04a23f26dee87bd987cc4a258c052d15.ppt
- Количество слайдов: 46
 Delirium in the ICU Alex Yartsev, 22/06/11
Delirium in the ICU Alex Yartsev, 22/06/11
 Symptoms associated with delirium • • Disorientation Hyper-arousal, agitation Apathy and withdrawal Incooperation / incomplete cooperation Aggression Hallucinations(visual > auditory), delusions Altered sleep-wake cycle Gleason OC (March 2003). "Delirium". Am Fam Physician 67 (5): 1027– 34
Symptoms associated with delirium • • Disorientation Hyper-arousal, agitation Apathy and withdrawal Incooperation / incomplete cooperation Aggression Hallucinations(visual > auditory), delusions Altered sleep-wake cycle Gleason OC (March 2003). "Delirium". Am Fam Physician 67 (5): 1027– 34
 Definition of delirium: • Chief features agreed upon • Classification varies depending on source Gleason OC (March 2003). "Delirium". Am Fam Physician 67 (5): 1027– 34
Definition of delirium: • Chief features agreed upon • Classification varies depending on source Gleason OC (March 2003). "Delirium". Am Fam Physician 67 (5): 1027– 34
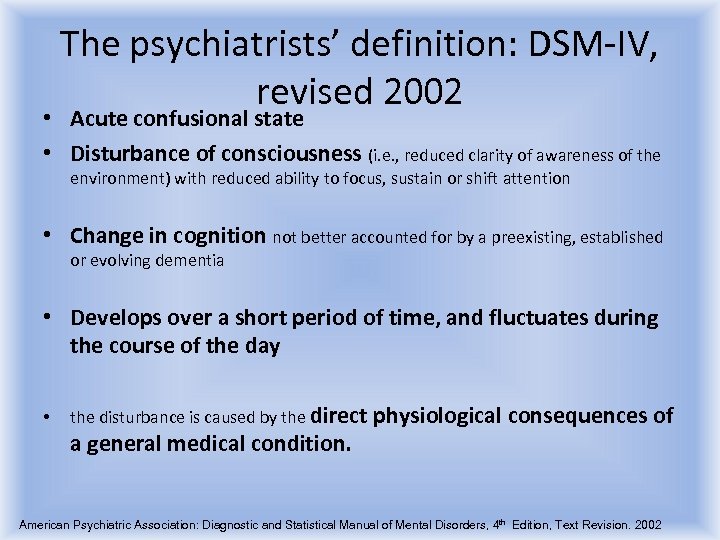 The psychiatrists’ definition: DSM-IV, revised 2002 • Acute confusional state • Disturbance of consciousness (i. e. , reduced clarity of awareness of the environment) with reduced ability to focus, sustain or shift attention • Change in cognition not better accounted for by a preexisting, established or evolving dementia • Develops over a short period of time, and fluctuates during the course of the day • the disturbance is caused by the direct physiological consequences of a general medical condition. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4 th Edition, Text Revision. 2002
The psychiatrists’ definition: DSM-IV, revised 2002 • Acute confusional state • Disturbance of consciousness (i. e. , reduced clarity of awareness of the environment) with reduced ability to focus, sustain or shift attention • Change in cognition not better accounted for by a preexisting, established or evolving dementia • Develops over a short period of time, and fluctuates during the course of the day • the disturbance is caused by the direct physiological consequences of a general medical condition. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4 th Edition, Text Revision. 2002
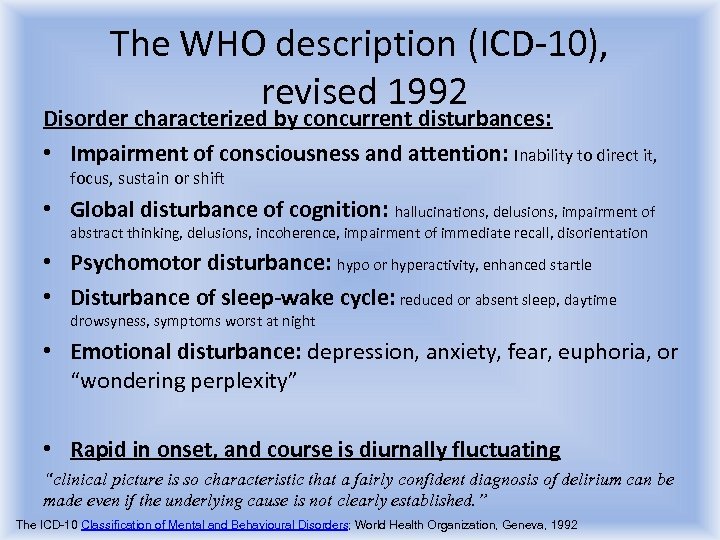 The WHO description (ICD-10), revised 1992 Disorder characterized by concurrent disturbances: • Impairment of consciousness and attention: Inability to direct it, focus, sustain or shift • Global disturbance of cognition: hallucinations, delusions, impairment of abstract thinking, delusions, incoherence, impairment of immediate recall, disorientation • Psychomotor disturbance: hypo or hyperactivity, enhanced startle • Disturbance of sleep-wake cycle: reduced or absent sleep, daytime drowsyness, symptoms worst at night • Emotional disturbance: depression, anxiety, fear, euphoria, or “wondering perplexity” • Rapid in onset, and course is diurnally fluctuating “clinical picture is so characteristic that a fairly confident diagnosis of delirium can be made even if the underlying cause is not clearly established. ” The ICD-10 Classification of Mental and Behavioural Disorders; World Health Organization, Geneva, 1992
The WHO description (ICD-10), revised 1992 Disorder characterized by concurrent disturbances: • Impairment of consciousness and attention: Inability to direct it, focus, sustain or shift • Global disturbance of cognition: hallucinations, delusions, impairment of abstract thinking, delusions, incoherence, impairment of immediate recall, disorientation • Psychomotor disturbance: hypo or hyperactivity, enhanced startle • Disturbance of sleep-wake cycle: reduced or absent sleep, daytime drowsyness, symptoms worst at night • Emotional disturbance: depression, anxiety, fear, euphoria, or “wondering perplexity” • Rapid in onset, and course is diurnally fluctuating “clinical picture is so characteristic that a fairly confident diagnosis of delirium can be made even if the underlying cause is not clearly established. ” The ICD-10 Classification of Mental and Behavioural Disorders; World Health Organization, Geneva, 1992
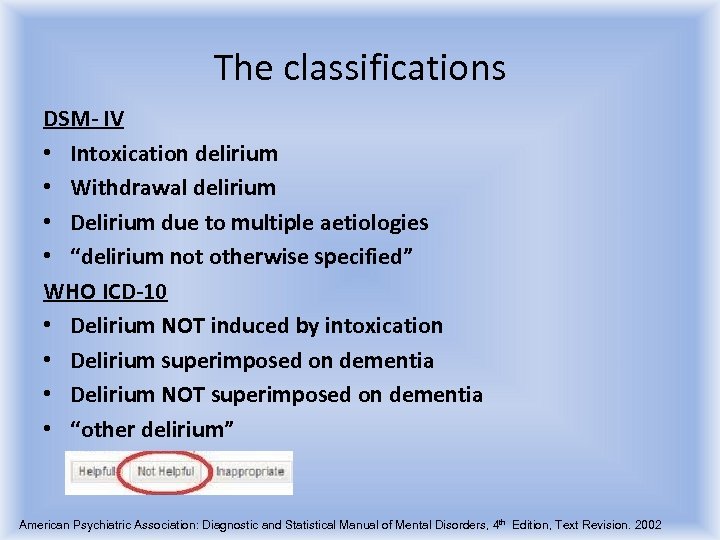 The classifications DSM- IV • Intoxication delirium • Withdrawal delirium • Delirium due to multiple aetiologies • “delirium not otherwise specified” WHO ICD-10 • Delirium NOT induced by intoxication • Delirium superimposed on dementia • Delirium NOT superimposed on dementia • “other delirium” American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4 th Edition, Text Revision. 2002
