4683977b2c63e2043ac5b8a60398700b.ppt
- Количество слайдов: 42

DELIRIUM
OBJECTIVES Know and understand: • What is delirium? • How to recognize and diagnose delirium • The predisposing or precipitating risk factors for delirium in elderly patients • How to evaluate and treat elderly patients with delirium • Interventions to prevent delirium Slide 2
TOPICS COVERED • Incidence and Morbidity • Recognition and Diagnosis • Neuropathophysiology • Predisposing and Precipitating Factors • Evaluation, Management, and Prevention Slide 3
DELIRIUM IS ALSO KNOWN AS…. Acute confusional state Acute mental status change Altered mental status Organic brain syndrome Reversible dementia Toxic or metabolic encephalopathy Slide 4
INCIDENCE OF DELIRIUM AMONG OLDER PATIENTS IS HIGH • 1/3 of older patients presenting to the ED • 1/3 of inpatients aged 70+ on general medical units, half of whom are delirious on admission Slide 5
MORBIDITY ASSOCIATED WITH DELIRIUM • 10 -fold risk of death in hospital • 3 - to 5 -fold risk of nosocomial complications, prolonged stay, postacute nursing-home placement • Poor functional recovery and risk of death up to 2 years following discharge • Persistence of delirium poor long-term outcomes Slide 6
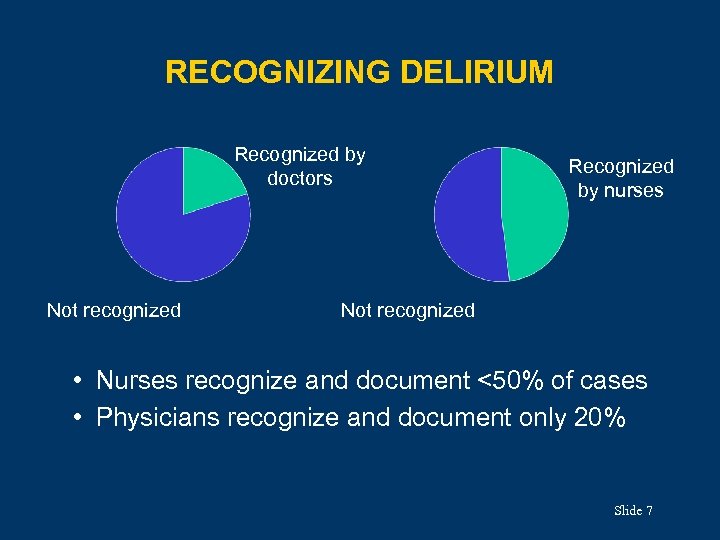
RECOGNIZING DELIRIUM Recognized by doctors Not recognized Recognized by nurses Not recognized • Nurses recognize and document <50% of cases • Physicians recognize and document only 20% Slide 7
DIAGNOSING DELIRIUM • DSM-IV criteria precise but difficult to apply • Confusion Assessment Method (CAM) Ø Clinically more useful Ø >95% sensitivity and specificity Slide 8
