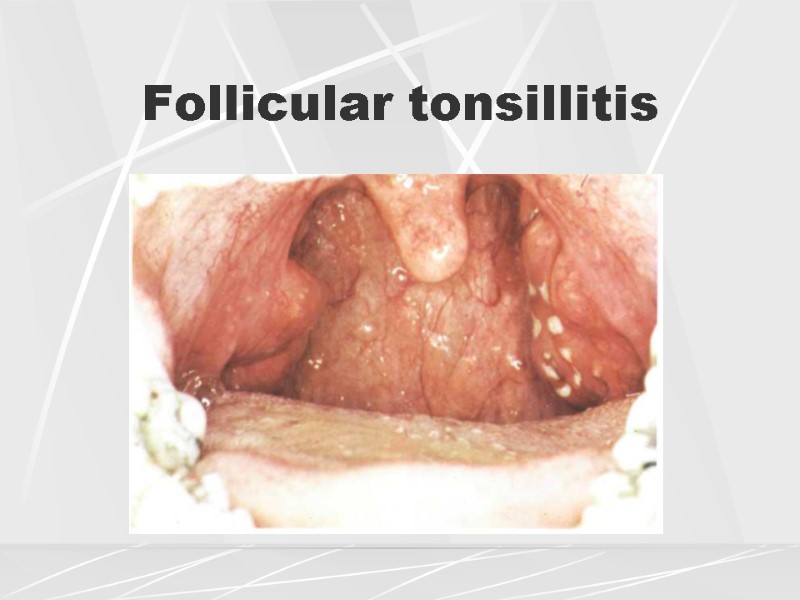
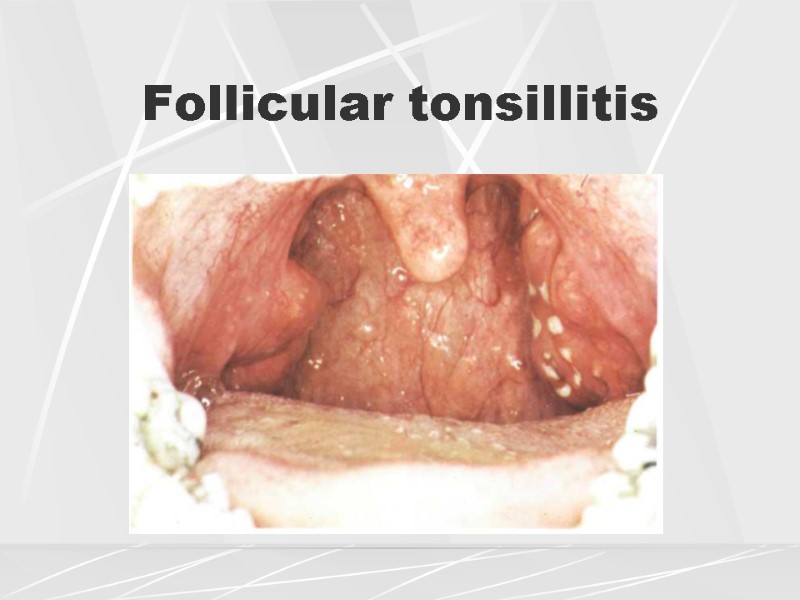 Follicular tonsillitis
Follicular tonsillitis
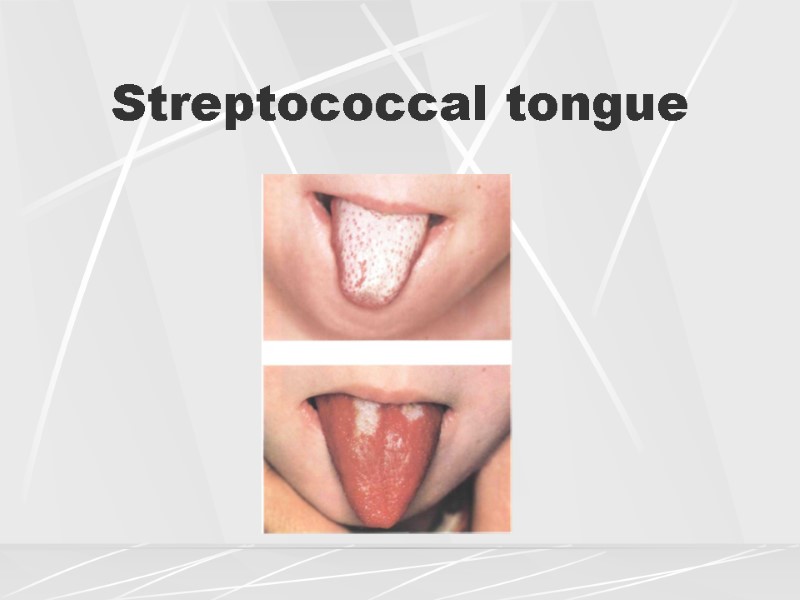 Streptococcal tongue
Streptococcal tongue
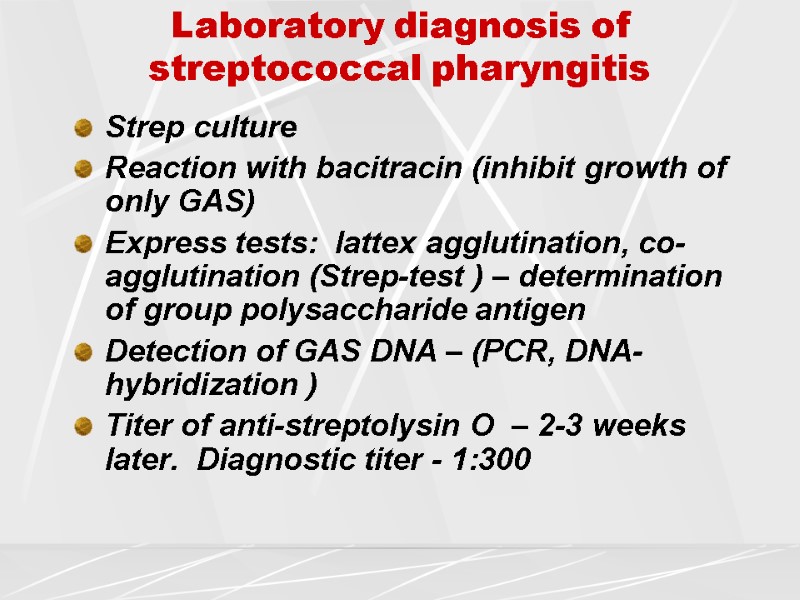
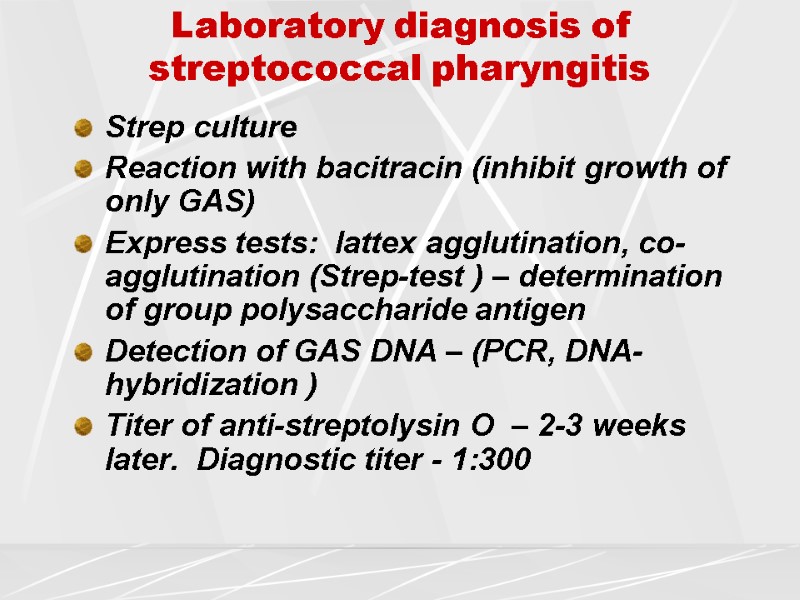 Laboratory diagnosis of streptococcal pharyngitis Strep culture Reaction with bacitracin (inhibit growth of only GAS) Express tests: lattex agglutination, co-agglutination (Strep-test ) – determination of group polysaccharide antigen Detection of GAS DNA – (PCR, DNA-hybridization ) Titer of anti-streptolysin O – 2-3 weeks later. Diagnostic titer - 1:300
Laboratory diagnosis of streptococcal pharyngitis Strep culture Reaction with bacitracin (inhibit growth of only GAS) Express tests: lattex agglutination, co-agglutination (Strep-test ) – determination of group polysaccharide antigen Detection of GAS DNA – (PCR, DNA-hybridization ) Titer of anti-streptolysin O – 2-3 weeks later. Diagnostic titer - 1:300
 GAS is the only widely spread etiology of pharyngitis which requires antibiotic therapy
GAS is the only widely spread etiology of pharyngitis which requires antibiotic therapy
 Antibiotics at streptococcal pharyngitis Penicillins (oral, parnetheral) Cephalosporins of 1-2 generation Macrolides
Antibiotics at streptococcal pharyngitis Penicillins (oral, parnetheral) Cephalosporins of 1-2 generation Macrolides
 EВV infection Infectious mononucleosis
EВV infection Infectious mononucleosis
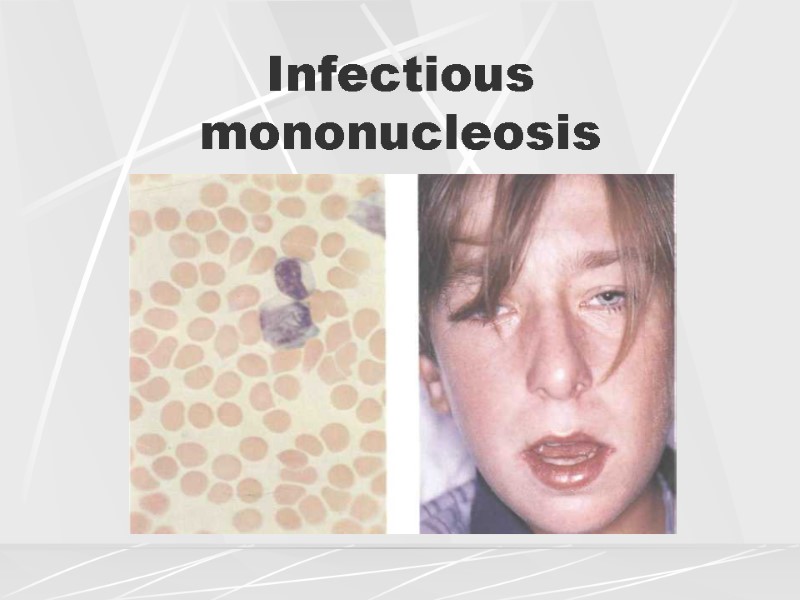
 Infectious mononucleosis is caused by Epstain-Barr virus and is characterized by: Intoxication Acute tonsillitis Generalized polylymphadenopathy, Hepatosplenomegaly
Infectious mononucleosis is caused by Epstain-Barr virus and is characterized by: Intoxication Acute tonsillitis Generalized polylymphadenopathy, Hepatosplenomegaly
