c94e06a79777241488b3478eee1149ca.ppt
- Количество слайдов: 66
 Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center End of life care around the world Charles Sprung MD
Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center End of life care around the world Charles Sprung MD
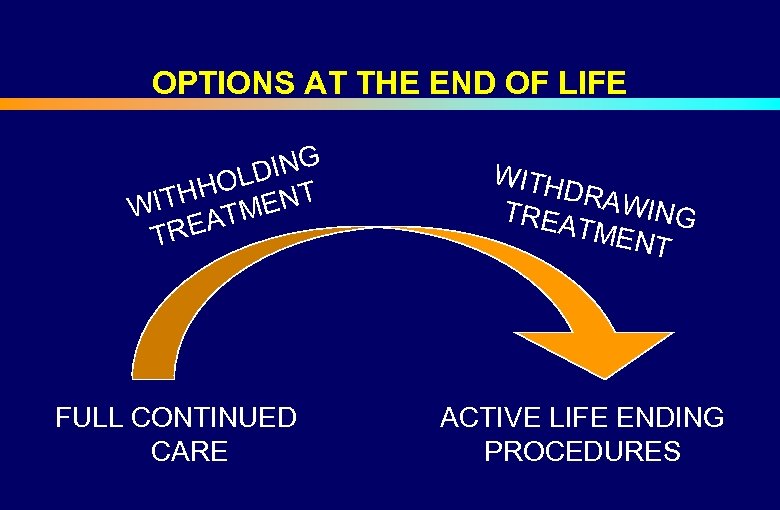 OPTIONS AT THE END OF LIFE DING HOL NT H WIT ATME TRE FULL CONTINUED CARE WITH DRAW ING TREA TMEN T ACTIVE LIFE ENDING PROCEDURES
OPTIONS AT THE END OF LIFE DING HOL NT H WIT ATME TRE FULL CONTINUED CARE WITH DRAW ING TREA TMEN T ACTIVE LIFE ENDING PROCEDURES
 END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
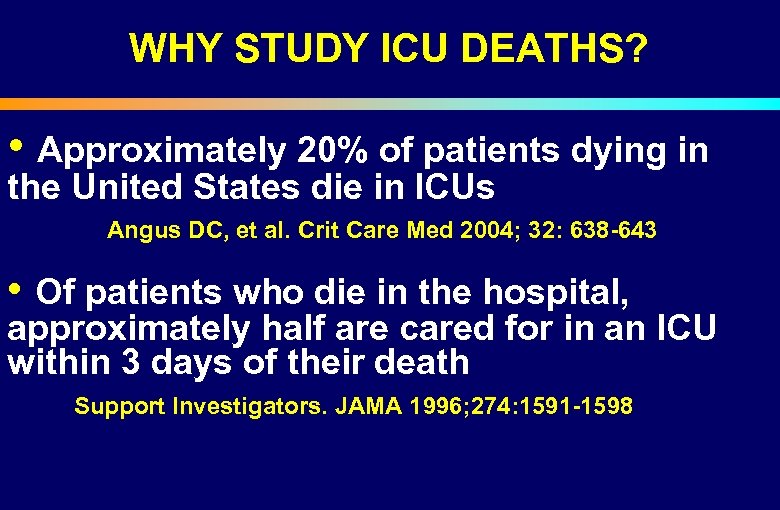 WHY STUDY ICU DEATHS? • Approximately 20% of patients dying in the United States die in ICUs Angus DC, et al. Crit Care Med 2004; 32: 638 -643 • Of patients who die in the hospital, approximately half are cared for in an ICU within 3 days of their death Support Investigators. JAMA 1996; 274: 1591 -1598
WHY STUDY ICU DEATHS? • Approximately 20% of patients dying in the United States die in ICUs Angus DC, et al. Crit Care Med 2004; 32: 638 -643 • Of patients who die in the hospital, approximately half are cared for in an ICU within 3 days of their death Support Investigators. JAMA 1996; 274: 1591 -1598
 END OF LIFE DECISION MAKING The majority of patients dying in ICUs do so after the decision to limit therapy Levin PD. Crit Care Med 2003; 31: S 1 -S 4
END OF LIFE DECISION MAKING The majority of patients dying in ICUs do so after the decision to limit therapy Levin PD. Crit Care Med 2003; 31: S 1 -S 4
 END OF LIFE DECISION MAKING IN DIFFERENT COUNTRIES • Majority of physicians withhold and withdraw treatments in North America and Europe Prendergast TJ. Am J Resp CCM 1998; 158: 1163 Sprung CL. JAMA 2003; 290: 790 • Physicians in Holland Belgium perform active euthanasia Hendin H. JAMA 1997; 277: 1720 Dellens L. LANCET 2000; 356: 1806 • Physicians withhold and do not withdraw therapies Eidelman LA. Intensive Care Med 1998; 24: 162 -166
END OF LIFE DECISION MAKING IN DIFFERENT COUNTRIES • Majority of physicians withhold and withdraw treatments in North America and Europe Prendergast TJ. Am J Resp CCM 1998; 158: 1163 Sprung CL. JAMA 2003; 290: 790 • Physicians in Holland Belgium perform active euthanasia Hendin H. JAMA 1997; 277: 1720 Dellens L. LANCET 2000; 356: 1806 • Physicians withhold and do not withdraw therapies Eidelman LA. Intensive Care Med 1998; 24: 162 -166
 END OF LIFE DECISION MAKING • Wide variations between countries, within cities and even in the same ICU • Explained by different physician values Cook DJ. JAMA 1995; 273: 703 -708
END OF LIFE DECISION MAKING • Wide variations between countries, within cities and even in the same ICU • Explained by different physician values Cook DJ. JAMA 1995; 273: 703 -708
 END OF LIFE DECISION MAKING • North American approach Autonomy • European approach Paternalistic
END OF LIFE DECISION MAKING • North American approach Autonomy • European approach Paternalistic
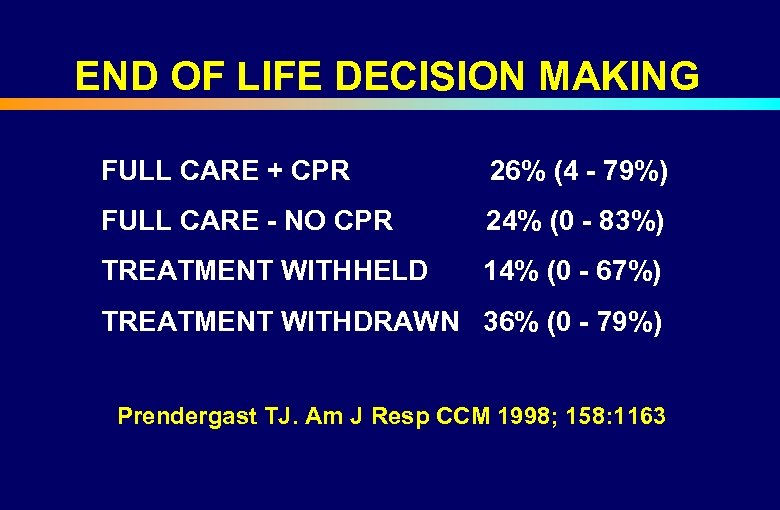 END OF LIFE DECISION MAKING FULL CARE + CPR 26% (4 - 79%) FULL CARE - NO CPR 24% (0 - 83%) TREATMENT WITHHELD 14% (0 - 67%) TREATMENT WITHDRAWN 36% (0 - 79%) Prendergast TJ. Am J Resp CCM 1998; 158: 1163
END OF LIFE DECISION MAKING FULL CARE + CPR 26% (4 - 79%) FULL CARE - NO CPR 24% (0 - 83%) TREATMENT WITHHELD 14% (0 - 67%) TREATMENT WITHDRAWN 36% (0 - 79%) Prendergast TJ. Am J Resp CCM 1998; 158: 1163
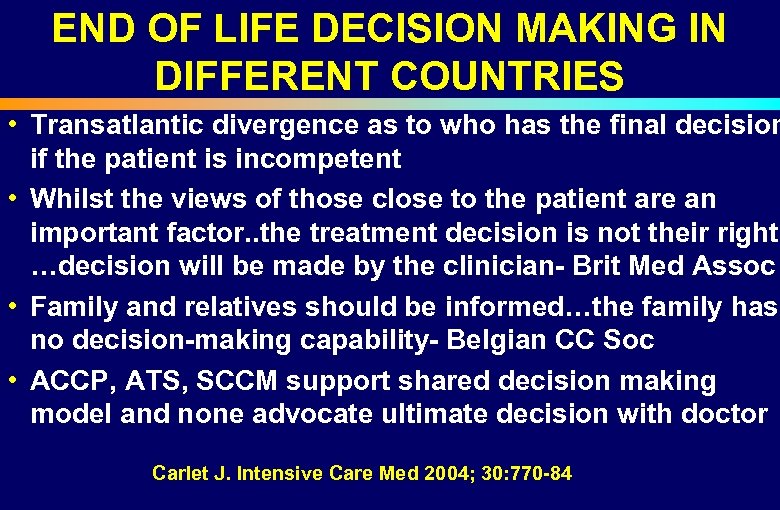 END OF LIFE DECISION MAKING IN DIFFERENT COUNTRIES • Transatlantic divergence as to who has the final decision if the patient is incompetent • Whilst the views of those close to the patient are an important factor. . the treatment decision is not their right …decision will be made by the clinician- Brit Med Assoc • Family and relatives should be informed…the family has no decision-making capability- Belgian CC Soc • ACCP, ATS, SCCM support shared decision making model and none advocate ultimate decision with doctor Carlet J. Intensive Care Med 2004; 30: 770 -84