DSM-IV DIAGNOSTIC CRITERIA • Disturbance of consciousness with reduced ability to focus, sustain, or shift attention • Change in cognition (eg, memory deficit, disorientation, language disturbance) or a perceptual disturbance not better accounted for by existing dementia • Development over a short time (hours to days) and fluctuation during the day • Evidence from history, physical, or labs that the disturbance is a direct physiologic consequence of a medical condition or a drug Slide 9
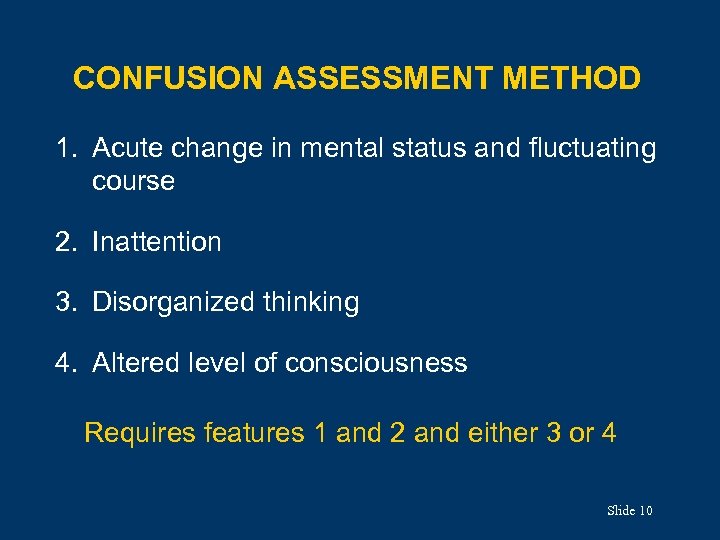
CONFUSION ASSESSMENT METHOD 1. Acute change in mental status and fluctuating course 2. Inattention 3. Disorganized thinking 4. Altered level of consciousness Requires features 1 and 2 and either 3 or 4 Slide 10
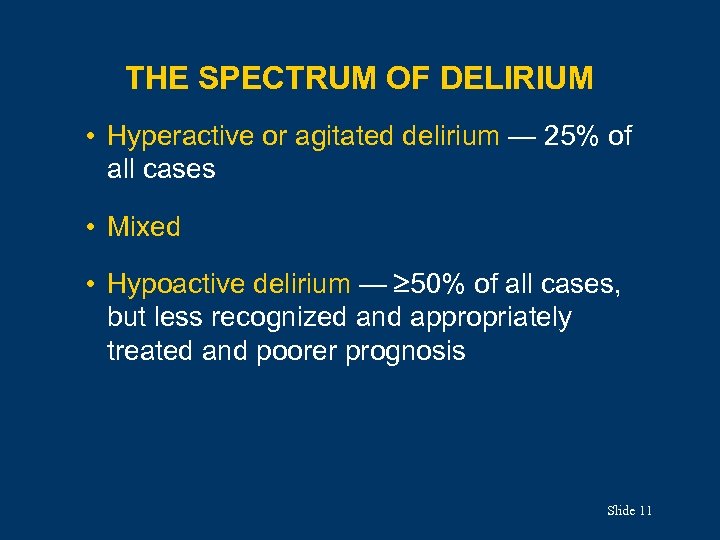
THE SPECTRUM OF DELIRIUM • Hyperactive or agitated delirium — 25% of all cases • Mixed • Hypoactive delirium — 50% of all cases, but less recognized and appropriately treated and poorer prognosis Slide 11
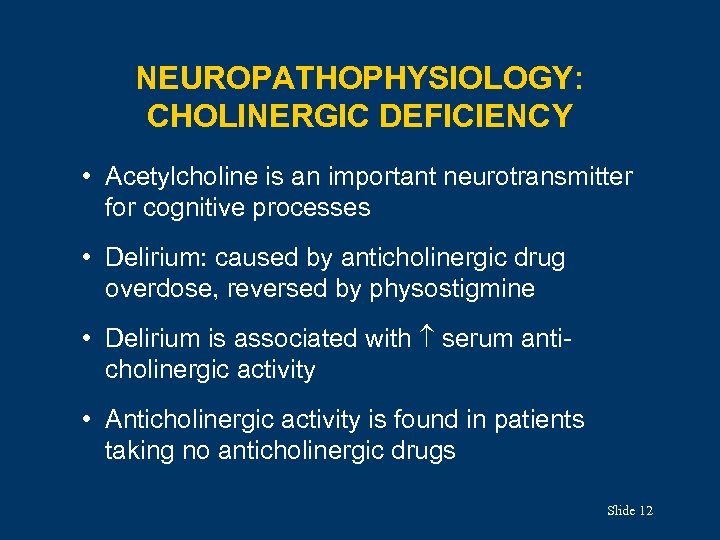
NEUROPATHOPHYSIOLOGY: CHOLINERGIC DEFICIENCY • Acetylcholine is an important neurotransmitter for cognitive processes • Delirium: caused by anticholinergic drug overdose, reversed by physostigmine • Delirium is associated with serum anticholinergic activity • Anticholinergic activity is found in patients taking no anticholinergic drugs Slide 12
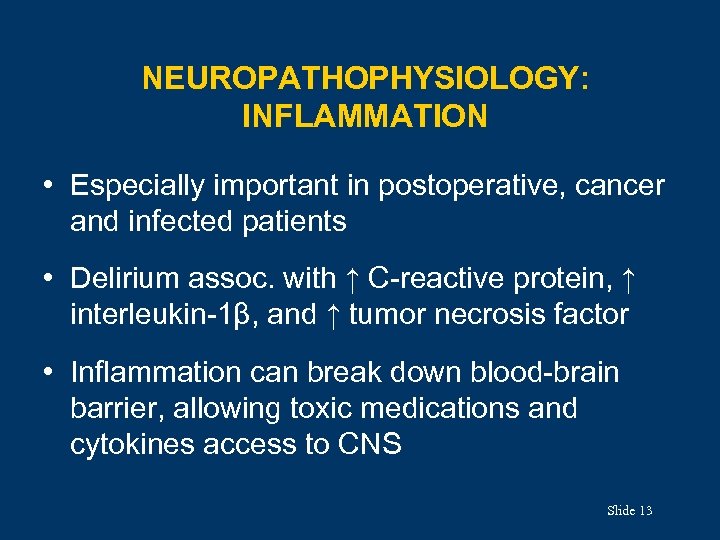
NEUROPATHOPHYSIOLOGY: INFLAMMATION • Especially important in postoperative, cancer and infected patients • Delirium assoc. with ↑ C-reactive protein, ↑ interleukin-1β, and ↑ tumor necrosis factor • Inflammation can break down blood-brain barrier, allowing toxic medications and cytokines access to CNS Slide 13
EPIDEMIOLOGICAL APPROACH • Delirium “caused” by “sum” of predisposing and precipitating factors • The more predisposing factors present, the fewer precipitating factors required to cause delirium Slide 14
PREDISPOSING FACTORS • Advanced age • Dementia • Functional impairment in ADLs • Medical comorbidity • History of alcohol abuse • Male sex • Sensory impairment ( vision, hearing) Slide 15