 Diseases with mononucleosis-like syndrome ЕВV infection – 90% (infectious mononucleosis) СМV infection (cytomegaloviral mononucleosis) HIV infection Rubella Toxoplasmosis Viral hepatitis
Diseases with mononucleosis-like syndrome ЕВV infection – 90% (infectious mononucleosis) СМV infection (cytomegaloviral mononucleosis) HIV infection Rubella Toxoplasmosis Viral hepatitis
 Etiology of EBV Family Herpesviridae – IV type DNA-containing Target cells - В- and Т- lymphocytes Life-long persistense in B-cells Oncogenic (Berkitt’s lymphoma, nasopharyngeal carcinoma, CNS lymphoma at HIV infection)
Etiology of EBV Family Herpesviridae – IV type DNA-containing Target cells - В- and Т- lymphocytes Life-long persistense in B-cells Oncogenic (Berkitt’s lymphoma, nasopharyngeal carcinoma, CNS lymphoma at HIV infection)
 Epidemiology of EBV infection Way of transmission: contact (saliva), sexual, hemotransfusions Children under 5 years – 80 % In 50 % asymptomatic After infection the person excretes the virus during 6 months; after – periodically through the life
Epidemiology of EBV infection Way of transmission: contact (saliva), sexual, hemotransfusions Children under 5 years – 80 % In 50 % asymptomatic After infection the person excretes the virus during 6 months; after – periodically through the life
 Pathogenesis of EBV infection Penetration and viral replication in pharyngeal mucosa Viremia Infection of peripheral B-lymphocytes Uncontrolled prolipheration of B-cells (CBC – absolute lymphocytosis and ESR) Responsive production of T-cells supressors (СД8+) for inhibition of B-cell proliferation (CBC – atypical mononuclears) Depression of cellular immunity
Pathogenesis of EBV infection Penetration and viral replication in pharyngeal mucosa Viremia Infection of peripheral B-lymphocytes Uncontrolled prolipheration of B-cells (CBC – absolute lymphocytosis and ESR) Responsive production of T-cells supressors (СД8+) for inhibition of B-cell proliferation (CBC – atypical mononuclears) Depression of cellular immunity