END OF LIFE DECISION MAKING IN DIFFERENT COUNTRIES • Transatlantic divergence as to who has the final decision if the patient is incompetent • Whilst the views of those close to the patient are an important factor. . the treatment decision is not their right …decision will be made by the clinician- Brit Med Assoc • Family and relatives should be informed…the family has no decision-making capability- Belgian CC Soc • ACCP, ATS, SCCM support shared decision making model and none advocate ultimate decision with doctor Carlet J. Intensive Care Med 2004; 30: 770 -84
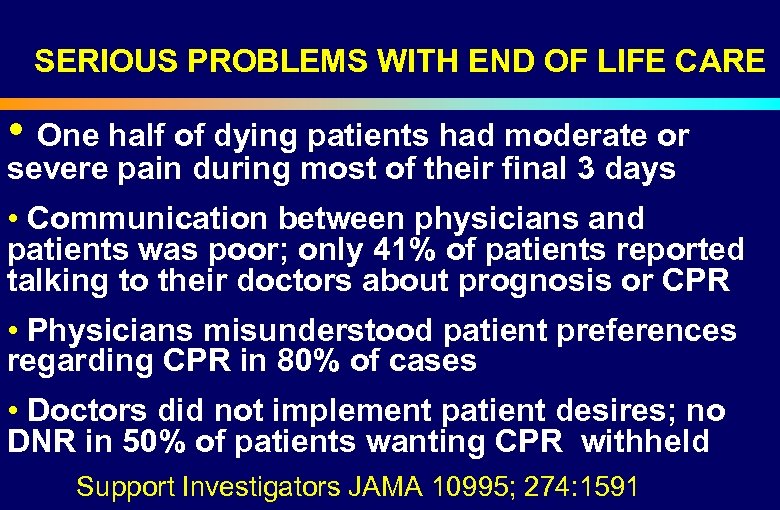 SERIOUS PROBLEMS WITH END OF LIFE CARE • One half of dying patients had moderate or severe pain during most of their final 3 days • Communication between physicians and patients was poor; only 41% of patients reported talking to their doctors about prognosis or CPR • Physicians misunderstood patient preferences regarding CPR in 80% of cases • Doctors did not implement patient desires; no DNR in 50% of patients wanting CPR withheld Support Investigators JAMA 10995; 274: 1591
SERIOUS PROBLEMS WITH END OF LIFE CARE • One half of dying patients had moderate or severe pain during most of their final 3 days • Communication between physicians and patients was poor; only 41% of patients reported talking to their doctors about prognosis or CPR • Physicians misunderstood patient preferences regarding CPR in 80% of cases • Doctors did not implement patient desires; no DNR in 50% of patients wanting CPR withheld Support Investigators JAMA 10995; 274: 1591
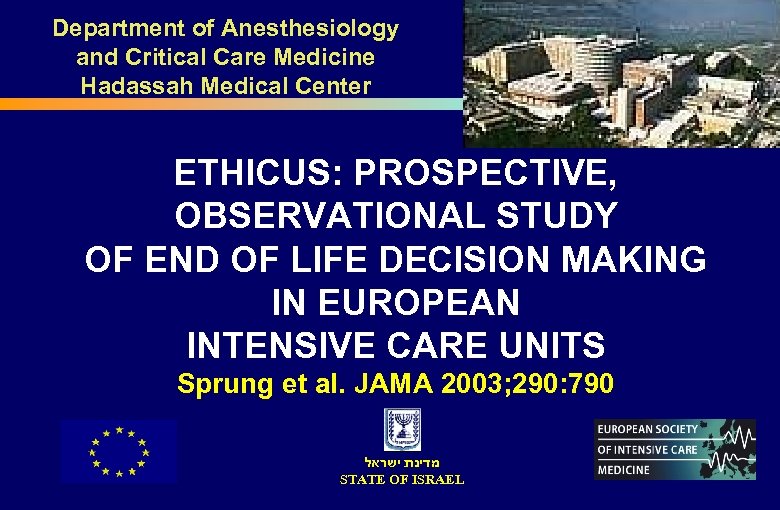 Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center ETHICUS: PROSPECTIVE, OBSERVATIONAL STUDY OF END OF LIFE DECISION MAKING IN EUROPEAN INTENSIVE CARE UNITS Sprung et al. JAMA 2003; 290: 790 מדינת ישראל STATE OF ISRAEL
Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center ETHICUS: PROSPECTIVE, OBSERVATIONAL STUDY OF END OF LIFE DECISION MAKING IN EUROPEAN INTENSIVE CARE UNITS Sprung et al. JAMA 2003; 290: 790 מדינת ישראל STATE OF ISRAEL
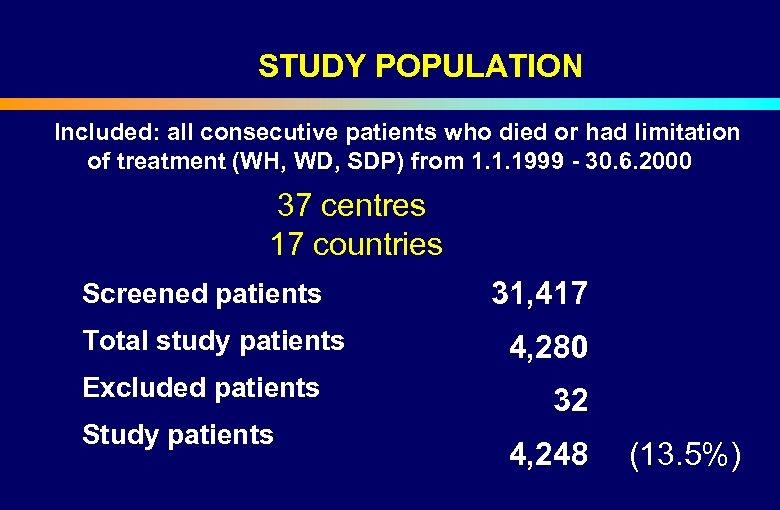 STUDY POPULATION Included: all consecutive patients who died or had limitation of treatment (WH, WD, SDP) from 1. 1. 1999 - 30. 6. 2000 37 centres 17 countries Screened patients Total study patients Excluded patients Study patients 31, 417 4, 280 32 4, 248 (13. 5%)
STUDY POPULATION Included: all consecutive patients who died or had limitation of treatment (WH, WD, SDP) from 1. 1. 1999 - 30. 6. 2000 37 centres 17 countries Screened patients Total study patients Excluded patients Study patients 31, 417 4, 280 32 4, 248 (13. 5%)
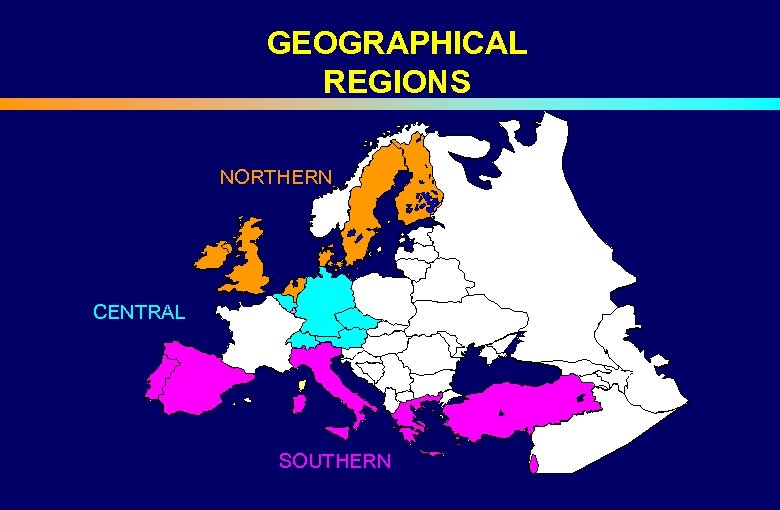 GEOGRAPHICAL REGIONS NORTHERN CENTRAL SOUTHERN
GEOGRAPHICAL REGIONS NORTHERN CENTRAL SOUTHERN
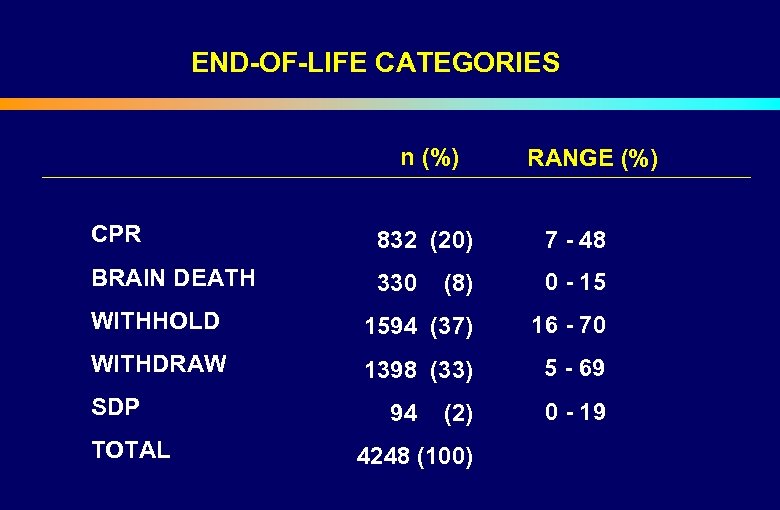 END-OF-LIFE CATEGORIES n (%) CPR RANGE (%) 832 (20) 7 - 48 BRAIN DEATH 330 (8) 0 - 15 WITHHOLD 1594 (37) 16 - 70 WITHDRAW 1398 (33) 5 - 69 SDP 94 (2) 0 - 19 TOTAL 4248 (100)
END-OF-LIFE CATEGORIES n (%) CPR RANGE (%) 832 (20) 7 - 48 BRAIN DEATH 330 (8) 0 - 15 WITHHOLD 1594 (37) 16 - 70 WITHDRAW 1398 (33) 5 - 69 SDP 94 (2) 0 - 19 TOTAL 4248 (100)
 END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
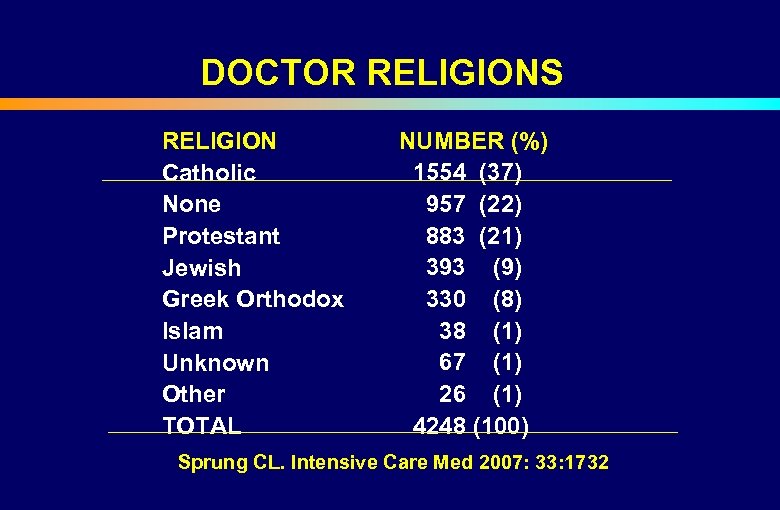 DOCTOR RELIGIONS RELIGION Catholic None Protestant Jewish Greek Orthodox Islam Unknown Other TOTAL NUMBER (%) 1554 (37) 957 (22) 883 (21) 393 (9) 330 (8) 38 (1) 67 (1) 26 (1) 4248 (100) Sprung CL. Intensive Care Med 2007: 33: 1732
DOCTOR RELIGIONS RELIGION Catholic None Protestant Jewish Greek Orthodox Islam Unknown Other TOTAL NUMBER (%) 1554 (37) 957 (22) 883 (21) 393 (9) 330 (8) 38 (1) 67 (1) 26 (1) 4248 (100) Sprung CL. Intensive Care Med 2007: 33: 1732
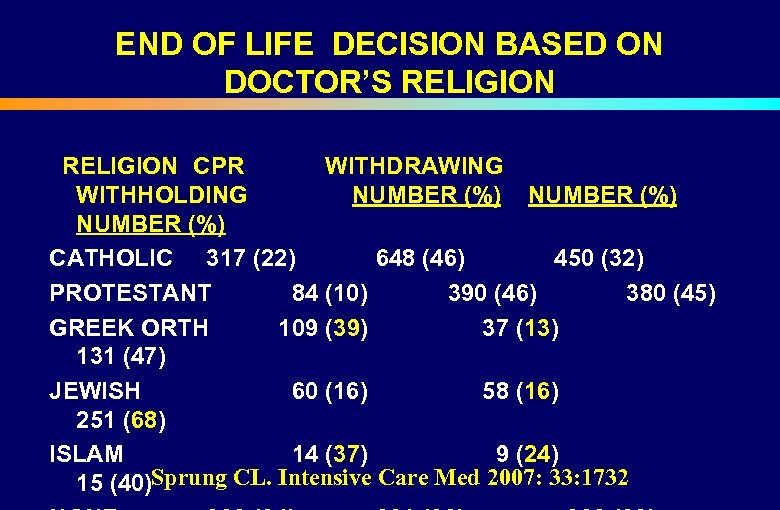 END OF LIFE DECISION BASED ON DOCTOR’S RELIGION CPR WITHDRAWING WITHHOLDING NUMBER (%) CATHOLIC 317 (22) 648 (46) 450 (32) PROTESTANT 84 (10) 390 (46) 380 (45) GREEK ORTH 109 (39) 37 (13) 131 (47) JEWISH 60 (16) 58 (16) 251 (68) ISLAM 14 (37) 9 (24) 15 (40)Sprung CL. Intensive Care Med 2007: 33: 1732
END OF LIFE DECISION BASED ON DOCTOR’S RELIGION CPR WITHDRAWING WITHHOLDING NUMBER (%) CATHOLIC 317 (22) 648 (46) 450 (32) PROTESTANT 84 (10) 390 (46) 380 (45) GREEK ORTH 109 (39) 37 (13) 131 (47) JEWISH 60 (16) 58 (16) 251 (68) ISLAM 14 (37) 9 (24) 15 (40)Sprung CL. Intensive Care Med 2007: 33: 1732
