Diabetes Charith Kumara Group-14 KSMU. Diabetes Mellitus Disease

Diabetes Charith Kumara Group-14 KSMU.
Diabetes Mellitus Disease in which the body doesn’t produce or properly use insulin, leading to hyperglycemia.
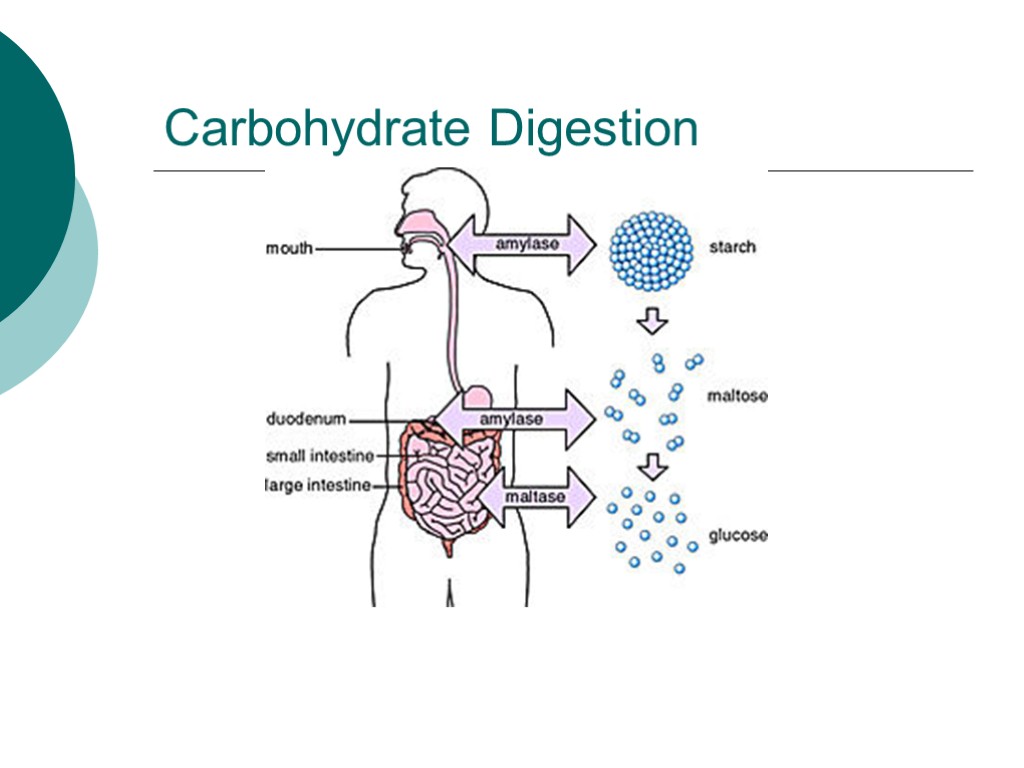
Carbohydrate Digestion
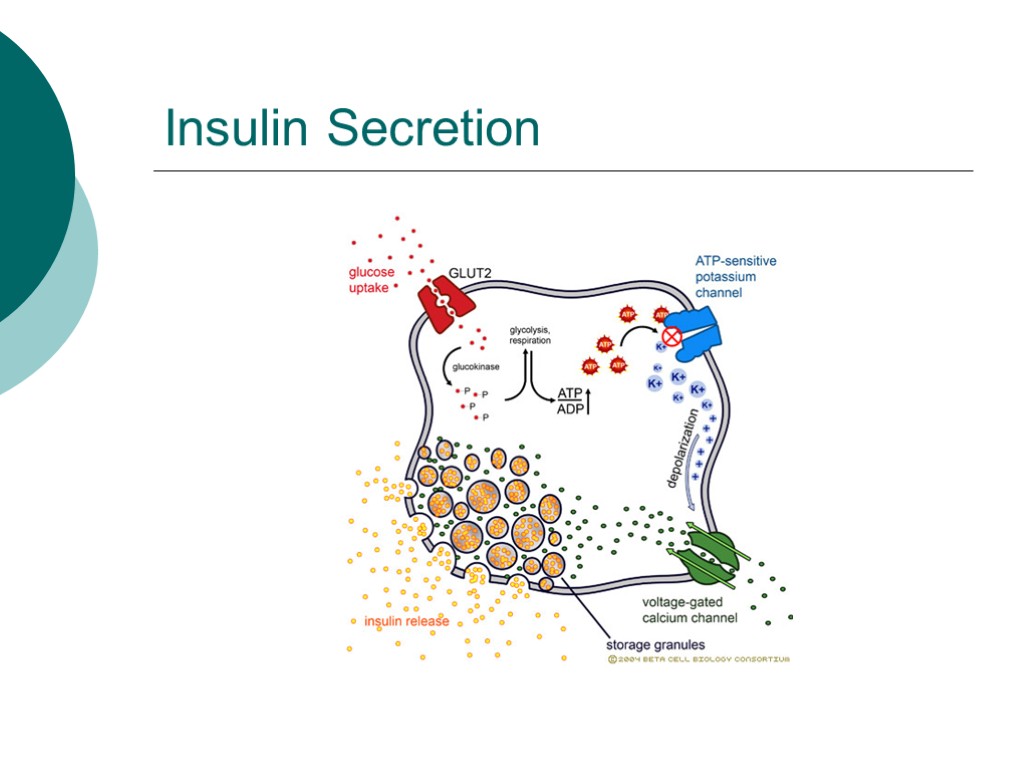
Insulin Secretion
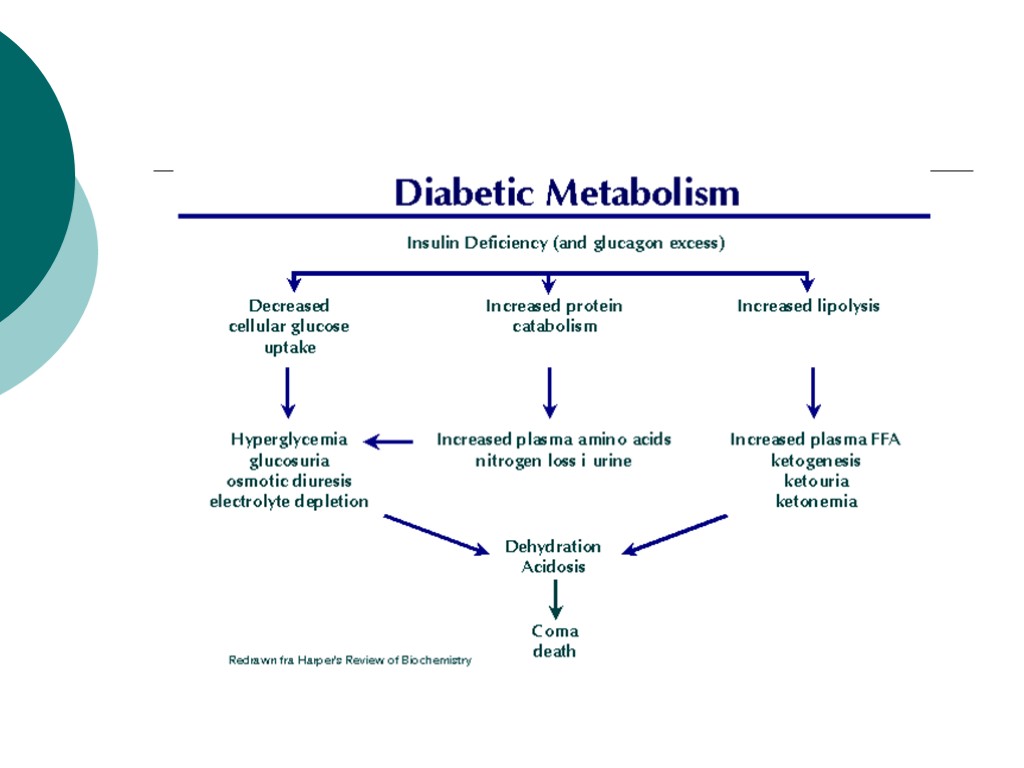
What goes wrong in diabetes? Multitude of mechanisms Insulin Regulation Secretion Uptake or breakdown Beta cells damage
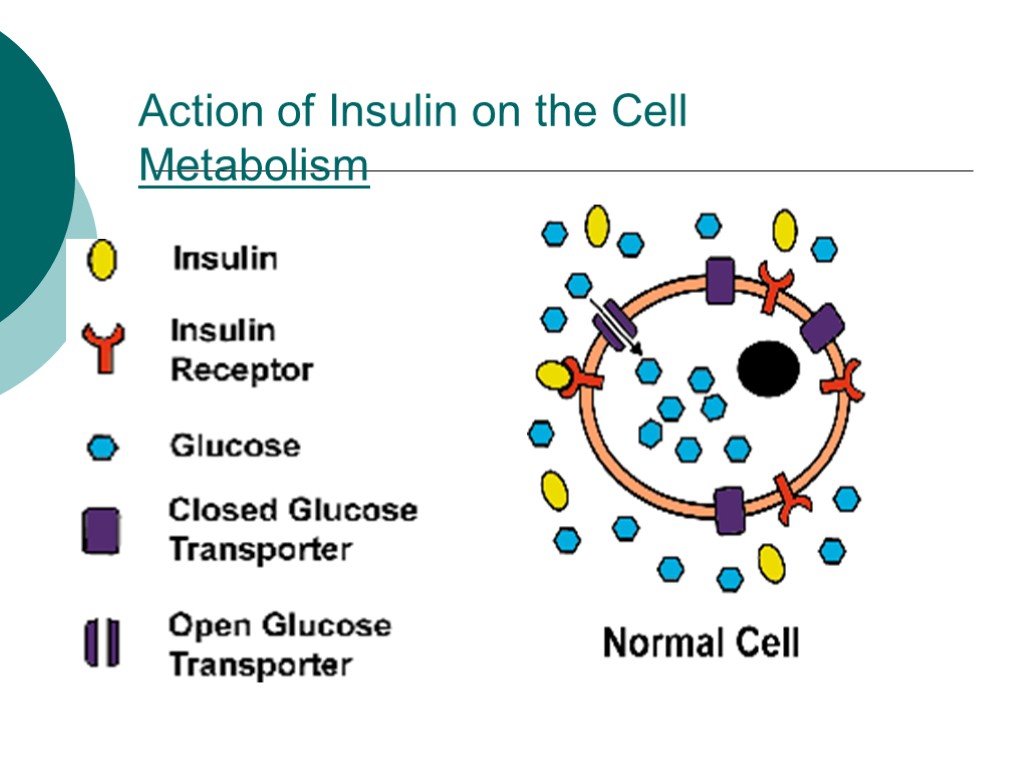
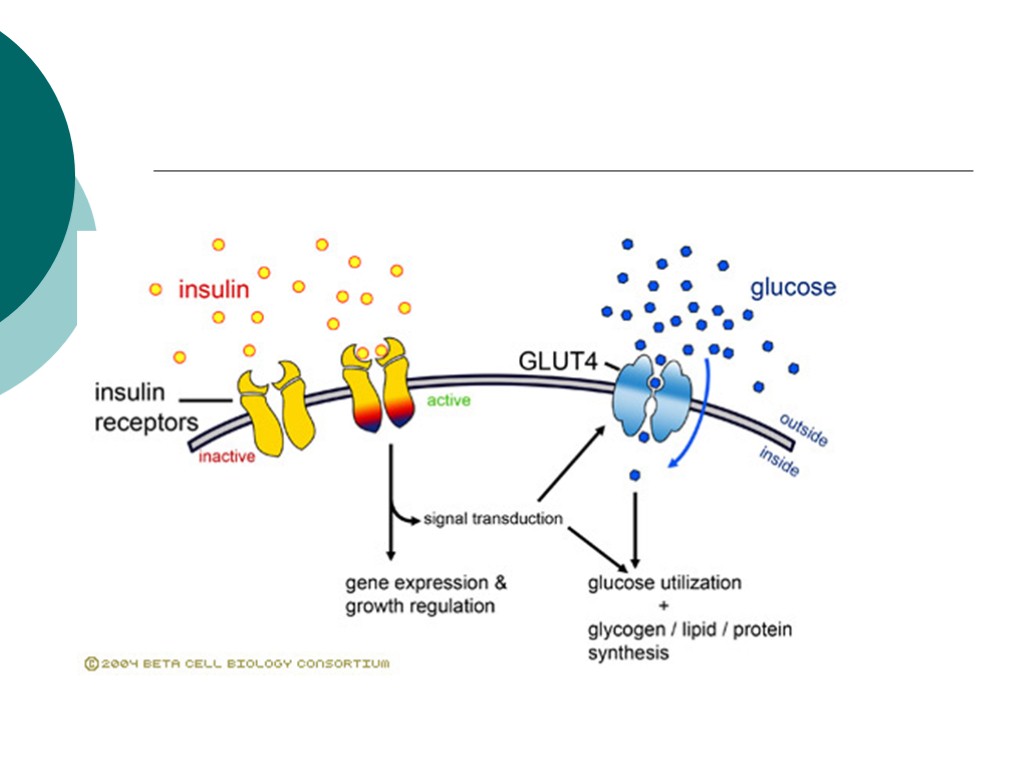
Action of Insulin on the Cell Metabolism
Action of Insulin on Carbohydrate, Protein and Fat Metabolism Carbohydrate Facilitates the transport of glucose into muscle and adipose cells Facilitates the conversion of glucose to glycogen for storage in the liver and muscle. Decreases the breakdown and release of glucose from glycogen by the liver
Action of Insulin on Carbohydrate, Protein and Fat Metabolism Protein Stimulates protein synthesis Inhibits protein breakdown; diminishes gluconeogenesis