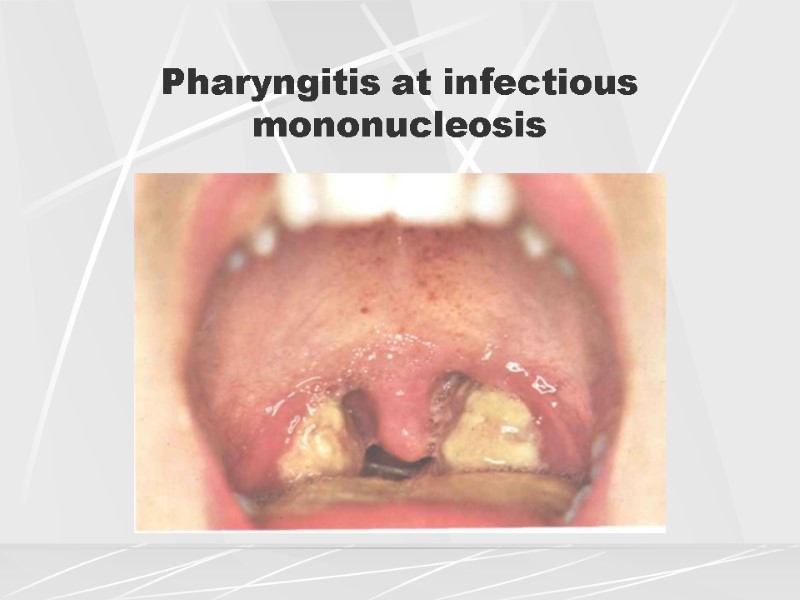
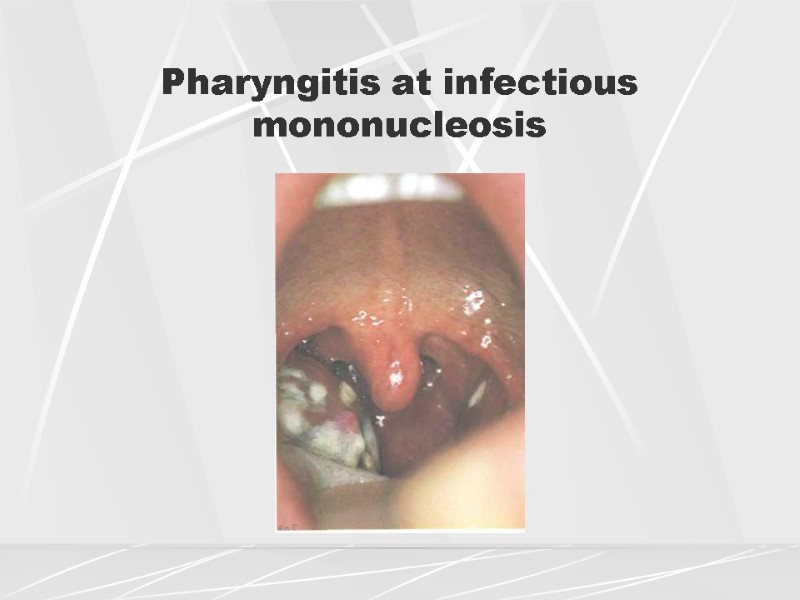
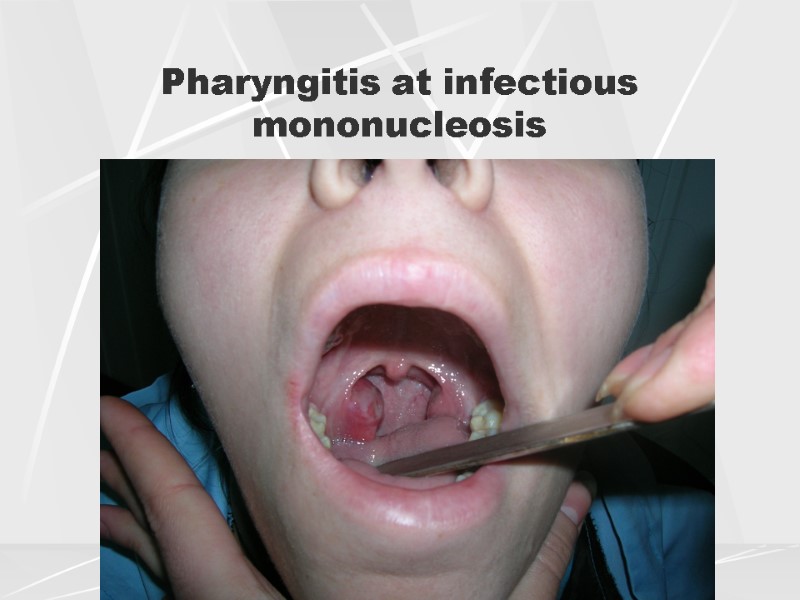
 Clinics of EBV infection Fever Lymphadenopathy Exudative pharyngitis (prominent) Adenoiditis, nasal obstruction Hepatomegaly Possible exanthema
Clinics of EBV infection Fever Lymphadenopathy Exudative pharyngitis (prominent) Adenoiditis, nasal obstruction Hepatomegaly Possible exanthema
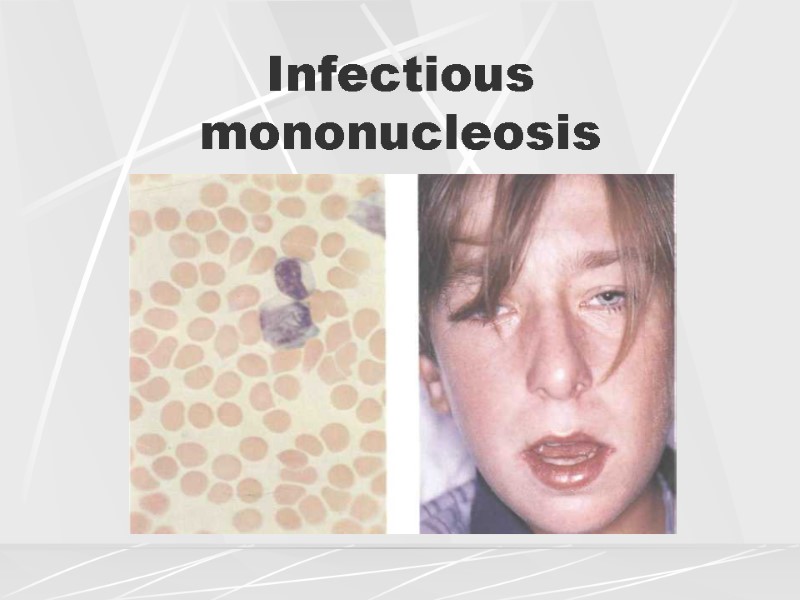 Infectious mononucleosis
Infectious mononucleosis
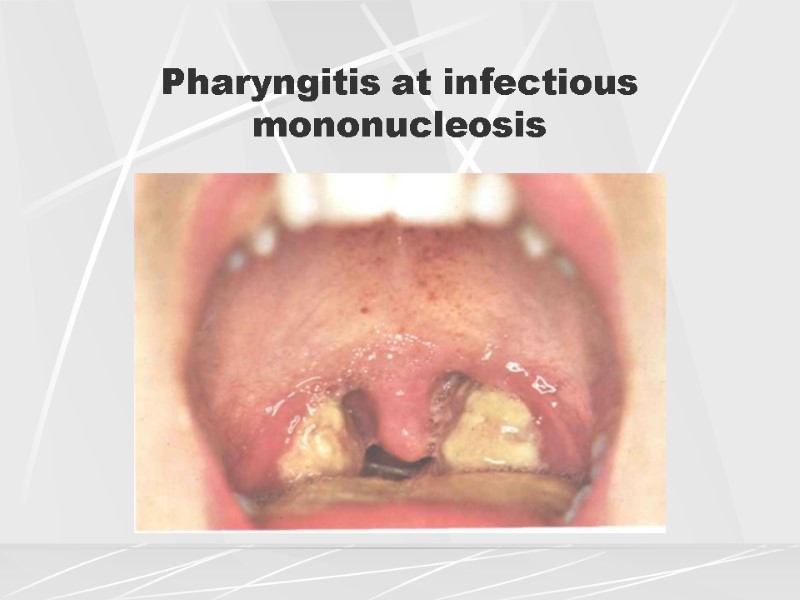 Pharyngitis at infectious mononucleosis
Pharyngitis at infectious mononucleosis
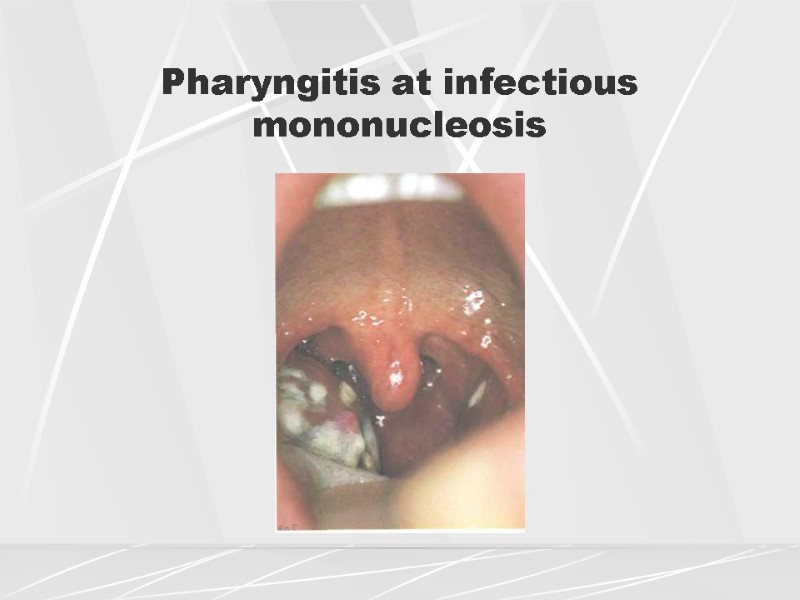 Pharyngitis at infectious mononucleosis
Pharyngitis at infectious mononucleosis
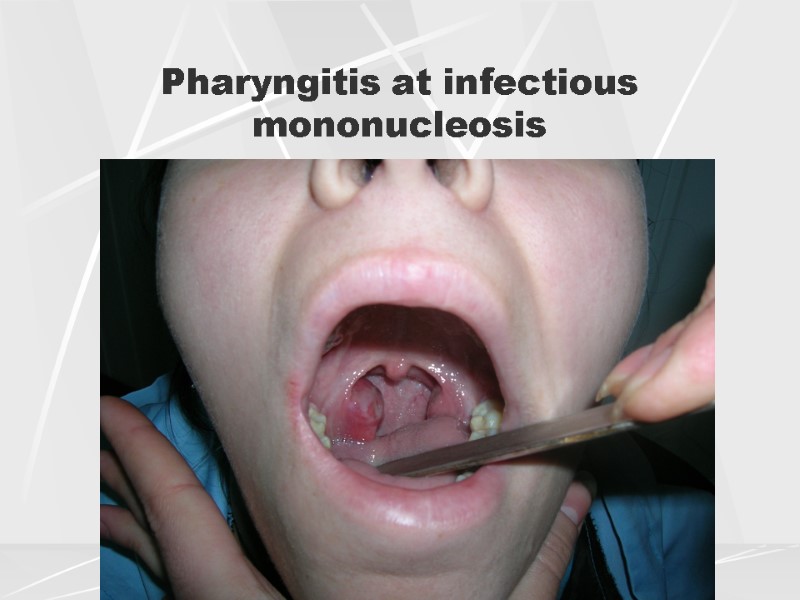 Pharyngitis at infectious mononucleosis
Pharyngitis at infectious mononucleosis
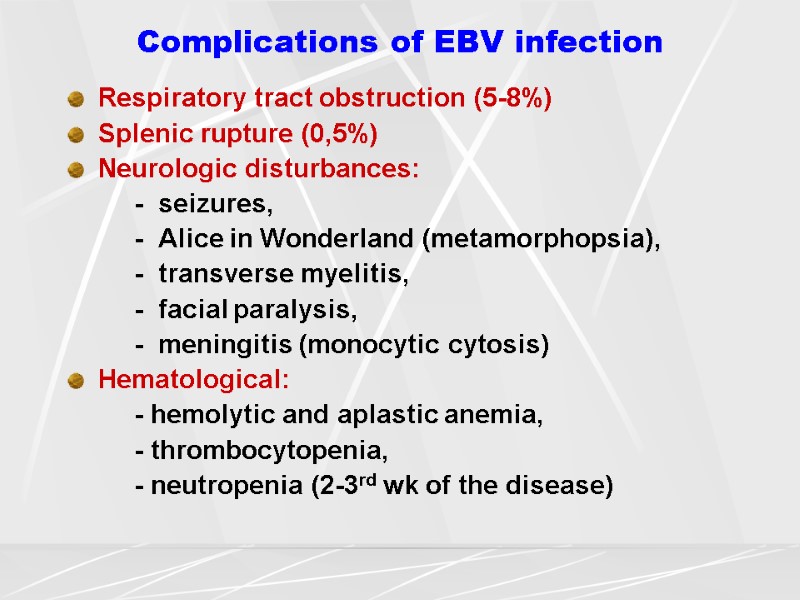
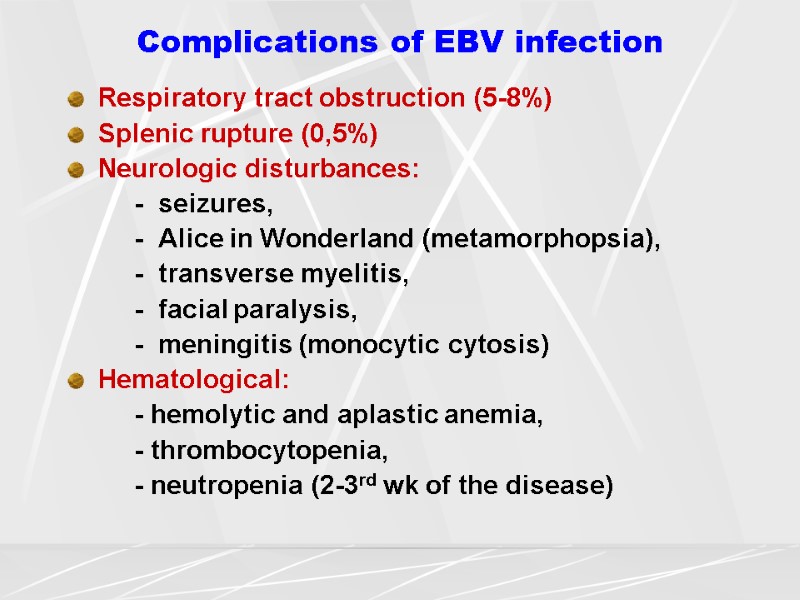 Complications of EBV infection Respiratory tract obstruction (5-8%) Splenic rupture (0,5%) Neurologic disturbances: - seizures, - Alice in Wonderland (metamorphopsia), - transverse myelitis, - facial paralysis, - meningitis (monocytic cytosis) Hematological: - hemolytic and aplastic anemia, - thrombocytopenia, - neutropenia (2-3rd wk of the disease)
Complications of EBV infection Respiratory tract obstruction (5-8%) Splenic rupture (0,5%) Neurologic disturbances: - seizures, - Alice in Wonderland (metamorphopsia), - transverse myelitis, - facial paralysis, - meningitis (monocytic cytosis) Hematological: - hemolytic and aplastic anemia, - thrombocytopenia, - neutropenia (2-3rd wk of the disease)
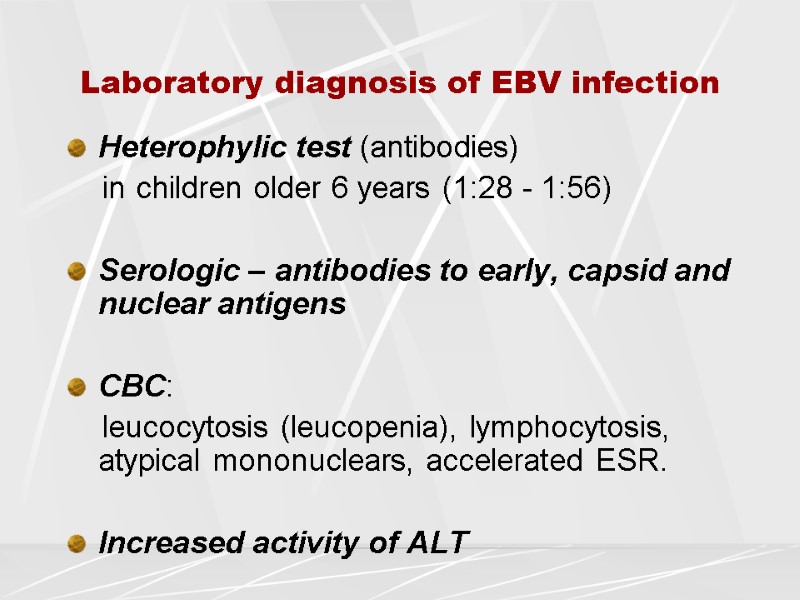
