a3e47dcdaacf2370a7fbdd490f4b57cd.ppt
- Количество слайдов: 52
 DIAGNOSIS AND MANAGEMENT OF YOUNG WOMEN WITH TURNER SYNDROME (TS) Carolyn Bondy, MD National Institute of Child Health, National Institutes of Health (NIH) Center for Human Reproduction April 9, 2013
DIAGNOSIS AND MANAGEMENT OF YOUNG WOMEN WITH TURNER SYNDROME (TS) Carolyn Bondy, MD National Institute of Child Health, National Institutes of Health (NIH) Center for Human Reproduction April 9, 2013
 I have no declarations and no conflict of interest in regards to this presentation
I have no declarations and no conflict of interest in regards to this presentation
 Objectives • • Criteria for diagnosis of Turner syndrome (TS) Epidemiology and chromosomal origins Diagnostic tests and screening evaluation Potential for endogenous fertility Outcomes of spontaneous and OD pregnancies Medical management Psychosocial concerns X chromosome genomic imprinting and ischemic heart disease
Objectives • • Criteria for diagnosis of Turner syndrome (TS) Epidemiology and chromosomal origins Diagnostic tests and screening evaluation Potential for endogenous fertility Outcomes of spontaneous and OD pregnancies Medical management Psychosocial concerns X chromosome genomic imprinting and ischemic heart disease
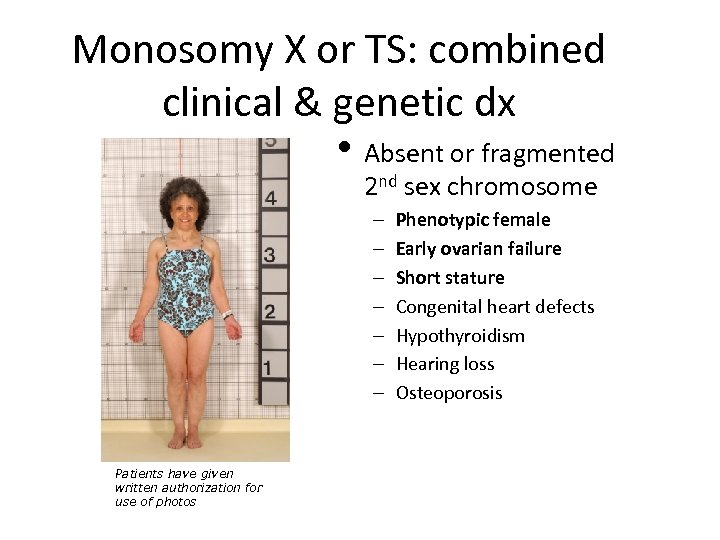 Monosomy X or TS: combined clinical & genetic dx • Absent or fragmented 2 nd sex chromosome – – – – Patients have given written authorization for use of photos Phenotypic female Early ovarian failure Short stature Congenital heart defects Hypothyroidism Hearing loss Osteoporosis
Monosomy X or TS: combined clinical & genetic dx • Absent or fragmented 2 nd sex chromosome – – – – Patients have given written authorization for use of photos Phenotypic female Early ovarian failure Short stature Congenital heart defects Hypothyroidism Hearing loss Osteoporosis
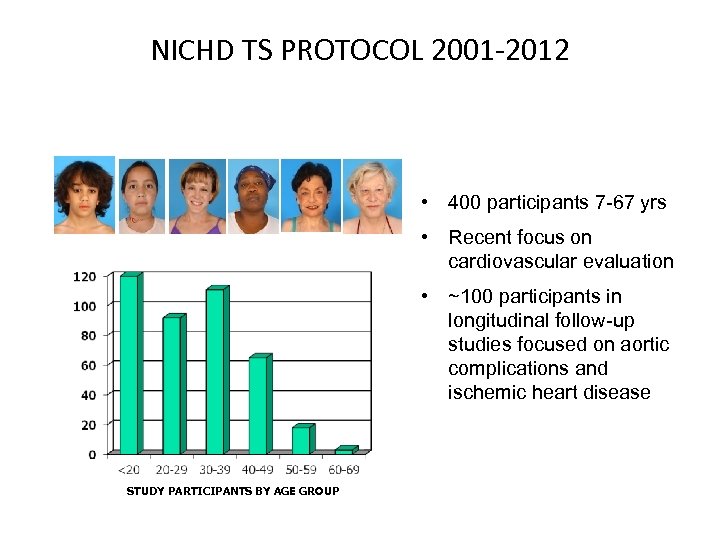 NICHD TS PROTOCOL 2001 -2012 • 400 participants 7 -67 yrs • Recent focus on cardiovascular evaluation • ~100 participants in longitudinal follow-up studies focused on aortic complications and ischemic heart disease STUDY PARTICIPANTS BY AGE GROUP
NICHD TS PROTOCOL 2001 -2012 • 400 participants 7 -67 yrs • Recent focus on cardiovascular evaluation • ~100 participants in longitudinal follow-up studies focused on aortic complications and ischemic heart disease STUDY PARTICIPANTS BY AGE GROUP
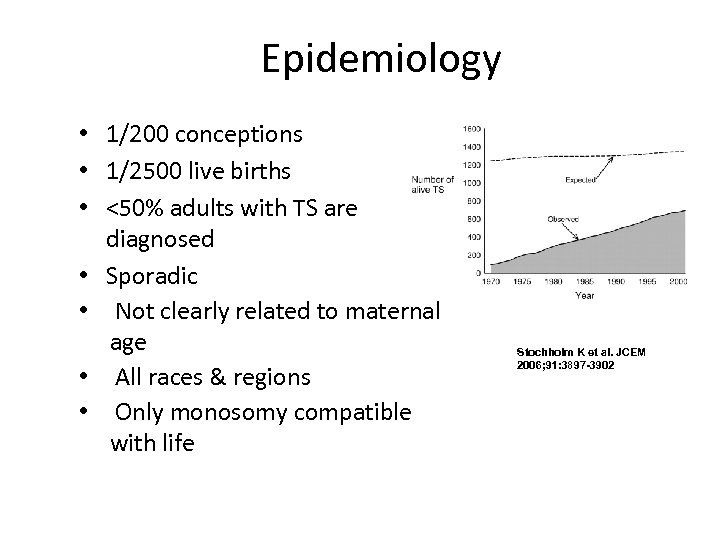 Epidemiology • 1/200 conceptions • 1/2500 live births • <50% adults with TS are diagnosed • Sporadic • Not clearly related to maternal age • All races & regions • Only monosomy compatible with life Stochholm K et al. JCEM 2006; 91: 3897 -3902
Epidemiology • 1/200 conceptions • 1/2500 live births • <50% adults with TS are diagnosed • Sporadic • Not clearly related to maternal age • All races & regions • Only monosomy compatible with life Stochholm K et al. JCEM 2006; 91: 3897 -3902
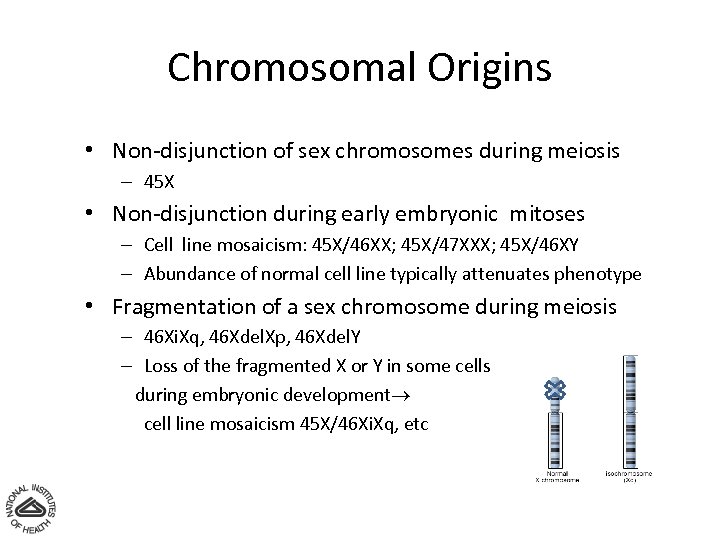 Chromosomal Origins • Non-disjunction of sex chromosomes during meiosis – 45 X • Non-disjunction during early embryonic mitoses – Cell line mosaicism: 45 X/46 XX; 45 X/47 XXX; 45 X/46 XY – Abundance of normal cell line typically attenuates phenotype • Fragmentation of a sex chromosome during meiosis – 46 Xi. Xq, 46 Xdel. Xp, 46 Xdel. Y – Loss of the fragmented X or Y in some cells during embryonic development cell line mosaicism 45 X/46 Xi. Xq, etc
Chromosomal Origins • Non-disjunction of sex chromosomes during meiosis – 45 X • Non-disjunction during early embryonic mitoses – Cell line mosaicism: 45 X/46 XX; 45 X/47 XXX; 45 X/46 XY – Abundance of normal cell line typically attenuates phenotype • Fragmentation of a sex chromosome during meiosis – 46 Xi. Xq, 46 Xdel. Xp, 46 Xdel. Y – Loss of the fragmented X or Y in some cells during embryonic development cell line mosaicism 45 X/46 Xi. Xq, etc
 The Lyon Hypothesis • In cells with multiple Xchromosomes, all but one are inactivated during embryogenesis • X-inactivation leads to clumped chromatin, termed Barr bodies, considered inert (Lyonization) • So is the 2 nd X totally superfluous?
The Lyon Hypothesis • In cells with multiple Xchromosomes, all but one are inactivated during embryogenesis • X-inactivation leads to clumped chromatin, termed Barr bodies, considered inert (Lyonization) • So is the 2 nd X totally superfluous?