Action of Insulin on Carbohydrate, Protein and Fat Metabolism Fat Stimulates lipogenesis- the transport of triglycerides to adipose tissue Inhibits lipolysis – prevents excessive production of ketones or ketoacidosis
Type I Diabetes Low or absent endogenous insulin Dependent on exogenous insulin for life Onset generally < 30 years 5-10% of cases of diabetes Onset sudden Symptoms: 3 P’s: polyuria, polydypsia, polyphagia
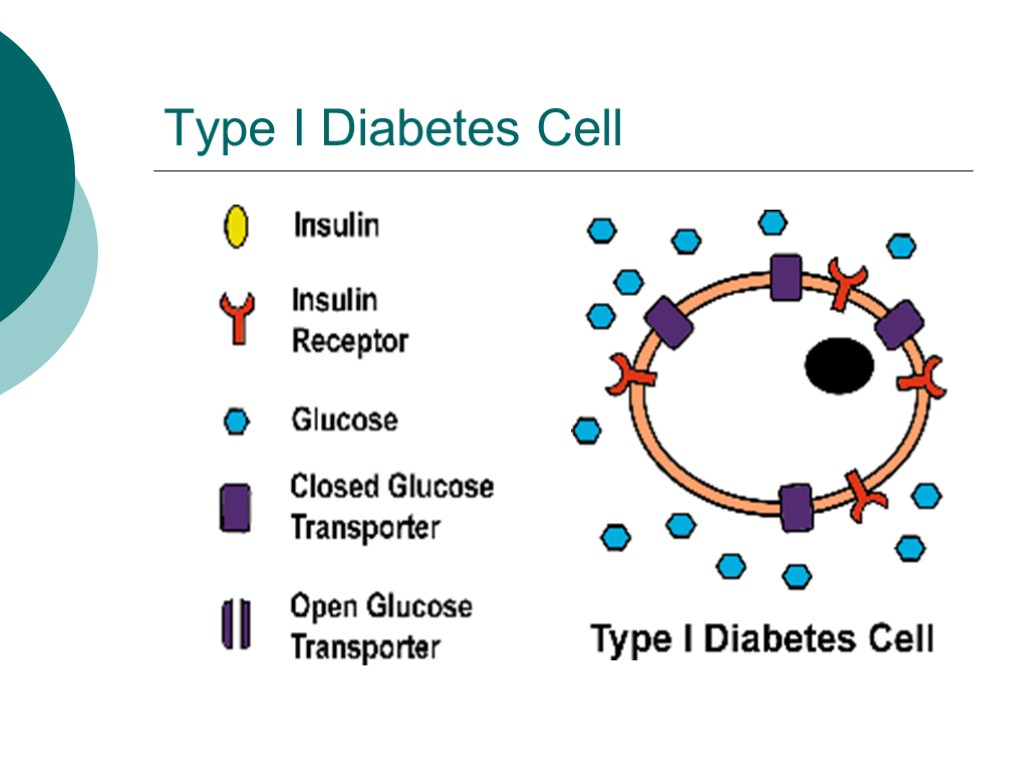
Type I Diabetes Cell
Type I Diabetes Genetic component to disease
Type II Diabetes Insulin levels may be normal, elevated or depressed Characterized by insulin resistance, diminished tissue sensitivity to insulin, and impaired beta cell function (delayed or inadequate insulin release) Often occurs >40 years
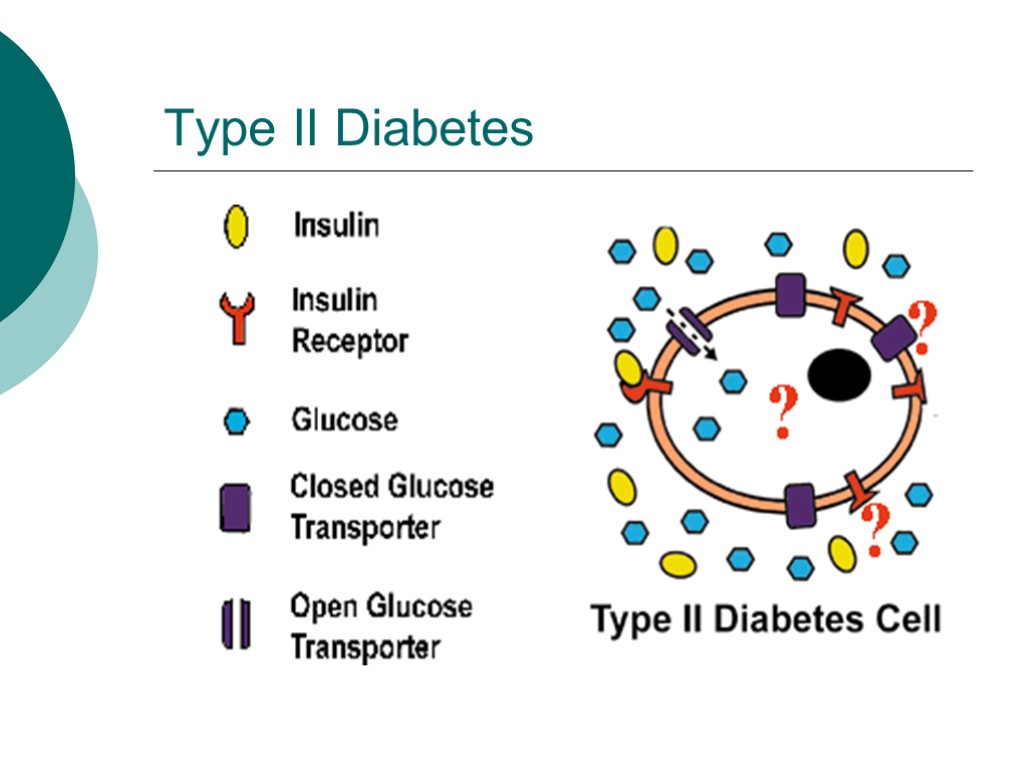
Type II Diabetes
Type II Diabetes Risk factors: family history, sedentary lifestyle, obesity and aging Controlled by weight loss, oral hypoglycemic agents and or insulin
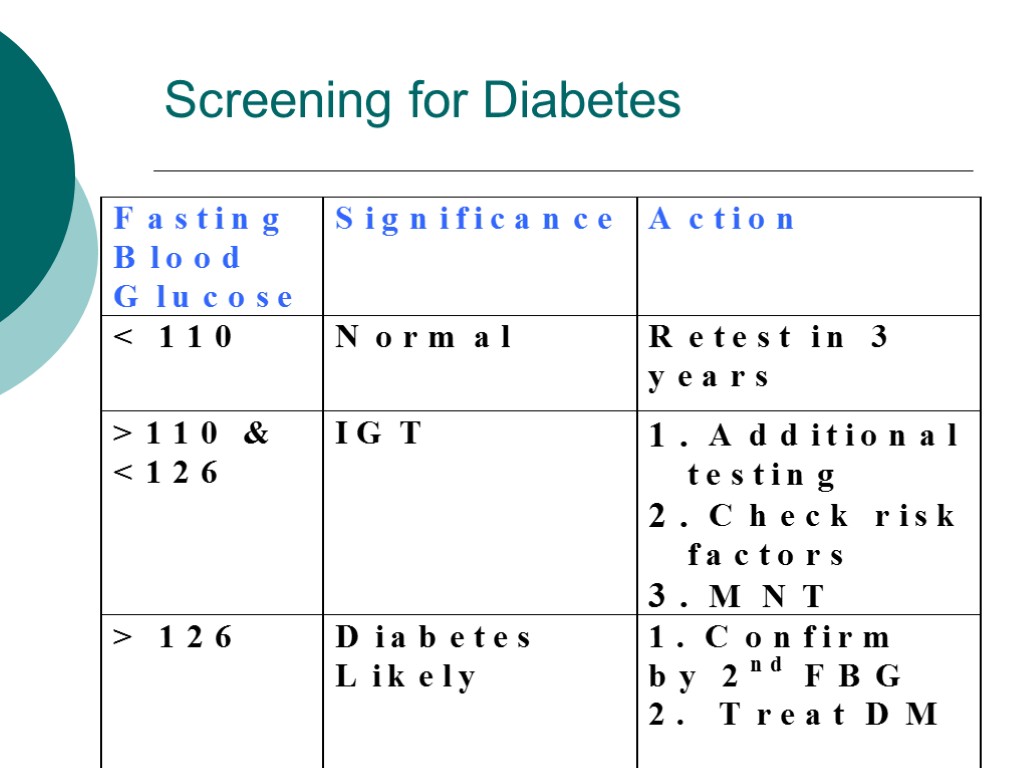
