Acute diarrhea.ppt
- Количество слайдов: 39
Diagnosis, treatment and prophylaxis of acute bowel infections in children
Acute bowel infections in children: definition Kośek M. , Bulletin of the World Health Organization, 2003 Acute bowel infections (ABІ) – is a heterogenic group of acute infectious diseases of gastro-intestinal tract with peroral way of contamination, which are caused by enterothropic causative agents (viruses, bacteria, protozoa, fungi) and/or their toxins; the main presentation of which is the acute diarrhea syndrome.
Acute bowel infections in children: importance Kośek M. , Bulletin of the World Health Organization, 2003 üABI posses the leading place in pediatric morbidity worldwide, the second place after respiratory diseases; üIn general, 3, 2 episodes of ABI per year per one child under 5 years in developing countries and 1, 3 episodes in developed countries; üAnnually about 2, 5 millions of children die from ABI in the world (2, 1 -4, 7); üIn developing countries it is the main cause of mortality for children under 5 years. Mean mortality is 4, 9 per 1000.
Etiological structure of ABI in children Viruses: 65% Rotavirus A, B, C, G Enteric adenoviruses 31, 40, 41 Caliciviruses (Norwalkvirus, Snow. Mountainvirus, Sapporovirus) Astrovirus, Pararotavirus, Parvovirus, Enteroviruses (68, 69), CMV
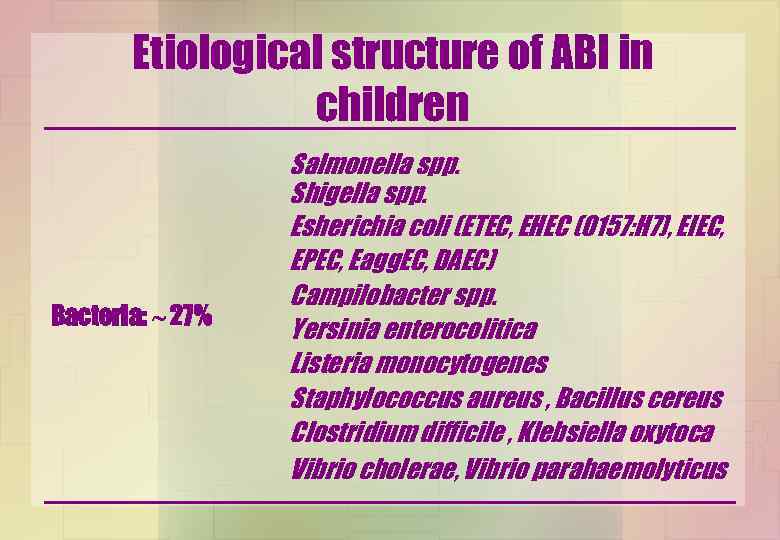
Etiological structure of ABI in children Bacteria: 27% Salmonella spp. Shigella spp. Esherichia coli (ETEC, EHEC (O 157: H 7), EIEC, EPEC, Eagg. EC, DAEC) Campilobacter spp. Yersinia enterocolitica Listeria monocytogenes Staphylococcus aureus , Bacillus cereus Clostridium difficile , Klebsiella oxytoca Vibrio cholerae, Vibrio parahaemolyticus
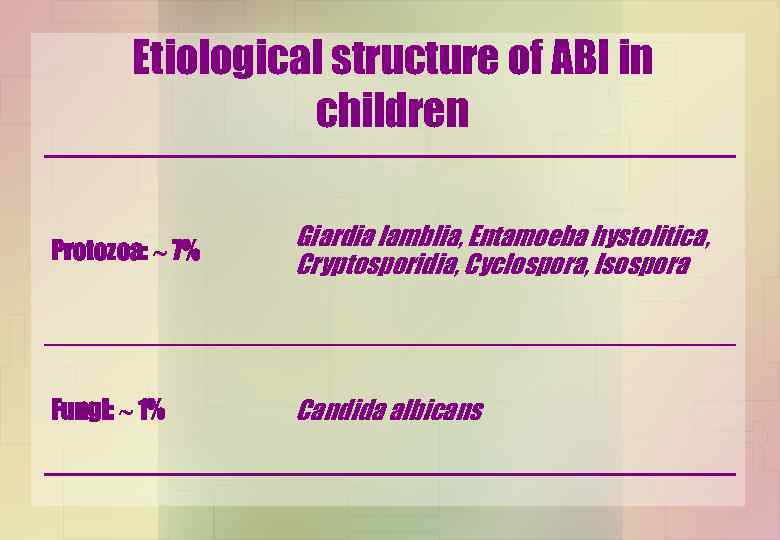
Etiological structure of ABI in children Protozoa: 7% Giardia lamblia, Entamoeba hystolitica, Cryptosporidia, Cyclospora, Isospora Fungi: 1% Candida albicans
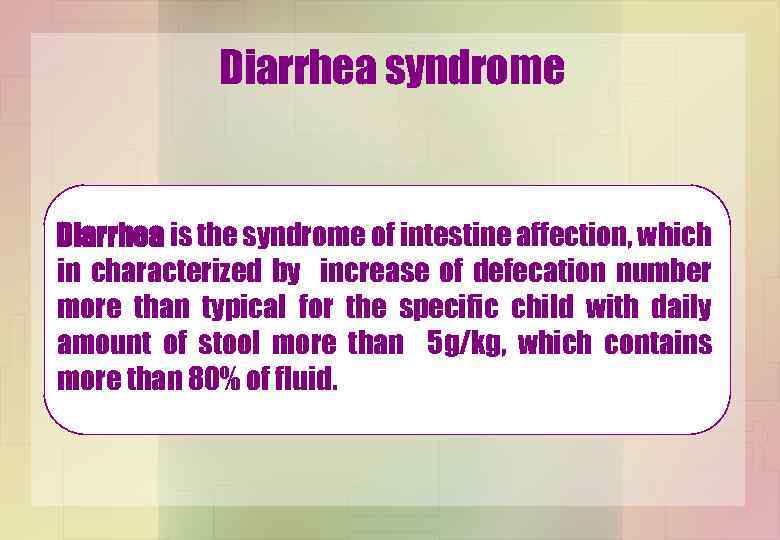
Diarrhea syndrome Diarrhea is the syndrome of intestine affection, which in characterized by increase of defecation number more than typical for the specific child with daily amount of stool more than 5 g/kg, which contains more than 80% of fluid.