The classifications DSM- IV • Intoxication delirium • Withdrawal delirium • Delirium due to multiple aetiologies • “delirium not otherwise specified” WHO ICD-10 • Delirium NOT induced by intoxication • Delirium superimposed on dementia • Delirium NOT superimposed on dementia • “other delirium” American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4 th Edition, Text Revision. 2002
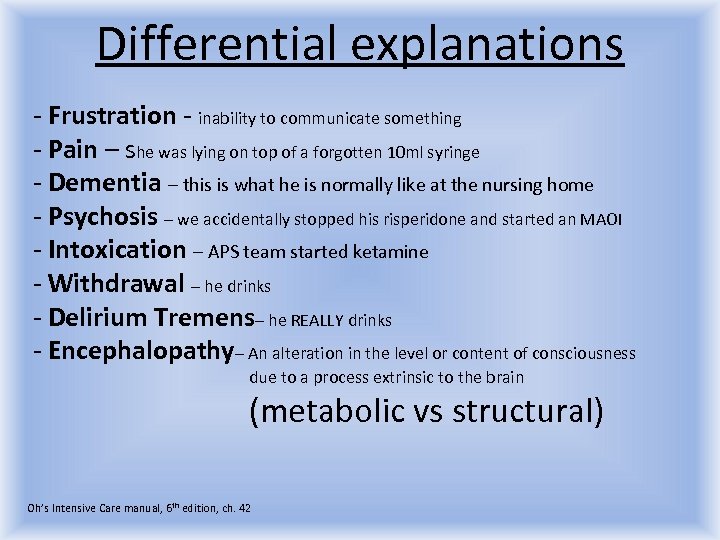 Differential explanations - Frustration - inability to communicate something - Pain – she was lying on top of a forgotten 10 ml syringe - Dementia – this is what he is normally like at the nursing home - Psychosis – we accidentally stopped his risperidone and started an MAOI - Intoxication – APS team started ketamine - Withdrawal – he drinks - Delirium Tremens– he REALLY drinks - Encephalopathy– An alteration in the level or content of consciousness due to a process extrinsic to the brain (metabolic vs structural) Oh’s Intensive Care manual, 6 th edition, ch. 42
Differential explanations - Frustration - inability to communicate something - Pain – she was lying on top of a forgotten 10 ml syringe - Dementia – this is what he is normally like at the nursing home - Psychosis – we accidentally stopped his risperidone and started an MAOI - Intoxication – APS team started ketamine - Withdrawal – he drinks - Delirium Tremens– he REALLY drinks - Encephalopathy– An alteration in the level or content of consciousness due to a process extrinsic to the brain (metabolic vs structural) Oh’s Intensive Care manual, 6 th edition, ch. 42
 A moment for Encephalopathy -ICU DELIRIUM …also… -Sepsis -Hepatic failure -Renal Failure -Hypoxia or hypercapnea -Hyper or hyponatremia -Hyper or hypoglycaemia -Hyper or hypothyroidism -Acidosis -Addisonian crisis…………………. . many others Oh’s Intensive Care manual, 6 th edition, ch. 42
A moment for Encephalopathy -ICU DELIRIUM …also… -Sepsis -Hepatic failure -Renal Failure -Hypoxia or hypercapnea -Hyper or hyponatremia -Hyper or hypoglycaemia -Hyper or hypothyroidism -Acidosis -Addisonian crisis…………………. . many others Oh’s Intensive Care manual, 6 th edition, ch. 42
 ICU Delirium - so, it’s the 5 th-7 th day of your admission. Or you are the night reg and its your 5 th - 7 th night shift - You havent slept Your circadian rhythm is disturbed You are full of mind-altering drugs You are constantly uncomfortable Your environment is noisy Your day is monotonous -Diagnosis of exclusion Oh’s Intensive Care manual, 6 th edition, ch. 42
ICU Delirium - so, it’s the 5 th-7 th day of your admission. Or you are the night reg and its your 5 th - 7 th night shift - You havent slept Your circadian rhythm is disturbed You are full of mind-altering drugs You are constantly uncomfortable Your environment is noisy Your day is monotonous -Diagnosis of exclusion Oh’s Intensive Care manual, 6 th edition, ch. 42
 Why is this a problem? -Irritates the nurse and doctor -Staff may get attacked -Tubes and lines get dislodged - damage to the patient and to the budget -Total tissue oxygen consumption increases -Quality of monitoring is compromised -Duration of stay is increased -Extubation is delayed (bolusbolus) - Higher incidence of nosocomial pneumonia (aspiration or otherwise) GL Fraser, RR Riker The frequency and cost of patient-initiated device removal in the ICU, - Pharmacotherapy, 2001 vol 21 issue 1 Pun BT, et al The importance of diagnosing and managing ICU delirium Chest. 2007 Aug; 132(2): 624 -36. Pandharipande P, Delirium: acute cognitive dysfunction in the critically ill Curr Opin Crit Care. 2005 Aug; 11(4): 360 -8. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141
Why is this a problem? -Irritates the nurse and doctor -Staff may get attacked -Tubes and lines get dislodged - damage to the patient and to the budget -Total tissue oxygen consumption increases -Quality of monitoring is compromised -Duration of stay is increased -Extubation is delayed (bolusbolus) - Higher incidence of nosocomial pneumonia (aspiration or otherwise) GL Fraser, RR Riker The frequency and cost of patient-initiated device removal in the ICU, - Pharmacotherapy, 2001 vol 21 issue 1 Pun BT, et al The importance of diagnosing and managing ICU delirium Chest. 2007 Aug; 132(2): 624 -36. Pandharipande P, Delirium: acute cognitive dysfunction in the critically ill Curr Opin Crit Care. 2005 Aug; 11(4): 360 -8. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141