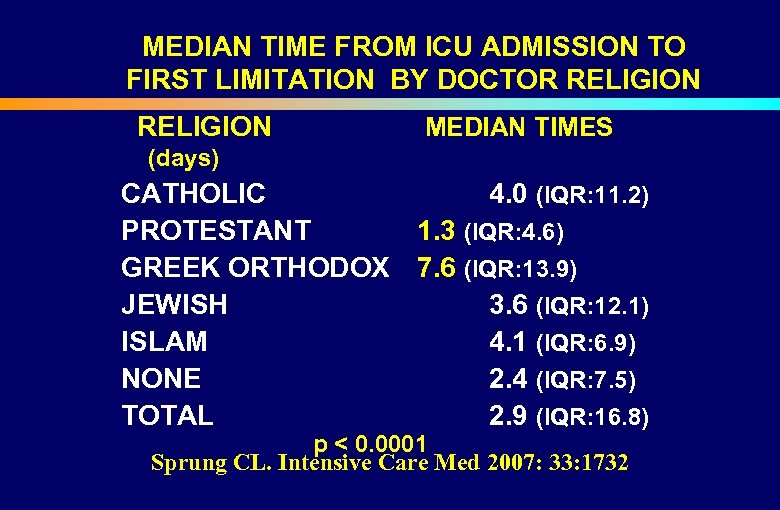 MEDIAN TIME FROM ICU ADMISSION TO FIRST LIMITATION BY DOCTOR RELIGION (days) CATHOLIC PROTESTANT GREEK ORTHODOX JEWISH ISLAM NONE TOTAL MEDIAN TIMES 4. 0 (IQR: 11. 2) 1. 3 (IQR: 4. 6) 7. 6 (IQR: 13. 9) 3. 6 (IQR: 12. 1) 4. 1 (IQR: 6. 9) 2. 4 (IQR: 7. 5) 2. 9 (IQR: 16. 8) p < 0. 0001 Sprung CL. Intensive Care Med 2007: 33: 1732
MEDIAN TIME FROM ICU ADMISSION TO FIRST LIMITATION BY DOCTOR RELIGION (days) CATHOLIC PROTESTANT GREEK ORTHODOX JEWISH ISLAM NONE TOTAL MEDIAN TIMES 4. 0 (IQR: 11. 2) 1. 3 (IQR: 4. 6) 7. 6 (IQR: 13. 9) 3. 6 (IQR: 12. 1) 4. 1 (IQR: 6. 9) 2. 4 (IQR: 7. 5) 2. 9 (IQR: 16. 8) p < 0. 0001 Sprung CL. Intensive Care Med 2007: 33: 1732
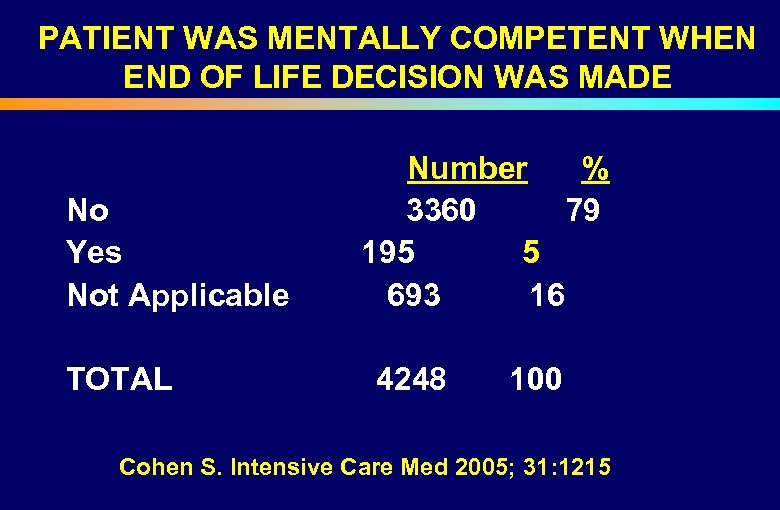 PATIENT WAS MENTALLY COMPETENT WHEN END OF LIFE DECISION WAS MADE Number % No 3360 79 Yes 195 5 Not Applicable 693 16 TOTAL 4248 100 Cohen S. Intensive Care Med 2005; 31: 1215
PATIENT WAS MENTALLY COMPETENT WHEN END OF LIFE DECISION WAS MADE Number % No 3360 79 Yes 195 5 Not Applicable 693 16 TOTAL 4248 100 Cohen S. Intensive Care Med 2005; 31: 1215
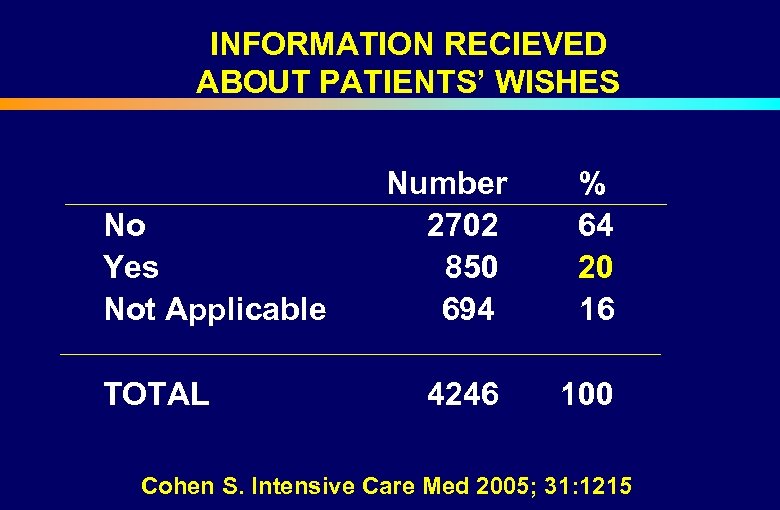 INFORMATION RECIEVED ABOUT PATIENTS’ WISHES Number % No 2702 64 Yes 850 20 Not Applicable 694 16 TOTAL 4246 100 Cohen S. Intensive Care Med 2005; 31: 1215
INFORMATION RECIEVED ABOUT PATIENTS’ WISHES Number % No 2702 64 Yes 850 20 Not Applicable 694 16 TOTAL 4246 100 Cohen S. Intensive Care Med 2005; 31: 1215
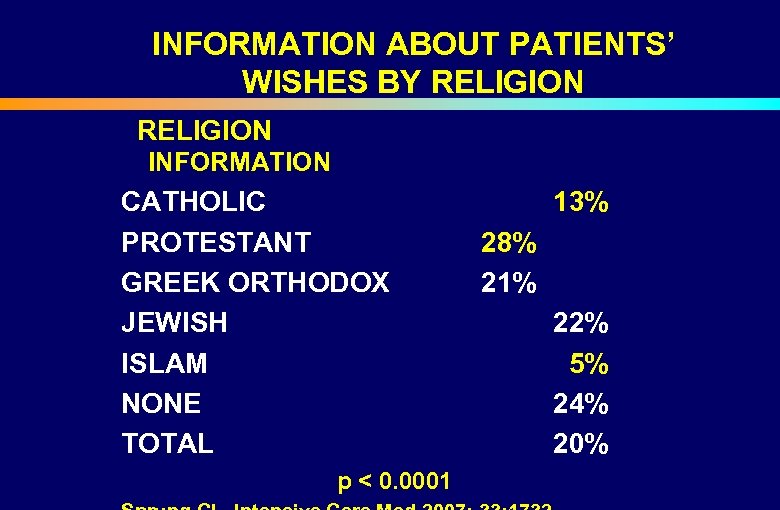 INFORMATION ABOUT PATIENTS’ WISHES BY RELIGION INFORMATION CATHOLIC PROTESTANT GREEK ORTHODOX JEWISH ISLAM NONE TOTAL 13% 28% 21% 22% 5% 24% 20% p < 0. 0001
INFORMATION ABOUT PATIENTS’ WISHES BY RELIGION INFORMATION CATHOLIC PROTESTANT GREEK ORTHODOX JEWISH ISLAM NONE TOTAL 13% 28% 21% 22% 5% 24% 20% p < 0. 0001
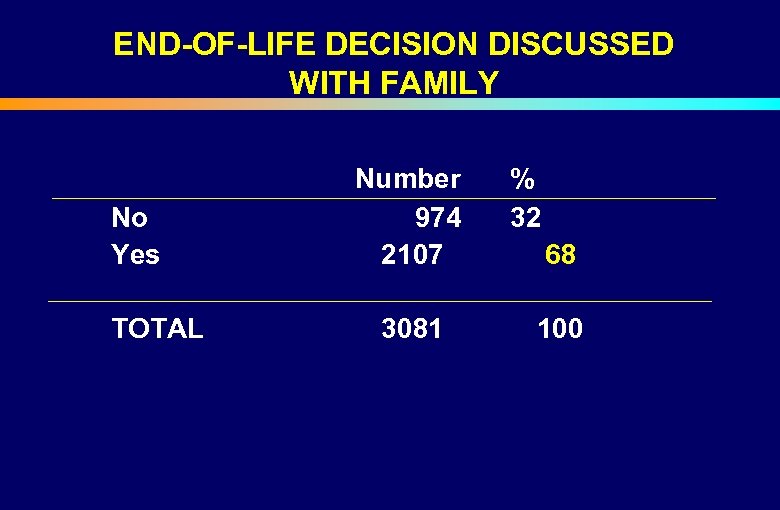 END-OF-LIFE DECISION DISCUSSED WITH FAMILY Number % No Yes 974 32 2107 68 TOTAL 3081 100
END-OF-LIFE DECISION DISCUSSED WITH FAMILY Number % No Yes 974 32 2107 68 TOTAL 3081 100
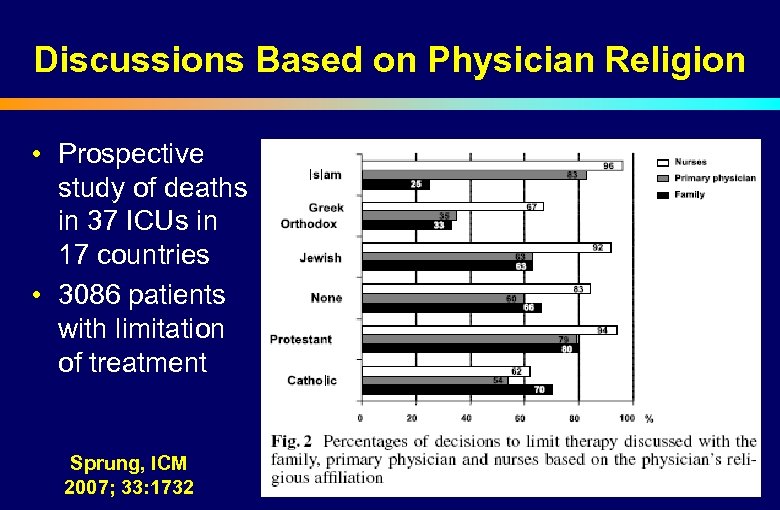 Discussions Based on Physician Religion • Prospective study of deaths in 37 ICUs in 17 countries • 3086 patients with limitation of treatment Sprung, ICM 2007; 33: 1732
Discussions Based on Physician Religion • Prospective study of deaths in 37 ICUs in 17 countries • 3086 patients with limitation of treatment Sprung, ICM 2007; 33: 1732
 END OF LIFE DECISION MAKING • Catholic physicians were less likely to withhold or withdraw therapies Vincent JL. Crit Care Med 1999; 27: 1626 SCCM Ethics Committee. Crit Care Med 1992; 20: 320 • Jewish physicians reported more likely to withhold or withdraw therapies SCCM Ethics Committee. Crit Care Med 1992; 20: 320 • Descriptive Israeli study demonstrated that Jewish physicians withheld and did not withdraw therapies Eidelman LA. Intensive Care Med 1998; 24: 162 -166
END OF LIFE DECISION MAKING • Catholic physicians were less likely to withhold or withdraw therapies Vincent JL. Crit Care Med 1999; 27: 1626 SCCM Ethics Committee. Crit Care Med 1992; 20: 320 • Jewish physicians reported more likely to withhold or withdraw therapies SCCM Ethics Committee. Crit Care Med 1992; 20: 320 • Descriptive Israeli study demonstrated that Jewish physicians withheld and did not withdraw therapies Eidelman LA. Intensive Care Med 1998; 24: 162 -166
 END OF LIFE DECISION MAKING • Ethnic beliefs may slowly be altered by exposure to different cultures • Process of acculturation- ethnic origin is tempered by the host society Levin PD. Crit Care Med 2003; 31: S 1 -S 4
END OF LIFE DECISION MAKING • Ethnic beliefs may slowly be altered by exposure to different cultures • Process of acculturation- ethnic origin is tempered by the host society Levin PD. Crit Care Med 2003; 31: S 1 -S 4
 END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
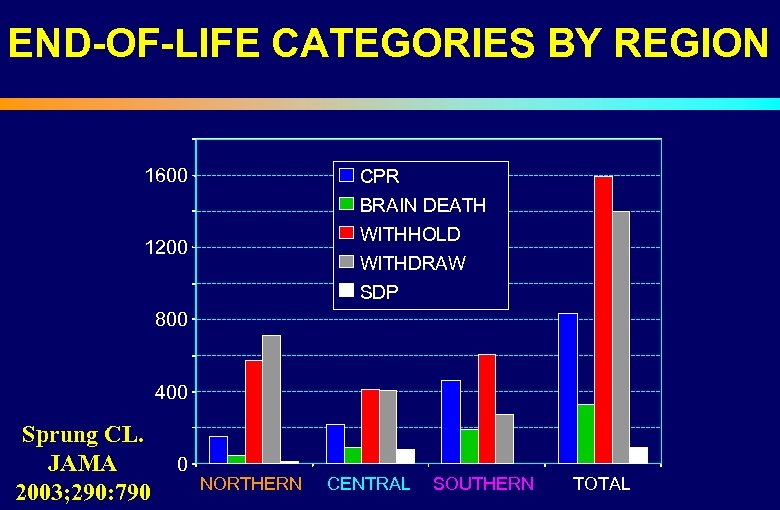 END-OF-LIFE CATEGORIES BY REGION 1600 CPR BRAIN DEATH WITHHOLD 1200 WITHDRAW SDP 800 400 Sprung CL. JAMA 2003; 290: 790 0 NORTHERN CENTRAL SOUTHERN TOTAL
END-OF-LIFE CATEGORIES BY REGION 1600 CPR BRAIN DEATH WITHHOLD 1200 WITHDRAW SDP 800 400 Sprung CL. JAMA 2003; 290: 790 0 NORTHERN CENTRAL SOUTHERN TOTAL
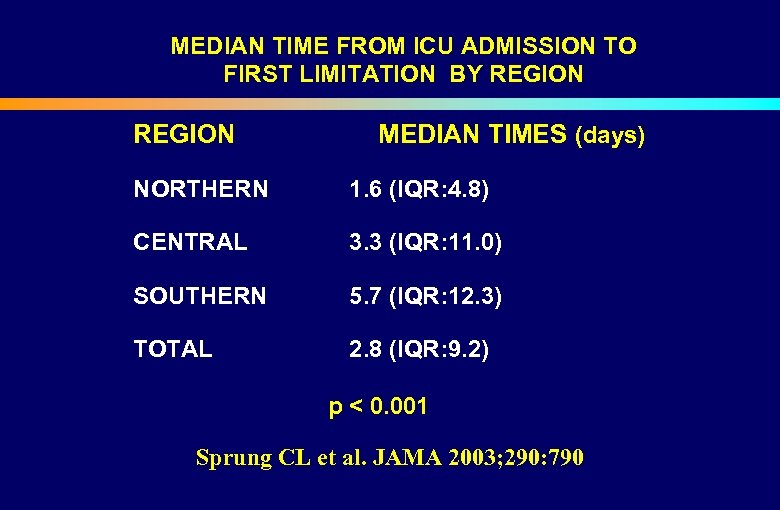 MEDIAN TIME FROM ICU ADMISSION TO FIRST LIMITATION BY REGION MEDIAN TIMES (days) NORTHERN 1. 6 (IQR: 4. 8) CENTRAL 3. 3 (IQR: 11. 0) SOUTHERN 5. 7 (IQR: 12. 3) TOTAL 2. 8 (IQR: 9. 2) p < 0. 001 Sprung CL et al. JAMA 2003; 290: 790