Screening for Diabetes
Management of Diabetes Mellitus Nutrition Blood glucose Medications Physical activity/exercise Behavior modification
Medical Nutrition Therapy Primary Goal – improve metabolic control Blood glucose Lipid (cholesterol) levels
Medical Nutrition Therapy Maintain short and long term body weight Reach and maintain normal growth and development Prevent or treat complications Improve and maintain nutritional status Provide optimal nutrition for pregnancy
Nutritional Management for Type I Diabetes Consistency and timing of meals Timing of insulin Monitor blood glucose regularly
Nutritional Management for Type II Diabetes Weight loss Smaller meals and snacks Physical activity Monitor blood glucose and medications
Diabetes Control and Complications Trial 10 year randomized, controlled, clinical trial Determine the effects of glucose control on the development of long term microvascular and neurologic complications in persons with type I diabetes. 1441 participants, ages 13 to 39
Diabetes Control and Complications Trial Conventional therapy: 1 - 2 insulin injections, self monitoring B.G routine contact with MD and case manager 4X/year. Intensive therapy: 3 or more insulin injections, with adjustments in dose according to B.G monitoring, planned dietary intake and anticipated exercise.
Diabetes Control and Complications Trial Results: 76% reduction in retinopathy 60% reduction in neuropathy 54% reduction in albuminuria 39% reduction in microalbuminuria Implication: Improved blood glucose control also applies to person with type II diabetes.
Nutrition Recommendations Carbohydrate 60-70% calories from carbohydrates and monounsaturated fats Protein 10-20% total calories
Nutrition Recommendations Fat <10% calories from saturated fat 10% calories from PUFA <300 mg cholesterol Fiber 20-35 grams/day Alcohol Type I – limit to 2 drinks/day, with meals Type II – substitute for fat calories
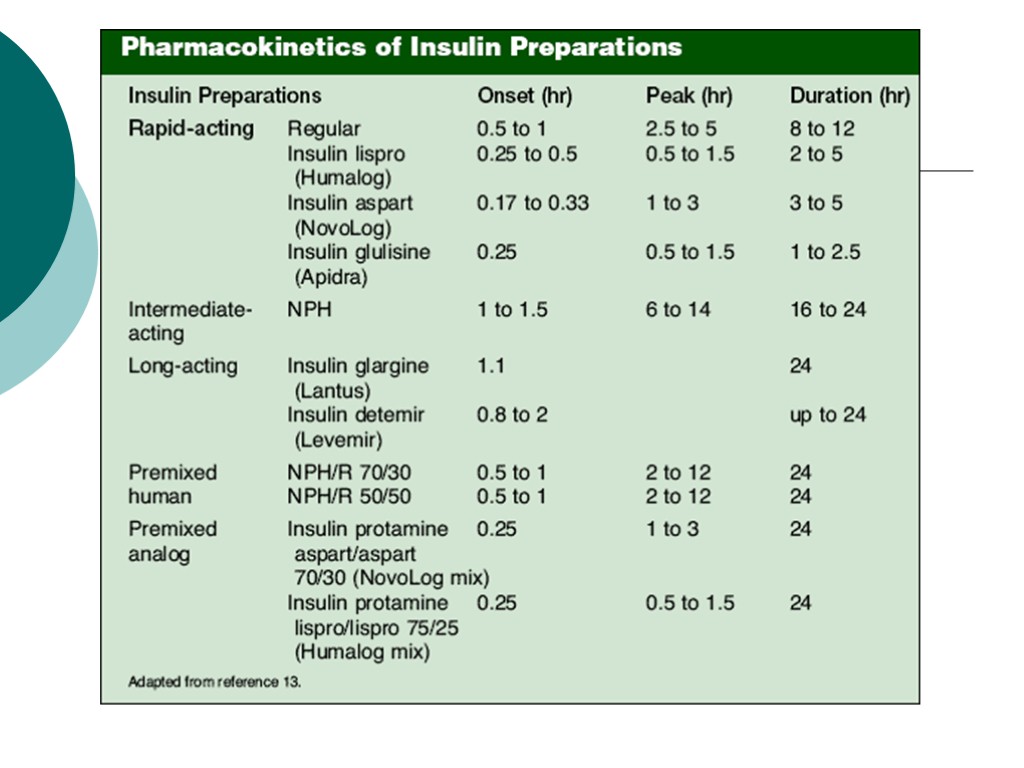
Types of Insulins Regular insulins Insulin analogs Pre-mixed insulin Short peptide mimics