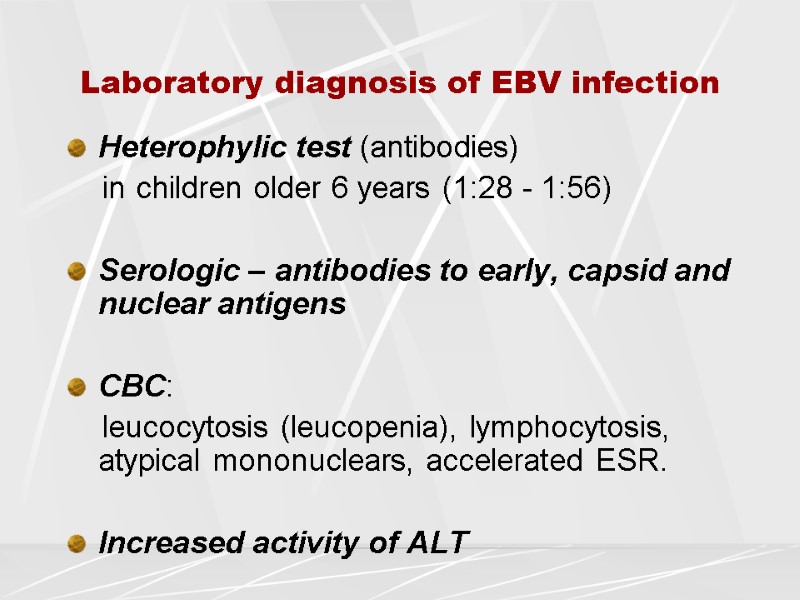 Laboratory diagnosis of EBV infection Heterophylic test (antibodies) in children older 6 years (1:28 - 1:56) Serologic – antibodies to early, capsid and nuclear antigens CBC: leucocytosis (leucopenia), lymphocytosis, atypical mononuclears, accelerated ESR. Increased activity of ALT
Laboratory diagnosis of EBV infection Heterophylic test (antibodies) in children older 6 years (1:28 - 1:56) Serologic – antibodies to early, capsid and nuclear antigens CBC: leucocytosis (leucopenia), lymphocytosis, atypical mononuclears, accelerated ESR. Increased activity of ALT
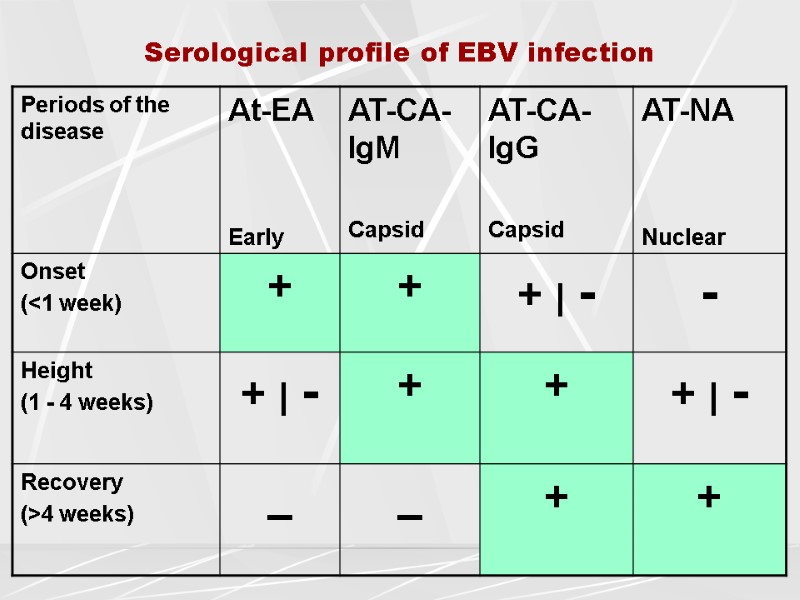
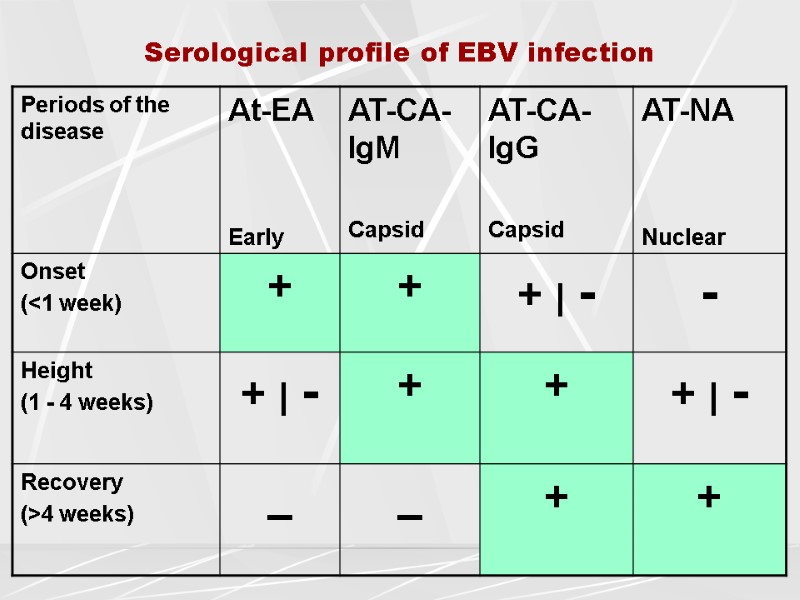 Serological profile of EBV infection
Serological profile of EBV infection
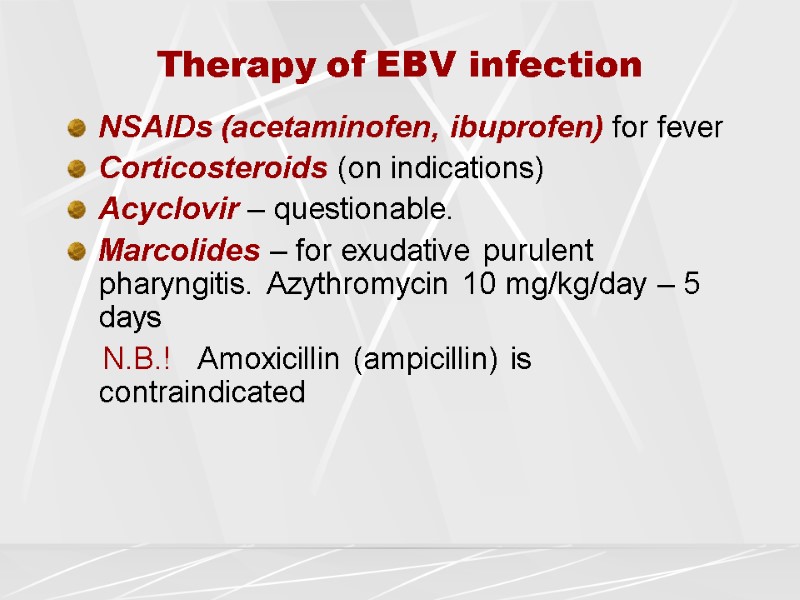
 Therapy of EBV infection NSAIDs (acetaminofen, ibuprofen) for fever Corticosteroids (on indications) Acyclovir – questionable. Marcolides – for exudative purulent pharyngitis. Azythromycin 10 mg/kg/day – 5 days N.B.! Amoxicillin (ampicillin) is contraindicated
Therapy of EBV infection NSAIDs (acetaminofen, ibuprofen) for fever Corticosteroids (on indications) Acyclovir – questionable. Marcolides – for exudative purulent pharyngitis. Azythromycin 10 mg/kg/day – 5 days N.B.! Amoxicillin (ampicillin) is contraindicated
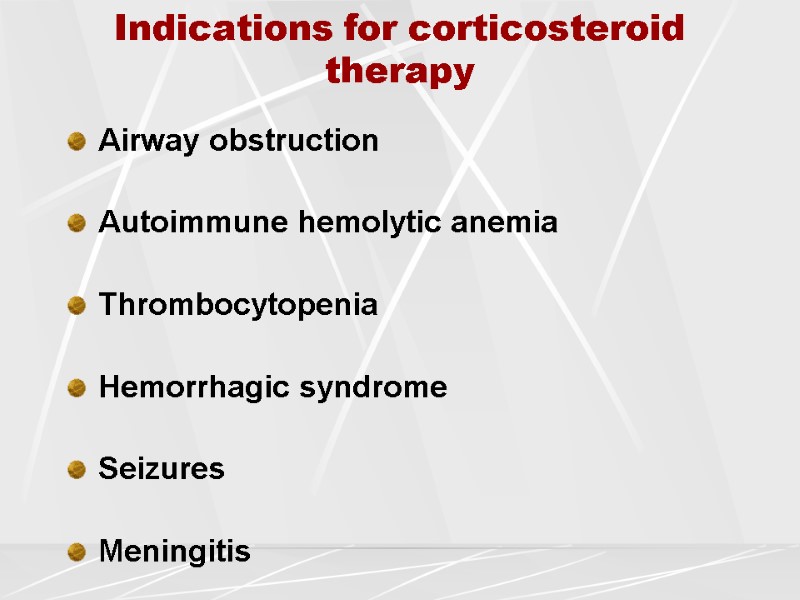
 Indications for corticosteroid therapy Airway obstruction Autoimmune hemolytic anemia Thrombocytopenia Hemorrhagic syndrome Seizures Meningitis
Indications for corticosteroid therapy Airway obstruction Autoimmune hemolytic anemia Thrombocytopenia Hemorrhagic syndrome Seizures Meningitis
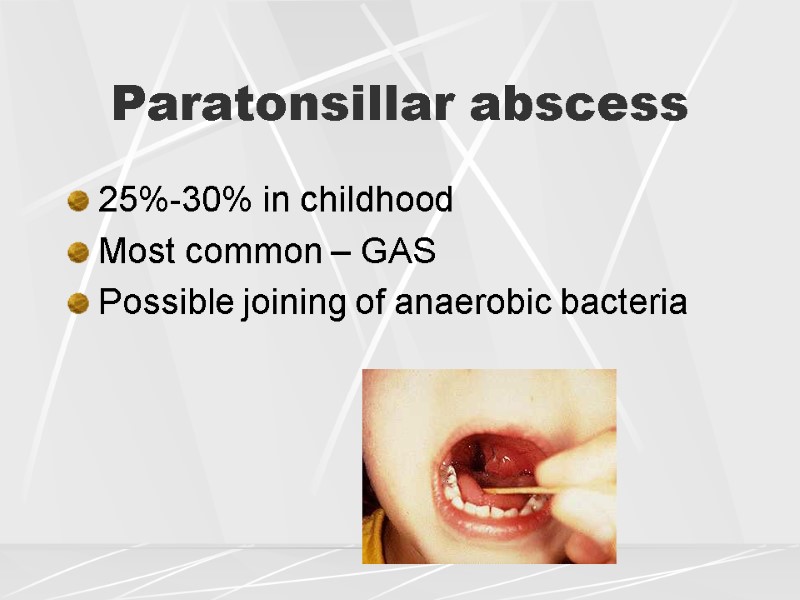 25%-30% in childhood Most common – GAS Possible joining of anaerobic bacteria Paratonsillar abscess
25%-30% in childhood Most common – GAS Possible joining of anaerobic bacteria Paratonsillar abscess