 How much of a problem is this? Prevalence between 30% and 80% Delirium is an independent predictor of -Increased mortality at 6 months (3. 2 HR, hazard ratio) -Increased length of stay (HR 2. 0) - In some studies, strongest independent determinant of length of stay Equivalent to organ failure ! In comparison, ARF in ICU = HR 4. 9 Weirdly, aggressive delirium has a better prognosis than “quiet” delirium Increased cost of care: - In some studies, cost increased by 39% ICU costs, 31% higher total hospital costs - From medical device removal alone, 1997 annual cost to one American 42 -bed ICU was $ 250, 000 ( = $351, 968 adjusted for inflation) ; GL Fraser, RR Riker The frequency and cost of patient-initiated device removal in the ICU, - Pharmacotherapy, 2001 vol 21 issue 1 Wesley Ely et al. Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit JAMA. 2004; 291(14): 1753 -1762 Ely et. al, The impact of delirium in the intensive care unit on hospital length of stay. INTENSIVE CARE MEDICINE Volume 27, Number 12, 1892 -1900 Pandharipande P, Delirium: acute cognitive dysfunction in the critically ill Curr Opin Crit Care. 2005 Aug; 11(4): 360 -8. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 http: //www. mc. vanderbilt. edu/icudelirium/index. html Milbrandt et. al, Costs associated with delirium in mechanically ventilated patients Critical Care Medicine: April 2004 - Volume 32 - Issue 4 - pp 955 -962 http: //www. usinflationcalculator. com/
How much of a problem is this? Prevalence between 30% and 80% Delirium is an independent predictor of -Increased mortality at 6 months (3. 2 HR, hazard ratio) -Increased length of stay (HR 2. 0) - In some studies, strongest independent determinant of length of stay Equivalent to organ failure ! In comparison, ARF in ICU = HR 4. 9 Weirdly, aggressive delirium has a better prognosis than “quiet” delirium Increased cost of care: - In some studies, cost increased by 39% ICU costs, 31% higher total hospital costs - From medical device removal alone, 1997 annual cost to one American 42 -bed ICU was $ 250, 000 ( = $351, 968 adjusted for inflation) ; GL Fraser, RR Riker The frequency and cost of patient-initiated device removal in the ICU, - Pharmacotherapy, 2001 vol 21 issue 1 Wesley Ely et al. Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit JAMA. 2004; 291(14): 1753 -1762 Ely et. al, The impact of delirium in the intensive care unit on hospital length of stay. INTENSIVE CARE MEDICINE Volume 27, Number 12, 1892 -1900 Pandharipande P, Delirium: acute cognitive dysfunction in the critically ill Curr Opin Crit Care. 2005 Aug; 11(4): 360 -8. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 http: //www. mc. vanderbilt. edu/icudelirium/index. html Milbrandt et. al, Costs associated with delirium in mechanically ventilated patients Critical Care Medicine: April 2004 - Volume 32 - Issue 4 - pp 955 -962 http: //www. usinflationcalculator. com/
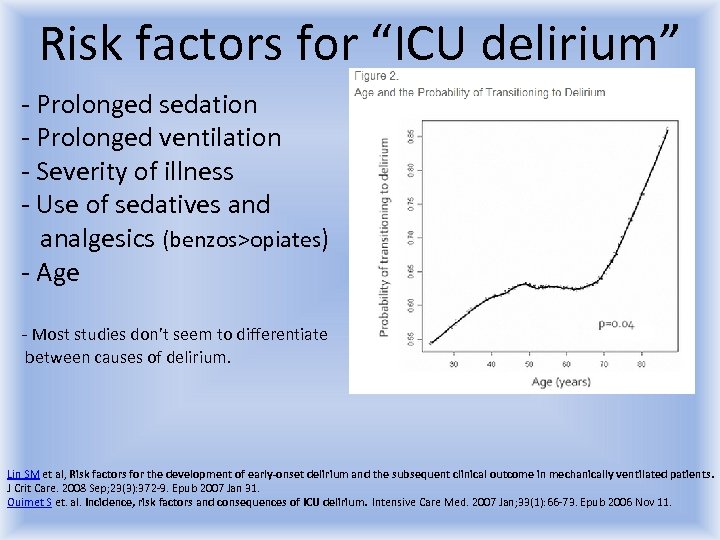 Risk factors for “ICU delirium” - Prolonged sedation - Prolonged ventilation - Severity of illness - Use of sedatives and analgesics (benzos>opiates) - Age - Most studies don’t seem to differentiate between causes of delirium. Lin SM et al, Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care. 2008 Sep; 23(3): 372 -9. Epub 2007 Jan 31. Ouimet S et. al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007 Jan; 33(1): 66 -73. Epub 2006 Nov 11.
Risk factors for “ICU delirium” - Prolonged sedation - Prolonged ventilation - Severity of illness - Use of sedatives and analgesics (benzos>opiates) - Age - Most studies don’t seem to differentiate between causes of delirium. Lin SM et al, Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care. 2008 Sep; 23(3): 372 -9. Epub 2007 Jan 31. Ouimet S et. al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007 Jan; 33(1): 66 -73. Epub 2006 Nov 11.
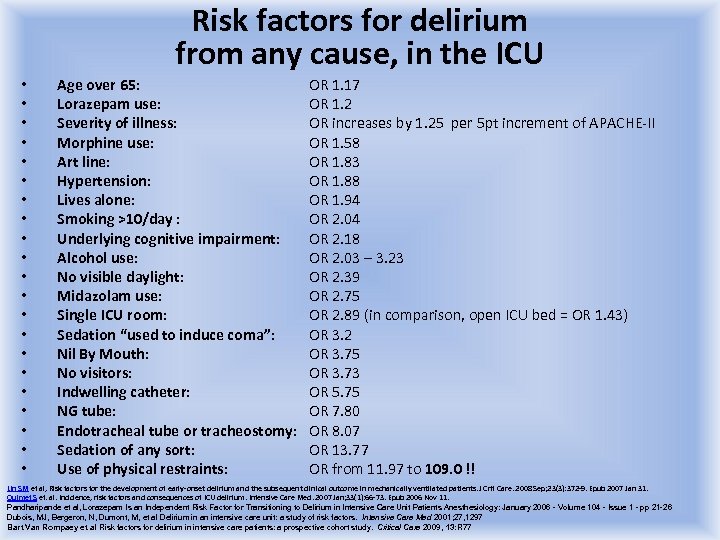 Risk factors for delirium from any cause, in the ICU • • • • • • Age over 65: Lorazepam use: Severity of illness: Morphine use: Art line: Hypertension: Lives alone: Smoking >10/day : Underlying cognitive impairment: Alcohol use: No visible daylight: Midazolam use: Single ICU room: Sedation “used to induce coma”: Nil By Mouth: No visitors: Indwelling catheter: NG tube: Endotracheal tube or tracheostomy: Sedation of any sort: Use of physical restraints: OR 1. 17 OR 1. 2 OR increases by 1. 25 per 5 pt increment of APACHE-II OR 1. 58 OR 1. 83 OR 1. 88 OR 1. 94 OR 2. 04 OR 2. 18 OR 2. 03 – 3. 23 OR 2. 39 OR 2. 75 OR 2. 89 (in comparison, open ICU bed = OR 1. 43) OR 3. 2 OR 3. 75 OR 3. 73 OR 5. 75 OR 7. 80 OR 8. 07 OR 13. 77 OR from 11. 97 to 109. 0 !! Lin SM et al, Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care. 2008 Sep; 23(3): 372 -9. Epub 2007 Jan 31. Ouimet S et. al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007 Jan; 33(1): 66 -73. Epub 2006 Nov 11. Pandharipande et al, Lorazepam Is an Independent Risk Factor for Transitioning to Delirium in Intensive Care Unit Patients Anesthesiology: January 2006 - Volume 104 - Issue 1 - pp 21 -26 Dubois, MJ, Bergeron, N, Dumont, M, et al Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 2001; 27, 1297 Bart Van Rompaey et al Risk factors for delirium in intensive care patients: a prospective cohort study. Critical Care 2009, 13: R 77
