a3f5df26ff72f31e3a8b8117b449bd43.ppt
- Количество слайдов: 1
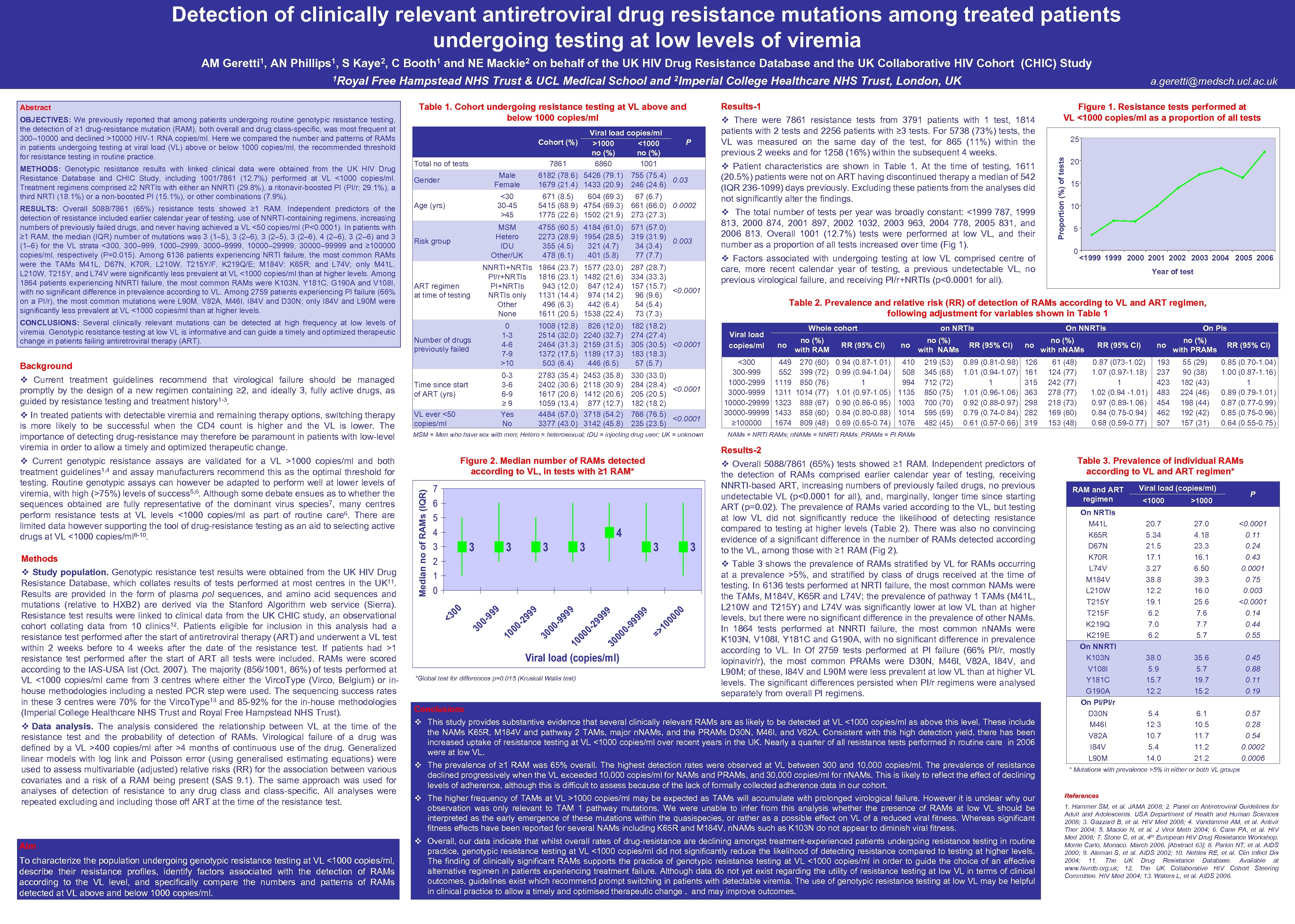 Detection of clinically relevant antiretroviral drug resistance mutations among treated patients undergoing testing at low levels of viremia AM Geretti 1, AN Phillips 1, S Kaye 2, C Booth 1 and NE Mackie 2 on behalf of the UK HIV Drug Resistance Database and the UK Collaborative HIV Cohort (CHIC) Study Free Hampstead NHS Trust & UCL Medical School and 2 Imperial College Healthcare NHS Trust, London, UK Abstract OBJECTIVES: We previously reported that among patients undergoing routine genotypic resistance testing, the detection of ≥ 1 drug-resistance mutation (RAM), both overall and drug class-specific, was most frequent at 300– 10000 and declined >10000 HIV-1 RNA copies/ml. Here we compared the number and patterns of RAMs in patients undergoing testing at viral load (VL) above or below 1000 copies/ml, the recommended threshold for resistance testing in routine practice. METHODS: Genotypic resistance results with linked clinical data were obtained from the UK HIV Drug Resistance Database and CHIC Study, including 1001/7861 (12. 7%) performed at VL <1000 copies/ml. Treatment regimens comprised ≥ 2 NRTIs with either an NNRTI (29. 8%), a ritonavir-boosted PI (PI/r; 29. 1%), a third NRTI (18. 1%) or a non-boosted PI (15. 1%), or other combinations (7. 9%). RESULTS: Overall 5088/7861 (65%) resistance tests showed ≥ 1 RAM. Independent predictors of the detection of resistance included earlier calendar year of testing, use of NNRTI-containing regimens, increasing numbers of previously failed drugs, and never having achieved a VL <50 copies/ml (P<0. 0001). In patients with ≥ 1 RAM, the median (IQR) number of mutations was 3 (1– 5), 3 (2– 6), 3 (2– 5), 3 (2– 6), 4 (2– 6), 3 (2– 6) and 3 (1– 6) for the VL strata <300, 300– 999, 1000– 2999, 3000– 9999, 10000– 29999, 30000– 99999 and ≥ 100000 copies/ml, respectively (P=0. 015). Among 6136 patients experiencing NRTI failure, the most common RAMs were the TAMs M 41 L, D 67 N, K 70 R, L 210 W, T 215 Y/F, K 219 Q/E; M 184 V; K 65 R; and L 74 V; only M 41 L, L 210 W, T 215 Y, and L 74 V were significantly less prevalent at VL <1000 copies/ml than at higher levels. Among 1864 patients experiencing NNRTI failure, the most common RAMs were K 103 N, Y 181 C, G 190 A and V 108 I, with no significant difference in prevalence according to VL. Among 2759 patients experiencing PI failure (66% on a PI/r), the most common mutations were L 90 M, V 82 A, M 46 I, I 84 V and D 30 N; only I 84 V and L 90 M were significantly less prevalent at VL <1000 copies/ml than at higher levels. CONCLUSIONS: Several clinically relevant mutations can be detected at high frequency at low levels of viremia. Genotypic resistance testing at low VL is informative and can guide a timely and optimized therapeutic change in patients failing antiretroviral therapy (ART). Table 1. Cohort undergoing resistance testing at VL above and below 1000 copies/ml Cohort (%) Total no of tests 6182 (78. 6) 5426 (79. 1) 1679 (21. 4) 1433 (20. 9) 755 (75. 4) 0. 03 246 (24. 6) <30 30 -45 >45 671 (8. 5) 604 (69. 3) 5415 (68. 9) 4754 (69. 3) 1775 (22. 6) 1502 (21. 9) 67 (6. 7) 661 (66. 0) 0. 0002 273 (27. 3) MSM Hetero IDU Other/UK 4755 (60. 5) 4184 (61. 0) 2273 (28. 9) 1954 (28. 5) 355 (4. 5) 321 (4. 7) 478 (6. 1) 401 (5. 8) 571 (57. 0) 319 (31. 9) 0. 003 34 (3. 4) 77 (7. 7) ART regimen at time of testing NNRTI+NRTIs PI/r+NRTIs PI+NRTIs only Other None 1864 (23. 7) 1816 (23. 1) 943 (12. 0) 1131 (14. 4) 496 (6. 3) 1611 (20. 5) 1577 (23. 0) 1482 (21. 6) 847 (12. 4) 974 (14. 2) 442 (6. 4) 1538 (22. 4) 287 (28. 7) 334 (33. 3) 157 (15. 7) <0. 0001 96 (9. 6) 54 (5. 4) 73 (7. 3) Number of drugs previously failed 0 1 -3 4 -6 7 -9 >10 1008 (12. 8) 2514 (32. 0) 2464 (31. 3) 1372 (17. 5) 503 (6. 4) 826 (12. 0) 2240 (32. 7) 2159 (31. 5) 1189 (17. 3) 446 (6. 5) 182 (18. 2) 274 (27. 4) 305 (30. 5) <0. 0001 183 (18. 3) 57 (5. 7) 0 -3 3 -6 6 -9 ≥ 9 Yes No 2783 (35. 4) 2402 (30. 6) 1617 (20. 6) 1059 (13. 4) 4484 (57. 0) 3377 (43. 0) 2453 (35. 8) 2118 (30. 9) 1412 (20. 6) 877 (12. 