6e8e2e35a806e655f866b845bfa9664a.ppt
- Количество слайдов: 80
 Diagnosis & Management of Transfusion Reactions Christopher J. Gresens, M. D. VP & Medical Director, Clinical Services Blood. Source
Diagnosis & Management of Transfusion Reactions Christopher J. Gresens, M. D. VP & Medical Director, Clinical Services Blood. Source
 Outline • Brief Contextual Discussions – How We Manufacture Blood Components – Donor Blood Testing and the Transfusion Transmitted Diseases • Acute Transfusion Reactions • Delayed Transfusion Reactions • Evaluation/Management of Suspected Transfusion Reactions • Miscellaneous Transfusion Reactions • Q&A
Outline • Brief Contextual Discussions – How We Manufacture Blood Components – Donor Blood Testing and the Transfusion Transmitted Diseases • Acute Transfusion Reactions • Delayed Transfusion Reactions • Evaluation/Management of Suspected Transfusion Reactions • Miscellaneous Transfusion Reactions • Q&A
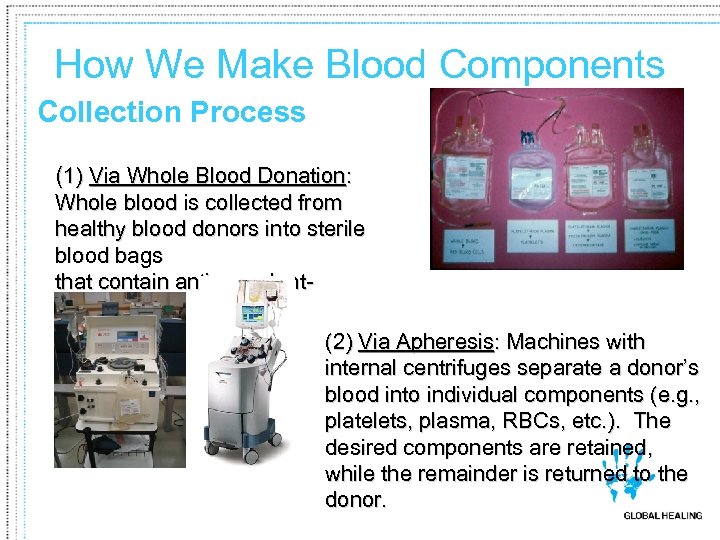 How We Make Blood Components Collection Process (1) Via Whole Blood Donation: Whole blood is collected from healthy blood donors into sterile blood bags that contain anticoagulantpreservative. (2) Via Apheresis: Machines with internal centrifuges separate a donor’s blood into individual components (e. g. , platelets, plasma, RBCs, etc. ). The desired components are retained, while the remainder is returned to the donor.
How We Make Blood Components Collection Process (1) Via Whole Blood Donation: Whole blood is collected from healthy blood donors into sterile blood bags that contain anticoagulantpreservative. (2) Via Apheresis: Machines with internal centrifuges separate a donor’s blood into individual components (e. g. , platelets, plasma, RBCs, etc. ). The desired components are retained, while the remainder is returned to the donor.
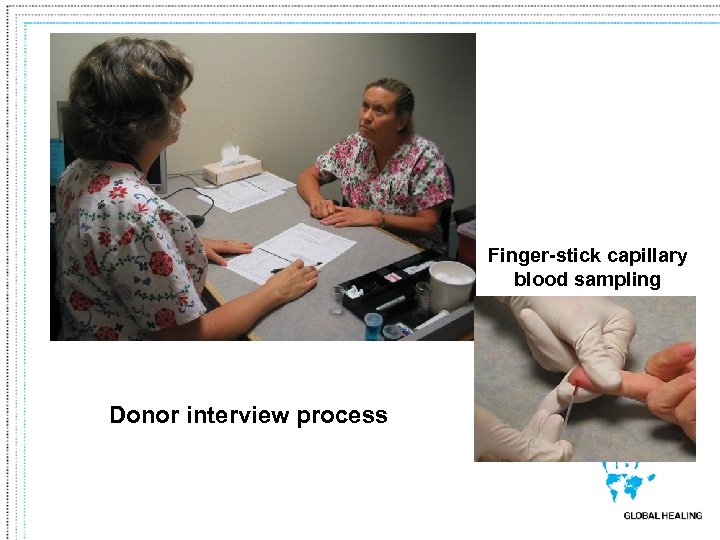 Finger-stick capillary blood sampling Donor interview process
Finger-stick capillary blood sampling Donor interview process
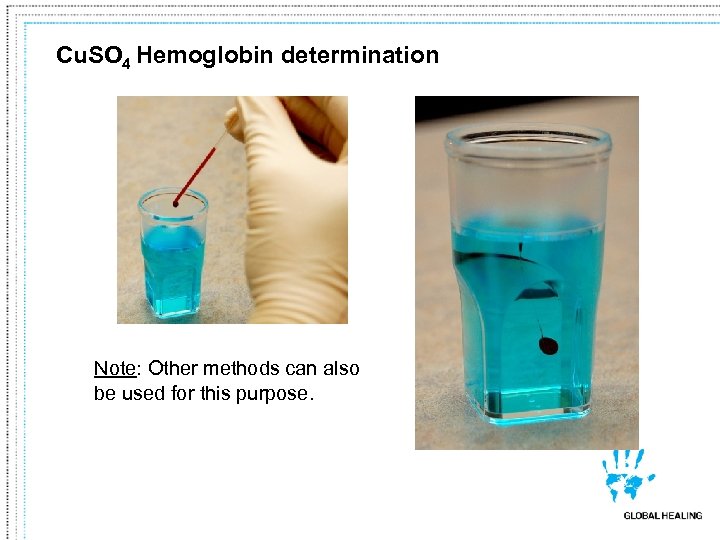 Cu. SO 4 Hemoglobin determination Note: Other methods can also be used for this purpose.
Cu. SO 4 Hemoglobin determination Note: Other methods can also be used for this purpose.
 BP, Pulse, and Temperature Check
BP, Pulse, and Temperature Check
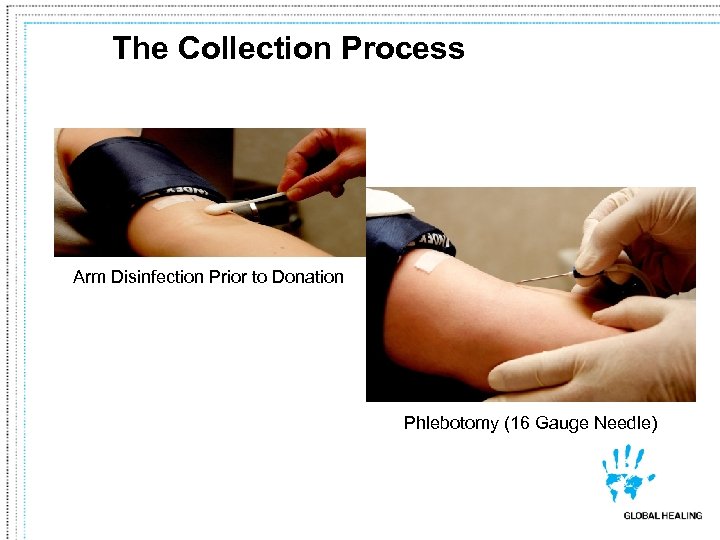 The Collection Process Arm Disinfection Prior to Donation Phlebotomy (16 Gauge Needle)
The Collection Process Arm Disinfection Prior to Donation Phlebotomy (16 Gauge Needle)
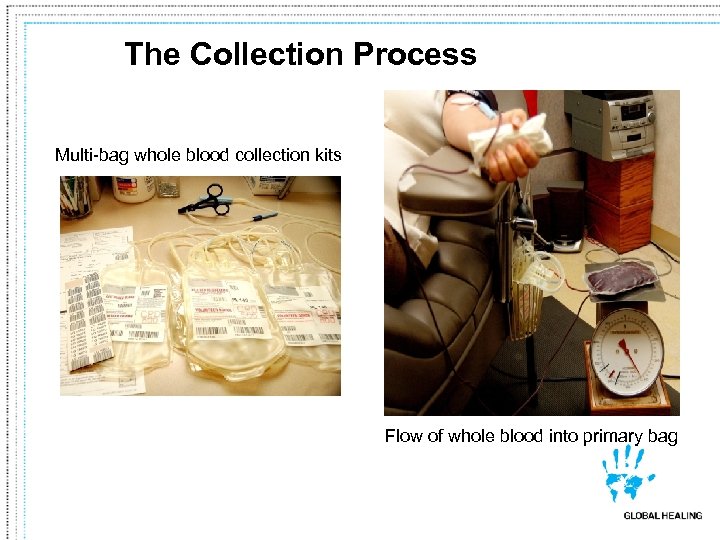 The Collection Process Multi-bag whole blood collection kits Flow of whole blood into primary bag
The Collection Process Multi-bag whole blood collection kits Flow of whole blood into primary bag