Risk factors for delirium from any cause, in the ICU • • • • • • Age over 65: Lorazepam use: Severity of illness: Morphine use: Art line: Hypertension: Lives alone: Smoking >10/day : Underlying cognitive impairment: Alcohol use: No visible daylight: Midazolam use: Single ICU room: Sedation “used to induce coma”: Nil By Mouth: No visitors: Indwelling catheter: NG tube: Endotracheal tube or tracheostomy: Sedation of any sort: Use of physical restraints: OR 1. 17 OR 1. 2 OR increases by 1. 25 per 5 pt increment of APACHE-II OR 1. 58 OR 1. 83 OR 1. 88 OR 1. 94 OR 2. 04 OR 2. 18 OR 2. 03 – 3. 23 OR 2. 39 OR 2. 75 OR 2. 89 (in comparison, open ICU bed = OR 1. 43) OR 3. 2 OR 3. 75 OR 3. 73 OR 5. 75 OR 7. 80 OR 8. 07 OR 13. 77 OR from 11. 97 to 109. 0 !! Lin SM et al, Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care. 2008 Sep; 23(3): 372 -9. Epub 2007 Jan 31. Ouimet S et. al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med. 2007 Jan; 33(1): 66 -73. Epub 2006 Nov 11. Pandharipande et al, Lorazepam Is an Independent Risk Factor for Transitioning to Delirium in Intensive Care Unit Patients Anesthesiology: January 2006 - Volume 104 - Issue 1 - pp 21 -26 Dubois, MJ, Bergeron, N, Dumont, M, et al Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 2001; 27, 1297 Bart Van Rompaey et al Risk factors for delirium in intensive care patients: a prospective cohort study. Critical Care 2009, 13: R 77
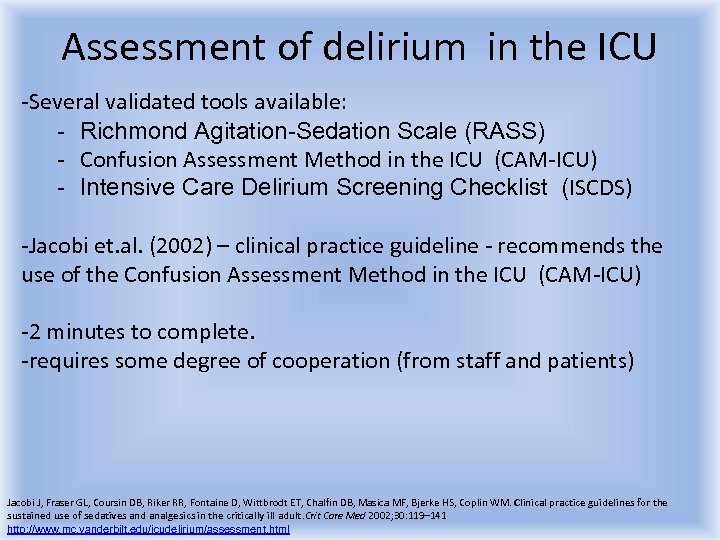 Assessment of delirium in the ICU -Several validated tools available: - Richmond Agitation-Sedation Scale (RASS) - Confusion Assessment Method in the ICU (CAM-ICU) - Intensive Care Delirium Screening Checklist (ISCDS) -Jacobi et. al. (2002) – clinical practice guideline - recommends the use of the Confusion Assessment Method in the ICU (CAM-ICU) -2 minutes to complete. -requires some degree of cooperation (from staff and patients) Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 http: //www. mc. vanderbilt. edu/icudelirium/assessment. html
Assessment of delirium in the ICU -Several validated tools available: - Richmond Agitation-Sedation Scale (RASS) - Confusion Assessment Method in the ICU (CAM-ICU) - Intensive Care Delirium Screening Checklist (ISCDS) -Jacobi et. al. (2002) – clinical practice guideline - recommends the use of the Confusion Assessment Method in the ICU (CAM-ICU) -2 minutes to complete. -requires some degree of cooperation (from staff and patients) Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 http: //www. mc. vanderbilt. edu/icudelirium/assessment. html
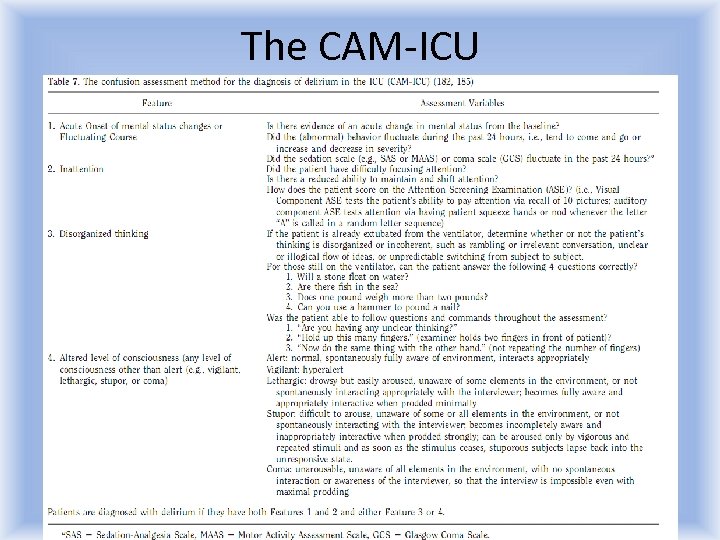 The CAM-ICU
The CAM-ICU
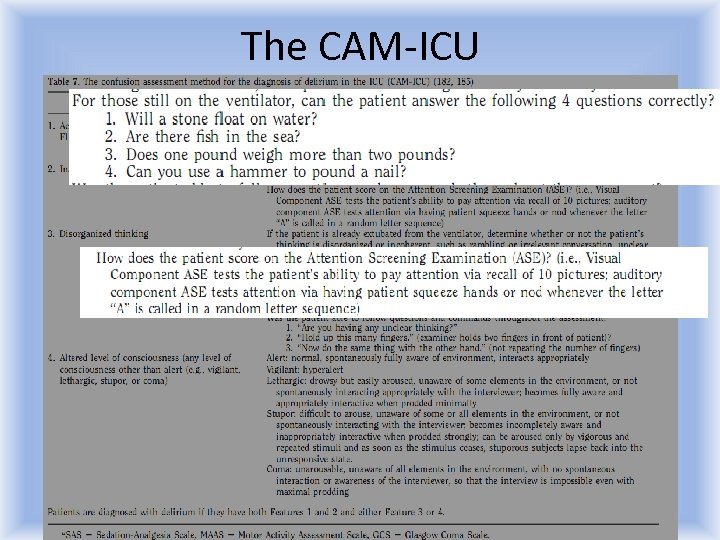 The CAM-ICU
The CAM-ICU
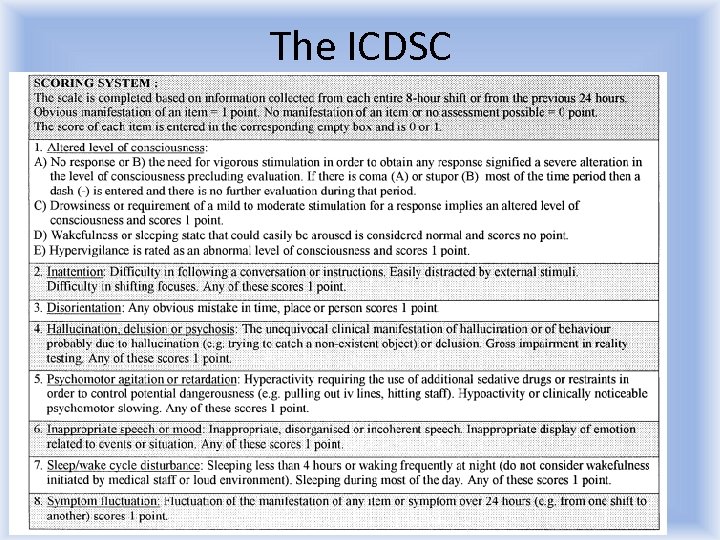 The ICDSC
The ICDSC
 Monitoring for delirium - Frequent reproducible assessment for pain and delirium -Jacobi et a. (2002, multidisciplinary task force) -recommend the use of a validated agitation/sedation measurement tool Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176.
Monitoring for delirium - Frequent reproducible assessment for pain and delirium -Jacobi et a. (2002, multidisciplinary task force) -recommend the use of a validated agitation/sedation measurement tool Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176.
 Delirium in the Australian ICU According to a 2008 survey, only 9% of all Australian units use any sort of delirium scale. In a snapshot survey, midazolam and propofol were the most frequently used sedatives Delirium was found in 21% of assessable patients. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8.
Delirium in the Australian ICU According to a 2008 survey, only 9% of all Australian units use any sort of delirium scale. In a snapshot survey, midazolam and propofol were the most frequently used sedatives Delirium was found in 21% of assessable patients. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8.
 Just calm down, Sir. You are in hospital. MANAGEMENT OF ICU DELIRIUM: -Preventative vs. reactive -Non-pharmacological vs pharmacological
Just calm down, Sir. You are in hospital. MANAGEMENT OF ICU DELIRIUM: -Preventative vs. reactive -Non-pharmacological vs pharmacological
 Prevention of ICU delirium -Mostly non-pharmacological measures -Mostly involving changes in the behaviour of the nurse and the intensivist, not the patient. -Mostly financially inexpensive -Mostly requiring greater effort than ad-hoc pharmacological interventions .
Prevention of ICU delirium -Mostly non-pharmacological measures -Mostly involving changes in the behaviour of the nurse and the intensivist, not the patient. -Mostly financially inexpensive -Mostly requiring greater effort than ad-hoc pharmacological interventions .