7) 3718 (54. 2) 3142 (45. 8) 330 (33. 0) 284 (28. 4) <0. 0001 205 (20. 5) 182 (18. 2) 766 (76. 5) <0. 0001 235 (23. 5) Gender Age (yrs) Risk group v Study population. Genotypic resistance test results were obtained from the UK HIV Drug Resistance Database, which collates results of tests performed at most centres in the UK 11. Results are provided in the form of plasma pol sequences, and amino acid sequences and mutations (relative to HXB 2) are derived via the Stanford Algorithm web service (Sierra). Resistance test results were linked to clinical data from the UK CHIC study, an observational cohort collating data from 10 clinics 12. Patients eligible for inclusion in this analysis had a resistance test performed after the start of antiretroviral therapy (ART) and underwent a VL test within 2 weeks before to 4 weeks after the date of the resistance test. If patients had >1 resistance test performed after the start of ART all tests were included. RAMs were scored according to the IAS-USA list (Oct. 2007). The majority (856/1001, 86%) of tests performed at VL <1000 copies/ml came from 3 centres where either the Virco. Type (Virco, Belgium) or inhouse methodologies including a nested PCR step were used. The sequencing success rates in these 3 centres were 70% for the Virco. Type 13 and 85 -92% for the in-house methodologies (Imperial College Healthcare NHS Trust and Royal Free Hampstead NHS Trust). v Data analysis. The analysis considered the relationship between VL at the time of the resistance test and the probability of detection of RAMs. Virological failure of a drug was defined by a VL >400 copies/ml after >4 months of continuous use of the drug. Generalized linear models with log link and Poisson error (using generalised estimating equations) were used to assess multivariable (adjusted) relative risks (RR) for the association between various covariates and a risk of a RAM being present (SAS 9. 1). The same approach was used for analyses of detection of resistance to any drug class and class-specific. All analyses were repeated excluding and including those off ART at the time of the resistance test. Aim To characterize the population undergoing genotypic resistance testing at VL <1000 copies/ml, describe their resistance profiles, identify factors associated with the detection of RAMs according to the VL level, and specifically compare the numbers and patterns of RAMs detected at VL above and below 1000 copies/ml. Time since start of ART (yrs) VL ever <50 copies/ml MSM = Men who have sex with men; Hetero = heterosexual; IDU = injecting drug user; UK = unknown Results-1 v There were 7861 resistance tests from 3791 patients with 1 test, 1814 patients with 2 tests and 2256 patients with ≥ 3 tests. For 5738 (73%) tests, the VL was measured on the same day of the test, for 865 (11%) within the previous 2 weeks and for 1258 (16%) within the subsequent 4 weeks. v Patient characteristics are shown in Table 1. At the time of testing, 1611 (20. 5%) patients were not on ART having discontinued therapy a median of 542 (IQR 236 -1099) days previously. Excluding these patients from the analyses did not significantly alter the findings. v The total number of tests per year was broadly constant: <1999 787, 1999 813, 2000 874, 2001 897, 2002 1032, 2003 963, 2004 778, 2005 831, and 2006 813. Overall 1001 (12. 7%) tests were performed at low VL, and their number as a proportion of all tests increased over time (Fig 1). v Factors associated with undergoing testing at low VL comprised centre of care, more recent calendar year of testing, a previous undetectable VL, no previous virological failure, and receiving PI/r+NRTIs (p<0. 0001 for all). Figure 1. Resistance tests performed at VL <1000 copies/ml as a proportion of all tests 25 20 15 10 5 0 <1999 2000 2001 2002 2003 2004 2005 2006 Year of test Table 2. Prevalence and relative risk (RR) of detection of RAMs according to VL and ART regimen, following adjustment for variables shown in Table 1 Whole cohort on NRTIs On NNRTIs On PIs Viral load copies/ml no no (%) with RAM RR (95% CI) no no (%) with NAMs RR (95% CI) no no (%) with n. NAMs RR (95% CI) no no (%) with PRAMs RR (95% CI) <300 300 -999 1000 -2999 3000 -9999 10000 -29999 30000 -99999 ≥ 100000 449 552 1119 1311 1323 1433 1674 270 (60) 399 (72) 850 (76) 1014 (77) 888 (67) 858 (60) 809 (48) 0. 