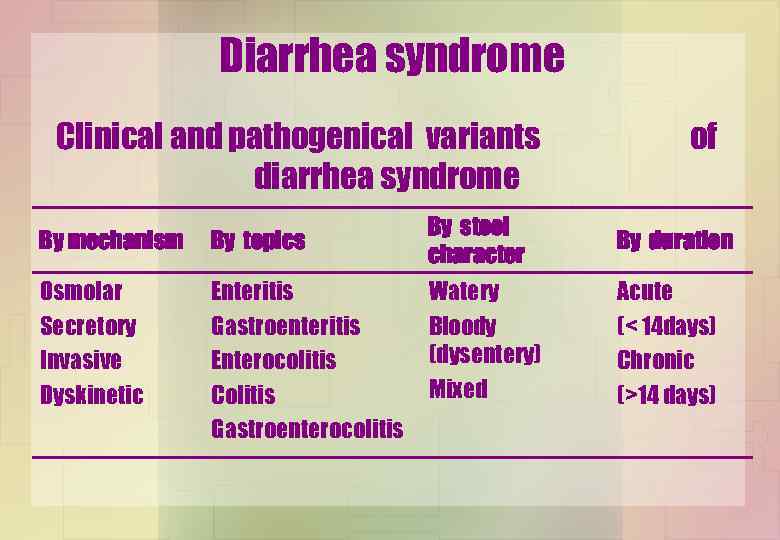
Diarrhea syndrome Clinical and pathogenical variants diarrhea syndrome By mechanism By topics Osmolar Secretory Invasive Dyskinetic Enteritis Gastroenteritis Enterocolitis Colitis Gastroenterocolitis of By stool character By duration Watery Bloody (dysentery) Mixed Acute (< 14 days) Chronic (>14 days)
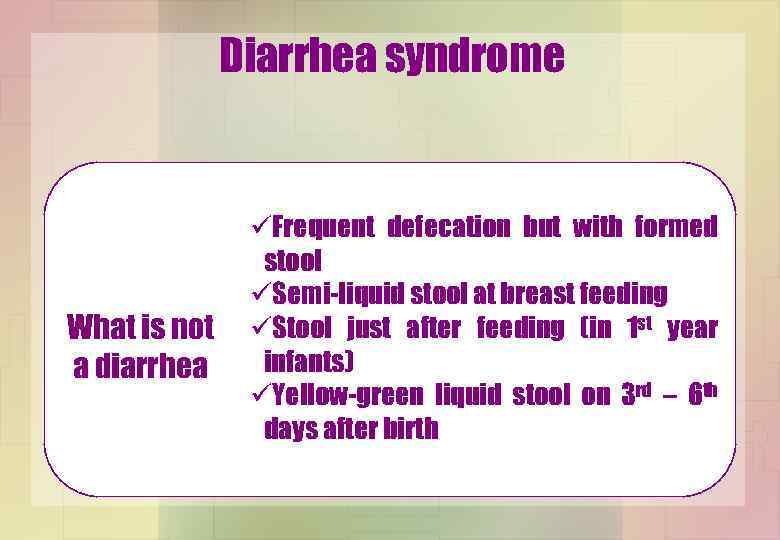
Diarrhea syndrome What is not a diarrhea üFrequent defecation but with formed stool üSemi-liquid stool at breast feeding üStool just after feeding (in 1 st year infants) üYellow-green liquid stool on 3 rd – 6 th days after birth
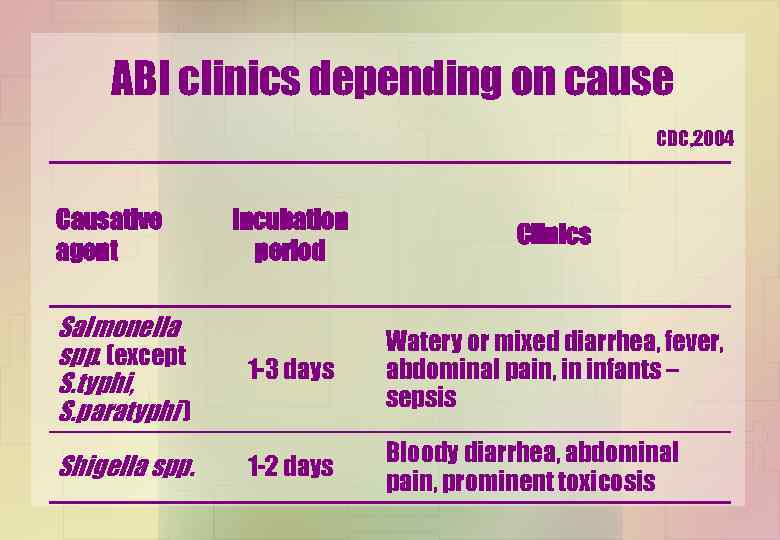
ABI clinics depending on cause CDC, 2004 Causative agent Salmonella spp. (except S. typhi, S. paratyphi ) Shigella spp. Incubation period Clinics 1 -3 days Watery or mixed diarrhea, fever, abdominal pain, in infants – sepsis 1 -2 days Bloody diarrhea, abdominal pain, prominent toxicosis
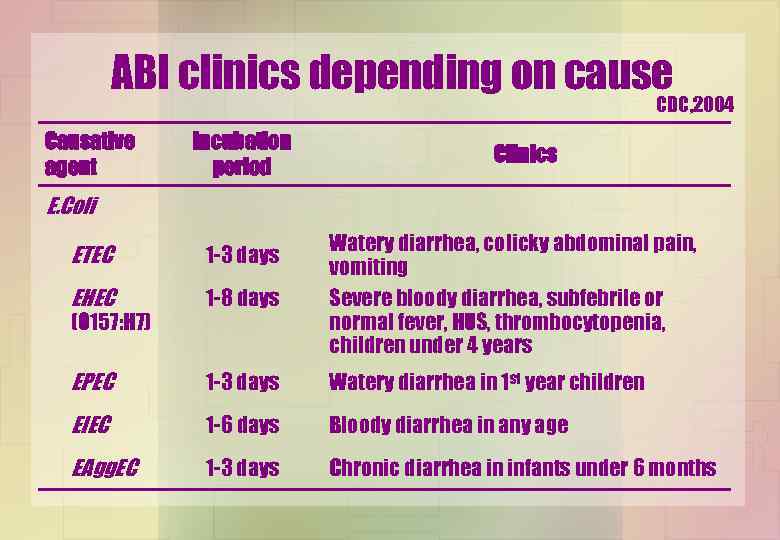
ABI clinics depending on cause CDC, 2004 Causative agent Incubation period Clinics E. Coli ETEC 1 -3 days EHEC 1 -8 days Watery diarrhea, colicky abdominal pain, vomiting Severe bloody diarrhea, subfebrile or normal fever, HUS, thrombocytopenia, children under 4 years EPEC 1 -3 days Watery diarrhea in 1 st year children EIEC 1 -6 days Bloody diarrhea in any age EAgg. EC 1 -3 days Chronic diarrhea in infants under 6 months (O 157: H 7)
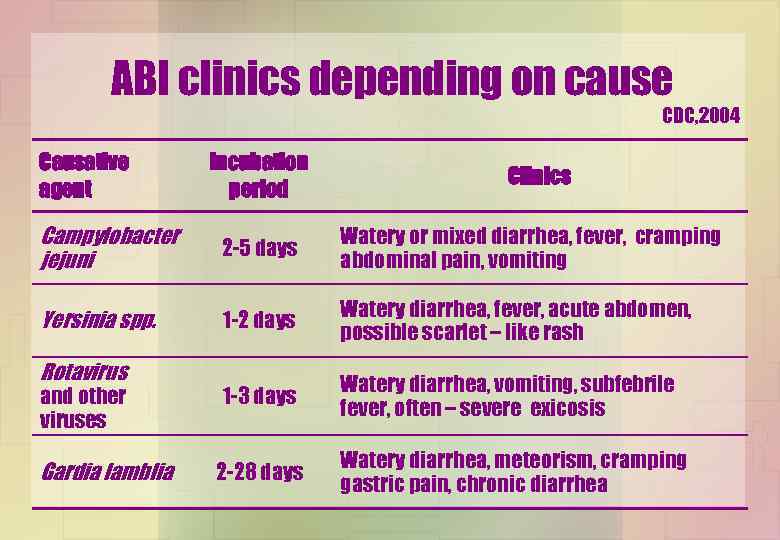