 Sedation holidays - Sedation Holidays -2000 study by Kress: landmark paper; 128 pts; -length of stay reduced from 9. 9 to 6. 6 days -9 vs 16 pts needed delirium workup -According to a 2008 survey, only 30% of Australian units use sedation holidays -According to the same survey, in a snapshot of 23 level III ICUs only 10% of patients have had the sedation turned off in the preceding 12 hr period Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. .
Sedation holidays - Sedation Holidays -2000 study by Kress: landmark paper; 128 pts; -length of stay reduced from 9. 9 to 6. 6 days -9 vs 16 pts needed delirium workup -According to a 2008 survey, only 30% of Australian units use sedation holidays -According to the same survey, in a snapshot of 23 level III ICUs only 10% of patients have had the sedation turned off in the preceding 12 hr period Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. .
 Quiet environment -EPA recommends a noise level below 45 d. B during the day and 35 d. B at night -ICUs have a mean 84 d. B -Patient survey: 203 survivors report nursing conversation and monitor alarms as the most irritating source of noise - noise levels in ICU have remained essentially unchanged despite advances in unit design -Seems as if white noise is preferred to intermittent noises Kahn DM, Cook TE, Carlisle CC, et al: Identification and modifi cation of environmental noise in an ICU setting. Chest 114: 535– 540, 199 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Christensen, 2007: Noise levels in a general intensive care unit: a descriptive study Nursing in Critical Care Volume 12, Issue 4, pages 188– 197,
Quiet environment -EPA recommends a noise level below 45 d. B during the day and 35 d. B at night -ICUs have a mean 84 d. B -Patient survey: 203 survivors report nursing conversation and monitor alarms as the most irritating source of noise - noise levels in ICU have remained essentially unchanged despite advances in unit design -Seems as if white noise is preferred to intermittent noises Kahn DM, Cook TE, Carlisle CC, et al: Identification and modifi cation of environmental noise in an ICU setting. Chest 114: 535– 540, 199 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Christensen, 2007: Noise levels in a general intensive care unit: a descriptive study Nursing in Critical Care Volume 12, Issue 4, pages 188– 197,
 Music -Chlan (1998)- statistically significant fall in blood pressure in ICU patients exposed to music picked by their families. -Decreases postoperative confusion outside the ICU in ortho geries patients -No studies of music as preventative or curative of delirium in ICU population -Most published work is an authors’ opinion. No trials. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176. Ruth M. et al, The effect of music listening on acute confusion and delirium in elders undergoing elective hip and knee surgery. J Clin Nurs. 2004 Sep; 13(6 B): 91 -6. Guzzetta CE: Effects of relaxation and music therapy on patients in a coronary care unit with presumptive acute myocardial infarction. Heart Lung 18(6): 609– 616, 1989 Byers JF, Smyth KA: Effect of a music intervention on noise annoyance, heart rate, and blood pressure in cardiac surgery patients. Am J Crit Care 6: 183– 191, 199
Music -Chlan (1998)- statistically significant fall in blood pressure in ICU patients exposed to music picked by their families. -Decreases postoperative confusion outside the ICU in ortho geries patients -No studies of music as preventative or curative of delirium in ICU population -Most published work is an authors’ opinion. No trials. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176. Ruth M. et al, The effect of music listening on acute confusion and delirium in elders undergoing elective hip and knee surgery. J Clin Nurs. 2004 Sep; 13(6 B): 91 -6. Guzzetta CE: Effects of relaxation and music therapy on patients in a coronary care unit with presumptive acute myocardial infarction. Heart Lung 18(6): 609– 616, 1989 Byers JF, Smyth KA: Effect of a music intervention on noise annoyance, heart rate, and blood pressure in cardiac surgery patients. Am J Crit Care 6: 183– 191, 199
 Diurnal rhythm, a good sleep -As part of a multicomponent strategy, nonpharmacological sleep pattern maintenance decreased incidence of delirium in elderly hospitalized patients from 15. 5 to 9. 9% Influence of sleep on delirium is not well studies in the ICU population ICU patients on average sleep ~ 2 hrs per day (as per polysomnography), but we tend to think that they sleep more. Propofol coma is not sleep for the purpose of rest. Rong-Fang Hu et al, 2009. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane database. (protocol in progress) Gerald L Weinhous et al. , Bench-to-bedside review: Delirium in ICU patients – importance of sleep deprivation Critical Care 2009, 13: 234 Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L: A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999, 340: 669 -676 Ely EW, Inouye SK, Bernanrd GR et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). J Am Med Assoc 2001; 286: 2703 -10 Mundigler G, Delle-Karth G, Koreny M, et al: Impaired circadian rhythm of melatonin secretion in sedated critically ill patients with severe sepsis. Crit Care Med 30: 536– 540, 2002 Edwards GB, Schuring LM: Pilot study: Validating staff nurses’ observations of sleep and wake states among critically ill patients using polysomnography. Am J Crit Care 2: 125– 131, 1993
Diurnal rhythm, a good sleep -As part of a multicomponent strategy, nonpharmacological sleep pattern maintenance decreased incidence of delirium in elderly hospitalized patients from 15. 5 to 9. 9% Influence of sleep on delirium is not well studies in the ICU population ICU patients on average sleep ~ 2 hrs per day (as per polysomnography), but we tend to think that they sleep more. Propofol coma is not sleep for the purpose of rest. Rong-Fang Hu et al, 2009. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane database. (protocol in progress) Gerald L Weinhous et al. , Bench-to-bedside review: Delirium in ICU patients – importance of sleep deprivation Critical Care 2009, 13: 234 Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L: A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999, 340: 669 -676 Ely EW, Inouye SK, Bernanrd GR et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). J Am Med Assoc 2001; 286: 2703 -10 Mundigler G, Delle-Karth G, Koreny M, et al: Impaired circadian rhythm of melatonin secretion in sedated critically ill patients with severe sepsis. Crit Care Med 30: 536– 540, 2002 Edwards GB, Schuring LM: Pilot study: Validating staff nurses’ observations of sleep and wake states among critically ill patients using polysomnography. Am J Crit Care 2: 125– 131, 1993
 Increased family presence - OR of delirium in unvisited patients is 3 times greater in one particular study which measured this. - No good scientific reason to restrict visitor presence - Presently, no solid evidence of benefit either. Tullman DF, Dracup K: Creating a healing environment for elders. AACN Clin Issues 11(1): 34– 50, 2000 Bart Van Rompaey et al Risk factors for delirium in intensive care patients: a prospective cohort study. Critical Care 2009, 13: R 77
Increased family presence - OR of delirium in unvisited patients is 3 times greater in one particular study which measured this. - No good scientific reason to restrict visitor presence - Presently, no solid evidence of benefit either. Tullman DF, Dracup K: Creating a healing environment for elders. AACN Clin Issues 11(1): 34– 50, 2000 Bart Van Rompaey et al Risk factors for delirium in intensive care patients: a prospective cohort study. Critical Care 2009, 13: R 77
 Increased medical presence -Does a daily visit from a geriatrician prevent delirium? - Marcantonio (2001) – orthopedic geries patients - Daily geriatrician review vs. management by the ortho team …. . The geriatrician was limited by study protocol to only making five recommendations per visit. Areas of recommendation were of the following nature: • maintain CNS oxygen delivery • Treat severe pain • Eliminate unnecessary medications • Appropriate environmental stimuli • Bladder/bowel control CAM measurements were performed. -Yes it does. NNT = 6. OR 0. 48. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. Journal-of-the-American-Geriatrics. Society 2001; 49(5): 516 -22
Increased medical presence -Does a daily visit from a geriatrician prevent delirium? - Marcantonio (2001) – orthopedic geries patients - Daily geriatrician review vs. management by the ortho team …. . The geriatrician was limited by study protocol to only making five recommendations per visit. Areas of recommendation were of the following nature: • maintain CNS oxygen delivery • Treat severe pain • Eliminate unnecessary medications • Appropriate environmental stimuli • Bladder/bowel control CAM measurements were performed. -Yes it does. NNT = 6. OR 0. 48. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. Journal-of-the-American-Geriatrics. Society 2001; 49(5): 516 -22
 Thiamine well established role in prevention of Wernicke’s encephalopathy - effect of thiamine deficinecy on astrocytes - change in glutamate uptake results in excitotoxicity - early stages are reversible Non-specific delirium? Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176.
