04c7410562a964ef66fa93fe25dd1433.ppt
- Количество слайдов: 37
Dialysis • Begun when the patient’s uremia can no longer be adequately managed conservatively • Initiated when the GFR <5 – 10% 0 f normal
Dialysis • The movement of fluid and molecules across a semipermeable membrane from one compartment to another
Dialysis • Two methods of dialysis available ØPeritoneal dialysis (PD) ØHemodialysis (HD)
General Principles of Dialysis • Diffusion • Osmosis • Ultrafiltration
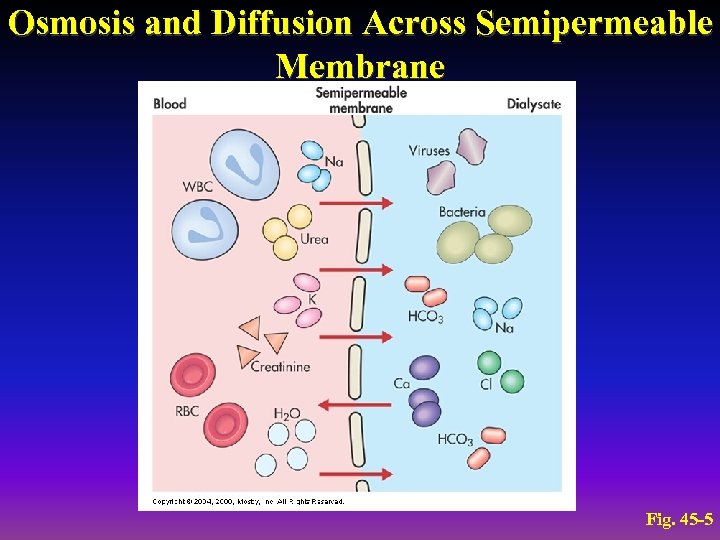
Osmosis and Diffusion Across Semipermeable Membrane Fig. 45 -5
DIALYSATE • Is an electrolyte solution that is similar to that of normal plasma, except contains no potassium • Different concentrations
Peritoneal Dialysis Solutions and Cycles • Available commercially in 1 - or 2 -L plastic bags with glucose concentrations of 1. 5%, 2. 5%, and 4. 25%
Peritoneal Dialysis Catheter Placement • Peritoneal access is obtained by inserting a catheter (Tenckhoff) through the anterior wall • Technique for catheter placement varies • Usually done via surgery
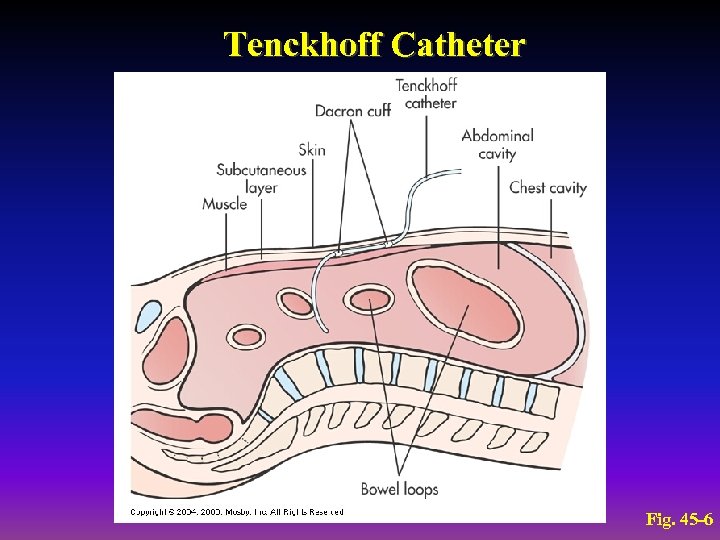
Tenckhoff Catheter Fig. 45 -6
Peritoneal Dialysis Solutions and Cycles • Three phases of the PD cycle ØInflow (fill) ØDwell (equilibration) ØDrain
Peritoneal Dialysis Complications • • • Exit site infection Peritonitis/Infection: cloudy dialysate Hypotension Abdominal pain (may be bowel perforation): brownish dialysate Bladder perforation: amber dialysate Outflow problems Hernias Lower back problems Bleeding Pulmonary complications Protein loss CHO and lipid abnormalities
Peritoneal Dialysis Types • Automated peritoneal dialysis (APD) • Continuous ambulatory peritoneal dialysis (CAPD)
Peritoneal Dialysis Advantages • • • Short training program Independence Ease of traveling Fewer dietary restrictions Greater mobility than with HD
Hemodialysis Vascular Access Sites • Shunts • Internal arteriovenous fistulas and grafts • Temporary vascular access
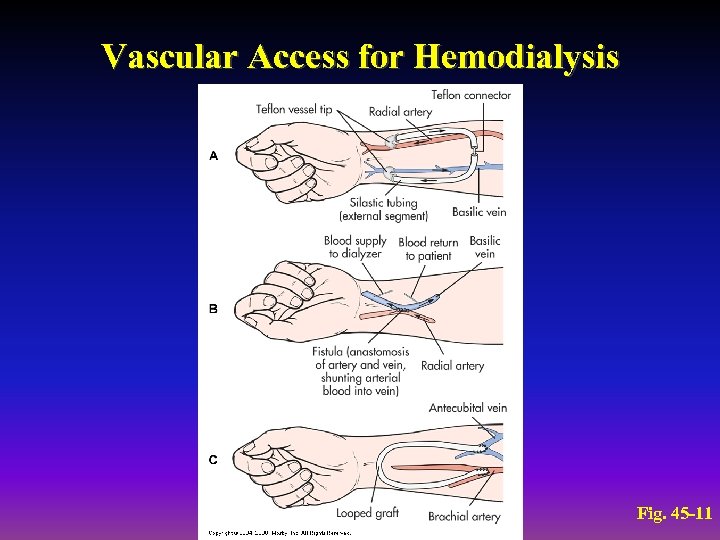
Vascular Access for Hemodialysis Fig. 45 -11