ABI clinics depending on cause CDC, 2004 Causative agent Incubation period Clinics Campylobacter jejuni 2 -5 days Watery or mixed diarrhea, fever, cramping abdominal pain, vomiting Yersinia spp. 1 -2 days Watery diarrhea, fever, acute abdomen, possible scarlet – like rash 1 -3 days Watery diarrhea, vomiting, subfebrile fever, often – severe exicosis 2 -28 days Watery diarrhea, meteorism, cramping gastric pain, chronic diarrhea Rotavirus and other viruses Gardia lamblia
Intestinal dehydration (intestinal toxico - exicosis) is a pathological condition characterized by acute fluid loss with or without electrolyte disturbances, which develops due to vomiting and/or diarrhea. The main clinical marker of dehydratation is acute body weight loss.
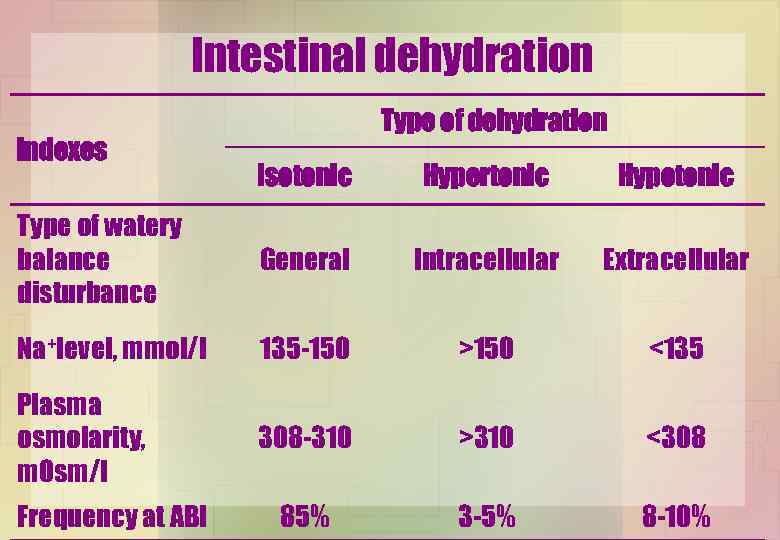
Intestinal dehydration indexes Type of dehydration Isotonic Hypertonic Hypotonic Type of watery balance disturbance General Intracellular Extracellular Na+level, mmol/l 135 -150 >150 <135 Plasma osmolarity, m. Osm/l 308 -310 >310 <308 85% 3 -5% 8 -10% Frequency at ABI
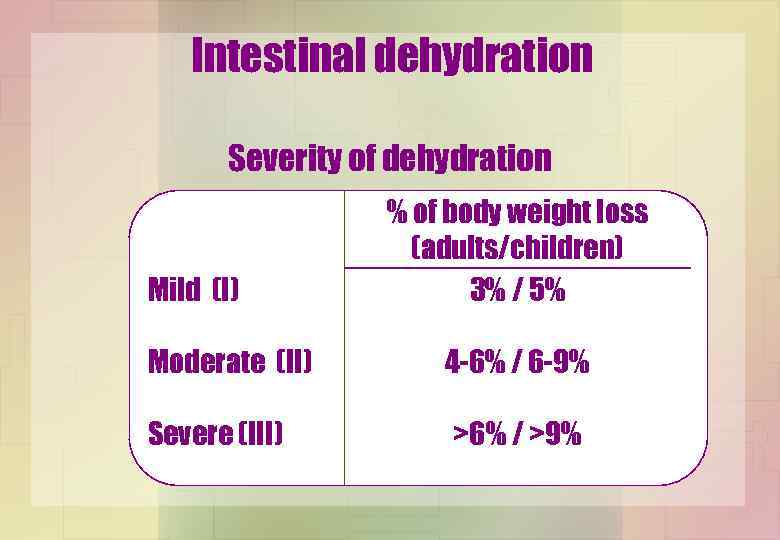
Intestinal dehydration Severity of dehydration Mild (І) % of body weight loss (adults/children) 3% / 5% Moderate (ІІ) 4 -6% / 6 -9% Severe (ІІІ) >6% / >9%
Intestinal dehydration Risk factors for dehydration development üAge less than 6 months üStool > 8 times per day üVomiting, combined with diarrhea, > 4 times per day
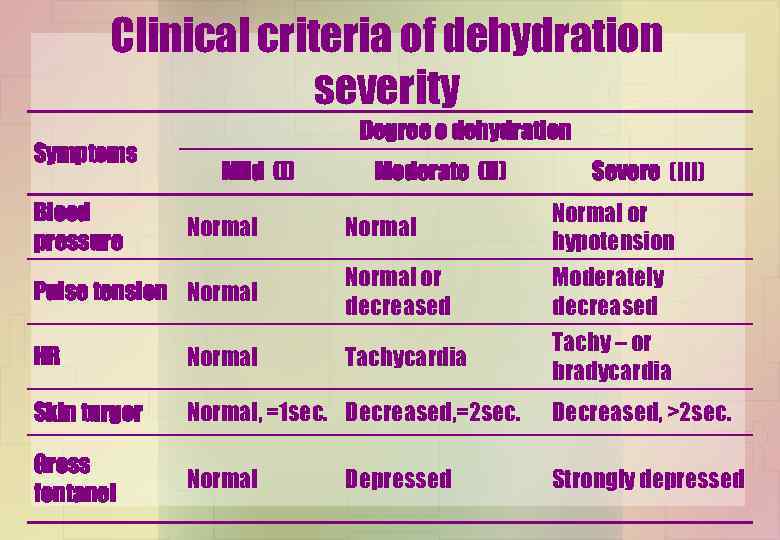
Clinical criteria of dehydration severity Symptoms Blood pressure Degree o dehydration Mild (І) Normal Moderate (ІІ) Normal Severe (ІІІ) Normal or hypotension Pulse tension Normal or decreased HR Normal Tachycardia Skin turgor Normal, =1 sec. Decreased, =2 sec. Decreased, >2 sec. Gross fontanel Normal Strongly depressed Depressed Moderately decreased Tachy – or bradycardia