94 (0. 87 -1. 01) 0. 99 (0. 94 -1. 04) 1 1. 01 (0. 97 -1. 05) 0. 90 (0. 86 -0. 95) 0. 84 (0. 80 -0. 88) 0. 69 (0. 65 -0. 74) 410 508 994 1135 1003 1014 1076 219 (53) 345 (68) 712 (72) 850 (75) 700 (70) 595 (59) 482 (45) 0. 89 (0. 81 -0. 98) 1. 01 (0. 94 -1. 07) 1 1. 01 (0. 96 -1. 06) 0. 92 (0. 88 -0. 97) 0. 79 (0. 74 -0. 84) 0. 61 (0. 57 -0. 66) 126 161 315 363 298 282 319 61 (48) 124 (77) 242 (77) 278 (77) 218 (73) 169 (60) 153 (48) 0. 87 (073 -1. 02) 1. 07 (0. 97 -1. 18) 1 1. 02 (0. 94 -1. 01) 0. 97 (0. 89 -1. 06) 0. 84 (0. 75 -0. 94) 0. 68 (0. 59 -0. 77) 193 237 423 483 454 462 507 55 (29) 90 (38) 182 (43) 224 (46) 198 (44) 192 (42) 157 (31) 0. 85 (0. 70 -1. 04) 1. 00 (0. 87 -1. 16) 1 0. 89 (0. 79 -1. 01) 0. 87 (0. 77 -0. 99) 0. 85 (0. 75 -0. 96) 0. 64 (0. 55 -0. 75) NAMs = NRTI RAMs; n. NAMs = NNRTI RAMs; PRAMs = PI RAMs Results-2 Figure 2. Median number of RAMs detected according to VL, in tests with ≥ 1 RAM* Median no of RAMs (IQR) Methods P Male Female Background v Current treatment guidelines recommend that virological failure should be managed promptly by the design of a new regimen containing ≥ 2, and ideally 3, fully active drugs, as guided by resistance testing and treatment history 1 -3. v In treated patients with detectable viremia and remaining therapy options, switching therapy is more likely to be successful when the CD 4 count is higher and the VL is lower. The importance of detecting drug-resistance may therefore be paramount in patients with low-level viremia in order to allow a timely and optimized therapeutic change. v Current genotypic resistance assays are validated for a VL >1000 copies/ml and both treatment guidelines 1, 4 and assay manufacturers recommend this as the optimal threshold for testing. Routine genotypic assays can however be adapted to perform well at lower levels of viremia, with high (>75%) levels of success 5, 6. Although some debate ensues as to whether the sequences obtained are fully representative of the dominant virus species 7, many centres perform resistance tests at VL levels <1000 copies/ml as part of routine care 6. There are limited data however supporting the tool of drug-resistance testing as an aid to selecting active drugs at VL <1000 copies/ml 8 -10. 7861 Viral load copies/ml >1000 <1000 no (%) 6860 1001 a. geretti@medsch. ucl. ac. uk Proportion (%) of tests 1 Royal *Global test for differences p=0. 015 (Kruskall Wallis test) v Overall 5088/7861 (65%) tests showed ≥ 1 RAM. Independent predictors of the detection of RAMs comprised earlier calendar year of testing, receiving NNRTI-based ART, increasing numbers of previously failed drugs, no previous undetectable VL (p<0. 0001 for all), and, marginally, longer time since starting ART (p=0. 02). The prevalence of RAMs varied according to the VL, but testing at low VL did not significantly reduce the likelihood of detecting resistance compared to testing at higher levels (Table 2). There was also no convincing evidence of a significant difference in the number of RAMs detected according to the VL, among those with ≥ 1 RAM (Fig 2). v Table 3 shows the prevalence of RAMs stratified by VL for RAMs occurring at a prevalence >5%, and stratified by class of drugs received at the time of testing. In 6136 tests performed at NRTI failure, the most common NAMs were the TAMs, M 184 V, K 65 R and L 74 V; the prevalence of pathway 1 TAMs (M 41 L, L 210 W and T 215 Y) and L 74 V was significantly lower at low VL than at higher levels, but there were no significant difference in the prevalence of other NAMs. In 1864 tests performed at NNRTI failure, the most common n. NAMs were K 103 N, V 108 I, Y 181 C and G 190 A, with no significant difference in prevalence according to VL. In Of 2759 tests performed at PI failure (66% PI/r, mostly lopinavir/r), the most common PRAMs were D 30 N, M 46 I, V 82 