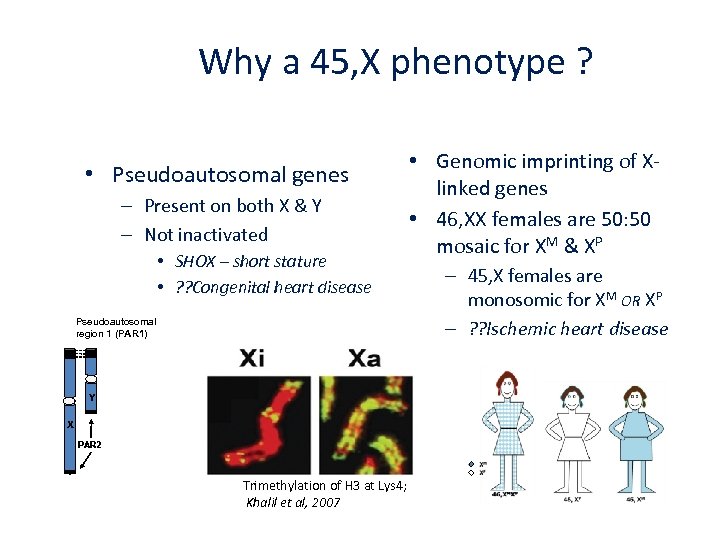 Why a 45, X phenotype ? • Pseudoautosomal genes – Present on both X & Y – Not inactivated • SHOX – short stature • ? ? Congenital heart disease Pseudoautosomal region 1 (PAR 1) Y X PAR 2 Trimethylation of H 3 at Lys 4; Khalil et al, 2007 • Genomic imprinting of Xlinked genes • 46, XX females are 50: 50 mosaic for XM & XP – 45, X females are monosomic for XM OR XP – ? ? Ischemic heart disease
Why a 45, X phenotype ? • Pseudoautosomal genes – Present on both X & Y – Not inactivated • SHOX – short stature • ? ? Congenital heart disease Pseudoautosomal region 1 (PAR 1) Y X PAR 2 Trimethylation of H 3 at Lys 4; Khalil et al, 2007 • Genomic imprinting of Xlinked genes • 46, XX females are 50: 50 mosaic for XM & XP – 45, X females are monosomic for XM OR XP – ? ? Ischemic heart disease
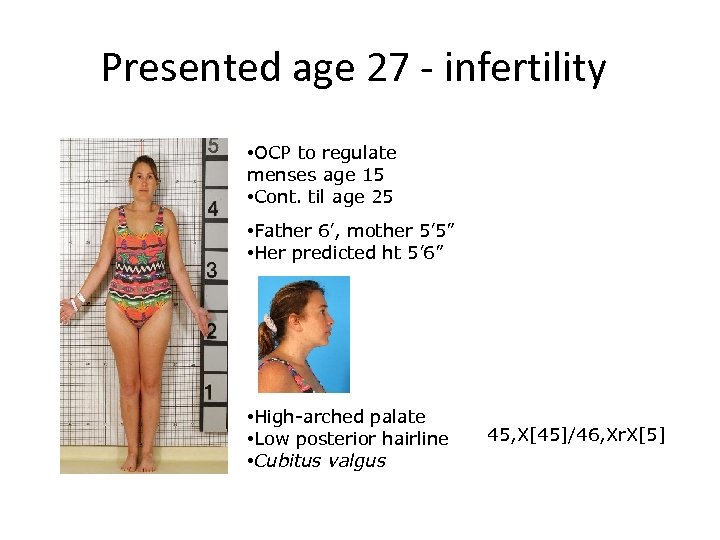 Presented age 27 - infertility • OCP to regulate menses age 15 • Cont. til age 25 • Father 6’, mother 5’ 5” • Her predicted ht 5’ 6” • High-arched palate • Low posterior hairline • Cubitus valgus 45, X[45]/46, Xr. X[5]
Presented age 27 - infertility • OCP to regulate menses age 15 • Cont. til age 25 • Father 6’, mother 5’ 5” • Her predicted ht 5’ 6” • High-arched palate • Low posterior hairline • Cubitus valgus 45, X[45]/46, Xr. X[5]
 Clues from PMH, FH and PE • Chronic otitis, shorter than sisters, less than mid-parental height (F-5” + M)/2; history Coarc repair, other CHD • Mx nevi, high-arched palate, short 4 th MCP or MTP, short or web neck, low hair line, low set ears
Clues from PMH, FH and PE • Chronic otitis, shorter than sisters, less than mid-parental height (F-5” + M)/2; history Coarc repair, other CHD • Mx nevi, high-arched palate, short 4 th MCP or MTP, short or web neck, low hair line, low set ears
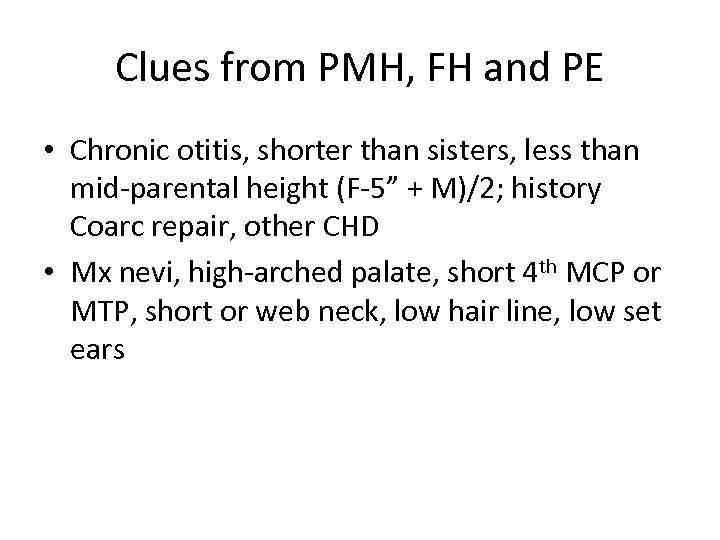
 To confirm the diagnosis of TS 20 -30 cell peripheral blood karyotype is gold standard 3 -5 ml blood in heparinized tube at room T˚ Cytogenetics referral lab 2 -3 wk turnaround & costly New methods Whole genome snp chips
To confirm the diagnosis of TS 20 -30 cell peripheral blood karyotype is gold standard 3 -5 ml blood in heparinized tube at room T˚ Cytogenetics referral lab 2 -3 wk turnaround & costly New methods Whole genome snp chips
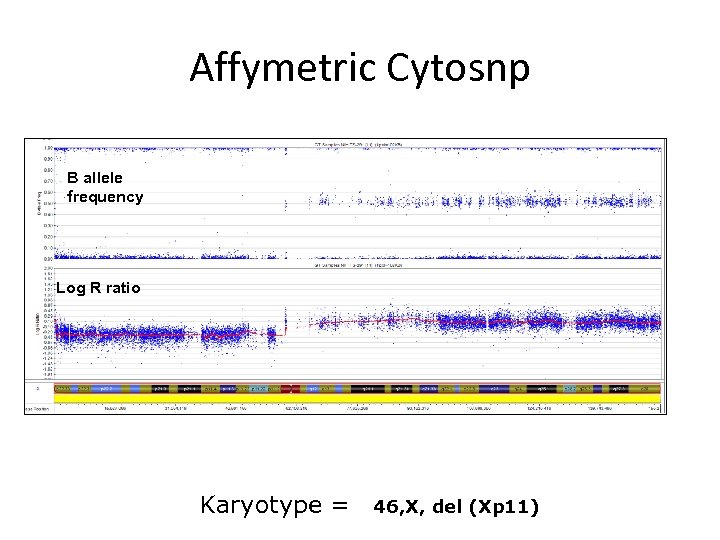 Affymetric Cytosnp B allele frequency Log R ratio Karyotype = 46, X, del (Xp 11)
Affymetric Cytosnp B allele frequency Log R ratio Karyotype = 46, X, del (Xp 11)
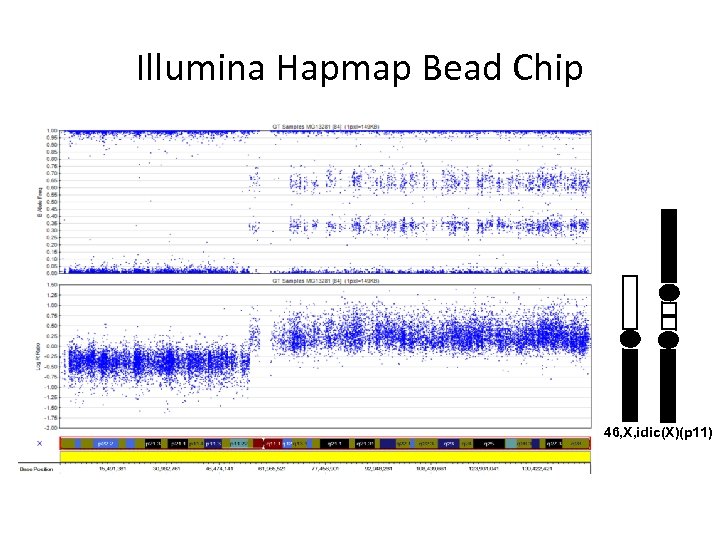 Illumina Hapmap Bead Chip 46, X, idic(X)(p 11)
Illumina Hapmap Bead Chip 46, X, idic(X)(p 11)
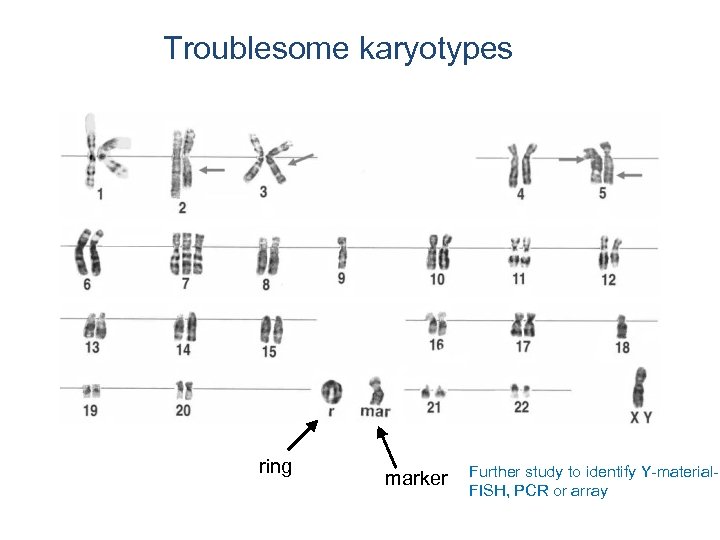 Troublesome karyotypes ring marker Further study to identify Y-material. FISH, PCR or array
Troublesome karyotypes ring marker Further study to identify Y-material. FISH, PCR or array
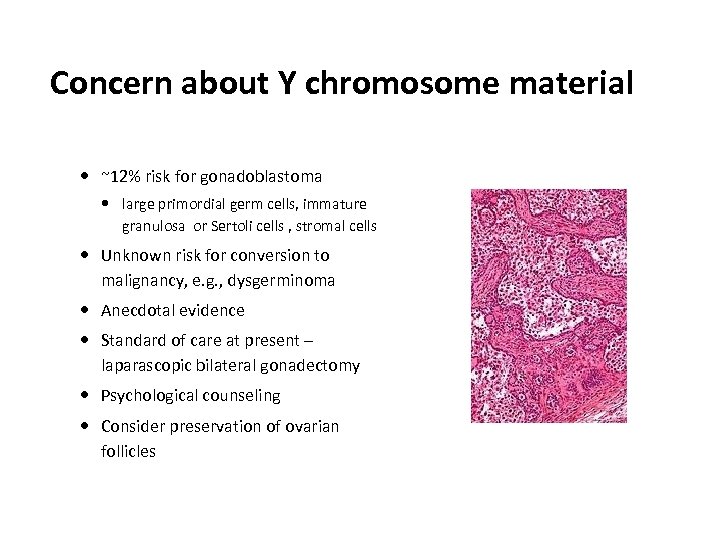 Concern about Y chromosome material ~12% risk for gonadoblastoma large primordial germ cells, immature granulosa or Sertoli cells , stromal cells Unknown risk for conversion to malignancy, e. g. , dysgerminoma Anecdotal evidence Standard of care at present – laparascopic bilateral gonadectomy Psychological counseling Consider preservation of ovarian follicles
Concern about Y chromosome material ~12% risk for gonadoblastoma large primordial germ cells, immature granulosa or Sertoli cells , stromal cells Unknown risk for conversion to malignancy, e. g. , dysgerminoma Anecdotal evidence Standard of care at present – laparascopic bilateral gonadectomy Psychological counseling Consider preservation of ovarian follicles
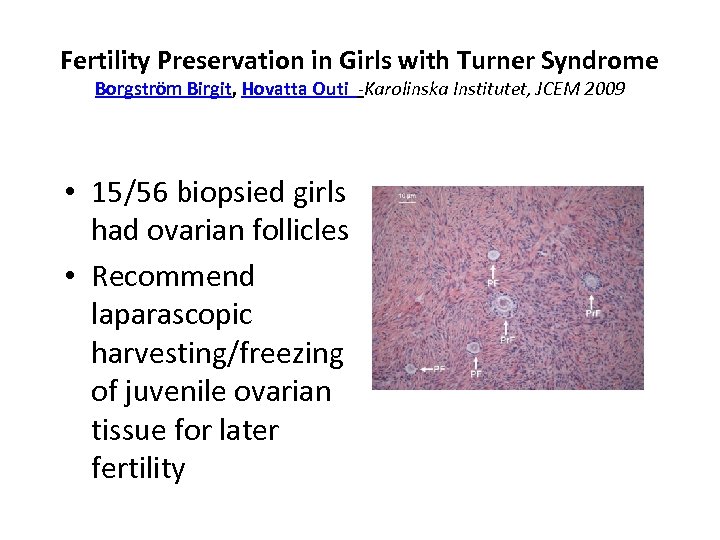 Fertility Preservation in Girls with Turner Syndrome Borgström Birgit, Hovatta Outi -Karolinska Institutet, JCEM 2009 • 15/56 biopsied girls had ovarian follicles • Recommend laparascopic harvesting/freezing of juvenile ovarian tissue for later fertility
Fertility Preservation in Girls with Turner Syndrome Borgström Birgit, Hovatta Outi -Karolinska Institutet, JCEM 2009 • 15/56 biopsied girls had ovarian follicles • Recommend laparascopic harvesting/freezing of juvenile ovarian tissue for later fertility