Hemodialysis Dialyzers • Long plastic cartridge that contains thousands of parallel hollow tubes or fibers
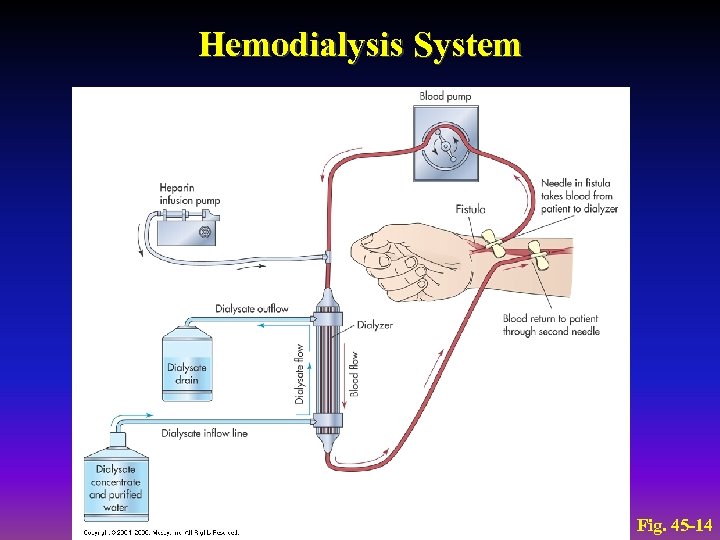
Hemodialysis System Fig. 45 -14
Hemodialysis Complications • • • Hypotension Muscle cramps Loss of blood Hepatitis Sepsis Disequilibrium syndrome
Hemodialysis Effectiveness and Adaptation • Cannot fully replace the metabolic and hormonal functions of the kidneys • Can ease many of the symptoms • Can prevent certain complications
Kidney Transplantation • Over 54, 000 patients currently awaiting cadaveric kidney transplants • Over 5200 living donor transplants done in 2002 • Extremely successful • 1 -year graft survival rate Ø 90% for cadaver transplants Ø 95% for live donor transplants
Kidney Transplantation Advantages of kidney transplant compared with dialysis: ØReverses many of the pathophysiologic changes associated with renal failure ØEliminates the dependence on dialysis ØLess expensive than dialysis after the 1 st year
Kidney Transplantation Recipient Selection • Candidacy determined by a variety of medical and psychosocial factors that vary among transplant centers Contraindications to transplantation: Ø Disseminated malignancies Ø Cardiac disease Ø Chronic respiratory failure Ø Extensive vascular disease Ø Chronic infection Ø Unresolved psychological disorders
Kidney Transplantation Histocompatability Studies • Purpose of testing is to identify the HLA antigens for both donors and potential recipients
Kidney Transplantation Donor Sources • • Compatible blood type cadaver donors Blood relatives Emotionally related living donors Altruistic living donors
Kidney Transplantation Surgical Procedure • Donor nephrectomy performed by a urologist or transplant surgeon • Begins an hour or two before the recipient’s surgery is started
Kidney Transplantation Kidney Transplant Recipient Transplanted kidney Ø Usually placed extraperitoneally in the iliac fossa Ø Right iliac fossa is preferred Before incision: Ø Urinary catheter placed into bladder Ø Antibiotic solution instilled • Distends the bladder • Decreases risk of infection