A, I 84 V, and L 90 M; of these, I 84 V and L 90 M were less prevalent at low VL than at higher VL levels. The significant differences persisted when PI/r regimens were analysed separately from overall PI regimens. Conclusions v This study provides substantive evidence that several clinically relevant RAMs are as likely to be detected at VL <1000 copies/ml as above this level. These include the NAMs K 65 R, M 184 V and pathway 2 TAMs, major n. NAMs, and the PRAMs D 30 N, M 46 I, and V 82 A. Consistent with this high detection yield, there has been increased uptake of resistance testing at VL <1000 copies/ml over recent years in the UK. Nearly a quarter of all resistance tests performed in routine care in 2006 were at low VL. v The prevalence of ≥ 1 RAM was 65% overall. The highest detection rates were observed at VL between 300 and 10, 000 copies/ml. The prevalence of resistance declined progressively when the VL exceeded 10, 000 copies/ml for NAMs and PRAMs, and 30, 000 copies/ml for n. NAMs. This is likely to reflect the effect of declining levels of adherence, although this is difficult to assess because of the lack of formally collected adherence data in our cohort. v The higher frequency of TAMs at VL >1000 copies/ml may be expected as TAMs will accumulate with prolonged virological failure. However it is unclear why our observation was only relevant to TAM 1 pathway mutations. We were unable to infer from this analysis whether the presence of RAMs at low VL should be interpreted as the early emergence of these mutations within the quasispecies, or rather as a possible effect on VL of a reduced viral fitness. Whereas significant fitness effects have been reported for several NAMs including K 65 R and M 184 V, n. NAMs such as K 103 N do not appear to diminish viral fitness. v Overall, our data indicate that whilst overall rates of drug-resistance are declining amongst treatment-experienced patients undergoing resistance testing in routine practice, genotypic resistance testing at VL <1000 copies/ml did not significantly reduce the likelihood of detecting resistance compared to testing at higher levels. The finding of clinically significant RAMs supports the practice of genotypic resistance testing at VL <1000 copies/ml in order to guide the choice of an effective alternative regimen in patients experiencing treatment failure. Although data do not yet exist regarding the utility of resistance testing at low VL in terms of clinical outcomes, guidelines exist which recommend prompt switching in patients with detectable viremia. The use of genotypic resistance testing at low VL may be helpful in clinical practice to allow a timely and optimised therapeutic change , and may improve outcomes. Table 3. Prevalence of individual RAMs according to VL and ART regimen* RAM and ART regimen On NRTIs M 41 L K 65 R D 67 N K 70 R L 74 V M 184 V L 210 W T 215 Y T 215 F K 219 Q K 219 E On NNRTI K 103 N V 108 I Y 181 C G 190 A On PI/PI/r D 30 N M 46 I V 82 A I 84 V L 90 M Viral load (copies/ml) P <1000 >1000 20. 7 5. 34 21. 5 17. 1 3. 27 38. 8 12. 2 19. 1 6. 2 7. 0 6. 2 27. 0 4. 18 23. 3 16. 1 6. 50 39. 3 16. 0 25. 6 7. 7 5. 7 <0. 0001 0. 11 0. 24 0. 43 0. 0001 0. 75 0. 003 <0. 0001 0. 14 0. 44 0. 55 38. 0 5. 9 15. 7 12. 2 35. 6 5. 7 19. 7 15. 2 0. 45 0. 88 0. 11 0. 19 5. 4 12. 3 10. 7 5. 4 14. 0 6. 1 10. 5 11. 7 11. 2 21. 2 0. 57 0. 28 0. 54 0. 0002 0. 0006 * Mutations with prevalence >5% in either or both VL groups References 1. Hammer SM, et al. JAMA 2008; 2. Panel on Antiretroviral Guidelines for Adult and Adolescents. USA Department of Health and Human Sciences 2008; 3. Gazzard B, et al. HIV Med 2008; 4. Vandamme AM, et al. Antivir Ther 2004; 5. Mackie N, et al. J Virol Meth 2004; 6. Cane PA, et al. HIV Med 2008; 7. Stone C, et al, 4 th European HIV Drug Resistance Workshop. Monte Carlo, Monaco. March 2006. [Abstract 63]; 8. Parkin NT, et al. AIDS 2000; 9. Aleman S, et al. AIDS 2002; 10. Nettles RE, et al. Clin Infect Dis 2004; 11. The UK Drug Resistance Database. Available at www. hivrdb. org. uk; 12. The UK Collaborative HIV Cohort Steering Committee. HIV Med 2004; 13. Waters L, et al. AIDS 2006.