Thiamine well established role in prevention of Wernicke’s encephalopathy - effect of thiamine deficinecy on astrocytes - change in glutamate uptake results in excitotoxicity - early stages are reversible Non-specific delirium? Kress JP, Pohlman AS, O'Conner MF, et al. Daily interruption of sedation infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471– 7 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Freedman NS et al. , Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155– 1162 Shehabi Y, Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Botha JA, Boyle MS, Ernest D, Freebairn RC, Jenkins IR, Roberts BL, Seppelt IM. Anaesth Intensive Care. 2008 Jul; 36(4): 570 -8. Chlan L: Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998; 27: 169– 176.
 Pharmacological prophylaxis for Prevention of ICU delirium: - Siddiqi et al. (2009): Cochrane meta-analysis Interventions for preventing delirium in hospitalised patients Salient findings: - Aizawa (2002): post-op geries in ICU. “delirium-free protocol” - Control sleep cycle with diazepam and pethidine. OR of delirium = 0. 10. - But, no difference in length of admission. - Bergren (1987): halothane vs epidural for #NOF geries. No difference in delirium. - Diaz (2001): citicoline (nootrope) vs placebo for post-op geries. No difference. - Kalisvaart (2005): haloperidol prophylactically, ortho geries. No difference. - Liptzin (2005): donepezil(Ach-ase inhibitor), post op geries. No difference. . Siddiqi N, Holt R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No. : CD 005563.
Pharmacological prophylaxis for Prevention of ICU delirium: - Siddiqi et al. (2009): Cochrane meta-analysis Interventions for preventing delirium in hospitalised patients Salient findings: - Aizawa (2002): post-op geries in ICU. “delirium-free protocol” - Control sleep cycle with diazepam and pethidine. OR of delirium = 0. 10. - But, no difference in length of admission. - Bergren (1987): halothane vs epidural for #NOF geries. No difference in delirium. - Diaz (2001): citicoline (nootrope) vs placebo for post-op geries. No difference. - Kalisvaart (2005): haloperidol prophylactically, ortho geries. No difference. - Liptzin (2005): donepezil(Ach-ase inhibitor), post op geries. No difference. . Siddiqi N, Holt R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No. : CD 005563.
 The path less travelled - CORRECT MAGNESIUM. -63 pts, 2009 RCT by Esen et al. : target 1. 0 -2. 0, in addition to remi + midaz: -Of the delirious pts, the magnesium group had fewer days of delirium (55% vs 89%) and needed less sedation Desired RASS score was reached at a lower dose, and maintained for longer. -That is the only such study -Previously, magnesium has also been used in the treatment of delirium tremens – subsequently falling out of favour Esen F et. al. Effect of magnesium on the incidence of delirium occurrence in the ICU Critical Care 2009 vol 13 supp 1 P 412 Beroz et al, PARENTERAL MAGNESIUM IN THE PROPHYLAXIS AND TREATMENT OF DELIRIUM TREMENS Am J Psychiatry 118: 1042 -1043, May 1962 Jermain DM; Controversies over the use of magnesium sulfate in delirium tremens. Ann Pharmacother. 1992 May; 26(5): 650 -2. b
The path less travelled - CORRECT MAGNESIUM. -63 pts, 2009 RCT by Esen et al. : target 1. 0 -2. 0, in addition to remi + midaz: -Of the delirious pts, the magnesium group had fewer days of delirium (55% vs 89%) and needed less sedation Desired RASS score was reached at a lower dose, and maintained for longer. -That is the only such study -Previously, magnesium has also been used in the treatment of delirium tremens – subsequently falling out of favour Esen F et. al. Effect of magnesium on the incidence of delirium occurrence in the ICU Critical Care 2009 vol 13 supp 1 P 412 Beroz et al, PARENTERAL MAGNESIUM IN THE PROPHYLAXIS AND TREATMENT OF DELIRIUM TREMENS Am J Psychiatry 118: 1042 -1043, May 1962 Jermain DM; Controversies over the use of magnesium sulfate in delirium tremens. Ann Pharmacother. 1992 May; 26(5): 650 -2. b
 Pharmacological Arsenal - Benzodiazepines - Opiates - Classical antipsychotics - Atypical antipsychotics - Cholinergic drugs - Dexmedetomidine / clonidine
Pharmacological Arsenal - Benzodiazepines - Opiates - Classical antipsychotics - Atypical antipsychotics - Cholinergic drugs - Dexmedetomidine / clonidine
 Choice of chemical restraints Cochrane contributions: - Benzodiazepines for delirium - Antipsychotics for delirium - Cholinesterase inhibitors for delirium Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
Choice of chemical restraints Cochrane contributions: - Benzodiazepines for delirium - Antipsychotics for delirium - Cholinesterase inhibitors for delirium Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
 Benzodiazepines -Cochrane: - only one trial fit their criteria, lorazepam vs. dexmedetomidine. -Authors conclusion: dex is better. -Recommendations: no evidence to support use of benzodiazepines outside of alcohol or benzo withdrawal-related delirium -In all other settings, benzodiazepines are found to be either ineffective or harmful (i. e. increase incidence of delirium) Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4
Benzodiazepines -Cochrane: - only one trial fit their criteria, lorazepam vs. dexmedetomidine. -Authors conclusion: dex is better. -Recommendations: no evidence to support use of benzodiazepines outside of alcohol or benzo withdrawal-related delirium -In all other settings, benzodiazepines are found to be either ineffective or harmful (i. e. increase incidence of delirium) Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4
 Opioids -Consensus is that they contribute more to generate delirium. -Limited role for delirium in general -Specific aetiologies: - delirium due to opioid withdrawal (controversial) - delirium due to severe pain Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Paintal et al, Management of Alcohol, Sedative-Hypnotic, and Opioid Withdrawal in the ICU PCCSU Article | 12. 01. 10.
Opioids -Consensus is that they contribute more to generate delirium. -Limited role for delirium in general -Specific aetiologies: - delirium due to opioid withdrawal (controversial) - delirium due to severe pain Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Paintal et al, Management of Alcohol, Sedative-Hypnotic, and Opioid Withdrawal in the ICU PCCSU Article | 12. 01. 10.