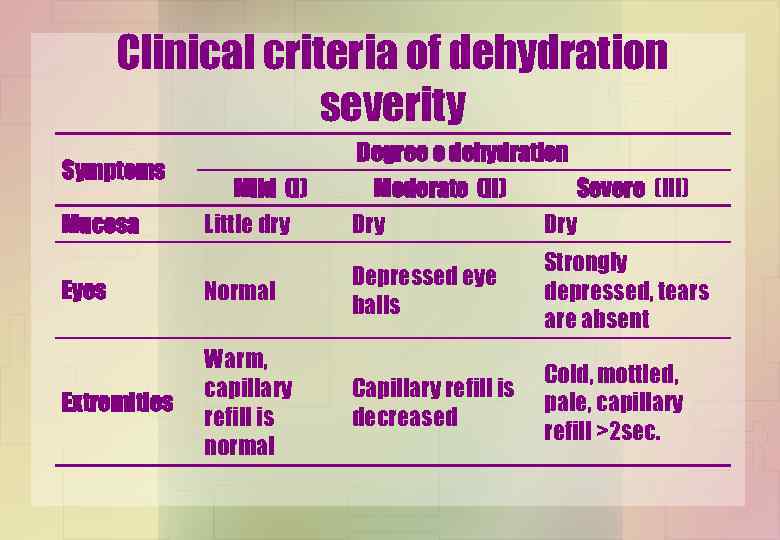
Clinical criteria of dehydration severity Symptoms Mucosa Mild (І) Little dry Eyes Normal Extremities Warm, capillary refill is normal Degree o dehydration Moderate (ІІ) Severe (ІІІ) Dry Depressed eye balls Strongly depressed, tears are absent Capillary refill is decreased Cold, mottled, pale, capillary refill >2 sec.
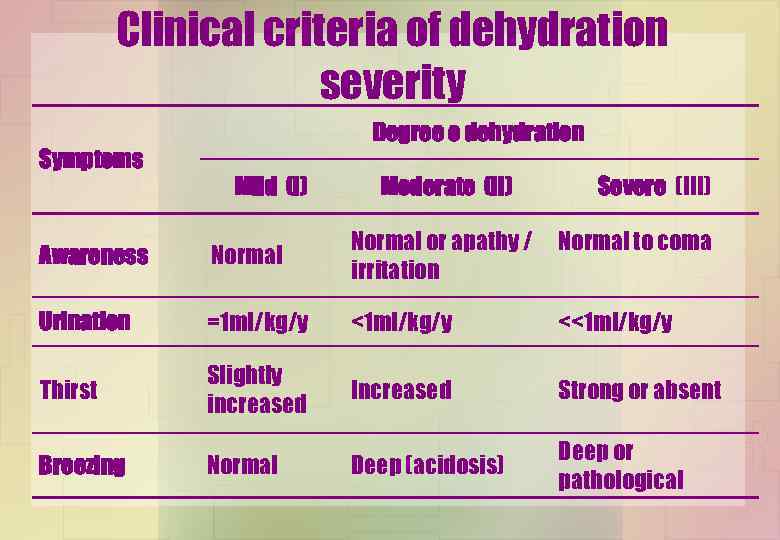
Clinical criteria of dehydration severity Symptoms Degree o dehydration Mild (І) Moderate (ІІ) Severe (ІІІ) Awareness Normal or apathy / irritation Urination =1 ml/kg/y <<1 ml/kg/y Thirst Slightly increased Increased Strong or absent Deep (acidosis) Deep or pathological Breezing Normal to coma
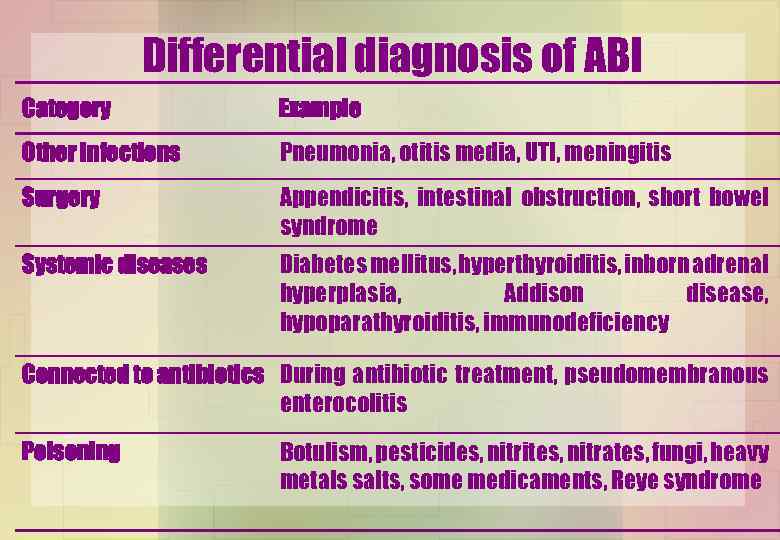
Differential diagnosis of ABI Category Example Other infections Pneumonia, otitis media, UTI, meningitis Surgery Appendicitis, intestinal obstruction, short bowel syndrome Systemic diseases Diabetes mellitus, hyperthyroiditis, inborn adrenal hyperplasia, Addison disease, hypoparathyroiditis, immunodeficiency Connected to antibiotics During antibiotic treatment, pseudomembranous enterocolitis Poisoning Botulism, pesticides, nitrites, nitrates, fungi, heavy metals salts, some medicaments, Reye syndrome
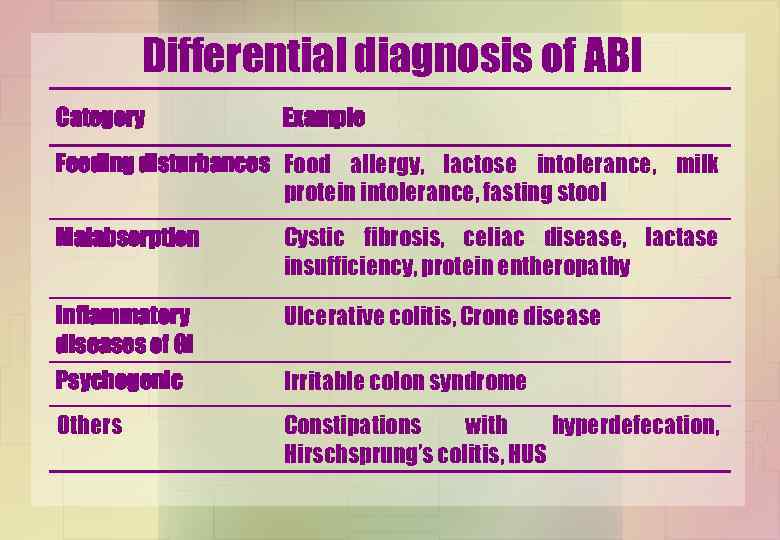
Differential diagnosis of ABI Category Example Feeding disturbances Food allergy, lactose intolerance, milk protein intolerance, fasting stool Malabsorption Cystic fibrosis, celiac disease, lactase insufficiency, protein entheropathy Inflammatory diseases of GI Psychogenic Ulcerative colitis, Crone disease Others Constipations with hyperdefecation, Hirschsprung’s colitis, HUS Irritable colon syndrome