Detection of clinically relevant antiretroviral drug resistance mutations among treated patients undergoing testing at low levels of viremia AM Geretti 1, AN Phillips 1, S Kaye 2, C Booth 1 and NE Mackie 2 on behalf of the UK HIV Drug Resistance Database and the UK Collaborative HIV Cohort (CHIC) Study Free Hampstead NHS Trust & UCL Medical School and 2 Imperial College Healthcare NHS Trust, London, UK Abstract OBJECTIVES: We previously reported that among patients undergoing routine genotypic resistance testing, the detection of ≥ 1 drug-resistance mutation (RAM), both overall and drug class-specific, was most frequent at 300– 10000 and declined >10000 HIV-1 RNA copies/ml. Here we compared the number and patterns of RAMs in patients undergoing testing at viral load (VL) above or below 1000 copies/ml, the recommended threshold for resistance testing in routine practice. METHODS: Genotypic resistance results with linked clinical data were obtained from the UK HIV Drug Resistance Database and CHIC Study, including 1001/7861 (12. 7%) performed at VL <1000 copies/ml. Treatment regimens comprised ≥ 2 NRTIs with either an NNRTI (29. 8%), a ritonavir-boosted PI (PI/r; 29. 1%), a third NRTI (18. 1%) or a non-boosted PI (15. 1%), or other combinations (7. 9%). RESULTS: Overall 5088/7861 (65%) resistance tests showed ≥ 1 RAM. Independent predictors of the detection of resistance included earlier calendar year of testing, use of NNRTI-containing regimens, increasing numbers of previously failed drugs, and never having achieved a VL <50 copies/ml (P<0. 0001). In patients with ≥ 1 RAM, the median (IQR) number of mutations was 3 (1– 5), 3 (2– 6), 3 (2– 5), 3 (2– 6), 4 (2– 6), 3 (2– 6) and 3 (1– 6) for the VL strata <300, 300– 999, 1000– 2999, 3000– 9999, 10000– 29999, 30000– 99999 and ≥ 100000 copies/ml, respectively (P=0. 015). Among 6136 patients experiencing NRTI failure, the most common RAMs were the TAMs M 41 L, D 67 N, K 70 R, L 210 W, T 215 Y/F, K 219 Q/E; M 184 V; K 65 R; and L 74 V; only M 41 L, L 210 W, T 215 Y, and L 74 V were significantly less prevalent at VL <1000 copies/ml than at higher levels. Among 1864 patients experiencing NNRTI failure, the most common RAMs were K 103 N, Y 181 C, G 190 A and V 108 I, with no significant difference in prevalence according to VL. Among 2759 patients experiencing PI failure (66% on a PI/r), the most common mutations were L 90 M, V 82 A, M 46 I, I 84 V and D 30 N; only I 84 V and L 90 M were significantly less prevalent at VL <1000 copies/ml than at higher levels. CONCLUSIONS: Several clinically relevant mutations can be detected at high frequency at low levels of viremia. Genotypic resistance testing at low VL is informative and can guide a timely and optimized therapeutic change in patients failing antiretroviral therapy (ART). Table 1. Cohort undergoing resistance testing at VL above and below 1000 copies/ml Cohort (%) Total no of tests 6182 (78. 6) 5426 (79. 1) 1679 (21. 4) 1433 (20. 9) 755 (75. 4) 0. 03 246 (24. 6) <30 30 -45 >45 671 (8. 5) 604 (69. 3) 5415 (68. 9) 4754 (69. 3) 1775 (22. 6) 1502 (21. 9) 67 (6. 7) 661 (66. 0) 0. 0002 273 (27. 3) MSM Hetero IDU Other/UK 4755 (60. 5) 4184 (61. 0) 2273 (28. 9) 1954 (28. 5) 355 (4. 5) 321 (4. 7) 478 (6. 1) 401 (5. 8) 571 (57. 0) 319 (31. 9) 0. 003 34 (3. 4) 77 (7. 7) ART regimen at time of testing NNRTI+NRTIs PI/r+NRTIs PI+NRTIs only Other None 1864 (23. 7) 1816 (23. 1) 943 (12. 0) 1131 (14. 4) 496 (6. 3) 1611 (20. 5) 1577 (23. 0) 1482 (21. 6) 847 (12. 4) 974 (14. 2) 442 (6. 4) 1538 (22. 4) 287 (28. 7) 334 (33. 3) 157 (15. 7) <0. 0001 96 (9. 6) 54 (5. 4) 73 (7. 3) Number of drugs previously failed 0 1 -3 4 -6 7 -9 >10 1008 (12. 8) 2514 (32. 0) 2464 (31. 3) 1372 (17. 5) 503 (6. 4) 826 (12. 0) 2240 (32. 7) 2159 (31. 5) 1189 (17. 3) 446 (6. 5) 182 (18. 2) 274 (27. 4) 305 (30. 5) <0. 0001 183 (18. 3) 57 (5. 7) 0 -3 3 -6 6 -9 ≥ 9 Yes No 2783 (35. 4) 2402 (30. 6) 1617 (20. 6) 1059 (13. 4) 4484 (57. 0) 3377 (43. 0) 2453 (35. 8) 2118 (30. 9) 1412 (20. 6) 877 (12. 7) 3718 (54. 2) 3142 (45. 8) 330 (33. 0) 284 (28. 