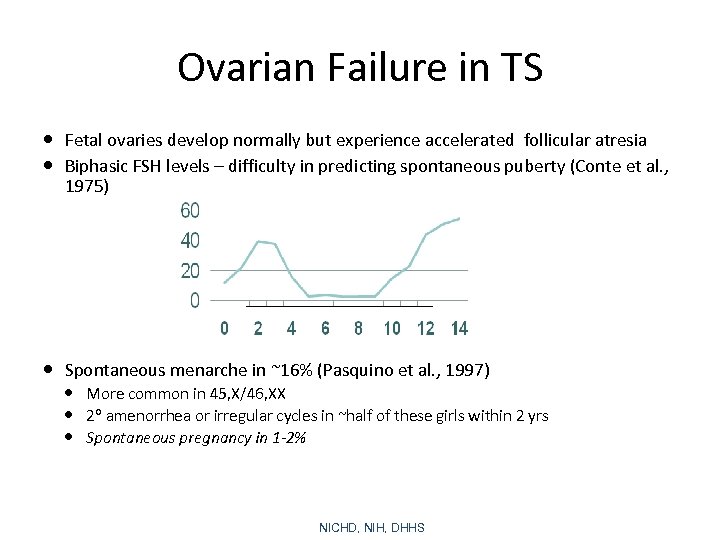 Ovarian Failure in TS Fetal ovaries develop normally but experience accelerated follicular atresia Biphasic FSH levels – difficulty in predicting spontaneous puberty (Conte et al. , 1975) Spontaneous menarche in ~16% (Pasquino et al. , 1997) More common in 45, X/46, XX 2 amenorrhea or irregular cycles in ~half of these girls within 2 yrs Spontaneous pregnancy in 1 -2% NICHD, NIH, DHHS
Ovarian Failure in TS Fetal ovaries develop normally but experience accelerated follicular atresia Biphasic FSH levels – difficulty in predicting spontaneous puberty (Conte et al. , 1975) Spontaneous menarche in ~16% (Pasquino et al. , 1997) More common in 45, X/46, XX 2 amenorrhea or irregular cycles in ~half of these girls within 2 yrs Spontaneous pregnancy in 1 -2% NICHD, NIH, DHHS
 Illustrative Case • Swedish woman with menarche and full pubertal development age 13, irregular menses • Premature menopause diagnosis ~age 32 • At least two unsuccessful IVF w/donated oocytes • Spontaneous pregnancy age 36 w/ NSVD • 2 nd spontaneous pregnancy age 38 – Htn, chest pain, aortic dissection 7 th month – Emergency C-section and aortic repair • Endocrine clinic- 45, X/46, X, del. Y—DX TS • Prophylactic gonadectomy age 40 Journal of Assisted Reproduction and Genetics 21; 229 -230,
Illustrative Case • Swedish woman with menarche and full pubertal development age 13, irregular menses • Premature menopause diagnosis ~age 32 • At least two unsuccessful IVF w/donated oocytes • Spontaneous pregnancy age 36 w/ NSVD • 2 nd spontaneous pregnancy age 38 – Htn, chest pain, aortic dissection 7 th month – Emergency C-section and aortic repair • Endocrine clinic- 45, X/46, X, del. Y—DX TS • Prophylactic gonadectomy age 40 Journal of Assisted Reproduction and Genetics 21; 229 -230,
 Comments… • Consider the diagnosis of TS – Hypergonadotropic hypogonadism • Do not assume infertility if Y chromosome material is detected – Oocyte preservation • Serious cardio complications in natural as well as ART pregnancies
Comments… • Consider the diagnosis of TS – Hypergonadotropic hypogonadism • Do not assume infertility if Y chromosome material is detected – Oocyte preservation • Serious cardio complications in natural as well as ART pregnancies
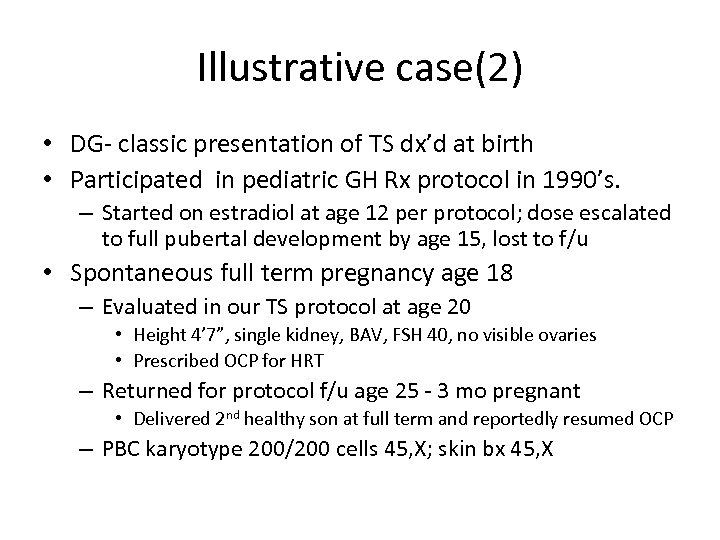 Illustrative case(2) • DG- classic presentation of TS dx’d at birth • Participated in pediatric GH Rx protocol in 1990’s. – Started on estradiol at age 12 per protocol; dose escalated to full pubertal development by age 15, lost to f/u • Spontaneous full term pregnancy age 18 – Evaluated in our TS protocol at age 20 • Height 4’ 7”, single kidney, BAV, FSH 40, no visible ovaries • Prescribed OCP for HRT – Returned for protocol f/u age 25 - 3 mo pregnant • Delivered 2 nd healthy son at full term and reportedly resumed OCP – PBC karyotype 200/200 cells 45, X; skin bx 45, X
Illustrative case(2) • DG- classic presentation of TS dx’d at birth • Participated in pediatric GH Rx protocol in 1990’s. – Started on estradiol at age 12 per protocol; dose escalated to full pubertal development by age 15, lost to f/u • Spontaneous full term pregnancy age 18 – Evaluated in our TS protocol at age 20 • Height 4’ 7”, single kidney, BAV, FSH 40, no visible ovaries • Prescribed OCP for HRT – Returned for protocol f/u age 25 - 3 mo pregnant • Delivered 2 nd healthy son at full term and reportedly resumed OCP – PBC karyotype 200/200 cells 45, X; skin bx 45, X
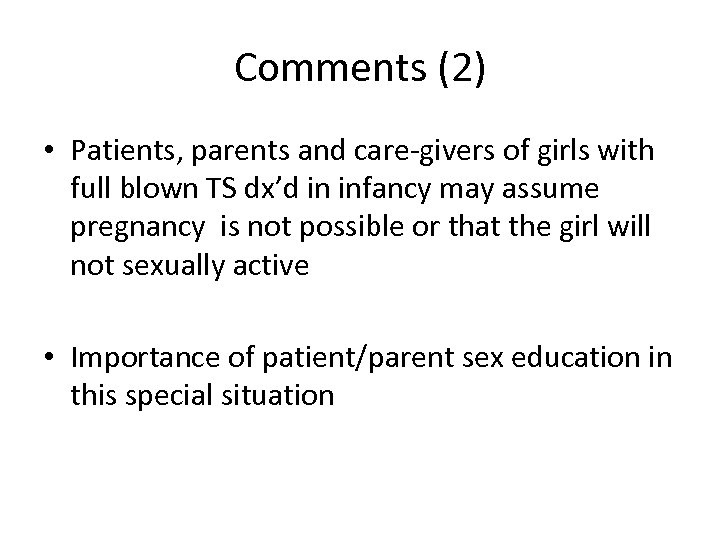 Comments (2) • Patients, parents and care-givers of girls with full blown TS dx’d in infancy may assume pregnancy is not possible or that the girl will not sexually active • Importance of patient/parent sex education in this special situation
Comments (2) • Patients, parents and care-givers of girls with full blown TS dx’d in infancy may assume pregnancy is not possible or that the girl will not sexually active • Importance of patient/parent sex education in this special situation