 Symptoms Throat pain / dysphagia 5-7 days No effect from antibiotics Trismus Pain at mouth opening Fever Muffled voice Pain irradiation into ear
Symptoms Throat pain / dysphagia 5-7 days No effect from antibiotics Trismus Pain at mouth opening Fever Muffled voice Pain irradiation into ear
 Oropharyngeal signs Assymetrical edema of soft tissue around tonsils with tonsillar dislocation Fluctuation by palpation Tonsils can be normal, or hyperemic, or covered with axudate Uvula is dislocated to healthy side Soft palate is hyperemic and edemstous Bilateral tonsillar involvement in 3% Malodor from mouth Cervical lymphadenopathy
Oropharyngeal signs Assymetrical edema of soft tissue around tonsils with tonsillar dislocation Fluctuation by palpation Tonsils can be normal, or hyperemic, or covered with axudate Uvula is dislocated to healthy side Soft palate is hyperemic and edemstous Bilateral tonsillar involvement in 3% Malodor from mouth Cervical lymphadenopathy
 Treatment Penicillin G benzathine : Adults - 600 mg (~1 million U) IV q6h Children -12,500-25,000 U/kg IV q6h + Metronidazole (Flagyl) 15 mg/kg or 1 g per 70-kg adults IV during 1 hour supportive dosage: 6 h infusion 7.5 mg/kg or 500 mg per 70-kg adults during 1 hour every 6-8h; not more than 4 g/d Clindamycin – infants and children : 15-25 mg/kg/d PO every 8h; 25-40 mg/kg/d IV/IM every 8h Erythromycin
Treatment Penicillin G benzathine : Adults - 600 mg (~1 million U) IV q6h Children -12,500-25,000 U/kg IV q6h + Metronidazole (Flagyl) 15 mg/kg or 1 g per 70-kg adults IV during 1 hour supportive dosage: 6 h infusion 7.5 mg/kg or 500 mg per 70-kg adults during 1 hour every 6-8h; not more than 4 g/d Clindamycin – infants and children : 15-25 mg/kg/d PO every 8h; 25-40 mg/kg/d IV/IM every 8h Erythromycin