Kidney Transplantation Nursing Management Preoperative Care • • • Emotional and physical preparation Immunosuppressive drugs ECG Chest x-ray Laboratory studies
Kidney Transplantation Nursing Management Postoperative Care Live donor ØCare is similar to laparoscopic nephrectomy ØClose monitoring of renal function Recipient ØMaintenance of fluid and electrolyte balance is 1 st priority
Kidney Transplantation Immunosuppressive Therapy Goals: Ø Adequately suppress the immune response Ø Maintain sufficient immunity to prevent overwhelming infection Medications: Ø Cyclosporin Ø Predisone Ø Prografin FK 506 (Tacrolimus) Ø Mycophenolate Mofetil (Cell. Cept)
Kidney Transplantation Complications Rejection ØHyperacute (antibody-mediated, humoral) rejection • Occurs minutes to hours after transplantation
Kidney Transplantation Complications Rejection ØAcute rejection • Occurs days to months after transplantation
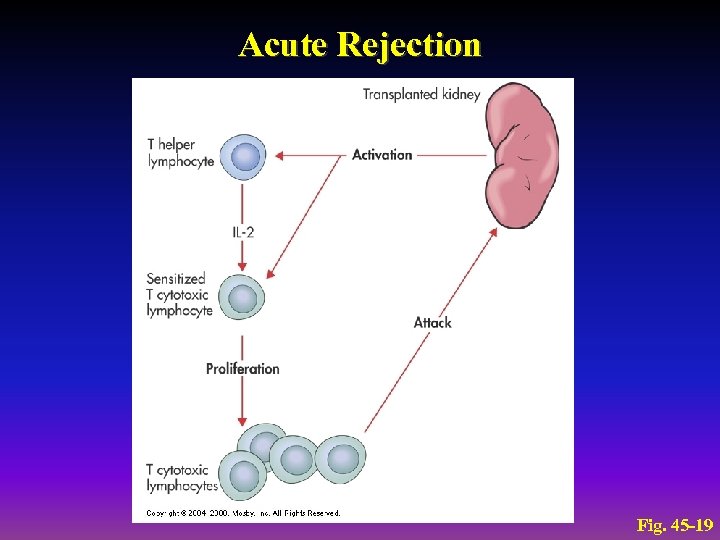
Acute Rejection Fig. 45 -19
Kidney Transplantation Complications Rejection ØChronic rejection • Process that occurs over months or years and is irreversible
Kidney Transplantation Complications Infection Ø Most common infections observed in the 1 st month: • Pneumonia • Wound infections • IV line and drain infections Ø Fungal infections Ø Viral infections • CMV • Epstein-Barr virus • Herpes simplex virus
Kidney Transplantation Complications Cardiovascular disease ØTransplant recipients have incidence of atherosclerotic vascular disease Malignancies ØPrimary cause is immunosuppressive therapy
Kidney Transplantation Complications Recurrence of original renal disease ØGlomerulonephritis ØIg. A nephropathy ØDiabetes mellitus ØFocal segmental sclerosis
Kidney Transplantation Complications Corticosteroid-related complications Ø Aseptic necrosis of the hips, knees, and other joints Ø Peptic ulcer disease Ø Glucose intolerance and diabetes Ø Hyperlipidemia Ø Cataracts Ø Increased incidence of infections and malignancies
04c7410562a964ef66fa93fe25dd1433.ppt