MEDIAN TIME FROM ICU ADMISSION TO FIRST LIMITATION BY REGION MEDIAN TIMES (days) NORTHERN 1. 6 (IQR: 4. 8) CENTRAL 3. 3 (IQR: 11. 0) SOUTHERN 5. 7 (IQR: 12. 3) TOTAL 2. 8 (IQR: 9. 2) p < 0. 001 Sprung CL et al. JAMA 2003; 290: 790
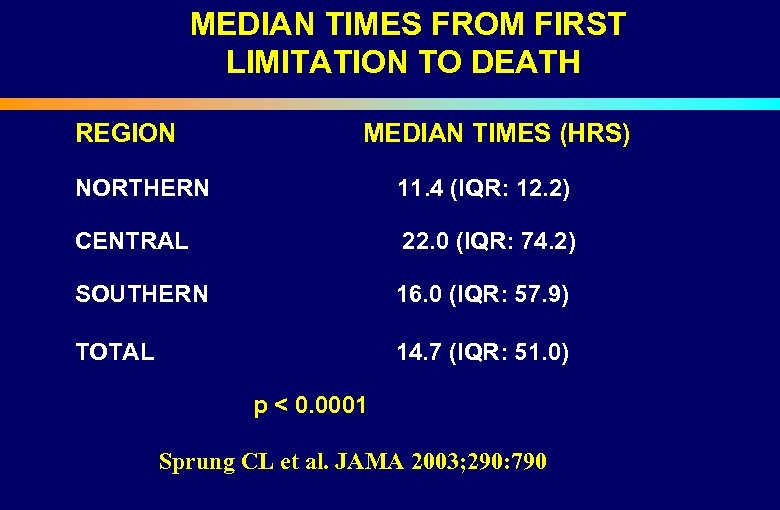 MEDIAN TIMES FROM FIRST LIMITATION TO DEATH REGION NORTHERN MEDIAN TIMES (HRS) 11. 4 (IQR: 12. 2) CENTRAL 22. 0 (IQR: 74. 2) SOUTHERN 16. 0 (IQR: 57. 9) TOTAL 14. 7 (IQR: 51. 0) p < 0. 0001 Sprung CL et al. JAMA 2003; 290: 790
MEDIAN TIMES FROM FIRST LIMITATION TO DEATH REGION NORTHERN MEDIAN TIMES (HRS) 11. 4 (IQR: 12. 2) CENTRAL 22. 0 (IQR: 74. 2) SOUTHERN 16. 0 (IQR: 57. 9) TOTAL 14. 7 (IQR: 51. 0) p < 0. 0001 Sprung CL et al. JAMA 2003; 290: 790
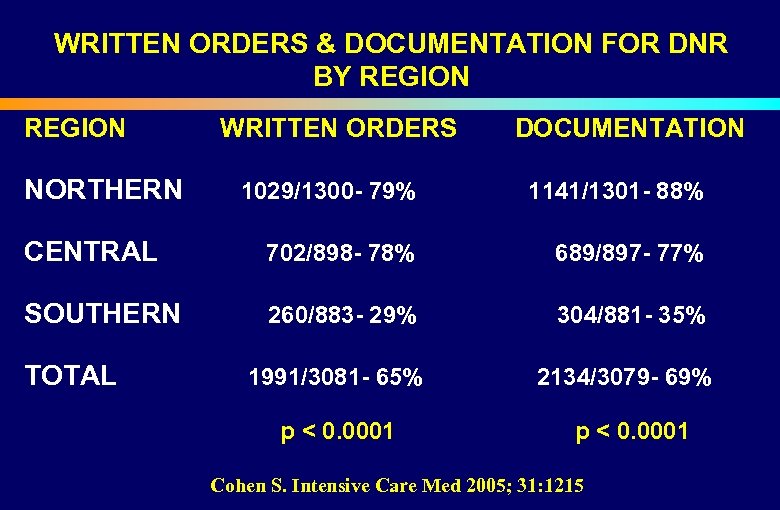 WRITTEN ORDERS & DOCUMENTATION FOR DNR BY REGION WRITTEN ORDERS DOCUMENTATION NORTHERN 1029/1300 - 79% 1141/1301 - 88% CENTRAL 702/898 - 78% 689/897 - 77% SOUTHERN 260/883 - 29% 304/881 - 35% TOTAL 1991/3081 - 65% 2134/3079 - 69% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215
WRITTEN ORDERS & DOCUMENTATION FOR DNR BY REGION WRITTEN ORDERS DOCUMENTATION NORTHERN 1029/1300 - 79% 1141/1301 - 88% CENTRAL 702/898 - 78% 689/897 - 77% SOUTHERN 260/883 - 29% 304/881 - 35% TOTAL 1991/3081 - 65% 2134/3079 - 69% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215
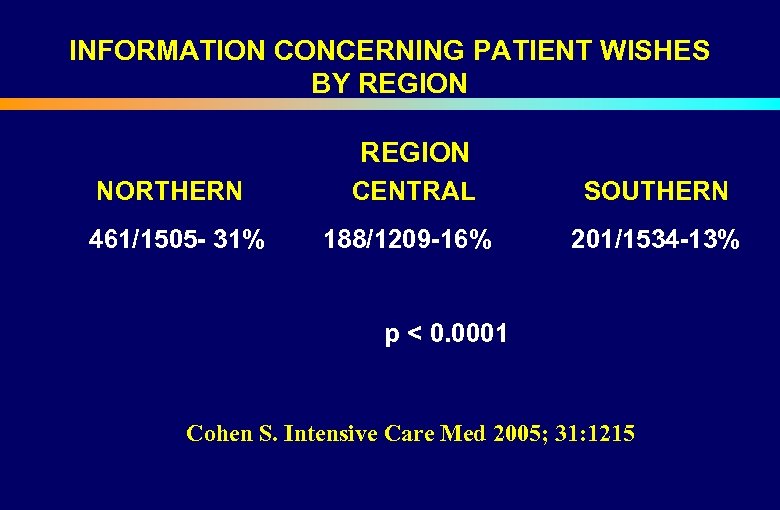 INFORMATION CONCERNING PATIENT WISHES BY REGION NORTHERN CENTRAL SOUTHERN 461/1505 - 31% 188/1209 -16% 201/1534 -13% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215
INFORMATION CONCERNING PATIENT WISHES BY REGION NORTHERN CENTRAL SOUTHERN 461/1505 - 31% 188/1209 -16% 201/1534 -13% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215
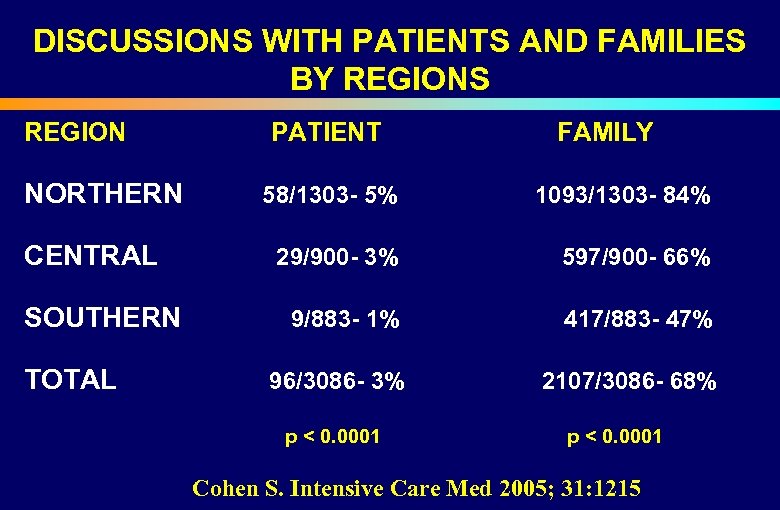 DISCUSSIONS WITH PATIENTS AND FAMILIES BY REGIONS REGION PATIENT NORTHERN 58/1303 - 5% FAMILY 1093/1303 - 84% CENTRAL 29/900 - 3% 597/900 - 66% SOUTHERN 9/883 - 1% 417/883 - 47% TOTAL 96/3086 - 3% p < 0. 0001 2107/3086 - 68% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215
DISCUSSIONS WITH PATIENTS AND FAMILIES BY REGIONS REGION PATIENT NORTHERN 58/1303 - 5% FAMILY 1093/1303 - 84% CENTRAL 29/900 - 3% 597/900 - 66% SOUTHERN 9/883 - 1% 417/883 - 47% TOTAL 96/3086 - 3% p < 0. 0001 2107/3086 - 68% p < 0. 0001 Cohen S. Intensive Care Med 2005; 31: 1215

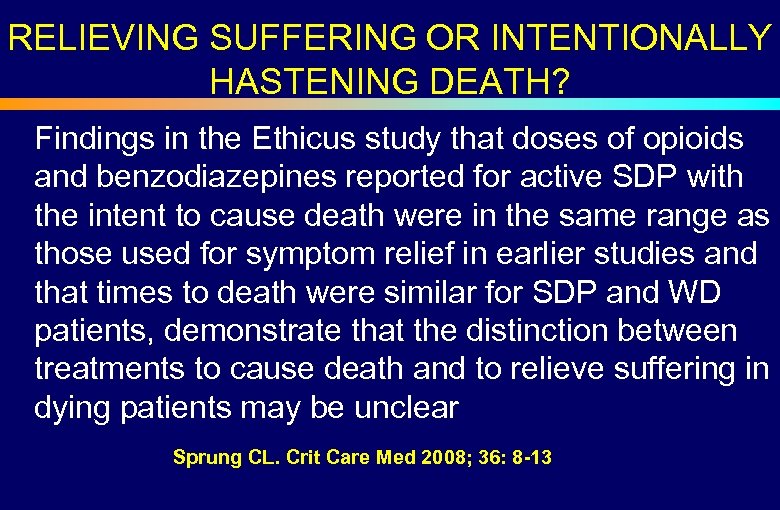 RELIEVING SUFFERING OR INTENTIONALLY HASTENING DEATH? Findings in the Ethicus study that doses of opioids and benzodiazepines reported for active SDP with the intent to cause death were in the same range as those used for symptom relief in earlier studies and that times to death were similar for SDP and WD patients, demonstrate that the distinction between treatments to cause death and to relieve suffering in dying patients may be unclear Sprung CL. Crit Care Med 2008; 36: 8 -13
RELIEVING SUFFERING OR INTENTIONALLY HASTENING DEATH? Findings in the Ethicus study that doses of opioids and benzodiazepines reported for active SDP with the intent to cause death were in the same range as those used for symptom relief in earlier studies and that times to death were similar for SDP and WD patients, demonstrate that the distinction between treatments to cause death and to relieve suffering in dying patients may be unclear Sprung CL. Crit Care Med 2008; 36: 8 -13
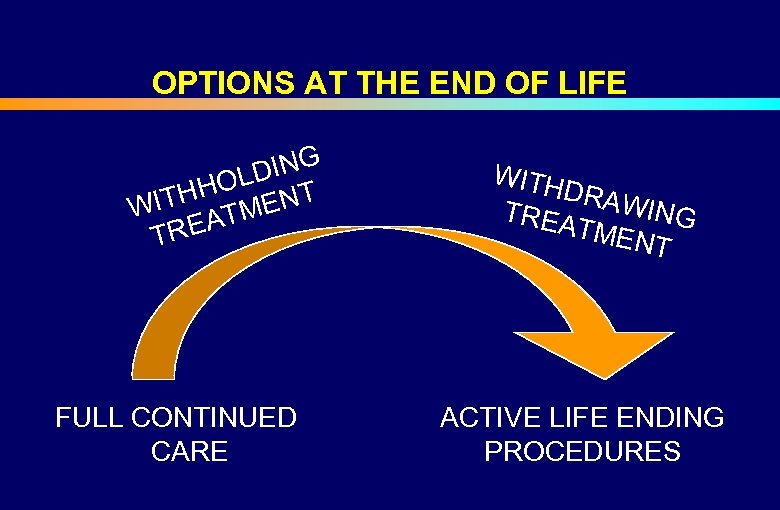 OPTIONS AT THE END OF LIFE DING HOL NT H WIT ATME TRE FULL CONTINUED CARE WITH DRAW ING TREA TMEN T ACTIVE LIFE ENDING PROCEDURES
OPTIONS AT THE END OF LIFE DING HOL NT H WIT ATME TRE FULL CONTINUED CARE WITH DRAW ING TREA TMEN T ACTIVE LIFE ENDING PROCEDURES
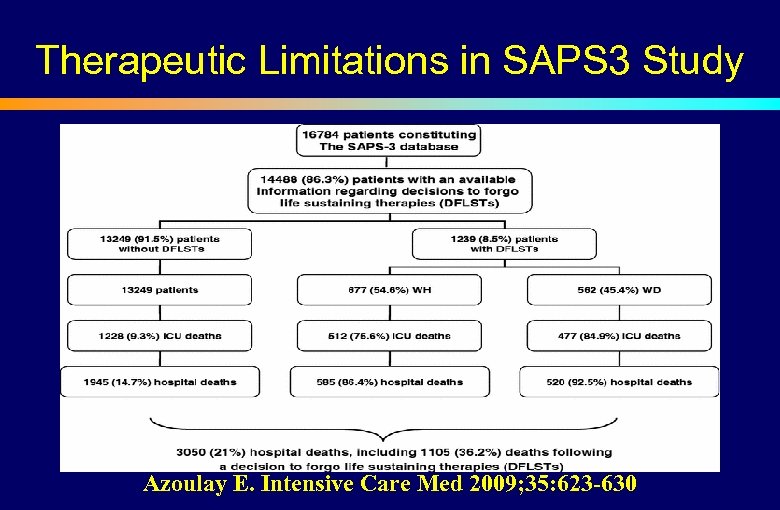 Therapeutic Limitations in SAPS 3 Study Azoulay E. Intensive Care Med 2009; 35: 623 -630
Therapeutic Limitations in SAPS 3 Study Azoulay E. Intensive Care Med 2009; 35: 623 -630
 Variations in Decisions to FLSTs • • Personal physician characteristics Case-mix and co-morbidities Experience Gender Specialty or time working in ICUs Religious beliefs and cultural background Organizational factors Presence of full time intensivist Azoulay E. Intensive Care Med 2009; 35: 623 -630
Variations in Decisions to FLSTs • • Personal physician characteristics Case-mix and co-morbidities Experience Gender Specialty or time working in ICUs Religious beliefs and cultural background Organizational factors Presence of full time intensivist Azoulay E. Intensive Care Med 2009; 35: 623 -630