 Diphtheria Acute anthroponous disease, caused by Gram(+) toxigenic bacillus Corynebacterium diphtheria, characterized by local fibrinous-inflammation of the mucus and/or skin, general intoxication and toxic complications: myocarditis, polyneuritis, nephrosis
Diphtheria Acute anthroponous disease, caused by Gram(+) toxigenic bacillus Corynebacterium diphtheria, characterized by local fibrinous-inflammation of the mucus and/or skin, general intoxication and toxic complications: myocarditis, polyneuritis, nephrosis
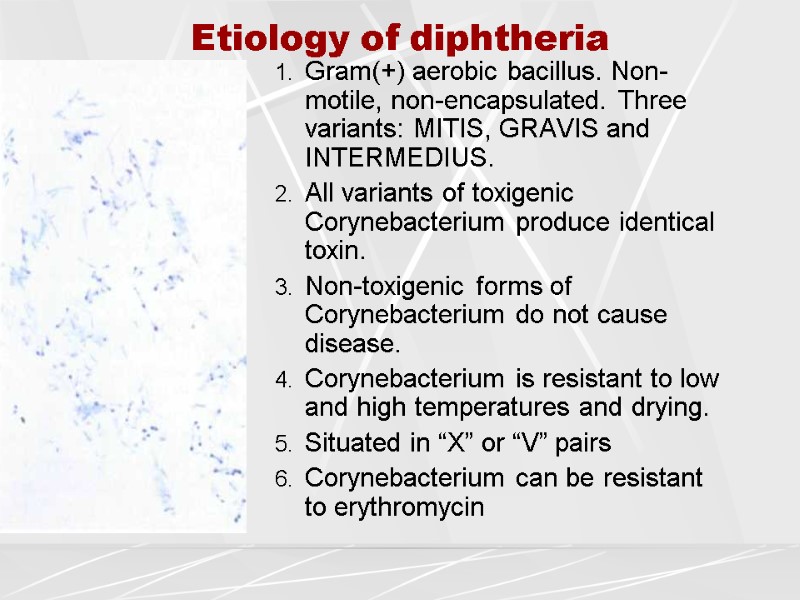
 Etiology of diphtheria Gram(+) aerobic bacillus. Non-motile, non-encapsulated. Three variants: MITIS, GRAVIS and INTERMEDIUS. All variants of toxigenic Corynebacterium produce identical toxin. Non-toxigenic forms of Corynebacterium do not cause disease. Corynebacterium is resistant to low and high temperatures and drying. Situated in “X” or “V” pairs Corynebacterium can be resistant to erythromycin
Etiology of diphtheria Gram(+) aerobic bacillus. Non-motile, non-encapsulated. Three variants: MITIS, GRAVIS and INTERMEDIUS. All variants of toxigenic Corynebacterium produce identical toxin. Non-toxigenic forms of Corynebacterium do not cause disease. Corynebacterium is resistant to low and high temperatures and drying. Situated in “X” or “V” pairs Corynebacterium can be resistant to erythromycin
 Epidemiology of diphtheria Season – cold Source – sicka and carriers Transmission – airborne 70% population vaccination prevents epidemics
Epidemiology of diphtheria Season – cold Source – sicka and carriers Transmission – airborne 70% population vaccination prevents epidemics
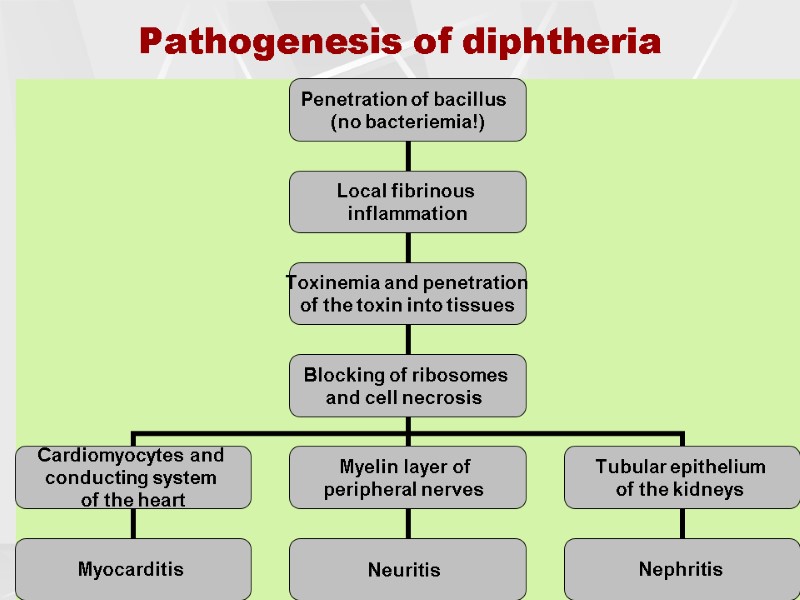
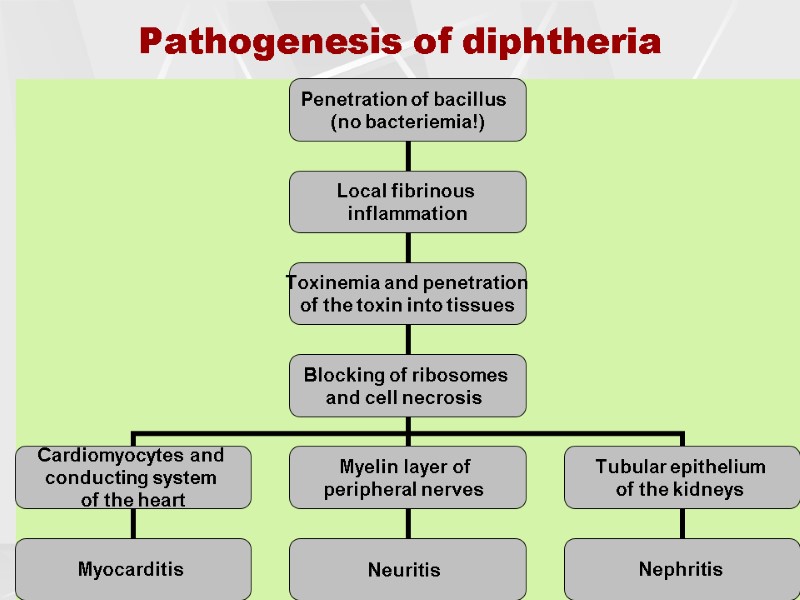 Pathogenesis of diphtheria
Pathogenesis of diphtheria
 Classification of diphtheria Diphtheria of tonsils Diphtheria of nose Diphtheria of larynx (croup, laryngitis) Diphtheria of eye Diphtheria of skin