4) <0. 0001 205 (20. 5) 182 (18. 2) 766 (76. 5) <0. 0001 235 (23. 5) Gender Age (yrs) Risk group v Study population. Genotypic resistance test results were obtained from the UK HIV Drug Resistance Database, which collates results of tests performed at most centres in the UK 11. Results are provided in the form of plasma pol sequences, and amino acid sequences and mutations (relative to HXB 2) are derived via the Stanford Algorithm web service (Sierra). Resistance test results were linked to clinical data from the UK CHIC study, an observational cohort collating data from 10 clinics 12. Patients eligible for inclusion in this analysis had a resistance test performed after the start of antiretroviral therapy (ART) and underwent a VL test within 2 weeks before to 4 weeks after the date of the resistance test. If patients had >1 resistance test performed after the start of ART all tests were included. RAMs were scored according to the IAS-USA list (Oct. 2007). The majority (856/1001, 86%) of tests performed at VL <1000 copies/ml came from 3 centres where either the Virco. Type (Virco, Belgium) or inhouse methodologies including a nested PCR step were used. The sequencing success rates in these 3 centres were 70% for the Virco. Type 13 and 85 -92% for the in-house methodologies (Imperial College Healthcare NHS Trust and Royal Free Hampstead NHS Trust). v Data analysis. The analysis considered the relationship between VL at the time of the resistance test and the probability of detection of RAMs. Virological failure of a drug was defined by a VL >400 copies/ml after >4 months of continuous use of the drug. Generalized linear models with log link and Poisson error (using generalised estimating equations) were used to assess multivariable (adjusted) relative risks (RR) for the association between various covariates and a risk of a RAM being present (SAS 9. 1). The same approach was used for analyses of detection of resistance to any drug class and class-specific. All analyses were repeated excluding and including those off ART at the time of the resistance test. Aim To characterize the population undergoing genotypic resistance testing at VL <1000 copies/ml, describe their resistance profiles, identify factors associated with the detection of RAMs according to the VL level, and specifically compare the numbers and patterns of RAMs detected at VL above and below 1000 copies/ml. Time since start of ART (yrs) VL ever <50 copies/ml MSM = Men who have sex with men; Hetero = heterosexual; IDU = injecting drug user; UK = unknown Results-1 v There were 7861 resistance tests from 3791 patients with 1 test, 1814 patients with 2 tests and 2256 patients with ≥ 3 tests. For 5738 (73%) tests, the VL was measured on the same day of the test, for 865 (11%) within the previous 2 weeks and for 1258 (16%) within the subsequent 4 weeks. v Patient characteristics are shown in Table 1. At the time of testing, 1611 (20. 5%) patients were not on ART having discontinued therapy a median of 542 (IQR 236 -1099) days previously. Excluding these patients from the analyses did not significantly alter the findings. v The total number of tests per year was broadly constant: <1999 787, 1999 813, 2000 874, 2001 897, 2002 1032, 2003 963, 2004 778, 2005 831, and 2006 813. Overall 1001 (12. 7%) tests were performed at low VL, and their number as a proportion of all tests increased over time (Fig 1). v Factors associated with undergoing testing at low VL comprised centre of care, more recent calendar year of testing, a previous undetectable VL, no previous virological failure, and receiving PI/r+NRTIs (p<0. 0001 for all). Figure 1. Resistance tests performed at VL <1000 copies/ml as a proportion of all tests 25 20 15 10 5 0 <1999 2000 2001 2002 2003 2004 2005 2006 Year of test Table 2. Prevalence and relative risk (RR) of detection of RAMs according to VL and ART regimen, following adjustment for variables shown in Table 1 Whole cohort on NRTIs On NNRTIs On PIs Viral load copies/ml no no (%) with RAM RR (95% CI) no no (%) with NAMs RR (95% CI) no no (%) with n. NAMs RR (95% CI) no no (%) with PRAMs RR (95% CI) <300 300 -999 1000 -2999 3000 -9999 10000 -29999 30000 -99999 ≥ 100000 449 552 1119 1311 1323 1433 1674 270 (60) 399 (72) 850 (76) 1014 (77) 888 (67) 858 (60) 809 (48) 0. 