PRECIPITATING FACTORS • Acute cardiac events • Acute pulmonary events • Bed rest • Drug withdrawal (sedatives, alcohol) • Fecal impaction • Fluid or electrolyte disturbances • Indwelling devices • Infections (esp. respiratory, urinary) • Medications • Restraints • Severe anemia • Uncontrolled pain • Urinary retention Slide 16
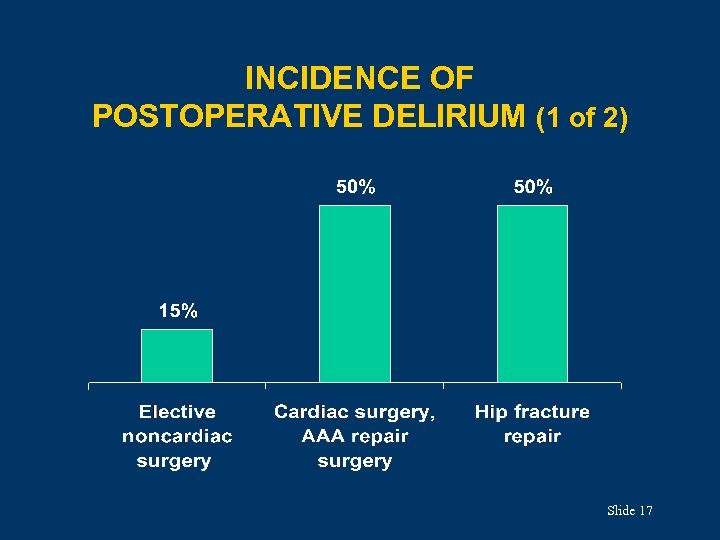
INCIDENCE OF POSTOPERATIVE DELIRIUM (1 of 2) Slide 17
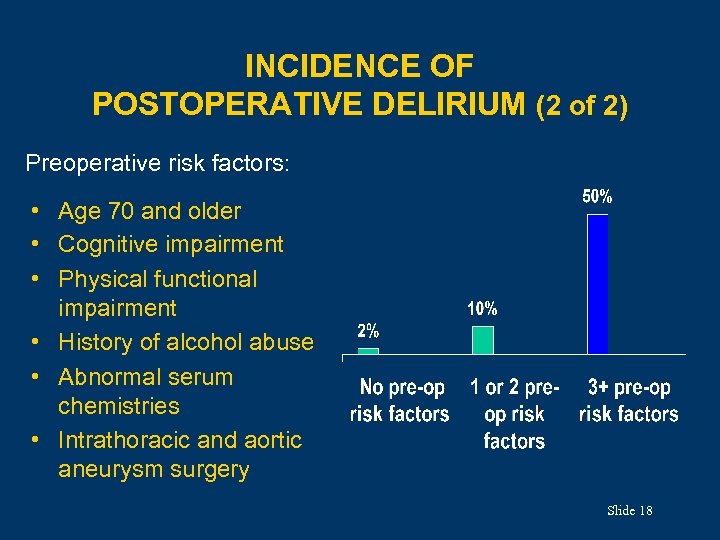
INCIDENCE OF POSTOPERATIVE DELIRIUM (2 of 2) Preoperative risk factors: • Age 70 and older • Cognitive impairment • Physical functional impairment • History of alcohol abuse • Abnormal serum chemistries • Intrathoracic and aortic aneurysm surgery Slide 18
KEYS TO PREVENTING POSTOPERATIVE DELIRIUM • Peak onset is on 2 nd postoperative day • Associated with postoperative pain, postoperative anemia, use of benzodiazepines and opioids (esp. meperidine) • Recommended: Ø Limit sedation Ø Provide adequate analgesia Slide 19
EVALUATION: HISTORY & PHYSICAL History • Focus on time course of cognitive changes, esp. their association with other symptoms or events • Medication review, including OTC drugs, alcohol Physical examination • • Vital signs Oxygen saturation General medical evaluation Neurologic and mental status examination Slide 20
EVALUATION: LABORATORY TESTING • Base on history and physical • Include CBC, electrolytes, renal function tests • Also helpful: UA , LFTs, serum drug levels, arterial blood gases, chest x-ray, ECG, cultures • Cerebral imaging rarely helpful, except with head trauma or new focal neurologic findings • EEG and CSF rarely helpful, except with associated seizure activity or signs of meningitis Slide 21