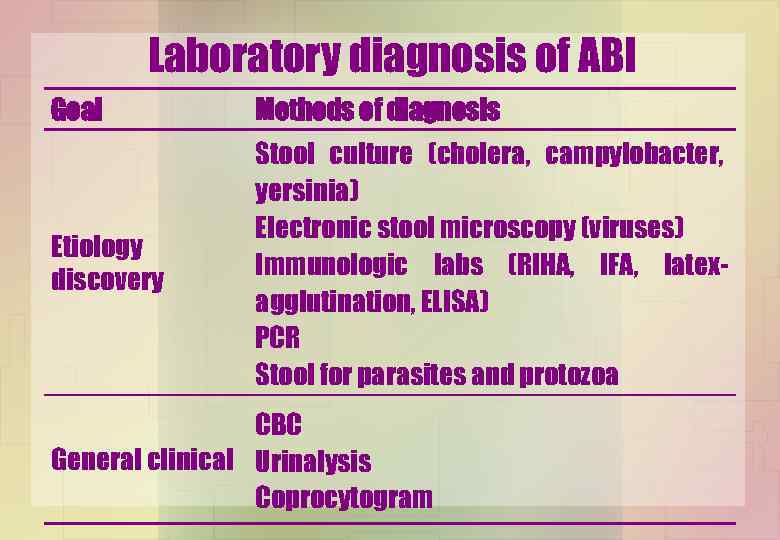
Laboratory diagnosis of ABI Goal Methods of diagnosis Etiology discovery Stool culture (cholera, campylobacter, yersinia) Electronic stool microscopy (viruses) Immunologic labs (RIHA, IFA, latexagglutination, ELISA) PCR Stool for parasites and protozoa CBC General clinical Urinalysis Coprocytogram
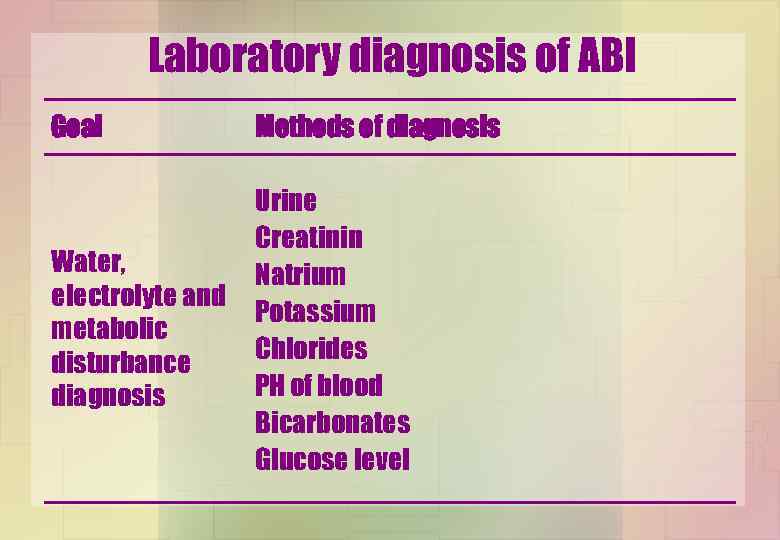
Laboratory diagnosis of ABI Goal Methods of diagnosis Water, electrolyte and metabolic disturbance diagnosis Urine Creatinin Natrium Potassium Chlorides РН of blood Bicarbonates Glucose level

Therapy of ABI üFor breast-fed children, to continue breast-feeding üFor formula-fed children, not to dilute formulas; special formulas are generally not needed Diet üRestore age-adequate feeding as soon as dehydration managed üBRAT (banana-rice-apple-tea) has no advantages comparing to feeding
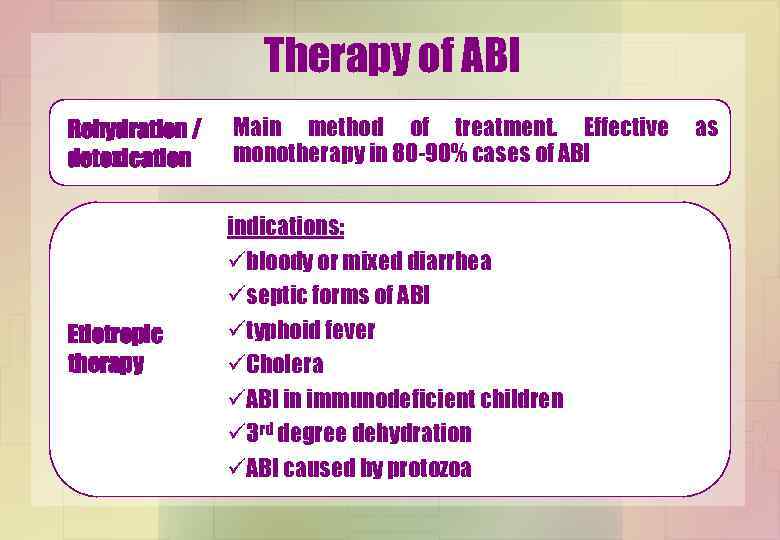
Therapy of ABI Rehydration / detoxication Main method of treatment. Effective monotherapy in 80 -90% cases of ABI Etiotropic therapy indications: übloody or mixed diarrhea üseptic forms of ABI ütyphoid fever üCholera üABI in immunodeficient children ü 3 rd degree dehydration üABI caused by protozoa as
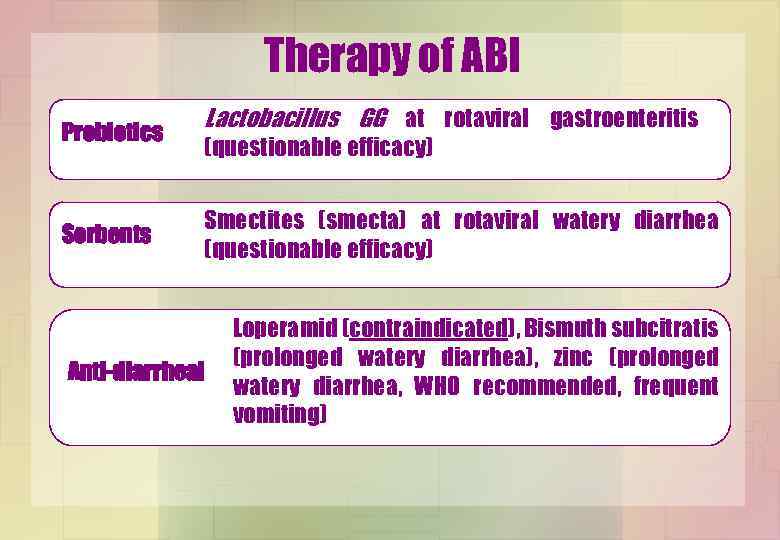
Therapy of ABI Probiotics Sorbents Lactobacillus GG at rotaviral gastroenteritis (questionable efficacy) Smectites (smecta) at rotaviral watery diarrhea (questionable efficacy) Anti-diarrheal Loperamid (contraindicated), Bismuth subcitratis (prolonged watery diarrhea), zinc (prolonged watery diarrhea, WHO recommended, frequent vomiting)