 Therapeutic Limitations in SAPS 3 Study • FLST decisions more common in hospitals without emergency departments, in smaller ICUs & ICUs with lower nurse-to-patient ratios and more physicians per ICU bed. • DFLSTs were more common when intensivists were present only during weekdays, when multidisciplinary meetings were held, and when nurses and intensivists performed clinical rounds together. • DFLSTs were less common in ICUs that had at least one full time intensivist and in those with intensivists available at night and over weekends. Azoulay E. Intensive Care Med 2009; 35: 623 -630
Therapeutic Limitations in SAPS 3 Study • FLST decisions more common in hospitals without emergency departments, in smaller ICUs & ICUs with lower nurse-to-patient ratios and more physicians per ICU bed. • DFLSTs were more common when intensivists were present only during weekdays, when multidisciplinary meetings were held, and when nurses and intensivists performed clinical rounds together. • DFLSTs were less common in ICUs that had at least one full time intensivist and in those with intensivists available at night and over weekends. Azoulay E. Intensive Care Med 2009; 35: 623 -630
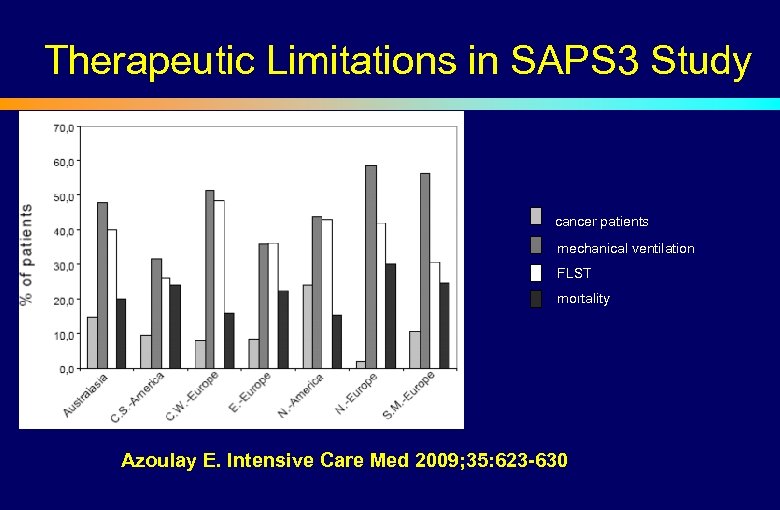 Therapeutic Limitations in SAPS 3 Study cancer patients mechanical ventilation FLST mortality Azoulay E. Intensive Care Med 2009; 35: 623 -630
Therapeutic Limitations in SAPS 3 Study cancer patients mechanical ventilation FLST mortality Azoulay E. Intensive Care Med 2009; 35: 623 -630
 END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
END OF LIFE DECISION MAKING • Differences between America, Europe and Israel • Religious and regional differences • Attitudes of patients, families, physicians and nurses • The Israeli Dying Patient Act, 2005
 Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center ETHICATT: SYSTEMATIC STUDY OF GENERAL ETHICAL PRINCIPLES INVOLVED IN END OF LIFE DECISIONS FOR PATIENTS IN EUROPEAN INTENSIVE CARE UNITS Sprung CL. Intensive Care Med 2007: 33: 104 מדינת ישראל STATE OF ISRAEL
Department of Anesthesiology and Critical Care Medicine Hadassah Medical Center ETHICATT: SYSTEMATIC STUDY OF GENERAL ETHICAL PRINCIPLES INVOLVED IN END OF LIFE DECISIONS FOR PATIENTS IN EUROPEAN INTENSIVE CARE UNITS Sprung CL. Intensive Care Med 2007: 33: 104 מדינת ישראל STATE OF ISRAEL
 ETHICATT STUDY • Empirical study of the attitudes of doctors, nurses, patients, and families involved in end of life decisions in different European countries • Performed in Czechia, Israel, the Netherlands, Portugal, Sweden and the UK • Criteria for inclusion: ICU doctors and nurses, patients previously hospitalized in the ICU within the last 12 months for more than 3 days and who could complete the questionnaire, and family members who were present most in the ICU during the patient’s hospitalization • Questionnaires completed 3 -6 months after patient was in ICU
ETHICATT STUDY • Empirical study of the attitudes of doctors, nurses, patients, and families involved in end of life decisions in different European countries • Performed in Czechia, Israel, the Netherlands, Portugal, Sweden and the UK • Criteria for inclusion: ICU doctors and nurses, patients previously hospitalized in the ICU within the last 12 months for more than 3 days and who could complete the questionnaire, and family members who were present most in the ICU during the patient’s hospitalization • Questionnaires completed 3 -6 months after patient was in ICU
 ETHICATT STUDY • Demographic data: country, age, sex, marital status, children, religiosity, income, years of practice and types of practice for doctors and nurses • 1899 questionnaires were completed by 528 doctors and 629 nurses who work in ICUs, 330 patients who survived ICU, 412 families of patients dying or surviving their ICU stay
ETHICATT STUDY • Demographic data: country, age, sex, marital status, children, religiosity, income, years of practice and types of practice for doctors and nurses • 1899 questionnaires were completed by 528 doctors and 629 nurses who work in ICUs, 330 patients who survived ICU, 412 families of patients dying or surviving their ICU stay