 Whole Blood Collection
Whole Blood Collection
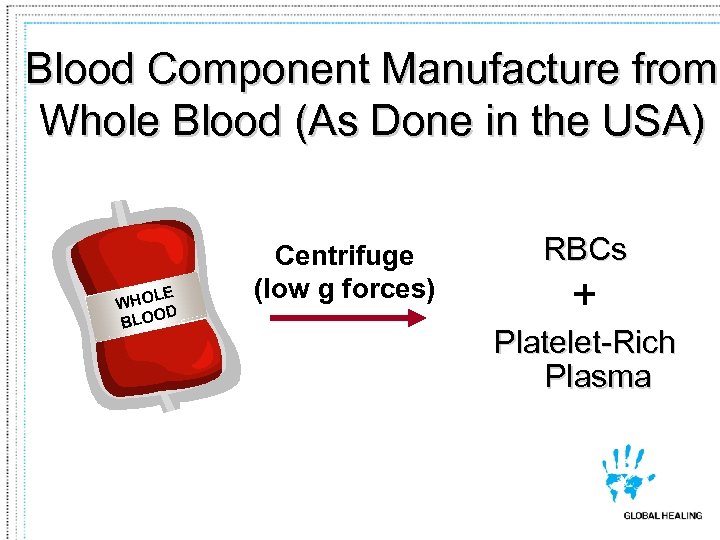 Blood Component Manufacture from Whole Blood (As Done in the USA) LE WHO D BLOO Centrifuge (low g forces) RBCs + Platelet-Rich Plasma
Blood Component Manufacture from Whole Blood (As Done in the USA) LE WHO D BLOO Centrifuge (low g forces) RBCs + Platelet-Rich Plasma
 Centrifuge Used for Component Manufacture
Centrifuge Used for Component Manufacture
 Multi-pack Collection Bag
Multi-pack Collection Bag
 Centrifuge - Interior
Centrifuge - Interior

 Blood Component Manufacture from Whole Blood • Leukoreduce • Possibly irradiate • Other RBCs + Platelet-Rich Plasma uge Centrif ces) for gher g (hi Platelets or Plasma Fre eze + Fresh Frozen Plasma (FFP) or “Plasma Frozen with 24 hours”
Blood Component Manufacture from Whole Blood • Leukoreduce • Possibly irradiate • Other RBCs + Platelet-Rich Plasma uge Centrif ces) for gher g (hi Platelets or Plasma Fre eze + Fresh Frozen Plasma (FFP) or “Plasma Frozen with 24 hours”
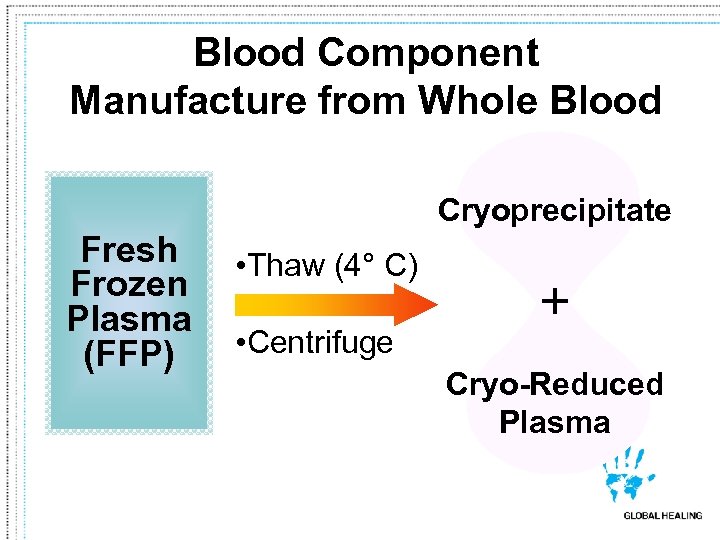 Blood Component Manufacture from Whole Blood Cryoprecipitate Fresh Frozen Plasma (FFP) • Thaw (4° C) • Centrifuge + Cryo-Reduced Plasma
Blood Component Manufacture from Whole Blood Cryoprecipitate Fresh Frozen Plasma (FFP) • Thaw (4° C) • Centrifuge + Cryo-Reduced Plasma
 Using the “Leftovers” Wisely maind) as k Pl ny Sent for fa o ( further processing Plasma Derivatives § § Albumin Factor VIII Immune globulin etc.
Using the “Leftovers” Wisely maind) as k Pl ny Sent for fa o ( further processing Plasma Derivatives § § Albumin Factor VIII Immune globulin etc.
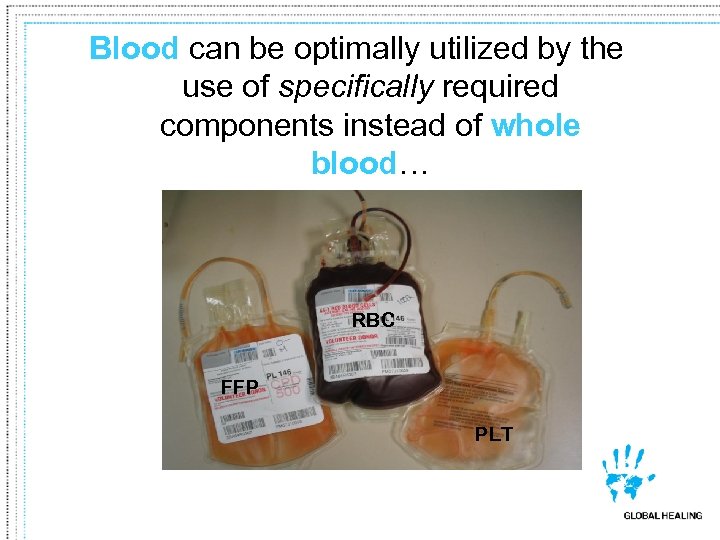 Blood can be optimally utilized by the use of specifically required components instead of whole blood… RBC FFP PLT
Blood can be optimally utilized by the use of specifically required components instead of whole blood… RBC FFP PLT
 “Shotgun” Approach vs. .
“Shotgun” Approach vs. .
 Component Therapy
Component Therapy
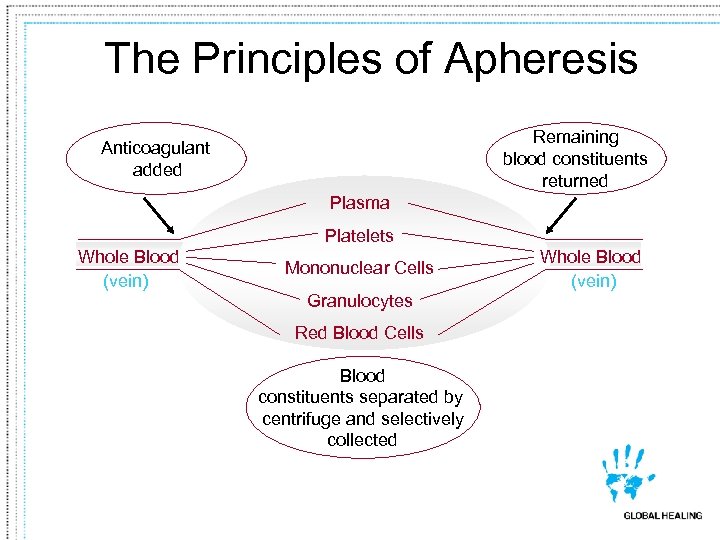 The Principles of Apheresis Remaining blood constituents returned Anticoagulant added Plasma Platelets Whole Blood (vein) Mononuclear Cells Granulocytes Red Blood Cells Blood constituents separated by centrifuge and selectively collected Whole Blood (vein)
The Principles of Apheresis Remaining blood constituents returned Anticoagulant added Plasma Platelets Whole Blood (vein) Mononuclear Cells Granulocytes Red Blood Cells Blood constituents separated by centrifuge and selectively collected Whole Blood (vein)
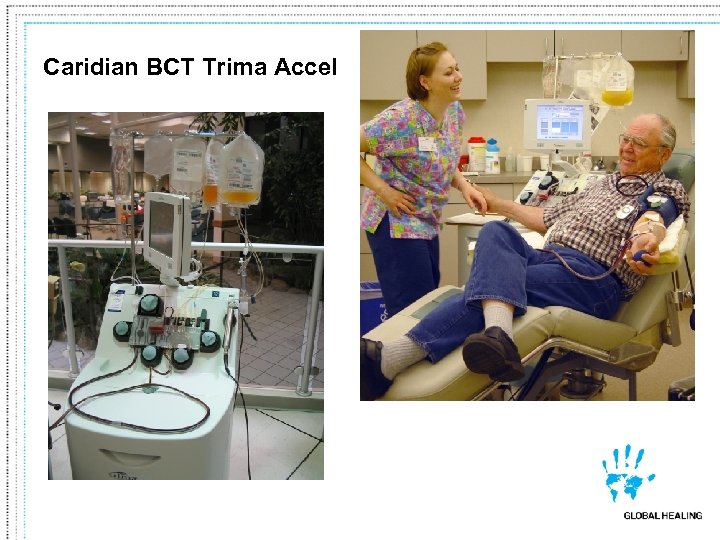 Caridian BCT Trima Accel
Caridian BCT Trima Accel
 Haemonetics PCS-2
Haemonetics PCS-2
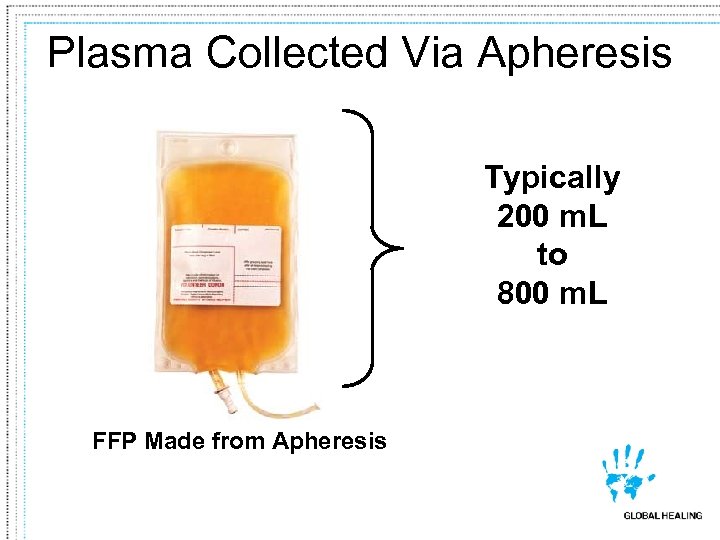 Plasma Collected Via Apheresis Typically 200 m. L to 800 m. L FFP Made from Apheresis