Therapy of ABI v. Children with risk factors of dehydration development v. Dehydration of 2 nd and 3 rd degree v. Bloody diarrhea Indications for v. Prominent abdominal pain hospitalization v. Decreased awareness v. Immunodeficient children v. Children with severe somatic pathology v. Inability to perform rehydration at home v. Inadequate parents
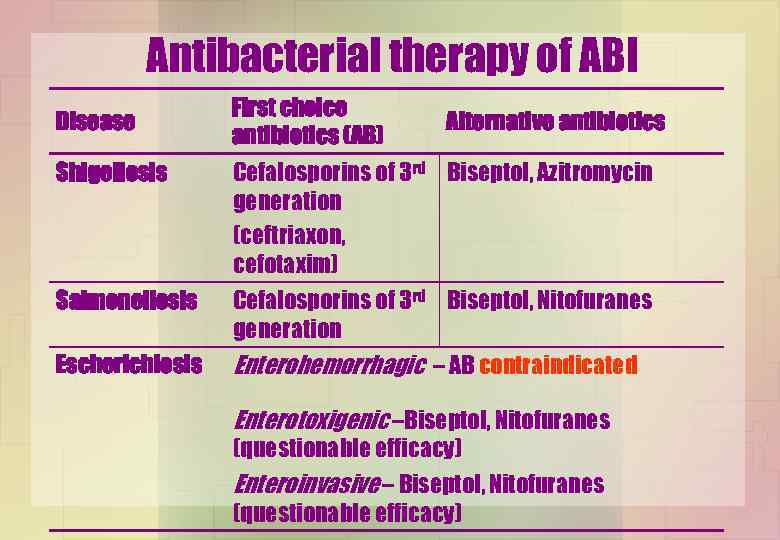
Antibacterial therapy of ABI Disease First choice antibiotics (AB) Alternative antibiotics Shigellosis Cefalosporins of 3 rd Biseptol, Azitromycin generation (ceftriaxon, cefotaxim) Salmonellosis Cefalosporins of 3 rd Biseptol, Nitofuranes generation Escherichiosis Enterohemorrhagic – АB contraindicated Еnterotoxigenic –Biseptol, Nitofuranes (questionable efficacy) Enteroinvasive – Biseptol, Nitofuranes (questionable efficacy)
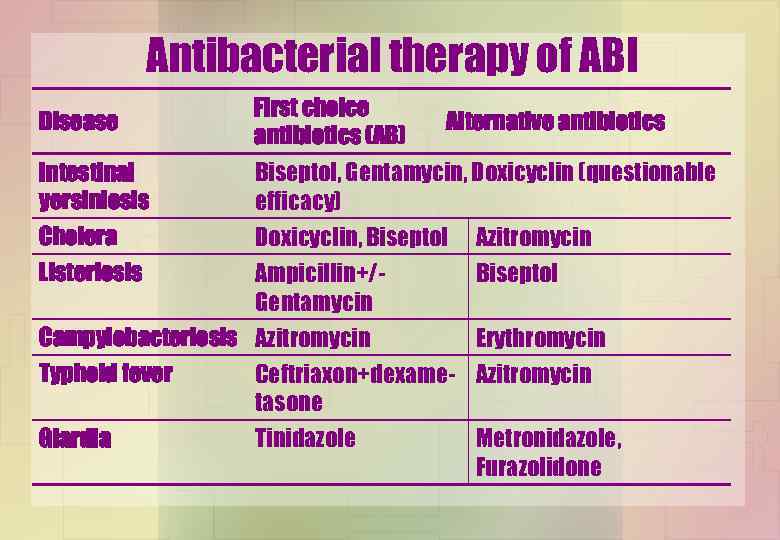
Antibacterial therapy of ABI Disease First choice antibiotics (AB) Intestinal yersiniosis Biseptol, Gentamycin, Doxicyclin (questionable efficacy) Cholera Listeriosis Alternative antibiotics Doxicyclin, Biseptol Ampicillin+/Gentamycin Campylobacteriosis Azitromycin Typhoid fever Giardia Azitromycin Biseptol Erythromycin Ceftriaxon+dexame- Azitromycin tasone Tinidazole Metronidazole, Furazolidone

Antibacterial therapy of ABI Fluoroquinolones (Ciprofloxacin, norfloxacin) are first-choice antibiotics for adults; and children older 16 years. For younger children - only in critical, lifethreatening cases.