Regular insulins: Human insulin: Humulin® (from E.coli), Novalin® (from yeast) NPH - neutral protamine Hagedorn (NPH), protamine mixed. Lente® insulin / Ultralente® insullin- zinc added
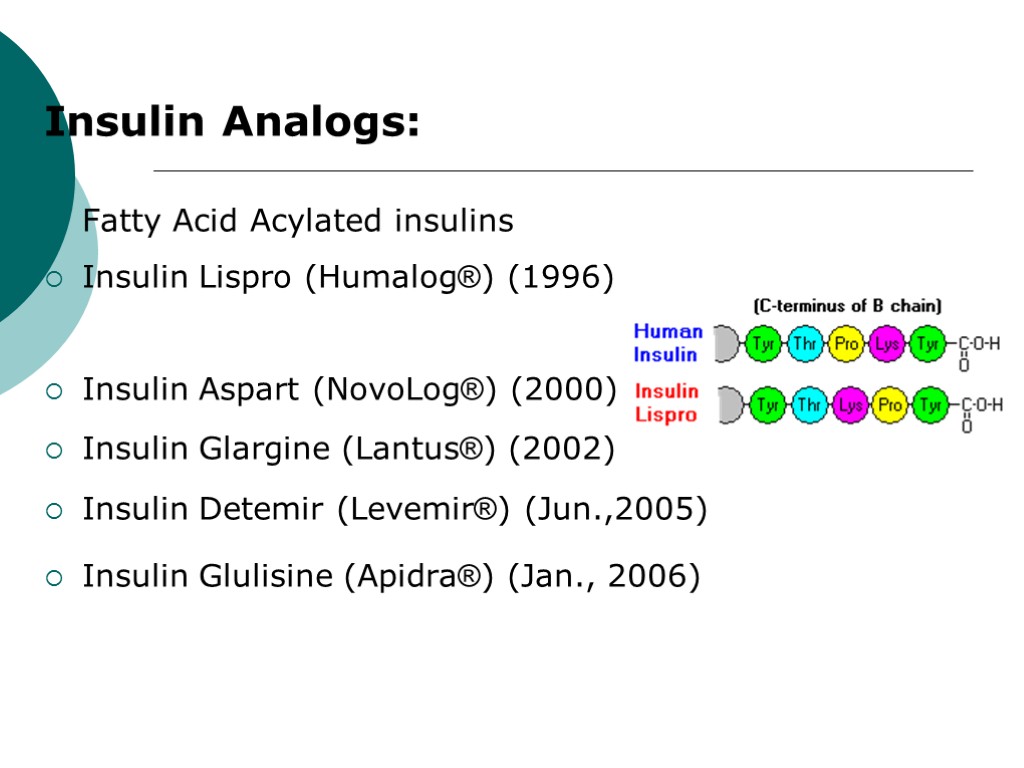
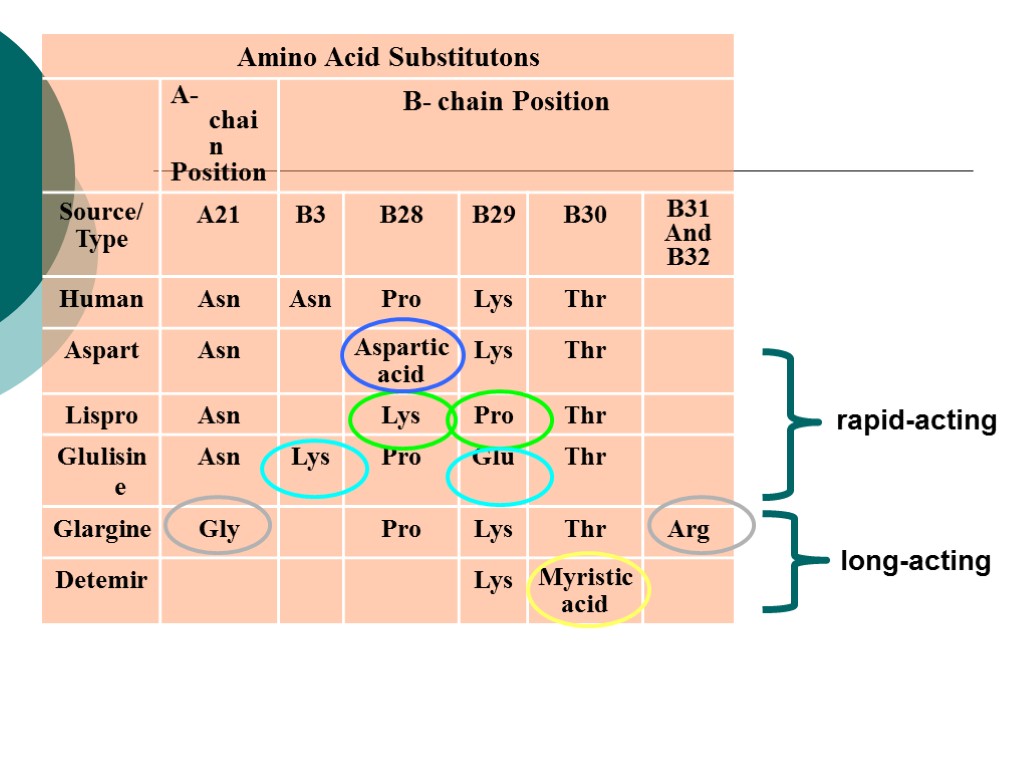
Insulin Analogs: Fatty Acid Acylated insulins Insulin Lispro (Humalog®) (1996) Insulin Aspart (NovoLog®) (2000) Insulin Glargine (Lantus®) (2002) Insulin Detemir (Levemir®) (Jun.,2005) Insulin Glulisine (Apidra®) (Jan., 2006)
Diabetes – Oral Medications Sulfonylureas Biguanides Sulfonylureas and biguanide combination drugs Thiazolidinediones Alpha-glycosidase inhibitors Meglitinides 6 Classes :
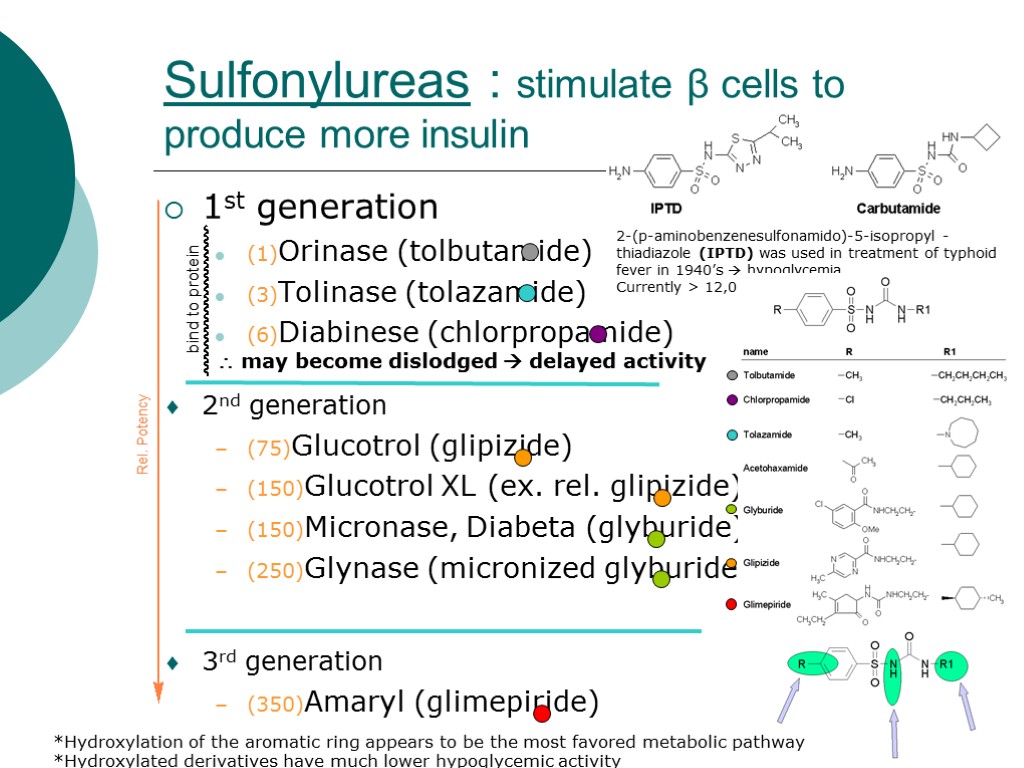
Sulfonylureas : stimulate β cells to produce more insulin 1st generation (1)Orinase (tolbutamide) (3)Tolinase (tolazamide) (6)Diabinese (chlorpropamide) 2nd generation (75)Glucotrol (glipizide) (150)Glucotrol XL (ex. rel. glipizide) (150)Micronase, Diabeta (glyburide) (250)Glynase (micronized glyburide) 3rd generation (350)Amaryl (glimepiride) 2-(p-aminobenzenesulfonamido)-5-isopropyl -thiadiazole (IPTD) was used in treatment of typhoid fever in 1940’s hypoglycemia Currently > 12,000 may become dislodged delayed activity *Hydroxylation of the aromatic ring appears to be the most favored metabolic pathway *Hydroxylated derivatives have much lower hypoglycemic activity
Mechanism of Action Sulfonylureas interact with receptors on pancreatic b-cells to block ATP-sensitive potassium channels This, in turn, leads to opening of calcium channels Which leads to the production of insulin
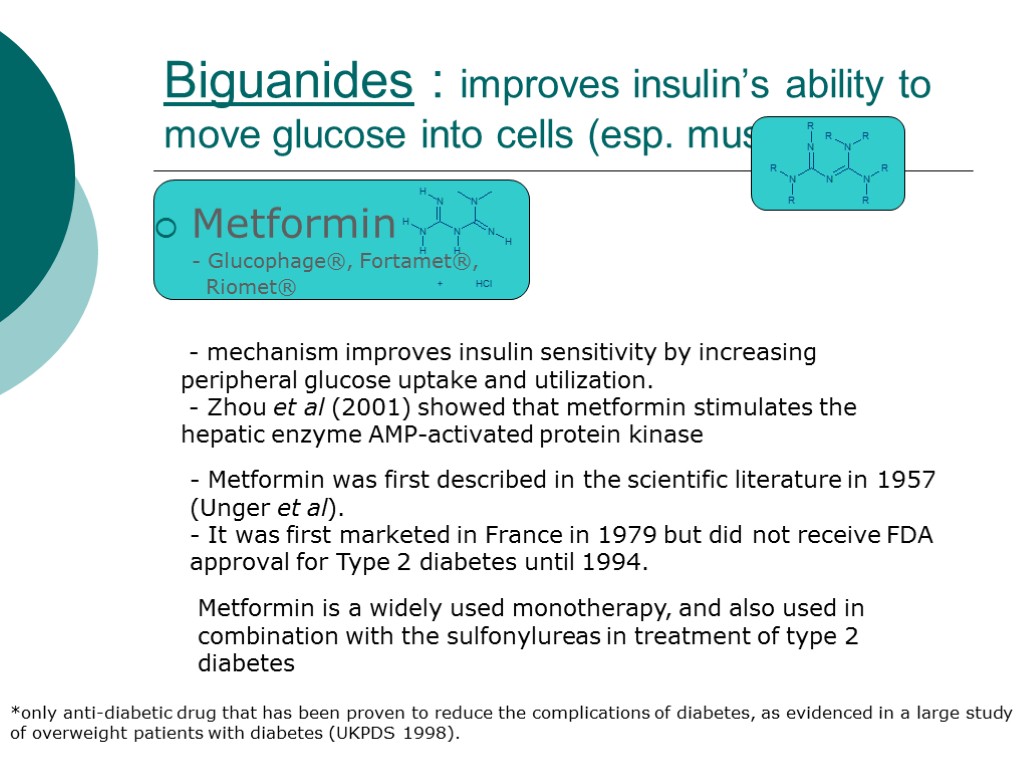
Biguanides : improves insulin’s ability to move glucose into cells (esp. muscle) Metformin - Glucophage®, Fortamet®, Riomet® *only anti-diabetic drug that has been proven to reduce the complications of diabetes, as evidenced in a large study of overweight patients with diabetes (UKPDS 1998). - Metformin was first described in the scientific literature in 1957 (Unger et al). - It was first marketed in France in 1979 but did not receive FDA approval for Type 2 diabetes until 1994. - mechanism