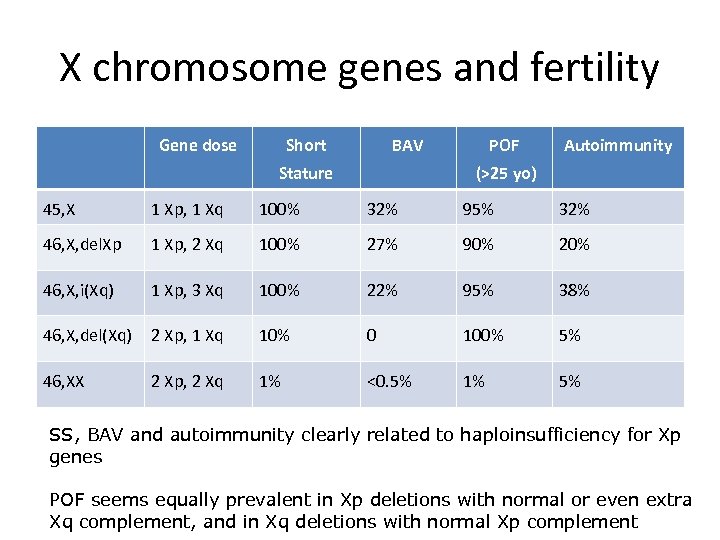 X chromosome genes and fertility Gene dose Short BAV Stature POF Autoimmunity (>25 yo) 45, X 1 Xp, 1 Xq 100% 32% 95% 32% 46, X, del. Xp 1 Xp, 2 Xq 100% 27% 90% 20% 46, X, i(Xq) 1 Xp, 3 Xq 100% 22% 95% 38% 46, X, del(Xq) 2 Xp, 1 Xq 10% 0 100% 5% 46, XX 2 Xp, 2 Xq 1% <0. 5% 1% 5% SS, BAV and autoimmunity clearly related to haploinsufficiency for Xp genes POF seems equally prevalent in Xp deletions with normal or even extra Xq complement, and in Xq deletions with normal Xp complement
X chromosome genes and fertility Gene dose Short BAV Stature POF Autoimmunity (>25 yo) 45, X 1 Xp, 1 Xq 100% 32% 95% 32% 46, X, del. Xp 1 Xp, 2 Xq 100% 27% 90% 20% 46, X, i(Xq) 1 Xp, 3 Xq 100% 22% 95% 38% 46, X, del(Xq) 2 Xp, 1 Xq 10% 0 100% 5% 46, XX 2 Xp, 2 Xq 1% <0. 5% 1% 5% SS, BAV and autoimmunity clearly related to haploinsufficiency for Xp genes POF seems equally prevalent in Xp deletions with normal or even extra Xq complement, and in Xq deletions with normal Xp complement
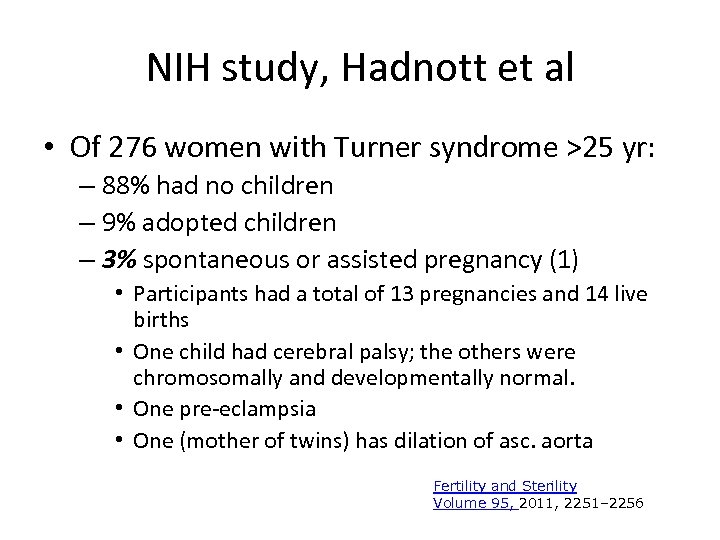 NIH study, Hadnott et al • Of 276 women with Turner syndrome >25 yr: – 88% had no children – 9% adopted children – 3% spontaneous or assisted pregnancy (1) • Participants had a total of 13 pregnancies and 14 live births • One child had cerebral palsy; the others were chromosomally and developmentally normal. • One pre-eclampsia • One (mother of twins) has dilation of asc. aorta Fertility and Sterility Volume 95, 2011, 2251– 2256
NIH study, Hadnott et al • Of 276 women with Turner syndrome >25 yr: – 88% had no children – 9% adopted children – 3% spontaneous or assisted pregnancy (1) • Participants had a total of 13 pregnancies and 14 live births • One child had cerebral palsy; the others were chromosomally and developmentally normal. • One pre-eclampsia • One (mother of twins) has dilation of asc. aorta Fertility and Sterility Volume 95, 2011, 2251– 2256
 Oocyte donation in TS • Karnis et al 2003 estimated ~2% maternal mortality (F&S) – Aortic rupture or dissection • Chevalier et al 2011 < 35% of women prescreened for CVS disease – Poor fetal and maternal outcomes; 2/93 patients died due to aortic rupture (JCEM) • Hagman et al 2013 reviewed 122 deliveries- no fatalities and generally good fetal outcomes
Oocyte donation in TS • Karnis et al 2003 estimated ~2% maternal mortality (F&S) – Aortic rupture or dissection • Chevalier et al 2011 < 35% of women prescreened for CVS disease – Poor fetal and maternal outcomes; 2/93 patients died due to aortic rupture (JCEM) • Hagman et al 2013 reviewed 122 deliveries- no fatalities and generally good fetal outcomes
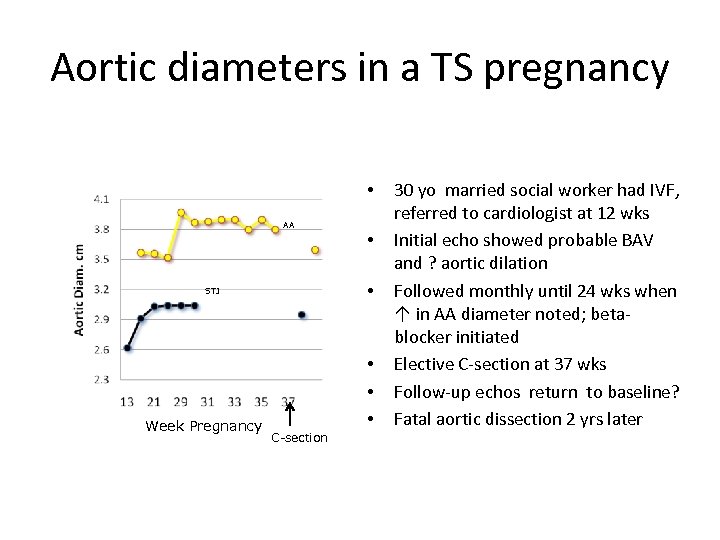 Aortic diameters in a TS pregnancy • AA • STJ Week Pregnancy • C-section • • • 30 yo married social worker had IVF, referred to cardiologist at 12 wks Initial echo showed probable BAV and ? aortic dilation Followed monthly until 24 wks when ↑ in AA diameter noted; betablocker initiated Elective C-section at 37 wks Follow-up echos return to baseline? Fatal aortic dissection 2 yrs later
Aortic diameters in a TS pregnancy • AA • STJ Week Pregnancy • C-section • • • 30 yo married social worker had IVF, referred to cardiologist at 12 wks Initial echo showed probable BAV and ? aortic dilation Followed monthly until 24 wks when ↑ in AA diameter noted; betablocker initiated Elective C-section at 37 wks Follow-up echos return to baseline? Fatal aortic dissection 2 yrs later
 ASRM pages Increased maternal cardiovascular mortality associated with pregnancy in women with Turner syndrome • Practice Committee of the American Society for Reproductive Medicine • Received 22 November 2011. Accepted 29 November 2011. Available online 21 December 2011. TS a relative contra-indication to pregnancy Comprehensive cardiological and maternal-fetal medicine eval. before considering pregnancy by oocyte donation. Cardiac MRI revealing any significant abnormality and/or ASI >2 cm/m 2 (ascending aortic diameter/BSA) represents an absolute contraindication for attempting pregnancy in a woman with Turner syndrome. Women with normal cardiac MRI and evaluation who decide to attempt pregnancy after thorough counseling are still at much higher risk for associated morbidity and mortality and require careful observation and frequent formal reevaluation throughout gestation and postpartum.