 Antipsychotics -? Is the patient actually psychotic? Nevermind. -There are so many! Which one? -Typical vs atypical -Which specific one to use? -Are there situations which might favour one over another? Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2009, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
Antipsychotics -? Is the patient actually psychotic? Nevermind. -There are so many! Which one? -Typical vs atypical -Which specific one to use? -Are there situations which might favour one over another? Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2009, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
 Classical antipsychotics: Haloperidol -Jacobi et al (2002) clinical practice guidelines recommend Haloperidol (level C data, small studies and case report series) -Cochrane library agrees to some extent: Lonergan et. al. (2007) compared haloperidol with risperidone and olanzapine Conclusion: haloperidol is better than placebo, but… - no better then atypical antipsychotics at low doses - still no better but with more side effects at high doses Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
Classical antipsychotics: Haloperidol -Jacobi et al (2002) clinical practice guidelines recommend Haloperidol (level C data, small studies and case report series) -Cochrane library agrees to some extent: Lonergan et. al. (2007) compared haloperidol with risperidone and olanzapine Conclusion: haloperidol is better than placebo, but… - no better then atypical antipsychotics at low doses - still no better but with more side effects at high doses Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
 Classical antipsychotics: Chlorpromazine -one double blind trial comparing it to lorazepam and haloperidol. -Not in an ICU setting (hospitalized AIDS patients) -- No treatment effect difference between haloperidol and chlorpromazine, but both were equally better than lorazepam. -Concern re. anticholinergic side effects. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Breitbart et al, A Double-Blind Trial of Haloperidol, Chlorpromazine, and Lorazepam in the Treatment of Delirium in Hospitalized AIDS Patients American Journal of Psychiatry 1996; 153: 231– 237
Classical antipsychotics: Chlorpromazine -one double blind trial comparing it to lorazepam and haloperidol. -Not in an ICU setting (hospitalized AIDS patients) -- No treatment effect difference between haloperidol and chlorpromazine, but both were equally better than lorazepam. -Concern re. anticholinergic side effects. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Breitbart et al, A Double-Blind Trial of Haloperidol, Chlorpromazine, and Lorazepam in the Treatment of Delirium in Hospitalized AIDS Patients American Journal of Psychiatry 1996; 153: 231– 237
 Atypical antipsychotics: -Olanzapine -Quetiapine -Risperidone -Aripiprazole -Amisulpride -Clozapine -Which is best? Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
Atypical antipsychotics: -Olanzapine -Quetiapine -Risperidone -Aripiprazole -Amisulpride -Clozapine -Which is best? Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Lonergan et. al. , Benzodiazepines for delirium. Cochrane Database of Systematic Reviews 2009, Issue 4 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Milbrandt et. al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005 Jan; 33(1): 226 -9; discussion 263 -5.
 Has anyone compared these drugs? …yes, but rarely, and on a small scale. -Kim et al (2010): risperidone vs olanzapine for delirium -32 SUBJECTS ONLY. Median age 70. -No significant difference in response in the under-70 age group -Olanzapine response was better in the over-70 age group - Devlin et al: amisulpride vs quetiapine for delirium - No significant difference Kim et al, Risperidone versus olanzapine for the treatment of delirium. Hum Psychopharmacol. 2010 Jun; 25(4): 298 -302. Devlin JW et al: Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med 38: 419 -427, 2010 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Lee et al, Amisulpride versus quetiapine for the treatment of delirium: a randomized, open prospective study International Clinical Psychopharmacology: November 2005 - Volume 20 - Issue 6 - pp 311 -314
Has anyone compared these drugs? …yes, but rarely, and on a small scale. -Kim et al (2010): risperidone vs olanzapine for delirium -32 SUBJECTS ONLY. Median age 70. -No significant difference in response in the under-70 age group -Olanzapine response was better in the over-70 age group - Devlin et al: amisulpride vs quetiapine for delirium - No significant difference Kim et al, Risperidone versus olanzapine for the treatment of delirium. Hum Psychopharmacol. 2010 Jun; 25(4): 298 -302. Devlin JW et al: Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med 38: 419 -427, 2010 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Lee et al, Amisulpride versus quetiapine for the treatment of delirium: a randomized, open prospective study International Clinical Psychopharmacology: November 2005 - Volume 20 - Issue 6 - pp 311 -314
 Non-comparison studies - Devlin et al (2010): quetiapine vs placebo in ICU delirium - Doing something was 50% better than doing nothing. - 40% vs 90% delirium resolution by 3 rd day of treatment. - Straker et al (2006): aripiprazole vs placebo in general delirium - Suggests it may be a better choice than others because of minimal QTc effect - Lonergan et al (2009): -Cochrane review of antipsychotics in delirium -Insufficient data to differentiate between atypicals Kim et al, Risperidone versus olanzapine for the treatment of delirium. Hum Psychopharmacol. 2010 Jun; 25(4): 298 -302. Devlin JW et al: Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med 38: 419 -427, 2010 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Straker et al. Aripiprazole in the Treatment of Delirium Psychosomatics 47: 385 -391, September-October 2006
Non-comparison studies - Devlin et al (2010): quetiapine vs placebo in ICU delirium - Doing something was 50% better than doing nothing. - 40% vs 90% delirium resolution by 3 rd day of treatment. - Straker et al (2006): aripiprazole vs placebo in general delirium - Suggests it may be a better choice than others because of minimal QTc effect - Lonergan et al (2009): -Cochrane review of antipsychotics in delirium -Insufficient data to differentiate between atypicals Kim et al, Risperidone versus olanzapine for the treatment of delirium. Hum Psychopharmacol. 2010 Jun; 25(4): 298 -302. Devlin JW et al: Efficacy and safety of quetiapine in critically ill patients with delirium: A prospective, multicenter, randomized, double-blind, placebo-controlled pilot study. Crit Care Med 38: 419 -427, 2010 Lonergan E, Britton AM, Luxenberg J. Antipsychotics for delirium. Cochrane Database of Systematic Reviews 2007, Issue 2. Straker et al. Aripiprazole in the Treatment of Delirium Psychosomatics 47: 385 -391, September-October 2006
 Clonidine -No broad studies of clonidine in delirium. -Formerly, popular for delirium tremens and opioid withdrawal Rubino et al (2010) – cardiothoracic ICU patients post aortic dissection repair 30 pts, clonidine infusion vs placebo clonidine group weaned from ventilator faster, had lower delirium scores Verner et al (1990) – post Ivor Lewis patients from German ICUs …all of who were withdrawing from alcohol clonidine group had fewer “psychovegetative” symptoms Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Rubino et al. Impact of clonidine administration on delirium and related respiratory weaning after surgical correction of acute type-A aortic dissection: results of a pilot study. Interact Cardio. Vasc Thorac Surg 2010; 10: 58 -62 Verner et al, Clonidine supplemented analgesia and sedation in prevention of postoperative delirium Anasth Intensivther Notfallmed. 1990 Aug; 25(4): 274 -80. Gold et al, CLONIDINE BLOCKS ACUTE OPIATE-WITHDRAWAL SYMPTOMS The Lancet, Volume 312, Issue 8090, Pages 599 - 602, 16 September 1978
Clonidine -No broad studies of clonidine in delirium. -Formerly, popular for delirium tremens and opioid withdrawal Rubino et al (2010) – cardiothoracic ICU patients post aortic dissection repair 30 pts, clonidine infusion vs placebo clonidine group weaned from ventilator faster, had lower delirium scores Verner et al (1990) – post Ivor Lewis patients from German ICUs …all of who were withdrawing from alcohol clonidine group had fewer “psychovegetative” symptoms Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Rubino et al. Impact of clonidine administration on delirium and related respiratory weaning after surgical correction of acute type-A aortic dissection: results of a pilot study. Interact Cardio. Vasc Thorac Surg 2010; 10: 58 -62 Verner et al, Clonidine supplemented analgesia and sedation in prevention of postoperative delirium Anasth Intensivther Notfallmed. 1990 Aug; 25(4): 274 -80. Gold et al, CLONIDINE BLOCKS ACUTE OPIATE-WITHDRAWAL SYMPTOMS The Lancet, Volume 312, Issue 8090, Pages 599 - 602, 16 September 1978