Plasma Collected Via Apheresis Typically 200 m. L to 800 m. L FFP Made from Apheresis
 Donor sample tubes being readied for testing
Donor sample tubes being readied for testing
 Infectious Disease testing (Abbott PRISM)
Infectious Disease testing (Abbott PRISM)
 Chagas Disease Testing (Ortho Platform)
Chagas Disease Testing (Ortho Platform)
 NAT – We recently converted to Chiron Ultrio (HIV, HBV, and HCV); we also do WNV by NAT
NAT – We recently converted to Chiron Ultrio (HIV, HBV, and HCV); we also do WNV by NAT
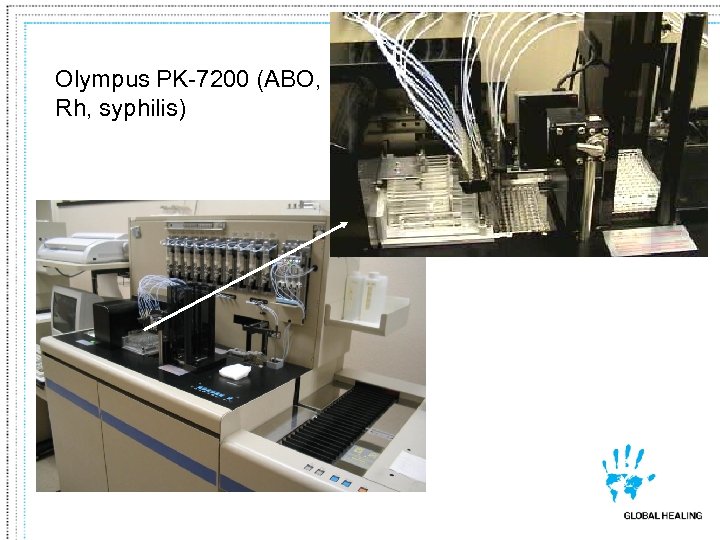 Olympus PK-7200 (ABO, Rh, syphilis)
Olympus PK-7200 (ABO, Rh, syphilis)
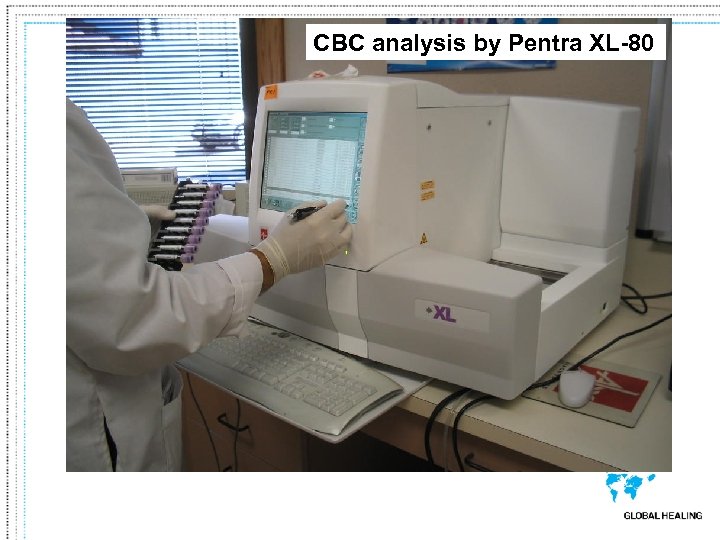 CBC analysis by Pentra XL-80
CBC analysis by Pentra XL-80
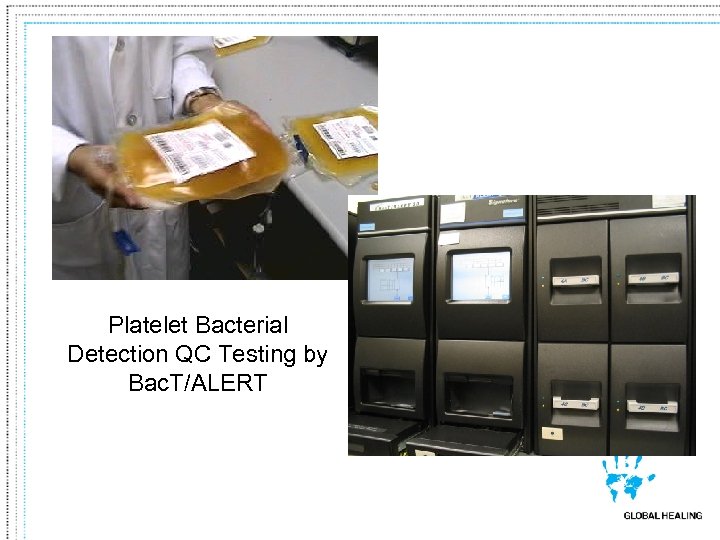 Platelet Bacterial Detection QC Testing by Bac. T/ALERT
Platelet Bacterial Detection QC Testing by Bac. T/ALERT
 Donor Blood Testing • • ABO Rh Antibody Screen Infectious Diseases – Syphilis – HBs. Ag – Anti-HIV-1/2 – Anti-HBc
Donor Blood Testing • • ABO Rh Antibody Screen Infectious Diseases – Syphilis – HBs. Ag – Anti-HIV-1/2 – Anti-HBc
 Donor Blood Testing • Infectious Diseases – Anti-HTLV-I/II – Anti-HCV – HIV Nucleic acid testing (NAT) – HCV NAT – WNV NAT – Anti-T. cruzi (Chagas disease) – (On some units) Anti-CMV
Donor Blood Testing • Infectious Diseases – Anti-HTLV-I/II – Anti-HCV – HIV Nucleic acid testing (NAT) – HCV NAT – WNV NAT – Anti-T. cruzi (Chagas disease) – (On some units) Anti-CMV
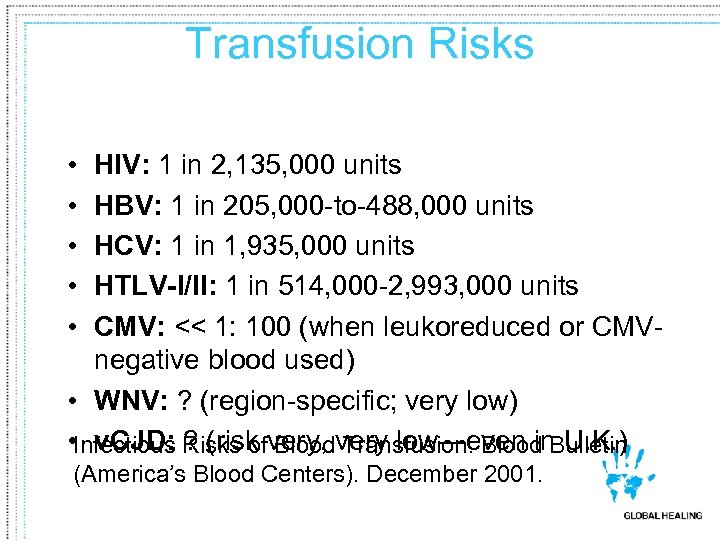 Transfusion Risks • • • HIV: 1 in 2, 135, 000 units HBV: 1 in 205, 000 -to-488, 000 units HCV: 1 in 1, 935, 000 units HTLV-I/II: 1 in 514, 000 -2, 993, 000 units CMV: << 1: 100 (when leukoreduced or CMVnegative blood used) • WNV: ? (region-specific; very low) • Infectious Risks ofvery, very low—even in U. K. ) v. CJD: ? (risk Blood Transfusion. Blood Bulletin (America’s Blood Centers). December 2001.
Transfusion Risks • • • HIV: 1 in 2, 135, 000 units HBV: 1 in 205, 000 -to-488, 000 units HCV: 1 in 1, 935, 000 units HTLV-I/II: 1 in 514, 000 -2, 993, 000 units CMV: << 1: 100 (when leukoreduced or CMVnegative blood used) • WNV: ? (region-specific; very low) • Infectious Risks ofvery, very low—even in U. K. ) v. CJD: ? (risk Blood Transfusion. Blood Bulletin (America’s Blood Centers). December 2001.
 Acute Transfusion Reactions
Acute Transfusion Reactions
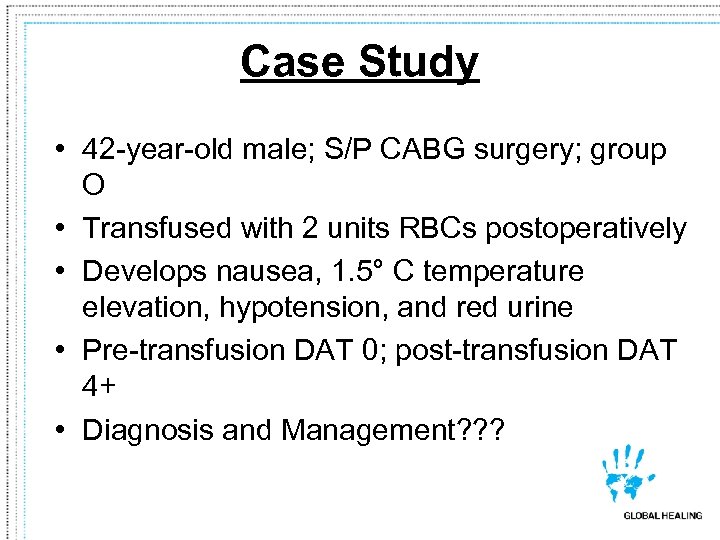 Case Study • 42 -year-old male; S/P CABG surgery; group O • Transfused with 2 units RBCs postoperatively • Develops nausea, 1. 5° C temperature elevation, hypotension, and red urine • Pre-transfusion DAT 0; post-transfusion DAT 4+ • Diagnosis and Management? ? ?