ASRM pages Increased maternal cardiovascular mortality associated with pregnancy in women with Turner syndrome • Practice Committee of the American Society for Reproductive Medicine • Received 22 November 2011. Accepted 29 November 2011. Available online 21 December 2011. TS a relative contra-indication to pregnancy Comprehensive cardiological and maternal-fetal medicine eval. before considering pregnancy by oocyte donation. Cardiac MRI revealing any significant abnormality and/or ASI >2 cm/m 2 (ascending aortic diameter/BSA) represents an absolute contraindication for attempting pregnancy in a woman with Turner syndrome. Women with normal cardiac MRI and evaluation who decide to attempt pregnancy after thorough counseling are still at much higher risk for associated morbidity and mortality and require careful observation and frequent formal reevaluation throughout gestation and postpartum.
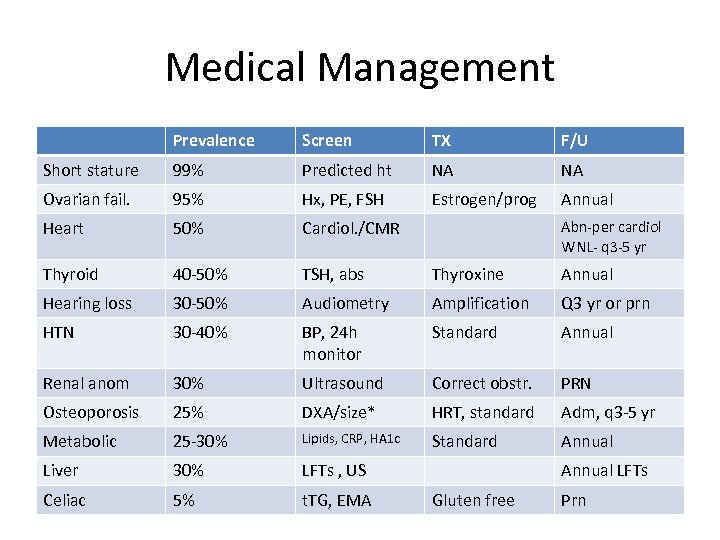 Medical Management Prevalence Screen TX F/U Short stature 99% Predicted ht NA NA Ovarian fail. 95% Hx, PE, FSH Estrogen/prog Annual Heart 50% Cardiol. /CMR Thyroid 40 -50% TSH, abs Thyroxine Annual Hearing loss 30 -50% Audiometry Amplification Q 3 yr or prn HTN 30 -40% BP, 24 h monitor Standard Annual Renal anom 30% Ultrasound Correct obstr. PRN Osteoporosis 25% DXA/size* HRT, standard Adm, q 3 -5 yr Metabolic 25 -30% Lipids, CRP, HA 1 c Standard Annual Liver 30% LFTs , US Celiac 5% t. TG, EMA Abn-per cardiol WNL- q 3 -5 yr Annual LFTs Gluten free Prn
Medical Management Prevalence Screen TX F/U Short stature 99% Predicted ht NA NA Ovarian fail. 95% Hx, PE, FSH Estrogen/prog Annual Heart 50% Cardiol. /CMR Thyroid 40 -50% TSH, abs Thyroxine Annual Hearing loss 30 -50% Audiometry Amplification Q 3 yr or prn HTN 30 -40% BP, 24 h monitor Standard Annual Renal anom 30% Ultrasound Correct obstr. PRN Osteoporosis 25% DXA/size* HRT, standard Adm, q 3 -5 yr Metabolic 25 -30% Lipids, CRP, HA 1 c Standard Annual Liver 30% LFTs , US Celiac 5% t. TG, EMA Abn-per cardiol WNL- q 3 -5 yr Annual LFTs Gluten free Prn
 • Gradual induction of sexual maturation beginning by age 12 • Full dose by age 18 through ~ age 40 – OC, 2 mg estradiol, 100 mg transdermal estradiol – Best choice for cycling is unknown – Adherence is paramount • Beginning age 35 -40 – lower dose, plan to taper and dc by age 50
• Gradual induction of sexual maturation beginning by age 12 • Full dose by age 18 through ~ age 40 – OC, 2 mg estradiol, 100 mg transdermal estradiol – Best choice for cycling is unknown – Adherence is paramount • Beginning age 35 -40 – lower dose, plan to taper and dc by age 50
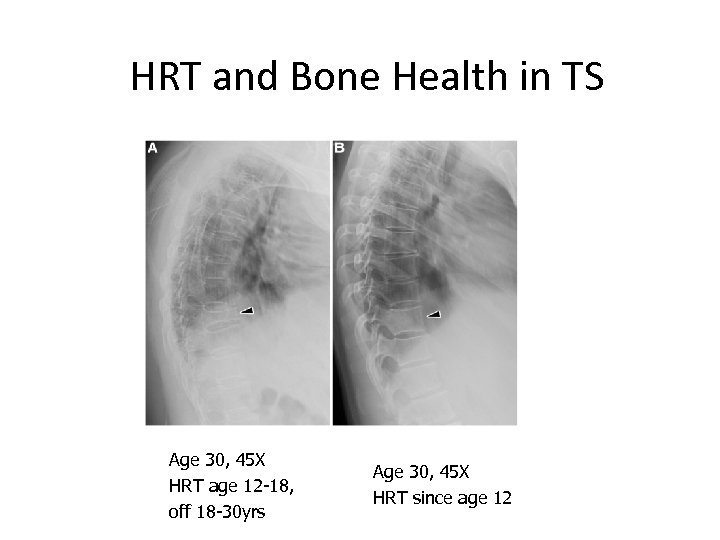 HRT and Bone Health in TS Age 30, 45 X HRT age 12 -18, off 18 -30 yrs Age 30, 45 X HRT since age 12
HRT and Bone Health in TS Age 30, 45 X HRT age 12 -18, off 18 -30 yrs Age 30, 45 X HRT since age 12
 SCREENING FOR CHD IN TS
SCREENING FOR CHD IN TS
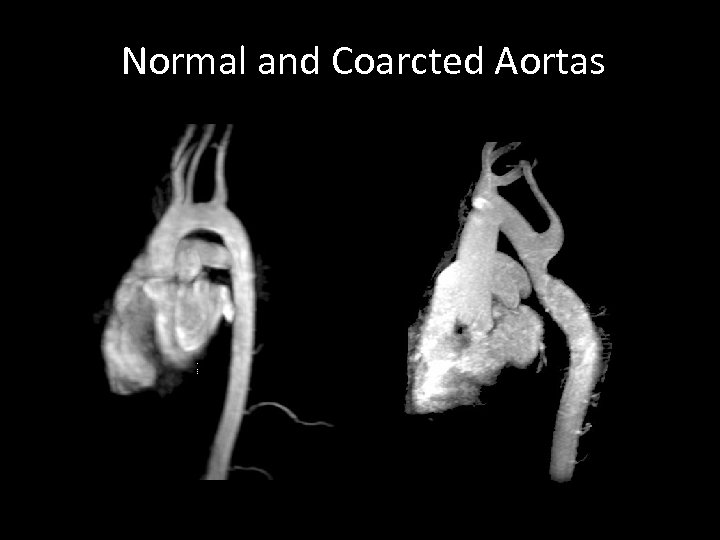 Normal and Coarcted Aortas
Normal and Coarcted Aortas
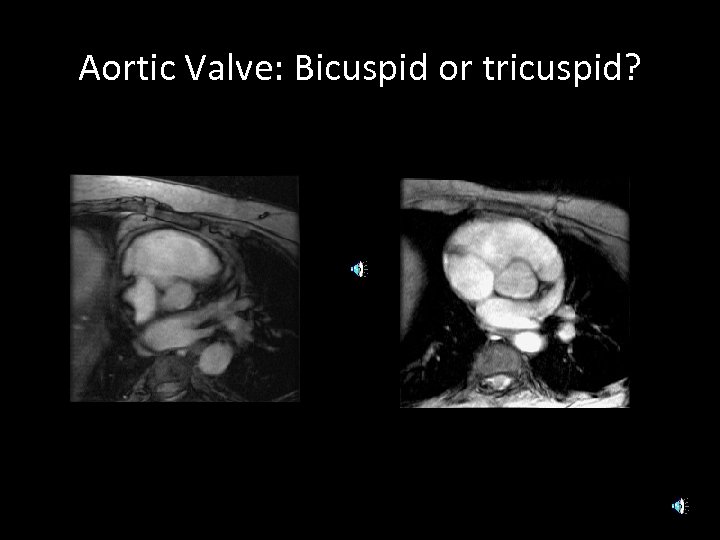 Aortic Valve: Bicuspid or tricuspid? TAV BAV
Aortic Valve: Bicuspid or tricuspid? TAV BAV
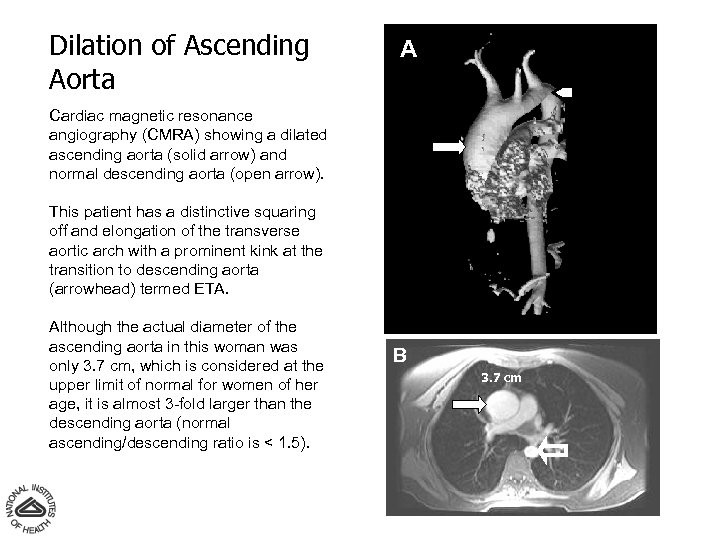 Dilation of Ascending Aorta A Cardiac magnetic resonance angiography (CMRA) showing a dilated ascending aorta (solid arrow) and normal descending aorta (open arrow). This patient has a distinctive squaring off and elongation of the transverse aortic arch with a prominent kink at the transition to descending aorta (arrowhead) termed ETA. Although the actual diameter of the ascending aorta in this woman was only 3. 7 cm, which is considered at the upper limit of normal for women of her age, it is almost 3 -fold larger than the descending aorta (normal ascending/descending ratio is < 1. 5). B 3. 7 cm
Dilation of Ascending Aorta A Cardiac magnetic resonance angiography (CMRA) showing a dilated ascending aorta (solid arrow) and normal descending aorta (open arrow). This patient has a distinctive squaring off and elongation of the transverse aortic arch with a prominent kink at the transition to descending aorta (arrowhead) termed ETA. Although the actual diameter of the ascending aorta in this woman was only 3. 7 cm, which is considered at the upper limit of normal for women of her age, it is almost 3 -fold larger than the descending aorta (normal ascending/descending ratio is < 1. 5). B 3. 7 cm