improves insulin sensitivity by increasing peripheral glucose uptake and utilization. - Zhou et al (2001) showed that metformin stimulates the hepatic enzyme AMP-activated protein kinase Metformin is a widely used monotherapy, and also used in combination with the sulfonylureas in treatment of type 2 diabetes
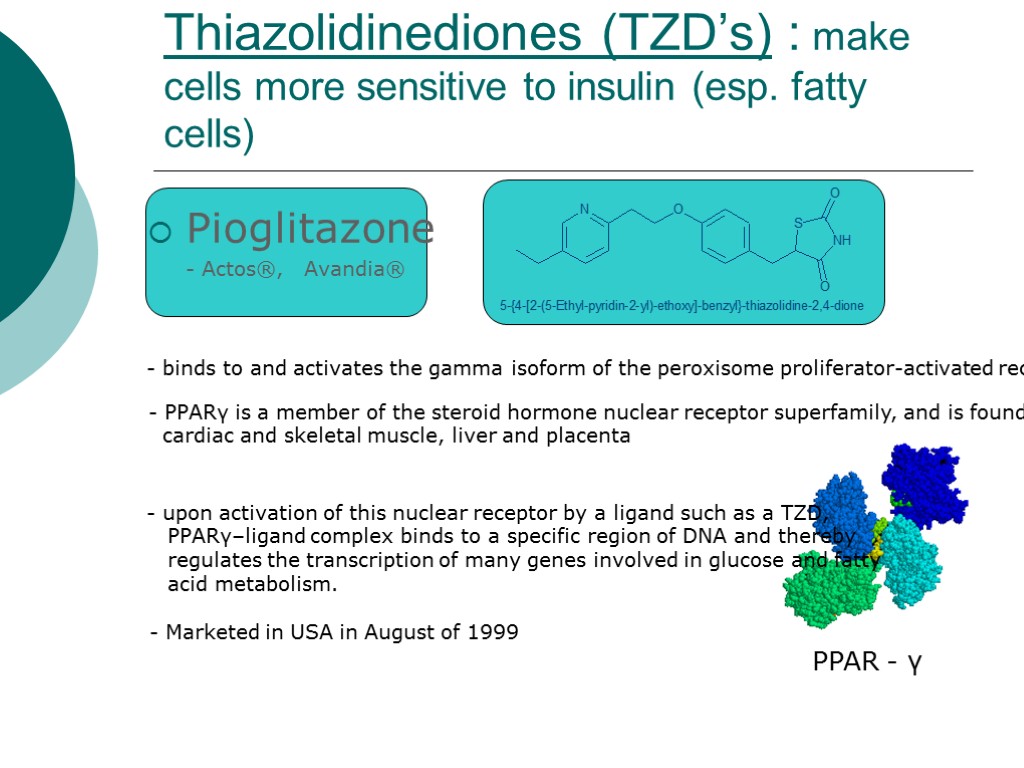
Thiazolidinediones (TZD’s) : make cells more sensitive to insulin (esp. fatty cells) Pioglitazone - Actos®, Avandia® - binds to and activates the gamma isoform of the peroxisome proliferator-activated receptor (PPARγ). - PPARγ is a member of the steroid hormone nuclear receptor superfamily, and is found in adipose tissue, cardiac and skeletal muscle, liver and placenta PPAR - γ upon activation of this nuclear receptor by a ligand such as a TZD, PPARγ–ligand complex binds to a specific region of DNA and thereby regulates the transcription of many genes involved in glucose and fatty acid metabolism. - Marketed in USA in August of 1999
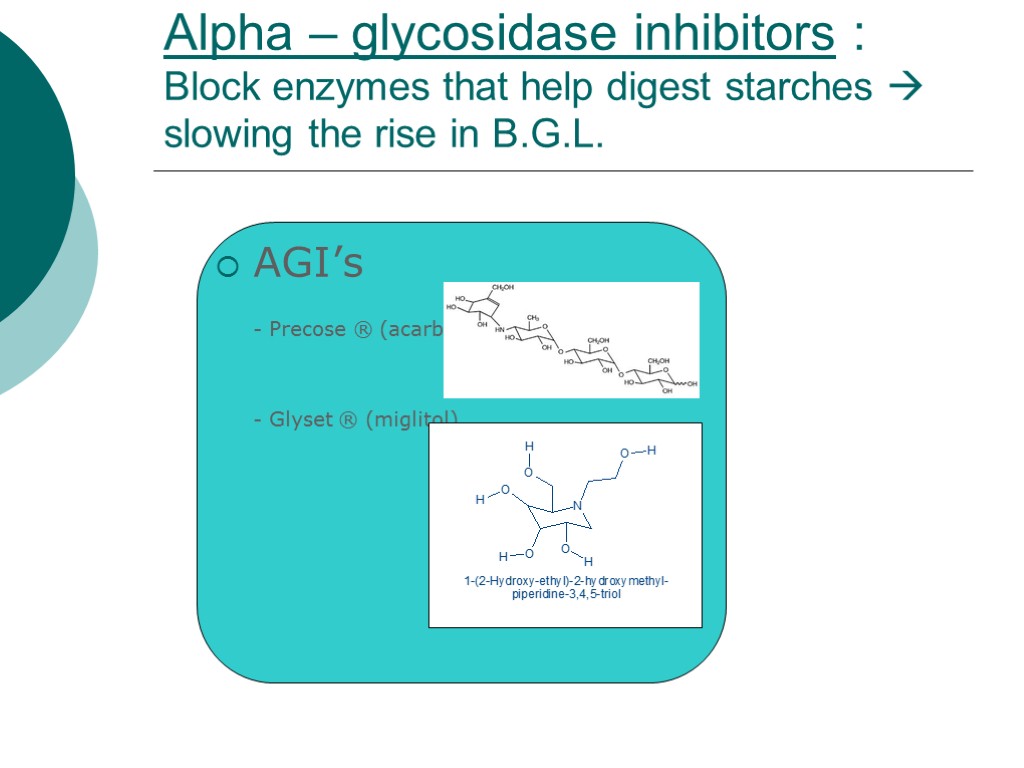