 END OF LIFE DECISIONS • Do patients and families want to be in ICUs, undergo CPR or mechanical ventilation? • Do patients or families want to have active euthanasia? • Do doctors want the same therapies for themselves as they want for their patients? Sprung CL. Intensive Care Med 2007: 33: 104
END OF LIFE DECISIONS • Do patients and families want to be in ICUs, undergo CPR or mechanical ventilation? • Do patients or families want to have active euthanasia? • Do doctors want the same therapies for themselves as they want for their patients? Sprung CL. Intensive Care Med 2007: 33: 104
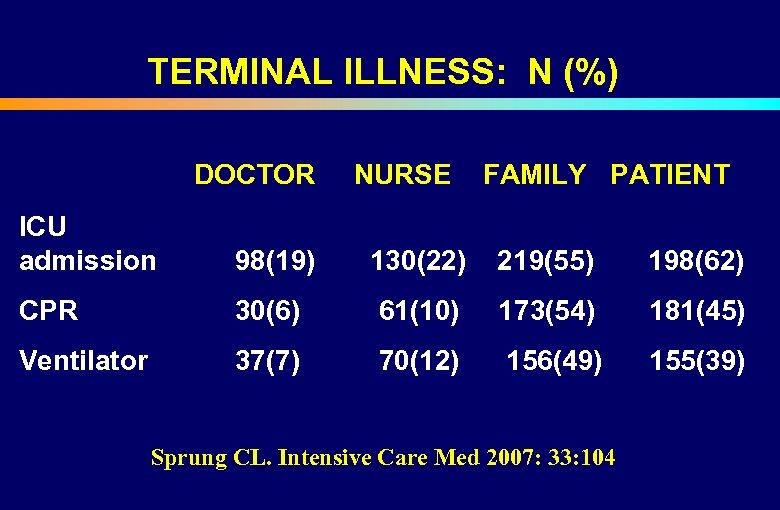 TERMINAL ILLNESS: N (%) DOCTOR NURSE FAMILY PATIENT ICU admission 98(19) 130(22) 219(55) 198(62) CPR 30(6) 61(10) 173(54) 181(45) Ventilator 37(7) 70(12) 156(49) 155(39) Sprung CL. Intensive Care Med 2007: 33: 104
TERMINAL ILLNESS: N (%) DOCTOR NURSE FAMILY PATIENT ICU admission 98(19) 130(22) 219(55) 198(62) CPR 30(6) 61(10) 173(54) 181(45) Ventilator 37(7) 70(12) 156(49) 155(39) Sprung CL. Intensive Care Med 2007: 33: 104
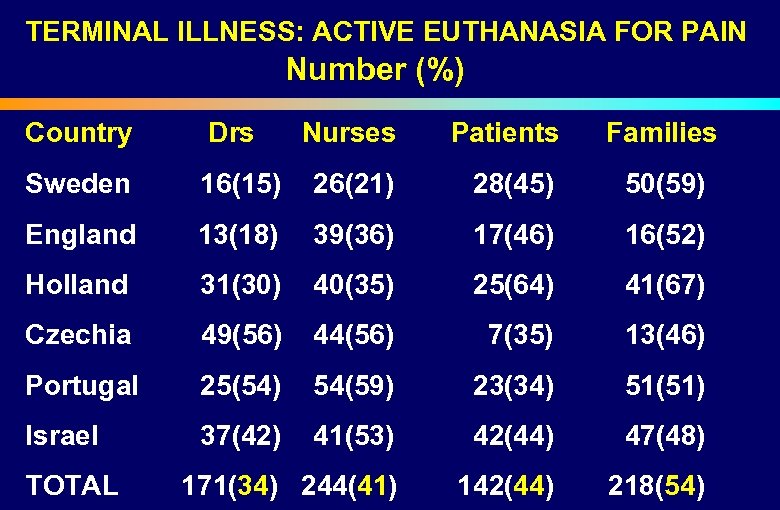 TERMINAL ILLNESS: ACTIVE EUTHANASIA FOR PAIN Number (%) Country Sweden Drs Nurses Patients Families 16(15) 26(21) 28(45) 50(59) England 13(18) 39(36) 17(46) 16(52) Holland 31(30) 40(35) 25(64) 41(67) Czechia 49(56) 44(56) 7(35) 13(46) Portugal 25(54) 54(59) 23(34) 51(51) Israel 37(42) 41(53) 42(44) 47(48) TOTAL 171(34) 244(41) 142(44) 218(54)
TERMINAL ILLNESS: ACTIVE EUTHANASIA FOR PAIN Number (%) Country Sweden Drs Nurses Patients Families 16(15) 26(21) 28(45) 50(59) England 13(18) 39(36) 17(46) 16(52) Holland 31(30) 40(35) 25(64) 41(67) Czechia 49(56) 44(56) 7(35) 13(46) Portugal 25(54) 54(59) 23(34) 51(51) Israel 37(42) 41(53) 42(44) 47(48) TOTAL 171(34) 244(41) 142(44) 218(54)

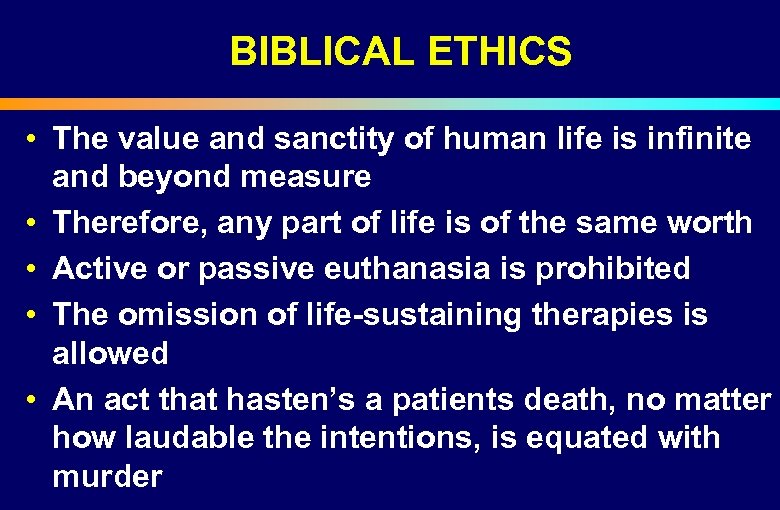 BIBLICAL ETHICS • The value and sanctity of human life is infinite and beyond measure • Therefore, any part of life is of the same worth • Active or passive euthanasia is prohibited • The omission of life-sustaining therapies is allowed • An act that hasten’s a patients death, no matter how laudable the intentions, is equated with murder
BIBLICAL ETHICS • The value and sanctity of human life is infinite and beyond measure • Therefore, any part of life is of the same worth • Active or passive euthanasia is prohibited • The omission of life-sustaining therapies is allowed • An act that hasten’s a patients death, no matter how laudable the intentions, is equated with murder
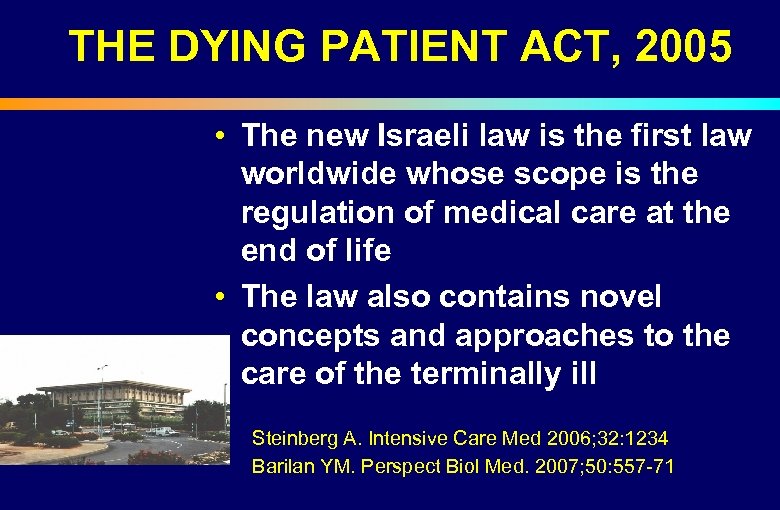 THE DYING PATIENT ACT, 2005 • The new Israeli law is the first law worldwide whose scope is the regulation of medical care at the end of life • The law also contains novel concepts and approaches to the care of the terminally ill Steinberg A. Intensive Care Med 2006; 32: 1234 Barilan YM. Perspect Biol Med. 2007; 50: 557 -71
THE DYING PATIENT ACT, 2005 • The new Israeli law is the first law worldwide whose scope is the regulation of medical care at the end of life • The law also contains novel concepts and approaches to the care of the terminally ill Steinberg A. Intensive Care Med 2006; 32: 1234 Barilan YM. Perspect Biol Med. 2007; 50: 557 -71
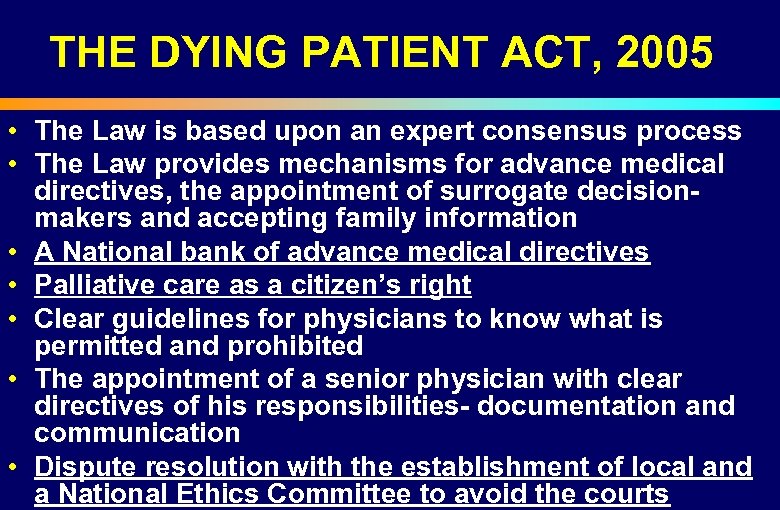 THE DYING PATIENT ACT, 2005 • The Law is based upon an expert consensus process • The Law provides mechanisms for advance medical directives, the appointment of surrogate decisionmakers and accepting family information • A National bank of advance medical directives • Palliative care as a citizen’s right • Clear guidelines for physicians to know what is permitted and prohibited • The appointment of a senior physician with clear directives of his responsibilities- documentation and communication • Dispute resolution with the establishment of local and a National Ethics Committee to avoid the courts
THE DYING PATIENT ACT, 2005 • The Law is based upon an expert consensus process • The Law provides mechanisms for advance medical directives, the appointment of surrogate decisionmakers and accepting family information • A National bank of advance medical directives • Palliative care as a citizen’s right • Clear guidelines for physicians to know what is permitted and prohibited • The appointment of a senior physician with clear directives of his responsibilities- documentation and communication • Dispute resolution with the establishment of local and a National Ethics Committee to avoid the courts