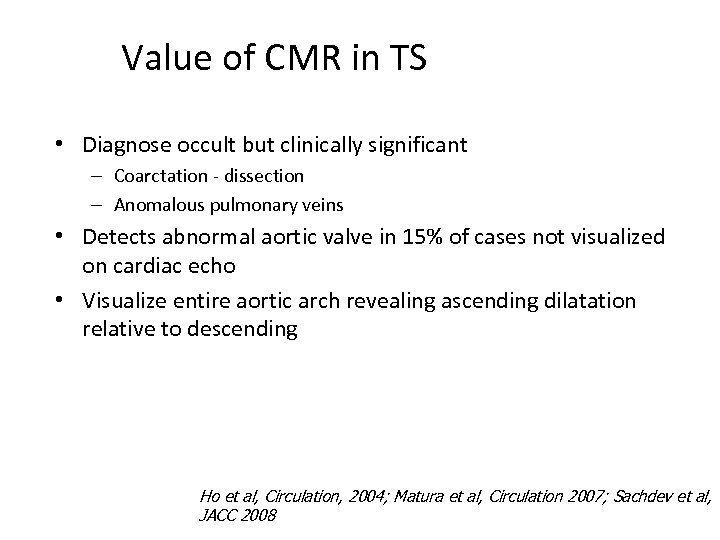 Value of CMR in TS • Diagnose occult but clinically significant – Coarctation - dissection – Anomalous pulmonary veins • Detects abnormal aortic valve in 15% of cases not visualized on cardiac echo • Visualize entire aortic arch revealing ascending dilatation relative to descending NICHD, NIH Ho et al, Circulation, 2004; Matura et al, Circulation 2007; Sachdev et al, JACC 2008
Value of CMR in TS • Diagnose occult but clinically significant – Coarctation - dissection – Anomalous pulmonary veins • Detects abnormal aortic valve in 15% of cases not visualized on cardiac echo • Visualize entire aortic arch revealing ascending dilatation relative to descending NICHD, NIH Ho et al, Circulation, 2004; Matura et al, Circulation 2007; Sachdev et al, JACC 2008
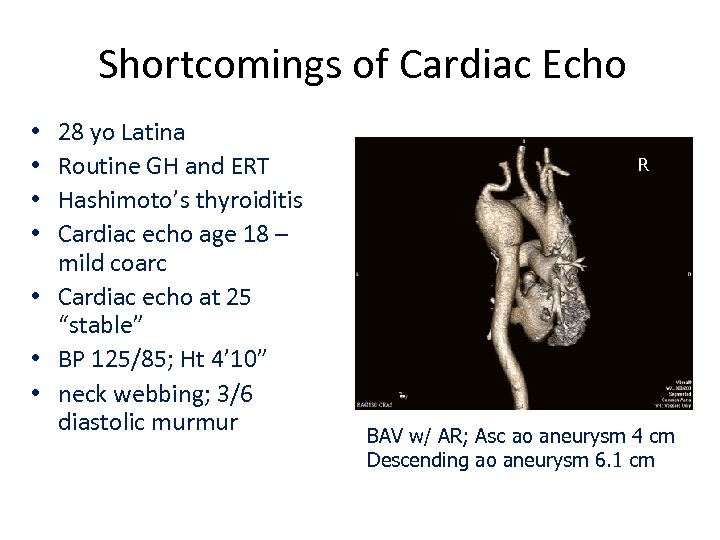 Shortcomings of Cardiac Echo 28 yo Latina Routine GH and ERT Hashimoto’s thyroiditis Cardiac echo age 18 – mild coarc • Cardiac echo at 25 “stable” • BP 125/85; Ht 4’ 10” • neck webbing; 3/6 diastolic murmur • • R BAV w/ AR; Asc ao aneurysm 4 cm Descending ao aneurysm 6. 1 cm
Shortcomings of Cardiac Echo 28 yo Latina Routine GH and ERT Hashimoto’s thyroiditis Cardiac echo age 18 – mild coarc • Cardiac echo at 25 “stable” • BP 125/85; Ht 4’ 10” • neck webbing; 3/6 diastolic murmur • • R BAV w/ AR; Asc ao aneurysm 4 cm Descending ao aneurysm 6. 1 cm
 Illustrative Case 3 • 62 yo woman referred for osteoporosis – PMH -Coarc repair age 12, always short, no puberty, Cochlear implants, no medications – Recent back pain prompted plain Xrays (aortic calcifications) and DXA (diffuse osteoporosis) – PE- Many signs of TS, appearing considerably older than 62. Disparity in right and left arm BP (R>L). Bilat carotid bruits. Tanner 1 breast and T 2 pubic hair. • What test(s) would you order?
Illustrative Case 3 • 62 yo woman referred for osteoporosis – PMH -Coarc repair age 12, always short, no puberty, Cochlear implants, no medications – Recent back pain prompted plain Xrays (aortic calcifications) and DXA (diffuse osteoporosis) – PE- Many signs of TS, appearing considerably older than 62. Disparity in right and left arm BP (R>L). Bilat carotid bruits. Tanner 1 breast and T 2 pubic hair. • What test(s) would you order?
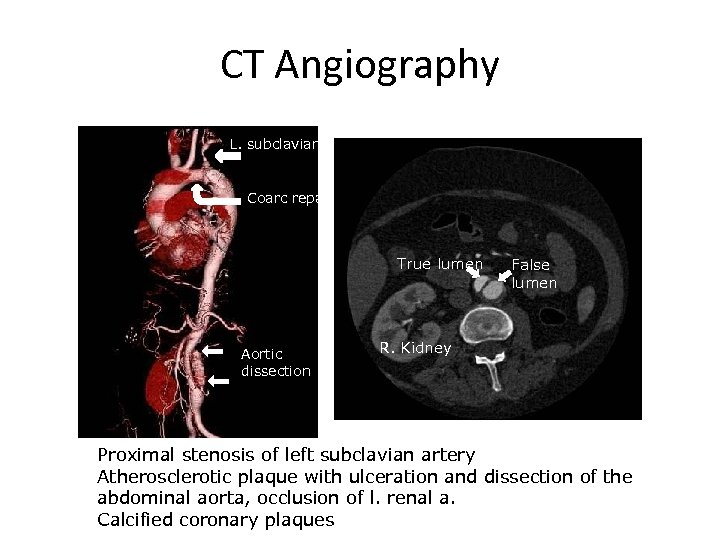 CT Angiography L. subclavian a. Coarc repair True lumen Aortic dissection False lumen R. Kidney Proximal stenosis of left subclavian artery Atherosclerotic plaque with ulceration and dissection of the abdominal aorta, occlusion of l. renal a. Calcified coronary plaques
CT Angiography L. subclavian a. Coarc repair True lumen Aortic dissection False lumen R. Kidney Proximal stenosis of left subclavian artery Atherosclerotic plaque with ulceration and dissection of the abdominal aorta, occlusion of l. renal a. Calcified coronary plaques
 Final comments • It is never too late to diagnose TS • There is an excess of atherosclerosis as well as congenital heart disease
Final comments • It is never too late to diagnose TS • There is an excess of atherosclerosis as well as congenital heart disease
 QOL Issues in TS • Carel et al in JCEM 2005 -2006 – disappointment with GH treatment for SS. Self-esteem and social adjustment in young women with TS more influenced by pubertal management and sexuality • NIH – major concerns related to TS (Sutton et al 2005) • • Infertility Short stature Sexual development and function Health
QOL Issues in TS • Carel et al in JCEM 2005 -2006 – disappointment with GH treatment for SS. Self-esteem and social adjustment in young women with TS more influenced by pubertal management and sexuality • NIH – major concerns related to TS (Sutton et al 2005) • • Infertility Short stature Sexual development and function Health
 Importance of “Truth Telling” • During interview sessions addressing concerns about living with TS, 30/97 participants spontaneously mentioned that all or part of their TS diagnosis had been withheld from them • Fifteen girls and women from whom a secret had been kept knew every aspect of their diagnosis except the infertility component – “The doctor finished his exam and I got dressed and went in. And he just kind of stopped, put his pen down and went, ‘you know you’re not having kids ever, don't you? ' So that was the hardest time. ” (Diagnosed at 17, learned of infertility at 19. ) – “I did get upset with my mother [when I found out]…. She… didn't explain. She said, ‘Well, what’s the big deal? ' I said, ‘I think it would have helped me to understand myself a little bit better. To tell—to fill in the gaps to tell you more of the story. ’” (Diagnosed at 17, learned infertile at 28) – “There I am at this sterile place. And I found out that since the age of 9 to 16, everyone knew something I had no knowledge of about me that was pretty darn important. I was told [I was infertile] in such a horrendous way. And all I knew was that the people that I trusted forever were willing to betray me. ” (Diagnosed at 9, learned infertile at 16). Sutton et al, Peds 2006