MANAGEMENT: GENERAL PRINCIPLES • Requires interdisciplinary effort by MDs, nurses, family, others • Multifactorial approach is most successful because multiple factors contribute to delirium • Failure to diagnose and manage delirium costly, life-threatening complications; loss of function Slide 22
KEYS TO EFFECTIVE MANAGEMENT • Identify and treat reversible contributors Ø Optimize medications (see next slide) Ø Treat infections, pain, fluid balance disorders, sensory deprivation • Maintain behavioral control Ø Behavioral and pharmacologic interventions • Anticipate and prevent complications Ø Urinary incontinence, immobility, falls, pressure ulcers, sleep disturbance, feeding disorders • Restore function Ø Hospital environment, cognitive reconditioning, ADL status, family education, discharge planning Slide 23
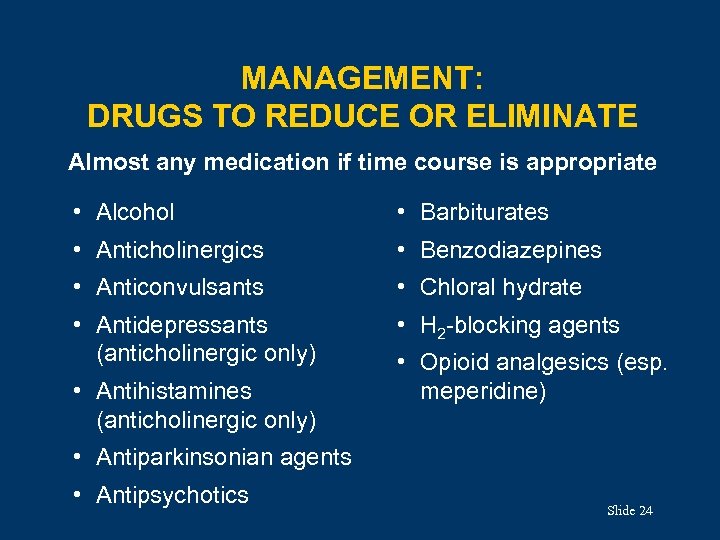
MANAGEMENT: DRUGS TO REDUCE OR ELIMINATE Almost any medication if time course is appropriate • Alcohol • Barbiturates • Anticholinergics • Benzodiazepines • Anticonvulsants • Chloral hydrate • Antidepressants (anticholinergic only) • H 2 -blocking agents • Antihistamines (anticholinergic only) • Opioid analgesics (esp. meperidine) • Antiparkinsonian agents • Antipsychotics Slide 24
MANAGEMENT: BEHAVIORAL PROBLEMS (1 of 2) • Provide “social” restraints: consider a sitter or allow family to stay in room • Avoid physical or pharmacologic restraints • If absolutely necessary, use haloperidol (see next slide) Ø Newer atypical antipsychotics are equally effective Ø Use lorazepam in sedative and alcohol withdrawal, and history of neuroleptic malignant syndrome Slide 25
MANAGEMENT: BEHAVIORAL PROBLEMS (2 of 2) Haloperidol use: • Mild delirium: 0. 25– 0. 5 mg po or 0. 125– 0. 25 mg IV/IM • Severe delirium: 0. 5– 2 mg IV/IM • Additional dosing q 60 min, as required • Assess for akathisia and extrapyramidal effects • Avoid in older people with parkinsonism • Monitor for QT interval prolongation, torsade de pointes, neuroleptic malignant syndrome, withdrawal dyskinesias Slide 26