Case Study • 42 -year-old male; S/P CABG surgery; group O • Transfused with 2 units RBCs postoperatively • Develops nausea, 1. 5° C temperature elevation, hypotension, and red urine • Pre-transfusion DAT 0; post-transfusion DAT 4+ • Diagnosis and Management? ? ?
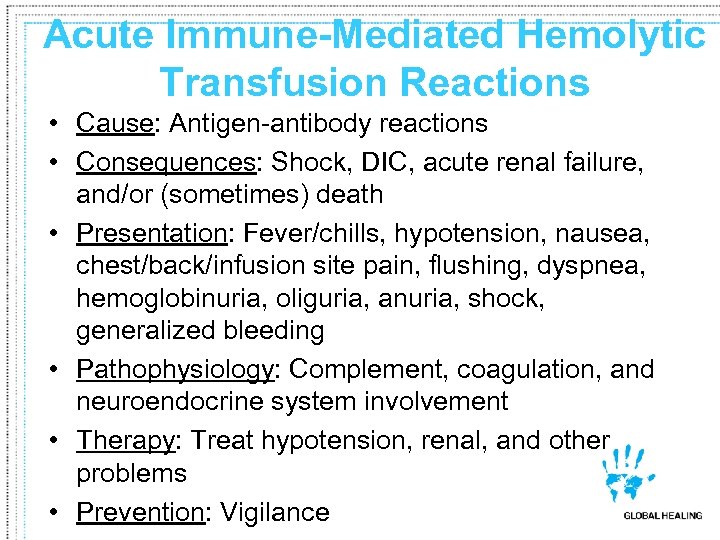 Acute Immune-Mediated Hemolytic Transfusion Reactions • Cause: Antigen-antibody reactions • Consequences: Shock, DIC, acute renal failure, and/or (sometimes) death • Presentation: Fever/chills, hypotension, nausea, chest/back/infusion site pain, flushing, dyspnea, hemoglobinuria, oliguria, anuria, shock, generalized bleeding • Pathophysiology: Complement, coagulation, and neuroendocrine system involvement • Therapy: Treat hypotension, renal, and other problems • Prevention: Vigilance
Acute Immune-Mediated Hemolytic Transfusion Reactions • Cause: Antigen-antibody reactions • Consequences: Shock, DIC, acute renal failure, and/or (sometimes) death • Presentation: Fever/chills, hypotension, nausea, chest/back/infusion site pain, flushing, dyspnea, hemoglobinuria, oliguria, anuria, shock, generalized bleeding • Pathophysiology: Complement, coagulation, and neuroendocrine system involvement • Therapy: Treat hypotension, renal, and other problems • Prevention: Vigilance
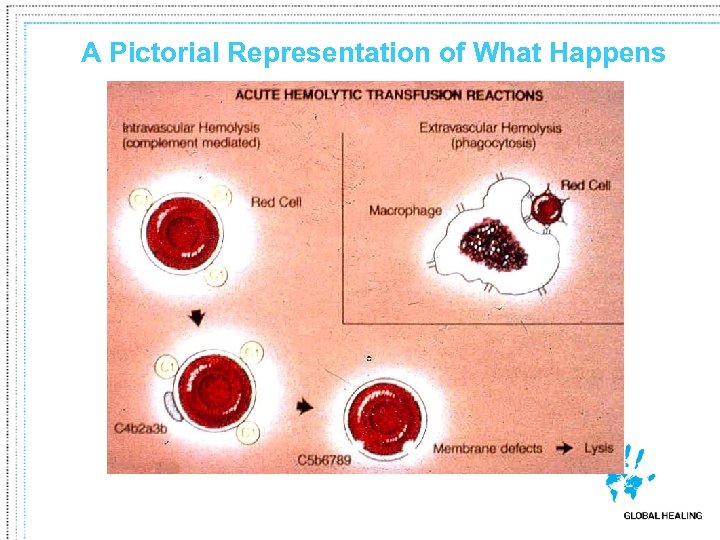 A Pictorial Representation of What Happens
A Pictorial Representation of What Happens
 Acute Non-Immune Hemolytic Transfusion Reactions • Examples: • • • Osmotic lysis Accidental freezing Accidental overheating Inadequate deglycerolization Mechanical hemolysis Intrinsic defects in either donor’s or recipient’s RBCs (e. g. , G-6 PD deficiency, sickle cell disease)
Acute Non-Immune Hemolytic Transfusion Reactions • Examples: • • • Osmotic lysis Accidental freezing Accidental overheating Inadequate deglycerolization Mechanical hemolysis Intrinsic defects in either donor’s or recipient’s RBCs (e. g. , G-6 PD deficiency, sickle cell disease)
 Case Study • 7 -year-old female with AML; postchemotherapy; group A • Transfused ½ plateletpheresis unit (CMV-negative, irradiated, & leukoreduced) • 20 minutes into transfusion, develops nausea, 2. 4° C temperature elevation, hypotension, and red urine • Diagnosis and Management? ? ?
Case Study • 7 -year-old female with AML; postchemotherapy; group A • Transfused ½ plateletpheresis unit (CMV-negative, irradiated, & leukoreduced) • 20 minutes into transfusion, develops nausea, 2. 4° C temperature elevation, hypotension, and red urine • Diagnosis and Management? ? ?
 Septic Transfusion Reactions • Presentation: High fever, shock, DIC, hemoglobinuria, renal failure, GI complications, generalized muscle pain • RBC Contaminants: Yersinia enterocolitica, Pseudomonas species, E. coli, etc. • Platelet Contaminants: Coagulase-negative Staphylococci, Salmonella, Staphylococcus aureus, etc. • Prevention: QC testing of all platelets, visual inspection of all blood products
Septic Transfusion Reactions • Presentation: High fever, shock, DIC, hemoglobinuria, renal failure, GI complications, generalized muscle pain • RBC Contaminants: Yersinia enterocolitica, Pseudomonas species, E. coli, etc. • Platelet Contaminants: Coagulase-negative Staphylococci, Salmonella, Staphylococcus aureus, etc. • Prevention: QC testing of all platelets, visual inspection of all blood products
 Bacteria from donor arm’s skin before and after cleansing Before After
Bacteria from donor arm’s skin before and after cleansing Before After
 Case Study • 60 -year-old male; GI bleeding; group AB • Transfused one unit RBCs • 2 minutes into transfusion, develops nausea, hypotension, and respiratory failure with wheezing (at first), followed by shallow, rapid breathing without wheezing • Diagnosis and Management? ? ?
Case Study • 60 -year-old male; GI bleeding; group AB • Transfused one unit RBCs • 2 minutes into transfusion, develops nausea, hypotension, and respiratory failure with wheezing (at first), followed by shallow, rapid breathing without wheezing • Diagnosis and Management? ? ?
 Anaphylactic Transfusion Reactions • Cause: Reaction against Ig. A or other plasma-soluble antigens in blood component • Presentation: (Absence of fever), respiratory and GI symptoms, shock, and/or syncope • Treatment: Give epinephrine, corticosteroids, etc. ; maintain airway • Prevention: Transfuse with Ig. A-deficient (and/or carefully washed) products when necessary
Anaphylactic Transfusion Reactions • Cause: Reaction against Ig. A or other plasma-soluble antigens in blood component • Presentation: (Absence of fever), respiratory and GI symptoms, shock, and/or syncope • Treatment: Give epinephrine, corticosteroids, etc. ; maintain airway • Prevention: Transfuse with Ig. A-deficient (and/or carefully washed) products when necessary
 Case Study • 22 -year-old female; spontaneous bleeding and coagulopathy (cause unknown); group O • Transfused with 2 units of FFP • 2 minutes into transfusion, develops 1. 4° C temperature elevation, hypotension, rapid respiratory compromise requiring intubation, foamy sputum, bilateral pulmonary edema on chest X-radiograph • Diagnosis and Management? ? ?
Case Study • 22 -year-old female; spontaneous bleeding and coagulopathy (cause unknown); group O • Transfused with 2 units of FFP • 2 minutes into transfusion, develops 1. 4° C temperature elevation, hypotension, rapid respiratory compromise requiring intubation, foamy sputum, bilateral pulmonary edema on chest X-radiograph • Diagnosis and Management? ? ?