Classification of diphtheria Diphtheria of tonsils Diphtheria of nose Diphtheria of larynx (croup, laryngitis) Diphtheria of eye Diphtheria of skin
 Clinics of diphtheria Incubational period = 2-10 days Acute disease onset Intoxication: moderate fever, headache, weakness Fibrinous pharyngitis Anterior cervical lymphadenitis Subcutaneous cervical tissue edema (+/-)
Clinics of diphtheria Incubational period = 2-10 days Acute disease onset Intoxication: moderate fever, headache, weakness Fibrinous pharyngitis Anterior cervical lymphadenitis Subcutaneous cervical tissue edema (+/-)
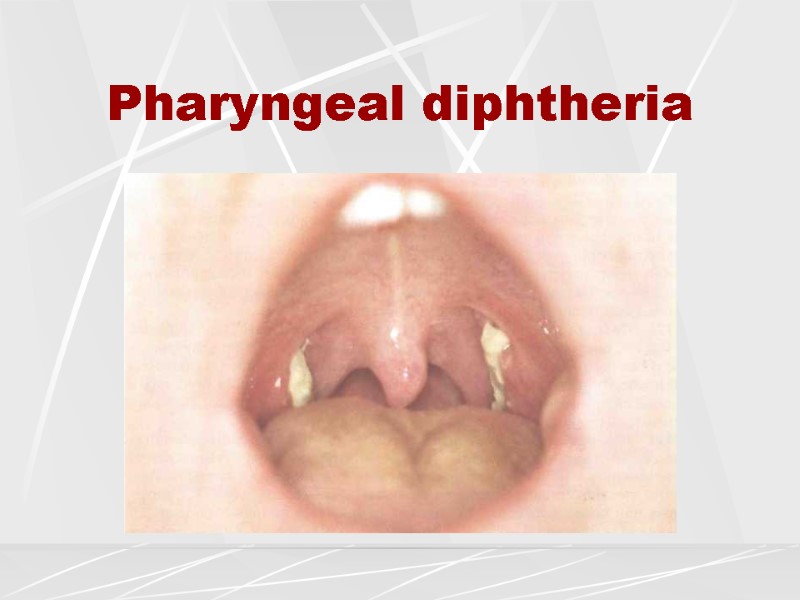
 Membranous pharyngitis Cyanotic hyperemia of pharynx Tonsillar edema Thick whitish-grayish covers, removed with bleeding of mucosa Are formed by 3rd day of diphtheria
Membranous pharyngitis Cyanotic hyperemia of pharynx Tonsillar edema Thick whitish-grayish covers, removed with bleeding of mucosa Are formed by 3rd day of diphtheria
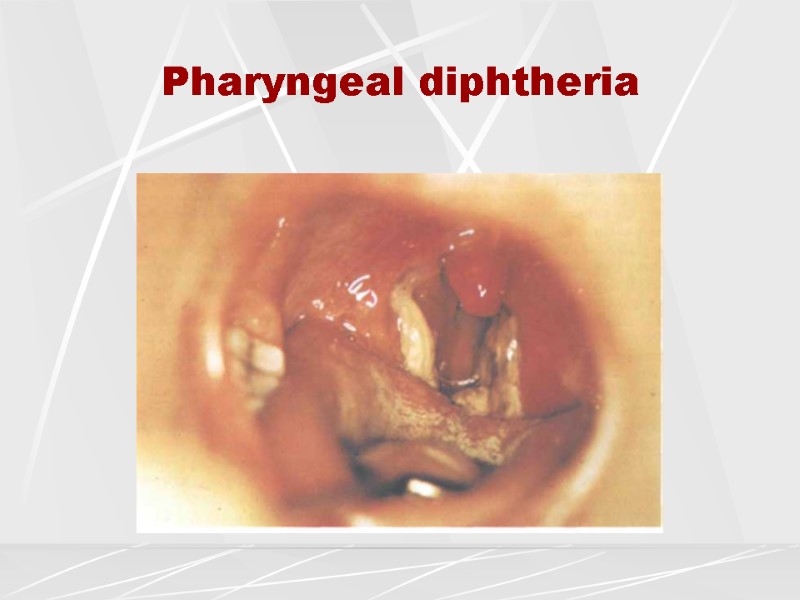
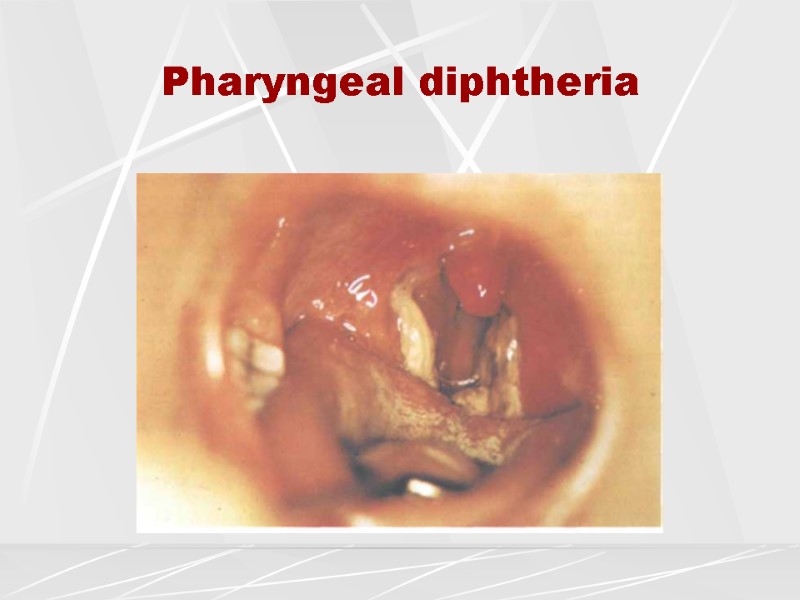 Pharyngeal diphtheria
Pharyngeal diphtheria
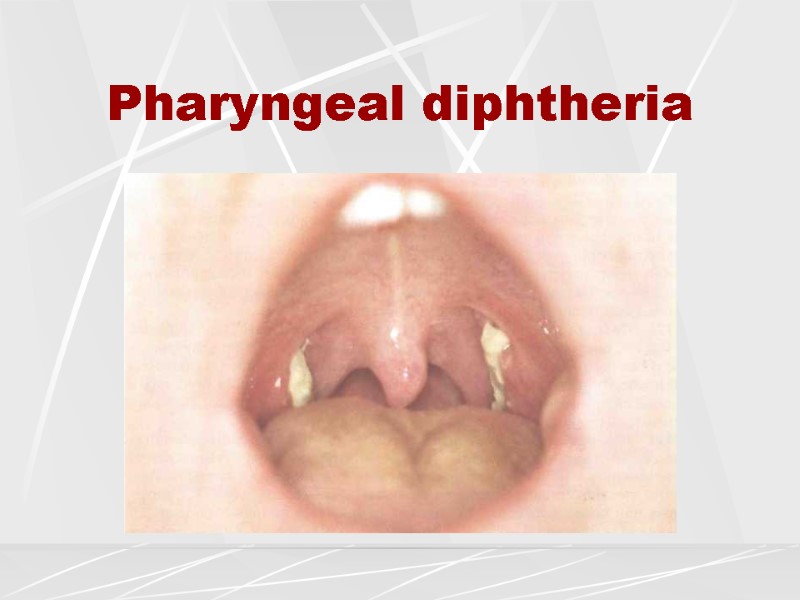 Pharyngeal diphtheria
Pharyngeal diphtheria
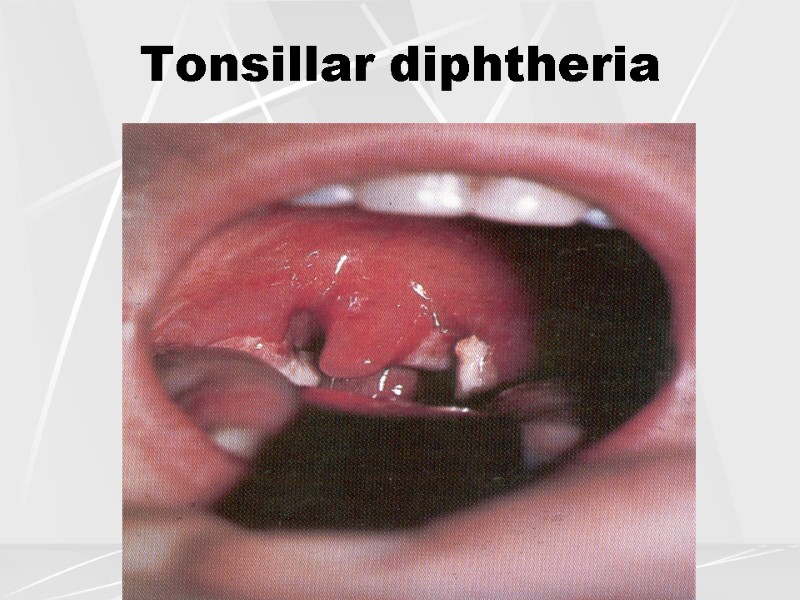
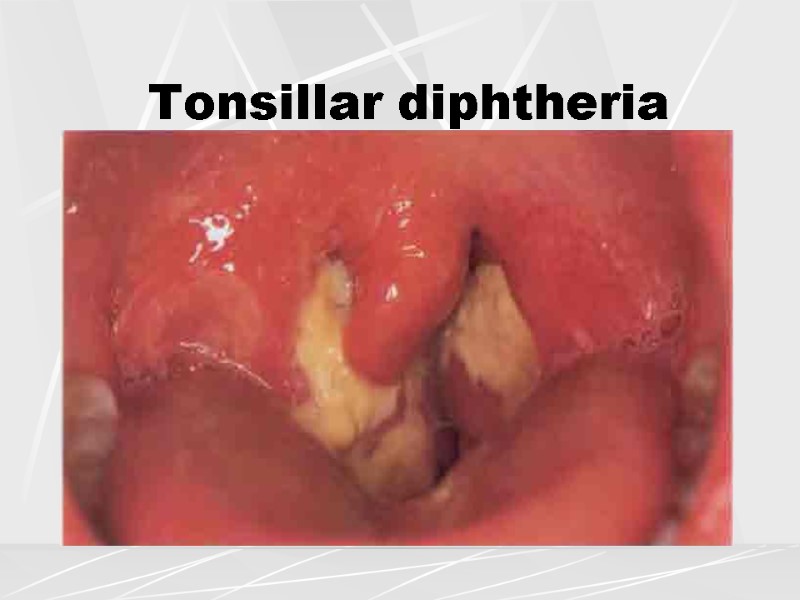
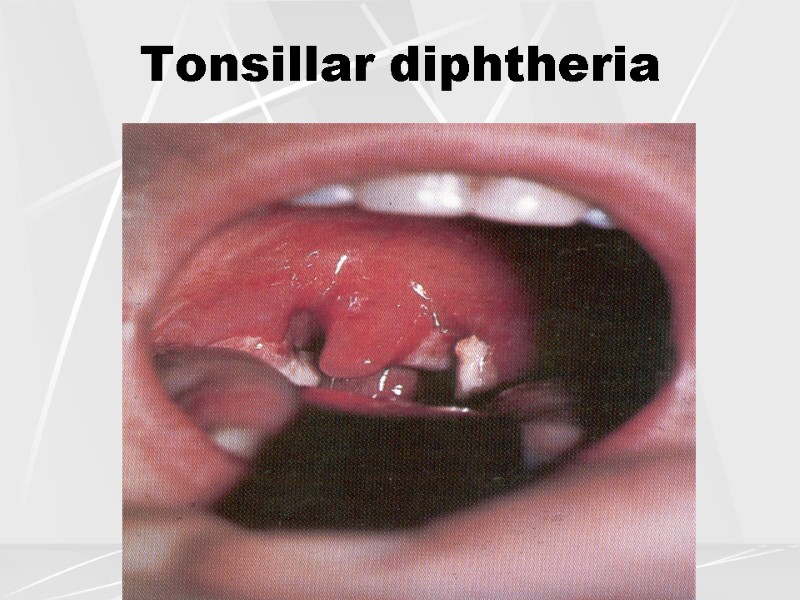 Tonsillar diphtheria
Tonsillar diphtheria
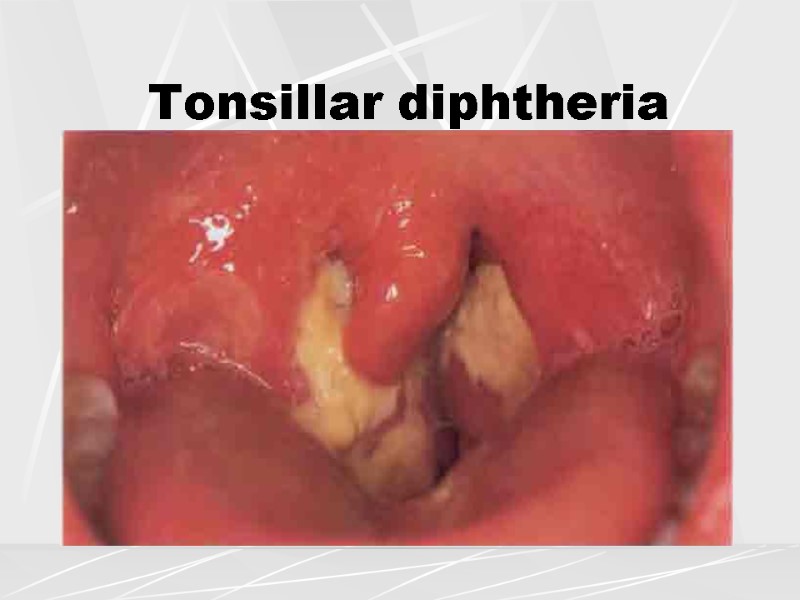 Tonsillar diphtheria
Tonsillar diphtheria
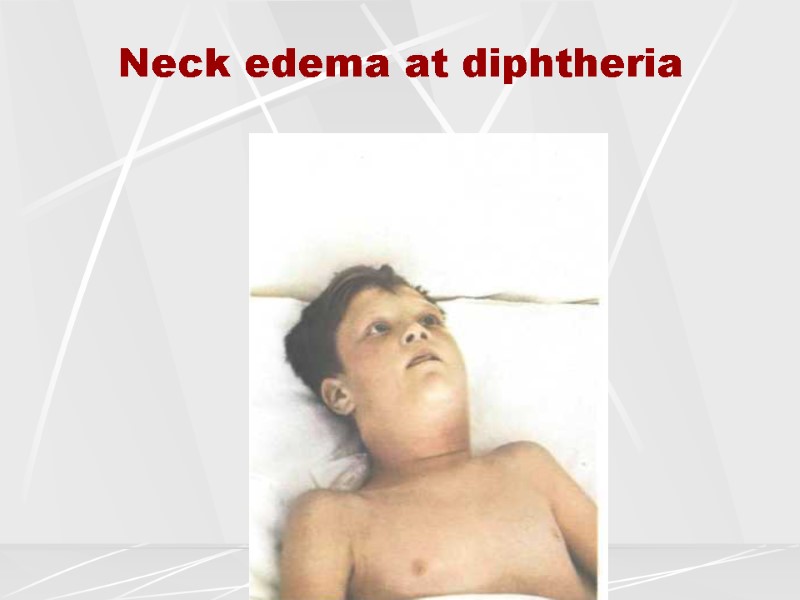
 Symptoms of severe diphtheria Toxic neck edema Hemorrhagic syndrome Shock (tachycardia, hypotension, oliguria)
Symptoms of severe diphtheria Toxic neck edema Hemorrhagic syndrome Shock (tachycardia, hypotension, oliguria)
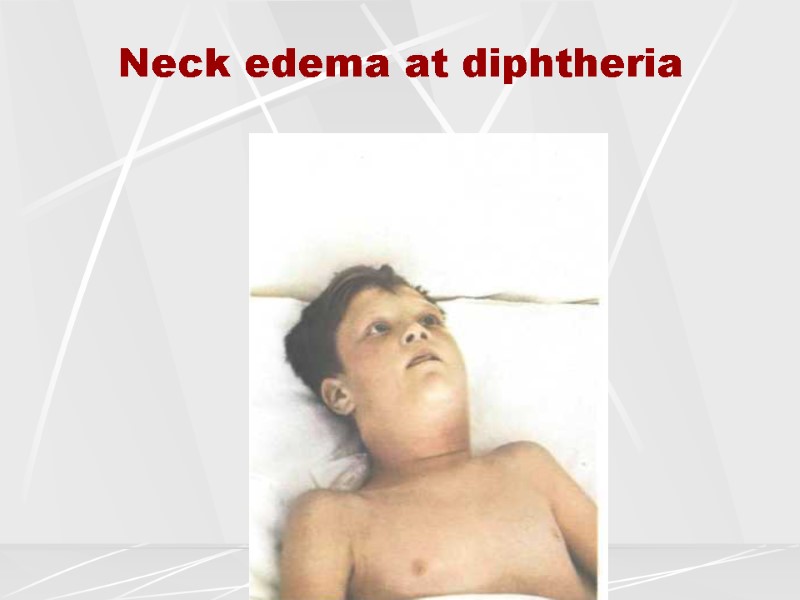 Neck edema at diphtheria
Neck edema at diphtheria
 Complications of diphtheria Myocarditis Neuropathies Nephritis
Complications of diphtheria Myocarditis Neuropathies Nephritis