94 (0. 87 -1. 01) 0. 99 (0. 94 -1. 04) 1 1. 01 (0. 97 -1. 05) 0. 90 (0. 86 -0. 95) 0. 84 (0. 80 -0. 88) 0. 69 (0. 65 -0. 74) 410 508 994 1135 1003 1014 1076 219 (53) 345 (68) 712 (72) 850 (75) 700 (70) 595 (59) 482 (45) 0. 89 (0. 81 -0. 98) 1. 01 (0. 94 -1. 07) 1 1. 01 (0. 96 -1. 06) 0. 92 (0. 88 -0. 97) 0. 79 (0. 74 -0. 84) 0. 61 (0. 57 -0. 66) 126 161 315 363 298 282 319 61 (48) 124 (77) 242 (77) 278 (77) 218 (73) 169 (60) 153 (48) 0. 87 (073 -1. 02) 1. 07 (0. 97 -1. 18) 1 1. 02 (0. 94 -1. 01) 0. 97 (0. 89 -1. 06) 0. 84 (0. 75 -0. 94) 0. 68 (0. 59 -0. 77) 193 237 423 483 454 462 507 55 (29) 90 (38) 182 (43) 224 (46) 198 (44) 192 (42) 157 (31) 0. 85 (0. 70 -1. 04) 1. 00 (0. 87 -1. 16) 1 0. 89 (0. 79 -1. 01) 0. 87 (0. 77 -0. 99) 0. 85 (0. 75 -0. 96) 0. 64 (0. 55 -0. 75) NAMs = NRTI RAMs; n. NAMs = NNRTI RAMs; PRAMs = PI RAMs Results-2 Figure 2. Median number of RAMs detected according to VL, in tests with ≥ 1 RAM* Median no of RAMs (IQR) Methods P Male Female Background v Current treatment guidelines recommend that virological failure should be managed promptly by the design of a new regimen containing ≥ 2, and ideally 3, fully active drugs, as guided by resistance testing and treatment history 1 -3. v In treated patients with detectable viremia and remaining therapy options, switching therapy is more likely to be successful when the CD 4 count is higher and the VL is lower. The importance of detecting drug-resistance may therefore be paramount in patients with low-level viremia in order to allow a timely and optimized therapeutic change. v Current genotypic resistance assays are validated for a VL >1000 copies/ml and both treatment guidelines 1, 4 and assay manufacturers recommend this as the optimal threshold for testing. Routine genotypic assays can however be adapted to perform well at lower levels of viremia, with high (>75%) levels of success 5, 6. Although some debate ensues as to whether the sequences obtained are fully representative of the dominant virus species 7, many centres perform resistance tests at VL levels <1000 copies/ml as part of routine care 6. There are limited data however supporting the tool of drug-resistance testing as an aid to selecting active drugs at VL <1000 copies/ml 8 -10. 7861 Viral load copies/ml >1000 <1000 no (%) 6860 1001 a. geretti@medsch. ucl. ac. uk Proportion (%) of tests 1 Royal *Global test for differences p=0. 015 (Kruskall Wallis test) v Overall 5088/7861 (65%) tests showed ≥ 1 RAM. Independent predictors of the detection of RAMs comprised earlier calendar year of testing, receiving NNRTI-based ART, increasing numbers of previously failed drugs, no previous undetectable VL (p<0. 0001 for all), and, marginally, longer time since starting ART (p=0. 02). The prevalence of RAMs varied according to the VL, but testing at low VL did not significantly reduce the likelihood of detecting resistance compared to testing at higher levels (Table 2). There was also no convincing evidence of a significant difference in the number of RAMs detected according to the VL, among those with ≥ 1 RAM (Fig 2). v Table 3 shows the prevalence of RAMs stratified by VL for RAMs occurring at a prevalence >5%, and stratified by class of drugs received at the time of testing. In 6136 tests performed at NRTI failure, the most common NAMs were the TAMs, M 184 V, K 65 R and L 74 V; the prevalence of pathway 1 TAMs (M 41 L, L 210 W and T 215 Y) and L 74 V was significantly lower at low VL than at higher levels, but there were no significant difference in the prevalence of other NAMs. In 1864 tests performed at NNRTI failure, the most common n. NAMs were K 103 N, V 108 I, Y 181 C and G 190 A, with no significant difference in prevalence according to VL. In Of 2759 tests performed at PI failure (66% PI/r, mostly lopinavir/r), the most common PRAMs were D 30 N, M 46 I, V 82 A, I 84 V, and L 90 M; of these, I 84 V and L 90 M were