 Transfusion-Related Acute Lung Injury (TRALI) • Causes § Major—Interaction between pre-existing (most often donor) HLA or granulocyte antibodies and WBCs of (usually) patient origin § Minor (? )—Neutrophil priming agent within donor blood that primes PMN oxidase in patient • Presentation: Acute respiratory insufficiency, fever, hypotension, CXR c/w pulmonary edema • Treatment: Respiratory support; ? corticosteroids
Transfusion-Related Acute Lung Injury (TRALI) • Causes § Major—Interaction between pre-existing (most often donor) HLA or granulocyte antibodies and WBCs of (usually) patient origin § Minor (? )—Neutrophil priming agent within donor blood that primes PMN oxidase in patient • Presentation: Acute respiratory insufficiency, fever, hypotension, CXR c/w pulmonary edema • Treatment: Respiratory support; ? corticosteroids
 Pre-TRALI Chest X-Radiograph
Pre-TRALI Chest X-Radiograph
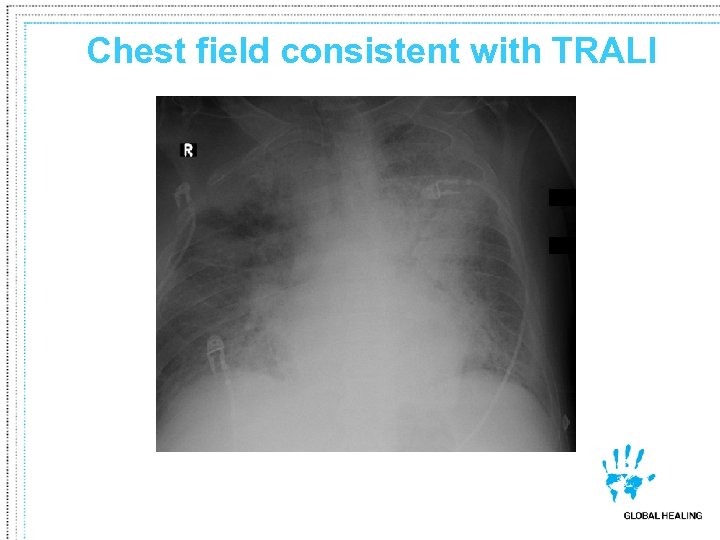 Chest field consistent with TRALI
Chest field consistent with TRALI
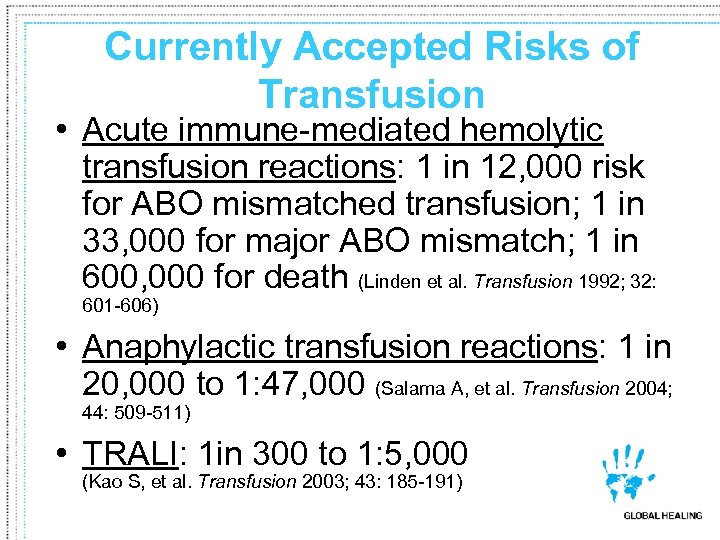 Currently Accepted Risks of Transfusion • Acute immune-mediated hemolytic transfusion reactions: 1 in 12, 000 risk for ABO mismatched transfusion; 1 in 33, 000 for major ABO mismatch; 1 in 600, 000 for death (Linden et al. Transfusion 1992; 32: 601 -606) • Anaphylactic transfusion reactions: 1 in 20, 000 to 1: 47, 000 (Salama A, et al. Transfusion 2004; 44: 509 -511) • TRALI: 1 in 300 to 1: 5, 000 (Kao S, et al. Transfusion 2003; 43: 185 -191)
Currently Accepted Risks of Transfusion • Acute immune-mediated hemolytic transfusion reactions: 1 in 12, 000 risk for ABO mismatched transfusion; 1 in 33, 000 for major ABO mismatch; 1 in 600, 000 for death (Linden et al. Transfusion 1992; 32: 601 -606) • Anaphylactic transfusion reactions: 1 in 20, 000 to 1: 47, 000 (Salama A, et al. Transfusion 2004; 44: 509 -511) • TRALI: 1 in 300 to 1: 5, 000 (Kao S, et al. Transfusion 2003; 43: 185 -191)
 Febrile Non-Hemolytic Reactions • Presentation: temperature > 1° C with no other explanations (sometimes with chills and rigors) • Causes • Reaction between recipient antibodies and donor WBCs or … • Production of cytokines during product storage • Treatment: Give antipyretics & symptomatic relief • Prevention: Pre-storage leukoreduction of blood
Febrile Non-Hemolytic Reactions • Presentation: temperature > 1° C with no other explanations (sometimes with chills and rigors) • Causes • Reaction between recipient antibodies and donor WBCs or … • Production of cytokines during product storage • Treatment: Give antipyretics & symptomatic relief • Prevention: Pre-storage leukoreduction of blood
 Allergic Transfusion Reactions • Cause: Unidentified (usually) plasma-soluble substances in donor blood reacting with recipient Ig. E • Presentation: Local erythema, hives, urticaria, (generally without other effects) • Treatment: Antihistamine (sometimes you may even restart transfusion) • Prevention: Pre-treatment with antihistamine or (very rarely) washing of cellular blood products
Allergic Transfusion Reactions • Cause: Unidentified (usually) plasma-soluble substances in donor blood reacting with recipient Ig. E • Presentation: Local erythema, hives, urticaria, (generally without other effects) • Treatment: Antihistamine (sometimes you may even restart transfusion) • Prevention: Pre-treatment with antihistamine or (very rarely) washing of cellular blood products
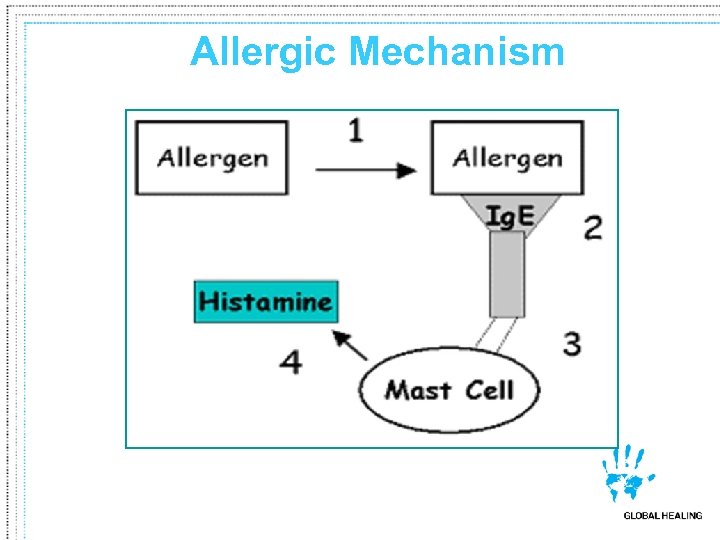 Allergic Mechanism
Allergic Mechanism
 Circulatory Overload • Cause: Poor patient tolerance for rapid increases in blood volume • Presentation: Dyspnea, severe headache, peripheral edema, rapid increase in systolic BP • Treatment: Sit patient up (if possible); diurese; give O 2; very rarely dialyze or even phlebotomize • Prevention: Transfuse in smallest volume increments possible, as slowly as possible
Circulatory Overload • Cause: Poor patient tolerance for rapid increases in blood volume • Presentation: Dyspnea, severe headache, peripheral edema, rapid increase in systolic BP • Treatment: Sit patient up (if possible); diurese; give O 2; very rarely dialyze or even phlebotomize • Prevention: Transfuse in smallest volume increments possible, as slowly as possible
 Other Acute Transfusion Reactions • • • Hypothermia and arrhythmias Citrate toxicity and hypocalcemia Air embolism Decreased 2, 3 -DPG levels Hyperkalemia
Other Acute Transfusion Reactions • • • Hypothermia and arrhythmias Citrate toxicity and hypocalcemia Air embolism Decreased 2, 3 -DPG levels Hyperkalemia
 Delayed Transfusion Reactions
Delayed Transfusion Reactions
 Case Study • 30 -year-old male; MVA; O-negative • Transfused with 43 RBCs approximately 5 weeks ago • Now has 3+ DAT, gradual decline in hemoglobin, no new serum antibody • Diagnosis and Management? ? ?
Case Study • 30 -year-old male; MVA; O-negative • Transfused with 43 RBCs approximately 5 weeks ago • Now has 3+ DAT, gradual decline in hemoglobin, no new serum antibody • Diagnosis and Management? ? ?