 Diagnosis of diphtheria Culture of С.diphtheriae with detection of toxigenicity Detection of antibodies in reaction of neutralization (protective level is 0,5 U\ml) Detection of antibodies in reaction of direct hemagglutination (protective level is 1:320) Detection of phage (PCR) Detection of toxin in blood serum CBC: leucocytosis, neutrophilosis, accelerated ESR At neuropathies – elevation of protein in CSF
Diagnosis of diphtheria Culture of С.diphtheriae with detection of toxigenicity Detection of antibodies in reaction of neutralization (protective level is 0,5 U\ml) Detection of antibodies in reaction of direct hemagglutination (protective level is 1:320) Detection of phage (PCR) Detection of toxin in blood serum CBC: leucocytosis, neutrophilosis, accelerated ESR At neuropathies – elevation of protein in CSF
 Therapy of diphtheria Antitoxin (serum): Minimal dosage: 20 - 40 thousand U Maximal dosage: 150 thousand U Route of injection: IM, IV Antibiotics (erythromycin, penicillin - 14 days)
Therapy of diphtheria Antitoxin (serum): Minimal dosage: 20 - 40 thousand U Maximal dosage: 150 thousand U Route of injection: IM, IV Antibiotics (erythromycin, penicillin - 14 days)
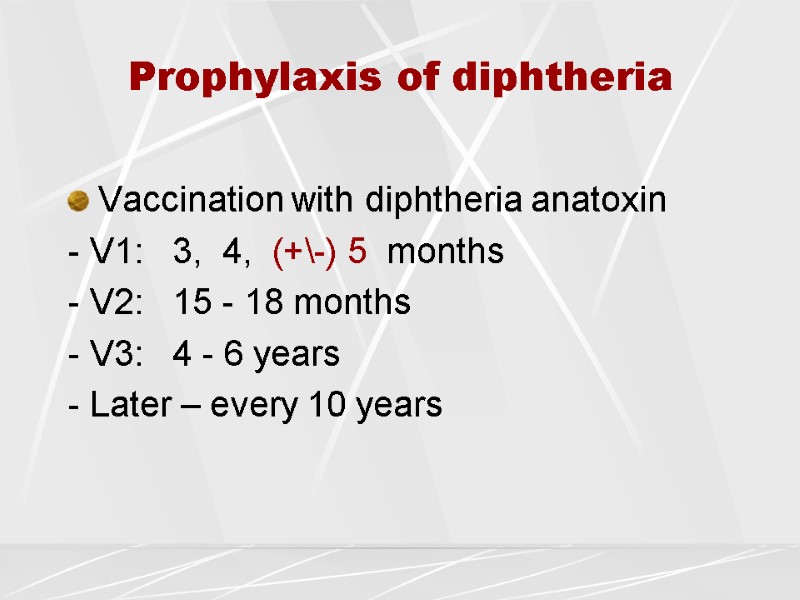
 Prophylaxis of diphtheria Vaccination with diphtheria anatoxin - V1: 3, 4, (+\-) 5 months - V2: 15 - 18 months - V3: 4 - 6 years - Later – every 10 years
Prophylaxis of diphtheria Vaccination with diphtheria anatoxin - V1: 3, 4, (+\-) 5 months - V2: 15 - 18 months - V3: 4 - 6 years - Later – every 10 years
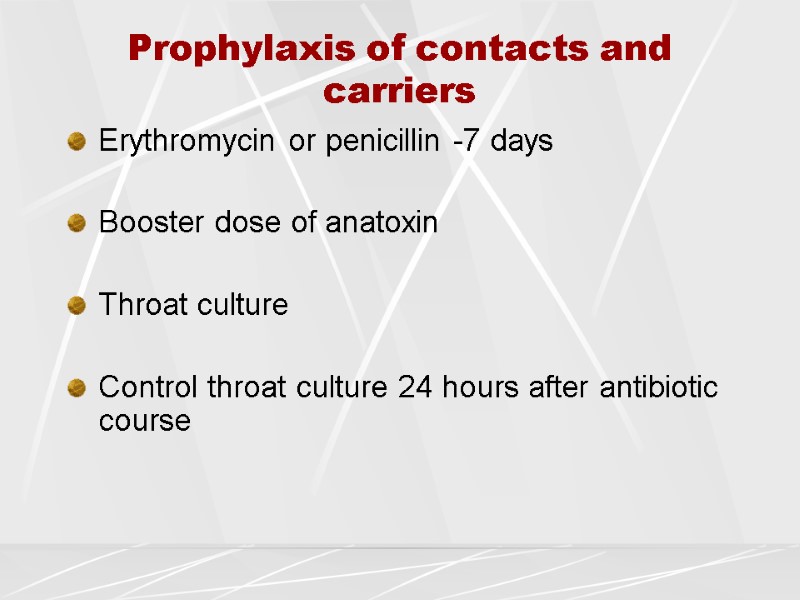
 Prophylaxis of contacts and carriers Erythromycin or penicillin -7 days Booster dose of anatoxin Throat culture Control throat culture 24 hours after antibiotic course
Prophylaxis of contacts and carriers Erythromycin or penicillin -7 days Booster dose of anatoxin Throat culture Control throat culture 24 hours after antibiotic course