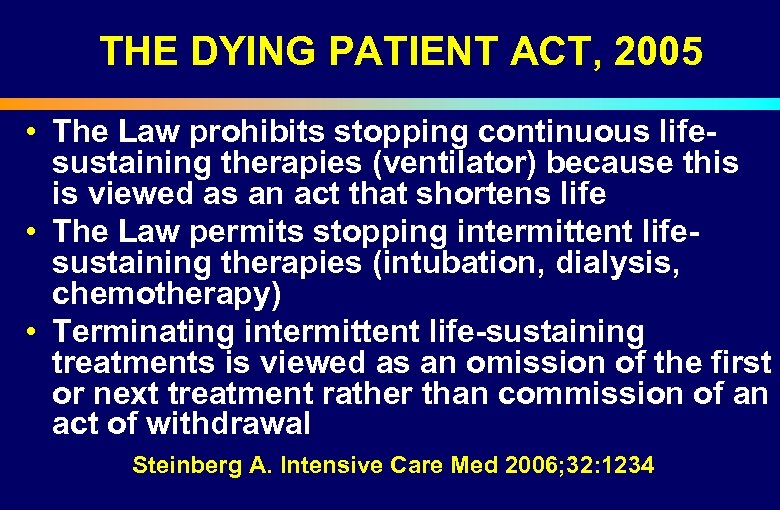 THE DYING PATIENT ACT, 2005 • The Law prohibits stopping continuous lifesustaining therapies (ventilator) because this is viewed as an act that shortens life • The Law permits stopping intermittent lifesustaining therapies (intubation, dialysis, chemotherapy) • Terminating intermittent life-sustaining treatments is viewed as an omission of the first or next treatment rather than commission of an act of withdrawal Steinberg A. Intensive Care Med 2006; 32: 1234
THE DYING PATIENT ACT, 2005 • The Law prohibits stopping continuous lifesustaining therapies (ventilator) because this is viewed as an act that shortens life • The Law permits stopping intermittent lifesustaining therapies (intubation, dialysis, chemotherapy) • Terminating intermittent life-sustaining treatments is viewed as an omission of the first or next treatment rather than commission of an act of withdrawal Steinberg A. Intensive Care Med 2006; 32: 1234
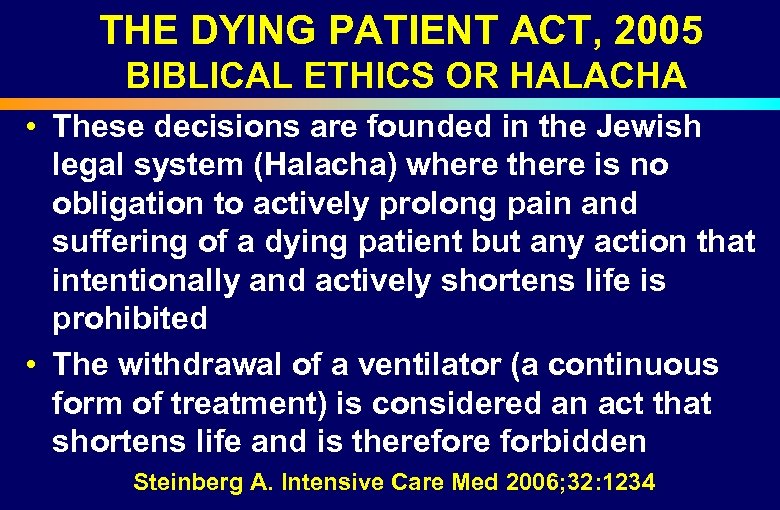 THE DYING PATIENT ACT, 2005 BIBLICAL ETHICS OR HALACHA • These decisions are founded in the Jewish legal system (Halacha) where there is no obligation to actively prolong pain and suffering of a dying patient but any action that intentionally and actively shortens life is prohibited • The withdrawal of a ventilator (a continuous form of treatment) is considered an act that shortens life and is therefore forbidden Steinberg A. Intensive Care Med 2006; 32: 1234
THE DYING PATIENT ACT, 2005 BIBLICAL ETHICS OR HALACHA • These decisions are founded in the Jewish legal system (Halacha) where there is no obligation to actively prolong pain and suffering of a dying patient but any action that intentionally and actively shortens life is prohibited • The withdrawal of a ventilator (a continuous form of treatment) is considered an act that shortens life and is therefore forbidden Steinberg A. Intensive Care Med 2006; 32: 1234
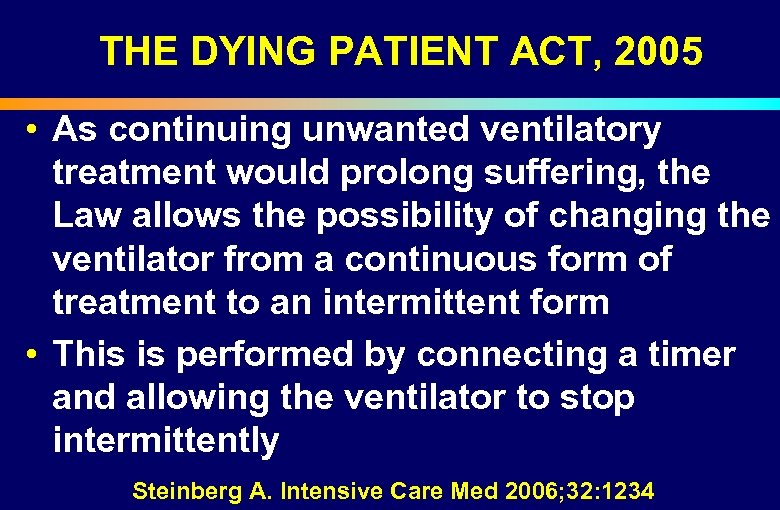 THE DYING PATIENT ACT, 2005 • As continuing unwanted ventilatory treatment would prolong suffering, the Law allows the possibility of changing the ventilator from a continuous form of treatment to an intermittent form • This is performed by connecting a timer and allowing the ventilator to stop intermittently Steinberg A. Intensive Care Med 2006; 32: 1234
THE DYING PATIENT ACT, 2005 • As continuing unwanted ventilatory treatment would prolong suffering, the Law allows the possibility of changing the ventilator from a continuous form of treatment to an intermittent form • This is performed by connecting a timer and allowing the ventilator to stop intermittently Steinberg A. Intensive Care Med 2006; 32: 1234
 THE DYING PATIENT ACT, 2005 TIMER ATTRIBUTES The “timer”, as a pragmatic solution would enable doctors to honor the wishes of patients and families without termination of continuous treatment of a dying patient which may cause his death ! Ravitsky V. BMJ 2005; 330: 415 -417
THE DYING PATIENT ACT, 2005 TIMER ATTRIBUTES The “timer”, as a pragmatic solution would enable doctors to honor the wishes of patients and families without termination of continuous treatment of a dying patient which may cause his death ! Ravitsky V. BMJ 2005; 330: 415 -417
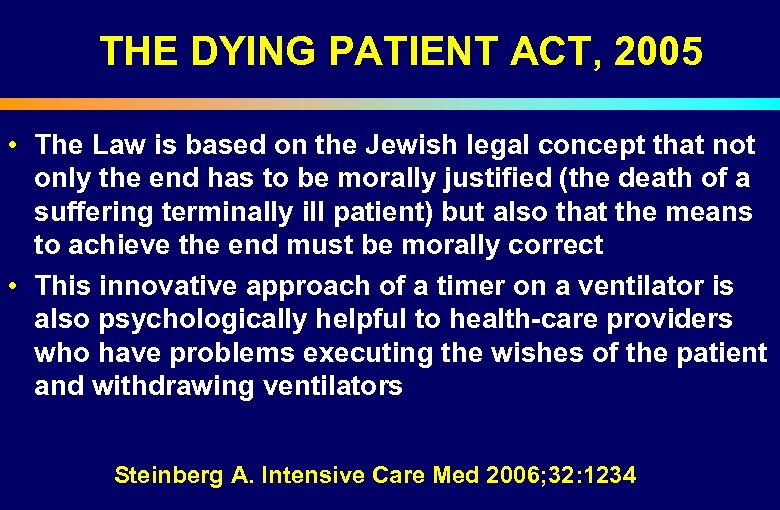 THE DYING PATIENT ACT, 2005 • The Law is based on the Jewish legal concept that not only the end has to be morally justified (the death of a suffering terminally ill patient) but also that the means to achieve the end must be morally correct • This innovative approach of a timer on a ventilator is also psychologically helpful to health-care providers who have problems executing the wishes of the patient and withdrawing ventilators Steinberg A. Intensive Care Med 2006; 32: 1234
THE DYING PATIENT ACT, 2005 • The Law is based on the Jewish legal concept that not only the end has to be morally justified (the death of a suffering terminally ill patient) but also that the means to achieve the end must be morally correct • This innovative approach of a timer on a ventilator is also psychologically helpful to health-care providers who have problems executing the wishes of the patient and withdrawing ventilators Steinberg A. Intensive Care Med 2006; 32: 1234