Rehydration therapy at ABI ESPGAN, 2005 ü For 1 st and 2 nd degree dehydration oral rehydration solutions (ОRS) must be used ü Peroral rehydration must be performed quickly (during 34 hours) ü Additional ORS must be used at further fluid loss due to diarrhea or vomiting ü 3 rd degree treatment must be performed by bolus IV infusion of normal saline (Ringer lactate)
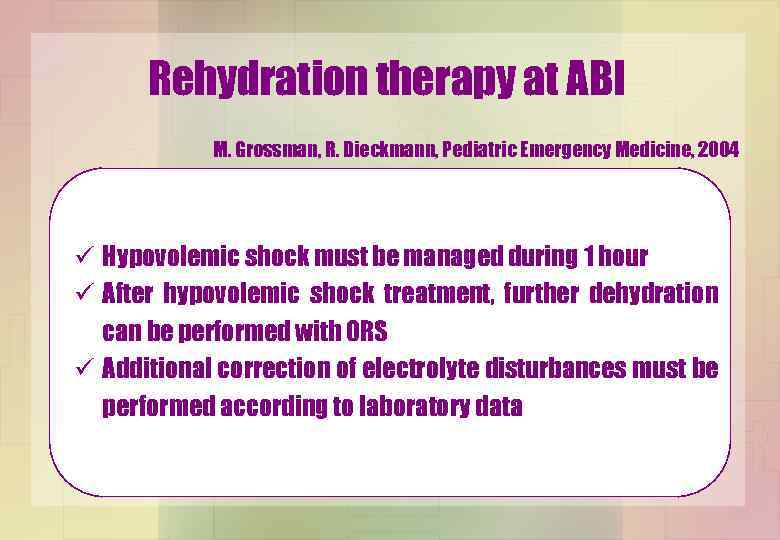
Rehydration therapy at ABI M. Grossman, R. Dieckmann, Pediatric Emergency Medicine, 2004 ü Hypovolemic shock must be managed during 1 hour ü After hypovolemic shock treatment, further dehydration can be performed with ORS ü Additional correction of electrolyte disturbances must be performed according to laboratory data
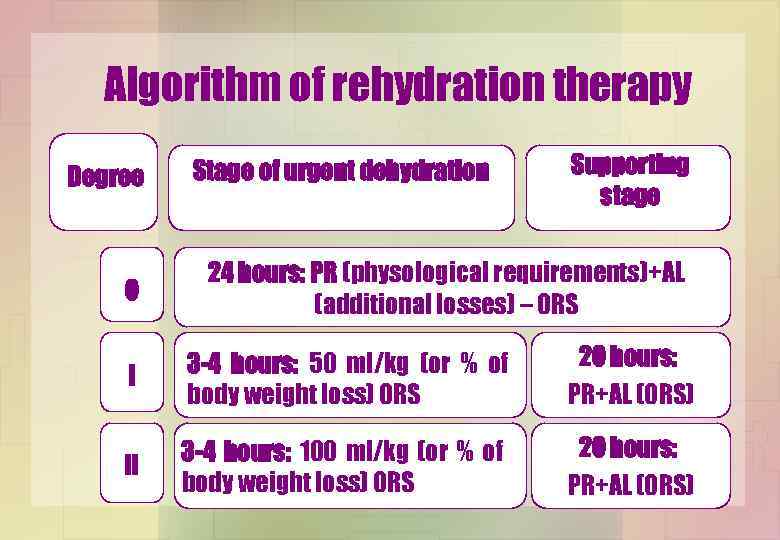
Algorithm of rehydration therapy Degree 0 Stage of urgent dehydration Supporting stage 24 hours: PR (physological requirements)+AL (additional losses) – ORS І 3 -4 hours: 50 ml/kg (or % of body weight loss) ORS 20 hours: PR+AL (ORS) ІІ 3 -4 hours: 100 ml/kg (or % of body weight loss) ORS 20 hours: PR+AL (ORS)
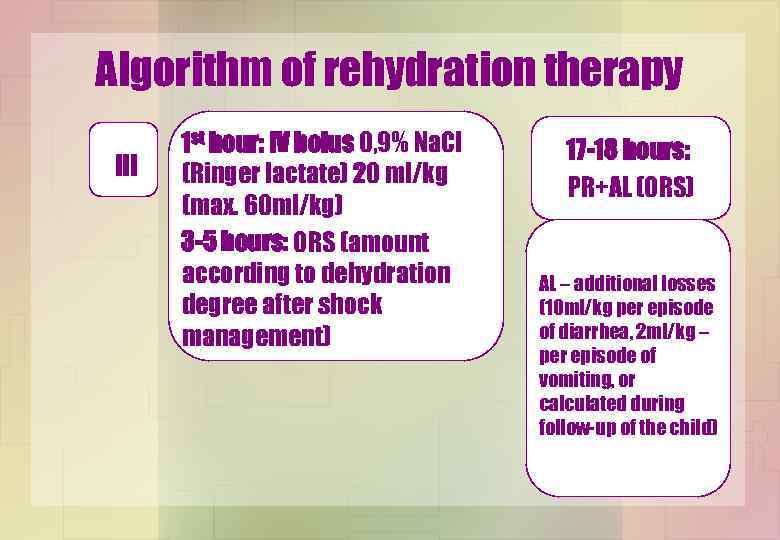
Algorithm of rehydration therapy ІІІ 1 st hour: IV bolus 0, 9% Na. Cl (Ringer lactate) 20 ml/kg (max. 60 ml/kg) 3 -5 hours: ORS (amount according to dehydration degree after shock management) 17 -18 hours: PR+AL (ORS) AL – additional losses (10 ml/kg per episode of diarrhea, 2 ml/kg – per episode of vomiting, or calculated during follow-up of the child)
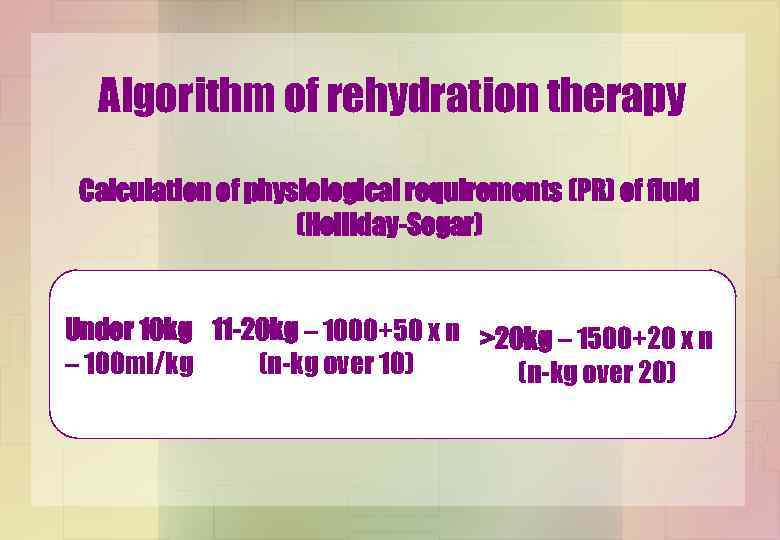