MANAGEMENT: REHABILITATION • Use orienting stimuli (clocks, calendar, radio) • Provide adequate socialization • Use eyeglasses and hearing aids appropriately • Mobilize patient as soon as possible • Ensure adequate intake of nutrition and fluids, by hand feeding if necessary • Educate and support the patient and family Slide 27
THE BEST MANAGEMENT IS PREVENTION • HELP program included interventions for cognitive impairment, sleep deprivation, immobility, sensory impairment, dehydration • Focus on nonpharmacologic approaches (eg, sleep protocol involving warm milk, back rubs, soothing music) • Limit or avoid psychoactive and other high-risk medications Slide 28
SUMMARY (1 of 2) • Delirium is common and associated with substantial morbidity for older people • Delirium can be diagnosed with high sensitivity and specificity using the CAM • A thorough history, physical, and focused labs will lead to the underlying cause(s) of delirium Slide 29
SUMMARY (2 of 2) • A careful medication review is mandatory; discontinue any likely to contribute to delirium, if possible • Managing delirium involves treating the primary disease, avoiding complications, managing behavioral problems, providing rehabilitation • The best treatment for delirium is prevention Slide 30
CASE 1 (1 of 4) • A 72 -year-old man is evaluated because nurses are concerned about his agitation, which increases markedly in the evenings. • He underwent emergency hip replacement 3 days ago after he fell and fractured his hip. • He requires antipsychotic agents to control his agitation at night: he yells “help me” constantly and is determined to get out of bed alone and walk. • In the year before his fall, he had stopped working and driving; the reasons are unclear. Slide 31