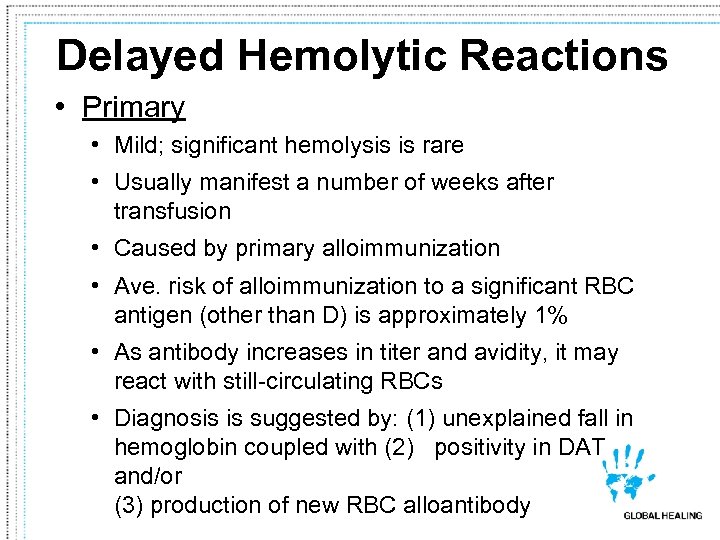 Delayed Hemolytic Reactions • Primary • Mild; significant hemolysis is rare • Usually manifest a number of weeks after transfusion • Caused by primary alloimmunization • Ave. risk of alloimmunization to a significant RBC antigen (other than D) is approximately 1% • As antibody increases in titer and avidity, it may react with still-circulating RBCs • Diagnosis is suggested by: (1) unexplained fall in hemoglobin coupled with (2) positivity in DAT and/or (3) production of new RBC alloantibody
Delayed Hemolytic Reactions • Primary • Mild; significant hemolysis is rare • Usually manifest a number of weeks after transfusion • Caused by primary alloimmunization • Ave. risk of alloimmunization to a significant RBC antigen (other than D) is approximately 1% • As antibody increases in titer and avidity, it may react with still-circulating RBCs • Diagnosis is suggested by: (1) unexplained fall in hemoglobin coupled with (2) positivity in DAT and/or (3) production of new RBC alloantibody
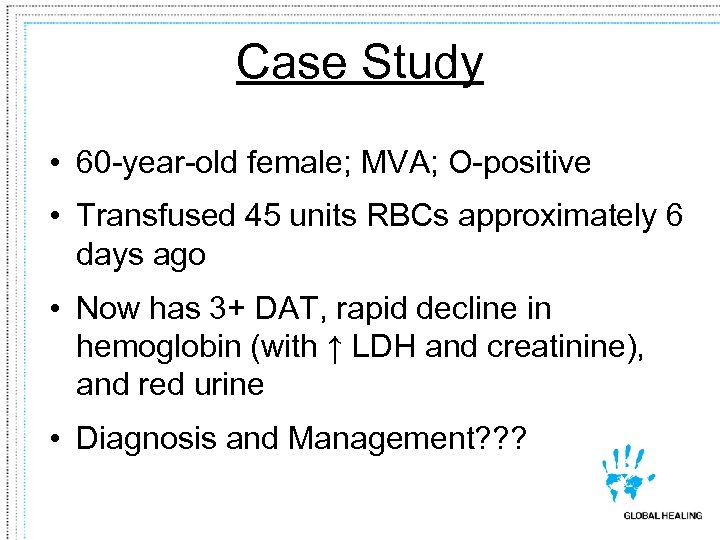 Case Study • 60 -year-old female; MVA; O-positive • Transfused 45 units RBCs approximately 6 days ago • Now has 3+ DAT, rapid decline in hemoglobin (with ↑ LDH and creatinine), and red urine • Diagnosis and Management? ? ?
Case Study • 60 -year-old female; MVA; O-positive • Transfused 45 units RBCs approximately 6 days ago • Now has 3+ DAT, rapid decline in hemoglobin (with ↑ LDH and creatinine), and red urine • Diagnosis and Management? ? ?
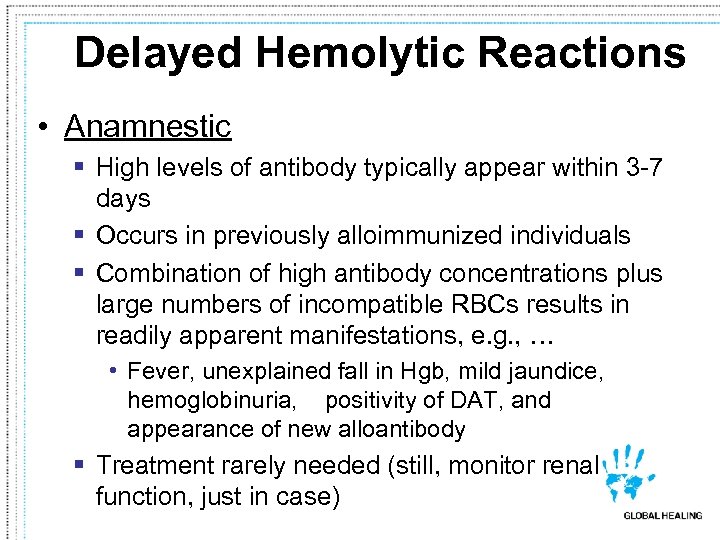 Delayed Hemolytic Reactions • Anamnestic § High levels of antibody typically appear within 3 -7 days § Occurs in previously alloimmunized individuals § Combination of high antibody concentrations plus large numbers of incompatible RBCs results in readily apparent manifestations, e. g. , … • Fever, unexplained fall in Hgb, mild jaundice, hemoglobinuria, positivity of DAT, and appearance of new alloantibody § Treatment rarely needed (still, monitor renal function, just in case)
Delayed Hemolytic Reactions • Anamnestic § High levels of antibody typically appear within 3 -7 days § Occurs in previously alloimmunized individuals § Combination of high antibody concentrations plus large numbers of incompatible RBCs results in readily apparent manifestations, e. g. , … • Fever, unexplained fall in Hgb, mild jaundice, hemoglobinuria, positivity of DAT, and appearance of new alloantibody § Treatment rarely needed (still, monitor renal function, just in case)
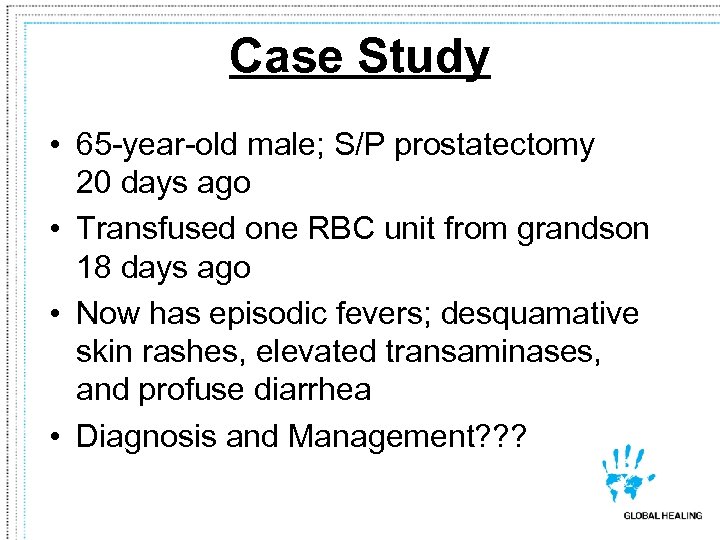 Case Study • 65 -year-old male; S/P prostatectomy 20 days ago • Transfused one RBC unit from grandson 18 days ago • Now has episodic fevers; desquamative skin rashes, elevated transaminases, and profuse diarrhea • Diagnosis and Management? ? ?
Case Study • 65 -year-old male; S/P prostatectomy 20 days ago • Transfused one RBC unit from grandson 18 days ago • Now has episodic fevers; desquamative skin rashes, elevated transaminases, and profuse diarrhea • Diagnosis and Management? ? ?