Algorithm of rehydration therapy Calculation of physiological requirements (PR) of fluid (Holliday-Segar) Under 10 kg 11 -20 kg – 1000+50 x n >20 kg – 1500+20 x n – 100 ml/kg (n-kg over 10) (n-kg over 20)
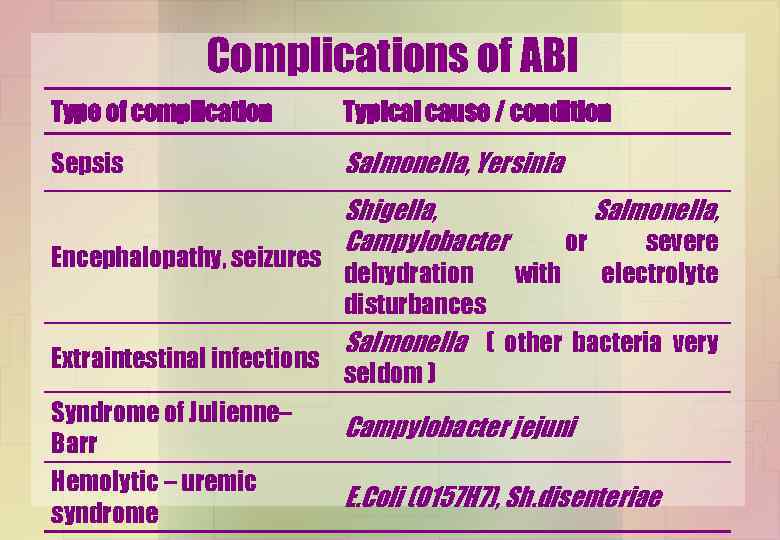
Complications of ABI Type of complication Typical cause / condition Sepsis Salmonella, Yersinia Encephalopathy, seizures Shigella, Campylobacter or Salmonella, severe electrolyte dehydration with disturbances Salmonella ( other bacteria very Extraintestinal infections seldom ) Syndrome of Julienne– Campylobacter jejuni Barr Hemolytic – uremic Е. Coli (O 157 H 7), Sh. disenteriae syndrome
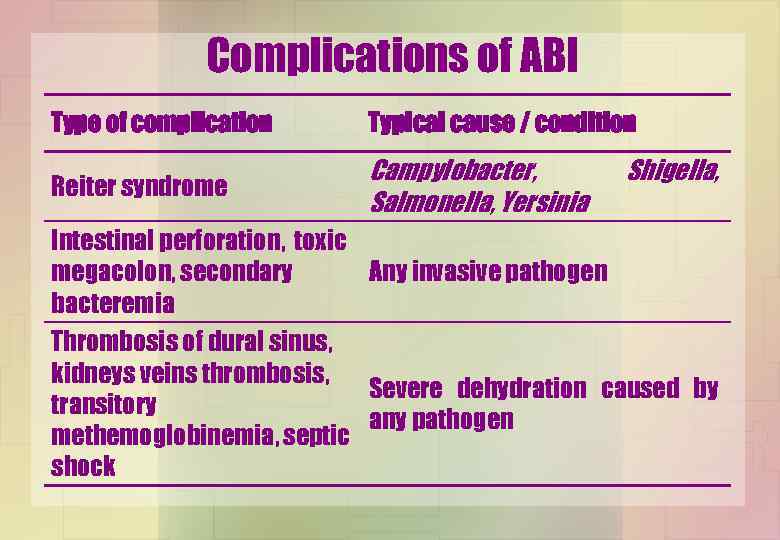
Complications of ABI Type of complication Typical cause / condition Reiter syndrome Campylobacter, Salmonella, Yersinia Shigella, Intestinal perforation, toxic megacolon, secondary Any invasive pathogen bacteremia Thrombosis of dural sinus, kidneys veins thrombosis, Severe dehydration caused by transitory any pathogen methemoglobinemia, septic shock
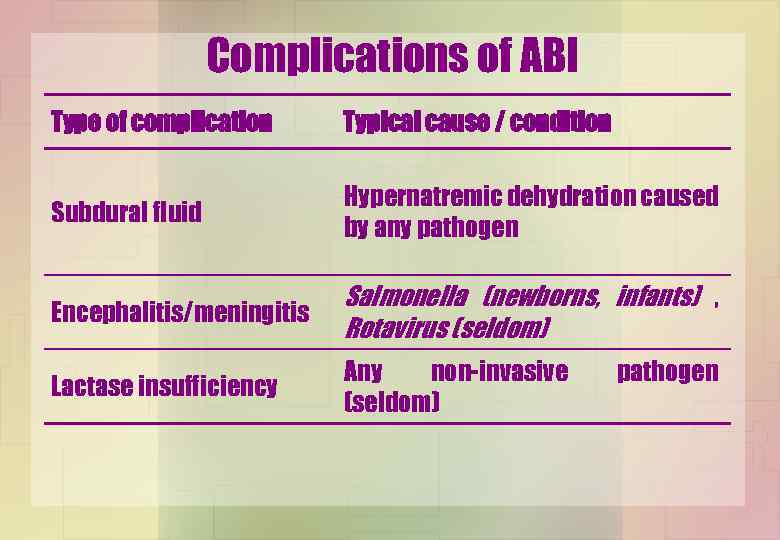
Complications of ABI Type of complication Typical cause / condition Subdural fluid Hypernatremic dehydration caused by any pathogen Encephalitis/meningitis Salmonella (newborns, infants) , Rotavirus (seldom) Lactase insufficiency Any non-invasive (seldom) pathogen
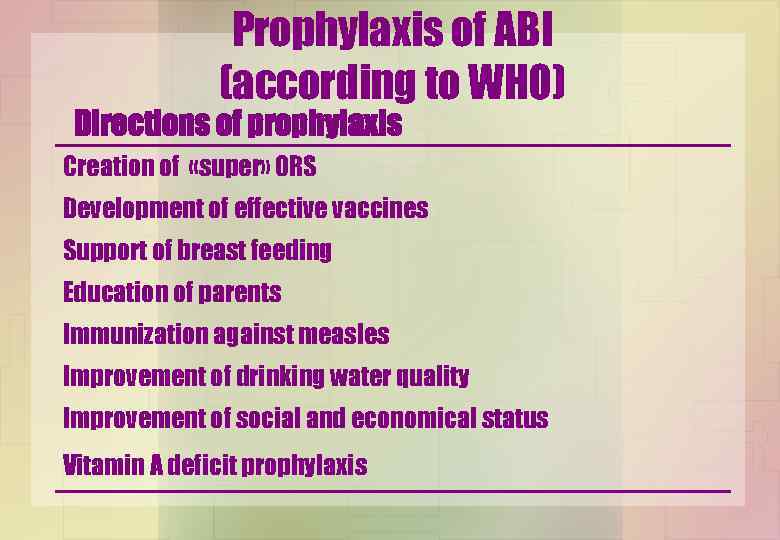
Prophylaxis of ABI (according to WHO) Directions of prophylaxis Creation of «super» ORS Development of effective vaccines Support of breast feeding Education of parents Immunization against measles Improvement of drinking water quality Improvement of social and economical status Vitamin A deficit prophylaxis
Acute diarrhea.ppt