Importance of “Truth Telling” • During interview sessions addressing concerns about living with TS, 30/97 participants spontaneously mentioned that all or part of their TS diagnosis had been withheld from them • Fifteen girls and women from whom a secret had been kept knew every aspect of their diagnosis except the infertility component – “The doctor finished his exam and I got dressed and went in. And he just kind of stopped, put his pen down and went, ‘you know you’re not having kids ever, don't you? ' So that was the hardest time. ” (Diagnosed at 17, learned of infertility at 19. ) – “I did get upset with my mother [when I found out]…. She… didn't explain. She said, ‘Well, what’s the big deal? ' I said, ‘I think it would have helped me to understand myself a little bit better. To tell—to fill in the gaps to tell you more of the story. ’” (Diagnosed at 17, learned infertile at 28) – “There I am at this sterile place. And I found out that since the age of 9 to 16, everyone knew something I had no knowledge of about me that was pretty darn important. I was told [I was infertile] in such a horrendous way. And all I knew was that the people that I trusted forever were willing to betray me. ” (Diagnosed at 9, learned infertile at 16). Sutton et al, Peds 2006
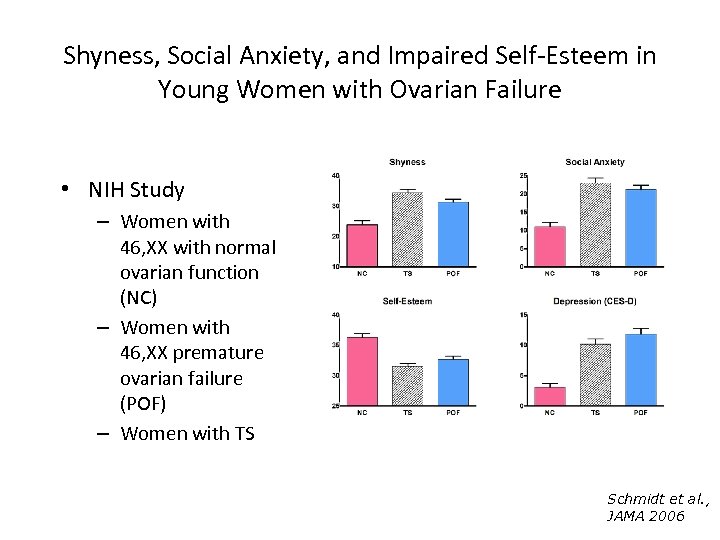 Shyness, Social Anxiety, and Impaired Self-Esteem in Young Women with Ovarian Failure • NIH Study – Women with 46, XX with normal ovarian function (NC) – Women with 46, XX premature ovarian failure (POF) – Women with TS NICHD, NIH Schmidt et al. , JAMA 2006
Shyness, Social Anxiety, and Impaired Self-Esteem in Young Women with Ovarian Failure • NIH Study – Women with 46, XX with normal ovarian function (NC) – Women with 46, XX premature ovarian failure (POF) – Women with TS NICHD, NIH Schmidt et al. , JAMA 2006
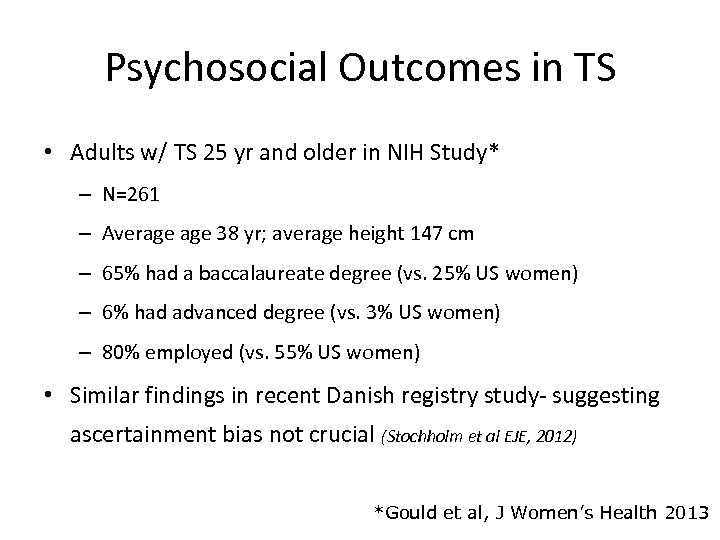 Psychosocial Outcomes in TS • Adults w/ TS 25 yr and older in NIH Study* – N=261 – Average 38 yr; average height 147 cm – 65% had a baccalaureate degree (vs. 25% US women) – 6% had advanced degree (vs. 3% US women) – 80% employed (vs. 55% US women) • Similar findings in recent Danish registry study- suggesting ascertainment bias not crucial (Stochholm et al EJE, 2012) *Gould et al, J Women’s Health 2013
Psychosocial Outcomes in TS • Adults w/ TS 25 yr and older in NIH Study* – N=261 – Average 38 yr; average height 147 cm – 65% had a baccalaureate degree (vs. 25% US women) – 6% had advanced degree (vs. 3% US women) – 80% employed (vs. 55% US women) • Similar findings in recent Danish registry study- suggesting ascertainment bias not crucial (Stochholm et al EJE, 2012) *Gould et al, J Women’s Health 2013
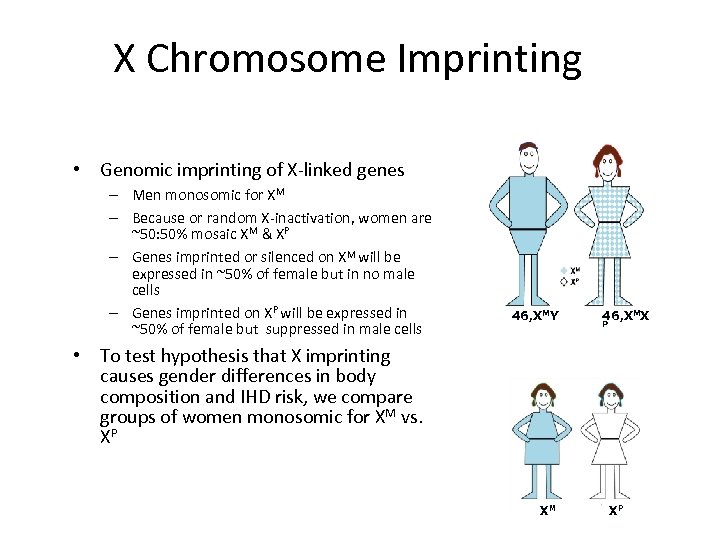 X Chromosome Imprinting • Genomic imprinting of X-linked genes – Men monosomic for XM – Because or random X-inactivation, women are ~50: 50% mosaic XM & XP – Genes imprinted or silenced on XM will be expressed in ~50% of female but in no male cells – Genes imprinted on XP will be expressed in ~50% of female but suppressed in male cells 46, XMY 46, XMX P • To test hypothesis that X imprinting causes gender differences in body composition and IHD risk, we compare groups of women monosomic for XM vs. XP NICHD, NIH XM XP
X Chromosome Imprinting • Genomic imprinting of X-linked genes – Men monosomic for XM – Because or random X-inactivation, women are ~50: 50% mosaic XM & XP – Genes imprinted or silenced on XM will be expressed in ~50% of female but in no male cells – Genes imprinted on XP will be expressed in ~50% of female but suppressed in male cells 46, XMY 46, XMX P • To test hypothesis that X imprinting causes gender differences in body composition and IHD risk, we compare groups of women monosomic for XM vs. XP NICHD, NIH XM XP
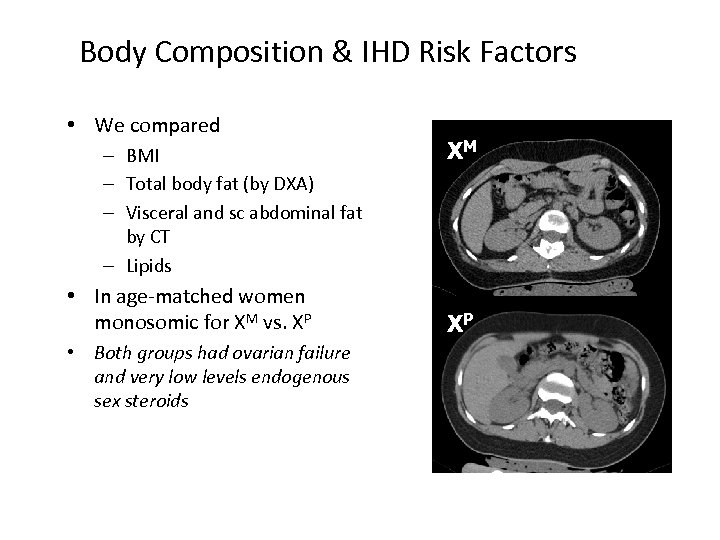 Body Composition & IHD Risk Factors • We compared – BMI – Total body fat (by DXA) – Visceral and sc abdominal fat by CT – Lipids • In age-matched women monosomic for XM vs. XP • Both groups had ovarian failure and very low levels endogenous sex steroids NICHD, NIH XM XP