 Transfusion-Associated Graft-Versus-Host Disease • Rare; usually fatal • Generally affects severely immunocompromised patients (exception to be discussed) • Mechanism: Donor T cells engraft in recipient and react against his/her “foreign” tissues • Clinical syndrome includes: Fever, skin rash, hepatitis, diarrhea, bone marrow suppression, infection, bleeding • Prevention: Irradiation of blood components with 25 Gy
Transfusion-Associated Graft-Versus-Host Disease • Rare; usually fatal • Generally affects severely immunocompromised patients (exception to be discussed) • Mechanism: Donor T cells engraft in recipient and react against his/her “foreign” tissues • Clinical syndrome includes: Fever, skin rash, hepatitis, diarrhea, bone marrow suppression, infection, bleeding • Prevention: Irradiation of blood components with 25 Gy
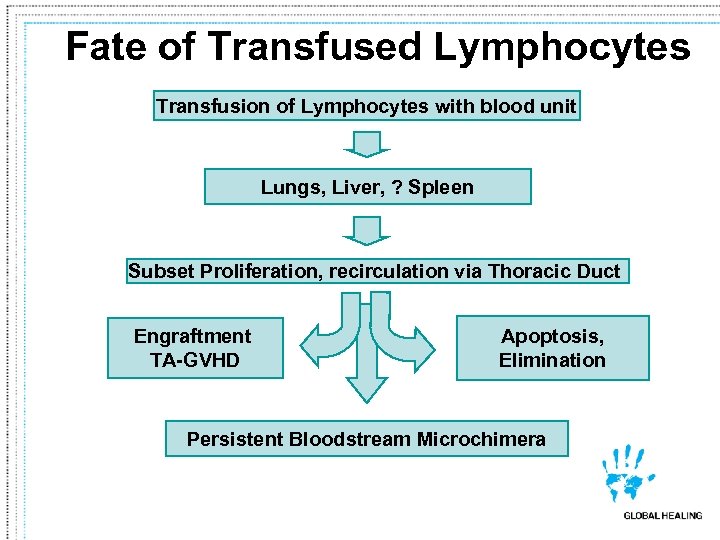 Fate of Transfused Lymphocytes Transfusion of Lymphocytes with blood unit Lungs, Liver, ? Spleen Subset Proliferation, recirculation via Thoracic Duct Engraftment TA-GVHD Apoptosis, Elimination Persistent Bloodstream Microchimera
Fate of Transfused Lymphocytes Transfusion of Lymphocytes with blood unit Lungs, Liver, ? Spleen Subset Proliferation, recirculation via Thoracic Duct Engraftment TA-GVHD Apoptosis, Elimination Persistent Bloodstream Microchimera
 TA-GVHD Diagnosis • Skin – Degeneration of epidermal basal layer with vacuolization – Dermal-epidermal layer separation and bullae formation – Mononuclear cell infiltration of upper dermis – Hyperkeratosis
TA-GVHD Diagnosis • Skin – Degeneration of epidermal basal layer with vacuolization – Dermal-epidermal layer separation and bullae formation – Mononuclear cell infiltration of upper dermis – Hyperkeratosis
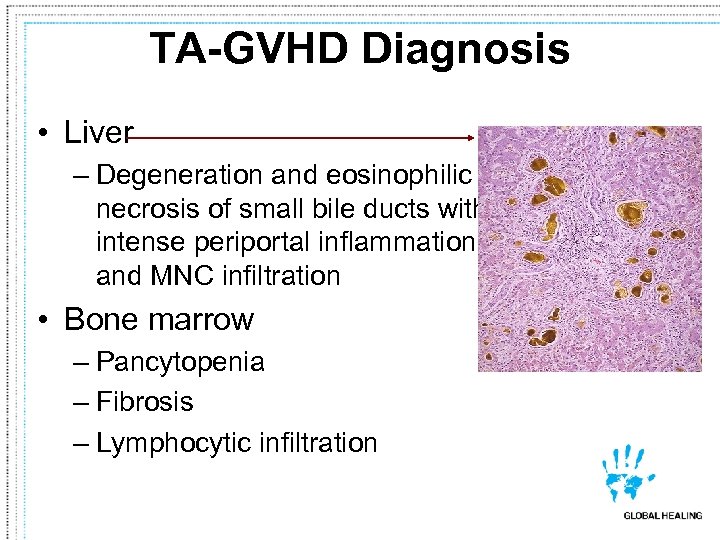 TA-GVHD Diagnosis • Liver – Degeneration and eosinophilic necrosis of small bile ducts with intense periportal inflammation and MNC infiltration • Bone marrow – Pancytopenia – Fibrosis – Lymphocytic infiltration
TA-GVHD Diagnosis • Liver – Degeneration and eosinophilic necrosis of small bile ducts with intense periportal inflammation and MNC infiltration • Bone marrow – Pancytopenia – Fibrosis – Lymphocytic infiltration
 Indications for Irradiated Blood • • Pre-/post-hematopoietic stem cell transplant Hodgkin’s disease Low birth weight neonate (< 1, 200 g) Neonatal exchange transfusion Intrauterine fetal transfusion Related donor HLA-matched donor or crossmatchcompatible platelet donor • Treatment with either fludarabine or 2 -CDA
Indications for Irradiated Blood • • Pre-/post-hematopoietic stem cell transplant Hodgkin’s disease Low birth weight neonate (< 1, 200 g) Neonatal exchange transfusion Intrauterine fetal transfusion Related donor HLA-matched donor or crossmatchcompatible platelet donor • Treatment with either fludarabine or 2 -CDA
 Case Study • 40 -year-old female; S/P mastectomy • Transfused 1 unit RBCs 8 days ago • Yesterday, platelet count ↓’d from 258 K/u. L to 4 K/u. L • Diagnosis and Management? ? ?
Case Study • 40 -year-old female; S/P mastectomy • Transfused 1 unit RBCs 8 days ago • Yesterday, platelet count ↓’d from 258 K/u. L to 4 K/u. L • Diagnosis and Management? ? ?
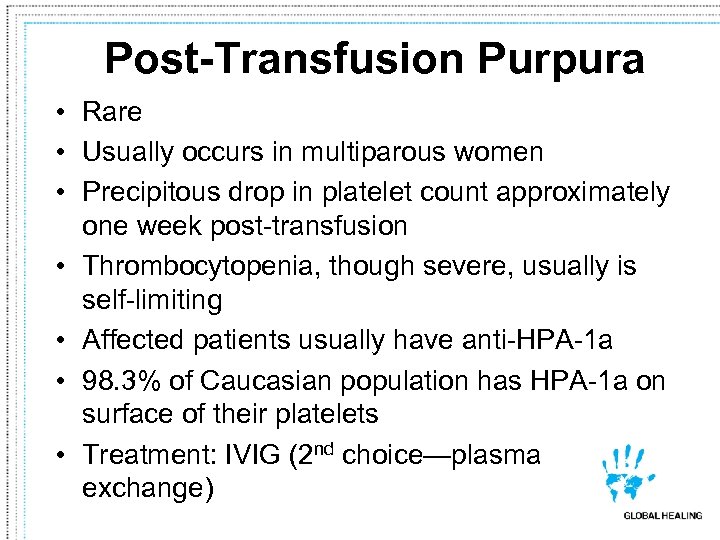 Post-Transfusion Purpura • Rare • Usually occurs in multiparous women • Precipitous drop in platelet count approximately one week post-transfusion • Thrombocytopenia, though severe, usually is self-limiting • Affected patients usually have anti-HPA-1 a • 98. 3% of Caucasian population has HPA-1 a on surface of their platelets • Treatment: IVIG (2 nd choice—plasma exchange)
Post-Transfusion Purpura • Rare • Usually occurs in multiparous women • Precipitous drop in platelet count approximately one week post-transfusion • Thrombocytopenia, though severe, usually is self-limiting • Affected patients usually have anti-HPA-1 a • 98. 3% of Caucasian population has HPA-1 a on surface of their platelets • Treatment: IVIG (2 nd choice—plasma exchange)
 Other Delayed Transfusion Reactions • Iron Overload • Immunomodulation • Other?
Other Delayed Transfusion Reactions • Iron Overload • Immunomodulation • Other?
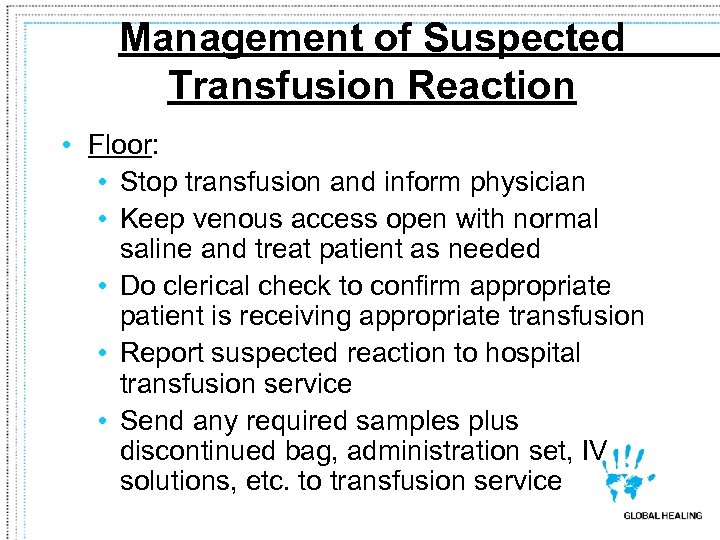 Management of Suspected Transfusion Reaction • Floor: • Stop transfusion and inform physician • Keep venous access open with normal saline and treat patient as needed • Do clerical check to confirm appropriate patient is receiving appropriate transfusion • Report suspected reaction to hospital transfusion service • Send any required samples plus discontinued bag, administration set, IV solutions, etc. to transfusion service
Management of Suspected Transfusion Reaction • Floor: • Stop transfusion and inform physician • Keep venous access open with normal saline and treat patient as needed • Do clerical check to confirm appropriate patient is receiving appropriate transfusion • Report suspected reaction to hospital transfusion service • Send any required samples plus discontinued bag, administration set, IV solutions, etc. to transfusion service
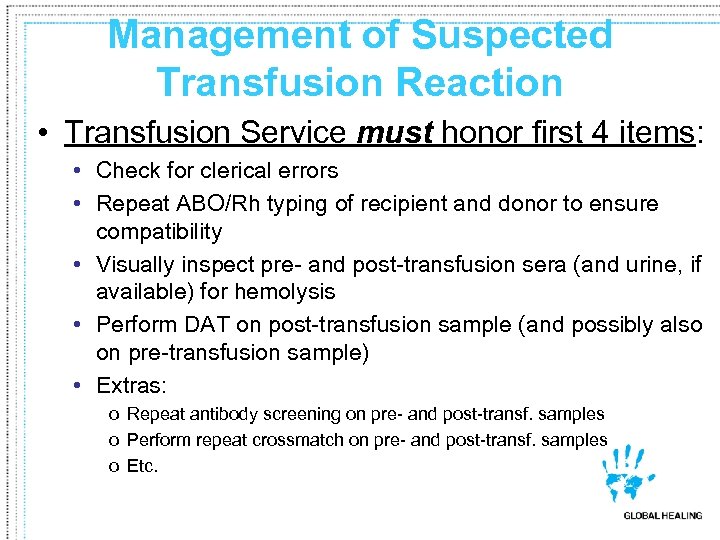 Management of Suspected Transfusion Reaction • Transfusion Service must honor first 4 items: • Check for clerical errors • Repeat ABO/Rh typing of recipient and donor to ensure compatibility • Visually inspect pre- and post-transfusion sera (and urine, if available) for hemolysis • Perform DAT on post-transfusion sample (and possibly also on pre-transfusion sample) • Extras: o Repeat antibody screening on pre- and post-transf. samples o Perform repeat crossmatch on pre- and post-transf. samples o Etc.