CASE 1 (2 of 4) • The patient’s history includes hypertension, benign prostatic hyperplasia, and osteoarthritis. There is no history of dementia. • On examination, he appears confused and is disoriented to place and time. • He has some pain with hip movements. • Neurologic findings are nonfocal. Slide 32
CASE 1 (3 of 4) Which of the following is most helpful in establishing the diagnosis of delirium? A. Order electrolytes, BUN, glucose, and thyrotropin. B. Determine why the patient stopped working and driving. C. Perform the digit-span memory test. D. Order CT of the brain. E. Review the patient’s medication list. Slide 33
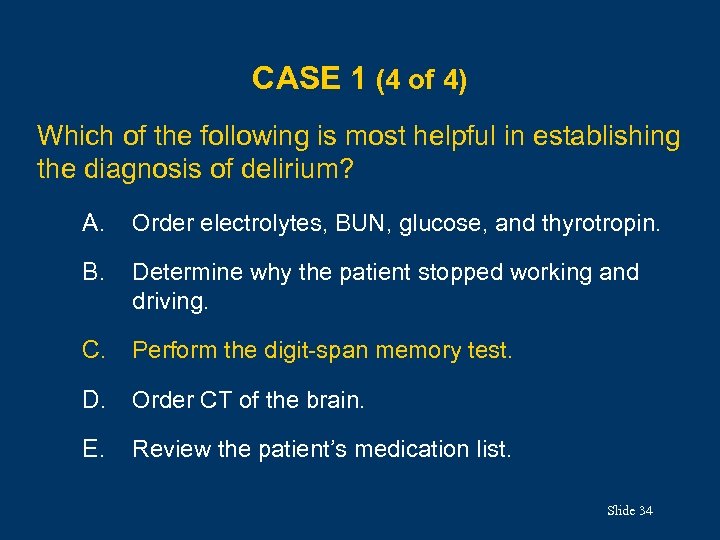
CASE 1 (4 of 4) Which of the following is most helpful in establishing the diagnosis of delirium? A. Order electrolytes, BUN, glucose, and thyrotropin. B. Determine why the patient stopped working and driving. C. Perform the digit-span memory test. D. Order CT of the brain. E. Review the patient’s medication list. Slide 34
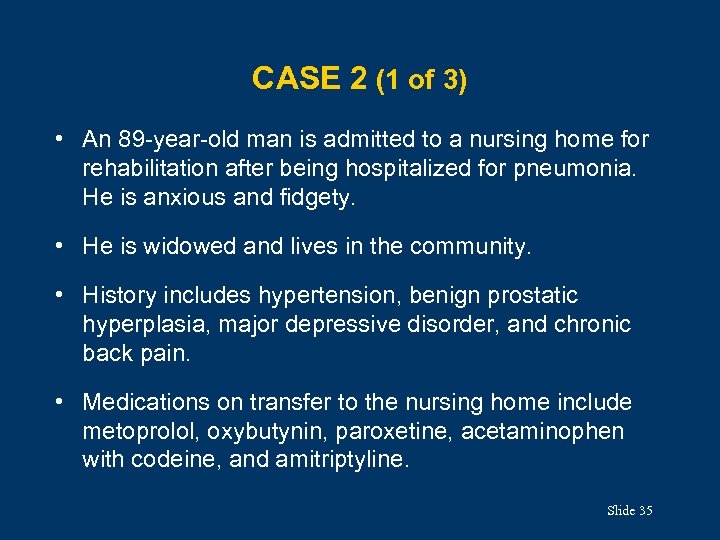
CASE 2 (1 of 3) • An 89 -year-old man is admitted to a nursing home for rehabilitation after being hospitalized for pneumonia. He is anxious and fidgety. • He is widowed and lives in the community. • History includes hypertension, benign prostatic hyperplasia, major depressive disorder, and chronic back pain. • Medications on transfer to the nursing home include metoprolol, oxybutynin, paroxetine, acetaminophen with codeine, and amitriptyline. Slide 35
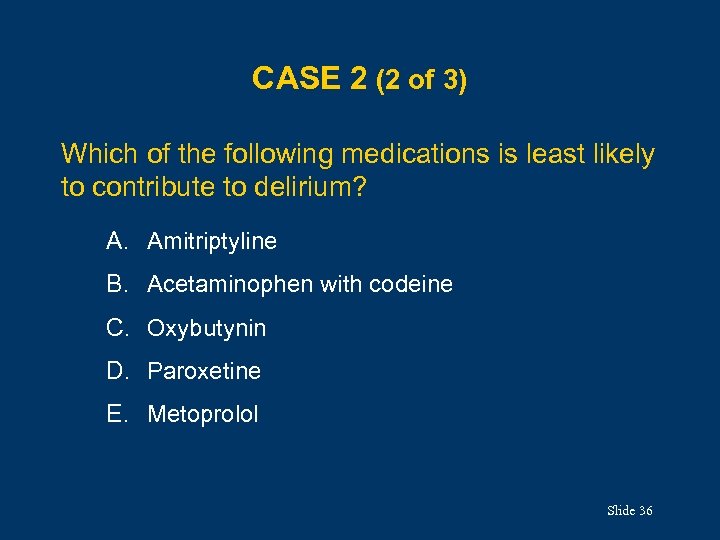
CASE 2 (2 of 3) Which of the following medications is least likely to contribute to delirium? A. Amitriptyline B. Acetaminophen with codeine C. Oxybutynin D. Paroxetine E. Metoprolol Slide 36
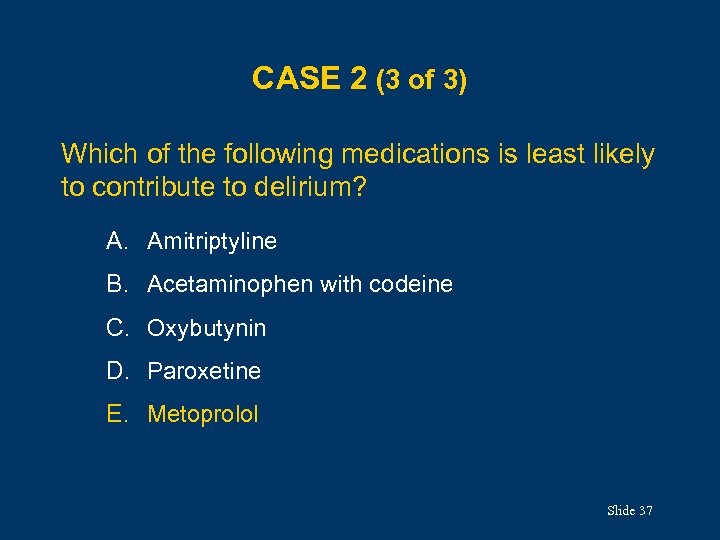