Body Composition & IHD Risk Factors • We compared – BMI – Total body fat (by DXA) – Visceral and sc abdominal fat by CT – Lipids • In age-matched women monosomic for XM vs. XP • Both groups had ovarian failure and very low levels endogenous sex steroids NICHD, NIH XM XP
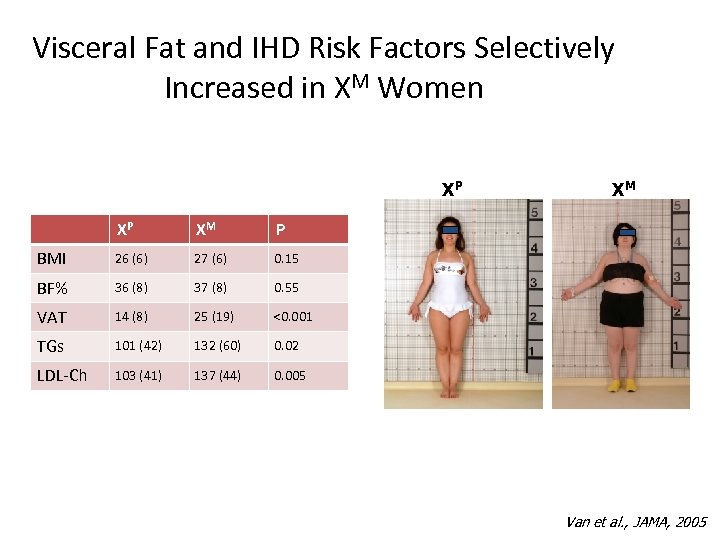 Visceral Fat and IHD Risk Factors Selectively Increased in XM Women XP XP XM P BMI 26 (6) 27 (6) 0. 15 BF% 36 (8) 37 (8) 0. 55 VAT 14 (8) 25 (19) <0. 001 TGs 101 (42) 132 (60) 0. 02 LDL-Ch 103 (41) 137 (44) XM 0. 005 NICHD, NIH Van et al. , JAMA, 2005
Visceral Fat and IHD Risk Factors Selectively Increased in XM Women XP XP XM P BMI 26 (6) 27 (6) 0. 15 BF% 36 (8) 37 (8) 0. 55 VAT 14 (8) 25 (19) <0. 001 TGs 101 (42) 132 (60) 0. 02 LDL-Ch 103 (41) 137 (44) XM 0. 005 NICHD, NIH Van et al. , JAMA, 2005
 Incidence of coronary disease related to parental origin of the single X • Further study to determine actual incidence of coronary atherosclerosis – >age 34 - CT Ca++ score – “pure” 45 X – Parental DNA for POO genotyping
Incidence of coronary disease related to parental origin of the single X • Further study to determine actual incidence of coronary atherosclerosis – >age 34 - CT Ca++ score – “pure” 45 X – Parental DNA for POO genotyping
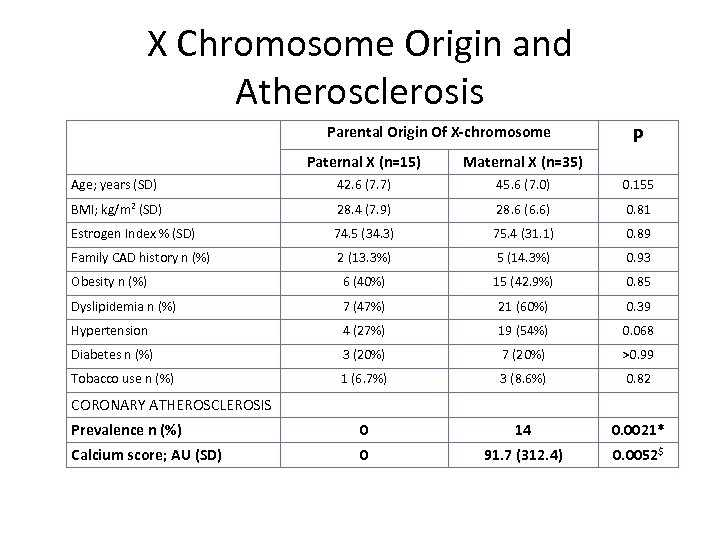 X Chromosome Origin and Atherosclerosis Parental Origin Of X-chromosome P Paternal X (n=15) Maternal X (n=35) Age; years (SD) 42. 6 (7. 7) 45. 6 (7. 0) 0. 155 BMI; kg/m 2 (SD) 28. 4 (7. 9) 28. 6 (6. 6) 0. 81 Estrogen Index % (SD) 74. 5 (34. 3) 75. 4 (31. 1) 0. 89 Family CAD history n (%) 2 (13. 3%) 5 (14. 3%) 0. 93 Obesity n (%) 6 (40%) 15 (42. 9%) 0. 85 Dyslipidemia n (%) 7 (47%) 21 (60%) 0. 39 Hypertension 4 (27%) 19 (54%) 0. 068 Diabetes n (%) 3 (20%) 7 (20%) >0. 99 Tobacco use n (%) 1 (6. 7%) 3 (8. 6%) 0. 82 Prevalence n (%) 0 14 0. 0021* Calcium score; AU (SD) 0 91. 7 (312. 4) 0. 0052$ CORONARY ATHEROSCLEROSIS
X Chromosome Origin and Atherosclerosis Parental Origin Of X-chromosome P Paternal X (n=15) Maternal X (n=35) Age; years (SD) 42. 6 (7. 7) 45. 6 (7. 0) 0. 155 BMI; kg/m 2 (SD) 28. 4 (7. 9) 28. 6 (6. 6) 0. 81 Estrogen Index % (SD) 74. 5 (34. 3) 75. 4 (31. 1) 0. 89 Family CAD history n (%) 2 (13. 3%) 5 (14. 3%) 0. 93 Obesity n (%) 6 (40%) 15 (42. 9%) 0. 85 Dyslipidemia n (%) 7 (47%) 21 (60%) 0. 39 Hypertension 4 (27%) 19 (54%) 0. 068 Diabetes n (%) 3 (20%) 7 (20%) >0. 99 Tobacco use n (%) 1 (6. 7%) 3 (8. 6%) 0. 82 Prevalence n (%) 0 14 0. 0021* Calcium score; AU (SD) 0 91. 7 (312. 4) 0. 0052$ CORONARY ATHEROSCLEROSIS
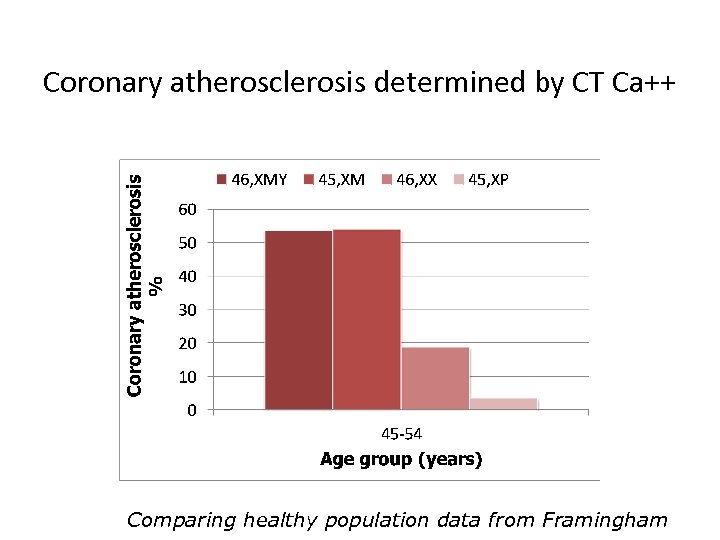 Coronary atherosclerosis determined by CT Ca++ Comparing healthy population data from Framingham
Coronary atherosclerosis determined by CT Ca++ Comparing healthy population data from Framingham
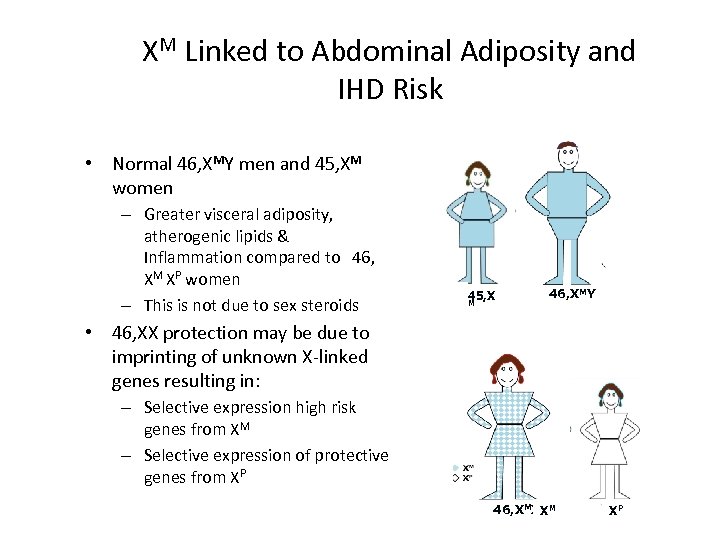 XM Linked to Abdominal Adiposity and IHD Risk • Normal 46, XMY men and 45, XM women – Greater visceral adiposity, atherogenic lipids & Inflammation compared to 46, XM XP women – This is not due to sex steroids 45, X M 46, XMY • 46, XX protection may be due to imprinting of unknown X-linked genes resulting in: – Selective expression high risk genes from XM – Selective expression of protective genes from XP NICHD, NIH P 46, XMXXM XP
XM Linked to Abdominal Adiposity and IHD Risk • Normal 46, XMY men and 45, XM women – Greater visceral adiposity, atherogenic lipids & Inflammation compared to 46, XM XP women – This is not due to sex steroids 45, X M 46, XMY • 46, XX protection may be due to imprinting of unknown X-linked genes resulting in: – Selective expression high risk genes from XM – Selective expression of protective genes from XP NICHD, NIH P 46, XMXXM XP
 Gratitude • NICHD – – – – Vladimir Bakalov Harley Gould Liat Gutin Clara Cheng Jian Zhou Helen Hougen Rachel Poliquin Kateri Mc. Carthy • NHLBI – Douglas R Rosing – Andrew Arai – Vandana Sachdev • NIH CC Radiology – Vincent Ho – Ahmed Gharib • Girls and women with TS and their familes
Gratitude • NICHD – – – – Vladimir Bakalov Harley Gould Liat Gutin Clara Cheng Jian Zhou Helen Hougen Rachel Poliquin Kateri Mc. Carthy • NHLBI – Douglas R Rosing – Andrew Arai – Vandana Sachdev • NIH CC Radiology – Vincent Ho – Ahmed Gharib • Girls and women with TS and their familes
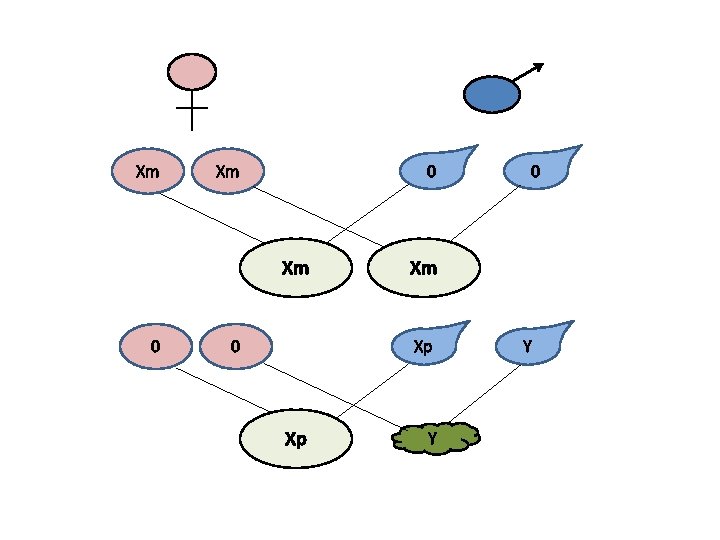 Xm Xm 0 0 Xm Xp Xp 0 Y Y
Xm Xm 0 0 Xm Xp Xp 0 Y Y