Management of Suspected Transfusion Reaction • Transfusion Service must honor first 4 items: • Check for clerical errors • Repeat ABO/Rh typing of recipient and donor to ensure compatibility • Visually inspect pre- and post-transfusion sera (and urine, if available) for hemolysis • Perform DAT on post-transfusion sample (and possibly also on pre-transfusion sample) • Extras: o Repeat antibody screening on pre- and post-transf. samples o Perform repeat crossmatch on pre- and post-transf. samples o Etc.
 Blood Banking Review/Updates • Miscellaneous Transfusion Complications • Is There a Problem with Older RBCs? • Septic Transfusion Reactions Revisited • FDA-Reported Transfusion-Related Fatalities for 2005 -06
Blood Banking Review/Updates • Miscellaneous Transfusion Complications • Is There a Problem with Older RBCs? • Septic Transfusion Reactions Revisited • FDA-Reported Transfusion-Related Fatalities for 2005 -06
 Is There a Problem with Older RBCs? • Study Methods § Retrospective review of 6002 coronary artery bypass graft/heart valve patients (1998 -2006). o 2872 received 8802 RBC units < 14 days old (median RBC age = 11 days). o 3130 received 10782 RBC units > 14 days old (median RBC age = 20 days). § Outcomes and survival rates were assessed C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
Is There a Problem with Older RBCs? • Study Methods § Retrospective review of 6002 coronary artery bypass graft/heart valve patients (1998 -2006). o 2872 received 8802 RBC units < 14 days old (median RBC age = 11 days). o 3130 received 10782 RBC units > 14 days old (median RBC age = 20 days). § Outcomes and survival rates were assessed C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
 Is There a Problem with Older RBCs? Study Results Outcome RBCs < 14 Days RBCs > 14 Days In-Hospital Mortality 1. 7% 2. 8% Intubation > 72 Hours 5. 6% 9. 7% Renal Failure 1. 6% 2. 7% Sepsis/Septicemia 2. 8% 4. 0% 1 -Year Mortality 7. 4% 11. 0% p = 0. 03 to < 0. 001 C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
Is There a Problem with Older RBCs? Study Results Outcome RBCs < 14 Days RBCs > 14 Days In-Hospital Mortality 1. 7% 2. 8% Intubation > 72 Hours 5. 6% 9. 7% Renal Failure 1. 6% 2. 7% Sepsis/Septicemia 2. 8% 4. 0% 1 -Year Mortality 7. 4% 11. 0% p = 0. 03 to < 0. 001 C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
 Is There a Problem with Older RBCs? • Caveats to Study – It was a retrospective study. – The authors assessed a very specific population of older heart surgery patients (i. e. , results may not generalize to other populations). – A prospective randomized clinical trial is needed to confirm or refute these findings. C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
Is There a Problem with Older RBCs? • Caveats to Study – It was a retrospective study. – The authors assessed a very specific population of older heart surgery patients (i. e. , results may not generalize to other populations). – A prospective randomized clinical trial is needed to confirm or refute these findings. C. J. Koch, et al. “Duration of Red-Cell Storage and Complications After Cardiac Surgery. NEJM. 2008; 358: 1229 -39.
 Septic Transfusion Reactions • Methods § Screened 43, 230 platelets for bacterial contamination using large-volume, automated culture method on samples obtained 24 hours post-donation. § Also, 4 -day-old and outdated units were re-cultured. • Results § 35 (0. 08%) of initial screenings were positive § Results of Repeat Cultures … o 18 of 8, 282 (0. 22%) expired units were positive o 4 of 3, 310 (0. 12%) 4 -day-old units were positive § Overall sensitivity of initial screening test was 29. 2% W. G. Murphy, et al. “Screening Platelet Concentrates for Bacterial Contamination. ” Vox Sang. 2008 [E-pub ahead of print].
Septic Transfusion Reactions • Methods § Screened 43, 230 platelets for bacterial contamination using large-volume, automated culture method on samples obtained 24 hours post-donation. § Also, 4 -day-old and outdated units were re-cultured. • Results § 35 (0. 08%) of initial screenings were positive § Results of Repeat Cultures … o 18 of 8, 282 (0. 22%) expired units were positive o 4 of 3, 310 (0. 12%) 4 -day-old units were positive § Overall sensitivity of initial screening test was 29. 2% W. G. Murphy, et al. “Screening Platelet Concentrates for Bacterial Contamination. ” Vox Sang. 2008 [E-pub ahead of print].
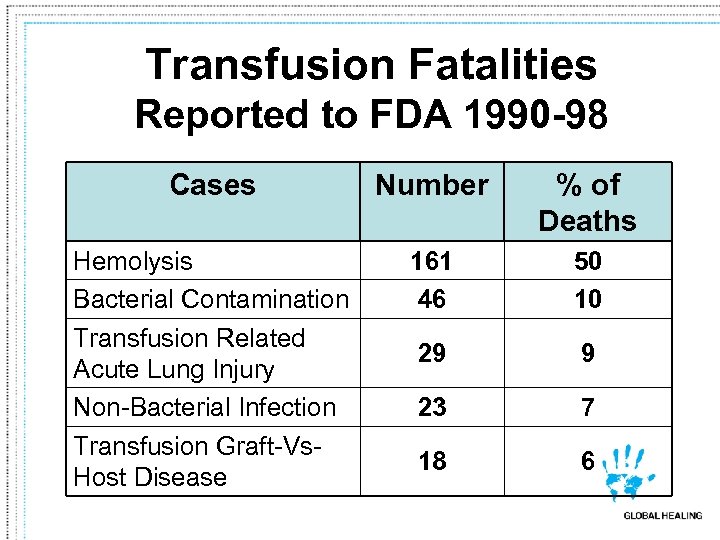 Transfusion Fatalities Reported to FDA 1990 -98 Cases Number % of Deaths Hemolysis Bacterial Contamination Transfusion Related Acute Lung Injury Non-Bacterial Infection Transfusion Graft-Vs. Host Disease 161 46 50 10 29 9 23 7 18 6 From Lee JH. FDA Workshop on Bacterial Contamination of Platelets, 1999
Transfusion Fatalities Reported to FDA 1990 -98 Cases Number % of Deaths Hemolysis Bacterial Contamination Transfusion Related Acute Lung Injury Non-Bacterial Infection Transfusion Graft-Vs. Host Disease 161 46 50 10 29 9 23 7 18 6 From Lee JH. FDA Workshop on Bacterial Contamination of Platelets, 1999
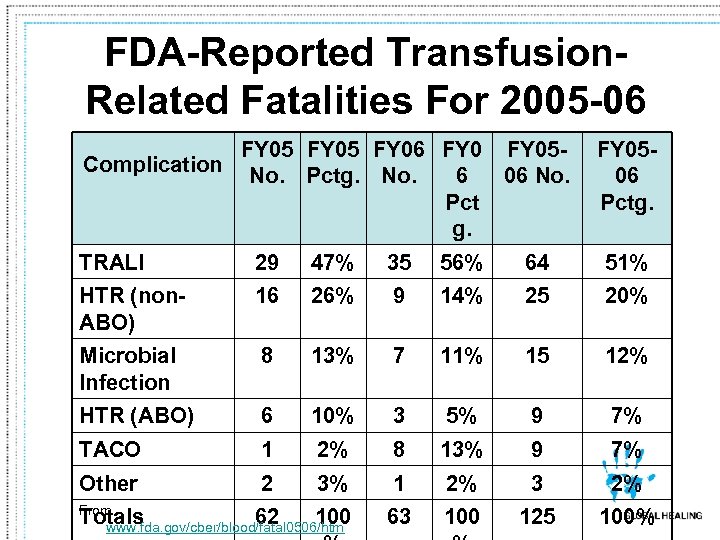 FDA-Reported Transfusion. Related Fatalities For 2005 -06 Complication FY 05 FY 06 FY 05 No. Pctg. No. 6 06 No. Pct g. FY 0506 Pctg. TRALI 29 47% 35 56% 64 51% HTR (non. ABO) 16 26% 9 14% 25 20% Microbial Infection 8 13% 7 11% 15 12% HTR (ABO) 6 10% 3 5% 9 7% TACO 1 2% 8 13% 9 7% Other 2 3% 1 2% 3 2% 63 100 125 100% From Totals 62 100 www. fda. gov/cber/blood/fatal 0506/htm
FDA-Reported Transfusion. Related Fatalities For 2005 -06 Complication FY 05 FY 06 FY 05 No. Pctg. No. 6 06 No. Pct g. FY 0506 Pctg. TRALI 29 47% 35 56% 64 51% HTR (non. ABO) 16 26% 9 14% 25 20% Microbial Infection 8 13% 7 11% 15 12% HTR (ABO) 6 10% 3 5% 9 7% TACO 1 2% 8 13% 9 7% Other 2 3% 1 2% 3 2% 63 100 125 100% From Totals 62 100 www. fda. gov/cber/blood/fatal 0506/htm
 Transfusion Reactions Summary – A Case Study-Based Focus on… • Acute Transfusion Reactions • Delayed Transfusion Reactions • Evaluation/Management of Suspected Transfusion Reactions • Miscellaneous Transfusion Complications
Transfusion Reactions Summary – A Case Study-Based Focus on… • Acute Transfusion Reactions • Delayed Transfusion Reactions • Evaluation/Management of Suspected Transfusion Reactions • Miscellaneous Transfusion Complications
 Q & A? Thank you!
Q & A? Thank you!
 Please donate blood. . . From Action Comics # 403 (1970) …You never know whose life you might save.
Please donate blood. . . From Action Comics # 403 (1970) …You never know whose life you might save.