less prevalent at low VL than at higher VL levels. The significant differences persisted when PI/r regimens were analysed separately from overall PI regimens. Conclusions v This study provides substantive evidence that several clinically relevant RAMs are as likely to be detected at VL <1000 copies/ml as above this level. These include the NAMs K 65 R, M 184 V and pathway 2 TAMs, major n. NAMs, and the PRAMs D 30 N, M 46 I, and V 82 A. Consistent with this high detection yield, there has been increased uptake of resistance testing at VL <1000 copies/ml over recent years in the UK. Nearly a quarter of all resistance tests performed in routine care in 2006 were at low VL. v The prevalence of ≥ 1 RAM was 65% overall. The highest detection rates were observed at VL between 300 and 10, 000 copies/ml. The prevalence of resistance declined progressively when the VL exceeded 10, 000 copies/ml for NAMs and PRAMs, and 30, 000 copies/ml for n. NAMs. This is likely to reflect the effect of declining levels of adherence, although this is difficult to assess because of the lack of formally collected adherence data in our cohort. v The higher frequency of TAMs at VL >1000 copies/ml may be expected as TAMs will accumulate with prolonged virological failure. However it is unclear why our observation was only relevant to TAM 1 pathway mutations. We were unable to infer from this analysis whether the presence of RAMs at low VL should be interpreted as the early emergence of these mutations within the quasispecies, or rather as a possible effect on VL of a reduced viral fitness. Whereas significant fitness effects have been reported for several NAMs including K 65 R and M 184 V, n. NAMs such as K 103 N do not appear to diminish viral fitness. v Overall, our data indicate that whilst overall rates of drug-resistance are declining amongst treatment-experienced patients undergoing resistance testing in routine practice, genotypic resistance testing at VL <1000 copies/ml did not significantly reduce the likelihood of detecting resistance compared to testing at higher levels. The finding of clinically significant RAMs supports the practice of genotypic resistance testing at VL <1000 copies/ml in order to guide the choice of an effective alternative regimen in patients experiencing treatment failure. Although data do not yet exist regarding the utility of resistance testing at low VL in terms of clinical outcomes, guidelines exist which recommend prompt switching in patients with detectable viremia. The use of genotypic resistance testing at low VL may be helpful in clinical practice to allow a timely and optimised therapeutic change , and may improve outcomes. Table 3. Prevalence of individual RAMs according to VL and ART regimen* RAM and ART regimen On NRTIs M 41 L K 65 R D 67 N K 70 R L 74 V M 184 V L 210 W T 215 Y T 215 F K 219 Q K 219 E On NNRTI K 103 N V 108 I Y 181 C G 190 A On PI/PI/r D 30 N M 46 I V 82 A I 84 V L 90 M Viral load (copies/ml) P <1000 >1000 20. 7 5. 34 21. 5 17. 1 3. 27 38. 8 12. 2 19. 1 6. 2 7. 0 6. 2 27. 0 4. 18 23. 3 16. 1 6. 50 39. 3 16. 0 25. 6 7. 7 5. 7 <0. 0001 0. 11 0. 24 0. 43 0. 0001 0. 75 0. 003 <0. 0001 0. 14 0. 44 0. 55 38. 0 5. 9 15. 7 12. 2 35. 6 5. 7 19. 7 15. 2 0. 45 0. 88 0. 11 0. 19 5. 4 12. 3 10. 7 5. 4 14. 0 6. 1 10. 5 11. 7 11. 2 21. 2 0. 57 0. 28 0. 54 0. 0002 0. 0006 * Mutations with prevalence >5% in either or both VL groups References 1. Hammer SM, et al. JAMA 2008; 2. Panel on Antiretroviral Guidelines for Adult and Adolescents. USA Department of Health and Human Sciences 2008; 3. Gazzard B, et al. HIV Med 2008; 4. Vandamme AM, et al. Antivir Ther 2004; 5. Mackie N, et al. J Virol Meth 2004; 6. Cane PA, et al. HIV Med 2008; 7. Stone C, et al, 4 th European HIV Drug Resistance Workshop. Monte Carlo, Monaco. March 2006. [Abstract 63]; 8. Parkin NT, et al. AIDS 2000; 9. Aleman S, et al. AIDS 2002; 10. Nettles RE, et al. Clin Infect Dis 2004; 11. The UK Drug Resistance Database. Available at www. hivrdb. org. uk; 12. The UK Collaborative HIV Cohort Steering Committee. HIV Med 2004; 13. Waters L, et al. AIDS 2006.