CASE 2 (3 of 3) Which of the following medications is least likely to contribute to delirium? A. Amitriptyline B. Acetaminophen with codeine C. Oxybutynin D. Paroxetine E. Metoprolol Slide 37
CASE 3 (1 of 4) • A 90 -year-old man is brought to the emergency department by his family because he has had an abrupt change in behavior. • The patient moved into his daughter and son-in-law’s house a few months ago, because he was no longer able to manage living alone. • A few days ago, he became aggressive and angry, and he hit his son-in-law for no apparent reason. • He has also become incontinent in the last few days. Slide 38
CASE 3 (2 of 4) • He has multiple bruises, which the family suspects are from falling. • The patient’s history includes moderate dementia and benign prostatic hyperplasia. • Blood pressure is 160/90 mm. Hg; all other vital signs are normal. The physical exam is unremarkable. • He is demanding to be released from “prison” and is aggressive with the staff. • He is uncooperative with the neurologic exam, but he appears to be moving all extremities well. Slide 39
CASE 3 (3 of 4) Which of the following is the most appropriate next step? A. Bladder scan B. Lumbar puncture C. Electroencephalography D. CT of the brain E. Basic metabolic panel, CBC, and pulse oximetry Slide 40
CASE 3 (4 of 4) Which of the following is the most appropriate next step? A. Bladder scan B. Lumbar puncture C. Electroencephalography D. CT of the brain E. Basic metabolic panel, CBC, and pulse oximetry Slide 41
ACKNOWLEDGMENTS Editor: Annette Medina-Walpole, MD GRS 7 Chapter Author: Edward R. Marcantonio, MD, SM GRS 7 Question Writer: Lynn Mc. Nicoll, MD Pharmacotherapy Editor: Judith L. Beizer, Pharm. D Medical Writers: Beverly A. Caley Faith Reidenbach Managing Editor: Andrea N. Sherman, MS Copyright © 2010 American Geriatrics Society Slide 42
4683977b2c63e2043ac5b8a60398700b.ppt