Αlpha – glycosidase inhibitors : Block enzymes that help digest starches slowing the rise in B.G.L. AGI’s - Precose ® (acarbose), - Glyset ® (miglitol)
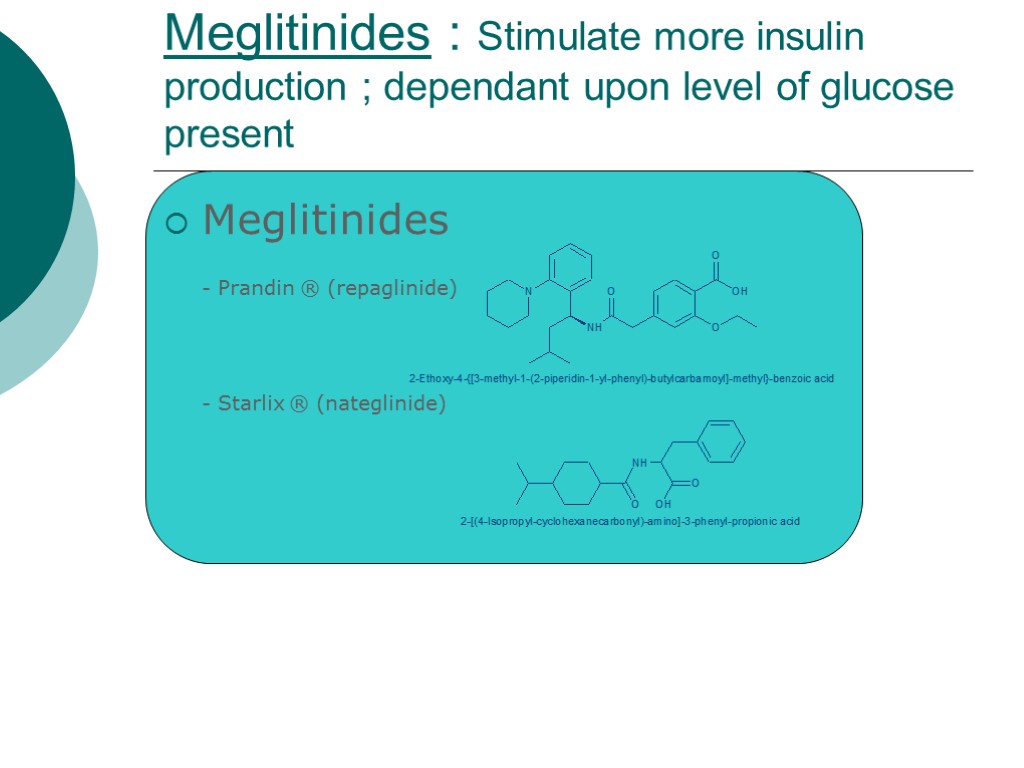
Meglitinides : Stimulate more insulin production ; dependant upon level of glucose present Meglitinides - Prandin ® (repaglinide) - Starlix ® (nateglinide)
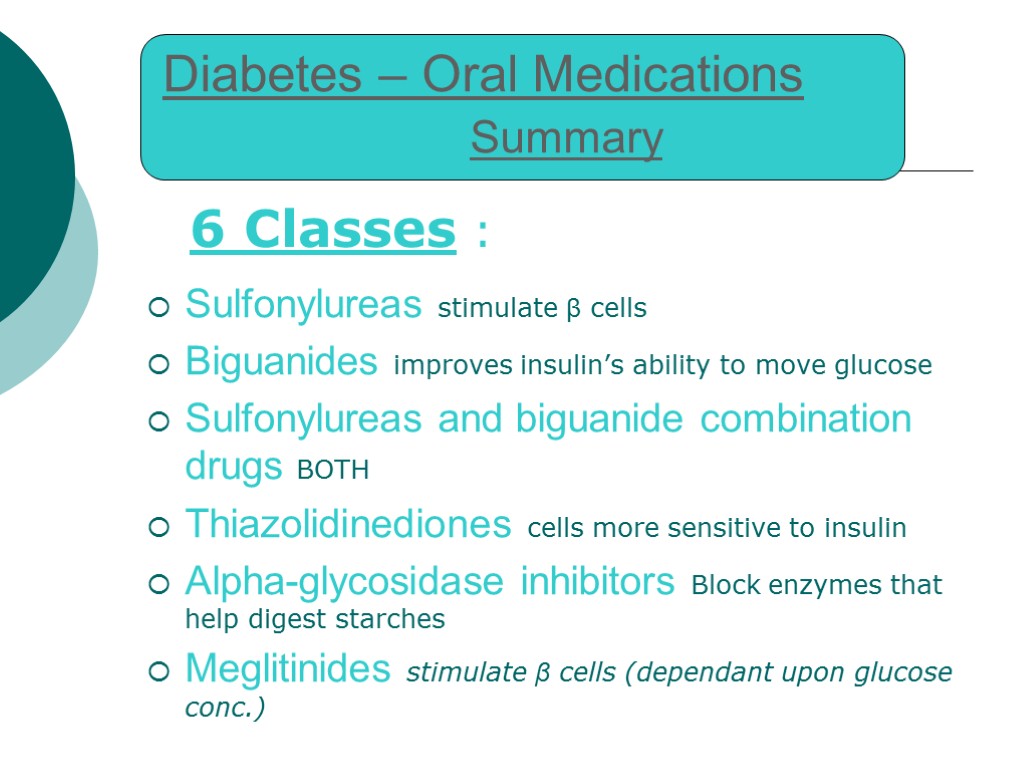
Diabetes – Oral Medications Summary 6 Classes : Sulfonylureas stimulate β cells Biguanides improves insulin’s ability to move glucose Sulfonylureas and biguanide combination drugs BOTH Thiazolidinediones cells more sensitive to insulin Alpha-glycosidase inhibitors Block enzymes that help digest starches Meglitinides stimulate β cells (dependant upon glucose conc.)
In Conclusion : 2 major types of diabetes (3 with Gestational) Type 1 => insulin dependant (5-10%) Type 2 => may treat with oral medication which may alter insulin production &/or sensitivity ; disease often succumbs to insulin dependence (>90%)
diabetes_mellitus.happa.ppt
- Количество слайдов: 42