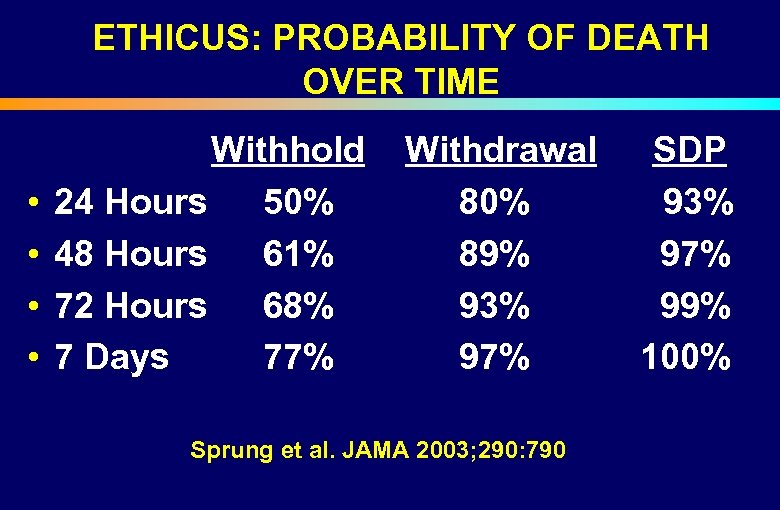 ETHICUS: PROBABILITY OF DEATH OVER TIME Withhold Withdrawal SDP 24 Hours 50% 80% 93% 48 Hours 61% 89% 97% 72 Hours 68% 93% 99% 7 Days 77% 97% 100% • • Sprung et al. JAMA 2003; 290: 790
ETHICUS: PROBABILITY OF DEATH OVER TIME Withhold Withdrawal SDP 24 Hours 50% 80% 93% 48 Hours 61% 89% 97% 72 Hours 68% 93% 99% 7 Days 77% 97% 100% • • Sprung et al. JAMA 2003; 290: 790
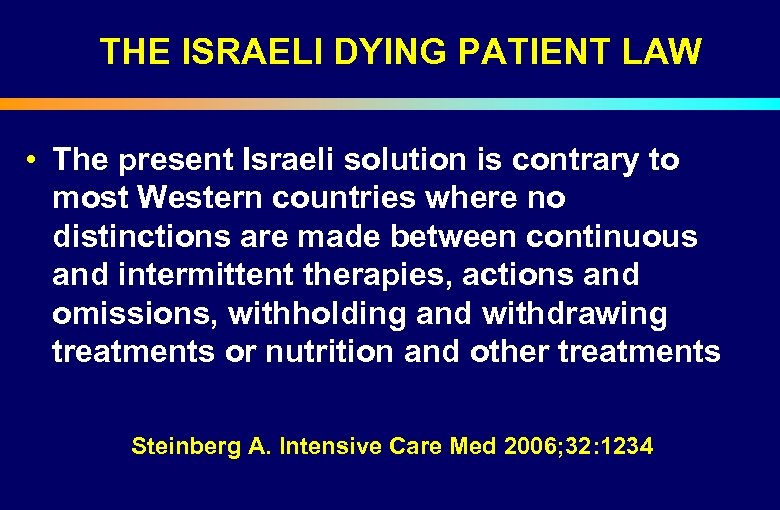 THE ISRAELI DYING PATIENT LAW • The present Israeli solution is contrary to most Western countries where no distinctions are made between continuous and intermittent therapies, actions and omissions, withholding and withdrawing treatments or nutrition and other treatments Steinberg A. Intensive Care Med 2006; 32: 1234
THE ISRAELI DYING PATIENT LAW • The present Israeli solution is contrary to most Western countries where no distinctions are made between continuous and intermittent therapies, actions and omissions, withholding and withdrawing treatments or nutrition and other treatments Steinberg A. Intensive Care Med 2006; 32: 1234

 CONCLUSIONS- 1 • End of life decisions commonly occur in North American and European ICUs • Limitations and variations appear similar in North American and European ICUs • Communication, decision making and documentation are very different in North America and Europe • End of life practices are different for physicians of different religions
CONCLUSIONS- 1 • End of life decisions commonly occur in North American and European ICUs • Limitations and variations appear similar in North American and European ICUs • Communication, decision making and documentation are very different in North America and Europe • End of life practices are different for physicians of different religions
 CONCLUSIONS- 2 • More withdrawal for Catholic, Protestant or physicians with no religions • More CPR for Greek Orthodox and Muslim doctors • Less discussions for Greek Orthodox and Muslim doctors • Differences in religions in various studies may relate to acculturation • Regional differences are likely due to diverse
CONCLUSIONS- 2 • More withdrawal for Catholic, Protestant or physicians with no religions • More CPR for Greek Orthodox and Muslim doctors • Less discussions for Greek Orthodox and Muslim doctors • Differences in religions in various studies may relate to acculturation • Regional differences are likely due to diverse
 CONCLUSIONS- 3 • Distinction between treatments to cause death and to relieve suffering in dying patients may be unclear • Patients and families desire more aggressive therapies than doctors and nurses • Patients and families desire active euthanasia for pain as do doctors and nurses
CONCLUSIONS- 3 • Distinction between treatments to cause death and to relieve suffering in dying patients may be unclear • Patients and families desire more aggressive therapies than doctors and nurses • Patients and families desire active euthanasia for pain as do doctors and nurses
 CONCLUSIONS- 4 a • The Israeli Dying Patient Act contains novel concepts and approaches to the care of the terminally ill which were developed by consensus and conform to Halacha • Timers to change ventilators from a continuous to an intermittent treatment • Palliative care as a citizen’s right • A National Bank of advance medical
CONCLUSIONS- 4 a • The Israeli Dying Patient Act contains novel concepts and approaches to the care of the terminally ill which were developed by consensus and conform to Halacha • Timers to change ventilators from a continuous to an intermittent treatment • Palliative care as a citizen’s right • A National Bank of advance medical
 WELPICUS • Welpicus- Consensus Guidelines for Worldwide End of Life Practice for Patients in Intensive Care Units • Worldwide ICU societies have participated in bringing together experts from at least 27 countries to develop Worldwide consensus for end of life practices
WELPICUS • Welpicus- Consensus Guidelines for Worldwide End of Life Practice for Patients in Intensive Care Units • Worldwide ICU societies have participated in bringing together experts from at least 27 countries to develop Worldwide consensus for end of life practices
 WHERE WAS YOUR ICU CARE?
WHERE WAS YOUR ICU CARE?