 Dexmedetomidine -More to minimize development of delirium than relieve its symptoms? -Dex plus propofol? Ruokonen et al (2009): 87 pts; adding Dex has no effect on length of stay, but decreases length of ventilation. -Dex vs Midazolam? Riker et al (2009): 375 pts; prevalence of delirium 54%(dex) vs 76% (midaz), also faster extubation -Dex vs lorazepam? Pandharipande et al (2007): 106 pts; Dex group: median 7 days without delirium, vs 3 for lorazepam -Dex vs haloperidol? Reade et. al (2009) 20 pts in whom extubation was impossible because of delirium: = dex reduced mean time to extubation from 42 hrs to 20 hrs …haloperidol was given as an infusion (? ) Mirski et al, Cognitive improvement during continuous sedation in critically ill, awake and responsive patients: The Acute Neurological ICU Sedation Trial (ANIST) Intensive Care Medicine 2010 vol 36 issue 9 1505 -1513 Ruokonen et al. Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. Intensive Care Medicine 2009 vol 35 issue 2 282 -90 Riker RR, et al Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA : the journal of the American Medical Association 2009 Feb 301 issue 5 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Pandharipande et al, Effect of Sedation With Dexmedetomidine vs Lorazepam on Acute Brain Dysfunction in Mechanically Ventilated Patients- The MENDS Randomized Controlled Trial. JAMA. 2007; 298(22): 26442653 Reade et al. , Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial Critical Care 2009, 13: R 75
Dexmedetomidine -More to minimize development of delirium than relieve its symptoms? -Dex plus propofol? Ruokonen et al (2009): 87 pts; adding Dex has no effect on length of stay, but decreases length of ventilation. -Dex vs Midazolam? Riker et al (2009): 375 pts; prevalence of delirium 54%(dex) vs 76% (midaz), also faster extubation -Dex vs lorazepam? Pandharipande et al (2007): 106 pts; Dex group: median 7 days without delirium, vs 3 for lorazepam -Dex vs haloperidol? Reade et. al (2009) 20 pts in whom extubation was impossible because of delirium: = dex reduced mean time to extubation from 42 hrs to 20 hrs …haloperidol was given as an infusion (? ) Mirski et al, Cognitive improvement during continuous sedation in critically ill, awake and responsive patients: The Acute Neurological ICU Sedation Trial (ANIST) Intensive Care Medicine 2010 vol 36 issue 9 1505 -1513 Ruokonen et al. Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. Intensive Care Medicine 2009 vol 35 issue 2 282 -90 Riker RR, et al Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA : the journal of the American Medical Association 2009 Feb 301 issue 5 Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30: 119– 141 Pandharipande et al, Effect of Sedation With Dexmedetomidine vs Lorazepam on Acute Brain Dysfunction in Mechanically Ventilated Patients- The MENDS Randomized Controlled Trial. JAMA. 2007; 298(22): 26442653 Reade et al. , Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial Critical Care 2009, 13: R 75
 Acetylcholinesterase inhibitors -Cochrane dementia and cognitive improvement group: found lots of poor quality published work on -Donepezil -Galantamine -Rivastigmine -Tacrine -Only one trial met quailty criteria, -the already mentioned Liptzin (2005) ( donepezil not useful in preventing post-op delirium) Conclusion: cant recommend them. The exception: Physostigmine has a defined role to play in the narrow context of delirium due to anticholinergic poisoning Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database of Systematic Reviews 2008, Issue 1 Duvoisin et al, Reversal of Central Anticholinergic Syndrome in Man by Physostigmine. JAMA. 1968; 206(9): 1963 -1965 Burns et al. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning Annals of Emergency Medicine Volume 35, Issue 4 , Pages 374 -381, April 2000.
Acetylcholinesterase inhibitors -Cochrane dementia and cognitive improvement group: found lots of poor quality published work on -Donepezil -Galantamine -Rivastigmine -Tacrine -Only one trial met quailty criteria, -the already mentioned Liptzin (2005) ( donepezil not useful in preventing post-op delirium) Conclusion: cant recommend them. The exception: Physostigmine has a defined role to play in the narrow context of delirium due to anticholinergic poisoning Overshott R, Karim S, Burns A. Cholinesterase inhibitors for delirium. Cochrane Database of Systematic Reviews 2008, Issue 1 Duvoisin et al, Reversal of Central Anticholinergic Syndrome in Man by Physostigmine. JAMA. 1968; 206(9): 1963 -1965 Burns et al. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning Annals of Emergency Medicine Volume 35, Issue 4 , Pages 374 -381, April 2000.
 Physical restraints -NOT IDEAL. -Increases the risk of PTSD, tissue injury, pressure areas. Inhumane. -Increases risk of delirium!. . . -Consensus: use the least restrictive therapy available. -ACCCM task force (2001 -2002) recommends use of restrains be reviewed every 24 hours LY Chang, KWK Wang… Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study - American Journal of Critical Care, 2008 – AACN 2008; 17: 408 -415 George J. Annas, J. D. , M. P. H. The Last Resort — The Use of Physical Restraints in Medical Emergencies N Engl J Med 1999; 341: 1408 -141 Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med; 33: 978 -85 Macciolli et. al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 11 Carrion MI, Ayuso D, Marcos M, et al: Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 2000; 28: 63– 66 Tominaga GT, Rduzwick H, Scannell G, et al: Decreasing unplanned extubations in the surgical intensive care unit. Am J Surg 1995; 170: 586 – 590 Girard et. al, Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study Crit Care. 2007; 11(1): R 28. Minnick A, Leipzig RM, Johnson ME: Elderly patients’ reports of physical restraints experiences in intensive care units. Am J Crit Care 2001; 10: 168 – 171
Physical restraints -NOT IDEAL. -Increases the risk of PTSD, tissue injury, pressure areas. Inhumane. -Increases risk of delirium!. . . -Consensus: use the least restrictive therapy available. -ACCCM task force (2001 -2002) recommends use of restrains be reviewed every 24 hours LY Chang, KWK Wang… Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study - American Journal of Critical Care, 2008 – AACN 2008; 17: 408 -415 George J. Annas, J. D. , M. P. H. The Last Resort — The Use of Physical Restraints in Medical Emergencies N Engl J Med 1999; 341: 1408 -141 Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med; 33: 978 -85 Macciolli et. al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 11 Carrion MI, Ayuso D, Marcos M, et al: Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 2000; 28: 63– 66 Tominaga GT, Rduzwick H, Scannell G, et al: Decreasing unplanned extubations in the surgical intensive care unit. Am J Surg 1995; 170: 586 – 590 Girard et. al, Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study Crit Care. 2007; 11(1): R 28. Minnick A, Leipzig RM, Johnson ME: Elderly patients’ reports of physical restraints experiences in intensive care units. Am J Crit Care 2001; 10: 168 – 171
 An argument for safe restraints -Tominaga et. al (1995) – no restraints = significant increase in self-extubations -Carrion et al (2000) – hand restraints = significantly reduced self-extubations LY Chang, KWK Wang… Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study - American Journal of Critical Care, 2008 – AACN 2008; 17: 408 -415 George J. Annas, J. D. , M. P. H. The Last Resort — The Use of Physical Restraints in Medical Emergencies N Engl J Med 1999; 341: 1408 -141 Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med; 33: 978 -85 Macciolli et. al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 11 Carrion MI, Ayuso D, Marcos M, et al: Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 2000; 28: 63– 66 Tominaga GT, Rduzwick H, Scannell G, et al: Decreasing unplanned extubations in the surgical intensive care unit. Am J Surg 1995; 170: 586 – 590 Girard et. al, Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study Crit Care. 2007; 11(1): R 28. Maccioli et al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 1
An argument for safe restraints -Tominaga et. al (1995) – no restraints = significant increase in self-extubations -Carrion et al (2000) – hand restraints = significantly reduced self-extubations LY Chang, KWK Wang… Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study - American Journal of Critical Care, 2008 – AACN 2008; 17: 408 -415 George J. Annas, J. D. , M. P. H. The Last Resort — The Use of Physical Restraints in Medical Emergencies N Engl J Med 1999; 341: 1408 -141 Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. (2007) Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med; 33: 978 -85 Macciolli et. al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 11 Carrion MI, Ayuso D, Marcos M, et al: Accidental removal of endotracheal and nasogastric tubes and intravascular catheters. Crit Care Med 2000; 28: 63– 66 Tominaga GT, Rduzwick H, Scannell G, et al: Decreasing unplanned extubations in the surgical intensive care unit. Am J Surg 1995; 170: 586 – 590 Girard et. al, Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study Crit Care. 2007; 11(1): R 28. Maccioli et al, Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies—American College of Critical Care Medicine Task Force 2001– 2002 Crit Care Med 2003 Vol. 31, No. 1
 Question and answer time.
Question and answer time.


